Search
- Page Path
- HOME > Search
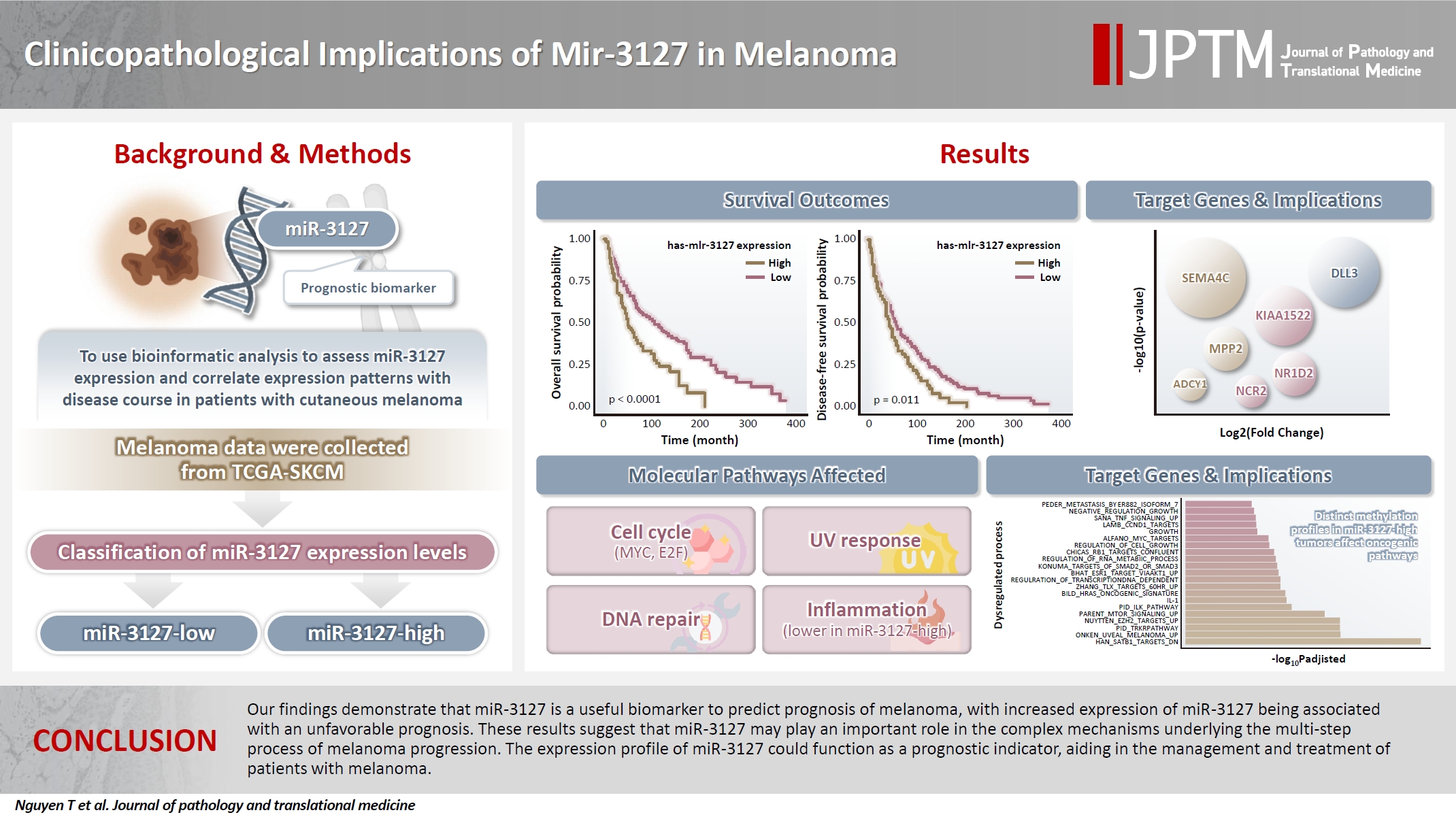
- Clinicopathological implications of miR-3127 in melanoma
- Truong Phan-Xuan Nguyen, Minh-Khang Le, Chau M. Bui, Vuong Gia Huy
- J Pathol Transl Med. 2025;59(6):371-381. Published online October 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.07.08
- 3,213 View
- 139 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Cutaneous melanoma is the most lethal of all skin cancers. Recent studies suggested that miR-3127 is dysregulated in multiple tumor types and has important roles in tumorigenesis and cancer progression, giving it potential as a prognostic biomarker. The aim of this study was to use bioinformatic analysis to assess miR-3127 expression and correlate expression patterns with disease course in patients with cutaneous melanoma. Methods: miRNA, mRNA sequencing, DNA methylation data, and clinical information of cutaneous melanoma cases were downloaded from the Human Cancer Atlas – Skin Cutaneous Melanoma (TCGA-SKCM). miR-3127 expression was classified into miR-3127–low and miR-3127–high clusters using maximally selected rank statistics. Results: Clustering analysis showed that high expression of miR-3127 (≥20.3 reads per million) was associated with worse progression-free (p < .001) and overall (p = .011) survival compared to low miR-3127 expression. More than five thousand differentially expressed genes between the two miR-3127 sample groups encoded cell differentiation markers, cytokines, growth factors, translocated cancer genes, and oncogenes. Pathway analysis revealed that miR-3127–high samples related to activity of proliferation, DNA repair, and ultraviolet response. Conclusions: The expression level of miR-3127 could act as a prognostic indicator for patients with melanoma.
- Metastatic choroidal melanoma in the breast: a case report and review of the literature
- Loay Abudalu, Vinisha Malhotra, Nabila Nasir, Sami Titi
- J Pathol Transl Med. 2023;57(4):238-241. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.07
- 5,021 View
- 128 Download
-
 Abstract
Abstract
 PDF
PDF - The breast is an unusual site for metastases, accounting for less than 2% of malignant breast lesions but include those from malignant melanomas, carcinomas, sarcomas, and lymphomas from various organs. We diagnosed a very rare case of metastatic choroidal melanoma for a 67-year-old female who presented with a right breast lump and who had been previously diagnosed with choroidal melanoma-monosomy 3 in 2017. To the best of our knowledge, only five such cases have been published so far, with one in a male patient.
- Clinicopathologic features and survival outcomes of ocular melanoma: a series of 31 cases from a tertiary university hospital
- Selin Kestel, Feriha Pınar Uyar Göçün, Betül Öğüt, Özlem Erdem
- J Pathol Transl Med. 2022;56(4):187-198. Published online May 3, 2022
- DOI: https://doi.org/10.4132/jptm.2022.03.10
- 7,846 View
- 209 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
We aimed to determine the effect of clinicopathologic features on overall survival among Caucasian ocular melanoma patients in the Central Anatolia region of Turkey.
Methods
This single-center study included conjunctival (n = 12) and uveal (n = 19) melanoma patients diagnosed between January 2008 and March 2020. Clinicopathologic features and outcomes were reviewed retrospectively. Five cases were tested for BRAF V600 mutations with real-time polymerase chain reaction, and one case was tested with nextgeneration sequencing. Survival was calculated using the Kaplan-Meier method.
