Search
- Page Path
- HOME > Search
- Immunohistochemical expression in idiopathic inflammatory myopathies at a single center in Vietnam
- Dat Quoc Ngo, Si Tri Le, Khanh Hoang Phuong Phan, Thao Thi Phuong Doan, Linh Ngoc Khanh Nguyen, Minh Hoang Dang, Thien Thanh Ly, Thu Dang Anh Phan
- J Pathol Transl Med. 2024;58(4):174-181. Published online June 25, 2024
- DOI: https://doi.org/10.4132/jptm.2024.05.02
- 4,448 View
- 270 Download
- 1 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The identification of idiopathic inflammatory myopathies (IIMs) requires a comprehensive analysis involving clinical manifestations and histological findings. This study aims to provide insights into the histopathological and immunohistochemical aspects of IIMs.
Methods
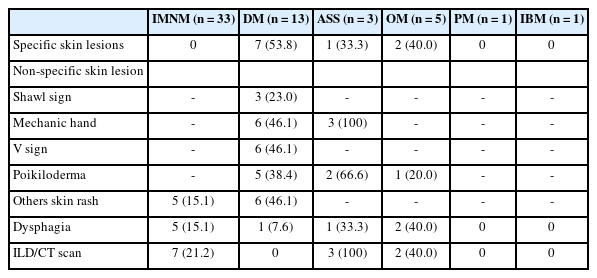
This retrospective case series involved 56 patients diagnosed with IIMs at the Department of Pathology, University of Medicine and Pharmacy at Ho Chi Minh City, from 2019 to 2023. The histology and immunohistochemical expression of HLA-ABC, HLA-DR, C5b-9, Mx1/2/3, and p62 were detected.
Results
We examined six categories of inflammatory myopathy, including immunemediated necrotizing myopathy (58.9%), dermatomyositis (DM; 23.2%), overlap myositis (8.9%), antisynthetase syndrome (5.4%), inclusion body myositis (IBM; 1.8%), and polymyositis (1.8%). The average age of the patients was 49.7 ± 16.1 years, with a female-to-male ratio of 3:1. Inflammatory cell infiltration in the endomysium was present in 62.5% of cases, perifascicular atrophy was found in 17.8%, and fiber necrosis was observed in 42 cases (75.0%). Rimmed vacuoles were present in 100% of cases in the IBM group. Immunohistochemistry showed the following positivity rates: HLA-ABC (89.2%), HLA-DR (19.6%), C5b-9 (57.1%), and Mx1/2/3 (10.7%). Mx1/2/3 expression was high in DM cases. p62 vacuole deposits were noted in the IBM case. The combination of membrane attack complex and major histocompatibility complex I helped detect IIMs in 96% of cases.
Conclusions
The diagnosis of IIMs and their subtypes should be based on clinical features and histopathological characteristics. Immunohistochemistry plays a crucial role in the diagnosis and differentiation of these subgroups. -
Citations
Citations to this article as recorded by- Evaluating the Diagnostic Potential of Myxovirus Resistance Protein 1 (MX1) and Myxovirus Resistance Protein 2 (MX2) As Biomarkers in Idiopathic Inflammatory Myopathies
Raghavee Neupane, Mustafa Haider, Perry Smith, Marc M Kesselman
Cureus.2026;[Epub] CrossRef - Rapidly Progressive Polymyositis With Vasculitis: The Pivotal Role of Histopathology in Diagnosis and Management
Amitha Venmanassery Karnalsingh, Arjun Karappilly Vijayan, Monica Roselin Edwin Peter, Dilan Davis
Cureus.2025;[Epub] CrossRef - Autoimmune Neuromuscular Disorders at a Molecular Crossroad: Linking Pathogenesis to Targeted Immunotherapy
Anca-Maria Florea, Dimela-Gabriela Luca, Eugenia Irene Davidescu, Bogdan-Ovidiu Popescu
International Journal of Molecular Sciences.2025; 26(23): 11736. CrossRef
- Evaluating the Diagnostic Potential of Myxovirus Resistance Protein 1 (MX1) and Myxovirus Resistance Protein 2 (MX2) As Biomarkers in Idiopathic Inflammatory Myopathies
- Diagnosis of interstitial lung diseases: from Averill A. Liebow to artificial intelligence
- Eunhee S. Yi, Paul Wawryko, Jay H. Ryu
- J Pathol Transl Med. 2024;58(1):1-11. Published online January 10, 2024
- DOI: https://doi.org/10.4132/jptm.2023.11.17
- 7,780 View
