Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(1); 2014 > Article
-
Original Article
P2X7 Receptor Expression in Coexistence of Papillary Thyroid Carcinoma with Hashimoto's Thyroiditis - Ji Hyun Kwon, Eun Sook Nam, Hyung Sik Shin, Seong Jin Cho, Hye Rim Park1, Mi Jung Kwon1
-
Korean Journal of Pathology 2014;48(1):30-35.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.30
Published online: February 25, 2014
Department of Pathology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, Seoul, Korea.
1Department of Pathology, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
-
Corresponding Authors: Eun Sook Nam, M.D. Department of Pathology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, 150 Seongan-ro, Gangdong-gu, Seoul 134-701, Korea. Tel: +82-2-2224-2349, Fax: +82-2-2224-2471, esnam@hallym.or.kr
Corresponding Authors: Hyung Sik Shin, M.D. Department of Pathology, Kangdong Sacred Heart Hospital, Hallym University College of Medicine, 150 Seongan-ro, Gangdong-gu, Seoul 134-701, Korea. Tel: +82-2-2224-2325, Fax: +82-2-2224-2471, shinn7064@hanmail.net
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- This study was aimed at investigating the relation of P2X7 receptor (P2X7R) expression with the clinicopathological features of papillary thyroid carcinoma (PTC) coexisting with Hashimoto's thyroiditis (HT).
-
Methods
- We examined 170 patients (84, PTC with HT; 86, PTC without HT). P2X7R expression was examined by immunohistochemical methods. The staining intensity and patterns were evaluated and scored using a semi-quantitative method.
-
Results
- The PTC with HT group was more likely to contain women and had less extrathyroid extension, lymph node (LN) metastasis, lymphovascular invasion, and recurrence than the PTC without HT group. Patients positive for P2X7R had significantly higher frequencies of lymphovascular invasion, extrathyroid extension, LN metastasis, and absence of HT. As shown by multivariate analysis, the expression of P2X7R was significantly higher if HT was absent and extrathyroid extension was present. In the PTC with HT group, the expression of P2X7R was significantly higher in patients with tumor multifocality, lymphovascular invasion, and extrathyroid extension. In the PTC without HT group, the expression of P2X7R was significantly higher in women and those having tumor multifocality.
-
Conclusions
- Coexistence of PTC with HT is associated with good prognostic factors, and P2X7R expression in PTC was correlated with poor prognostic factors and the absence of HT.
- Patients and tissue samples
- This study was conducted using formalin-fixed, paraffin-embedded tissue samples obtained from 170 PTC patients who underwent thyroid surgery at Kangdong Sacred Heart Hospital between January 2006 and December 2007. Among the 170 patients, 84 had available data including the preoperative serum thyroid autoantibodies and pathology reports for HT. HT was diagnosed on the basis of histological findings of diffuse lymphoplasmacytic infiltration with germinal centers, parenchymal atrophy with oncocytic change, and variable amounts of stromal fibrosis throughout the thyroid gland. Lymphovascular invasion was assessed with light microscopy and defined as tumor cells that were present within a vascular space with identification of endothelial lining.15 After histological review, PTC cases were categorized into two groups, PTC with HT (n=84) or PTC without HT (n=86). Clinical information including age, sex, treatment modality, and survival or recurrence was adapted from medical records and radiologic findings and then analyzed. All glass slides from 170 patients with PTC were reviewed by two pathologists for diagnosis confirmation and selection of a representative section for immunohistochemical study. Diagnosis and histologic differentiation were evaluated according to the World Health Organization classification, and tumor staging was based on the American Joint Committee on Cancer updated tumor-node-metastasis cancer staging system. This study was approved by Institutional Ethics Committee of Kangdong Sacred Heart Hospital Seoul, Korea.
- Tissue microarray block preparation
- After a case review for diagnostic confirmation, a tissue microarray was constructed. The largest definite tumor area was selected for the tissue microarray block. A circle was drawn on the slide around the most representative area. Using the slide as a guide, core samples were obtained from each paraffin-embedded block using a tissue microarray tool (Quick-Ray, Unitma, Seoul, Korea). A punch size 3 mm in diameter was used. Nine cores were embedded in each block in 3×3 arrangements. In total, 19 tissue microarray blocks were produced from the 170 tumor samples.