Results
Thirty-one patients had a mean initial age of 58.32 years (median, 61 years; range 25 to 78 years). There were 13 male and 18 female patients. The median follow-up time was 43.5 months (range, 6 to 155 months) for conjunctival melanoma and 35 months (range, 8 to 151 months) for uveal melanoma. When this study ended, eight of the 12 conjunctival melanoma patients (66.7%) and nine of the 19 uveal melanoma patients (47.4%) had died. The presence of tumor-infiltrating lymphocytes was related to improved overall survival in conjunctival melanoma (p = .014), whereas the presence of ulceration (p = .030), lymphovascular invasion (p = .051), tumor in the left eye (p = .012), tumor thickness of > 2 mm (p = .012), and mitotic count of >1/mm² (p = .012) reduced the overall survival in conjunctival melanoma. Uveal melanoma tumors with the largest diameter of 9.1–15 mm led to the lowest overall survival among subgroups (p = .035). Involvement of the conjunctiva (p=.005) and lens (p = .003) diminished overall survival in uveal melanoma. BRAF V600 mutation was present in one case of conjunctival melanoma, GNAQ R183Q mutation was present in one case of uveal melanoma. Patients with uveal melanoma presented with an advanced pathological tumor stage compared to those with conjunctival melanoma (p = .019).
Conclusions
This study confirmed the presence of tumor-infiltrating lymphocytes as a favorable factor in conjunctival melanoma and conjunctival and lens involvement as unfavorable prognostic factors in uveal melanoma for overall survival, respectively. -
Citations
Citations to this article as recorded by- Toward Precision Medicine: Gene Therapy Applications in the Management of Uveal Melanoma
Alireza Azani, Vahid Ghassemifar, Zahra Mehrdad, Maryam Saberivand, Anahid Bagheripour, Safa Tahmasebi, Hossein Gharedaghi, Malihe Sharafi, Hassan Foroozand, Mohammad Saeed Soleimani Meigoli, Saba Pourali, Arash Salmaninejad, Faeze Ahmadi Beni, Qumars Beh
Cancer Reports.2025;[Epub] CrossRef - Uveal melanoma in the Iranian population: two decades of patient management in a tertiary eye center
Hamid Riazi-Esfahani, Abdulrahim Amini, Babak Masoomian, Mehdi Yaseri, Siamak Sabour, Ali Rashidinia, Mojtaba Arjmand, Seyed Mohsen Rafizadeh, Mohammadkarim Johari, Elias Khalili Pour, Fariba Ghassemi
International Journal of Retina and Vitreous.2024;[Epub] CrossRef - Clinical features and prognosis of patients with metastatic ocular and orbital melanoma: A bi‐institutional study
Xin Liu, Han Yue, Shiyu Jiang, Lin Kong, Yu Xu, Yong Chen, Chunmeng Wang, Yan Wang, Xiaoli Zhu, Yunyi Kong, Xiaowei Zhang, Jiang Qian, Zhiguo Luo
Cancer Medicine.2023; 12(15): 16163. CrossRef - Metastatic melanoma: clinicopathologic features and overall survival comparison
Selin Kestel, Feriha Pınar Uyar Göçün, Betül Öğüt, Özlem Erdem
Acta Dermatovenerologica Alpina Pannonica et Adriatica.2022;[Epub] CrossRef
- Toward Precision Medicine: Gene Therapy Applications in the Management of Uveal Melanoma
- Primary Malignant Melanoma of the Breast: A Report of Two Cases
- Jiwon Koh, Jihyeon Lee, So Youn Jung, Han Sung Kang, Tak Yun, Youngmee Kwon
- J Pathol Transl Med. 2019;53(2):119-124. Published online November 26, 2018
- DOI: https://doi.org/10.4132/jptm.2018.10.18
- 8,886 View
- 179 Download
- 7 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Primary malignant melanoma of the breast (PMMB) is a rare tumor with only a few case reports available in the literature. We report two cases of PMMB, one derived from the breast parenchyma and the other from the breast skin. The first case consisted of atypical epithelioid cells without overt melanocytic differentiation like melanin pigments. The tumor cells showed diffuse positivity for S100 protein, tyrosinase, and BRAF V600E. However, the tumor cells were negative for cytokeratin, epithelial membrane antigen, and HMB-45. The second case showed atypical melanocytic proliferation with heavy melanin pigmentation. The tumor cells were positive for S100 protein, HMB-45, tyrosinase, and BRAF V600E. These two cases represent two distinct presentations of PMMB in terms of skin involvement, melanin pigmentation, and HMB-45 positivity. Although PMMB is very rare, the possibility of this entity should be considered in malignant epithelioid neoplasms in the breast parenchyma.
-
Citations
Citations to this article as recorded by- First Case of Primary Breast Melanoma in Central America: Case Report and Literature Review
Ana García‐Urbina, Denis Espinoza‐Vásquez, Johanna Obregón‐Silva, Arlin Montoya Rodríguez
Clinical Case Reports.2025;[Epub] CrossRef - Primary nipple melanoma in a patient with breast cancer: A diagnosis to consider
Lucia Giudice, Sofia Vidali, Pietro Antonini, Elena Nucci, Federica Di Naro, Ludovica Anna Incardona, Vania Vezzosi, Vincenzo De Giorgi, Jacopo Nori
Radiology Case Reports.2024; 19(12): 6359. CrossRef - Is primary breast melanoma a true pathological entity? The argument against it
Alexis R. Narvaez-Rojas, Samantha Linhares, Shaina Sedighim, Kyle Daniel Klingbeil, Clara Milikowski, George Elgart, Natalia Jaimes, Lynn Feun, Jose Lutzky, Gabriel De la Cruz Ku, Eli Avisar, Mecker G. Möller
Heliyon.2024; 10(18): e37224. CrossRef - Comprehensive Literature Review on Melanoma of Unknown Primary Site Triggered by an Intriguing Case Report
Eliza-Maria Bordeanu-Diaconescu, Andrei Cretu, Andreea Grosu-Bularda, Mihaela-Cristina Andrei, Florin-Vlad Hodea, Catalina-Stefania Dumitru, Valentin Enache, Cosmin-Antoniu Creanga, Ioan Lascar, Cristian-Sorin Hariga
Diagnostics.2024; 14(19): 2210. CrossRef - Primary malignant melanoma of the breast: A case report without relapse
Alejandro Caballero, Mario Perez, Issis Rodriguez
Malignancy Spectrum.2024; 1(4): 339. CrossRef - Primary Malignant Melanoma of the Breast Presenting as a Breast Abscess: A Case Report
Hyung In Choi, You Me Kim, Junwon Min, Yong Moon Lee, Hee Jeong Kim
Journal of the Korean Society of Radiology.2023; 84(3): 763. CrossRef - Case Report: Care Report: Primary malignant melanoma of the breast
Juee Meghe, Yeshwant Lamture, Varsha Gajhbhiye, Pankaj Gharde, Akash Inamdar
F1000Research.2023; 12: 1323. CrossRef - Series of rare cases of breast tumour: 8-year review at mankweng Breast Oncology clinic, Limpopo, South Africa
Mirza M. Z. U. Bhuiyan
EUREKA: Health Sciences.2023; (4): 3. CrossRef - Primary breast parenchyma melanoma: case report
Eduardo Doria, Gion Aléssio Rocha Brunn, Diego Noya Brandão, Rafael Silva Ribeiro, Adriano Mata Pires Freire Carvalho, Miguel Ângelo Brandrão
Brazilian Journal of Oncology.2021;[Epub] CrossRef - Malignant melanoma of the breast: controversies in the diagnosis and therapeutic management of a rare nosologic entity
