Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 52(3); 2018 > Article
-
Original Article
Cytologic Diagnosis of Noninvasive Follicular Thyroid Neoplasm with Papillary-like Nuclear Features and Its Impact on the Risk of Malignancy in the Bethesda System for Reporting Thyroid Cytopathology: An Institutional Experience - Milim Kim1,2,*, Joung Eun Kim3,*, Hyun Jeong Kim1, Yul Ri Chung1,2, Yoonjin Kwak2, So Yeon Park1,2
-
Journal of Pathology and Translational Medicine 2018;52(3):171-178.
DOI: https://doi.org/10.4132/jptm.2018.04.03
Published online: April 3, 2018
1Department of Pathology, Seoul National University Bundang Hospital, Seongnam, Korea
2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea
3Seoul National University College of Medicine, Seoul, Korea
- Corresponding Author So Yeon Park, MD, PhD Department of Pathology, Seoul National University Bundang Hospital, 82 Gumi-ro 173beon-gil, Bundang-gu, Seongnam 13620, Korea Tel: +82-31-787-7712 Fax: +82-31-787-4012 E-mail: sypmd@snu.ac.kr
- *Milim Kim and Joung Eun Kim contributed equally to this work.
© 2018 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- This study was performed to analyze cytologic diagnosis of noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) and its impact on the risk of malignancy (ROM) in the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC).
-
Methods
- Five thousand five hundred and forty-nine cases of thyroid fine-needle aspiration cytology (FNAC) diagnosed between 2012 and 2014 were included in this study. Diagnostic categories based on TBSRTC were compared with final surgical diagnoses, and the ROM in each category was calculated both when NIFTP was included in malignant lesions and when excluded from malignant lesions.
-
Results
- Of the 5,549 thyroid FNAC cases, 1,891 cases underwent surgical resection. In final diagnosis, 1,700 cases were revealed as papillary thyroid carcinoma (PTC), and 25 cases were reclassified as NIFTP. The cytologic diagnoses of NIFTP were non-diagnostic in one, benign in five, atypia of undetermined significance (AUS) in 14, follicular neoplasm in two, and suspicious for malignancy in three cases. Collectively, NIFTP/encapsulated follicular variant of PTC (EFVPTC) were more frequently classified as benign, AUS, or follicular neoplasm and less frequently categorized as malignant compared to conventional PTCs. Exclusion of NIFTP from malignant diagnoses resulted in a slight decrease in malignancy rates in non-diagnostic, benign, AUS, follicular neoplasm, and suspicious for malignancy categories without any statistical significance.
-
Conclusions
- The decrease in the ROM was not significant when NIFTP was excluded from malignant lesions. In thyroid FNACs, NIFTP/EFVPTCs were mostly classified into indeterminate categories. Therefore, it might be feasible to separate NIFTP/EFVPTC from conventional PTC on FNAC to guide clinicians to conservative management for patients with NIFTP/EFVPTC.
- Case selection
- We retrospectively reviewed a total of 5,624 thyroid FNAC specimens from 5,127 patients, diagnosed at Seoul National University Bundang Hospital from January 2012 to December 2014. Of the 5,624 FNACs, 1,784 (31.7%) were consult cases from outside hospitals. Of the 5,127 patients, 174 patients had multiple thyroid nodules for which FNAC was performed separately and each counted as an individual case in this study. In the 71 patients who had repeated FNACs for the same nodule, the diagnostic category with the highest ROM was selected. Finally, 5,549 thyroid FNACs were included in this study. All thyroid FNAC slides were prepared with conventional smear with Papanicolaou staining and were diagnosed according to the diagnostic categories of TBSRTC [2]. In our institution, category III (AUS) is subcategorized into four subgroups: (1) AUS-NA, AUS having focal nuclear atypia (NA) suggestive of papillary carcinoma, but not diagnostic for category V (suspicious for malignancy); (2) AUS-MF, AUS showing a predominant population of microfollicles (MFs), but not sufficient for diagnosis of category IV (follicular neoplasm); (3) AUS-HC, AUS showing predominance of Hurthle cells (HC); and (4) AUS-others, AUS not otherwise specified. This study was approved by the Institutional Review Board (IRB) of Seoul National University Bundang Hospital (IRB No. B-1803-456-102), and the requirement for informed consent was waived.
- Pathologic review of surgical resection specimens
- Of the 5,549 thyroid FNACs, cases with subsequent surgical resection were extracted from the electronic medical records. Histologic diagnoses for surgical resection specimens were reviewed and matched with the results of FNACs for the corresponding nodules. For PTC, we re-evaluated histologic variants such as conventional type, encapsulated follicular variant, infiltrative follicular variant, tall cell variant and etc. We carefully reviewed all the slides of EFVPTC and identified NIFTP according to the recently proposed diagnostic criteria [4]. For a histological diagnosis of NIFTP, a thyroid tumor had to fulfill the following criteria: (1) encapsulation or clear demarcation, (2) follicular growth pattern, (3) nuclear features of PTC (nuclear score 2–3), (4) no capsular or vascular invasion, and (5) no aggressive histology (no tumor necrosis, no high mitotic activity). Regarding the follicular growth pattern, specific conditions were set as follows: (1) < 1% papillae, (2) no psammoma bodies, and (3) < 30% solid/trabecular/insular pattern. The ROM in each category of TBSRTC was calculated using cases with subsequent surgical resection or all FNAC cases.
- Statistical analyses
- Statistical analyses were performed using SPSS statistics ver. 22.0 (IBM Corp., Armonk, NY, USA). The Pearson chi-square test or Fisher exact test was used to compare the frequencies of categorical variables between two groups. A p-value of less than .05 was considered statistically significant. All p-values reported were two-sided.
MATERIALS AND METHODS
- Diagnostic categories of TBSRTC
- Diagnostic categories of the 5,549 thyroid FNACs and their frequencies are as follows (Table 1): 727 cases (13.1%) of category I (non-diagnostic), 2,125 cases (38.3%) of category II (benign), 882 cases (15.9%) of category III (AUS), 44 cases (0.8%) of category IV (follicular neoplasm), 499 cases (9.0%) of category V (suspicious for malignancy), and 1,272 cases (22.9) of category VI (malignant). The 882 cases of AUS were composed of 542 AUS-NA (61.4%), 132 AUS-MF (15.0%), 73 AUS-HC (8.3%), and 135 AUS-others (15.3%).
