Search
- Page Path
- HOME > Search
- Adjunctive markers for classification and diagnosis of central nervous system tumors: results of a multi-center neuropathological survey in Korea
- Yoon Jin Cha, Se Hoon Kim, Na Rae Kim
- J Pathol Transl Med. 2020;54(2):165-170. Published online February 20, 2020
- DOI: https://doi.org/10.4132/jptm.2020.02.04
- 8,244 View
- 224 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The revised 4th 2016 World Health Organization (WHO) classification of tumors of the central nervous system (CNS) classification has adopted integrated diagnosis encompassing the histology and molecular features of CNS tumors. We aimed to investigate the immunohistochemistry, molecular testing, and testing methods for diagnosis of CNS tumors in pathological labs of tertiary centers in Korea, and evaluate the adequacy of tests for proper diagnosis in daily practice.
Methods
A survey, composed of eight questions concerning molecular testing for diagnosis of CNS tumors, was sent to 10 neuropathologists working in tertiary centers in Korea.
Results
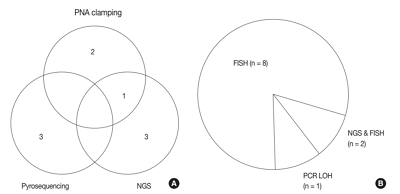
For diagnosis of astrocytic and oligodendroglial tumors, all 10 centers performed isocitrate dehydrogenase mutations testing and 1p/19q loss of heterozygosity. For glioneuronal tumors, immunohistochemistry (IHC) assays for synaptophysin (n = 9), CD34 (n = 7), BRAF(VE1) (n = 5) were used. For embryonal tumors, particularly in medulloblastoma, four respondents used IHC panel (growth factor receptor bound protein 2-associated protein 1, filamin A, and yes-associated protein 1) for molecular subclassification. Regarding meningioma, all respondents performed Ki-67 IHC and five performed telomerase reverse transcriptase promoter mutation.
Conclusions
Most tertiary centers made proper diagnosis in line with 2016 WHO classification. As classification of CNS tumors has evolved to be more complex and more ancillary tests are required, these should be performed considering the effect of necessity and justification. -
Citations
Citations to this article as recorded by- Exploring the role of epidermal growth factor receptor variant III in meningeal tumors
Rashmi Rana, Vaishnavi Rathi, Kirti Chauhan, Kriti Jain, Satnam Singh Chhabra, Rajesh Acharya, Samir Kumar Kalra, Anshul Gupta, Sunila Jain, Nirmal Kumar Ganguly, Dharmendra Kumar Yadav, Timir Tripathi
PLOS ONE.2021; 16(9): e0255133. CrossRef
- Exploring the role of epidermal growth factor receptor variant III in meningeal tumors
- Frozen Cytology of Meningeal Malignant Solitary Fibrous Tumor/Hemangiopericytoma
- Myunghee Kang, Na Rae Kim, Dong Hae Chung, Gie-Taek Yie
- J Pathol Transl Med. 2019;53(3):192-197. Published online April 11, 2019
- DOI: https://doi.org/10.4132/jptm.2019.03.20
- 7,818 View
- 160 Download
- 7 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - A 51-year-old woman presented with severe dizziness. The brain magnetic resonance image revealed a 5.5 cm multiloculated mass with a thick rim in the left temporal lobe. Cytological examination of frozen diagnosis of the mass showed hypercellular sheets of round and rhabdoid cells in a hemorrhagic background, and two mitotic figures were observed. Histologically, the excised dura-based mass consisted of predominantly round cells with small foci of rhabdoid tumor cells in a pseudoalveolar pattern in a hemorrhagic background, and the cells showed nuclear positivity for signal transducer and activator of transcription 6 as well as frequent mitosis. The mass was diagnosed as a grade 3 solitary fibrous tumor (SFT)/hemangiopericytoma (HPC). The cytological diagnosis of SFT/HPC is challenging because of the heterogeneous cytological findings, such as histological heterogeneity, and because there are no standardized cytological criteria for malignant SFT/HPC. Cytological findings, such as singly scattered small cells, hypercellularity, rare ropy collagen, and round and rhabdoid cells with pseudoalveolar pattern, may assist in the diagnosis of malignant SFT/HPC.
-
Citations
Citations to this article as recorded by- A Rare Case of Cervical Solitary Fibrous Tumor in a Pediatric Patient: Case Report and Literature Review
Eleonora Becattini, Lorenzo Sgarbanti, Giuseppina Bevacqua, Valentina Grespi, Carlo Conti
NeuroSci.2025; 6(2): 49. CrossRef - Meningeal Solitary Fibrous Tumor: A Cytological Report With Emphasis on the Usefulness of Immunocytochemical Analysis for STAT6
Hiroyuki Okanishi, Mitsuaki Ishida, Naoto Kohno, Isako Kataoka, Mari Tomiuka, Mayumi Uragami, Shizuka Ono, Chihiro Deguchi, Reika Takeda, Yoshitaka Kurisu, Yoshinobu Hirose
Diagnostic Cytopathology.2025;[Epub] CrossRef - Cytologic features of mesenchymal, melanocytic and haematolymphoid tumours of the central nervous system and metastases
Carmen Bárcena, José A. Jiménez‐Heffernan
Cytopathology.2024; 35(5): 590. CrossRef - A Hemangiopericytoma in the External Auditory Canal: A Rare Clinical Presentation and Management
Vaibhavi Patil, Prasad Deshmukh, Sagar S Gaurkar , Ayushi Ghosh Moulic, Jasleen Kaur
Cureus.2024;[Epub] CrossRef - Scoring system for intraoperative diagnosis of intracranial schwannoma by squash cytology
Hirotaka Fujita, Takuma Tajiri, Tomohisa Machida, Nozomi Nomura, Suguru Toguchi, Hitoshi Itoh, Shinichiro Hiraiwa, Tomoko Sugiyama, Chie Inomoto, Masaaki Imai, Shinri Oda, Masami Shimoda, Naoya Nakamura
Cytopathology.2022; 33(2): 196. CrossRef - Occurrence of a solitary fibrous tumor adjacent to the resection bed of a high-grade meningioma: A case report
Coby Cunningham, Rocco Dabecco, Justin Davanzo
Interdisciplinary Neurosurgery.2021; 25: 101277. CrossRef - A case of solitary fibrous tumor arising in the meninge
Saori NAKANISHI, Naoto KURODA, Toshiko TAKAI, Mari KOJIMA, Misato OONOGI
The Journal of the Japanese Society of Clinical Cytology.2021; 60(4): 224. CrossRef - Intraoperative frozen cytology of intraosseous cystic meningioma in the sphenoid bone
Na Rae Kim, Gie-Taek Yie
Journal of Pathology and Translational Medicine.2020; 54(6): 508. CrossRef
- A Rare Case of Cervical Solitary Fibrous Tumor in a Pediatric Patient: Case Report and Literature Review
- Intraoperative Frozen Cytology of Central Nervous System Neoplasms: An Ancillary Tool for Frozen Diagnosis
- Myunghee Kang, Dong Hae Chung, Na Rae Kim, Hyun Yee Cho, Seung Yeon Ha, Sangho Lee, Jungsuk An, Jae Yeon Seok, Gie-Taek Yie, Chan Jong Yoo, Sang Gu Lee, Eun Young Kim, Woo Kyung Kim, Seong Son, Sun Jin Sym, Dong Bok Shin, Hee Young Hwang, Eung Yeop Kim, Kyu Chan Lee
- J Pathol Transl Med. 2019;53(2):104-111. Published online January 14, 2019
- DOI: https://doi.org/10.4132/jptm.2018.11.10
- 14,676 View
- 684 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pathologic diagnosis of central nervous system (CNS) neoplasms is made by comparing light microscopic, immunohistochemical, and molecular cytogenetic findings with clinicoradiologic observations. Intraoperative frozen cytology smears can improve the diagnostic accuracy for CNS neoplasms. Here, we evaluate the diagnostic value of cytology in frozen diagnoses of CNS neoplasms.