- Immunohistochemistry
- The 4-µm thick tissue sections were deparaffinized using EZ Prep solution. CC1 standard (pH 8.4 buffer contained Tris/Borate/ethylenediaminetetraacetic acid) was used for antigen retrieval. DAB inhibitor (3% H2O2 endogenous peroxidase) was blocked for 4 minutes at 37℃. Slides were incubated with anti-P2X7R antibodies (1:300, goat IgG, Abcam, Cambridge, UK) for 40 minutes at 37℃, and then incubated with a secondary antibody (Universal HRP Multimer, Ventana Medical Systems, Melbourne, VIC, Australia) for 8 minutes at 37℃. After incubation, slides were stained with the DAB H2O2 substrate for 8 minutes, followed by hematoxylin and bluing reagent counterstaining at 37℃. A reaction buffer (pH 7.6, Tris buffer) was used as a washing solution.
- Immunohistochemical evaluation
- Both the intensity of immunohistochemical staining and the proportion of stained tumor cells were semi-quantitatively evaluated. The staining intensity was scored as follows: 0, negative; 1, weak; 2, moderate; and 3, strong. Staining proportion was rated according to the percentage of positive cells and scored as follows: 0, less than 10%; 1, 11% to 25%; 2, 26% to 75%; 3, more than 75%. The scores of staining intensity and proportion were multiplied to produce a weighted immunoreactive score (0-6). Cases with a score ≥3 were considered high expression and those with a score ≤2 were defined as low expression. Two pathologists blinded to the patients' clinical data interpreted all immunostained slides, and cases with discrepant scores were reevaluated to achieve a consensus score.
- Statistical analysis
- Results are expressed as mean±standard deviation or frequencies and proportions where appropriate. Comparisons between groups were performed using the Student's t-tests for continuous data. Differences in the frequency of single variables were tested using the χ2 test. Univariate and multivariate analyses were used to estimate the influence of P2X7R expression on clinicopathological parameters. SPSS ver. 18 (SPSS Inc., Chicago, IL, USA) was used for all statistical analyses, and a p<.05 was considered statistically significant.
MATERIALS AND METHODS
- Clinicopathological features
- Patients consisted of 18 men and 152 women with an age range of 26 to 76 years (mean, 47.5±11.7 years). The 170 cases consisted of 150 conventional PTC (88.2%) and 20 variants (11.8%), including follicular variants (n=16), oncocytic variants (n=3), and a diffuse sclerosing variant (n=1). Extrathyroid extension and lymphovascular invasion were identified in 45.9% (78/170) and 48.8% (83/170) of cases, respectively. In addition, 64 patients (37.6%) had multifocality. Lymph node metastasis was identified in 41.8% (71/170) of cases. The clinical and pathological characteristics according to the presence of HT are summarized in Table 1. PTC patients with HT were more likely to be women (p=.01), with less lymphovascular invasion (p<.001) and extrathyroid extension (p<.001). Less lymph node metastasis (p<.001) was evident among the PTC with HT group compared to the PTC without HT group. There were no statistical differences in terms of age, histological variant, tumor size, or tumor multifocality between the PTC with HT and PTC without HT groups. Of the 84 patients with HT, only one patient (1.2%) had recurrence during a mean follow-up of 64.3±11.1 months, whereas six (7%) patients without HT had recurrence during a mean follow-up of 64.8±8.6 months. Lower recurrence (p=.026) was noted in the PTC with HT group, however, this observation is not mentioned in the table because of the low number of patients. Two patients expired during the follow-up period, but their cause of death was not clear; hence, they were excluded.
