Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 54(3); 2020 > Article
-
Original Article
Sarcoma metastasis to the pancreas: experience at a single institution -
Miseon Lee1
 , Joon Seon Song1
, Joon Seon Song1 , Seung-Mo Hong1
, Seung-Mo Hong1 , Se Jin Jang1
, Se Jin Jang1 , Jihun Kim1
, Jihun Kim1 , Ki Byung Song2
, Ki Byung Song2 , Jae Hoon Lee2
, Jae Hoon Lee2 , Kyung-Ja Cho, MD, PhD1
, Kyung-Ja Cho, MD, PhD1
-
Journal of Pathology and Translational Medicine 2020;54(3):220-227.
DOI: https://doi.org/10.4132/jptm.2020.03.04
Published online: April 22, 2020
1Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
2Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- Corresponding Author: Kyung-Ja Cho, MD, PhD, Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-4545, Fax: +82-2-472-7898, E-mail: kjc@amc.seoul.kr
© 2020 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Metastatic synovial sarcoma masquerading as primary neuroendocrine tumor of pancreas: a diagnostic conundrum
Sherrin Jacob, Balamurugan Thirunavukkarasu, Rajni Yadav, Anany Gupta, Samagra Agarwal, Shamim A. Shamim, Sameer Rastogi, Adarsh Barwad, Deepali Jain
Clinical Journal of Gastroenterology.2025; 18(3): 499. CrossRef - Metastatic tumors to the pancreas: An institutional experience
Matthew Romanish, Rana Naous
Annals of Diagnostic Pathology.2025; 79: 152528. CrossRef - Visceral Metastases of Osteosarcoma in the Hepatopancreatobiliary System
Anna Hohensteiner, Lars Kowalscheck, Kevin Döring, Gerhard Martin Hobusch, Raphael Johannes Tanios, Oliver Strobel, Reinhard Windhager, Philipp Theodor Funovics
Journal of Clinical Medicine.2025; 14(24): 8702. CrossRef - Metastatic clear cell sarcoma of the pancreas: A sporadic cancer
Vittorio Gebbia, Carlo Carnaghi
World Journal of Clinical Cases.2024; 12(18): 3291. CrossRef - Metastatic clear cell sarcoma of the pancreas: An overview
Rachid Ait Addi
World Journal of Clinical Cases.2024; 12(29): 6262. CrossRef - Myxofibrosarcoma with pancreatic metastasis, a case report and literature reviews
Kodai ABE, Yasutomo SEKIDO, Yasuo KABESHIMA
Suizo.2024; 39(5): 334. CrossRef - Metástasis pancreática de sarcoma, un hallazgo infrecuente
Daniel Aparicio-López, Jorge Chóliz-Ezquerro, Carlos Hörndler-Algárate, Mario Serradilla-Martín
Gastroenterología y Hepatología.2023; 46(5): 376. CrossRef - Pancreatic metastasis from sarcoma, an infrequent finding
Daniel Aparicio-López, Jorge Chóliz-Ezquerro, Carlos Hörndler-Algárate, Mario Serradilla-Martín
Gastroenterología y Hepatología (English Edition).2023; 46(5): 376. CrossRef - Acute pancreatitis secondary to osteosarcoma metastasis
Pablo Salmón Olavarría, Ana Gordo Ortega, Maren Eizagirre Ubegun, Verónica Ubieto Capella, Elena Carracedo Vega, Juan Carrascosa Gil, David Ruiz-Clavijo García
Revista Española de Enfermedades Digestivas.2023;[Epub] CrossRef - First Recurrence of Synovial Sarcoma Presenting With Solitary Pancreatic Mass
Raja R Narayan, Greg W Charville, Daniel Delitto, Kristen N Ganjoo
Cureus.2022;[Epub] CrossRef - Intravenous Leiomyosarcoma of the Lower Extremity: As Peripheral as It Gets
Levent F Umur, Selami Cakmak, Mehmet Isyar, Hamdi Tokoz
Cureus.2021;[Epub] CrossRef - Could the burden of pancreatic cancer originate in childhood?