Aikaterini Mastoraki, Dimitrios Schizas, Ilias Giannakodimos, Athanasios Rebakos, Ioannis Margaris, Ioannis Katsaros, Ilias Vagios, Pantelis Vassiliu, Emmanouil Pikoulis
International Journal of Dermatology.2020; 59(9): 1057. CrossRef - Uncommon Subtypes of Malignant Melanomas: A Review Based on Clinical and Molecular Perspectives
Matías Chacón, Yanina Pfluger, Martín Angel, Federico Waisberg, Diego Enrico
Cancers.2020; 12(9): 2362. CrossRef - Primary Melanoma of the Breast Parenchyma: An Oncoplastic Approach
Emma Snashall, Tamara Kiernan, Aenone Harper-Machin, Rieka Taghizadeh
Plastic and Reconstructive Surgery - Global Open.2020; 8(12): e3276. CrossRef - Significance of 5-S-Cysteinyldopa as a Marker for Melanoma
Kazumasa Wakamatsu, Satoshi Fukushima, Akane Minagawa, Toshikazu Omodaka, Tokimasa Hida, Naohito Hatta, Minoru Takata, Hisashi Uhara, Ryuhei Okuyama, Hironobu Ihn
International Journal of Molecular Sciences.2020; 21(2): 432. CrossRef
- First Case of Primary Breast Melanoma in Central America: Case Report and Literature Review
- The Major Role of NF-κB in the Depth of Invasion on Acral Melanoma by Decreasing CD8+ T Cells
- Hermin Aminah Usman, Bethy S. Hernowo, Maringan Diapari Lumban Tobing, Reti Hindritiani
- J Pathol Transl Med. 2018;52(3):164-170. Published online April 20, 2018
- DOI: https://doi.org/10.4132/jptm.2018.04.04
- 7,873 View
- 115 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The tumor microenvironment including immune surveillance affects malignant melanoma (MM) behavior. Nuclear factor κB (NF-κB) stimulates the transcription of various genes in the nucleus and plays a role in the inflammatory process and in tumorigenesis. CD8+ T cells have cytotoxic properties important in the elimination of tumors. However, inhibitory receptors on the cell surface will bind to programmed death-ligand 1 (PD-L1), causing CD8+ T cells to lose their ability to initiate an immune response. This study analyzed the association of NF-κB and PD-L1 expression levels and CD8+ T-cell counts with depth of invasion of acral MM, which may be a predictor of aggressiveness related to an increased risk of metastasis.
Methods
A retrospective cross-sectional study was conducted in the Department of Anatomical Pathology, Faculty of Medicine, Universitas Padjadjaran/Hasan Sadikin Hospital using 96 cases of acral melanoma. Immunohistochemical staining was performed on paraffin blocks using anti–NF-κB, –PD-L1, and -CD8 antibodies and invasion depth was measured using dotSlide-imaging software.
Results
The study showed significant associations between the individual expression of NF-κB and PD-L1 and CD8+ T-cell number, with MM invasion depth. NF-κB was found to be a confounding variable of CD8+ T-cell number (p < .05), but not for PD-L1 expression (p = .154). Through multivariate analysis it was found that NF-κB had the greatest association with the depth of invasion (p < .001), whereas PD-L1 was unrelated to the depth of invasion because it depends on the number of CD8+ T cells (p = .870).
Conclusions
NF-κB plays a major role in acral MM invasion, by decreasing the number of CD8+ T cells in acral MM. -
Citations
Citations to this article as recorded by- The Roles of Vitamin D Receptor (VDR) and CD8+ T‐Lymphocytes in Acral and Mucosal Melanoma Invasion Depth
Hermin Aminah Usman, Fitria Sholihah, Birgitta M. Dewayani, Octavianus Giovani
Journal of Cutaneous Pathology.2025; 52(3): 227. CrossRef - Possible Mechanisms of Oxidative Stress-Induced Skin Cellular Senescence, Inflammation, and Cancer and the Therapeutic Potential of Plant Polyphenols
Hui-Min Liu, Ming-Yan Cheng, Meng-Han Xun, Zhi-Wei Zhao, Yun Zhang, Wei Tang, Jun Cheng, Jia Ni, Wei Wang
International Journal of Molecular Sciences.2023; 24(4): 3755. CrossRef - Clinical features, molecular pathology, and immune microenvironmental characteristics of acral melanoma
Jianping Gui, Zhen Guo, Di Wu
Journal of Translational Medicine.2022;[Epub] CrossRef - High Expression of COX-2 Associated with the Depth of Invasion on Acral Melanoma by Increasing TGF-β1
Nastassa Gipsyianti, Afiati Aziz, Bethy S Hernowo, Hermin A Usman
Clinical, Cosmetic and Investigational Dermatology.2021; Volume 14: 209. CrossRef - More than just acral melanoma: the controversies of defining the disease
Sara S Bernardes, Ingrid Ferreira, David E Elder, Aretha B Nobre, Héctor Martínez‐Said, David J Adams, Carla Daniela Robles‐Espinoza, Patricia A Possik
The Journal of Pathology: Clinical Research.2021; 7(6): 531. CrossRef - CD103+ T Lymphocyte Count Linked to the Thickness of Invasion on Acral Melanoma without E-Cadherin Involvement
Fauzan Ali Zainal Abidin, Hermin Aminah Usman, Sri Suryanti, Bethy S Hernowo
Clinical, Cosmetic and Investigational Dermatology.2021; Volume 14: 1783. CrossRef - Translational pathology, genomics and the development of systemic therapies for acral melanoma
Yian Ann Chen, Jamie K. Teer, Zeynep Eroglu, Jheng-Yu Wu, John M. Koomen, Florian A. Karreth, Jane L. Messina, Keiran S.M. Smalley
Seminars in Cancer Biology.2020; 61: 149. CrossRef
- The Roles of Vitamin D Receptor (VDR) and CD8+ T‐Lymphocytes in Acral and Mucosal Melanoma Invasion Depth
- Comparison of Three
BRAF Mutation Tests in Formalin-Fixed Paraffin Embedded Clinical Samples - Soomin Ahn, Jeeyun Lee, Ji-Youn Sung, So Young Kang, Sang Yun Ha, Kee-Taek Jang, Yoon-La Choi, Jung-Sun Kim, Young Lyun Oh, Kyoung-Mee Kim
- Korean J Pathol. 2013;47(4):348-354. Published online August 26, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.348
- 9,875 View
- 60 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Recently,
BRAF inhibitors showed dramatic treatment outcomes inBRAF V600 mutant melanoma. Therefore, the accuracy ofBRAF mutation test is critical.Methods BRAF mutations were tested by dual-priming oligonucleotide-polymerase chain reaction (DPO-PCR), direct sequencing and subsequently retested with a real-time PCR assay, cobas 4800 V600 mutation test. In total, 64 tumors including 34 malignant melanomas and 16 papillary thyroid carcinomas were analyzed. DNA was extracted from formalin-fixed paraffin embedded tissue samples and the results of cobas test were directly compared with those of DPO-PCR and direct sequencing.Results BRAF mutations were found in 23 of 64 (35.9%) tumors. There was 9.4% discordance among 3 methods. Out of 6 discordant cases, 4 cases were melanomas; 3 cases wereBRAF V600E detected only by cobas test, but were not detected by DPO-PCR and direct sequencing. One melanoma patient withBRAF mutation detected only by cobas test has been on vemurafenib treatment for 6 months and showed a dramatic response to vemurafenib. DPO-PCR failed to detect V600K mutation in one case identified by both direct sequencing and cobas test.Conclusions In direct comparison of the currently available DPO-PCR, direct sequencing and real-time cobas test for
