Search
- Page Path
- HOME > Search
- Single umbilical artery and associated birth defects in perinatal autopsies: prenatal diagnosis and management
- Manushree Saxena, Bhagyashri Hungund
- J Pathol Transl Med. 2024;58(5):214-218. Published online July 9, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.03
- 1,687 View
- 255 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The umbilical cord forms the connection between the fetus and the placenta at the feto-maternal interface and normally comprises two umbilical arteries and one umbilical vein. In some cases, only a single umbilical artery (SUA) is present. This study was conducted to evaluate associations between SUA and other congenital malformations discovered in perinatal autopsies and to ascertain the existence of preferential associations between SUA and certain anomalies.
Methods
We evaluated records of all fetuses sent for autopsy to the Department of Pathology during the 10-year period from 2013 through 2022 (n = 1,277). The data were obtained from the hospital’s pathology laboratory records. The congenital anomalies were grouped by organ or system for analysis and included cardiovascular, urinary tract, nervous system, gastrointestinal tract, musculoskeletal, and lung anomalies.
Results
A SUA was present in 8.61% of the autopsies. The gestational age of the affected fetuses ranged between 13 to 40 weeks. An SUA presented as an isolated single anomaly in 44 cases (3.4%). Of the 110 SUA cases, 60% had other congenital anomalies. There was a significant association between birth defects and SUAs (p < .001). Strong associations between SUA and urinary tract, lung, and musculoskeletal anomalies were observed.
Conclusions
A SUA is usually seen in association with other congenital malformations rather than as an isolated defect. Therefore, examination for associated anomalies when an SUA is detected either antenatally or postnatally is imperative. The findings of this study should be helpful in counseling expectant mothers and their families in cases of SUA.
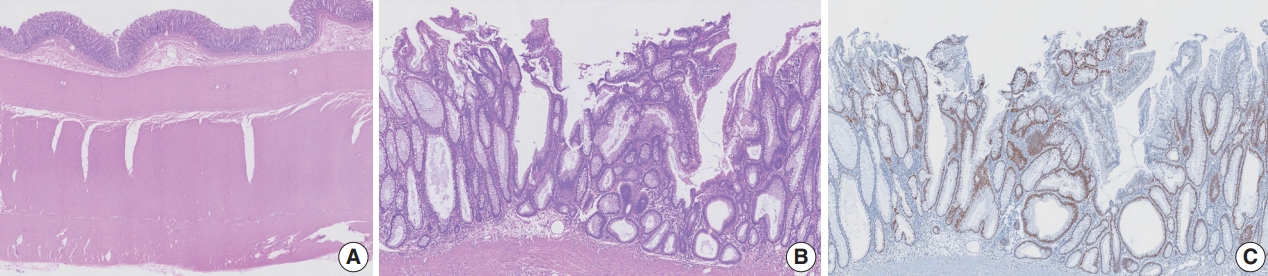
- Tubular adenoma arising in tubular colonic duplication: a case report
- Heonwoo Lee, Hyeong Rok An, Chan Wook Kim, Young Soo Park
- J Pathol Transl Med. 2024;58(4):198-200. Published online July 3, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.04
- 1,062 View
- 183 Download
-
 Abstract
Abstract
 PDF
PDF - Colonic duplication constitutes a rare congenital anomaly, characterized by the presence of hollow cystic or tubular structures exhibiting an epithelial-lined intestinal wall. Diagnostic challenges persist due to its low incidence and manifestation of nonspecific symptoms such as abdominal pain or constipation, resulting in a reluctance to pursue surgical resection. As associated malignancies in colonic duplication are rare, the inherent malignant potential of these anomalies remains undetermined. Additionally, despite reported instances of associated malignancies in colonic duplication, there is an absence of reports in the literature detailing tubular adenoma within these cases. The histologic features of the presented case are particularly noteworthy, situated at the precancerous stage, intimating potential progression towards adenocarcinoma within colonic duplication.