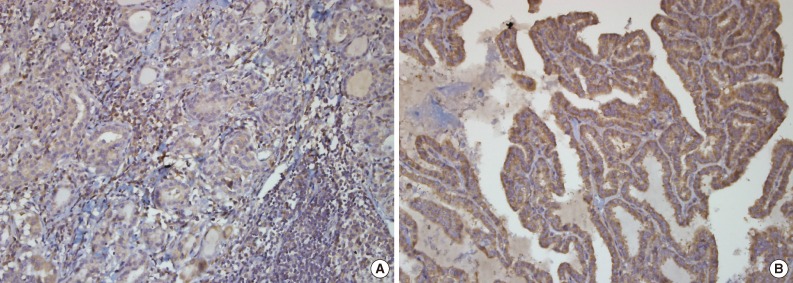
- P2X7R expression in PTC
- The 170 patients consisted of 90 having high P2X7R expression and 80 having low P2X7R expression. Of the 90 patients with high P2X7R expression, 66 patients had PTC only (73.3%) and 24 patients had PTC with HT (26.7%). P2X7R was mainly expressed in the cytoplasm of PTC (Fig. 1). High P2X7R expression was significantly associated with lymphovascular invasion (p<.001), extrathyroid extension (p<.001), and lymph node metastasis (p<.001). However, tumor size, tumor multifocality, and histological variant were not statistically associated with P2X7R expression (Table 2). Table 3 shows results of the multivariate logistic analysis investigating factors that potentially affect P2X7R expression. No significant association between P2X7R expression and age (odds ratio [OR], 1.42; 95% confidence interval [CI], 0.63 to 3.21; p=.40), gender (OR, 0.75; 95% CI, 0.2 to 2.8; p=.67), tumor multifocality (OR, 1.15; 95% CI, 0.31 to 3.99; p=.87), lymphovascular invasion (OR, 1.31; 95% CI, 0.48 to 3.61; p=.59), or lymph node metastasis (OR, 1.81; 95% CI, 0.71 to 4.6; p=.21) was found. However, there was a significant association between high P2X7R expression and extrathyroid extension (OR, 3.16; 95% CI, 1.31 to 7.6; p=.01).
- Expression of P2X7R in PTC with or without HT
- High P2X7R expression was significantly associated with an absence of HT (OR, 5.43; 95% CI, 2.45 to 12; p<.001). In the group with coexisting HT, P2X7R expression was significantly higher in patients with tumor multifocality (p=.05), lymphovascular invasion (p<.001), and extrathyroid extension (p<.001) (Table 4). For the PTC without HT group, P2X7R expression was significantly higher in women (p<.001) and the tumor multifocality group (p<.001) (Table 5).
RESULTS
- In the present study, we found that PTC with HT correlated with more favorable biological characteristics than PTC without HT. In PTC, the absence of HT was associated with high frequencies of female patients, extrathyroid extension, lymph node metastasis, lymphovascular invasion, and frequent recurrences. Similarly, the presence of autoimmune thyroiditis in thyroid cancer has been correlated with good prognosis. Recent meta-analysis demonstrated that PTCs with coexisting HT are strongly associated with female patients, tumor multifocality, the absence of extrathyroidal extension, absence of lymph node metastasis, and high recurrence-free survival rates.16 Kim et al.7 also suggested that PTC coexisting with HT may protect against central lymph node metastasis. Huang et al.17 reported that coexisting HT with either PTC or follicular thyroid carcinoma is linked with improved clinical stage and favorable prognosis. The mechanisms by which cancer cells may be destroyed by autoimmunity have been suggested. Lymphocytic infiltrates in thyroid cancer contain cytotoxic T lymphocytes, and Fas-mediated apoptosis is the major mechanism by which cytotoxic T lymphocytes cause target cell lysis.3 In addition, interleukin-1, secreted by infiltrating lymphocytes, inhibits human thyroid carcinoma cell growth.18
- Only three articles have been published on the possible link between thyroid cancer and P2X7R expression.13,14,19 In vitro study has shown that thyroid papillary carcinoma cell lines express high levels of P2X7R.13 Gu et al.14 suggested that P2X7R expression is associated with lymph node metastasis in PTCs. In their logistic regression analysis, P2X7R expression, tumor size, and capsular invasion are predictors for lymph node metastasis, suggesting that P2X7R expression may predict the aggressiveness of PTC.14 However, these studies have not demonstrated the association between P2X7R expression and PTC with HT.