BRAF mutation, real-time PCR assay is the most sensitive method.-
Citations
Citations to this article as recorded by- Preoperative BRAFV600E mutation detection in thyroid carcinoma by immunocytochemistry
Kristine Zøylner Swan, Stine Horskær Madsen, Steen Joop Bonnema, Viveque Egsgaard Nielsen, Marie Louise Jespersen
APMIS.2022; 130(11): 627. CrossRef - Strategy to reduce unnecessary surgeries in thyroid nodules with cytology of Bethesda category III (AUS/FLUS): a retrospective analysis of 667 patients diagnosed by surgery
Yong Joon Suh, Yeon Ju Choi
Endocrine.2020; 69(3): 578. CrossRef - A new primer construction technique that effectively increases amplification of rare mutant templates in samples
Jr-Kai Huang, Ling Fan, Tao-Yeuan Wang, Pao-Shu Wu
BMC Biotechnology.2019;[Epub] CrossRef - BRAF and NRAS mutations and antitumor immunity in Korean malignant melanomas and their prognostic relevance: Gene set enrichment analysis and CIBERSORT analysis
Kyueng-Whan Min, Ji-Young Choe, Mi Jung Kwon, Hye Kyung Lee, Ho Suk Kang, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Yun Joong Kim, Nan Young Kim, Ho Young Kim
Pathology - Research and Practice.2019; 215(12): 152671. CrossRef - The association between dermoscopic features and BRAF mutational status in cutaneous melanoma: Significance of the blue-white veil
Miquel Armengot-Carbó, Eduardo Nagore, Zaida García-Casado, Rafael Botella-Estrada
Journal of the American Academy of Dermatology.2018; 78(5): 920. CrossRef - Comparison of Five Different Assays for the Detection of BRAF Mutations in Formalin-Fixed Paraffin Embedded Tissues of Patients with Metastatic Melanoma
Claire Franczak, Julia Salleron, Cindy Dubois, Pierre Filhine-Trésarrieu, Agnès Leroux, Jean-Louis Merlin, Alexandre Harlé
Molecular Diagnosis & Therapy.2017; 21(2): 209. CrossRef - Validation of an NGS mutation detection panel for melanoma
Anne Reiman, Hugh Kikuchi, Daniela Scocchia, Peter Smith, Yee Wah Tsang, David Snead, Ian A Cree
BMC Cancer.2017;[Epub] CrossRef - Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
Journal of Pathology and Translational Medicine.2016; 50(4): 258. CrossRef - Immunohistochemistry with the anti-BRAF V600E (VE1) antibody: impact of pre-analytical conditions and concordance with DNA sequencing in colorectal and papillary thyroid carcinoma
Katerina Dvorak, Birte Aggeler, John Palting, Penny McKelvie, Andrew Ruszkiewicz, Paul Waring
Pathology.2014; 46(6): 509. CrossRef
- Preoperative BRAFV600E mutation detection in thyroid carcinoma by immunocytochemistry
- Frequency of
BRAF Mutation and Clinical Relevance for Primary Melanomas - Hyoun Wook Lee, Ki Hoon Song, Jin Woo Hong, Su Young Jeon, Dong Yeob Ko, Ki Ho Kim, Hyuk Chan Kwon, Suee Lee, Sung Hyun Kim, Dae Cheol Kim
- Korean J Pathol. 2012;46(3):246-252. Published online June 22, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.3.246
- 10,144 View
- 59 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Background This study was conducted to clarify the frequency of the
BRAF mutation in primary melanomas and its correlation with clinicopathologic parameters.Methods We analyzed the frequency of
BRAF mutation in patients with primary cutaneous melanoma (n=58) or non-cutaneous one (n=27) by performing dual priming oligonucleotide-based multiplex real-time polymerase chain reaction to isolate and to purify the DNA from the formalin-fixed and paraffin-embedded tumors.Results The
BRAF mutation was found in 17.2% (10/58) of patients with primary cutaneous melanoma and 11.1% (3/27) of those with non-cutaneous melanoma. The frequency ofBRAF mutation was not correlated with any clinicopathologic parameters with the exception of the patient age. The frequency of theBRAF mutation was significantly higher in patients younger than 60 years as compared with those older than 60 years (p=0.005).Conclusions Compared with previous reports, our results showed that the frequency of the
BRAF mutation was relatively lower in patients with primary cutaneous melanoma. Besides, our results also showed that the frequency of theBRAF mutation had an inverse correlation with the age. Further studies are warranted to exclude methodological bias, to elucidate the difference in the frequency of theBRAF mutation from the previous reports from a Caucasian population and to provide an improved understanding of the molecular pathogenesis of malignant melanoma.-
Citations
Citations to this article as recorded by- Prevalence and clinicopathological correlation of BRAF V600E mutations in ameloblastoma: A PCR study from a tertiary centre in South India
Logeswari Jayamani, Kavitha Bottu, Leena Dennis Joseph, Ganthimathy Sekhar
Journal of Stomatology Oral and Maxillofacial Surgery.2026; 127(1): 102575. CrossRef - . Prevalence and prognostic mutation V600E in the BRAF gene in stage I cutaneous melanoma
K. S. Titov, M. V. Sorokina, D. N. Grekov, S. S. Lebedev
Bone and soft tissue sarcomas, tumors of the skin.2024; 16(3): 61. CrossRef - Clinicopathological Features of Patients with Malignant Melanoma Diagnosis and Prognostic and Predictive Importance of Neuthrophil-Lymphocyte Ratio
Yasemin SAĞDIÇ KARATEKE, Lütfiye DEMİR, Murat DİNÇER, Bülent YILDIZ
OSMANGAZİ JOURNAL OF MEDICINE.2023;[Epub] CrossRef - Genetic characteristics and response to systemic therapies of acral lentiginous melanoma at a tertiary care center—a retrospective review
Taylor Jamerson, Vito W. Rebecca, Crystal Aguh
Journal of the National Medical Association.2022; 114(1): 7. CrossRef - Comparative study of cutaneous melanoma and its associated issues between people of African decent and Caucasians
Ehiaghe L. Anaba
Dermatologic Therapy.2021;[Epub] CrossRef -
BRAF, KIT, and NRAS Mutations of Acral Melanoma in White Patients
Emi Dika, Giulia Veronesi, Annalisa Altimari, Mattia Riefolo, Giulia Maria Ravaioli, Bianca Maria Piraccini, Martina Lambertini, Elena Campione, Elisa Gruppioni, Michelangelo Fiorentino, Barbara Melotti, Manuela Ferracin, Annalisa Patrizi
American Journal of Clinical Pathology.2020; 153(5): 664. CrossRef - Clinical Application of Next-Generation Sequencing–Based Panel toBRAFWild-Type Advanced Melanoma Identifies Key Oncogenic Alterations and Therapeutic Strategies
Changhee Park, Miso Kim, Min Jung Kim, Hyeongmin Kim, Chan-Young Ock, Bhumsuk Keam, Tae Min Kim, Dong-Wan Kim, Jong-Il Kim, Dae Seog Heo