- Comparison of diagnostic categories of TBSRTC with final surgical diagnoses
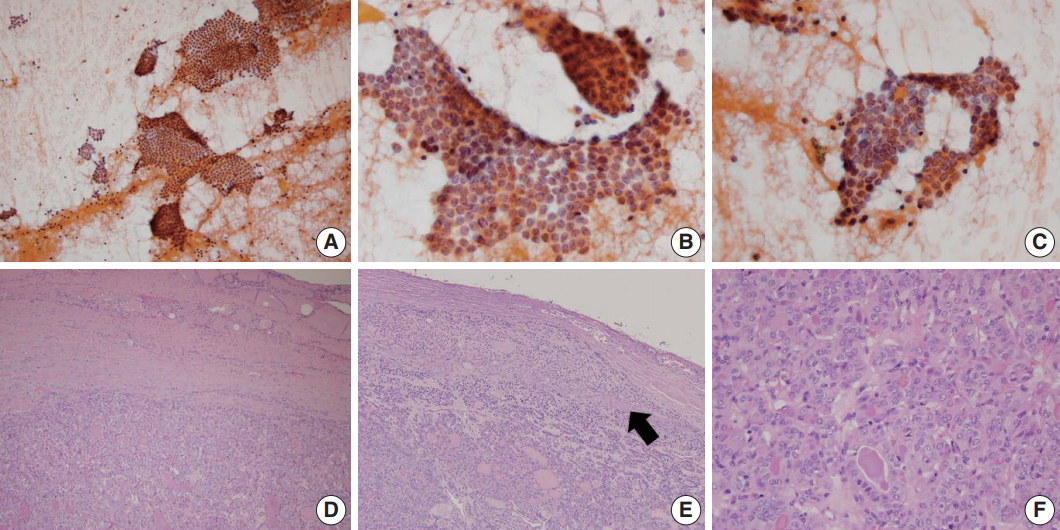
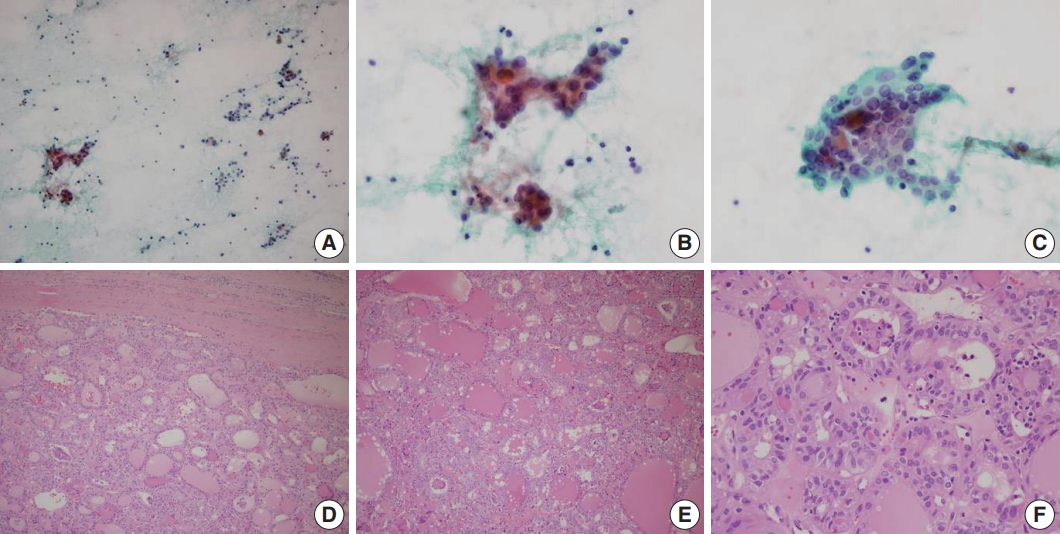
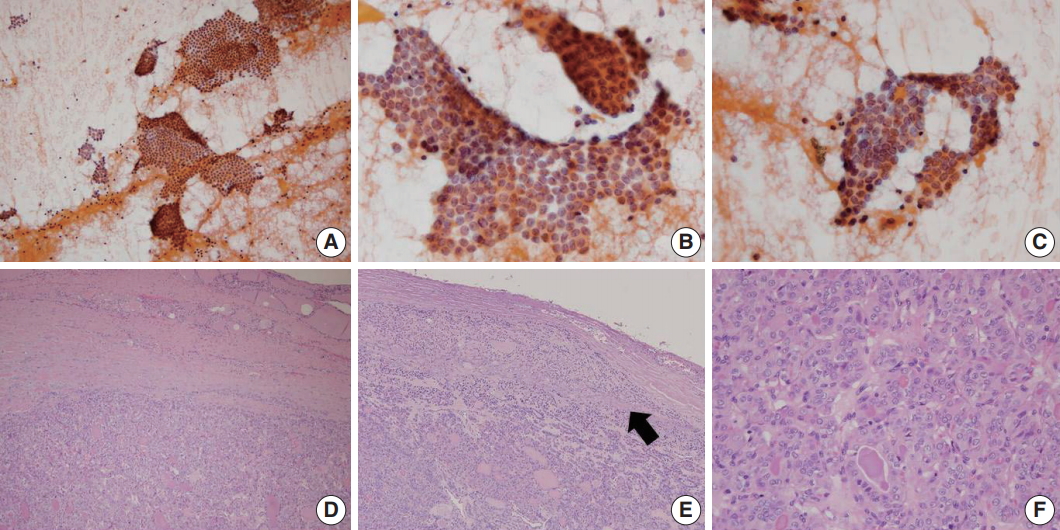
- Of the 5,549 thyroid FNAC cases, 1,891 cases underwent surgical resection. Final surgical diagnoses are presented in Table 2. In surgical resection specimens, 1,700 cases were revealed as PTC including 1,445 conventional PTCs, 70 EFVTPTCs, 62 infiltrative follicular variant of PTC (infiltrative FVPTCs), 106 tall cell variants, and 17 other rare variants (Table 3). Of the 70 EFVPTCs in surgical resection specimens, 25 cases were finally reclassified as NIFTP after reviewing of the slides. The cytologic diagnoses of NIFTP were non-diagnostic in one (4.0%), benign in five (20.0%), AUS in 14 (56.0%) (Fig. 1), follicular neoplasm in two (8.0%), and suspicious for malignancy in three (12.0%). Of the 14 cases with AUS diagnoses, nine showed NA and five revealed MF pattern. The non-diagnostic case was diagnosed as follicular neoplasm in a repeated core needle biopsy. Diagnostic categories of FNAC for invasive EFVPTC were as follows: non-diagnostic in four (8.8%), benign in four (8.8%), AUS in 17 (37.8%), follicular neoplasm in two (8.3%), suspicious for malignancy in 10 (8.3%), and malignant in eight (17.8%) (Fig. 2). When comparing the cytologic diagnoses of NIFTP and EFVPTC with capsular or vascular invasion, malignant cytologic diagnoses were found in invasive EFVPTC only with a statistical difference (p = .044). However, there were no statistically significant differences in the frequencies of other diagnostic categories.