Smaranda Diaconescu, Georgiana Emmanuela Gîlcă-Blanariu, Silvia Poamaneagra, Otilia Marginean, Gabriela Paduraru, Gabriela Stefanescu
World Journal of Gastroenterology.2021; 27(32): 5322. CrossRef - Staged Surgical Resection of Primary Pulmonary Synovial Sarcoma with Synchronous Multiple Pancreatic Metastases: Report of a Rare Case and Review of the Literature
Panagiotis Dorovinis, Nikolaos Machairas, Stylianos Kykalos, Paraskevas Stamopoulos, George Agrogiannis, Nikolaos Nikiteas, Georgios C. Sotiropoulos
Journal of Gastrointestinal Cancer.2021; 52(3): 1151. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


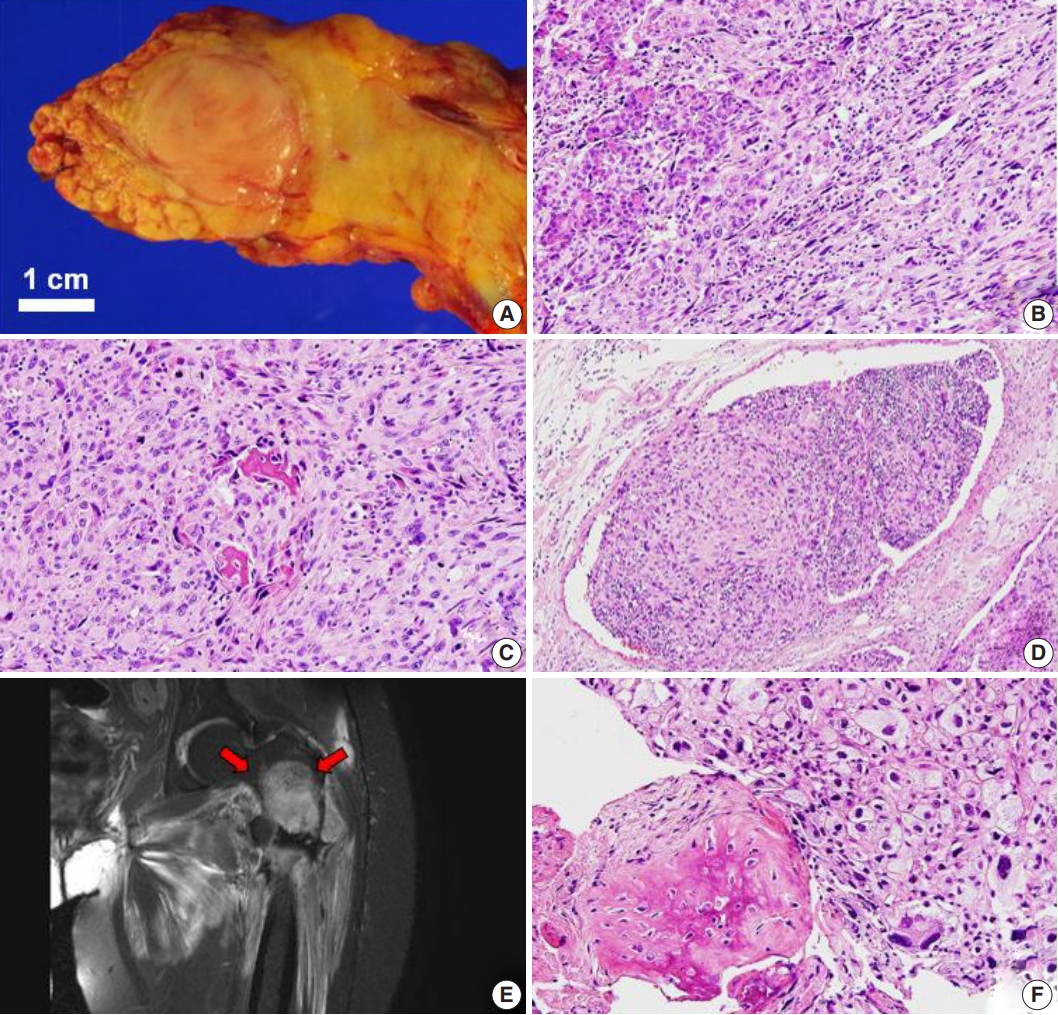
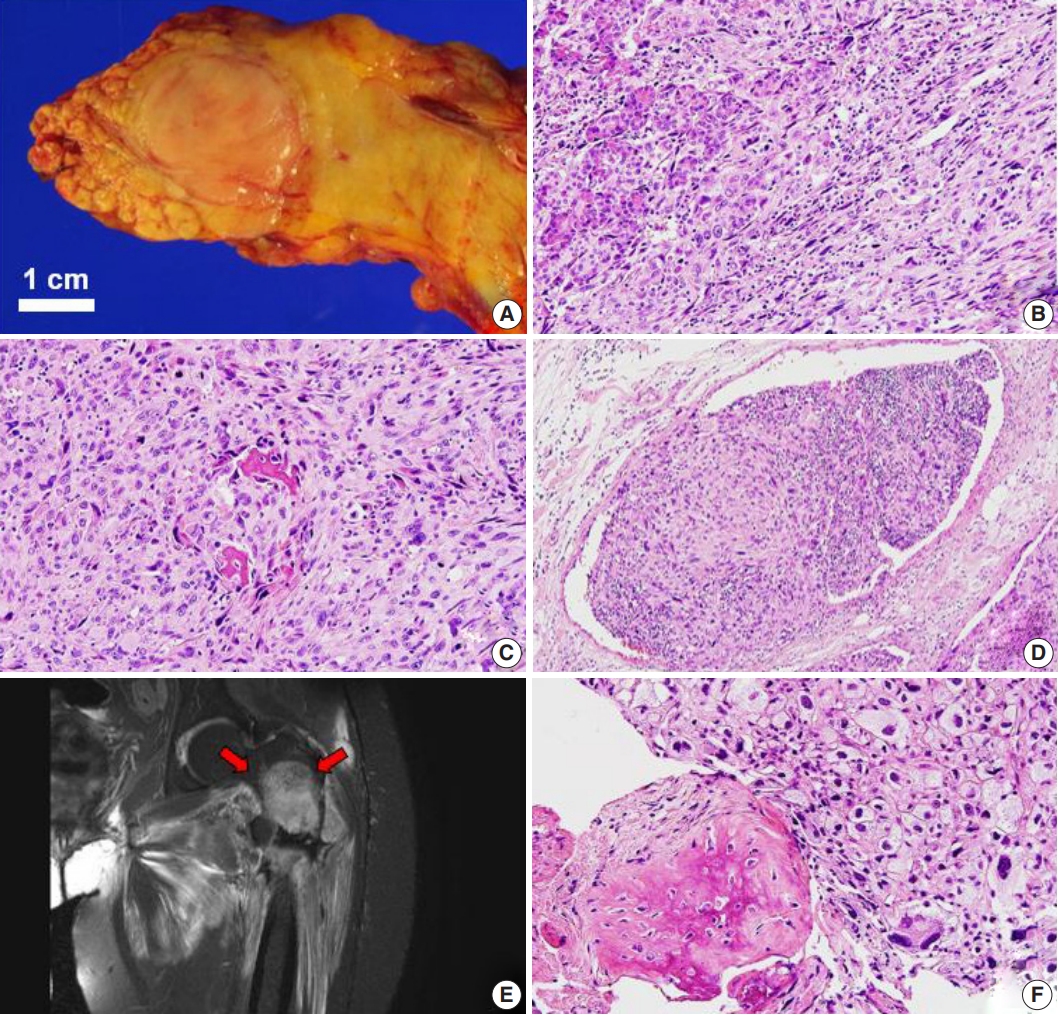
Fig. 1.