- Congenital Peribronchial Myofibroblastic Tumor: A Case Study and Literature Review
- Yuil Kim, Ha Young Park, Junhun Cho, Joungho Han, Eun Yoon Cho
- Korean J Pathol. 2013;47(2):172-176. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.172
- 7,485 View
- 60 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Congenital peribronchial myofibroblastic tumor (CPMT) is a benign pulmonary spindle cell neoplasm of intrauterine and perinatal period, which is thought to arise from primitive peribronchial mesenchyme. We present a case detected incidentally in a one-month-old infant. The solid and partially necrotic tumor involved the right middle and lower lobes of the lung with extension to the diaphragm. Histologically, the tumor was composed of fasciculated monotonous spindle cells, proliferating peribronchiolar cartilage and round cells with rich vasculature, and high mitotic activity was identified in the round cell area. Immunohistochemical and electron microscopic studies showed that the spindle cells were myofibroblastic in phenotype. Although the tumor showed several malignant pathological features, recurrence was not observed in the two-year follow-up period, consistent with the benign clinical behavior of CPMT.
-
Citations
Citations to this article as recorded by- Congenital peribronchial myofibroblastic tumor (CPMT): a case report with long term follow-up and next-generation sequencing (NGS)
Ping Zhou, Shuang Li, Weiya Wang, Yuan Tang, Lili Jiang
BMC Pediatrics.2023;[Epub] CrossRef - Neonatal congenital lung tumors — the importance of mid-second-trimester ultrasound as a diagnostic clue
Stephan L. Waelti, Laurent Garel, Dorothée Dal Soglio, Françoise Rypens, Michael Messerli, Josée Dubois
Pediatric Radiology.2017; 47(13): 1766. CrossRef - Congenital peribronchial myofibroblastic tumor: Case report and review of literature
Jolanta Jedrzkiewicz, Eric Scaife, Bo Hong, Sarah South, Mouied Alashari
Journal of Pediatric Surgery Case Reports.2015; 3(4): 154. CrossRef - Perinatal Thoracic Mass Lesions: Pre- and Postnatal Imaging
Evan J. Zucker, Monica Epelman, Beverley Newman
Seminars in Ultrasound, CT and MRI.2015; 36(6): 501. CrossRef - Prenatal imaging and immunohistochemical analysis of congenital peribronchial myofibroblastic tumor
Y.‐A. Tu, W.‐C. Lin, H.‐J. Chen, J.‐C. Shih
Ultrasound in Obstetrics & Gynecology.2015; 46(2): 247. CrossRef - A Congenital Peribronchial Myofibroblastic Tumor Detected in a Premature Infant at 28 Weeks but That Resolved in the Late Stage of Pregnancy
Bo Xia, Gang Yu, Chun Hong, Lei Zhang, Jing Tang, Cuifen Liu
Medicine.2015; 94(42): e1842. CrossRef - Congenital peribronchial myofibroblastic tumor
Yuka Hotokebuchi, Kenichi Kohashi, Satoshi Toyoshima, Naoko Matsumoto, Toshinori Nakashima, Yoshinao Oda
Pathology International.2014; 64(4): 189. CrossRef
- Congenital peribronchial myofibroblastic tumor (CPMT): a case report with long term follow-up and next-generation sequencing (NGS)
- Pathologic Review of Cystic and Cavitary Lung Diseases
- Na Rae Kim, Joungho Han
- Korean J Pathol. 2012;46(5):407-414. Published online October 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.407
- 16,809 View
- 299 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Pulmonary cystic and cavitary lesions caused by diverse etiologies are commonly encountered in chest imaging. The terms "cyst" and "cavity" are used to describe air-filled regions in the center of a nodule or consolidation of the lung. To date, only radiologic aspects of these lesions have been addressed. The morphologies of pulmonary cystic and cavitary lesions exhibit a broad spectrum, ranging from benign to malignant pulmonary diseases of acquired or congenital origin, including variable infectious diseases. In this review, we summarized the differential diagnosis of pathological entities to provide pathologists and radiologists with an overview of the diseases most commonly associated with pulmonary cystic and cavitary lesions in adults and children. The results showed slightly different patterns in the distribution of the diseases in the two groups. The most common causes of cavitary lesions include malignancy and infection in adults, and congenital malformation in children. Therefore, identification of pathologic entities correlating with the radiologic findings, clinical course, and location of the lesion is important in the evaluation of cystic and cavitary lung lesions in order to avoid unnecessary surgical procedures or delayed treatment.