- Comparison of diagnostic categories of TBSRTC between conventional PTC, NIFTP/EFVPTC, and infiltrative FVPTC
- When comparing diagnostic categories between conventional PTC and NIFTP/EFVPTCs (Table 4), 924 of 1,445 conventional PTCs (63.9%) were diagnosed as category VI, whereas eight of the 70 NIFTP/EFVPTCs (11.4%) were diagnosed as malignancy (p < .001). Four NIFTP/EFVPTCs (5.7%) and none of the conventional PTCs were categorized as follicular neoplasm on FNAC (p < .001). While 144 conventional PTCs (10.0%) were classified as AUS, 31 NIFTP/EFVPTCs (44.3%) were classified as AUS (p<.001). In particular, only three of 1,445 conventional PTCs (0.2%) were classified as AUS-MF, whereas 10 of 70 NIFTP/EFVPTCs (14.3%) revealed AUS-MF pattern (p < .001). Six conventional PTCs (0.4%) and nine NIFTP/EFVPTCs (12.9%) were classified as benign on FNAC (p < .001). Collectively, NIFTP/EFVPTCs were more frequently classified as benign, AUS, or follicular neoplasm diagnostic categories and less frequently diagnosed as malignant compared with conventional PTCs. Similarly, infiltrative FVPTC was more frequently diagnosed as AUS (p < .001) and follicular neoplasm (p = .041) and less frequently diagnosed as malignant (p < .001), compared with conventional PTCs (Table 4). When comparing cytologic diagnoses between infiltrative FVPTCs and NIFTP/EFVPTCs (Table 4), infiltrative FVPTCs were less frequently classified as benign and more frequently diagnosed as malignant, compared with NIFTP/EFVPTCs (p = .019 and p = .033, respectively).
- Impact of NIFTP on ROM in each diagnostic category of TBSRTC
- When NIFTPs were regarded as malignant tumors, the ROM in each diagnostic category of FNAC was as follows in histology-proven cases: non-diagnostic, 65.8%; benign, 33.3%; AUS, 75.8%; follicular neoplasm, 37.0%; suspicious for malignancy, 99.2%; malignant, 100% (Table 5). Next, we assessed the impact of NIFTP on the ROM in each diagnostic category. When excluding NIFTP from malignant diagnoses, an absolute decrease ranged from 0% to 9.2% and a relative decrease ranged from 0% to 27.6%. The ROM seemed to change largely in benign (33.3% to 24.1%) and AUS-MF categories (52.8% to 43.3%), but there were no statistical differences in ROMs in all diagnostic categories whether NIFTP was included in malignancy diagnoses or not.
- When the ROMs were calculated in total FNAC cases, the ROM including NIFTP in each diagnostic category was as follows: non-diagnostic, 6.6%; benign, 0.8%; AUS, 26.3%; follicular neoplasm, 22.7%; suspicious for malignancy, 78.2%; malignant, 81.6% (Table 6). Exclusion of NIFTP from malignant diagnoses resulted in an absolute decrease of 0% to 4.5% and a relative decrease of 0% to 25.0% without any statistical difference.
RESULTS
- Introduction of NIFTP has created some challenges for thyroid FNAC: among them, its impact on the ROM in the diagnostic categories of TBSRTC and the resulting need for modification of clinical management guidelines may be critical. Previous studies from Western countries have revealed decreases in the ROM across all TBSRTC categories, and significant reductions in the ROM were detected in the three indeterminate TBSRTC categories upon reclassification of noninvasive EFVPTC as NIFTP [8,9,11]. However, in this study, introduction of the term NIFTP resulted in an insignificant decrease in the ROM in the diagnostic categories of non-diagnostic, benign, AUS, follicular neoplasm, and suspicious for malignancy.
- The decrease in the risk of malignancies in each diagnostic category after the introduction of NIFTP will vary according to the institutional frequency and preceding FNAC diagnoses of NIFTP [9,17]. While NIFTP comprises 7%–28% of PTCs in previous studies from Western countries [8,11-14], its proportion is quite low in Asian countries, ranging from 0% to 4.7% of PTCs [15,16]. In this study, NIFTP represented 1.5% of all PTCs. Thus, exclusion of NIFTP from malignant diagnoses and the resultant decrease in the ROM in diagnostic categories of TBSRTC was not significant. The incidence of NIFTP may be directly linked to the incidence of EFVPTC. In this study, EFVPTC comprised 4.1% of all PTCs and it was reported to account for 0.7% to 5.5% of PTCs in Asian counties [15,16]. However, EFVPTC represented about 24% of all PTC cases in Western countries with its incidence increasing [4,18].
- Previous studies have shown that NIFTP is usually diagnosed into indeterminate categories, that is, AUS/FLUS, follicular neoplasm/suspicious for a follicular neoplasm, and suspicious for malignancy. Comparative studies on cytomorphologic features of NIFTP and conventional PTC revealed that cytologic features of PTC such as nuclear pseudoinclusions, crowding, irregularities, and clearing are less frequent in NIFTP compared to conventional PTC [19,20]. Especially, among the various nuclear features of PTC, nuclear pseudoinclusions are known to be almost absent in NIFTP [20,21]. Moreover, by definition, NIFTP should not have papillae and psammomatous calcification which can be found in cytologic smear of conventional PTC. Thus, the borderline nuclear features, lack of papillae and predominance of MFs in NIFTP lead to cytologic diagnoses of indeterminate categories, and rarely to malignant category. Accordingly, it is reasonable that changes in ROM are significant in indeterminate categories but insignificant in malignant category after the introduction of NIFTP. Similar to the previous studies [11,13,19], our study showed that NIFTP was most frequently diagnosed as AUS. Five cases were even diagnosed as benign: however, this can be explained by the frequent focal PTC-like nuclear changes in NIFTP.
