Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 54(3); 2020 > Article
-
Editorial
New insights into classification and risk stratification of encapsulated thyroid tumors with a predominantly papillary architecture -
Chan Kwon Jung1,2
 , So Yeon Park3
, So Yeon Park3 , Jang-Hee Kim4
, Jang-Hee Kim4 , Kennichi Kakudo5
, Kennichi Kakudo5
-
Journal of Pathology and Translational Medicine 2020;54(3):197-203.
DOI: https://doi.org/10.4132/jptm.2020.04.29
Published online: May 14, 2020
1Department of Hospital Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea
2Cancer Research Institute, College of Medicine, The Catholic University of Korea, Seoul, Korea
3Department of Pathology, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea
4Department of Pathology, Ajou University School of Medicine, Suwon, Korea
5Department of Pathology and Thyroid Disease Center, Izumi City General Hospital, Izumi, Japan
- Corresponding Author: Chan Kwon Jung, MD, PhD Department of Pathology, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpo-daero, Seocho-gu, Seoul 06591, Korea Tel: +82-2-2258-1622, Fax: +82-2-2258-1627, E-mail: ckjung@catholic.ac.kr
© 2020 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- This study was approved by the Institutional Review Boards of Seoul St. Mary’s Hospital (IRB No. KC20ZASI0282), Seoul National University Bundang Hospital (IRB No. B-2004-611-103), and Ajou University Hospital (IRB No. AJIRB-BMREXP-20-074) with a waiver of informed consent.
Ethics Statement
Author contributions
Conceptualization: CKJ, KK.
Data curation: CKJ, SYP, JHK, KK.
Formal analysis: CKJ.
Funding acquisition: CKJ.
Investigation: CKJ.
Methodology: CKJ, SYP, JHK, KK.
Project administration: CKJ.
Resources: CKJ.
Supervision: CKJ.
Validation: CKJ, SYP, JHK, KK.
Visualization: CKJ, KK.
Writing—original draft: CKJ.
Writing—review & editing: CKJ, SYP, JHK, KK.
Conflicts of Interest
C.K.J. and S.Y.P. are the editors-in-chief of Journal of Pathology and Translational Medicine. J.H.K. and K.K. are editorial-board members of the journal.
Funding
This research was funded by a grant (2017R1D1A1B03029597) from the Basic Science Research Program through the National Research Foundation of Korea funded by the Ministry of Science and ICT.
| Tumor behavior | Invasion | Nuclear scorea | Papillary architecture |
Predominantly follicular growth |
|
|---|---|---|---|---|---|
| Presence of true papillae | Absence of true papillae | ||||
| Benign | Absent | 0 to 1 | Follicular adenoma with papillary hyperplasia | Follicular adenoma, conventional type | Follicular adenoma, conventional type |
| Borderline | Absent | 2 (rarely 3) | NEPRAS | - | NIFTP |
| Questionable | 2 (rarely 3) | - | - | WDT-UMP | |
| Malignant | Present | 1 (rarely 0) | Follicular carcinoma | Follicular carcinoma | Follicular carcinoma |
| Present | 2 to 3 | Papillary carcinoma, encapsulated classic variant | Papillary carcinoma, encapsulated classic variant with predominant follicular growth | Papillary carcinoma, invasive encapsulated follicular variant | |
NEPRAS, noninvasive encapsulated papillary RAS-like thyroid tumor; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; WDTUMP, well-differentiated tumor of uncertain malignant potential.
aNuclear score is calculated as the sum of all categories of nuclear features of papillary carcinoma: (1) nuclear size and shape (nuclear enlargement, overlapping, crowding, and elongation), (2) nuclear membrane irregularities (irregular nuclear contours, grooves, and pseudoinclusions), (3) chromatin characteristics (chromatin clearing, margination of chromatin to the membrane, glassy nuclei) [14].