Methods
Cases were selected from patients undergoing both frozen cytology and frozen sections. Diagnostic accuracy was evaluated.
Results
Four hundred and fifty-four cases were included in this retrospective single-center review study covering a span of 10 years. Five discrepant cases (1.1%) were found after excluding 53 deferred cases (31 cases of tentative diagnosis, 22 cases of inadequate frozen sampling). A total of 346 cases of complete concordance and 50 cases of partial concordance were classified as not discordant cases in the present study. Diagnostic accuracy of intraoperative frozen diagnosis was 87.2%, and the accuracy was 98.8% after excluding deferred cases. Discrepancies between frozen and permanent diagnoses (n = 5, 1.1%) were found in cases of nonrepresentative sampling (n = 2) and misinterpretation (n = 3). High concordance was observed more frequently in meningeal tumors (97/98, 99%), metastatic brain tumors (51/52, 98.1%), pituitary adenomas (86/89, 96.6%), schwannomas (45/47, 95.8%), high-grade astrocytic tumors (47/58, 81%), low grade astrocytic tumors (10/13, 76.9%), non-neoplastic lesions (23/36, 63.9%), in decreasing frequency.
Conclusions
Using intraoperative cytology and frozen sections of CNS tumors is a highly accurate diagnostic ancillary method, providing subtyping of CNS neoplasms, especially in frequently encountered entities. -
Citations
Citations to this article as recorded by- Intraoperative Integrated Diagnostic System for Malignant Central Nervous System Tumors
Takahiro Hayashi, Kensuke Tateishi, Shinichiro Matsuyama, Hiromichi Iwashita, Yohei Miyake, Akito Oshima, Hirokuni Honma, Jo Sasame, Katsuhiro Takabayashi, Kyoka Sugino, Emi Hirata, Naoko Udaka, Yuko Matsushita, Ikuma Kato, Hiroaki Hayashi, Taishi Nakamur
Clinical Cancer Research.2024; 30(1): 116. CrossRef - A multicenter proof-of-concept study on deep learning-based intraoperative discrimination of primary central nervous system lymphoma
Xinke Zhang, Zihan Zhao, Ruixuan Wang, Haohua Chen, Xueyi Zheng, Lili Liu, Lilong Lan, Peng Li, Shuyang Wu, Qinghua Cao, Rongzhen Luo, Wanming Hu, Shanshan lyu, Zhengyu Zhang, Dan Xie, Yaping Ye, Yu Wang, Muyan Cai
Nature Communications.2024;[Epub] CrossRef - Advancements in Neurosurgical Intraoperative Histology
Ali A. Mohamed, Emma Sargent, Cooper Williams, Zev Karve, Karthik Nair, Brandon Lucke-Wold
Tomography.2024; 10(5): 693. CrossRef - Unveiling the potential application of intraoperative brain smear for brain tumor diagnosis in low-middle-income countries: A comprehensive systematic review
Muhammad Shakir, Ahmed Altaf, Hawra Hussain, Syed Muhammad Aqeel Abidi, Zoey Petitt, Mahnoor Tariq, Ahmed Gilani, S. Ather Enam
Surgical Neurology International.2023; 14: 325. CrossRef - A Comparative Study of Squash Smear Cytology Diagnosis and Radiological Diagnosis with Histopathology in Central Nervous System Lesions
B N Kumarguru, G Santhipriya, S Kranthi Kumar, R Ramesh Kumar, A S Ramaswamy, P Janakiraman
Journal of Cytology.2022; 39(1): 1. CrossRef - Intraoperative squash cytology provides a qualitative intraoperative diagnosis for cases in which frozen section yields a diagnosis of equivocal brain tumour
Hirotaka Fujita, Takuma Tajiri, Tomohisa Machida, Nozomi Nomura, Suguru Toguchi, Hitoshi Itoh, Shinichiro Hiraiwa, Tomoko Sugiyama, Masaaki Imai, Shinri Oda, Masami Shimoda, Naoya Nakamura
Cytopathology.2020; 31(2): 106. CrossRef - Intraoperative frozen cytology of intraosseous cystic meningioma in the sphenoid bone
Na Rae Kim, Gie-Taek Yie
Journal of Pathology and Translational Medicine.2020; 54(6): 508. CrossRef - Use of 5-Aminolevulinic Acid for Confirmation of Lesional Biopsy Sample in Presumed High-Grade Glioma
Victoria L. Watson, Jeffrey W. Cozzens
World Neurosurgery.2019; 132: 21. CrossRef
- Intraoperative Integrated Diagnostic System for Malignant Central Nervous System Tumors
- Primary Peripheral Gamma Delta T-Cell Lymphoma of the Central Nervous System: Report of a Case Involving the Intramedullary Spinal Cord and Presenting with Myelopathy
- Jeemin Yim, Seung Geun Song, Sehui Kim, Jae Won Choi, Kyu-Chong Lee, Jeong Mo Bae, Yoon Kyung Jeon
- J Pathol Transl Med. 2019;53(1):57-61. Published online October 1, 2018
- DOI: https://doi.org/10.4132/jptm.2018.08.21
- 7,352 View
- 159 Download
- 5 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Primary central nervous system lymphoma of T-cell origin (T-PCNSL) is rare, and its clinicopathological features remain unclear. Peripheral T-cell lymphoma of γδ T-cell origin is an aggressive lymphoma mainly involving extranodal sites. Here, we report a case of γδ T-PCNSL involving the intramedullary spinal cord and presenting with paraplegia. A 75-year-old Korean woman visited the hospital complaining of back pain and lower extremity weakness. Magnetic resonance imaging revealed multifocal enhancing intramedullary nodular lesions in the thoracic and lumbar spinal cord. An enhancing nodular lesion was observed in the periventricular white matter of the lateral ventricle in the brain. There were no other abnormalities in systemic organs or skin. Laminectomy and tumor removal were performed. The tumor consisted of monomorphic, medium-to-large atypical lymphocytes with pale-to-eosinophilic cytoplasm. Immunohistochemically, the tumor cells were CD3(+), TCRβF1(-), TCRγ(+), CD30(-), CD4(-), CD8(-), CD56(+), TIA1(+), granzyme B(+), and CD103(+). Epstein-Barr virus in situ was negative. This case represents a unique T-PCNSL of γδ T-cell origin involving the spinal cord.