- 437 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Histopathologic criteria of usual interstitial pneumonia (UIP)/idiopathic pulmonary fibrosis (IPF) were defined over the years and endorsed by leading organizations decades after Dr. Averill A. Liebow first coined the term UIP in the 1960s as a distinct pathologic pattern of fibrotic interstitial lung disease. Novel technology and recent research on interstitial lung diseases with genetic component shed light on molecular pathogenesis of UIP/IPF. Two antifibrotic agents introduced in the mid-2010s opened a new era of therapeutic approaches to UIP/IPF, albeit contentious issues regarding their efficacy, side effects, and costs. Recently, the concept of progressive pulmonary fibrosis was introduced to acknowledge additional types of progressive fibrosing interstitial lung diseases with the clinical and pathologic phenotypes comparable to those of UIP/IPF. Likewise, some authors have proposed a paradigm shift by considering UIP as a stand-alone diagnostic entity to encompass other fibrosing interstitial lung diseases that manifest a relentless progression as in IPF. These trends signal a pendulum moving toward the tendency of lumping diagnoses, which poses a risk of obscuring potentially important information crucial to both clinical and research purposes. Recent advances in whole slide imaging for digital pathology and artificial intelligence technology could offer an unprecedented opportunity to enhance histopathologic evaluation of interstitial lung diseases. However, current clinical practice trends of moving away from surgical lung biopsies in interstitial lung disease patients may become a limiting factor in this endeavor as it would be difficult to build a large histopathologic database with correlative clinical data required for artificial intelligence models.
-
Citations
Citations to this article as recorded by- Identification of early genes in the pathophysiology of fibrotic interstitial lung disease in a new model of pulmonary fibrosis
Nathan Hennion, Corentin Bedart, Léonie Vandomber, Frédéric Gottrand, Sarah Humez, Cécile Chenivesse, Jean-Luc Desseyn, Valérie Gouyer
Cellular and Molecular Life Sciences.2025;[Epub] CrossRef - Radiological Insights into UIP Pattern: A Comparison Between IPF and Non-IPF Patients
Stefano Palmucci, Miriam Adorna, Angelica Rapisarda, Alessandro Libra, Sefora Fischetti, Gianluca Sambataro, Letizia Antonella Mauro, Emanuele David, Pietro Valerio Foti, Claudia Mattina, Corrado Spatola, Carlo Vancheri, Antonio Basile
Journal of Clinical Medicine.2025; 14(12): 4162. CrossRef
- Identification of early genes in the pathophysiology of fibrotic interstitial lung disease in a new model of pulmonary fibrosis
- Idiopathic Noncirrhotic Portal Hypertension: An Appraisal
- Hwajeong Lee, Aseeb Ur Rehman, M. Isabel Fiel
- J Pathol Transl Med. 2016;50(1):17-25. Published online November 11, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.23
- 23,567 View
- 329 Download
- 30 Web of Science
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF - Idiopathic noncirrhotic portal hypertension is a poorly defined clinical condition of unknown etiology. Patients present with signs and symptoms of portal hypertension without evidence of cirrhosis. The disease course appears to be indolent and benign with an overall better outcome than cirrhosis, as long as the complications of portal hypertension are properly managed. This condition has been recognized in different parts of the world in diverse ethnic groups with variable risk factors, resulting in numerous terminologies and lack of standardized diagnostic criteria. Therefore, although the diagnosis of idiopathic noncirrhotic portal hypertension requires clinical exclusion of other conditions that can cause portal hypertension and histopathologic confirmation, this entity is under-recognized clinically as well as pathologically. Recent studies have demonstrated that variable histopathologic entities with different terms likely represent a histologic spectrum of a single entity of which obliterative portal venopathy might be an underlying pathogenesis. This perception calls for standardization of the nomenclature and formulation of widely accepted diagnostic criteria, which will facilitate easier recognition of this disorder and will highlight awareness of this entity.