Molecular Cancer Therapeutics.2020; 19(3): 937. CrossRef - BRAF and NRAS mutations and antitumor immunity in Korean malignant melanomas and their prognostic relevance: Gene set enrichment analysis and CIBERSORT analysis
Kyueng-Whan Min, Ji-Young Choe, Mi Jung Kwon, Hye Kyung Lee, Ho Suk Kang, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Yun Joong Kim, Nan Young Kim, Ho Young Kim
Pathology - Research and Practice.2019; 215(12): 152671. CrossRef - Acral melanoma: correlating the clinical presentation to the mutational status
Giulia M. Ravaioli, Emi Dika, Martina Lambertini, Marco A. Chessa, Pier Alessandro Fanti, Annalisa Patrizi
Giornale Italiano di Dermatologia e Venereologia.2019;[Epub] CrossRef - Sunrise in melanoma management: Time to focus on melanoma burden in Asia
John Wen‐Cheng Chang, Jun Guo, Chia‐Yen Hung, Si Lu, Sang Joon Shin, Richard Quek, Anthony Ying, Gwo Fuang Ho, Huu Sau Nguyen, Boman Dhabhar, Virote Sriuranpong, Maria Luisa Tiambeng, Nugroho Prayogo, Naoya Yamazaki
Asia-Pacific Journal of Clinical Oncology.2017; 13(6): 423. CrossRef - Detection ofBRAF,NRAS,KIT,GNAQ,GNA11andMAP2K1/2mutations in Russian melanoma patients using LNA PCR clamp and biochip analysis
Marina Emelyanova, Lilit Ghukasyan, Ivan Abramov, Oxana Ryabaya, Evgenia Stepanova, Anna Kudryavtseva, Asiya Sadritdinova, Cholpon Dzhumakova, Tatiana Belysheva, Sergey Surzhikov, Lyudmila Lyubchenko, Alexander Zasedatelev, Tatiana Nasedkina
Oncotarget.2017; 8(32): 52304. CrossRef - Metaanalysis of BRAF mutations and clinicopathologic characteristics in primary melanoma
Soo Young Kim, Soo Nyung Kim, Hyung Jin Hahn, Yang Won Lee, Yong Beom Choe, Kyu Joong Ahn
Journal of the American Academy of Dermatology.2015; 72(6): 1036. CrossRef - Diagnostic Effectiveness of PCR-based Tests DetectingBRAFMutation for Treating Malignant Melanoma: A Systematic Review
Hae-Won Shin, Ryeo-Jin Ko, Min Lee, Hee-Young Bang, Kye-Chul Kwon, Jong-Woo Park, Sun-Hoe Koo
Laboratory Medicine Online.2014; 4(4): 203. CrossRef - KIT, NRAS, BRAF and PTEN mutations in a sample of Swedish patients with acral lentiginous melanoma
Abdlsattar Zebary, Katarina Omholt, Ismini Vassilaki, Veronica Höiom, Diana Lindén, Lisa Viberg, Lena Kanter-Lewensohn, Carolina Hertzman Johansson, Johan Hansson
Journal of Dermatological Science.2013; 72(3): 284. CrossRef
- Prevalence and clinicopathological correlation of BRAF V600E mutations in ameloblastoma: A PCR study from a tertiary centre in South India
- Primary Malignant Melanoma Arising in an Ovarian Mature Cystic Teratoma: A Case Report and Literature Review.
- Sangho Lee, Ji Hoon Kim, Gyu Rak Chon, Aeree Kim, Baek Hui Kim
- Korean J Pathol. 2011;45(6):659-664.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.659
- 4,848 View
- 30 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Ovarian primary malignant melanoma is very uncommon with only 44 reported cases in the literature. A 71-year-old woman with an ovarian mass and multiple nodules in the liver presented to our hospital. She was treated with bilateral salpingo-oophorectomy, and malignant melanoma was found in the mature cystic teratoma of the ovary. Malignant melanoma cells were also found in the ascitic fluid. She died 5 months later. Here we report a very uncommon case of malignant melanoma arising in an ovarian mature cystic teratoma with a review of the literature.
-
Citations
Citations to this article as recorded by- Malignant Transformation of an Ovarian Mature Cystic Teratoma to a Malignant Melanoma
Rita Rathore, Sana Ahuja, Nuneno Nakhro, Pallavi Punhani, Sufian Zaheer
Indian Journal of Surgical Oncology.2024; 15(2): 380. CrossRef - Malignant melanoma arising in mature teratoma with pugnacious spread: A case report
Sumedha Gupta, Shalu Solanki, Saritha Shamsunder, Sana Ahuja, Vinayak Varma
Indian Journal of Obstetrics and Gynecology Research.2024; 11(1): 119. CrossRef - Therapeutic Management of Rare Primary Ovarian Neoplasms: Carcinosarcoma, Leiomyosarcoma, Melanoma and Carcinoid
Mateusz Kozłowski, Katarzyna Nowak, Agnieszka Kordek, Aneta Cymbaluk-Płoska
International Journal of Environmental Research and Public Health.2021; 18(15): 7819. CrossRef - Primary form of malignant melanoma in an ovarian mature cystic teratoma: case report and literature review
Fatemeh Samiee-rad, Amir Abdollah Zangivand, Kamran Soleimanitadi
Comparative Clinical Pathology.2017; 26(4): 989. CrossRef - Malignant melanoma arising in a mature teratoma: A case report with review of the recent literature
Lorna A. Brudie, Faizan Khan, Michael J. Radi, Melissa M. Yates, Sarfraz Ahmad
Gynecologic Oncology Reports.2016; 16: 47. CrossRef - Metastasizing Primary Malignant Melanoma of the Ovary: A Diagnostic Enigma
Narendra Hulikal, Manilal Banoth, Revanth Gangasani, Praveen C. Suresh, Radhika Kottu, Asha Thota
Journal of Gynecologic Surgery.2015; 31(3): 166. CrossRef
- Malignant Transformation of an Ovarian Mature Cystic Teratoma to a Malignant Melanoma
- Alteration of Apoptosis-Related Proteins (Apaf-1, Caspase-9, Bcl-2, p53, and Survivin) According to Malignant Progression in Cutaneous Melanocytic Lesions.
- Yeo Ju Kang, Ji Han Jung, Kwnag Il Yim, Kyo Young Lee, Youn Soo Lee, Seok Jin Kang, Chang Suk Kang, Si Yong Kim
- Korean J Pathol. 2011;45(3):247-253.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.247
- 3,980 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Apoptosis protease activating factor-1 (Apaf-1), caspase-9, Bcl-2, p53, and survivin are important factors in the pathway of apoptosis, but their clinicopathologic significance remains unclear in human cutaneous melanoma. We investigated the expression of these proteins and their clinical value in human cutaneous melanocytic lesions.
METHODS
We performed an immunohistochemical analysis to examine the expression and distribution of Apaf-1, caspase-9, Bcl-2, p53, and survivin in 36 cases of malignant melanoma (22 cases of primary melanoma and 14 cases of metastatic melanoma) and 41 cases of melanocytic nevus.
RESULTS
The expression of p53 was significantly higher in malignant melanoma than in melanocytic nevus (p<0.01), however the expressions of Apaf-1 and caspase-9 were significantly lower in malignant melanoma compared with melanocytic nevus (p<0.01 and p=0.027, respectively). Also, there was a significant difference for Bcl-2 staining between primary melanomas and metastatic lesions (p=0.004). Nuclear staining for survivin were absent in nevus, but were positive in 14 of 36 melanomas (p<0.01).
CONCLUSIONS
The altered expression of Apaf-1, caspase-9, p53, and survivin are considered to be related to malignant progression in human cutaneous melanocytic lesions. Loss of Bcl-2 can be considered as a prognostic marker of malignant melanomas.