-
Citations
Citations to this article as recorded by- B-Cell Lymphoma Intramedullary Tumor: Case Report and Systematic Review
Daniel Gregório Gonsalves, Paulo Eduardo Albuquerque Zito Raffa, Gabriela Gerenutti de Sousa, Melissa Esposito Gomes Rigueiral, Iracema Araújo Estevão, Cesar Cozar Pacheco, Roger Thomaz Rotta Medeiros, Paulo Roberto Franceschini, Paulo Henrique Pires de A
Asian Journal of Neurosurgery.2023; 18(02): 231. CrossRef - Primary intramedullary spinal cord lymphoma misdiagnosed as longitudinally extensive transverse myelitis: a case report and literature review
Huizhen Ge, Li Xu, Huajie Gao, Suqiong Ji
BMC Neurology.2023;[Epub] CrossRef - Clinicopathologic and Genetic Features of Primary T-cell Lymphomas of the Central Nervous System
Jeemin Yim, Jiwon Koh, Sehui Kim, Seung Geun Song, Jeong Mo Bae, Hongseok Yun, Ji-Youn Sung, Tae Min Kim, Sung-Hye Park, Yoon Kyung Jeon
American Journal of Surgical Pathology.2022; 46(4): 486. CrossRef - Peripheral T-Cell Lymphomas Involving the Central Nervous System: A Report From the Czech Lymphoma Study Group Registry
Heidi Mocikova, Robert Pytlík, Katerina Benesova, Andrea Janikova, Juraj Duras, Alice Sykorova, Katerina Steinerova, Vit Prochazka, Vit Campr, David Belada, Marek Trneny
Frontiers in Oncology.2022;[Epub] CrossRef
- B-Cell Lymphoma Intramedullary Tumor: Case Report and Systematic Review
- An Autopsy Case of Epstein-Barr Virus–Associated Diffuse Large B-Cell Lymphoma of the Central Nervous System in an Immunocompromised Host
- Sun-Young Park, Seong Ik Kim, Hannah Kim, Yoojin Lee, Sung-Hye Park
- J Pathol Transl Med. 2018;52(1):51-55. Published online August 4, 2017
- DOI: https://doi.org/10.4132/jptm.2017.01.23
- 9,630 View
- 174 Download
- 2 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Lymphomas arising in the central nervous system (CNS) of immunocompromised hosts are most commonly non-Hodgkin’s lymphomas and are highly associated with Epstein-Barr virus (EBV). Here we report an autopsy case of EBV-associated CNS diffuse large B-cell lymphoma (DLBCL) in a host suffering from systemic lupus erythematosus who underwent immunosuppressive therapy. After autopsy, EBV-associated CNS DLBCL as well as pulmonary mixed aspergillosis and Pneumocystis jirovecii pneumonia were added to the cause of clinical manifestations of complicated pneumonia and cerebral hemorrhage in this immunocompromised patient. In conclusion, complex disease processes were revealed by autopsy in this case, indicating that the clinicopathological correlations observed through autopsy can improve our understanding of disease progression and contribute to the management of similar patients in the future.
-
Citations
Citations to this article as recorded by- Primary central nervous system lymphoma in neuropsychiatric systemic lupus erythematosus: case-based review
Takanori Ichikawa, Yasuhiro Shimojima, Dai Kishida, Tomoki Kaneko, Yoshiki Sekijima
Rheumatology International.2021; 41(5): 1009. CrossRef
- Primary central nervous system lymphoma in neuropsychiatric systemic lupus erythematosus: case-based review
- Meningeal Solitary Fibrous Tumors with Delayed Extracranial Metastasis
- Nayoung Han, Hannah Kim, Soo Kee Min, Sun-Ha Paek, Chul-Kee Park, Seung-Hong Choi, U-Ri Chae, Sung-Hye Park
- J Pathol Transl Med. 2016;50(2):113-121. Published online December 14, 2015
- DOI: https://doi.org/10.4132/jptm.2015.10.30
- 12,871 View
- 119 Download
- 25 Web of Science
- 22 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The term solitary fibrous tumor (SFT) is preferred over meningeal hemangiopericytoma (HPC), because NAB2-STAT6 gene fusion has been observed in both intracranial and extracranial HPCs. HPCs are now considered cellular variants of SFTs. Methods: This study analyzes 19 patients with STAT6-confirmed SFTs, who were followed for over 11 years in a single institution. Ten patients (10/19, 56.2%) had extracranial metastases (metastatic group), while the remainder (9/19) did not (non-metastatic group). These two groups were compared clinicopathologically. Results: In the metastatic group, the primary metastatic sites were the lungs (n = 6), bone (n = 4), and liver (n = 3). There was a mean lag time of 14.2 years between the diagnosis of the initial meningeal tumor to that of systemic metastasis. The median age at initial tumor onset was 37.1 years in the metastatic group and 52.5 in the non-metastatic group. The 10-year survival rates of the metastatic- and non-metastatic groups were 100% and 33%, respectively. The significant prognostic factors for poor outcomes on univariate analysis included advanced age (≥45 years) and large initial tumor size (≥5 cm). In contrast, the patients with higher tumor grade, high mitotic rate (≥5/10 high-power fields), high Ki-67 index (≥5%), and the presence of necrosis or CD34 positivity showed tendency of poor prognosis but these parameters were not statistically significant poor prognostic markers. Conclusions: Among patients with SFTs, younger patients (<45 years) experienced longer survival times and paradoxically had more frequent extracranial metastases after long latent periods than did older patients. Therefore, young patients with SFTs require careful surveillance and follow-up for early detection of systemic metastases. -