- In the present study, PTC with HT correlates with good prognostic factors. PTC with high P2X7R expression showed significantly higher frequencies of lymphovascular invasion, extrathyroid extension, lymph node metastasis, and absence of HT. In the multivariate analysis, high P2X7R expression was independently associated with the absence of HT and the presence of extrathyroid extension. Our results suggested that P2X7R expression in PTC correlates with poor prognostic factors.
- In the PTC with HT group, the expression of P2X7R was significantly higher in tumor multifocality, lymphovascular invasion, and extrathyroid extension. As for the PTC without HT group, the expression of P2X7R was significantly higher in females and those with tumor multifocality. These results may imply that a different mechanism of P2X7R expression may be involved according to coexistence of HT. Recently, Beynon et al.20 reported that activated memory T-cells primed by interferon-β suppress the activation of monocytes by inhibiting P2X7R-mediated signaling, indicating that P2X7R expression in HT may be associated with activated T lymphocytes of HT.
- In conclusion, the occurrence of PTC in HT individuals may predict a favorable tumor behavior such as less tumor multifocality, lymphovascular invasion, and extrathyroid extension, compared to those having PTC without HT. P2X7R expression in PTC was correlated with poor prognostic factors and the absence of HT.
DISCUSSION
- 1. Jung KW, Park S, Kong HJ, et al. Cancer statistics in Korea: incidence, mortality, survival, and prevalence in 2009. Cancer Res Treat 2012; 44: 11-24. ArticlePubMedPMCPDF
- 2. Loh KC, Greenspan FS, Dong F, Miller TR, Yeo PP. Influence of lymphocytic thyroiditis on the prognostic outcome of patients with papillary thyroid carcinoma. J Clin Endocrinol Metab 1999; 84: 458-463. ArticlePubMed
- 3. Chistiakov DA. Immunogenetics of Hashimoto's thyroiditis. J Autoimmune Dis 2005; 2: 1.ArticlePubMedPMCPDF
- 4. Schäffler A, Palitzsch KD, Seiffarth C, et al. Coexistent thyroiditis is associated with lower tumour stage in thyroid carcinoma. Eur J Clin Invest 1998; 28: 838-844. ArticlePubMedPDF
- 5. Singh B, Shaha AR, Trivedi H, Carew JF, Poluri A, Shah JP. Coexistent Hashimoto's thyroiditis with papillary thyroid carcinoma: impact on presentation, management, and outcome. Surgery 1999; 126: 1070-1076. ArticlePubMed
- 6. Del Rio P, Cataldo S, Sommaruga L, Concione L, Arcuri MF, Sianesi M. The association between papillary carcinoma and chronic lymphocytic thyroiditis: does it modify the prognosis of cancer? Minerva Endocrinol 2008; 33: 1-5. PubMed
- 7. Kim SS, Lee BJ, Lee JC, et al. Coexistence of Hashimoto's thyroiditis with papillary thyroid carcinoma: the influence of lymph node metastasis. Head Neck 2011; 33: 1272-1277. ArticlePubMed
- 8. Ralevic V, Burnstock G. Receptors for purines and pyrimidines. Pharmacol Rev 1998; 50: 413-492. ArticlePubMed