-
Citations
Citations to this article as recorded by- Weakly-Supervised Segmentation-Based Quantitative Characterization of Pulmonary Cavity Lesions in CT Scans
Wenyu Xing, Yanping Yang, Yanan Zhou, Tao Jiang, Yifang Li, Yuanlin Song, Dongni Hou, Dean TA
IEEE Journal of Translational Engineering in Health and Medicine.2024; 12: 457. CrossRef - Chemotherapy-induced cavitating Wilms' tumor pulmonary metastasis: Active disease or scarring? A case report and literature review
Angelo Zarfati, Cristina Martucci, Alessandro Crocoli, Annalisa Serra, Giorgio Persano, Alessandro Inserra
Frontiers in Pediatrics.2023;[Epub] CrossRef - High-Resolution Computed Tomography of Cystic Lung Disease
Joanna E. Kusmirek, Cristopher A. Meyer
Seminars in Respiratory and Critical Care Medicine.2022; 43(06): 792. CrossRef - Miliary tuberculosis in a paediatric patient with psoriasis
Jacob Kilgore, Jonathon Pelletier, Bradford Becken, Stephen Kenny, Samrat Das, Lisa Parnell
BMJ Case Reports.2021; 14(3): e237580. CrossRef - Atypical pulmonary metastases in children: the spectrum of radiologic findings
Michal Scolnik, Luda Glozman, Ronen Bar-Yoseph, Michal Gur, Yazeed Toukan, Lea Bentur, Anat Ilivitzki
Pediatric Radiology.2021; 51(10): 1907. CrossRef - Radiographic and CT appearance of cavitary pulmonary lesions in a lamb
J Kan, J Bauquier, D Tyrrell, K O'Byrne, AW Stent, B Brosnan
Australian Veterinary Journal.2021; 99(12): 529. CrossRef - Community-acquired Achromobacter xylosoxidans infection presenting as a cavitary lung disease in an immunocompetent patient
Chan Hee Hwang, Woo Jin Kim, Hye Young Jwa, Sung Heon Song
Yeungnam University Journal of Medicine.2020; 37(1): 54. CrossRef - Clinical Research of Pulmonary Langerhans Cell Histiocytosis in Children
Dong Wang, Lei Cui, Zhi-Gang Li, Li Zhang, Hong-Yun Lian, Hong-Hao Ma, Yun-Ze Zhao, Xiao-Xi Zhao, Tian-You Wang, Rui Zhang
Chinese Medical Journal.2018; 131(15): 1793. CrossRef - Benign features of infection‐related tumor‐like lesions of the lung: A retrospective imaging review study
Chun‐Chao Huang, Sho‐Ting Hung, Wei‐Chin Chang, Chin‐Yin Sheu
Journal of Medical Imaging and Radiation Oncology.2017; 61(4): 481. CrossRef - Cavitary lung disease in renal transplant recipients: A single center experience
Gizem Kumru, Serkan Akturk, Siyar Erdogmus, Aysegul Gursoy Coruh, Acar Tuzuner, Sule Sengul, Kenan Keven
Transplantation Reports.2017; 2(4): 19. CrossRef - Solitary lung cavities: CT findings in malignant and non-malignant disease
C.S. Nin, V.V.S. de Souza, G.R.T. Alves, R.H. do Amaral, K.L. Irion, E. Marchiori, B. Hochhegger
Clinical Radiology.2016; 71(11): 1132. CrossRef - Radial endobronchial ultrasound with a guide sheath for diagnosis of peripheral cavitary lung lesions: a retrospective study
Manabu Hayama, Norio Okamoto, Hidekazu Suzuki, Motohiro Tamiya, Takayuki Shiroyama, Ayako Tanaka, Takuji Nishida, Takashi Nishihara, Nobuko Uehara, Naoko Morishita, Kunimitsu Kawahara, Tomonori Hirashima
BMC Pulmonary Medicine.2016;[Epub] CrossRef - An infant with a hyperlucent chest mass: An unexpected diagnosis
Zarmina Ehsan, Jaimie D. Nathan, Carolyn M. Kercsmar
Pediatric Pulmonology.2015; 50(12): E52. CrossRef - The Pseudocavitation Sign of Lung Adenocarcinoma
Tina D. Tailor, Rodney A. Schmidt, Keith D. Eaton, Douglas E. Wood, Sudhakar N. J. Pipavath
Journal of Thoracic Imaging.2015; 30(5): 308. CrossRef - A Case of Pulmonary Artery Sarcoma Presented as Cavitary Pulmonary Lesions
Daniel Min, Ji-Hyun Lee, Hye-Cheol Jeong, Jung-Hyun Kim, Suk-Pyo Shin, Hong-Min Kim, Kyu Hyun Han, Hye Yun Jeong, Eun-Kyung Kim
Tuberculosis and Respiratory Diseases.2014; 76(3): 136. CrossRef
- Weakly-Supervised Segmentation-Based Quantitative Characterization of Pulmonary Cavity Lesions in CT Scans
- Congenital Pulmonary Lymphangiectasia, Associated with Total Anomalous Pulmonary Venous Return.