Citations
Citations to this article as recorded by- High-grade, metastatic disease, and adjuvant radiotherapy are independent prognostic factors for progression-free survival in patients with solitary fibrous tumors
Jan Paul Alker, Ramin Rahmanzade, Thomas Held, Christel Herold-Mende, Andreas Unterberg, Felix Sahm, Sandro Manuel Krieg, Gerhard Jungwirth
Neuro-Oncology Advances.2025;[Epub] CrossRef - Meningeal malignant solitary fibrous tumor with multiple recurrence, extracranial extension, cervical lymph node metastases: case report and review of the literature
Rong He, Peng Zhong, Juntao Hu, Guangkuo Guo, He Xiao, Lin Lei, Yun Liu, Mingying Geng, Jungang Ma
Discover Oncology.2025;[Epub] CrossRef - A Case of Intracranial Solitary Fibrous Tumor Followed by Distant Metastasis without Local Recurrence
Masafumi YOSHIDA, Koki MORIYOSHI, Kento DOI, Yukihiro YAMAO, Natsue KISHIDA, Hiroya UEMURA, Shunichi FUKUDA
NMC Case Report Journal.2025; 12: 181. CrossRef - The association between WHO grading and the long-term outcomes and radiotherapy efficacy of intracranial solitary fibrous tumors
Leihao Ren, Lingyang Hua, AO Feng, Jiaojiao Deng, Hiroaki Wakimoto, Tareq Juratli, Qing Xie, Ye Gong
Acta Neuropathologica Communications.2025;[Epub] CrossRef - Meningeal Solitary Fibrous Tumor: A Single-Center Retrospective Cohort Study
Siyer Roohani, Yasemin Alberti, Maximilian Mirwald, Felix Ehret, Carmen Stromberger, Soleiman Fabris Roohani, Katja Bender, Anne Flörcken, Sven Märdian, Daniel Zips, David Kaul, Manish Charan
Sarcoma.2024; 2024: 1. CrossRef - De-differentiation associated with drop metastasis of a recurrent intracranial solitary fibrous tumor: a case report and literature review
Chenhui Zhao, Xiran Fan, Wanwan Gao, Fan Zhang, Haijun Lv, Xiaochun Jiang, Guangfu Di
International Journal of Neuroscience.2022; 132(8): 843. CrossRef - Long-term extracranial metastatic relapse of an intraventricular solitary fibrous tumor: a case report
Tarek Assi, Elie Samaha, Hussein Nassereddine
Anti-Cancer Drugs.2022; 33(1): e764. CrossRef - Multidisciplinary Treatment of Liver Metastases from Intracranial SFTs/HPCs: A Report of Three Consecutive Cases
Felix J. Krendl, Franka Messner, Gregor Laimer, Angela Djanani, Andreas Seeber, Georg Oberhuber, Dietmar Öfner, Dominik Wolf, Stefan Schneeberger, Reto Bale, Christian Margreiter
Current Oncology.2022; 29(11): 8720. CrossRef - A review of solitary fibrous tumor/hemangiopericytoma tumor and a comparison of risk factors for recurrence, metastases, and death among patients with spinal and intracranial tumors.
Enrico Giordan, Elisabetta Marton, Alexandra M. Wennberg, Angela Guerriero, Giuseppe Canova
Neurosurgical Review.2021; 44(3): 1299. CrossRef - Intracranial Solitary Fibrous Tumor of the Skull Base: 2 Cases and Systematic Review of the Literature
Sricharan Gopakumar, Visish M. Srinivasan, Caroline C. Hadley, Adrish Anand, Marc Daou, Patrick J. Karas, Jacob Mandel, Shankar P. Gopinath, Akash J. Patel
World Neurosurgery.2021; 149: e345. CrossRef - Hemangiopericytoma/Solitary Fibrous Tumor in the central nervous system. Experience with surgery and radiotherapy as a complementary treatment: A 10-year analysis of a heterogeneous series in a single tertiary center
Pedro Miguel González-Vargas, José Luis Thenier-Villa, Pablo Sanromán Álvarez, Alexandre Serantes Combo, Lourdes Calero Félix, Raúl Alejandro Galárraga Campoverde, Eva Azevedo González, Álvaro Martín-Gallego, Rosa Martínez-Rolan, Adolfo de la Lama Zaragoz
Neurocirugía.2020; 31(1): 14. CrossRef - Hemangiopericytoma/Solitary Fibrous Tumor in the central nervous system. Experience with surgery and radiotherapy as a complementary treatment: A 10-year analysis of a heterogeneous series in a single tertiary center
Pedro Miguel González-Vargas, José Luis Thenier-Villa, Pablo Sanromán Álvarez, Alexandre Serantes Combo, Lourdes Calero Félix, Raúl Alejandro Galárraga Campoverde, Eva Azevedo González, Álvaro Martín-Gallego, Rosa Martínez-Rolan, Adolfo de la Lama Zaragoz
Neurocirugía (English Edition).2020; 31(1): 14. CrossRef - Solitary fibrous tumor/hemangiopericytoma: treatment results based on the 2016 WHO classification
Kyoung Su Sung, Ju Hyung Moon, Eui Hyun Kim, Seok-Gu Kang, Se Hoon Kim, Chang-Ok Suh, Sun Ho Kim, Kyu-Sung Lee, Won Seok Chang, Jong Hee Chang
Journal of Neurosurgery.2019; 130(2): 418. CrossRef - Grading of meningeal solitary fibrous tumors/hemangiopericytomas: analysis of the prognostic value of the Marseille Grading System in a cohort of 132 patients
Nicolas Macagno, Rob Vogels, Romain Appay, Carole Colin, Karima Mokhtari, Benno Küsters, Pieter Wesseling, Dominique Figarella‐Branger, Uta Flucke, Corinne Bouvier
Brain Pathology.2019; 29(1): 18. CrossRef - Solitary fibrous tumor of the pineal region with delayed ectopic intracranial metastasis: A case report and review of the literature
Yongjie Wang, Jingying Zhang, Qichang Liu, Fuyi Liu, Xiangdong Zhu, Jianmin Zhang