- 9. Slater M, Danieletto S, Gidley-Baird A, Teh LC, Barden JA. Early prostate cancer detected using expression of non-functional cytolytic P2X7 receptors. Histopathology 2004; 44: 206-215. ArticlePubMed
- 10. Slater M, Danieletto S, Barden JA. Expression of the apoptotic calcium channel P2X7 in the glandular epithelium. J Mol Histol 2005; 36: 159-165. ArticlePubMedPDF
- 11. Li X, Qi X, Zhou L, et al. Decreased expression of P2X7 in endometrial epithelial pre-cancerous and cancer cells. Gynecol Oncol 2007; 106: 233-243. ArticlePubMedPMC
- 12. Wang Q, Wang L, Feng YH, Li X, Zeng R, Gorodeski GI. P2X7 receptor-mediated apoptosis of human cervical epithelial cells. Am J Physiol Cell Physiol 2004; 287: C1349-C1358. ArticlePubMed
- 13. Solini A, Cuccato S, Ferrari D, et al. Increased P2X7 receptor expression and function in thyroid papillary cancer: a new potential marker of the disease? Endocrinology 2008; 149: 389-396. ArticlePubMedPDF
- 14. Gu LQ, Li FY, Zhao L, et al. Association of XIAP and P2X7 receptor expression with lymph node metastasis in papillary thyroid carcinoma. Endocrine 2010; 38: 276-282. ArticlePubMedPDF
- 15. Kim S, Park HK, Jung HY, et al. ERG immunohistochemistry as an endothelial marker for assessing lymphovascular invasion. Korean J Pathol 2013; 47: 355-364. ArticlePubMedPMC
- 16. Lee JH, Kim Y, Choi JW, Kim YS. The association between papillary thyroid carcinoma and histologically proven Hashimoto's thyroiditis: a meta-analysis. Eur J Endocrinol 2013; 168: 343-349. ArticlePubMed
- 17. Huang BY, Hseuh C, Chao TC, Lin KJ, Lin JD. Well-differentiated thyroid carcinoma with concomitant Hashimoto's thyroiditis present with less aggressive clinical stage and low recurrence. Endocr Pathol 2011; 22: 144-149. ArticlePubMedPDF
- 18. Giordano C, Stassi G, De Maria R, et al. Potential involvement of Fas and its ligand in the pathogenesis of Hashimoto's thyroiditis. Science 1997; 275: 960-963. ArticlePubMed
- 19. Dardano A, Falzoni S, Caraccio N, et al. 1513A>C polymorphism in the P2X7 receptor gene in patients with papillary thyroid cancer: correlation with histological variants and clinical parameters. J Clin Endocrinol Metab 2009; 94: 695-698. PubMed
- 20. Beynon V, Quintana FJ, Weiner HL. Activated human CD4+CD45RO+ memory T-cells indirectly inhibit NLRP3 inflammasome activation through downregulation of P2X7R signalling. PLoS One 2012; 7: e39576.ArticlePubMedPMC
REFERENCES
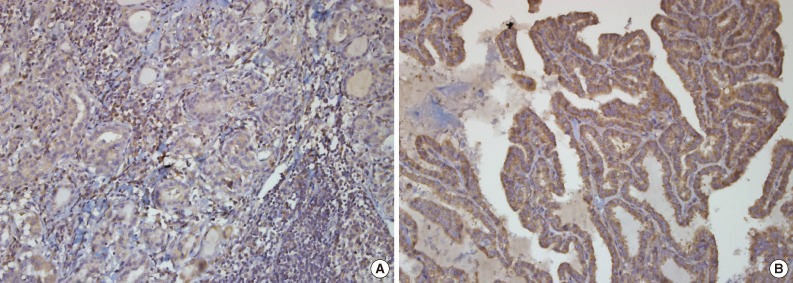
Figure & Data
References
Citations

- Research Progress in the Relationship Between P2X7R and Cervical Cancer
Yiqing Tang, Cuicui Qiao, Qianqian Li, Xiaodi Zhu, Ronglan Zhao, Xiaoxiang Peng
Reproductive Sciences.2023; 30(3): 823. CrossRef - Warthin-like papillary thyroid carcinoma: a case report and comprehensive review of the literature
Abdel Mouhaymen Missaoui, Fatma Hamza, Wafa Belabed, Manel Mellouli, Mohamed Maaloul, Slim Charfi, Issam Jardak, Tahya Sellami-Boudawara, Nabila Rekik, Mohamed Abid