| Reference | Age (yr) | Sex | FNA categorya | Size (cm) | Invasion | Nuclear score | Papillary component | Cystic change | Psammoma bodies | Molecular profile | Immunohistochemistry |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Index case, Ohba et al. (2019) [2] | 26 | M | II, IV | 2.3 | Absent | 2 | Dominant | Present | Present | KRAS G12A; BRAF, NRAS, HRAS, and TERT promoter: wild type | Ki-67 index 1%–2% |
| Rosario (2020) [1] | 35 | F | IV | 4.0 | Absent | 2 | < 1% | NA | NA | BRAF wild type | |
| 43 | F | III | 2.2 | Absent | 2 | 1% | NA | NA | BRAF wild type | ||
| 48 | M | IV | 3.5 | Absent | 2 | 1% | NA | NA | BRAF wild type | ||
| Case 1 | 9 | M | V | 3.7 | Absent | 2 | Dominant | Present | Present | KRAS G12V; BRAF and NRAS: wild type | CK19, focal +; HBME1, focal +; CD56, focal loss; ALK, negative; Pan-Trk, negative |
| Case 2 | 38 | M | III | 1.2 | Capsular | 2 | Dominant | Present | Absent | NRAS Q61R; BRAF, HRAS, KRAS, and TERT promoter: wild type | |
| Case 3 | 21 | M | II | 4.0 | Capsular | 2 | Dominant | Present | Absent | BRAF, NRAS, HRAS, and KRAS: wild type |
- 1. Rosario PW. Noninvasive encapsulated papillary RAS-like thyroid tumor (NEPRAS) or encapsulated papillary thyroid carcinoma (PTC). J Pathol Transl Med 2020 Mar 4 [Epub]. https://doi.org/10.4132/jptm.2020.02.05. ArticlePDF