-
Citations
Citations to this article as recorded by- Nodular regenerative hyperplasia: The role of the CK7 immunohistochemistry pattern of expression in diagnosis
Brooke B Bartow, Deepti Dhall, Goo Lee, Manjula Garapati, Chirag R Patel, Sameer Al Diffalha
American Journal of Clinical Pathology.2025; 163(2): 196. CrossRef - The potential roles of gut microbiome in porto-sinusoidal vascular disease: an under-researched crossroad
Yangjie Li, Lingna Lyu, Huiguo Ding
Frontiers in Microbiology.2025;[Epub] CrossRef - A Case of Non-cirrhotic Portal Hypertension With Antiphospholipid Syndrome
Mili Shah, Razia Gill, Priya Hotwani, Hamsika Moparty, Naresh Kumar, Dhir Gala, Vikash Kumar
Cureus.2024;[Epub] CrossRef - Systemic Disease and Portal Hypertension
Talal Khurshid Bhatti, Paul Y. Kwo
Current Hepatology Reports.2024; 23(1): 162. CrossRef - Porto-sinusoidal Vascular Disease: Classification and Clinical Relevance
Madhumita Premkumar, Anil C. Anand
Journal of Clinical and Experimental Hepatology.2024; 14(5): 101396. CrossRef - Evaluation of the histologic and immunohistochemical (CD34, glutamine synthetase) findings in idiopathic non-cirrhotic portal hypertension (INCPH)
Melek Büyük, Neslihan Berker, Doğu Vurallı Bakkaloğlu, İbrahim Volkan Şenkal, Zerrin Önal, Mine Güllüoğlu
Hepatology International.2024; 18(3): 1011. CrossRef - Porto-sinusoidal Vascular Disease and Portal Hypertension
Sarah Noble, Marguerite Linz, Eduardo Correia, Akram Shalaby, Leonardo Kayat Bittencourt, Seth N. Sclair
Clinics in Liver Disease.2024; 28(3): 455. CrossRef - Histopathological features of idiopathic portal hypertension: A systematic review and meta-analysis
Adnan Malik, Sohira Malik, Ahsan Farooq, Muhammad Imran Malik, Sadia Javaid
Science Progress.2024;[Epub] CrossRef - Porto-Sinusoidal Vascular Disease: A Concise Updated Summary of Epidemiology, Pathophysiology, Imaging, Clinical Features, and Treatments
Su Jin Jin, Won-Mook Choi
Korean Journal of Radiology.2023; 24(1): 31. CrossRef - Aetiology and clinical outcomes of non-cirrhotic portal hypertension in Singapore
PikEu Jason Chang, KimJun Kevin Teh, Mithun Sharma
Singapore Medical Journal.2023;[Epub] CrossRef - A Unique Presentation of Familial Idiopathic Colonic Varices
John Gallagher, Bill Quach, Tomoki Sempokuya, Anita Sivaraman
ACG Case Reports Journal.2023; 10(11): e01185. CrossRef - Obliterative Portal Venopathy
Thomas D. Schiano, Maria Isabel Fiel
Current Hepatology Reports.2023; 22(4): 263. CrossRef - Case report: Oxaliplatin-induced idiopathic non-cirrhotic portal hypertension: a case report and literature review
Jiayuan Ye, Yilian Xie, Yaojiang Xu, Nan Chen, Yifei Tu
Frontiers in Medicine.2023;[Epub] CrossRef - Clinical Course of Porto-Sinusoidal Vascular Disease Is Distinct From Idiopathic Noncirrhotic Portal Hypertension
Katharina Wöran, Georg Semmler, Mathias Jachs, Benedikt Simbrunner, David Josef Maria Bauer, Teresa Binter, Katharina Pomej, Albert Friedrich Stättermayer, Philipp Schwabl, Theresa Bucsics, Rafael Paternostro, Katharina Lampichler, Matthias Pinter, Michae
Clinical Gastroenterology and Hepatology.2022; 20(2): e251. CrossRef - Porto-sinusoidal vascular disorder
Andrea De Gottardi, Christine Sempoux, Annalisa Berzigotti
Journal of Hepatology.2022; 77(4): 1124. CrossRef - Interventional Management of Portal Hypertension in Cancer Patients
Max Kabolowsky, Lyndsey Nguyen, Brett E. Fortune, Ernesto Santos, Sirish Kishore, Juan C. Camacho
Current Oncology Reports.2022; 24(11): 1461. CrossRef - Pathological and imaging features of idiopathic non-cirrhotic portal hypertension
Ming-Jie Tan, Hui Liu, Hui-Guo Ding
World Chinese Journal of Digestology.2022; 30(16): 729. CrossRef - Bioinformatics Analysis of Common Genetic and Molecular Traits and Association of Portal Hypertension with Pulmonary Hypertension
MingYu Chen, YouPeng Chen, Ikram Ud Din
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - Key histopathologic features in idiopathic noncirrhotic portal hypertension: an interobserver agreement study and proposal for diagnostic criteria