Frontiers in Endocrinology.2023;[Epub] CrossRef - Mapping the path towards novel treatment strategies: a bibliometric analysis of Hashimoto’s thyroiditis research from 1990 to 2023
Manping Guo, Qingna Li, Xingfang Liu, Yiming Wang, Qiaoning Yang, Rui Li, Yang Zhao, Chenfei Li, Song Sheng, Hangkun Ma, Zhenghong Li, Rui Gao
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between Hashimoto thyroiditis and clinical outcomes of papillary thyroid carcinoma: A meta-analysis
Qizhi Tang, Weiyu Pan, Liangyue Peng, Francis Moore
PLOS ONE.2022; 17(6): e0269995. CrossRef - Hashimoto’s Thyroiditis Minimizes Lymph Node Metastasis in BRAF Mutant Papillary Thyroid Carcinomas
Peter P. Issa, Mahmoud Omar, Yusef Buti, Chad P. Issa, Bert Chabot, Christopher J. Carnabatu, Ruhul Munshi, Mohammad Hussein, Mohamed Aboueisha, Mohamed Shama, Ralph L. Corsetti, Eman Toraih, Emad Kandil
Biomedicines.2022; 10(8): 2051. CrossRef - Overexpression of PD-L1 in Papillary Carcinoma and Its Association with Clinicopathological Variables
Servet KOCAÖZ, Gülay TURAN
Düzce Tıp Fakültesi Dergisi.2021; 23(3): 252. CrossRef - Effect of P2X7 receptor on tumorigenesis and its pharmacological properties
Wen-jun Zhang, Ce-gui Hu, Zheng-ming Zhu, Hong-liang Luo
Biomedicine & Pharmacotherapy.2020; 125: 109844. CrossRef - P2X7 in Cancer: From Molecular Mechanisms to Therapeutics
Romain Lara, Elena Adinolfi, Catherine A. Harwood, Mike Philpott, Julian A. Barden, Francesco Di Virgilio, Shaun McNulty
Frontiers in Pharmacology.2020;[Epub] CrossRef - The P2X7 Receptor in Inflammatory Diseases: Angel or Demon?
Luiz E. B. Savio, Paola de Andrade Mello, Cleide Gonçalves da Silva, Robson Coutinho-Silva
Frontiers in Pharmacology.2018;[Epub] CrossRef - Patients with Oncocytic Variant Papillary Thyroid Carcinoma Have a Similar Prognosis to Matched Classical Papillary Thyroid Carcinoma Controls
Azadeh A. Carr, Tina W.F. Yen, Diana I. Ortiz, Bryan C. Hunt, Gilbert Fareau, Becky L. Massey, Bruce H. Campbell, Kara L. Doffek, Douglas B. Evans, Tracy S. Wang
Thyroid.2018; 28(11): 1462. CrossRef - Extracellular purines, purinergic receptors and tumor growth
F Di Virgilio, E Adinolfi
Oncogene.2017; 36(3): 293. CrossRef - Multifaceted Effects of Extracellular Adenosine Triphosphate and Adenosine in the Tumor–Host Interaction and Therapeutic Perspectives
Paola de Andrade Mello, Robson Coutinho-Silva, Luiz Eduardo Baggio Savio
Frontiers in Immunology.2017;[Epub] CrossRef - Potential role of P2X7R in esophageal squamous cell carcinoma proliferation
André A Santos, Angélica R Cappellari, Fernanda O de Marchi, Marina P Gehring, Aline Zaparte, Caroline A Brandão, Tiago Giuliani Lopes, Vinicius D da Silva, Luis Felipe Ribeiro Pinto, Luiz Eduardo Baggio Savio, Aline Cristina Abreu Moreira-Souza, Robson C
Purinergic Signalling.2017; 13(3): 279. CrossRef - Potential relationship between Hashimoto's thyroiditis and BRAFV600E mutation status in papillary thyroid cancer