- 2. Ohba K, Mitsutake N, Matsuse M, et al. Encapsulated papillary thyroid tumor with delicate nuclear changes and a KRAS mutation as a possible novel subtype of borderline tumor. J Pathol Transl Med 2019; 53: 136-41. ArticlePubMedPMCPDF
- 3. Lloyd RV, Osamura RY, Klöppel G, Rosai J. WHO classification of tumours of endocrine organs. 4th ed. Lyon: IARC Press, 2017; 65-91.
- 4. Mete O, Asa SL. Thyroid tumor capsular invasion: the bottom line or much ado about nothing? Endocr Pathol 2020 Mar 4 [Epub]. https://doi.org/10.1007/s12022-020-09621-6. ArticlePDF
- 5. Jung CK, Kim C. Effect of lowering the diagnostic threshold for encapsulated follicular variant of papillary thyroid carcinoma on the prevalence of non-invasive follicular thyroid neoplasm with papillary-like nuclear features: a single-institution experience in Korea. J Basic Clin Med 2017; 6: 26-8.
- 6. Hirokawa M, Carney JA, Goellner JR, et al. Observer variation of encapsulated follicular lesions of the thyroid gland. Am J Surg Pathol 2002; 26: 1508-14. ArticlePubMed
- 7. Lloyd RV, Erickson LA, Casey MB, et al. Observer variation in the diagnosis of follicular variant of papillary thyroid carcinoma. Am J Surg Pathol 2004; 28: 1336-40. ArticlePubMed
- 8. Zhu Y, Li Y, Jung CK, et al. Histopathologic assessment of capsular invasion in follicular thyroid neoplasms: an observer variation study. Endocr Pathol 2020 Mar 31 [Epub]. https://doi.org/10.1007/s12022-020-09620-7. ArticlePDF
- 9. Tallini G, Tuttle RM, Ghossein RA. The history of the follicular variant of papillary thyroid carcinoma. J Clin Endocrinol Metab 2017; 102: 15-22. ArticlePubMedPDF
