Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 55(5); 2021 > Article
-
Case Study
Appendiceal actinomycosis mimicking appendiceal tumor, appendicitis or inflammatory bowel disease -
You-Na Sung
 , Jihun Kim
, Jihun Kim
-
Journal of Pathology and Translational Medicine 2021;55(5):349-354.
DOI: https://doi.org/10.4132/jptm.2020.05.17
Published online: June 26, 2020
Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- Corresponding Author: Jihun Kim, MD, PhD, Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 05505, Korea Tel: +82-2-3010-4556, Fax: +82-2-472-7898, E-mail: jihunkim@amc.seoul.kr
• Received: March 31, 2020 • Revised: May 12, 2020 • Accepted: May 17, 2020
© 2021 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Persistent intra-abdominal abscess with intestinal obstruction following seven failed drainage procedures over 3.5 years: a case report
Ayman Shemes, Salma Samra, Ahmed Mohamed, Amr A. Elgharib
BMC Surgery.2025;[Epub] CrossRef - Appendicular actinomycosis: The first reported case of an uncommon finding of a common ailment from Nepal
Sujan Bohara, Manoj Khadka, Pawan Singh Bhat, Prajwal Syangtang, Badal Karki, Bhagawan Shrestha, Shoshan Arja Acharya, Khusbhu Khetan, Jyoti Rayamajhi, Sushil Bahadur Rawal
Clinical Case Reports.2023;[Epub] CrossRef - Abdominopelvic actinomycosis: An unexpected diagnosis in an elderly female with a destructive-appearing soft tissue mass
Elise Hyser, Drashti Antala, Harvey Friedman, Jonathan Stake
IDCases.2022; 28: e01479. CrossRef - Diagnosing granulomatous disease during appendectomy
Atilla Şenaylı
Clinical Case Reports.2021;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Appendiceal actinomycosis mimicking appendiceal tumor, appendicitis or inflammatory bowel disease


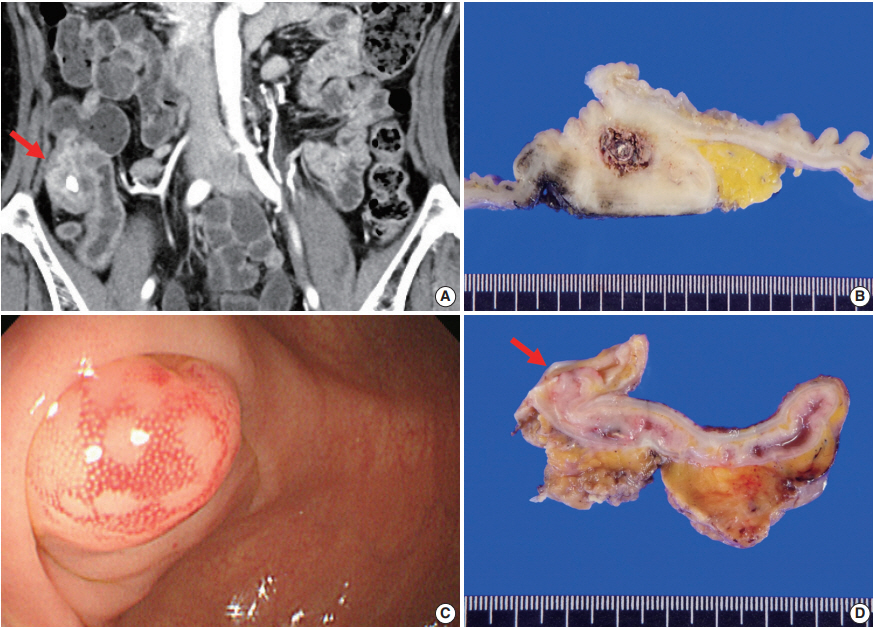
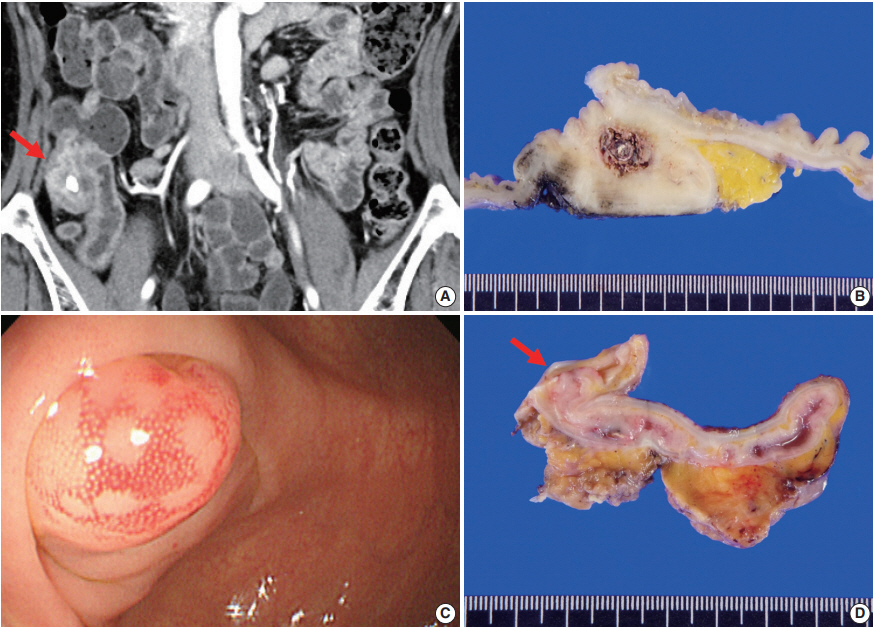
Fig. 1. Radiologic, colonoscopic, and gross features. (A) Contrast-enhanced computed tomography of case No. 1 shows appendicolith, fat infiltration with prominent wall thickening with contrast enhancement in the appendiceal base (arrow). (B) The resected appendix shows marked mural thickening, dilated appendiceal lumen and central fecalith. (C) Colonoscopic image of case No. 2 shows an approximately 10 mm-sized hyperemic mucosal bulging around the appendiceal orifice. (D) Cut surface of the resected specimen shows mucosal bulging (about 1.0cm in great dimension) on the orifice of appendix (arrow).