- In this study, FNAC diagnoses of NIFTP and EFVPTC with invasion did not show a significant difference in other diagnostic categories except for malignant category. As the distinction between invasive EFVPTC and NIFTP is basically based on the demonstration of capsular and/or vascular invasion, their cytologic features can be overlapping. However, 17.8% of invasive EFVPTC but none of the NIFTC was categorized as malignant in FNAC. It is thought that NIFTP progresses to invasive EFVPTC and thus, invasive EFVPTC may show more typical nuclear features of PTC compared to NIFTP. Recently, Chandler et al. [21] reported that predominantly MF pattern, absence of pseudoinclusions, and less frequent nuclear elongation and grooves are more likely to be associated with NIFTP in comparison with invasive EFVPTC. However, other previous studies did not demonstrate differences in FNAC diagnostic categories between them [15,22]. Maletta et al. [22] reported that EFVPTC with invasion were typically diagnosed as follicular neoplasm or suspicious for malignancy and nuclear features including size, contour irregularities, and chromatin clearing did not differ between NIFTP and invasive EFVPTC.
- There are a few limitations in this study. As a tertiary medical center, malignant cytologic diagnoses comprised as much as 22.9% of all FNAC diagnoses in our institution. That is, our study population had selection bias, and thus, the incidence of NIFTP in this study may not reflect its normal distribution. Moreover, we reviewed only EFVPTC cases to find NIFTP. Some cases which were previously diagnosed as follicular adenoma or even nodular hyperplasia may have incomplete PTC-like nuclei and may have been missed. For these reasons, there is a possibility that NIFTP was underestimated in this study.
- To conclude, in this study, the decrease in the ROM was not significant when NIFTP was excluded from malignant lesions due to the low frequency of NIFTP. NIFTP/EFVPTCs were more frequently classified as benign, AUS, or follicular neoplasm categories and less frequently diagnosed as malignant, when compared with conventional PTCs. Though there are no drastic changes in the 2017 revision of TBSRTC, it emphasizes that malignant diagnoses should be limited to cases with classic features of PTC including true papillae, psammoma bodies, and nuclear pseudoinclusions to avoid false-positives due to NIFTP [3]. It appears that in thyroid FNACs, NIFTP/EFVPTCs are mostly classified into indeterminate diagnostic categories. Therefore, it might be feasible to separate NIFTP/EFVPTC from conventional PTC on FNAC to guide clinicians to conservative management for patients with NIFTP/EFVPTC.
DISCUSSION
| FNAC diagnostic category | No. of surgical specimens |
Final diagnosis |
Othera | |||
|---|---|---|---|---|---|---|
| Nodular hyperplasia | Follicular adenoma | Follicular carcinoma | Papillary carcinoma | |||
| Non-diagnostic | 73 | 14 (19.2) | 11 (15.1) | 1 (1.4) | 47 (64.4) | 0 |
| Benign | 54 | 28 (51.9) | 6 (11.1) | 2 (3.7) | 16 (29.6) | 2 (3.7) |
| AUS | 306 | 34 (11.1) | 40 (13.1) | 15 (4.9) | 211 (68.9) | 6 (2.0) |
| AUS-NA | 215 | 12 (5.6) | 12 (5.6) | 4 (1.9) | 185 (86.0) | 2 (0.9) |
| AUS-MF | 53 | 8 (15.1) | 17 (32.1) | 11 (20.7) | 17 (32.1) | 0 |
| AUS-HC | 17 | 7 (41.2) | 9 (52.9) | 0 | 0 | 1 (5.9) |
| AUS-others | 21 | 7 (33.3) | 2 (9.5) | 0 | 9 (42.9) | 3 (14.3) |
| Follicular neoplasm | 27 | 7 (25.9) | 10 (37.0) | 5 (18.5) | 5 (18.5) | 0 |
| Suspicious for malignancy | 393 | 2 (0.5) | 1 (0.3) | 2 (0.5) | 387 (98.5) | 1 (0.3) |
| Malignant | 1,038 | 0 | 0 | 1 (0.1) | 1,034 (99.6) | 3 (0.3) |
| Total | 1,891 | 85 (4.5) | 68 (3.6) | 26 (1.4) | 1,700 (89.9) | 12 (0.6) |
Values are presented as number (%).
FNAC, fine needle aspiration cytology; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.
aOther includes two cases of parathyroid adenoma in benign; two medullary carcinomas, one poorly differentiated carcinoma, two anaplastic carcinomas, and one lymphoma in AUS; one medullary carcinoma in suspicious for malignancy; one medullary carcinoma, one anaplastic carcinoma, and one thymic carcinoma in malignant category.
| FNAC diagnostic category |
Variants of PTC in final diagnosis |
|||||
|---|---|---|---|---|---|---|
| Conventional | NIFTP | Invasive encapsulated follicular variant | Infiltrative follicular variant | Tall cell variant | Other rare variants | |
| Non-diagnostic | 32 (2.2) | 1 (4.0) | 4 (8.8) | 5 (7.7) | 3 (2.8) | 2 (11.8) |
| Benign | 6 (0.4) | 5 (20.0) | 4 (8.8) | 1 (1.6) | 0 | 0 |
| AUS | 144 (10.0) | 14 (56.0) | 17 (37.8) | 25 (40.3) | 8 (7.5) | 3 (17.6) |
| AUS-NA | 135 (9.3) | 9 (36.0) | 11 (24.4) | 21 (33.9) | 7 (6.6) | 2 (11.8) |
| AUS-MF | 3 (0.2) | 5 (20.0) | 5 (11.1) | 4 (6.4) | 0 | 0 |
| AUS-HC | 0 | 0 | 0 | 0 | 0 | 0 |
| AUS-others | 6 (0.4) | 0 | 1 (2.2) | 0 | 1 (0.9) | 1 (5.9) |
| Follicular neoplasm | 0 | 2 (8.0) | 2 (8.3) | 1 (1.6) | 0 | 0 |
| Suspicious for malignancy | 339 (23.5) | 3 (12.0) | 10 (4.4) | 14 (22.6) | 20 (18.9) | 1 (5.9) |
| Malignant | 924 (63.9) | 0a | 8 (17.8)a | 16 (25.8) | 75 (70.8) | 11 (64.7) |
| Total No. | 1,445 | 25 | 45 | 62 | 106 | 17 |
Values are presented as number (%).