Medicine.2019; 98(21): e15737. CrossRef - Case report: neonatal giant forehead hemangiopericytoma with a 5-year follow-up
AiJun Peng, LiBing Zhang, Hai Zhao, LiangXue Zhou
Medicine.2019; 98(47): e17888. CrossRef - Liquid Biopsy in Rare Cancers: Lessons from Hemangiopericytoma
Chiara Nicolazzo, Luciano Colangelo, Alessandro Corsi, Guido Carpino, Angela Gradilone, Chiara Sonato, Cristina Raimondi, Eugenio Gaudio, Paola Gazzaniga, Walter Gianni
Analytical Cellular Pathology.2018; 2018: 1. CrossRef - Surveillance for metastatic hemangiopericytoma-solitary fibrous tumors-systematic literature review on incidence, predictors and diagnosis of extra-cranial disease
Tarini Ratneswaren, Florence Rosie Avila Hogg, Mathew Joseph Gallagher, Keyoumars Ashkan
Journal of Neuro-Oncology.2018; 138(3): 447. CrossRef - Intracranial Solitary Fibrous Tumor
Eveline Claus, Patrick Seynaeve, Jeroen Ceuppens, Alain Vanneste, Koenraad Verstraete
Journal of the Belgian Society of Radiology.2017;[Epub] CrossRef - Comparison and evaluation of risk factors for meningeal, pleural, and extrapleural solitary fibrous tumors: A clinicopathological study of 92 cases confirmed by STAT6 immunohistochemical staining
Ji Min Kim, Yoon-La Choi, Yu Jin Kim, Hyung Kyu Park
Pathology - Research and Practice.2017; 213(6): 619. CrossRef - Molecular Testing of Brain Tumor
Sung-Hye Park, Jaekyung Won, Seong-Ik Kim, Yujin Lee, Chul-Kee Park, Seung-Ki Kim, Seung-Hong Choi
Journal of Pathology and Translational Medicine.2017; 51(3): 205. CrossRef - Solitary fibrous tumour presenting with a single bone metastasis: report of six cases and literature review
Vittoria Colia, Salvatore Provenzano, Carlo Morosi, Paola Collini, Salvatore Lorenzo Renne, Paolo G. Dagrada, Claudia Sangalli, Angelo Paolo Dei Tos, Andrea Marrari, Paolo G. Casali, Silvia Stacchiotti
Clinical Sarcoma Research.2016;[Epub] CrossRef
- High-grade, metastatic disease, and adjuvant radiotherapy are independent prognostic factors for progression-free survival in patients with solitary fibrous tumors
- The Continuing Value of Ultrastructural Observation in Central Nervous System Neoplasms in Children
- Na Rae Kim, Sung-Hye Park
- J Pathol Transl Med. 2015;49(6):427-437. Published online October 13, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.19
- 9,727 View
- 78 Download
-
 Abstract
Abstract
 PDF
PDF - Central nervous system (CNS) neoplasms are the second most common childhood malignancy after leukemia and the most common solid organ neoplasm in children. Diagnostic dilemmas with small specimens from CNS neoplasms are often the result of multifactorial etiologies such as frozen or fixation artifact, biopsy size, or lack of knowledge about rare or unfamiliar entities. Since the late 1950s, ultrastructural examination has been used in the diagnosis of CNS neoplasms, though it has largely been replaced by immunohistochemical and molecular cytogenetic studies. Nowadays, pathologic diagnosis of CNS neoplasms is achieved through intraoperative cytology, light microscopy, immunohistochemistry, and molecular cytogenetic results. However, the utility of electron microscopy (EM) in the final diagnosis of CNS neoplasms and investigation of its pathogenetic origin remains critical. Here, we reviewed the distinguishing ultrastructural features of pediatric CNS neoplasms and emphasize the continuing value of EM in the diagnosis of CNS neoplasms.
- Diagnostic Accuracy of Cerebrospinal Fluid (CSF) Cytology in Metastatic Tumors: An Analysis of Consecutive CSF Samples
- Yoon Sung Bae, June-Won Cheong, Won Seok Chang, Sewha Kim, Eun Ji Oh, Se Hoon Kim
- Korean J Pathol. 2013;47(6):563-568. Published online December 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.563
- 9,907 View
- 70 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Cerebrospinal fluid (CSF) examination can be used to verify the presence of primary malignancies as well as cases of central nervous system (CNS) metastasis. Because of its importance, there have been several studies concerning the sensitivity of CSF cytology. To determine the practical use and reproducibility of diagnoses based on CSF cytology, we evaluated this test by analyzing cytology results from consecutive CSF samples.
Methods Between July 2010 and June 2013, 385 CSF cytology samples from 42 patients were collected. The samples were gathered using a ventricular catheter and reservoir. CSF cytology of all patients was examined more than two times with immunocytochemistry for cytokeratin.
Results Primary neoplastic sites and histologic types of patients' metastatic cancer were diverse. The overall sensitivity for detecting malignancy was 41.3%. Even within short-term intervals, diagnoses frequently changed.
Conclusions Our results were inconsistent, with low sensitivity, when compared to the results of previous studies. However, CSF evaluation can still provide valuable diagnostic and prognostic information because adjuvant treatments are now routinely performed in patients with CNS metastasis. Negative CSF cytology results should not be ignored, and continuous CSF follow-up is essential for following the clinical course of patients with metastatic cancer involving the CNS.