- 10. Kakudo K, Bychkov A, Abelardo A, Keelawat S, Kumarasinghe P. Malpractice climate is a key difference in thyroid pathology practice between North America and the rest of the world. Arch Pathol Lab Med 2019; 143: 1171.ArticlePDF
- 11. Cancer Genome Atlas Research Network. Integrated genomic characterization of papillary thyroid carcinoma. Cell 2014; 159: 676-90. PubMedPMC
- 12. Yoo SK, Lee S, Kim SJ, et al. Comprehensive analysis of the transcriptional and mutational landscape of follicular and papillary thyroid cancers. PLoS Genet 2016; 12: e1006239.ArticlePubMedPMC
- 13. Jung SH, Kim MS, Jung CK, et al. Mutational burdens and evolutionary ages of thyroid follicular adenoma are comparable to those of follicular carcinoma. Oncotarget 2016; 7: 69638-48. ArticlePubMedPMC
- 14. Nikiforov YE, Seethala RR, Tallini G, et al. Nomenclature revision for encapsulated follicular variant of papillary thyroid carcinoma: a paradigm shift to reduce overtreatment of indolent tumors. JAMA Oncol 2016; 2: 1023-9. ArticlePubMedPMC
- 15. Jeon S, Kim Y, Jeong YM, Bae JS, Jung CK. CCND1 splice variant as a novel diagnostic and predictive biomarker for thyroid cancer. Cancers (Basel) 2018; 10: E437.Article