Rui‐chao Zeng, Lang‐ping Jin, En‐dong Chen, Si‐yang Dong, Ye‐feng Cai, Guan‐li Huang, Quan Li, Chun Jin, Xiao‐hua Zhang, Ou‐chen Wang
Head & Neck.2016;[Epub] CrossRef - Papillary thyroid carcinoma in Hashimoto’s thyroiditis as an incidental finding
Al Mogrampi Saad, A. Krexi, N. Papoulidis, M. Verroiotou, D. Michalakis, I. Fardellas
Hellenic Journal of Surgery.2016; 88(1): 47. CrossRef - Association of Hashimoto's thyroiditis and thyroid cancer
Salem I. Noureldine, Ralph P. Tufano
Current Opinion in Oncology.2015; 27(1): 21. CrossRef - Cribriform-morular variant of papillary thyroid carcinoma: a study of 3 cases featuring the PIK3CA mutation
Mi Jung Kwon, Young-Soo Rho, Jin Cheol Jeong, Hyung Sik Shin, Jong Seok Lee, Seong Jin Cho, Eun Sook Nam
Human Pathology.2015; 46(8): 1180. CrossRef - Understanding the roles of the P2X7 receptor in solid tumour progression and therapeutic perspectives
Sébastien Roger, Bilel Jelassi, Isabelle Couillin, Pablo Pelegrin, Pierre Besson, Lin-Hua Jiang
Biochimica et Biophysica Acta (BBA) - Biomembranes.2015; 1848(10): 2584. CrossRef - Purinergic signaling pathways in endocrine system
Ivana Bjelobaba, Marija M. Janjic, Stanko S. Stojilkovic
Autonomic Neuroscience.2015; 191: 102. CrossRef - P2X7 receptor stimulates breast cancer cell invasion and migration via the AKT pathway
JIYI XIA, XIAOLAN YU, LI TANG, GANG LI, TAO HE
Oncology Reports.2015; 34(1): 103. CrossRef - Regulation of the P2X7R by microRNA-216b in human breast cancer
Luming Zheng, Xukui Zhang, Feng Yang, Jian Zhu, Peng Zhou, Fang Yu, Lei Hou, Lei Xiao, Qingqing He, Baocheng Wang
Biochemical and Biophysical Research Communications.2014; 452(1): 197. CrossRef

Fig. 1
| Characteristic | PTC with HT (n = 84) | PTC without HT (n = 86) | p-value |
|---|---|---|---|
| Age at diagnosis (yr) | 47.1 ± 11.6 | 48.8 ± 12.2 | .33 |
| < 45 | 30 (35.7) | 22 (25.6) | |
| ≥ 45 | 54 (64.3) | 64 (74.4) | |
| Gender | .01 | ||
| Male | 4 (4.7) | 14 (16.3) | |
| Female | 80 (95.3) | 72 (83.7) | |
| Histological variant | .14 | ||
| Variants | 13 (15.4) | 7 (8.1) | |
| Conventional | 71 (84.6) | 79 (91.9) | |
| Tumor multifocality | .84 | ||
| Yes | 31 (36.9) | 33 (38.4) | |
| No | 53 (63.1) | 53 (61.6) | |
| Tumor size (cm) | .11 | ||
| < 2 | 76 (90.4) | 70 (81.4) | |
| 2-4 | 6 (7.1) | 15 (17.4) | |
| > 4 | 2 (2.5) | 1 (1.2) | |
| Lymphovascular invasion | < .001 | ||
| Yes | 24 (28.6) | 59 (68.6) | |
| No | 60 (71.4) | 27 (31.4) | |
| Extrathyroid extension | < .001 | ||
| Yes | 23 (27.4) | 55 (64) | |
| No | 61 (72.6) | 31 (36) | |
| Lymph node metastasis | < .001 | ||
| Yes | 20 (23.8) | 51 (59.3) | |
| No | 64 (76.2) | 35 (40.7) |
| Characteristic | P2X7R low expression (n = 80) | P2X7R high expression (n = 90) | p-value |
|---|---|---|---|
| Age at diagnosis (yr) | 47.5 ± 12.2 | 48.4 ± 11.7 | .13 |
| < 45 | 29 (36.2) | 23 (25.6) | |
| ≥ 45 | 51 (63.8) | 67 (74.4) | |