FNAC, fine needle aspiration cytology; PTC, papillary thyroid carcinoma; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.
ap = .044, Fisher exact test.
| FNAC diagnostic category | Conventional PTC | NIFTP/EFVPTC | Infiltrative FVPTC | p-valuea | p-valueb | p-valuec |
|---|---|---|---|---|---|---|
| Non-diagnostic | 32 (2.2) | 5 (7.1) | 5 (7.7) | .025 | 1.000 | .016 |
| Benign | 6 (0.4) | 9 (12.9) | 1 (1.6) | < .001 | .019 | .259 |
| AUS | 144 (10.0) | 31 (44.3) | 25 (40.3) | < .001 | .646 | < .001 |
| AUS-NA | 135 (9.3) | 20 (28.6) | 21(33.9) | < .001 | .511 | < .001 |
| AUS-MF | 3 (0.2) | 10 (14.3) | 4 (6.4) | < .001 | .167 | < .001 |
| AUS-HC | 0 (0) | 0 (0) | 0 (0) | 1.000 | 1.000 | 1.000 |
| AUS-others | 6 (0.4) | 1 (1.4) | 0 (0) | .282 | 1.000 | 1.000 |
| Follicular neoplasm | 0 (0) | 4 (5.7) | 1 (1.6) | < .001 | .370 | .041 |
| Suspicious for malignancy | 339 (23.5) | 13 (18.6) | 14 (22.6) | .344 | .569 | .873 |
| Malignant | 924 (63.9) | 8 (11.4) | 16 (25.8) | < .001 | .033 | < .001 |
Values are presented as number (%).
PTC, papillary thyroid carcinoma; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; EFVPTC, encapsulated follicular variant of papillary thyroid carcinoma; FVPTC, follicular variant of papillary thyroid carcinoma; FNAC, fine-needle aspiration cytology; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.
aConventional PTC vs. NIFTP/EFVPTC;
bNIFTP/EFVPTC vs. infiltrative FVPTC;
cConventional PTC vs. infiltrative FVPTC.
- 1. Baloch ZW, Seethala RR, Faquin WC, et al. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP): a changing paradigm in thyroid surgical pathology and implications for thyroid cytopathology. Cancer Cytopathol 2016; 124: 616-20. ArticlePubMed
- 2. Cibas ES, Ali SZ. The Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2009; 19: 1159-65. ArticlePubMed
- 3. Cibas ES, Ali SZ. The 2017 Bethesda System for Reporting Thyroid Cytopathology. Thyroid 2017; 27: 1341-6. ArticlePubMed
- 4. Nikiforov YE, Seethala RR, Tallini G, et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol 2016; 2: 1023-9. ArticlePubMedPMC
- 5. Hauch A, Al-Qurayshi Z, Randolph G, Kandil E. Total thyroidectomy is associated with increased risk of complications for low- and high-volume surgeons. Ann Surg Oncol 2014; 21: 3844-52. ArticlePubMedPDF
- 6. Iyer NG, Morris LG, Tuttle RM, Shaha AR, Ganly I. Rising incidence of second cancers in patients with low-risk (T1N0) thyroid cancer who receive radioactive iodine therapy. Cancer 2011; 117: 4439-46. ArticlePubMedPMC
- 7. Ohori NP, Wolfe J, Carty SE, et al. The influence of the noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) resection diagnosis on the false-positive thyroid cytology rate relates to quality assurance thresholds and the application of NIFTP criteria. Cancer Cytopathol 2017; 125: 692-700. ArticlePubMedPDF
- 8. Strickland KC, Howitt BE, Marqusee E, et al. The impact of noninvasive follicular variant of papillary thyroid carcinoma on rates of malignancy for fine-needle aspiration diagnostic categories. Thyroid 2015; 25: 987-92. ArticlePubMed
- 9. Zhou H, Baloch ZW, Nayar R, et al. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP): Implications for the risk of malignancy (ROM) in the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC). Cancer Cytopathol 2018; 126: 20-6. PubMed
- 10. Kiernan CM, Weiss VL, Mehrad M, Ely K, Baregamian N, Solórzano CC. New terminology-noninvasive follicular neoplasm with papillary-like nuclear features (NIFTP) and its effect on the rate of malignancy at a single institution. Surgery 2018; 163: 55-9. ArticlePubMed
- 11. Faquin WC, Wong LQ, Afrogheh AH, et al. Impact of reclassifying noninvasive follicular variant of papillary thyroid carcinoma on the risk of malignancy in The Bethesda System for Reporting Thyroid Cytopathology. Cancer Cytopathol 2016; 124: 181-7. ArticlePubMed
- 12. Li W, Sciallis A, Lew M, Pang J, Jing X. Implementing noninvasive follicular thyroid neoplasm with papillary-like nuclear features may potentially impact the risk of malignancy for thyroid nodules categorized as AUS/FLUS and FN/SFN. Diagn Cytopathol 2018; 46: 148-53. ArticlePubMedPDF
- 13. Mainthia R, Wachtel H, Chen Y, et al. Evaluating the projected surgical impact of reclassifying noninvasive encapsulated follicular variant of papillary thyroid cancer as noninvasive follicular thyroid neoplasm with papillary-like nuclear features. Surgery 2018; 163: 60-5. ArticlePubMed
- 14. Singh R, Avila J, Jo K, et al. Patients with non-invasive follicular thyroid neoplasm with papillary-like nuclear features are unlikely to have malignant preoperative cytology. Ann Surg Oncol 2017; 24: 3300-5. ArticlePubMedPDF
- 15. Hirokawa M, Higuchi M, Suzuki A, Hayashi T, Kuma S, Miyauchi A. Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: a single-institutional experience in Japan. Endocr J 2017; 64: 1149-55. ArticlePubMed
- 16. Bychkov A, Hirokawa M, Jung CK, et al. Low rate of noninvasive follicular thyroid neoplasm with papillary-like nuclear features in Asian practice. Thyroid 2017; 27: 983-4. ArticlePubMed