- 16. Cho U, Mete O, Kim MH, Bae JS, Jung CK. Molecular correlates and rate of lymph node metastasis of non-invasive follicular thyroid neoplasm with papillary-like nuclear features and invasive follicular variant papillary thyroid carcinoma: the impact of rigid criteria to distinguish non-invasive follicular thyroid neoplasm with papillary-like nuclear features. Mod Pathol 2017; 30: 810-25. ArticlePubMedPDF
- 17. Choden S, Keelawat S, Jung CK, Bychkov A. VE1 immunohistochemistry improves the limit of genotyping for detecting BRAF(V600E) mutation in papillary thyroid cancer. Cancers (Basel) 2020; 12: E596.Article
- 18. Nikiforov YE, Baloch ZW, Hodak SP, et al. Change in diagnostic criteria for noninvasive follicular thyroid neoplasm with papillarylike nuclear features. JAMA Oncol 2018; 4: 1125-6. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- The Asian Thyroid Working Group, from 2017 to 2023
Kennichi Kakudo, Chan Kwon Jung, Zhiyan Liu, Mitsuyoshi Hirokawa, Andrey Bychkov, Huy Gia Vuong, Somboon Keelawat, Radhika Srinivasan, Jen-Fan Hang, Chiung-Ru Lai
Journal of Pathology and Translational Medicine.2023; 57(6): 289. CrossRef - Updates in the Pathologic Classification of Thyroid Neoplasms: A Review of the World Health Organization Classification
Yanhua Bai, Kennichi Kakudo, Chan Kwon Jung
Endocrinology and Metabolism.2020; 35(4): 696. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure




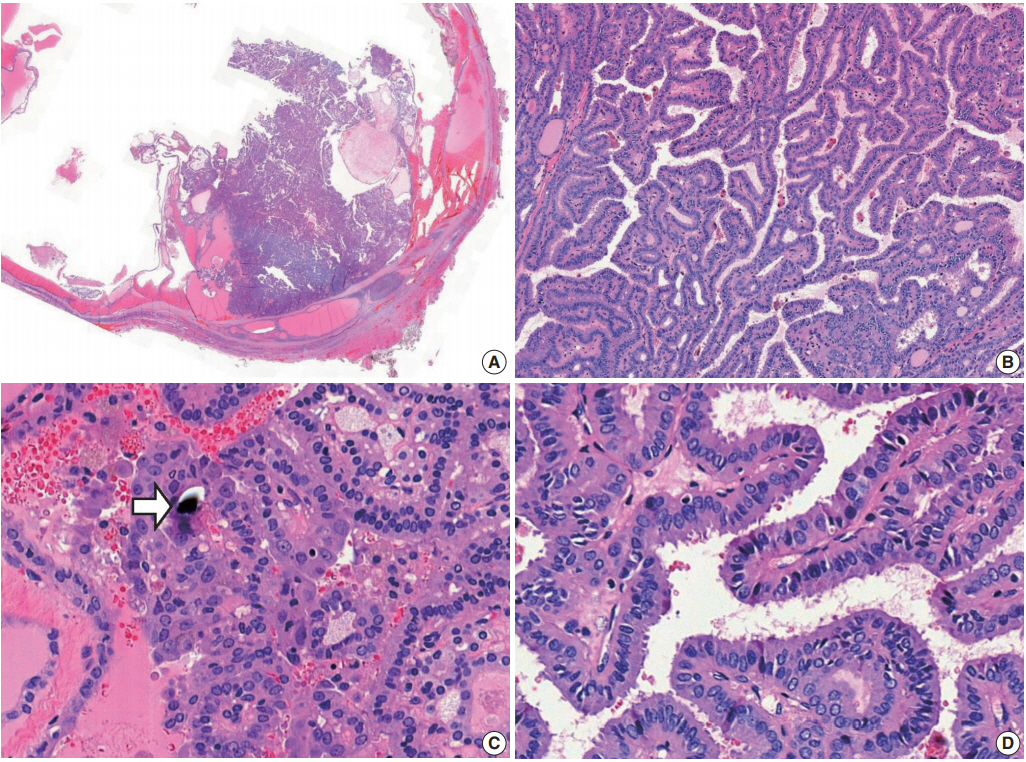
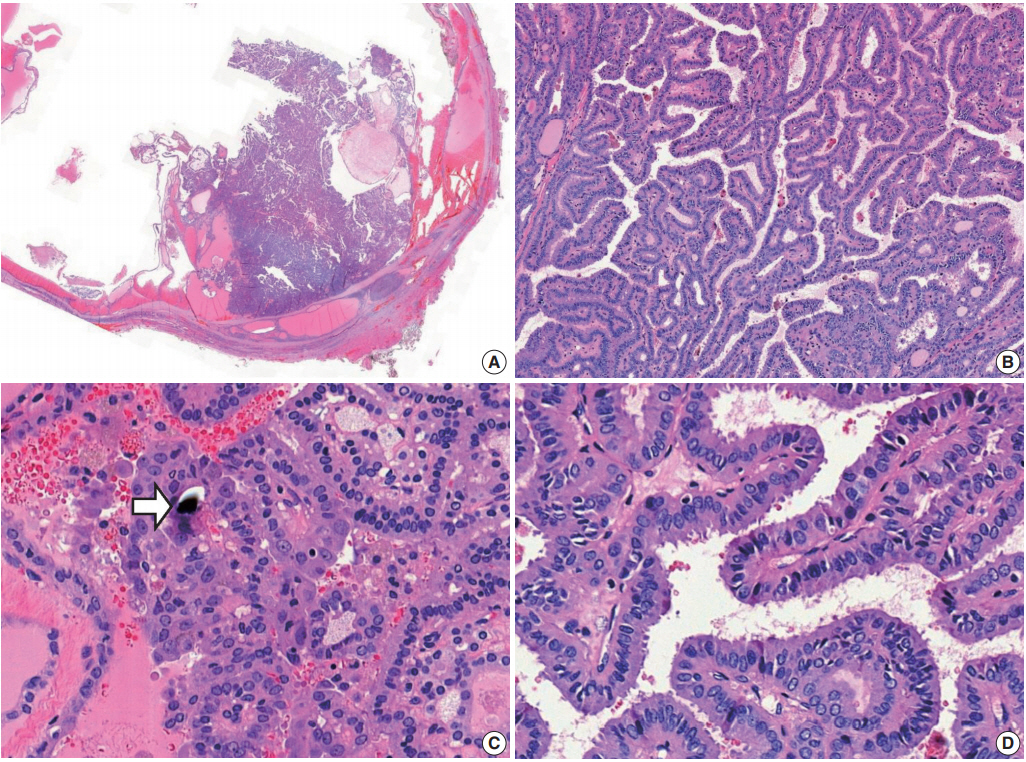
Fig. 1.
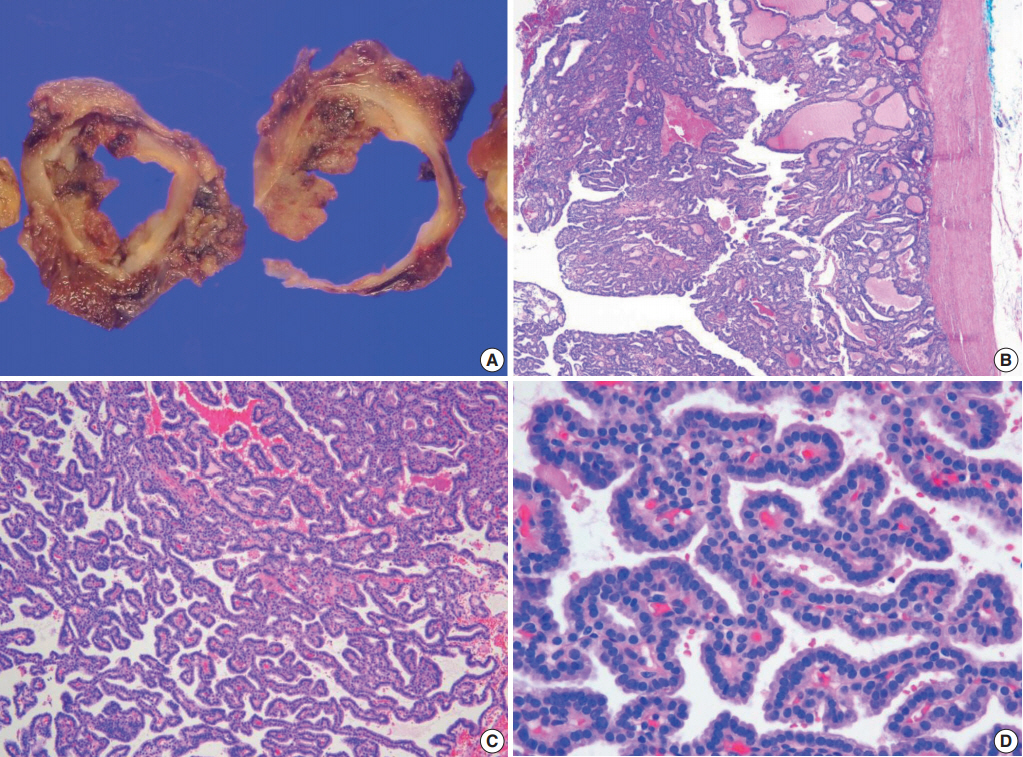
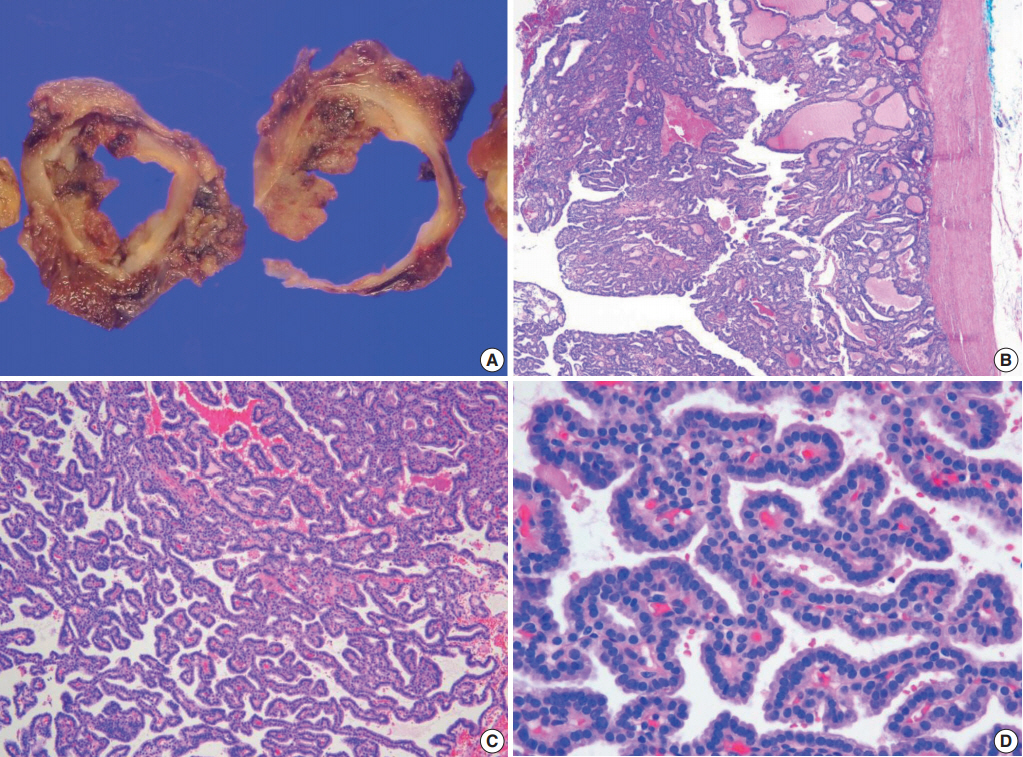
Fig. 2.