- Primary Malignant Melanoma of the Male Urethra.
- Seung Wook Lee, Eun Kyung Kim, Won Mi Lee, Jung Man Jo, Tag Keun Yoo, Jeong Yoon Kang
- Korean J Pathol. 2010;44(6):662-665.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.6.662
- 3,662 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - Primary malignant melanoma occurring within the male urethra is very rare. Here we report a case of malignant melanoma of the urethra in a 74-year-old man. He presented with asymptomatic gross hematuria for 5 months. His glans penis and adjacent penile skin had become discolored black 10 years ago. Cystourethroscopy showed a smooth oval-shaped elevated mass in the fossa navicularis. There were no abnormal findings in the proximal urethra and urinary bladder. Computed tomography did not detect any inguinal lymph node enlargement or distant metastases. The patient underwent partial penectomy and ilioinguinal lymph node dissection. Grossly, the distal urethra revealed an ovoid pigmented nodule, that measured 1 x 0.5 cm. Microscopic findings showed a nodular malignant melanoma arising in the urethral mucosa with pagetoid spread to the epidermis of the glans penis. There were no recurrences over a period of 12 months after surgery without chemotherapy. This is the second case of a primary malignant melanoma of the male urethra in Korea.
- Primary Malignant Melanoma of the Urinary Bladder: A Case Report.
- Sung Hak Lee, Eun Deok Chang, Eun Jung Lee, Chang Suk Kang
- Korean J Pathol. 2010;44(2):216-219.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.216
- 4,261 View
- 44 Download
-
 Abstract
Abstract
 PDF
PDF - Primary malignant melanoma in the bladder is very rare, with only 18 cases having been currently reported. A 65-year-old male patient presented with a 5-month history of gross hematuria. On ultrasonography, an 8.1 x 6.1 cm mass was revealed on the bladder wall. A partial cystectomy was performed. Microscopically, the tumor was composed of atypical, pigmented melanocytes that were positive for S-100 protein and they were negative for human melanoma black-45. Although he underwent supportive therapy, an 8.7 x 5.9 cm mass occupying the prevesical space was noted on a follow-up computed tomography scan 4 months later. Two nodules of the left lower lung and multiple enlarged lymph nodes in the left external iliac chain were also revealed. The patient declined any further treatment. The histogenesis of primary bladder melanoma is uncertain, but an origin from neural crest cells has been proposed. The prognosis for patients with this tumor is still poor despite the availability of several therapeutic options.
- Ethnic Differences of the p53 Genetic Alteration in Cutaneous Malignant Melanoma.
- Won Sang Park, Eun Young Na, Sang Kyu Lee, Sug Hyung Lee, Su Young Kim, Seok Jin Kang, Kye Yong Song, Suk Woo Nam, Nam Jin Yoo, Jung Young Lee
- Korean J Pathol. 2001;35(2):158-164.
- 1,960 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
There are significant differences in the clincopathologic pattern including the incidence, favor site, and histopathologic type between cutaneous malignant melanomas arising from whites, asians and blacks. These differences might suggest that there is a racial difference in the molecular tumorigenesis mechanism of malignant melanoma.
METHODS
To determine the ethnic differences in tumorigenesis of malignant melanoma, we performed loss of heterozygosity (LOH) and sequencing analyses of the p53 gene in cutaneous malignant melanomas arising from 22 white American, 30 Korean and 15 black African patients.
RESULTS
The frequency of LOH of the p53 gene is only 12.5% in white American patients, but the frequency is significantly higher in Korean (42.1%) and black African (61.5%) patients. We also detected 17 mutations (nonsense: 1, missense: 16) of the p53 gene in the cutaneous malignant melanomas of Koreans and black Africans, but none in those of white Americans: among the 16 missense mutations, 10 mutations were C:G to T:A transitional mutations. Of these, we also detected one GG (CC) to AA (TT) tandem mutation at the pyrimidine sequence.
CONCLUSION
These results strongly suggest that there might be a racial difference in molecular carcinogenesis mechanisms among the cutaneous malignant melanomas occurring in white American, Korean and black African patients. But the role of the p53 genetic alteration in the genesis of melanomas in Korean and black African patients is subject to further evaluation.
- Clinicopathological Analysis on the 104 Cases of Malignant Melanoma.
- Kye Yong Song, Kyeong Cheon Jung, Kwang Hyun Cho, Je Geun Chi, Eui Geun Ham
- Korean J Pathol. 1997;31(6):566-573.
- 2,296 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - The cliniopathological analysis was done on the 104 cases of malignant melanoma diagnosed at the Seoul National University Hospital (SNUH) from 1984 to 1993. The basic clinical data and the pathological items were based on the New Mexico Melanoma Registry Worksheet. The results were as follows. The male to female ratio was 1 : 0.79. Primary cutaneous melanoma was more common in the male (M : F=1 : 0.56) but primary extracutaneous melanoma with slight female dominancy (M : F=1 : 1.25). The peak age was the 6th decade in both cutaneous and extracutaneous malignant melanoma. In 66% (35 cases) of primary cutaneous malignant melanoma, the primary site was located in the acral area (including cases of acral lentiginous and nodular type), of which 63% (41% of total cutaneous melanoma) was acral lentiginous type. Major components of tumor cells were epithelioid. Clark's level of tumor was III or more at the time of the first visit in the majority of the cases (85%). The incidence rate of extracutaneous melanoma was 34.6% (36 cases) among the primary melanoma, and the eyeball (17.3%) was the most prevalent organ. All these features suggest that the racial difference between the Korean and the Caucasian is evident and also that etiologic role of sun damage is not quite marked in the Korean. We also suggest that an early detection program is very important to cure this malignant tumor.
- Balloon Cell Malignant Melanoma: A case report.
- Ji Young Seo, Soon Young Kim, Jeong Hee Kang, Young Ok Kim, Bang Hur
- Korean J Pathol. 1999;33(7):537-539.
- 2,490 View
- 44 Download
-
 Abstract
Abstract
 PDF
PDF - Balloon cell malignant melanoma (BCMM) is a rare histologic variant of malignant melanoma, which is composed either predominantly or entirely of large clear or foamy cells. The incidence of balloon cell malignant melanoma is about 0.15% of all cutaneous malignant melanomas. Recently, we experienced a case of cutaneous balloon cell malignant melanoma in the right lower abdomen with right inguinal and both axillary lymph node metastasis in a 56-year-old man. The cutaneous lesion was 4.5 3.5 cm in size, a well-demarcated black nodular mass, involving abdominal skin and subcutaneous tissue. The tumor was histologically composed of two types of tumor cells: predominant clear cell and focal, pigmented spindle cell. The nodal lesion was composed entirely of clear cells. Both clear and spindle cells showed positive reaction for S-100 protein and HMB-45 on immunohistochemistry.
- Primary Malignant Melanoma arising in Mucosa of the Palatine Tonsil: A case report.
- Ki Jung Yun, Hyang Jeong Jo, Hyung Bae Moon, Sang Won Yoon
- Korean J Pathol. 1996;30(1):65-67.
- 2,508 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - Maligant melanomas of the oral or nasal cavity, and the vulvovaginal area are relatively common among the melanomas of non-ocular mucosa. But, primary malignant melanoma arising in the mucosa of the palatine tonsil is rare. We present a case of primary malignant melanoma arising in the mucosa of the palatine tonsil. A 36-year-old male was admitted for evaluation of a recurrent sore throat. Tonsillectomy was performed on the basis of clinical suspicion of chronic tonsillitis. Grossly, the left tonsil was focally dark. Microscopically, the tonsillar mucosa was diffusely infiltrated with tumor cells. Tumor cells revealed numerous melanin pigments. Intraepithelial nests of tumor cells were noted, but pagetoid spread of tumor cells was not found. Tumor cells were positive for S-100 protein and HMB45 stain. There was no evidence of melanoma in the skin or eye.