- 17. Hung YP, Barletta JA. A user's guide to non-invasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP). Histopathology 2018; 72: 53-69. ArticlePubMedPDF
- 18. Jung CK, Little MP, Lubin JH, et al. The increase in thyroid cancer incidence during the last four decades is accompanied by a high frequency of BRAF mutations and a sharp increase in RAS mutations. J Clin Endocrinol Metab 2014; 99: E276-85. ArticlePubMedPDF
- 19. Brandler TC, Zhou F, Liu CZ, et al. Can noninvasive follicular thyroid neoplasm with papillary-like nuclear features be distinguished from classic papillary thyroid carcinoma and follicular adenomas by fine-needle aspiration? Cancer Cytopathol 2017; 125: 378-88. ArticlePubMedPDF
- 20. Strickland KC, Vivero M, Jo VY, et al. Preoperative cytologic diagnosis of noninvasive follicular thyroid neoplasm with papillary-like nuclear features: a prospective analysis. Thyroid 2016; 26: 1466-71. ArticlePubMed
- 21. Chandler JB, Colunga M, Prasad ML, et al. Identification of distinct cytomorphologic features in the diagnosis of NIFTP at the time of preoperative FNA: implications for patient management. Cancer Cytopathol 2017; 125: 865-75. PubMed
- 22. Maletta F, Massa F, Torregrossa L, et al. Cytological features of “noninvasive follicular thyroid neoplasm with papillary-like nuclear features” and their correlation with tumor histology. Hum Pathol 2016; 54: 134-42. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- High Rates of Unnecessary Surgery for Indeterminate Thyroid Nodules in the Absence of Molecular Test and the Cost-Effectiveness of Utilizing Molecular Test in an Asian Population: A Decision Analysis
Man Him Matrix Fung, Ching Tang, Gin Wai Kwok, Tin Ho Chan, Yan Luk, David Tak Wai Lui, Carlos King Ho Wong, Brian Hung Hin Lang
Thyroid®.2025; 35(2): 166. CrossRef - Spatial transcriptomics reveals prognosis‐associated cellular heterogeneity in the papillary thyroid carcinoma microenvironment
Kai Yan, Qing‐Zhi Liu, Rong‐Rong Huang, Yi‐Hua Jiang, Zhen‐Hua Bian, Si‐Jin Li, Liang Li, Fei Shen, Koichi Tsuneyama, Qing‐Ling Zhang, Zhe‐Xiong Lian, Haixia Guan, Bo Xu
Clinical and Translational Medicine.2024;[Epub] CrossRef - Cytological Features of “Non-invasive Follicular Tumour with Papillary Like Nuclear Features” – A Single Institutional Experience in India
K Amita, HB Rakshitha, M Sanjay, Prashantha Kalappa
Journal of Cytology.2023; 40(1): 28. CrossRef - Detailed fine needle aspiration cytopathology findings of noninvasive follicular thyroid neoplasm with papillary‐like nuclear features with nuclear grading correlated to that of biopsy and Bethesda category and systematic review
Sevgiye Kaçar Özkara, Gupse Turan
Diagnostic Cytopathology.2023; 51(12): 758. CrossRef - Non-Invasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features Is Not a Cytological Diagnosis, but It Influences Cytological Diagnosis Outcomes: A Systematic Review and Meta-Analysis
Elina Haaga, David Kalfert, Marie Ludvíková, Ivana Kholová
Acta Cytologica.2022; 66(2): 85. CrossRef - Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: its updated diagnostic criteria, preoperative cytologic diagnoses and impact on the risk of malignancy
Hee Young Na, So Yeon Park
Journal of Pathology and Translational Medicine.2022; 56(6): 319. CrossRef - Usage and Diagnostic Yield of Fine-Needle Aspiration Cytology and Core Needle Biopsy in Thyroid Nodules: A Systematic Review and Meta-Analysis of Literature Published by Korean Authors
Soon-Hyun Ahn
Clinical and Experimental Otorhinolaryngology.2021; 14(1): 116. CrossRef - Comprehensive DNA Methylation Profiling Identifies Novel Diagnostic Biomarkers for Thyroid Cancer
Jong-Lyul Park, Sora Jeon, Eun-Hye Seo, Dong Hyuck Bae, Young Mun Jeong, Yourha Kim, Ja Seong Bae, Seon-Kyu Kim, Chan Kwon Jung, Yong Sung Kim
Thyroid.2020; 30(2): 192. CrossRef - Differences in surgical resection rate and risk of malignancy in thyroid cytopathology practice between Western and Asian countries: A systematic review and meta‐analysis
Huy Gia Vuong, Hanh Thi Tuyet Ngo, Andrey Bychkov, Chan Kwon Jung, Trang Huyen Vu, Kim Bach Lu, Kennichi Kakudo, Tetsuo Kondo
Cancer Cytopathology.2020; 128(4): 238. CrossRef - Noninvasive follicular neoplasm with papillary like nuclear features: A comprehensive analysis with a diagnostic algorithm
Chanchal Rana, Shreyamsa Manjunath, Pooja Ramakant, Kulranjan Singh, Suresh Babu, Anand Mishra
Diagnostic Cytopathology.2020; 48(4): 330. CrossRef - Noninvasive follicular thyroid neoplasm with papillary‐like nuclear features and the risk of malignancy in The Bethesda System for the Reporting of Thyroid Cytopathology
Danielle Elliott Range, Xiaoyin “Sara” Jiang
Diagnostic Cytopathology.2020; 48(6): 531. CrossRef - Did Introducing a New Category of Thyroid Tumors (Non-invasive Follicular Thyroid Neoplasm with Papillary-like Nuclear Features) Decrease the Risk of Malignancy for the Diagnostic Categories in the Bethesda System for Reporting Thyroid Cytopathology?