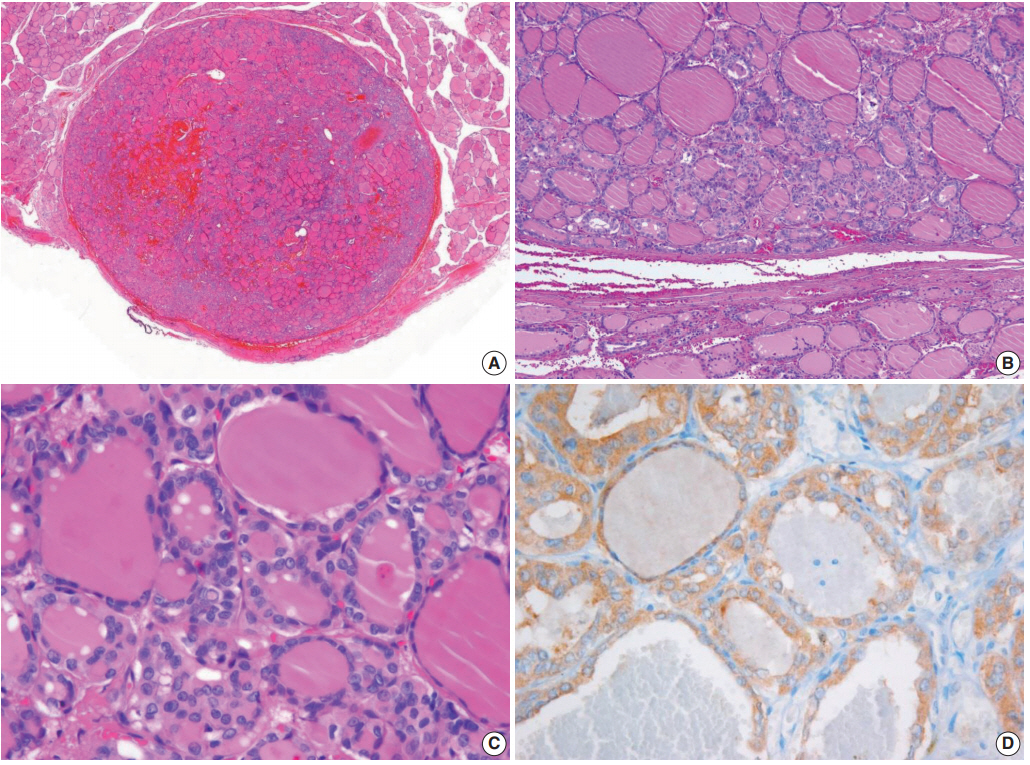
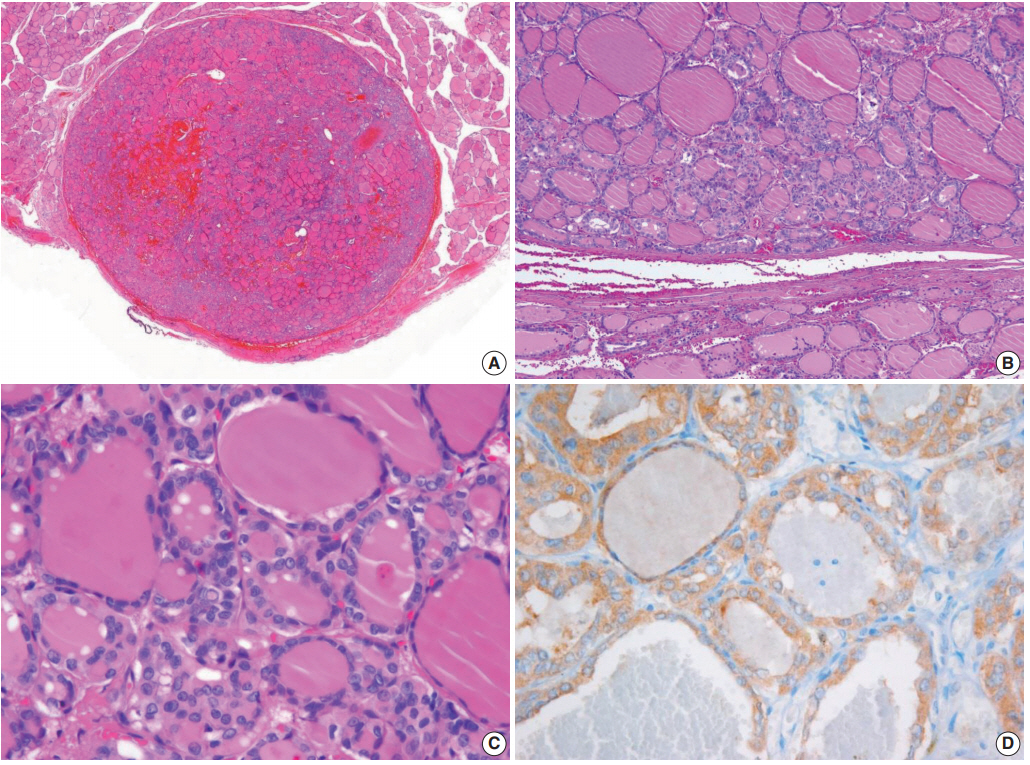
Fig. 3.