- Malignant Melanoma Arising in Giant Congenital Melanocytic Nevus: A case report.
- Jung Sun Kim, Sang Yong Song, Kye Yong Song, Je G Chi
- Korean J Pathol. 1993;27(6):650-655.
- 2,216 View
- 39 Download
-
 Abstract
Abstract
 PDF
PDF - Giant congenital melanocytic nevus is found in 0.1% of live born infants. If present, this lesion has a 6.3% chance to develop malignant melanoma. We report such a case in a 22-year-old woman who had multiple pigmented skin lesions since birth. Rapidly growing masses were recently detected in the 19 cm-sized occipital pigmented lesion. Removed scalp lesion revealed yellowish white lobulated soft nodules in the background of pigmented nevus. Microscopically, the nodules consisted of epithelioid cells with prominent nucleoli, and pleomorphic cells including signetring cells. These cells seldom contained melanin pigment. There were metastatic aggregates of tumor cells in the cervical lymph node, which were reminiscent of germinal centers of lymph nodes. S-100 protein immunostaining was helpful to distinguish them. Incidentally, focally scattered pigmented spindle cells were seen in the capsule of a lymph node
- Malignant Melanoma of the Anus: Report of a case.
- Eun Sun Jung, Byung Kee Kim, Sun Moo Kim, Sang In Shim
- Korean J Pathol. 1996;30(3):276-278.
- 1,885 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - This report describes a primary malignant melanoma which developed in the anus, as documented by light microscopy and immunohistochemistry. A 53-year-old woman had a 4 month history of a protruding mass in the anal canal. The mass was located in the squamo-columnar junction of the anal canal, measuring 5.0x4.5 cm. Its cut surface was dark brown and poorly circumscribed. The histologic appearance was characterized by epithelioid or spindle cells with prominant nucleoli and frequent atypical mitosis. Melanin pigments were strongly seen in Fontana-Masson stain. Immunoreactivity revealed that the cytoplasm of tumor cells was strongly positive with antibody directed against S-100 protein, vimentin and it was focally positive with neuron specific enolase.
- Cytopathologic Observation of Primary Malignant Melanoma of the Lung: A case report.
- Yun Mee Kim, Jong Hee Nam, Min Cheol Lee, Joo Yong Yoo, Kyu Hyuk Cho
- Korean J Pathol. 1991;25(4):367-375.
- 2,017 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - The pulmonary cytology has reached a high level of accuracy. By the examination of the sputum and/or bronchial brushings, it is now possible to make a diagnosis in 70% to 90% of patients with cancer. Primary melanoma of the lung is very rare and there have been reported about 20 cases in the world literature. We present a case of primary malignant melanoma of the lung in a 61-year-old male diagnosed by cytologic examination of sputum, bronchial brushing and aspirated pleural fluid. Histologic examination of bronchoscopic biopsy and examination of the skin and other primary sites confirmed the diagnosis.
- Cytologic Features of Papnicolaou Smears of Malignant Melanoma Arising in Vagina: A Cese Report.
- Myung Suk Kang, Bohng Hee Kim, Jae Hoon Park, Youn Wha Kim, Yong Koo Park, Ju Hie Lee, Moon Ho Yang
- J Pathol Transl Med. 1995;6(2):209-214.
- 1,846 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Primary malignant melanoma of vagina is a rare tumor which is easily misinterpretated in routine cytologic examination. We lately experienced a case of primary malignant melanoma of the vagina with direct cervical extension diagnosed by Pap smear. The cervicovaginal smear showed variable sized clusters of epithelial cells or singly scattered abnormal epithelial cells. Most of the tumor cells had round hyperchromatic nuclei with prominent nucleoli and brownish pigments in cytoplasm. The cytologic findings are compared with histologic features of resected specimen.
- Expression of bcl-2 and c-myc Proteins in Epidermal and Melanocytic Tumors.
- Young Ha Oh, Chan Kum Park, Jung Dal Lee
- Korean J Pathol. 1996;30(9):810-818.
- 2,128 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - bcl-2 and c-myc protein expression were studied in 44 epidermal (8 seborrheic keratoses, 21 squamous cell carcinomas, and 15 basal cell carcinomas), and 26 melanocytic tumors(8 nevi, and malignant melanomas) by immunohistochemistry using the specific anti-bcl-2 and anti-c-myc monoclonal antibodies. 14 out of 15 basal cell carcinomas(BCC) (93.3%) showed expression of bcl-2 protein, 12 of which (85.7%) showed coexpression of c-myc protein. In the melanocytic tumors, 7 out of 8 nevi showed bcl-2 expression (87.5%). Five of these 7 cases (62.5%) also showed c-myc protein expression. Eight of 18 malignant melanomas(MM) (44.4%) showed expression of bcl-2 protein and 7 of these 8 cases (38.9%) also showed c-myc protein expression. All seborrheic keratoses and squamous cell carcinoma(SCC) were negative for bcl-2 proteins. 12 of 15 SCCs(80%) were positive for c-myc protein. In conclusion, bcl-2 and c-myc proteins were coexpressed in BCCs, nevi, and MMs. Coexpression of bcl-2 and c-myc proteins in these tumors was statistically significant(p<0.01), while no considerable differences of bcl-2 and c-myc expression were found between nevi and MMs. These results suggests that bcl-2 may cooperate with c-myc to promote tumorigenesis of BCCs, nevi, and MMs(p<0.01).
- Cytologic Features of Metastatic Melanoma.
- Jae Hee Suh, Joo Ryung Huh, Gyung Yub Gong
- J Pathol Transl Med. 1996;7(2):185-191.
- 3,842 View
- 155 Download
-
 Abstract
Abstract
 PDF
PDF - Metastatic melanoma is often difficult to diagnose morphologically. However, the prognostic and therapeutic decision in cases of metastatic melanoma depends upon the morphologic documentation of the metastatic disease, which may rapidly and accurately be done by cytologic methods such as aspiration cytology of clinically suspicious lesion. Cytological features of 12 metastatic melanoma are described. Evaluation for melanin pigment, background composition, cytoplasmic vacuoles, intranuclear inclusions, bi or multinucleated cells, eccentric nuclei, nucleoli, and degree of cellular cohesion were made. the presence of melanin pigment, prominent nucleoli, intranuclear cytoplasmic inclusions, lack of cell cohesion, and eccentric nuclei are the important and useful cytologic features in the diagnosis of metastatic melanoma. Bior multinucleated cells, cytoplasmic vacuoles, and bloody background are also frequently found in smears from metastatic melanoma.
- Metastatic Melanoma Mimicking a Papillary Carcinoma of the Thyroid in Fine Needle Aspiration Cytology: A Case Report.
- Young Ok Hong, Jae Hee Suh, Hee Jeong Cha, Hye Jeong Choi, Young Min Kim
- J Pathol Transl Med. 2007;18(2):161-164.