Jiancong Liang, Chanjuan Shi, William D. Dupont, Safia N. Salaria, Won Jae Huh, Hernan Correa, Joseph T. Roland, Roman E. Perri, Mary Kay Washington
Modern Pathology.2021; 34(3): 592. CrossRef - Histological analyses of trucut liver biopsies from patients with noncirrhotic portal fibrosis and extra-hepatic portal vein obstruction
ArchanaGeorge Vallonthaiel, Vandana Baloda, Lavleen Singh, Rajni Yadav, Ragini Kilambi, Sudha Battu, Vishnubhatla Sreenivas, Sujoy Pal, SubratK Acharya, Siddhartha DattaGupta, Shalimar, Prasenjit Das
Indian Journal of Pathology and Microbiology.2021; 64(5): 127. CrossRef - Nodular regenerative hyperplasia – An under-recognized vascular disorder of liver
Neha Bakshi, Natasha Gulati, Archana Rastogi, Abhijit Chougule, Chhagan Bihari, Ankur Jindal
Pathology - Research and Practice.2020; 216(4): 152833. CrossRef - Interobserver study on histologic features of idiopathic non-cirrhotic portal hypertension
Michel Kmeid, Chunlai Zuo, Stephen M. Lagana, Won-Tak Choi, Jingmei Lin, Zhaohai Yang, Xiuli Liu, Maria Westerhoff, M. Isabel Fiel, Kajsa Affolter, Eun-Young K. Choi, Hwajeong Lee
Diagnostic Pathology.2020;[Epub] CrossRef - Histology of portal vascular changes associated with idiopathic non‐cirrhotic portal hypertension: nomenclature and definition
Maria Guido, Venancio A F Alves, Charles Balabaud, Prithi S Bathal, Paulette Bioulac‐Sage, Romano Colombari, James M Crawford, Amar P Dhillon, Linda D Ferrell, Ryan M Gill, Prodromos Hytiroglou, Yasuni Nakanuma, Valerie Paradis, Alberto Quaglia, Pierre E
Histopathology.2019; 74(2): 219. CrossRef - Idiopathic noncirrhotic portal hypertension
M. Isabel Fiel, Thomas D. Schiano
Seminars in Diagnostic Pathology.2019; 36(6): 395. CrossRef - Pathology of idiopathic non-cirrhotic portal hypertension
Maria Guido, Samantha Sarcognato, Diana Sacchi, Guido Colloredo
Virchows Archiv.2018; 473(1): 23. CrossRef - Spectrum of histopathological changes in patients with non-cirrhotic portal fibrosis
Abhijit Chougule, Archana Rastogi, Rakhi Maiwall, Chhagan Bihari, Vikrant Sood, Shiv Kumar Sarin
Hepatology International.2018; 12(2): 158. CrossRef - Hepatocellular nodules in vascular liver diseases
Christine Sempoux, Charles Balabaud, Valérie Paradis, Paulette Bioulac-Sage
Virchows Archiv.2018; 473(1): 33. CrossRef - Systemic lupus erythematosus complicated by noncirrhotic portal hypertension: A case report and review of literature
Qi-Bin Yang, Yong-Long He, Chun-Mei Peng, Yu-Feng Qing, Qi He, Jing-Guo Zhou
World Journal of Clinical Cases.2018; 6(13): 688. CrossRef - Prevalence of histological features of idiopathic noncirrhotic portal hypertension in general population: a retrospective study of incidental liver biopsies
Chunlai Zuo, Vaibhav Chumbalkar, Peter F. Ells, Daniel J. Bonville, Hwajeong Lee
Hepatology International.2017; 11(5): 452. CrossRef - The pathological differential diagnosis of portal hypertension
Raouf E. Nakhleh
Clinical Liver Disease.2017; 10(3): 57. CrossRef - Hepatic vascular diseases
Naziheh Assarzadegan, Robert A. Anders, Kiyoko Oshima
Diagnostic Histopathology.2017; 23(12): 553. CrossRef
- Nodular regenerative hyperplasia: The role of the CK7 immunohistochemistry pattern of expression in diagnosis
- Usual Interstitial Pneumonia with Lung Cancer: Clinicopathological Analysis of 43 Cases
- Dae Hyun Song, In Ho Choi, Sang Yun Ha, Kang Min Han, Jae Jun Lee, Min Eui Hong, Kyeongman Jeon, Man Pyo Chung, Jhingook Kim, Joungho Han
- Korean J Pathol. 2014;48(1):10-16. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.10
- 11,272 View
- 79 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Previous studies have suggested an association between usual interstitial pneumonia (UIP) and lung cancer (Ca). However, clinical and histological information is not enough to determine such an association, due to the low incidence and short survival time of patients with both conditions.