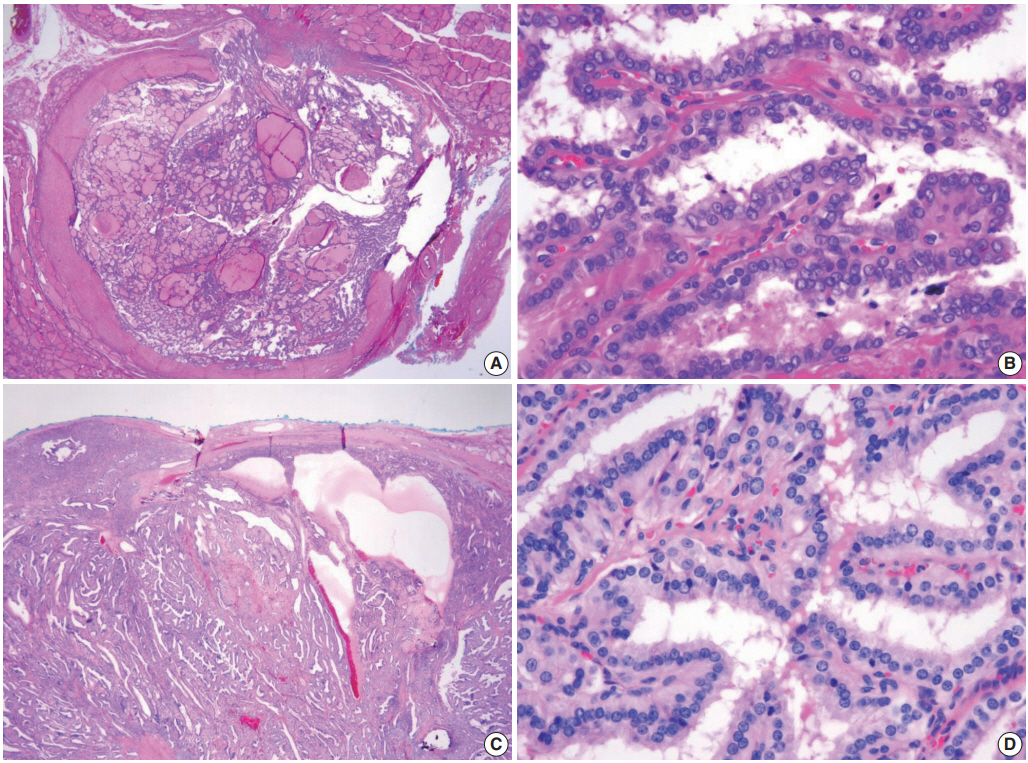
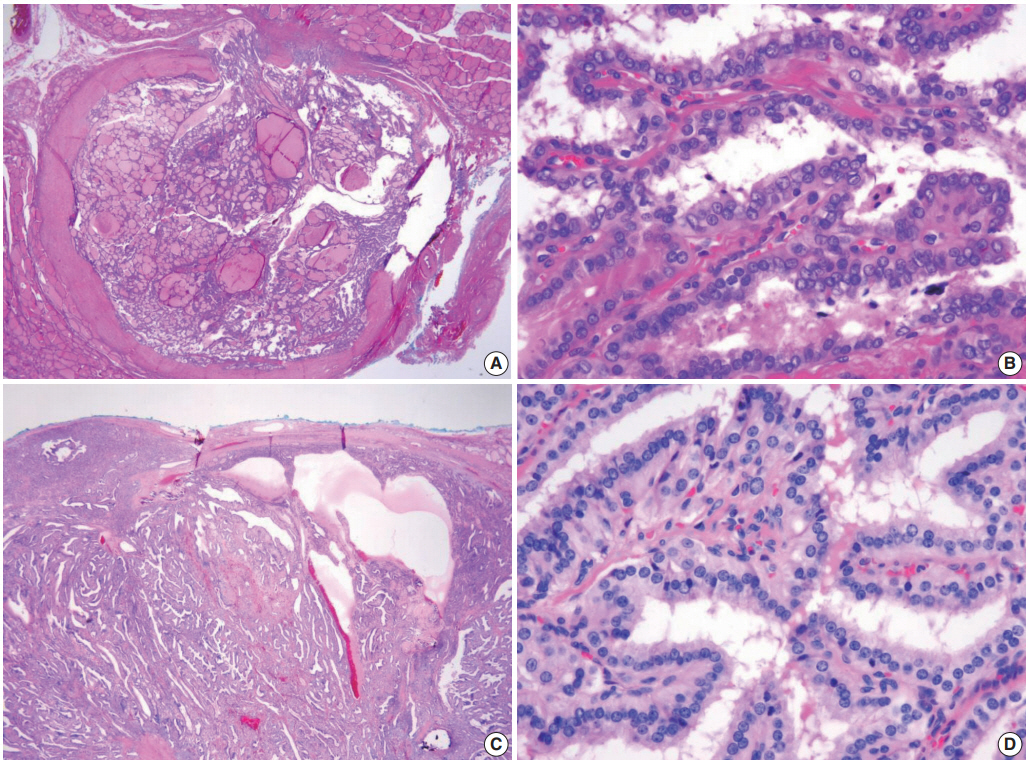
Fig. 4.