Janusz Kopczyński, Agnieszka Suligowska, Kornelia Niemyska, Iwona Pałyga, Agnieszka Walczyk, Danuta Gąsior-Perczak, Artur Kowalik, Kinga Hińcza, Ryszard Mężyk, Stanisław Góźdź, Aldona Kowalska
Endocrine Pathology.2020; 31(2): 143. CrossRef - High risk of malignancy in cases with atypia of undetermined significance on fine needle aspiration of thyroid nodules even after exclusion of NIFTP
Sevgiye Kaçar Özkara, Büşra Yaprak Bayrak, Gupse Turan
Diagnostic Cytopathology.2020; 48(11): 986. CrossRef - The importance of risk of neoplasm as an outcome in cytologic‐histologic correlation studies on thyroid fine needle aspiration
Yu‐Hsin Chen, Kristen L. Partyka, Rae Dougherty, Harvey M. Cramer, Howard H. Wu
Diagnostic Cytopathology.2020; 48(12): 1237. CrossRef - Preoperative diagnostic categories of fine needle aspiration cytology for histologically proven thyroid follicular adenoma and carcinoma, and Hurthle cell adenoma and carcinoma: Analysis of cause of under- or misdiagnoses
Hee Young Na, Jae Hoon Moon, June Young Choi, Hyeong Won Yu, Woo-Jin Jeong, Yeo Koon Kim, Ji-Young Choe, So Yeon Park, Paula Soares
PLOS ONE.2020; 15(11): e0241597. CrossRef - How is noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) shaping the way we interpret thyroid cytology?
Michiya Nishino
Journal of the American Society of Cytopathology.2019; 8(1): 1. CrossRef - Cytological Diagnoses Associated with Noninvasive Follicular Thyroid Neoplasms with Papillary-Like Nuclear Features According to the Bethesda System for Reporting Thyroid Cytopathology: A Systematic Review and Meta-Analysis
Massimo Bongiovanni, Luca Giovanella, Francesco Romanelli, Pierpaolo Trimboli
Thyroid.2019; 29(2): 222. CrossRef - Preoperative Diagnostic Categories of Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features in Thyroid Core Needle Biopsy and Its Impact on Risk of Malignancy
Hee Young Na, Ji Won Woo, Jae Hoon Moon, June Young Choi, Woo-Jin Jeong, Yeo Koon Kim, Ji-Young Choe, So Yeon Park
Endocrine Pathology.2019; 30(4): 329. CrossRef - Papillary Thyroid Microcarcinoma: Reclassification to Non-Invasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features (NIFTP): a Retrospective Clinicopathologic Study
Khurram Shafique, Virginia A. LiVolsi, Kathleen Montone, Zubair W. Baloch
Endocrine Pathology.2018; 29(4): 339. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


Fig. 1.
Fig. 2.
| FNAC diagnostic category | No. (%) |
|---|---|
| I. Non-diagnostic | 727 (13.1) |
| II. Benign | 2,125 (38.3) |
| III. Atypia of undetermined significance (AUS) | 882 (15.9) |
| IIIA. AUS-NA | 542 (61.4) |
| IIIB. AUS-MF | 132 (15.0) |
| IIIC. AUS-HC | 73 (8.3) |
| IIID. AUS-others | 135 (15.3) |
| IV. Follicular neoplasm | 44 (0.8) |
| V. Suspicious for malignancy | 499 (9.0) |
| VI. Malignant | 1272 (22.9) |
| Total | 5,549 (100) |
| FNAC diagnostic category | No. of surgical specimens | Final diagnosis |
Other |
|||
|---|---|---|---|---|---|---|
| Nodular hyperplasia | Follicular adenoma | Follicular carcinoma | Papillary carcinoma | |||
| Non-diagnostic | 73 | 14 (19.2) | 11 (15.1) | 1 (1.4) | 47 (64.4) | 0 |
| Benign | 54 | 28 (51.9) | 6 (11.1) | 2 (3.7) | 16 (29.6) | 2 (3.7) |
| AUS | 306 | 34 (11.1) | 40 (13.1) | 15 (4.9) | 211 (68.9) | 6 (2.0) |
| AUS-NA | 215 | 12 (5.6) | 12 (5.6) | 4 (1.9) | 185 (86.0) | 2 (0.9) |
| AUS-MF | 53 | 8 (15.1) | 17 (32.1) | 11 (20.7) | 17 (32.1) | 0 |
| AUS-HC | 17 | 7 (41.2) | 9 (52.9) | 0 | 0 | 1 (5.9) |
| AUS-others | 21 | 7 (33.3) | 2 (9.5) | 0 | 9 (42.9) | 3 (14.3) |
| Follicular neoplasm | 27 | 7 (25.9) | 10 (37.0) | 5 (18.5) | 5 (18.5) | 0 |
| Suspicious for malignancy | 393 | 2 (0.5) | 1 (0.3) | 2 (0.5) | 387 (98.5) | 1 (0.3) |
| Malignant | 1,038 | 0 | 0 | 1 (0.1) | 1,034 (99.6) | 3 (0.3) |
| Total | 1,891 | 85 (4.5) | 68 (3.6) | 26 (1.4) | 1,700 (89.9) | 12 (0.6) |
| FNAC diagnostic category | Variants of PTC in final diagnosis |
|||||
|---|---|---|---|---|---|---|
| Conventional | NIFTP | Invasive encapsulated follicular variant | Infiltrative follicular variant | Tall cell variant | Other rare variants | |
| Non-diagnostic | 32 (2.2) | 1 (4.0) | 4 (8.8) | 5 (7.7) | 3 (2.8) | 2 (11.8) |
| Benign | 6 (0.4) | 5 (20.0) | 4 (8.8) | 1 (1.6) | 0 | 0 |
| AUS | 144 (10.0) | 14 (56.0) | 17 (37.8) | 25 (40.3) | 8 (7.5) | 3 (17.6) |
| AUS-NA | 135 (9.3) | 9 (36.0) | 11 (24.4) | 21 (33.9) | 7 (6.6) | 2 (11.8) |
| AUS-MF | 3 (0.2) | 5 (20.0) | 5 (11.1) | 4 (6.4) | 0 | 0 |
| AUS-HC | 0 | 0 | 0 | 0 | 0 | 0 |
| AUS-others | 6 (0.4) | 0 | 1 (2.2) | 0 | 1 (0.9) | 1 (5.9) |