Methods We retrospectively reviewed the clinical and histological records of Ca patients with UIP between January 1999 and August 2013 at the Samsung Medical Center, Seoul, Korea. We found 43 patients who had Ca with UIP (UIP-Ca). Previously reported data of eighty-four patients with UIP-only were included as a comparison group.
Results Smoking is related to poor prognosis in patients with UIP-Ca, and the number of patients with a high smoking index of more than 30 pack-years significantly increased in UIP-Ca patients compared with UIP-only patients. There is no significant prognostic differentiation between UIP-Ca patients and UIP-only patients. Microscopically, UIP-Ca patients showed characteristically heterogeneous histological patterns and degrees of differentiation. There were many foci of squamous metaplasia or dysplasia at the peripheral area of squamous cell carcinomas.
Conclusions We report 43 cases of UIP-Ca. Our results suggest that smoking is related to cancer occurrence in UIP patients and poor prognosis in UIP-Ca patients.
-
Citations
Citations to this article as recorded by- Treatable traits in interstitial lung disease: a narrative review
Megan Harrison, Chloe Lawler, Fiona Lake, Vidya Navaratnam, Caitlin Fermoyle, Yuben Moodley, Tamera J. Corte
Therapeutic Advances in Respiratory Disease.2025;[Epub] CrossRef - Usual Interstitial Pneumonia and Lung Cancer
Lamiyae Senhaji, Meryem Karhate, Abir Bouhamdi, Mounia Serraj, Mohamed ElBiaze, Mohammed Chakib Benjelloun, Badreddine Alami, Bouchra Amara
Cureus.2025;[Epub] CrossRef - Prognosis of idiopathic pulmonary fibrosis without anti-fibrotic therapy: a systematic review
Yet H. Khor, Yvonne Ng, Hayley Barnes, Nicole S.L. Goh, Christine F. McDonald, Anne E. Holland
European Respiratory Review.2020; 29(157): 190158. CrossRef - Linfoma difuso de células B grandes pulmonar en paciente con neumonía intersticial no específica
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica.2019; 15(6): e151. CrossRef - Diffuse Large B-cell Lymphoma of the Lung in a Patient With Nonspecific Interstitial Pneumonia
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica (English Edition).2019; 15(6): e151. CrossRef - Characteristics of lung cancer among patients with idiopathic pulmonary fibrosis and interstitial lung disease – analysis of institutional and population data
Joo Heung Yoon, Mehdi Nouraie, Xiaoping Chen, Richard H Zou, Jacobo Sellares, Kristen L Veraldi, Jared Chiarchiaro, Kathleen Lindell, David O Wilson, Naftali Kaminski, Timothy Burns, Humberto Trejo Bittar, Samuel Yousem, Kevin Gibson, Daniel J Kass
Respiratory Research.2018;[Epub] CrossRef - Genomic profiles of lung cancer associated with idiopathic pulmonary fibrosis
Ji An Hwang, Deokhoon Kim, Sung‐Min Chun, SooHyun Bae, Joon Seon Song, Mi Young Kim, Hyun Jung Koo, Jin Woo Song, Woo Sung Kim, Jae Cheol Lee, Hyeong Ryul Kim, Chang‐Min Choi, Se Jin Jang
The Journal of Pathology.2018; 244(1): 25. CrossRef - Survival after repeated surgery for lung cancer with idiopathic pulmonary fibrosis: a retrospective study
Seijiro Sato, Yuki Shimizu, Tatsuya Goto, Akihiko Kitahara, Terumoto Koike, Hiroyuki Ishikawa, Takehiro Watanabe, Masanori Tsuchida
BMC Pulmonary Medicine.2018;[Epub] CrossRef - Alveolar Squamous Cell Metaplasia: Preneoplastic Lesion?