| Tumor behavior | Invasion | Nuclear score |
Papillary architecture | Predominantly follicular growth |
|
|---|---|---|---|---|---|
| Presence of true papillae | Absence of true papillae | ||||
| Benign | Absent | 0 to 1 | Follicular adenoma with papillary hyperplasia | Follicular adenoma, conventional type | Follicular adenoma, conventional type |
| Borderline | Absent | 2 (rarely 3) | NEPRAS | - | NIFTP |
| Questionable | 2 (rarely 3) | - | - | WDT-UMP | |
| Malignant | Present | 1 (rarely 0) | Follicular carcinoma | Follicular carcinoma | Follicular carcinoma |
| Present | 2 to 3 | Papillary carcinoma, encapsulated classic variant | Papillary carcinoma, encapsulated classic variant with predominant follicular growth | Papillary carcinoma, invasive encapsulated follicular variant | |
| Reference | Age (yr) | Sex | FNA category |
Size (cm) | Invasion | Nuclear score | Papillary component | Cystic change | Psammoma bodies | Molecular profile | Immunohistochemistry |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Index case, Ohba et al. (2019) [2] | 26 | M | II, IV | 2.3 | Absent | 2 | Dominant | Present | Present | KRAS G12A; BRAF, NRAS, HRAS, and TERT promoter: wild type | Ki-67 index 1%–2% |
| Rosario (2020) [1] | 35 | F | IV | 4.0 | Absent | 2 | < 1% | NA | NA | BRAF wild type | |
| 43 | F | III | 2.2 | Absent | 2 | 1% | NA | NA | BRAF wild type | ||
| 48 | M | IV | 3.5 | Absent | 2 | 1% | NA | NA | BRAF wild type | ||
| Case 1 | 9 | M | V | 3.7 | Absent | 2 | Dominant | Present | Present | KRAS G12V; BRAF and NRAS: wild type | CK19, focal +; HBME1, focal +; CD56, focal loss; ALK, negative; Pan-Trk, negative |
| Case 2 | 38 | M | III | 1.2 | Capsular | 2 | Dominant | Present | Absent | NRAS Q61R; BRAF, HRAS, KRAS, and TERT promoter: wild type | |
| Case 3 | 21 | M | II | 4.0 | Capsular | 2 | Dominant | Present | Absent | BRAF, NRAS, HRAS, and KRAS: wild type |
NEPRAS, noninvasive encapsulated papillary RAS-like thyroid tumor; NIFTP, noninvasive follicular thyroid neoplasm with papillary-like nuclear features; WDTUMP, well-differentiated tumor of uncertain malignant potential. Nuclear score is calculated as the sum of all categories of nuclear features of papillary carcinoma: (1) nuclear size and shape (nuclear enlargement, overlapping, crowding, and elongation), (2) nuclear membrane irregularities (irregular nuclear contours, grooves, and pseudoinclusions), (3) chromatin characteristics (chromatin clearing, margination of chromatin to the membrane, glassy nuclei) [
FNA, fine-needle aspiration cytology; M, male; F, female; NA, not available. Based on the categories of the Bethesda System for Reporting Thyroid Cytopathology.

 E-submission
E-submission