- 2,562 View
- 42 Download
-
 Abstract
Abstract
 PDF
PDF - Metastasis to the thyroid gland is very rare in clinical practice. We recently encountered a 65-year-old woman who presented with a large thyroid nodule that mimicked the cytologic features of a papillary thyroid carcinoma on fine needle aspiration biopsy (FNAB). Although initially diagnosed as a papillary thyroid carcinoma, a thorough clinical work-up revealed multiple lesions in the bones, liver, and nasal cavity, which were confirmed as metastases of a malignant melanoma. Despite a thorough physical examination, however, the primary skin lesion could not be identified. Although FNAB shows a high degree of accuracy in diagnosing primary thyroid tumors, it is less accurate in diagnosing metastases to the thyroid gland. A thorough clinical history with appropriate immunohistochemical staining assays is necessary for the accurate diagnosis of metastatic malignant melanoma.
- Primary Malignant Melanoma of the Esophagus: A case report.
- Lee So Maeng, Kyoung Mee Kim, Eun Jung Lee, Anhi Lee, Sang In Shim
- Korean J Pathol. 1998;32(9):694-696.
- 1,974 View
- 10 Download
-
 Abstract
Abstract
- This report presents an unusual case of primary malignant melanoma in the midesophagus. The patient was a 36-year-old woman presenting with dysphagia and odynophagia. The resected esophagus and proximal stomach showed a dark purple large polypoid mass, measuring 6.0 3.3 2.0 cm, with a diffuse tan pigmentation of surrounding mucosa in the mid-esophagus and two small daughter nodules, up to 1.2 0.3 cm, in the lower esophagus near the gastro-esophageal junction. A microscopic examination revealed a malignant melanoma of epithelioid cell type confined to mucosa and submucosa with a diffuse melanosis. Cytoplasmic immunoreactivity for HMB 45 and S-100 protein were noted. An electron microscopic examination revealed large, loosely cohesive variable shaped cells with a few cytoplasmic premelanosomes.
- Primary Mucosal Desmoplastic Melanoma of Gingiva: A Case Report.
- Gawon Choi, Jeong Won Kim, Soon Yuhl Nam, Kyung Ja Cho
- Korean J Pathol. 2006;40(6):456-460.
- 2,014 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Desmoplastic melanoma (DM) is a rare malignant melanoma variant. Although DM mainly affects the skin chronically exposed to the sun, a small number of mucosal DM have been reported. Primary mucosal DM is difficult to diagnose because of its rarity and atypical histopathologic features. Here, we report a case of DM in a 52 year-old female who presented with a right cervical mass and upper gingival pigmentation. A CT scan revealed an ill-defined infiltrative mass 2 cm in size under the pigmented mucosa. She subsequently underwent a partial maxillectomy with neck dissection. Gross examination revealed that the mass exhibited a grayish white fibrotic cut surface and that the maxillary bone had been destroyed. Microscopically, the main mass was composed of cigar-shaped or wavy spindle cells with desmoplastic stroma under the melanoma in situ. The diagnosis of DM was confirmed immunohistochemically with S100 protein positivity and HMB45 negativity. The patient has survived for 29 months after the operation with a presumed metastatic focus.
- Immunohistochemical Evaluation of HMB-45 and S-100 Protein in Melanocytic Tumors.
- Chang Soo Park, Hwan Kim, Hyang Mi Ko, Kyung Soo Kim, Ji Shin Lee
- Korean J Pathol. 1995;29(2):189-196.
- 3,804 View
- 63 Download
-
 Abstract
Abstract
 PDF
PDF - Immunohistochemical staining on paraffin sections for S-100 protein improved diagnostic accuracy for melanocytic tumor. But specificity of S-100 protein in the diagnosis of melanocytic tumor is very low, because S-100 protein was also expressed in neurogenic tumor and salivary gland tumor. To investigate a specific tumor marker for the malignant melanoma, immunohistochemical staining for HMB-45 and S-100 protein was performed on the paraffin sections of 25 cases of malignant melanoma and 46 cases of nevi. Positive reaction for HMB-45 and S-100 protein was diffusely identified in the cytoplasm of tumor cells. Positive ratio for HMB-45 was 100% in malignant melanoma, 92% in junctional component of compound nevus and 0% in intradermal nevus. Positive ratio for S-100 protein was 92% in malignant melanoma, 100% in compound nevus and 100% in intradermal nevus. The sensitivity and specificity for HMB-45 in malignant melanoma were 100%, but those for S-100 protein were 92% in sensitivity and 86.7% in specificity. These results indicate that HMB-45 has a high sensitivity and specificity for malignant melanoma cells and it can be quite useful for the histopathological diagnosis of malignant melanoma.
- Fine Needle Aspiration Cytology of Metastatic Melanoma in the Breast: A Case Report.
- Young Lyun Oh, Young Hyeh Ko
- J Pathol Transl Med. 1998;9(1):111-116.
- 2,215 View
- 30 Download
-
 Abstract
Abstract
 PDF
PDF - Although the characteristic cytologic features of melanoma have been well described, the diagnosis of metastatic melanoma by fine needle aspiration cytology (FNAC) may be difficult in the case of amelanotic melanoma and in the absence of awareness of clinical history. Furthermore, when the breast is the site of initial presentation, it could simulate a primary breast carcinoma leading to misdiagnosis. The recognition of metastatic malignant melanoma in FNAC material is essential to avoid an unnecessary mastectomy and to ensure appropriate chemotherapy. We experienced a case of metastatic melanoma of breast which presented as solitary breast mass in a 56-year-old woman. She had a history of surgical excision of right foot for melanoma one year ago. The cytologic smears were composed of noncohesive epithelioid cells with round or eccentric nuclei, bi-or multi-nucleation, prominent nucleoli, fine chromatin, and intranuclear inclusions. The cytoplasm of tumor cells had scanty melanin pigment but were diffusely positive for S-100 protein.
- Immunohistochemical Study on the Expression of Mutated p53 Protein and Bcl-2 Protein in Melanocytic Lesions of Skin.
- Wha Jin Lee, Joon Hyuk Choi, Won Hee Choi
- Korean J Pathol. 1997;31(2):112-120.
- 2,022 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - To investigate the immunohistochemical expression of mutated p53 protein and bcl-2 protein in the cutaneous melanocytic lesion, 15 cases of compound nevus, 10 cases of congenital melanocytic nevus, 15 cases of primary malignant melanoma(4 cases less than 1.5 mm thick and 11 cases more than 1.5 mm thick), and 10 cases of metastatic malignant melanoma(7 cases in lymph node and 3 cases in soft tissue) were examined. All cases of compound nevi and of congenital melanocytic nevi showed no immunoreactivity for p53 protein. p53 protein overexpression was observed in 75%(3/4) wth primary malignant melanoma less than 1.5 mm thick, 81%(9/11) with primary malignant melanoma more than 1.5 mm thick, and 100%(10/10) with metastatic malignant melanoma. The difference in p53 protein overexpression was statistically significant between benign nevi and malignant melanoma(p<0.01). Bcl-2 protein expression was observed in 73%(11/15) with compound nevus, 70%(7/10) with congenital melanocytic nevus, 75% (3/4) in primary malignant melanoma less than 1.5 mm thick, 54%(6/11) with primary malignant melanoma more than 1.5 mm thick, and 40%(4/10) with metastatic malignant melanoma. These findings suggested that mutation of p53 gene may be an important mechanism in the development of malignant melanoma. Although bcl-2 protein was expressed in cutaneous melanocytic lesion, no correlation was found between p53 protein and bcl-2 protein expression in malignant melanoma.

 E-submission
E-submission



 First
First Prev
Prev