- Seong Wook Hwang, Mee Seon Kim, Po Eun Park, Tae In Park
- Korean J Pathol. 2011;45(6):650-653.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.650
- 3,073 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF - Congenital pulmonary lymphangiectasia (CPL) is very rare. It shows diffuse pulmonary lymphatic dilatation without lymphatic proliferation. CPL can occur as a primary disorder or arise secondarily from other diseases such as the obstruction of pulmonary veins or lymphatics. The prognosis of CPL is very poor. Approximately 50% of infants are stillborn and most others usually die within the first day of life. The present case showed diffuse lymphangiectasia in the subpleural, interlobular, and peribronchovascular areas. The flat lining cells were immunohistochemically positive for D2-40 and CD31. CPL is usually diagnosed by clinicoradiological or postmortem examinations. However, our case was diagnosed by an antemortem lung biopsy. We report a case of CPL with total anomalous pulmonary venous return.
- Coexistence of Intrapulmonary Bronchogenic Cyst and Congenital Cystic Adenomatoid Malformation: A Case Report.
- Mee Hye Oh, Eun Ah Jung, Ji Hye Lee, Hyun Deuk Cho, Ki Hyun Seo, Seock Yeol Lee, Young Tong Kim
- Korean J Pathol. 2011;45(1):92-95.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.92
- 2,819 View
- 20 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Congenital cystic lesions of the lung are uncommon and a conjunction of two or more lesions is very rare. We report here on a case of coexisting intrapulmonary bronchogenic cyst and congenital cystic adenomatoid malformation in a 13-year-old female with a cystic mass in the right upper lobe of the lung. Computed tomography showed a cystic lesion measuring 2.5 cm with an air fluid level and surrounding multicystic lesions in the right upper lobe. On gross examination, the cut surface showed a cystic mass containing inspissated mucinous material, and the cystic mass was surrounded by multiple small cysts. Microscopically, the larger cystic cavity was lined with pseudostratified ciliated columnar epithelium. The submucosal tissue contained mucinous glands and plates of cartilage. The surrounding smaller cysts or irregular spaces were lined with bronchiolar-type respiratory epithelium. We propose that this hybrid lung lesion may represent the missing link in a common embryologic pathway determined by the timing of mesenchymal and epithelial interactions.
-
Citations
Citations to this article as recorded by- Case 2: Coexisting Cystic Lesions of Lung in a Term Neonate: A Management Dilemma
Bichitrananda Raut, Aakriti Soni, Susanta Kumar Badatya, Satish Saluja, Manoj Modi, Arun Soni
NeoReviews.2018; 19(9): e542. CrossRef
- Case 2: Coexisting Cystic Lesions of Lung in a Term Neonate: A Management Dilemma
- VATER Association: Three autopsy case reports with imusual defects.
- Mi Ja Lee, Myeong Cherl Kook, Je G Chi
- Korean J Pathol. 1995;29(5):678-683.
- 1,493 View
- 10 Download
-
 Abstract
Abstract
- VATER association represents vertebral defects, anal atresia, tracheo-esophageal fistula with without esophageal atresia, renal defects and radial limb dysplasia. The probability of the simultaneous occurrence of any three of these defects is so unlikely that it suggests a sporadic non-random association. This non-random association appears to be related to some chromosomal anomalies, the caudal regression syndrome, mesodermal defects in early developmental period or the matemal use of sex hormones during embryogenesis. We report three autopsy cases of the VATER association that showed most of the known major and minor defects as well as an unusual concurrence of other defects, i.e., scoliosis, talipes varus, absent penis, urethral agenesis and stenosis, rectourethral fistula, rib anomaly, single umbilical artery, Meckel's diverticulum, diaphragmatic hemia, absent rectum, short neck, simian crease, low set ear, and hypoplastic lung.