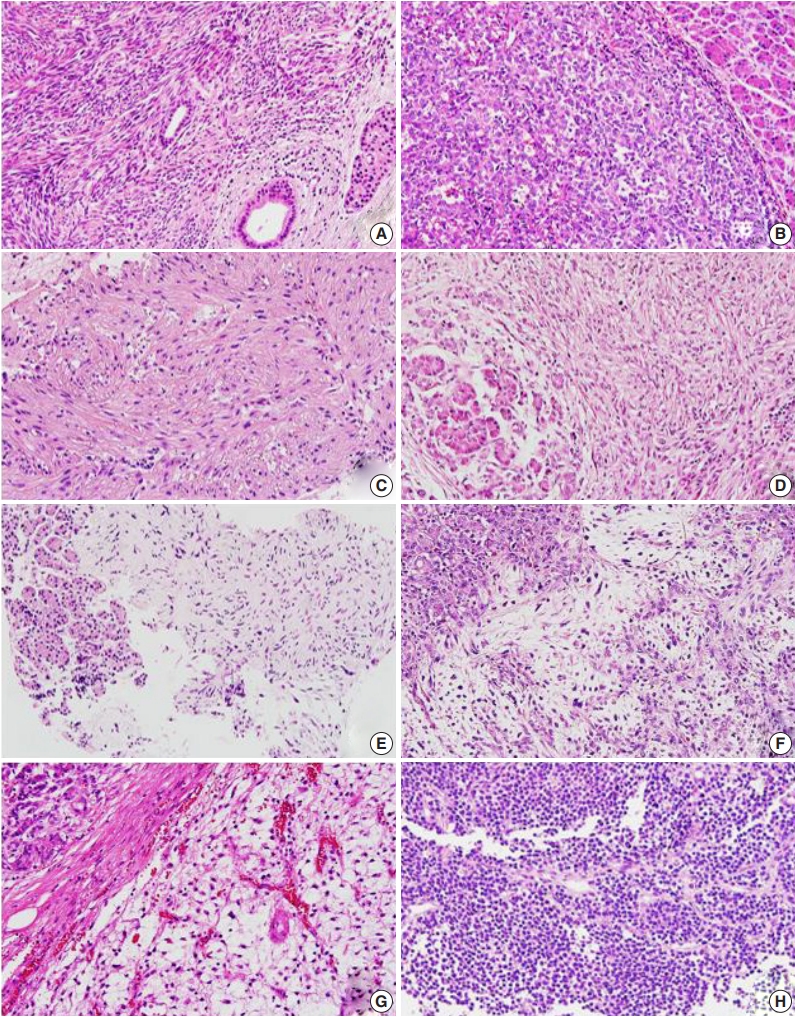
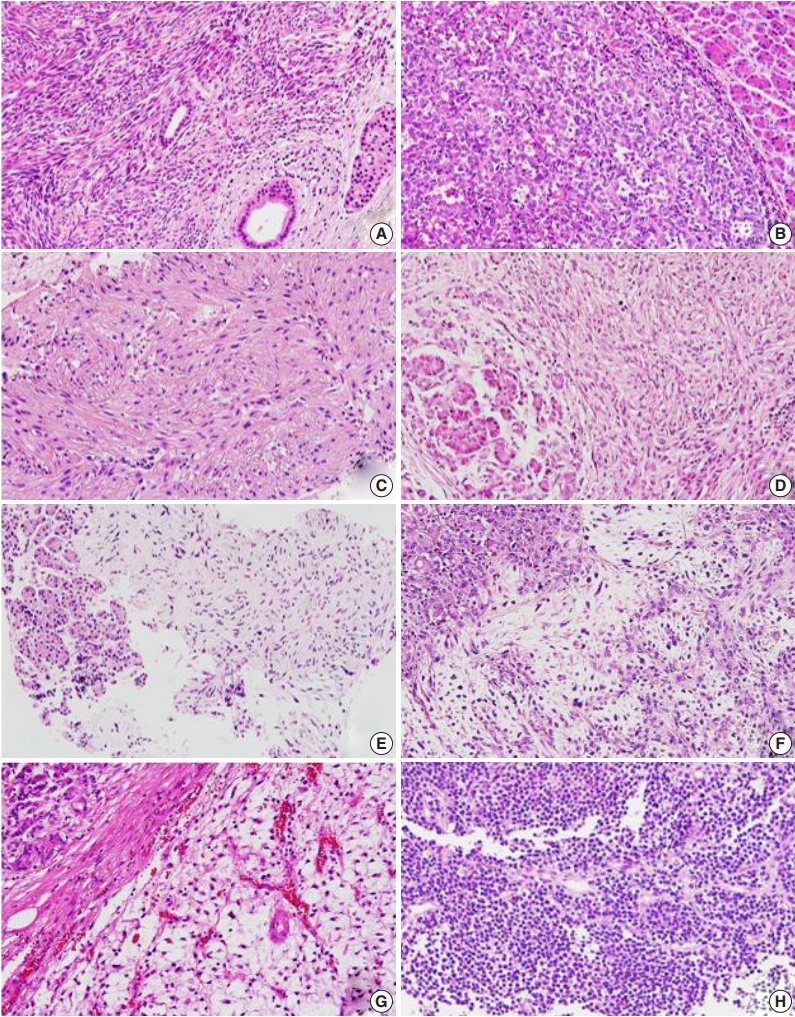
Fig. 2.