-
Citations
Citations to this article as recorded by- Analytical validation of the Belay Vantage™ assay for evaluation of MGMT promoter methylation using enzymatically converted tumorDNA from cerebrospinal fluid
Kala F Schilter, Qian Nie, Jennifer N Adams, Rakshitha Jagadish, Anthony Acevedo, Alexandra Larson, Samantha A Vo, Brett A Domagala, Kyle M Hernandez, Christopher Douville, Yuxuan Wang, Brian Coe, Chetan Bettegowda, Honey V Reddi
Cancer Genetics.2025; 294-295: 94. CrossRef - Analytical Validation and Clinical Sensitivity of the Belay Summit Assay for the Detection of DNA Variants in Cerebrospinal Fluid of Primary and Metastatic Central Nervous System Cancer
Qian Nie, Kala F. Schilter, Kyle M. Hernandez, Jennifer N. Adams, Rakshitha Jagadish, Anthony Acevedo, Alexandra Larson, Brett A. Domagala, Samantha A. Vo, Sakshi Khurana, Kathleen Mitchell, Dean Ellis, Baymuhammet Muhammedov, Yuxuan Wang, Christopher Dou
The Journal of Molecular Diagnostics.2025; 27(7): 615. CrossRef - Demonstrating the clinical utility of genomic profiling using cerebrospinal fluid to inform management of central nervous system tumors – a meta analysis of the literature
Sakshi Khurana, Qian Nie, Kala F. Schilter, Honey V. Reddi
The Journal of Liquid Biopsy.2025; 9: 100317. CrossRef - Application of the International System for Serous Fluid Cytopathology in Cerebrospinal Fluid Cytology
Ioannina Vidali, Konstantinos Christofidis, Georgia Bairaktari, Maria Sevastiadou, Alexandros Pergaris, Aglaia Dimitrakopoulou, Panagiota Keramari, Panagiota Mikou
Cytopathology.2025; 36(6): 589. CrossRef - The Spectrum of Malignant Diagnoses in Cerebrospinal Fluid (CSF) Cytology in Both Pediatric and Adult Populations: A Single‐Institutional Retrospective Review
Nida Babar, Asif Loya, Sajid Mushtaq, Maryam Hameed, Usman Hassan, Mudassar Hussain
Diagnostic Cytopathology.2025; 53(12): 620. CrossRef - Molecular Analysis of Cerebrospinal Fluid Tumor-Derived DNA to Aid in the Diagnosis and Targeted Treatment of Breast Cancer Brain Metastasis
Michael Youssef, Alexandra Larson, Vindhya Udhane, Viriya Keo, Kala F. Schilter, Qian Nie, Honey V. Reddi
Diseases.2025; 13(10): 336. CrossRef - Numb cheek syndrome in breast cancer: a case report
Zhibin Tan, Si Ying Tan
Frontiers in Oncology.2024;[Epub] CrossRef - Utility and performance of cell blocks in cerebrospinal fluid cytology: Experience at two teaching hospitals
Hyeji Yoon, Constance V. Chen, Vimal Krishnan, Jill Grochowski, Gioia Iezza, Poonam Vohra, Ronald Balassanian, Nancy Y. Greenland
Cancer Cytopathology.2024; 132(10): 621. CrossRef - Liquid biopsy for evaluating mutations and chromosomal aberrations in cerebrospinal fluid from patients with primary or metastatic CNS tumors
Ahmad Charifa, Sally Agersborg, Arash Mohtashamian, Andrew Ip, Andre Goy, Maher Albitar
The Journal of Liquid Biopsy.2024; 6: 100281. CrossRef - Body fluids
Shyam H. Nemade, Meherbano M. Kamal
Indian Journal of Pathology and Microbiology.2023; 66(1): 75. CrossRef - Standardizing a volume benchmark for cerebrospinal fluids for optimal diagnostic accuracy
David Kim, Susan A. Alperstein, Momin T. Siddiqui
Diagnostic Cytopathology.2021; 49(2): 258. CrossRef - Evaluating Infectious, Neoplastic, Immunological, and Degenerative Diseases of the Central Nervous System with Cerebrospinal Fluid-Based Next-Generation Sequencing
Konstantinos I. Tsamis, Hercules Sakkas, Alexandros Giannakis, Han Suk Ryu, Constantina Gartzonika, Ilias P. Nikas
Molecular Diagnosis & Therapy.2021; 25(2): 207. CrossRef - Imaging of Intraspinal Tumors
Luke N. Ledbetter, John D. Leever
Radiologic Clinics of North America.2019; 57(2): 341. CrossRef - Isolated leptomeningeal carcinomatosis and possible fungal meningitis as late sequelae of oesophageal adenocarcinoma
Richard Dumbill, Sanja Thompson, Heiko Peschl, GDH Turner, Charles Woodrow
BMJ Case Reports.2019; 12(11): e230117. CrossRef - Cytomorphological and immunocytochemical examinations of cerebrospinal fluid in primary and metastatic brain lesions
M. V. Savostikova, L. Ya. Fomina, E. S. Fedoseeva, E. Yu. Furminskaya
Onkologiya. Zhurnal imeni P.A.Gertsena.2018; 7(1): 28. CrossRef - Metastatic Breast Carcinoma in Cerebrospinal Fluid: A Cytopathological Review of 15 Cases
Rema Rao, Syed A. Hoda, Alan Marcus, Rana S. Hoda
The Breast Journal.2017; 23(4): 456. CrossRef - Clinicocytological analysis of cases with positive cerebrospinal fluid in our hospital
Nozomi IWAMOTO, Mitsuaki ISHIDA, Akiko KAGOTANI, Nozomi KASUGA, Muneo IWAI, Yuji HAYASHI, Namie ARITA, Yoshimitsu MIYAHIRA, Ryoji KUSHIMA
The Journal of the Japanese Society of Clinical Cytology.2016; 55(5): 291. CrossRef
- Analytical validation of the Belay Vantage™ assay for evaluation of MGMT promoter methylation using enzymatically converted tumorDNA from cerebrospinal fluid
- Intracranial Fibromatosis: A Case Report.
- Jeong Ju Lee, Jeoung Hun Kim, Shin Kwang Khang, Kyung Ja Cho, Jihun Kim
- Korean J Pathol. 2011;45:S89-S92.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.S1.S89
- 4,198 View
- 30 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Fibromatosis can occur at various sites, but intracranial fibromatosis is exceptionally rare. Here, we report a case of intracranial fibromatosis arising in the suprasellar area of a 52-year-old woman who had undergone a surgery at that site. A computed tomography scan revealed a heavily calcified, highly enhancing, poorly demarcated mass in the left sellar area that extended into the left suprasellar, parasellar areas, and orbital apex and completely encased the left distal inferior cerebral artery. Histologic and immunohistochemical features were compatible with those of fibromatosis, although the cellularity was focally higher than usual. The etiology of extra-abdominal fibromatosis is unknown, but physical injuries such as trauma and irradiation have been reported to be associated with its occurrence. Although fibromatosis is rare in the intracranial area, it should be considered as a differential diagnosis when an intracranial mass occurs at a previously injured site.
-
Citations
Citations to this article as recorded by- Infantile Intracranial Aggressive Fibromatosis: Report of Two Cases with a Review of the Literature
Baocheng Wang, Jie Ma, Huiming Jin
Pediatric Neurosurgery.2012; 48(3): 181. CrossRef
- Infantile Intracranial Aggressive Fibromatosis: Report of Two Cases with a Review of the Literature
- Cytologic Features and Distribution of Primary Sites of Malignant Cells in Cerebrospinal Fluid .
- Yeon Mee Kim, Mi Yeong Jeon, Je Geun Chi
- J Pathol Transl Med. 2000;11(2):65-73.
- 2,059 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Cytologic evaluation of cerebrospinal fluid(CSF) is an effective mean for diagnosing many disorders involving the central nervous systems(CNS). One of the most important reasons for cytologic examination of CSF is to detect metastatic or primary neoplasms of the CNS. We did a retrospective study of 1,438 CSF specimens obtained between 1992 and 1996. A total of 1,205 adult and 233 pediatric CSF specimens from 947 patients were accessed at the Department of Pathology of Seoul National University Hospital and Children's Hospital, respectively. Among 1,438 CSF cytology specimens, 169 cases(11.8%, 77 patients) including 135 adult cases(59 patients) and 34 pediatric cases(18 patients) were positive for malignant cells. Diagnoses included 60 metastatic carcinomas(adult, 60; pediatric, 0); 46 malignant lymphomas(adult, 44; pediatric, 2); 21 leukemias(adult, 20; pediatric, 1); 4 retinoblastomas(adult, 0; pediatric 4); 2 rhabdomyosarcomas(adult, 0; pediatric, 2); 1 multiple myeloma(adult, 1; pediatric, 0), and 35 primary CNS neoplasms(adult, 10; pediatric, 25). The most commonly identified metastatic carcinomas in adults were adenocarcinoma. Their primary sites were the lung, gastrointestinal tract, and breast in order of frequency. The most common primary CNS neoplasm in children was medulloblastoma.