Adriana Handra-Luca
Journal of Pathology and Translational Medicine.2018; 52(6): 355. CrossRef - Low expression of long noncoding RNA CDKN2B-AS1 in patients with idiopathic pulmonary fibrosis predicts lung cancer by regulating the p53-signaling pathway
Yufeng Du, Xiaoyan Hao, Xuejun Liu
Oncology Letters.2018;[Epub] CrossRef - A clinicopathological study of surgically resected lung cancer in patients with usual interstitial pneumonia
Yasutaka Watanabe, Yoshinori Kawabata, Nobuyuki Koyama, Tomohiko Ikeya, Eishin Hoshi, Noboru Takayanagi, Shinichiro Koyama
Respiratory Medicine.2017; 129: 158. CrossRef - Risk of the preoperative underestimation of tumour size of lung cancer in patients with idiopathic interstitial pneumonias
Mariko Fukui, Kazuya Takamochi, Takeshi Matsunaga, Shiaki Oh, Katsutoshi Ando, Kazuhiro Suzuki, Atsushi Arakawa, Toshimasa Uekusa, Kenji Suzuki
European Journal of Cardio-Thoracic Surgery.2016; 50(3): 428. CrossRef - The Idiopathic Interstitial Pneumonias: Histology and Imaging
Diane C. Strollo, Teri J. Franks, Jeffrey R. Galvin
Seminars in Roentgenology.2015; 50(1): 8. CrossRef - Do Chest Expansion Exercises Aid Re‐shaping the Diaphragm Within the First 72 Hours Following Lung Transplantation in a Usual Interstitial Pneumonia Patient?
Massimiliano Polastri, Erika Venturini, Saverio Pastore, Andrea Dell'Amore
Physiotherapy Research International.2015; 20(3): 191. CrossRef - Scrotal wall metastasis from a primary lung adenocarcinoma
Marie-Louise M. Coussa-Koniski, Pia A. Maalouf, Nehme E. Raad, Noha A. Bejjani
Respiratory Medicine Case Reports.2015; 15: 77. CrossRef - The Ratio KL-6 to SLX in Serum for Prediction of the Occurrence of Drug-Induced Interstitial Lung Disease in Lung Cancer Patients with Idiopathic Interstitial Pneumonias Receiving Chemotherapy
Kosuke Kashiwabara, Hiroshi Semba, Shinji Fujii, Shinsuke Tsumura, Ryota Aoki
Cancer Investigation.2015; 33(10): 516. CrossRef - Idiopathic pulmonary fibrosis will increase the risk of lung cancer
Li Junyao, Yang Ming, Li Ping, Su Zhenzhong, Gao Peng, Zhang Jie
Chinese Medical Journal.2014; 127(17): 3142. CrossRef
- Treatable traits in interstitial lung disease: a narrative review
- Idiopathic Duct Centric Pancreatitis in Korea: A Clinicopathological Study of 14 Cases.
- Hyo Jeong Kang, Tae Jun Song, Eunsil Yu, Jihun Kim
- Korean J Pathol. 2011;45(5):491-497.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.5.491
- 4,231 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Idiopathic duct centric pancreatitis (IDCP) is a subtype of autoimmune pancreatitis (AIP) that is histologically characterized by granulocytic epithelial lesion and scarce IgG4-positive cells. This subtype of AIP has not been documented in Asian countries.
METHODS
We reviewed 38 histologically confirmed AIP cases and classified them into lymphoplasmacytic sclerosing pancreatitis (LPSP) and IDCP. Then, clinicopathological characteristics were compared between LPSP and IDCP.
RESULTS
Fourteen cases (36.8%) were IDCP. IDCP affected younger patients more than LPSP. IDCP was associated with ulcerative colitis in 35.7% of cases, whereas LPSP was associated with IgG4-related sclerosing diseases such as cholangitis, retroperitoneal fibrosis or sialadenitis in 41.7% of cases. IDCP was microscopically characterized by neutrophilic ductoacinitis with occasional granulocytic epithelial lesions, whereas LPSP was characterized by storiform inflammatory cell-rich fibrosis and obliterative phlebitis. IgG4-positive cells were not detected in any IDCP case but more than 20 IgG4-positive cells per high-power-field were invariably detected in LPSP cases. All patients with IDCP responded dramatically to steroids without recurrence, whereas 33.3% of patients with LPSP developed recurrences.
CONCLUSIONS
IDCP is clinicopathologically distinct from LPSP and can be diagnosed when neutrophilic ductoacinitis or granulocytic epithelial lesions are observed in a pancreatic biopsy under the appropriate clinical setting.
- Expression of Glomerular-Smooth Muscle Actin and Vimentin in Idiopathic Membranous Nephropathy as Prognostic Indicators.
- Min Jin Lee, Ok Kyung Kim
- Korean J Pathol. 2001;35(1):26-34.
- 2,172 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The natural history of idiopathic membranous nephropathy (IMN) is heterogeneous with some patients showing spontaneous remission while others show a progressive course leading to end-stage renal failure. We tried to assess quantitatively alpha-smooth muscle actin (alpha-SMA) and vimentin expression as markers to predict the outcome of membranous nephropathy.