- Infantile Myofibromatosis(Congenital Generalized Fibromatosis): Associated with multiple congenital malformations and basaloid follicular hamartomas in the skin.
- Eun Sook Nam, Yoo Hun Kim, Han Kyeom Kim, Insun Kim, Je Geun Chi
- Korean J Pathol. 1995;29(6):776-782.
- 1,809 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Infantile myofibromatosis with systemic involvement is a very rare disease and is characterized by numerous nodules composed of spindle cells of a myofibroblastic nature. There are often disseminated throughout the subcutis, muscle, skeleton and viscera. We report an autopsy case of infantile myofibromatosis in a stillborn female fetus of 32 weeks of gestation. The nodules, Imm to 2 cm, were found over the whole body and viscera. The involved viscera were the heart, tongue, esophagus, gastrointestinal tract, portal areas of the liver, spleen anc pancreas. There were also associated malformations, viz., frontal meningoencephalocele, flexion defer-mities, syndactyly, cleft palate, agenesis of corpus callosum, pachygyria, diaphragmatic hemia, renal hypoplasia, etc. Multiple basaloid follicular hamartomas of the skin were noted on the face and extremeties. There are no previous reports in the literature of infantile myofibromatosis in conjunction with the above skin lesion and congenital malformations.
- Congenital Uterine Cyst: A case report.
- Chang Ho Cho
- Korean J Pathol. 1996;30(10):954-956.
- 1,695 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - I experienced a case of a congenital intramural cyst of the uterine fundus. On examination by light and electron microscope it was composed of a single layer of thin atrophied lining epithelium without secretory activity and was found to be derived from the paramesonephric duct. This case is presented with a brief review of the literature.
- Congenital Anomalies Observed by Autopsies at the Seoul National University Children's Hospital.
- Jin Haeng Chung, Jeong Wook Seo, Chong Jai Kim, Chul Woo Kim, Je G Chi
- Korean J Pathol. 1997;31(2):93-99.
- 1,584 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - A retrospective analysis was performed on the 968 cases of fetal or pediatric autopsies over five year period (1990-1994), at the Seoul National University Children's Hospital. Age/mode distribution of cases were artificial abortus(30.6%), spontaneous abortus(12.0%), stillbirth(21.9%), neonates(29%), infants(2.8%) and children(0.9%). Male/female ratio was 1.21. Overall incidence of congenital anomalies was 60.8% and 34.0% of all cases had anomalies involving multiple organ systems. Percentage of cases with any anomaly was 71.6% in artificial abortus, 35.3% in spontaneous abortus, 59% in still births, 65.5% in neonates and 38.9% in infant and children. Common organ systems involved were the cardiovascular system (39.0%), musculoskeletal system (23.6%), nervous system (22.6%), gastrointestinal system (19.9%), and urinary system (14.6%). From these results, we found that the congenital anomalies were most significant diseases of the perinatal period and the cardiovascular anomalies were the most common anomalies of them.
- Congenital Cystic Disease of the Kidney overview and a classification.
- Mee Joo, Yeon Mee Kim, Chong Jai Kim, Yeon Lim Suh, Jeong Wook Seo, Je Geun Chi
- Korean J Pathol. 1997;31(3):233-243.
- 1,558 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - The congenital renal cystic disease encompasses a complex group of pathologic and clinical entities. We retrospectively reviewed 42 cases of congenital renal cystic lesions classified into four Potter types in a series of 2,063 consecutive autopsies from 1981 to 1996. According to our study based on morphologic, clinical, genetic features and associated anomalies, type I and III are relatively compatible with Potter's original definition. However, it was reasonable that type II and IV are classified to the same group because of: 1) very similar histologic findings representing dysplastic kidney, 2) many associated anomalies, 3) no evidence of inheritance, and 4) presence of a combined type. Syndrome associated cysts, such as Meckel-Gruber syndrome, were also separately classified. If the dysplastic evidence was insufficient for diagnosis to the dysplastic kidney in type II and IV, then these cases would be better classified into a cystic disease associated with congenital hydronephrosis. We propose a classification of the congenital cystic disease of the kidney to be: 1) dysplastic kidney, 2) cystic disease associated with congenital hydronephrosis, 3) polycystic kidney, and 4) syndromic cystic disease.