| Case No. | Sex/age at pancreatic metastasis (yr) | Primary tumor |
Pathologic diagnosis | Interval between primary tumor detection and pancreatic metastasis (mo) | Pancreatic metastasis |
Associated metastases | Survival after pancreatic metastasis (mo) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Location | Size (cm) | Treatment | Local recurrence | Location | No. of pancreatic metastases | Size (largest, cm) | Treatment | Type of procedure | Dead | Alive | |||||
| 1 | F/62 | Lung | 7.5 | OP | No | Synovial sarcoma, FNCLCC grade 3 | 40 | Body | Single | 2.7 | NeoCTx + OP | DP | No | - | 92 |
| 2 | M/45 | Lung | 7 | OP | Yes | Malignant solitary fibrous tumor, FNCLCC grade 3 | 11 | Tail | Single | 2.6 | OP + RTx and CTx | T | Umbilicus, adrenal gland | 24 | - |
| 3 | F/48 | Brain | 7.5 | OP + RTx | Yes | Solitary fibrous tumor/ hemangiopericytoma, WHO grade III | 64 | Body, tail | Multiple | 3.5 | RTx + OP | DP | Bone (femur, tibia), breast, lung | 31 | - |
| 4 | F/70 | Brain | NA | OP + RTx | Yes | Solitary fibrous tumor/ hemangiopericytoma, WHO grade III | 135 | Head | Single | 2.6 | OP + RTx | PPPD | Bone (humerus), lung, | - | 41 |
| 5 | F/58 | Bone (tibia) | 6 | NeoCTx + OP + CTx | No | Undifferentiated pleomorphic sarcoma, FNCLCC grade 3 | 88 | Head | Single | 3.5 | RTx + CTx | Biopsy | Bone (pelvis) | - | 10 |
| 6 | F/57 | Bone (femur) | 9 | OP + RTx + CTx | No | Osteosarcoma, FNCLCC grade 3 | 15 mo prior | Tail | Single | 2.7 | OP + CTx | DP | Skin (scalp), bone (rib, ilium, sternum, pelvis), brain | 18 | - |
| 7 | F/32 | Bone (skull) | 4 | OP + RTx | No | Mesenchymal chondrosarcoma, FNCLCC grade 3 | 65 | Tail | Single | 19 | OP | DP | Lung, mesentery, bone (femur) | 48 | - |
| 8 | F/28 | Bone (femur) | 11.7 | NeoCTx + OP + CTx | No | High-grade spindle-cell sarcoma, type uncertain, FNCLCC grade 3 | 20 | Body | Single | 4 | OP | DP | Bone (pelvis) | 11 | - |
| 9 | F/35 | Pulmonary vein | 4.6 | RTx + OP | Yes | Intimal sarcoma, FNCLCC grade 2 | 14 | Tail | Single | 2.6 | CTx | Biopsy | Retroperitoneal LN, bone (left humerus), lung | 29 | - |
| 10 | M/52 | Soft tissue (knee) | 8.2 | OP + RTx + CTx | No | Myxofibrosarcoma, FNCLCC grade 2 | 26 | Head | Single | 2.5 | OP | PPPD | No | - | 4 |
| 11 | M/35 | Soft tissue (thigh) | 22 | OP | No | Myxoid liposarcoma, FNCLCC grade 2 | 0 | Tail | Multiple | 11 | OP + CTx | DP | Bone (humerus) | 16 | - |
| 12 | F/60 | Uterus | 8.5 | OP | Yes (vaginal stump) | Rhabdomyosarcoma, subtype uncertain, FNCLCC grade 3 | 8 | Head, body, tail | Multiple | NA | CTx | Biopsy | No | 5 | - |
F, female; OP, operation; FNCLCC, Fédération Nationale des Centres de Lutte Contre le Cancer; NeoCTx, neoadjuvant chemotherapy; DP, distal pancreatectomy; M, male; RTx, radiation therapy; CTx, adjuvant chemotherapy; T, tumorectomy; WHO, World Health Organization; NA, not available; PPPD, pylorus-preserving pancreaticoduodenectomy; LN, lymph node.

 E-submission
E-submission