METHODS
This study included 24 patients with biopsy proven IMN. We measured the volume of the positive area for alpha-SMA and vimentin within the glomeruli and compared the results with 5 patients in the normal control group. We evaluated glomerular alpha-SMA and vimentin expression in correlation with BUN and serum creatinine level at the time of diagnosis and after treatment.
RESULTS
Glomerular alpha-SMA and vimentin in IMN were higher than in the control group. Glomerular alpha-SMA was significantly higher in progressive IMN than in non-progressive IMN. The glomerular alpha-SMA was sifnificantly correlated with BUN and serum creatinine at last follow-up (p<0.05), but there was no statistically significant correlation at diagnosis. The glomerular vimentin was not different between progressive and non-progressive groups.
CONCLUSION
These data suggest that the expression of glomerular alpha-SMA may be a useful prognostic indicator and may be able to differentiate between patients with membranous nephropathy who respond well to treatment and those who continue to progress.
- Chronic Hepatitis in the Idiopathic Hypereosinophilic Syndrome: A case report .
- Kyeong Hee Kim, Hae Joung Sul, Sung Chul Jun, Dae Young Kang
- Korean J Pathol. 1999;33(8):624-626.
- 2,054 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Chronic hepatitis associated with the idiopathic hypereosinophilic syndrome has been very rarely reported worldwide. Recently, we experienced a case of chronic hepatitis with piecemeal necrosis as the clinical feature of the idiopathic hypereosinophilic syndrome. The patient was a 49-year-old woman who complained of a mild fever, nausea, vomiting, and pain in the right upper quadrant. The eosinophil count of peripheral blood increased up to 14,020/microliter (64% of WBC). Liver biopsy specimen showed severe porto-periportal inflammation with marked eosinophilic infiltration and ballooning degeneration of hepatocytes. Corticosteroid therapy significantly normalized the eosinophil count of peripheral blood.
- Pathology of Chronic Interstitial Lung Disease.
- Dong Hwan Shin
- Korean J Pathol. 1998;32(1):1-8.
- 2,904 View
- 52 Download
-
 Abstract
Abstract
 PDF
PDF - Interstitial lung disease is a generic term for a heterogeneous group of lung disease that primarily affect the interstitium although the disease is not clearly restricted to the interstitium. The majority of interstitial lung diseases represent inflammatory insults to the microscopic anatomic space bounded by the basement membrane of epithelial and endothelial cells, which may occur as slowly developing process and ultimately end up as end-stage honeycomb fibrosis. The currently prevalent classification of interstitial pneumonia with practical utility and easy reproducibility pertaining only to idopathic interstitial pneumonia encompasses several different entities some of which may represent different aspects of the same condition. Honeycomb fibrosis is usually caused by a variety of pulmonary disease including chronic interstitial lung disease. It is important to recognize that usual inter-stitial pneumonia and honeycomb fibrosis are not synonymous. In the era of chemotherapy for malignant tumor, aggressive immunosuppression for autoimmune diseases and transplant recipients and acquired immunodeficiency syndrome, lung disease in the immunocompromised host has been common. Diagnostic lung biopsy becomes increasingly needed because proper treatment of interstitial lung disease relies on correct morphologic diagnosis. This review summarizes the pathologic spectrum of idiopathic interstitial pneumonias together with other inflammatory process with known or suggestive etiologies simulating interstitial pneumonias.
- Cytomegalovirus Infection in Idiopathic Inflammatory Bowel Disease: Clinicopathologic Analysis of 6 Cases.
- Won Ae Lee, Hye Sung Hahn, Woo Ho Kim, Yong Il Kim
- Korean J Pathol. 1998;32(2):125-130.
- 2,248 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - Cytomegalovirus (CMV) infection is an uncommon association with idiopathic inflammatory bowel disease (IBD) often leading to a variety of serious complications. A total of 41 resected cases of IBD were examined to elucidate the pathologic features of intestinal CMV infection which was assessed by histologic examination and confirmed by immunohistochemistry with CMV antibody. Six cases were positve for CMV antibody; five cases in 19 ulcerative colitis (UC, 26.3%) and one case in 22 Crohn's disease (CD, 4.5%). Of 7 cases of the steroid-treated UC group, five cases were superinfected with CMV (71.4%) but none in 12 cases of the steroid-untreated UC group. All of the five CMV-positive cases in UC showed deep ulceration and transmural inflammation, while none of 10 UC cases without above features were CMV positive. Fibrinoid necrosis and thrombi were found in 83.3% of the CMV infected group, while none in the CMV-negative group of UC cases (p=0.01). We conclude that IBD, particularly UC, is susceptible to the CMV infection when steroid hormone is administered, and that deep colonic ulceration, transmural inflammation and fibrinoid necrosis of vasculature may suggest superinfection of CMV in UC patients. It seems that deep colonic ulceration may be the consequence of an ischemic change following vascular luminal occlusion or vasculitis by CMV infection.