| Follicular neoplasm | 0 | 2 (8.0) | 2 (8.3) | 1 (1.6) | 0 | 0 |
| Suspicious for malignancy | 339 (23.5) | 3 (12.0) | 10 (4.4) | 14 (22.6) | 20 (18.9) | 1 (5.9) |
| Malignant | 924 (63.9) | 0 |
8 (17.8) |
16 (25.8) | 75 (70.8) | 11 (64.7) |
| Total No. | 1,445 | 25 | 45 | 62 | 106 | 17 |
| FNAC diagnostic category | Conventional PTC | NIFTP/EFVPTC | Infiltrative FVPTC | p-value |
p-value |
p-value |
|---|---|---|---|---|---|---|
| Non-diagnostic | 32 (2.2) | 5 (7.1) | 5 (7.7) | .025 | 1.000 | .016 |
| Benign | 6 (0.4) | 9 (12.9) | 1 (1.6) | < .001 | .019 | .259 |
| AUS | 144 (10.0) | 31 (44.3) | 25 (40.3) | < .001 | .646 | < .001 |
| AUS-NA | 135 (9.3) | 20 (28.6) | 21(33.9) | < .001 | .511 | < .001 |
| AUS-MF | 3 (0.2) | 10 (14.3) | 4 (6.4) | < .001 | .167 | < .001 |
| AUS-HC | 0 (0) | 0 (0) | 0 (0) | 1.000 | 1.000 | 1.000 |
| AUS-others | 6 (0.4) | 1 (1.4) | 0 (0) | .282 | 1.000 | 1.000 |
| Follicular neoplasm | 0 (0) | 4 (5.7) | 1 (1.6) | < .001 | .370 | .041 |
| Suspicious for malignancy | 339 (23.5) | 13 (18.6) | 14 (22.6) | .344 | .569 | .873 |
| Malignant | 924 (63.9) | 8 (11.4) | 16 (25.8) | < .001 | .033 | < .001 |
| FNAC diagnostic category | No. | No. of malignancy including NIFTP (%) | No. of malignancy excluding NIFTP (%) | Absolute decrease in ROM (%) | Relative decrease in ROM (%) |
|---|---|---|---|---|---|
| Non-diagnostic | 73 | 48 (65.8) | 47 (64.4) | 1.4 | 2.1 |
| Benign | 54 | 18 (33.3) | 13 (24.1) | 9.2 | 27.6 |
| AUS | 306 | 232 (75.8) | 218 (71.2) | 4.6 | 6.1 |
| AUS-NA | 215 | 191 (88.8) | 182 (84.7) | 4.1 | 4.6 |
| AUS-MF | 53 | 28 (52.8) | 23 (43.3) | 9.5 | 18.0 |
| AUS-HC | 17 | 1 (5.9) | 1 (5.9) | 0 | 0 |
| AUS-others | 21 | 12 (44.4) | 12 (44.4) | 0 | 0 |
| Follicular neoplasm | 27 | 10 (37.0) | 8 (29.6) | 7.4 | 20.0 |
| Suspicious for malignancy | 393 | 390 (99.2) | 387 (98.5) | 0.7 | 0.7 |
| Malignant | 1,038 | 1,038 (100) | 1,038 (100) | 0 | 0 |
| Total | 1,891 | 1,736 (91.8) | 1,711 (90.5) | 1.3 | 1.4 |
| FNAC diagnostic category | No. | No. of malignancy including NIFTP (%) | No. of malignancy excluding NIFTP (%) | Absolute decrease in ROM (%) | Relative decrease in ROM (%) |
|---|---|---|---|---|---|
| Non-diagnostic | 727 | 48 (6.6) | 47 (6.5) | 0.1 | 1.5 |
| Benign | 2,125 | 18 (0.8) | 13 (0.6) | 0.2 | 25.0 |
| AUS | 882 | 232 (26.3) | 218 (24.7) | 1.6 | 6.1 |
| AUS-NA | 542 | 191 (35.2) | 182 (33.6) | 1.6 | 4.5 |
| AUS-MF | 132 | 28 (21.2) | 23 (17.4) | 3.8 | 17.9 |
| AUS-HC | 73 | 1 (1.4) | 1 (1.4) | 0 | 0 |
| AUS-others | 135 | 12 (8.9) | 12 (8.9) | 0 | 0 |
| Follicular neoplasm | 44 | 10 (22.7) | 8 (18.2) | 4.5 | 19.8 |
| Suspicious for malignancy | 499 | 390 (78.2) | 387 (77.6) | 0.6 | 0.8 |
| Malignant | 1,272 | 1,038 (81.6) | 1,038 (81.6) | 0 | 0 |
| Total | 5,549 | 1,736 (31.3) | 1,711 (30.8) | 0.5 | 1.6 |
TBSRTC, the Bethesda System for Reporting Thyroid Cytopathology; FNAC, fine-needle aspiration cytology; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.
Values are presented as number (%). FNAC, fine needle aspiration cytology; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells. Other includes two cases of parathyroid adenoma in benign; two medullary carcinomas, one poorly differentiated carcinoma, two anaplastic carcinomas, and one lymphoma in AUS; one medullary carcinoma in suspicious for malignancy; one medullary carcinoma, one anaplastic carcinoma, and one thymic carcinoma in malignant category.
Values are presented as number (%). FNAC, fine needle aspiration cytology; PTC, papillary thyroid carcinoma; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells. p = .044, Fisher exact test.
Values are presented as number (%). PTC, papillary thyroid carcinoma; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; EFVPTC, encapsulated follicular variant of papillary thyroid carcinoma; FVPTC, follicular variant of papillary thyroid carcinoma; FNAC, fine-needle aspiration cytology; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells. Conventional PTC vs. NIFTP/EFVPTC; NIFTP/EFVPTC vs. infiltrative FVPTC; Conventional PTC vs. infiltrative FVPTC.
NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; FNAC, fine needle aspiration cytology; ROM, risk of malignancy; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.
NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; FNAC, fine needle aspiration cytology; ROM, risk of malignancy; AUS, atypia of undetermined significance; NA, nuclear atypia; MF, microfollicles; HC, Hurthle cells.

 E-submission
E-submission