- The Pattern of Cell Proliferation and Apoptosis in Human Embryonic and Fetal Brain.
- Suk Jin Choi, Jung Ran Kim
- Korean J Pathol. 2002;36(1):38-44.
- 2,143 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Cell proliferation and apoptosis account for the major morphogenetic mechanisms during development of the central nervous system. We investigated these processes in developing human brains.
METHODS
We examined human embryonic and fetal brains. Cell proliferation was analysed by classical histology and MIB-1 immunohistochemistry; cell death was investigated by the TdT-mediated dUTP-biotin nick end labelling method.
RESULTS
Most proliferating cells were observed in the ventricular zone (VZ) in the 3rd-10th week of gestational age (GA), and in both the VZ and the subventricular zone (SV) in the 19-24th week of GA. The proliferation index of the VZ was highest in the 8th week of GA and then decreased as the GA advanced. Apoptotic cells were observed in the VZ as early as the 5th week of GA. They were also observed in the intermediate zone in the 19-24th week of GA, although they were significantly lower in amount compared to that in the VZ and SV.
CONCLUSIONS
These results suggest that apoptosis occurring early in the embryonic period is related to a cellular mechanism which selects and determines the cells that are committed to migration and differentiation during the development of the human brain.
- Cytology of Crush Preparation in Central Nervous System Lesion.
- Young Il Yang, Sul Mi Park, Young Joo Kim, Shin Kwang Khang
- J Pathol Transl Med. 1994;5(2):79-89.
- 2,116 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - This study was performed in order to evaluate the accuracy and the usefulness of the cytology of crush preparation in central nervous system(CNS) lesions. Forty four intraoperative biopsies were performed at the time of craniotomy including 34 benign and 10 malignant lesions. Crush preparations were prepared from tiny tissue fragments of craiotomy products. All cases were stained with toluidine blue. Intraoperative diagnoses made on cytologic examination were compared with the final paraffin section diagnoses. Comparison between the results of the cytologic and histologic findings revealed an overall diagnostic accuracy of 88.6%. This study attests to the diagnostic accuracy of cytologic examination in CNS lesions. The detailed cytologic features are described and important criteria for the cytodiagnosis of CNS lesions are discussed.
- Diagnostic Accuracy of Fine Needle Aspiration Cytology in Thyroid Lesions: Analysis of Histologically Confirmed 153 Cases.
- Kyeong Mee Park, Ill Hyang Ko
- J Pathol Transl Med. 1996;7(2):122-133.
- 2,024 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - This is a retrospective review of fine-needle aspiration cytology(FNAC) smears of 153 cases of thyroid disease performed during August 1989 to July 1995, which were confirmed histologically following surgical operations. FNAC results showed 63 cases(41.2%) of adenomatous goiter, 45 cases(29.4%) of papillary carcinoma, 29 cases(19.0%) of follicular neoplasm, 4 cases(2.6%) of follicular variant of papillary carcinoma, 4 cases(2.6%) of Hashimoto's thyroiditis, 4 cases(2.6%) of Hurthle cell neoplasm, 2 cases(1.3%) of medullary carcinoma and one case(O.7%) each of subacute thyroiditis and of anaplastic carcinoma. The overall accuracy of cytological diagnosis was 83.7%. These data strongly suggest thyroid FNAC is a reliable preoperative diagnostic tool, but FNAC has been less valuable in the diagnosis of follicular lesions than any other disease of the thyroid. Adenomatous goiter was not infrequently interpreted as follicular neoplasia that requires surgery for diagnostic .conformation and vice versa. The following findings are considered to be compatible with follicular neoplasm: 1) microfolticles, 2) nuclear grooving, 3) irregularity of nuclear membrane, and 4) irregular arrangement or crowding of follicular cells in groups. The FNAC criteria of adenomatous goiter are as follows: 1) atrophic follicular cells, 2) presence of macrophages, 3) abundant colloid, and 4) large follicles. It is recommended that aspiration of thyroid lesions in order to analyse with critical clinico pathological approach and surgery is considered only for nodules that are clinically suspicious or unresponsive to hormone therapy or when a diagnosis of follicular neoplasm is made.
- Malignant Rhabdoid Tumor of the Cerebellum in an Adult: A case report.
- Young Min Kim, Jae Hee Suh, Tae Sook Kim, Shin Kwang Khang
- Korean J Pathol. 1998;32(6):460-465.
- 2,191 View
- 10 Download
-
 Abstract
Abstract
- Malignant rhabdoid tumor (MRT) is a rare and highly aggressive neoplasm of infancy and childhood. Although it was originally described and most frequently reported in the kidney, it may occur in various extra-renal sites such as the liver, thymus, and soft tissue. In the last decade primary central nervous system (CNS) MRTs have been reported in both the supra- and infratentorial compartments. Patients with CNS MRT were generally below the age of two and reports in adults are extremely rare. This is a case of primary cerebellar MRT in a 24-year-old woman, who had presented with intermittent headache, vocal cord palsy, and cerebellar dysfunctions such as abnormal finger to nose test and tandem gait. By magnetic resonance imaging scan, a well-enhancing solid mass was demonstrated at the posterior fossa filling the 4th ventricle, which extended into the medulla and cervical cord via the foramen of Magendie. Histologically, the monotonous polygonal tumor cells were arranged in diffuse sheet with occasional hemorrhagic necrosis. The nuclei were vesicular and eccentrically located due to eosinophilic, PAS-positive, intracytoplasmic inclusions with prominent nucleoli. They were diffusely or focally immunoreactive for vimentin, neurofilament, cytokeratin, GFAP, synaptophysin, and smooth muscle actin, while epithelial membrane antigen and desmin were negative. Ultrastructurally, the polyhedral tumor cells were densely packed with primitive intercellular junctions. Scanty fibrillar intermediate filaments were intermingled with cellular organelles. Postoperatively, craniospinal irradiation and systemic chemotherapy have been done and she has been free of tumor recurrence during the 13 months' follow-up periods.
- Crush Cytology Features and Differential Diagnosis of Meningiomas and Schwannomas in Central Nervous System.