- Clinicopathologic Analysis of Membranous Glomerulonephropathy.
- Seok Hoon Jeon, Moon Hyang Park
- Korean J Pathol. 1998;32(6):420-430.
- 2,145 View
- 10 Download
-
 Abstract
Abstract
- Membranous glomerulonephropathy (MGN) is the most common primary cause of the nephrotic syndrome in adults, accounting for about 20% of the cases in most series. MGN is idiopathic in the majority of cases, however approximately 25% of adults have identifiable causes (secondary MGN). To evaluate the clinical and pathologic characteristics of MGN, we reviewed the clinical data and renal biopsies from 141 cases of MGN. The mean age of the patients at biopsy was 43 years old, but patients of all age were seen (range from 3 to 76 years of age). There were 88 males and 53 females. There were 99 idiopathic MGN cases and 42 secondary MGN cases. The associated causes of secondary MGN included hepatitis B infection (18 cases), SLE (10 cases), drugs (4 cases), post-transplantation MGN (5 cases), diabetes mellitus (4 cases), syphilis (1 case) and hepatitis B infection associated with rheumatoid arthritis. The prevalence of histologic stages by Ehrenreich and Churg was as follows. Stage I was 24 cases, stage II was 72 cases, stage III was 35 cases, and stage IV was 9 cases. All patients had proteinuria. Nephrotic syndrome was observed in 39%, edema in 73%, microscopic hematuria in 49%, gross hematuria in 28%, hypertension in 13%, and the serum creatinine level above 1.5 mg/dl was in 13%. Cases with glomerulosclerosis was observed in 45 cases with an increased percentage of glomerulosclerosis in the higher grade. Immunofluorescence (IF) examination showed predominantly granular IgG (118 cases) and C3 (84 cases) stainings along the glomerular capillary wall. In idiopathic MGN, sparse mesangial IF staining was noted up to 10% of the cases. However, mesangial IF staining in SLE was observed in 33%, hepatitis B infection in 28% and diabetes mellitus in 50%. An electron microscopic examination revealed subepithelial electron dense deposits of immune complex in all cases. The prevalence of mesangial and subendothelial electron dense deposit in idiopathic MGN was present in 19% and 6%, respectively. In SLE cases, mesangial and subendothelial deposits were observed in 78% and 56%, respectively. In hepatitis B infection, mesangial and subendothelial deposits were observed in 54% and 69%, respectively. In conclusion, immune deposits in the mesangium are scanty in idiopathic MGN, and if pronounced this should increase suspicion of underlying systemic diseases, such as SLE or other infectious diseases.
- Clinicopathological Analysis of Eight Cases of Idiopathic Portal Hypertension.
- Kyungeun Kim, Young Suk Lim, Kyung Mo Kim, Eunsil Yu
- Korean J Pathol. 2006;40(5):348-353.
- 2,172 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Idiopathic portal hypertension (IPH) is a rare clinicopathologic entity that shows clinical evidences of portal hypertension with no pathologic features of cirrhosis.
METHODS
The clinical and pathologic features of 8 cases with IPH were analyzed via the medical records along with the biopsy or resected liver specimens.
RESULTS
Six patients were male and two were female. The chief complaints were sudden variceal bleeding in seven patients and abdominal pain in one patient. Six patients were treated with varix ligation and one was treated with splenectomy after the failure of bleeding control. One patient underwent a liver transplantation due to severe symptoms of portal hypertension. The prognosis of all the patients was excellent. Microscopically, the portal tracts were variably fibrotic, and the portal veins in them were sclerotic, obliterated or dilated in 7 cases; pathologic abnormalities were absent in 1 case. Cirrhosis was absent in all cases, while septal fibrosis was present in one resected liver.
CONCLUSIONS
IPH is a minor cause of portal hypertension. However, a liver biopsy to show the subtle portal vascular changes and fibrosis in patients who have the clinical symptoms of portal hypertension is important for making the diagnosis of IPH.

 E-submission
E-submission


 First
First Prev
Prev