| Gender | .08 | ||
| Male | 5 (6.2) | 13 (14.4) | |
| Female | 75 (93.8) | 77 (85.6) | |
| Histological variant | .78 | ||
| Variants | 10 (12.5) | 10 (11.1) | |
| Conventional | 70 (87.5) | 80 (88.9) | |
| Tumor multifocality | .12 | ||
| Yes | 35 (43.8) | 29 (32.2) | |
| No | 45 (56.2) | 61 (67.8) | |
| Tumor size (cm) | .55 | ||
| < 2 | 70 (87.5) | 76 (84.4) | |
| 2-4 | 8 (10) | 13 (14.4) | |
| > 4 | 2 (2.5) | 1 (1.2) | |
| Lymphovascular invasion | < .001 | ||
| Yes | 23 (28.8) | 60 (66.7) | |
| No | 57 (71.2) | 30 (33.3) | |
| Extrathyroid extension | < .001 | ||
| Yes | 20 (25) | 58 (64.4) | |
| No | 60 (75) | 32 (35.6) | |
| Lymph node metastasis | < .001 | ||
| Yes | 21 (26.2) | 50 (55.6) | |
| No | 59 (73.8) | 40 (44.4) | |
| Hashimoto’s thyroiditis | < .001 | ||
| Yes | 60 (75) | 24 (26.7) | |
| No | 20 (25) | 66 (73.3) |
| Factor | Odds ratio | 95% Confidence interval | p-value |
|---|---|---|---|
| Age | 1.42 | 0.63-3.21 | .4 |
| Gender | 0.75 | 0.2-2.8 | .67 |
| Multifocality | 1.15 | 0.31-3.99 | .87 |
| Lymphovascular invasion | 1.31 | 0.48-3.61 | .59 |
| Lymph node metastasis | 1.81 | 0.71-4.6 | .21 |
| Extrathyroid extension | 3.16 | 1.31-7.6 | .01 |
| Hashimoto’s thyroiditis | 5.43 | 2.45-12 | < .001 |
| Characteristic | P2X7R (scores 0-2) (n = 60) | P2X7R (scores 3-9) (n = 24) | p-value |
|---|---|---|---|
| Age at diagnosis (yr) | .07 | ||
| < 45 | 25 | 5 | |
| ≥ 45 | 35 | 19 | |
| Gender | .33 | ||
| Male | 2 | 2 | |
| Female | 58 | 22 | |
| Histological variant | .85 | ||
| Variants | 9 | 4 | |
| Conventional | 51 | 20 | |
| Tumor multifocality | .05 | ||
| Yes | 26 | 5 | |
| No | 34 | 19 | |
| Tumor size (cm) | .17 | ||
| < 2 | 52 | 24 | |
| 2-4 | 6 | 0 | |
| > 4 | 2 | 0 | |
| Lymphovascular invasion | < .01 | ||
| Yes | 12 | 12 | |
| No | 48 | 12 | |
| Extrathyroid extension | < .01 | ||
| Yes | 11 | 12 | |
| No | 49 | 12 | |
| Lymph node metastasis | .47 | ||
| Yes | 13 | 7 | |
| No | 47 | 17 |
| Characteristic | P2X7R (scores 0-2) (n = 20) | P2X7R (scores 3-9) (n = 66) | p-value |
|---|---|---|---|
| Age at diagnosis (yr) | < .01 | ||
| < 45 | 19 | 11 | |
| ≥ 45 | 1 | 55 | |
| Gender | .74 | ||
| Male | 3 | 12 | |
| Female | 17 | 54 | |
| Histological variant | .55 | ||
| Variants | 1 | 6 | |
| Conventional | 19 | 60 | |
| Tumor multifocality | < .01 | ||
| Yes | 0 | 34 | |
| No | 20 | 32 | |
| Tumor size (cm) | .84 | ||
| < 2 | 16 | 53 | |
| 2-4 | 4 | 12 | |
| > 4 | 0 | 1 | |
| Lymphovascular invasion | .48 | ||
| Yes | 5 | 22 | |
| No | 15 | 44 | |
| Extrathyroid extension | .13 | ||
| Yes | 10 | 21 | |
| No | 10 | 45 | |
| Lymph node metastasis | .94 | ||
| Yes | 8 | 27 | |
| No | 12 | 39 |
Values are presented as mean±standard deviation or number (%). PTC, papillary thyroid carcinoma; HT, Hashimoto's thyroiditis.
P2X7R, P2X7 receptor.
P2X7R, P2X7 receptor.
P2X7R, P2X7 receptor.
P2X7R, P2X7 receptor.

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article