- Young Ju Kim, Mi Yeong Jeon, Young Il Yang, Chan Hwan Kim, Hae Kyoung Yoon, Shin Kwang Khang
- J Pathol Transl Med. 1996;7(2):169-176.
- 2,849 View
- 59 Download
-
 Abstract
Abstract
 PDF
PDF - This study was performed in order to evaluate the usefulness of the crush cytologic features and differential diagnosis between meningiomas and schwannomas in the central nervous system. Deeply seated and unusually located meningiomas and schwannomas with equivocal or erroneous frozen section diagnosis can be correctly diagnosed cytologically in crush preparations. Twenty-four meningiomas and nine schwannomas were studied by frozen section and crush preparation technique. These tumors displayed distinctive cytologic features. In meningiomas, the tumor tissue fragments were easy to crush, and the tumor cells were arranged in small clusters, flat sheets, papilla-like, whorling pattern or singly. Individual tumor cells displayed round or oval nuclei with finely granular chromatin pattern and inconspicuous small nucleoli. Occasionally psammoma bodies, nuclear pseudoinclusion or nuclear grooves were found. In schwannomas, tissue fragments were hard in consistency and difficult to crush. The crushed tissue presented as thick, irregular fragments with sharp borders. The cells showed ill-defined cytoplasm and round, oval, cigar-shaped or curved nuclei. It is important to emphasize that the smear pattern under low-power view and cytologic features are helpful in discriminating between these two tumors.
- Cytologic Features of Intracranial Germ Cell Tumors in Crush Preparation.
- Hyunee Yim, Jung Sun Kim, Chul Shim
- J Pathol Transl Med. 1996;7(2):177-184.
- 1,821 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - Intraoperative cytologic examination of intracranial tumors using crush preparation provides useful information in operative decision making. The diminutive nature of many biopsy specimens, particularly those obtained by stereotactic neurosurgical procedures emphasizes the importance of combining the cytologic smear method with conventional frozen section interpretation. The great advantage of the cytologic smear method resides in its suitability for the study of minute fragments of tissue, allowing retention of the majority of the specimen for optimal processing. We present the cytologic features of 3 cases of intracranial germ cell tumors(2 germinomas and 1 endodermal sinus tumor), using crush preparation during intrao perative diagnosis and compare them with histologic findings. The cytologic features of the germ cell tumors were similar to those of the respective gonadal counterparts. The cytologic differential diagnosis of both types of germ cell tumors is described.
- Prognostic Implications of Ki-67 Labelling Index and p53, bcl-2 Protein Expression in the Primary Central Nervous System Lymphoma.
- Jae Ho Han, Woo Ick Yang, Tai Seung Kim
- Korean J Pathol. 2000;34(6):456-464.
- 2,127 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - It has been claimed that CNS lymphoma, a rare neoplasm accounting for only a small fraction of malignant brain tumors, occurs with increasing frequency in immunologically normal as well as immunocompromised individuals. We investigated the prognostic value of Ki-67 index, p53, and bcl-2 oncoprotein expression in relation to the clinicopathological parameters in the primary CNS lymphoma patients. The tumors were graded by Kiel classification and the Working formulation and included 33 high-grade, 4 intermediate-grade, and 5 low-grade lymphomas. The phenotype was determined in 38 cases: 30 were B cell type and 8 were T cell type. All cases displayed variable degrees of nuclear Ki-67 staining from 1.0% to 92.0% (mean 51.1%). A highly significant correlation was established between the proportion of Ki-67 positive cells and the classification into grades (p=0.0002) and phenotypes (p=0.0002). Overexpression of p53 and bcl-2 protein was found in 37.1% and 51.4% of 35 patients, respectively. And p53 expression was significantly increased in B cell type (p=0.02). On Kaplan-Meier survival curve, the phenotype, grade of tumors, and p53 and bcl-2 protein expression were not correlated with overall survival. On multivariate analyses, overall survival was independently influenced by Ki-67 index. In conclusion, it is suggested that Ki-67 proliferating index is the most important marker for predicting biologic behavior of the primary CNS lymphoma.
- Primary Central Nervous System Lymphomas; A Clinicopathologic Study of 18 Cases.
- Yu Kyung Jeong, Young Hyeh Ko, Dong Kyu Na, Yeon Lim Suh, Sang Yong Song, Dae Shik Kim, Mi Kyung Kim, Howe Jung Ree
- Korean J Pathol. 1998;32(9):670-679.
- 2,179 View
- 10 Download
-
 Abstract
Abstract
- The incidence of a primary central nervous system (CNS) lymphoma in western countries is about 1% of all the intracranial tumors and has increased 2.2% over the last decade. A similar pattern of increased frequency is observed in Korea. Although most CNS lymphomas in western countries are high grade tumors carrying poor prognosis, the clinicopathologic features of the Korean CNS lymphoma have not been well studied. We report clinicopathological features of 18 cases of histologically proven primary brain lymphoma. The mean age of the patients was 50 years and there was no sex difference. The clinical and radiological characteristics included multiple site of occurrence, infrequent extracranial spread, and frequent seeding via cerebrospinal fluid. No patients were immune-compromised host. Of 18 cases, 15 cases were of B-lineage and 2 cases were of T-lineage. According to REAL classification, there were 12 cases of diffuse large B cell lymphoma, two cases of B cell lymphomas of small lymphoid cell, and two cases of peripheral T cell lymphoma, unspecified. The remaining subtypes were not subclassified because of inadequate material. Pleomorphic cytologic features and necrosis of varying extent were frequent in the cases of diffuse large B-cell lymphoma. These results suggest that overall clinicopathologic features of primary malignant lymphomas of the central nervous system in Korea are similar to those of western countries.
- Histologic and Immunopathologic Study of Central Nervous System Lymphoma.
- Yee Jeong Kim, Tae Seung Kim, Woo Ick Yang, Kyu Rae Kim
- Korean J Pathol. 1992;26(5):476-483.
- 2,022 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Twelve cases of primary malignant lymphoma of the central nervous system experienced between 1980 and 1990 were investigated by histological and immunohistochemical findings correlated with clinical observation. Of the 12 patients, 6 were male and 6 were female. Their ages ranged from 31 to 58 years(mean, 45.8 years). All Tumors were supratentorial except 1 case which was found in the spinal cord. The fronto-parietal lobe was the most common site, which accounted for 66.7%. Histologically, all the tumors showed unfavorable histology. Diffuse large cell type was the most frequent(66.7%). Immunohistochemical studies using monoclonal antibodies revealed predominance of B-cell phenotype. Although most cases were treated with a combination of surgery and irradiation, the outcome was poor in all.

 E-submission
E-submission

 First
First Prev
Prev