- Congenital Hepatic Fibrosis with Caroli's Disease.
- Yoon Jung Kim, Soon Ae Oak, In Chul Lee
- Korean J Pathol. 1997;31(3):275-279.
- 1,591 View
- 15 Download
-
 Abstract
Abstract
 PDF
PDF - Congenital hepatic fibrosis is an inherited, congenital disorder of the liver, and is occasionally associated with cystic disease of the liver and kidney. We present a case of congenital hepatic fibrosis with Caroli's disease. A 21-year-old woman had suffered from an episodic fever with headaches for 3 years. In laboratory examination, the liver function test was within the normal limits. Esophageal varix was noted by an endoscopic examination. Hepatosplenomegaly and multiple dilated bile ducts were seen by abdominal CT scanning. An orthotopic whole liver transplantation was done. The liver was fibrotic and enlarged. Multiple cystically dilated intrahepatic ducts were noted. Microscopically, diffuse portal fibrosis and widening with proliferation of bile ductules were seen. Intrahepatic bile ducts were markedly dilated and tortuous. The liver cell cords were well preserved.
- Congenital Mesoblastic Nephroma.
- Seok Hoon Jeon, Seung Sam Paik, Nam Hoon Kim, Moon Hyang Park, Jung Dal Lee
- Korean J Pathol. 1997;31(4):375-378.
- 1,671 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Mesoblastic nephroma is an important differential diagnosis of a renal mass occurring in the neonatal period or in early childhood. It is a rare monomorphous congenital renal neoplasm most commonly recognized during the first 3 months of life. With the widespread application of ultrasound imaging, many cases are recognized prior to birth. We report a case of mesoblastic nephroma detected by ultrasonograph at 36 weeks of intrauterine fetal life and removed after birth. It showed a well circumscribed, grayish white, solid mass measuring 4x3x2 cm. The tumor was predominantly a classic type with a focal cellular pattern. Immunohistochemical and electron microscopic studies were done.
- Achondrogenesis Type 2: An autopsy case.
- Joon Mee Kim, Young Chae Chu, Soo Kee Min, Hee Jeung Cha, Je Geun Chi
- Korean J Pathol. 1997;31(5):482-488.
- 1,983 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Achondrogenesis type 2 is a lethal form of congenital skeletal dysplasia characterized by severe short-limbed dwarfism, decreased vertebral ossification and normal ossification of the skull. We report an autopsy case of achondrogenesis type 2 in a female fetus terminated at 29 weeks of gestation. External morphology revealed a relatively large head, short upper and lower extremities, short neck, and distended abdomen. The x-ray finding showed normal calvarial ossification, hypoplastic ilium and unossified ischium, and metaphyseal flares of the femur and tibia. Histologically, chondrocytes were large and irregular with increased vascularity.
- A Sialoblastoma Associated with a Hepatoblastoma: An autopsy case report.
- Sun Lee, Youn Wha Kim, Jae Hoon Park, Yong Koo Park, Ju hie Lee, Moon Ho Yang
- Korean J Pathol. 1997;31(11):1222-1226.
- 1,830 View
- 10 Download
-
 Abstract
Abstract
- Sialoblastoma is defined as a rare, congenital or perinatal, aggressive and potentially low-grade malignant, basaloid gland neoplasm that occurs in the major salivary glands. We report a case of a congenital sialoblastoma in the left parotid gland, associated with a hepatoblastoma in a female infant. At birth, a huge mass in the left neck and hepatomegaly were noted. Grossly, the neck mass was well-circumscribed, lobulated and gray tan. Microscopically, the tumor was composed of basaloid aggregates of primitive uniform cells with focal ductal differentiation. The liver showed a well-circumscribed gray tan tumor with extensive hemorrhage and cystic change. Microscopically, the liver revealed characteristic findings of hepatoblastoma. To the best of our knowledge, this is the first case of coexistence of a congenital sialoblastoma and a hepatoblastoma, reported in the literature.

 E-submission
E-submission


 First
First Prev
Prev