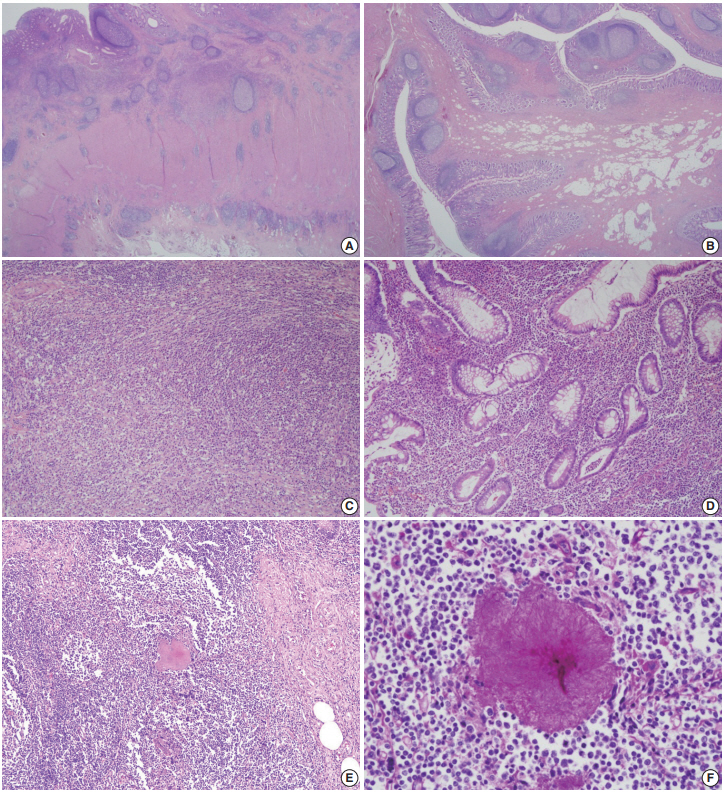
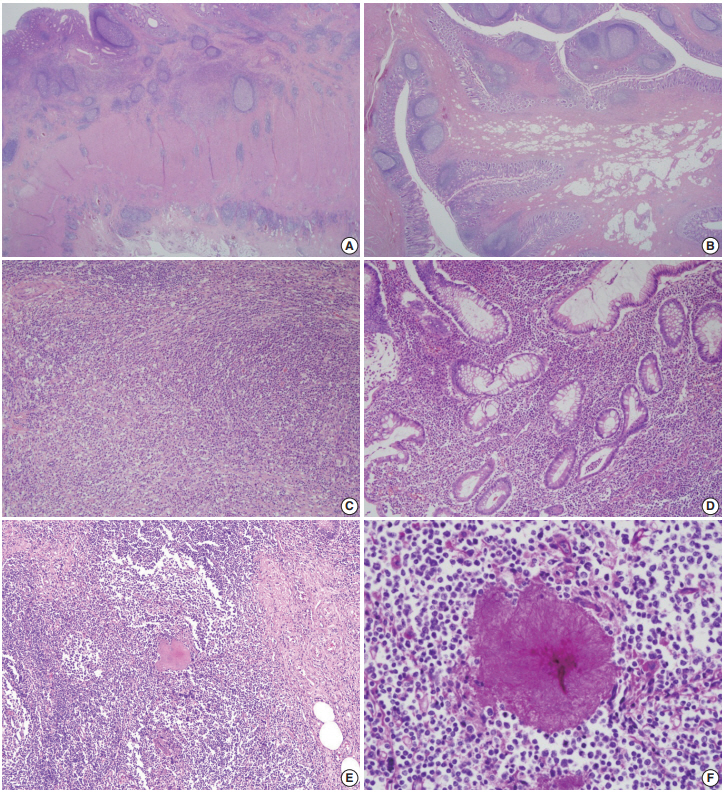
Fig. 2. Representative microscopic pictures. (A) Chronic transmural inflammation with scattered lymphoid follicles or aggregates are observed. (B) The bulging mucosa in colonoscopy is hypertrophic fibroadipose tissue that is covered by inflamed mucosa. (C) One of the fibroinflammatory foci shows marked lymphoplasmacytic infiltration with fibrosis that is reminiscent of inflammatory pseudotumor. (D) The inflamed mucosa of the appendix shows marked lymphoplasmacytosis, crypt abscess, and crypt distortion. (E) An actinomycotic colony is surrounded by mixed inflammatory cell infiltrates. (F) The filamentous nature is better demonstrated by Periodic acid–Schiff staining.
Fig. 1.
Fig. 2.
Appendiceal actinomycosis mimicking appendiceal tumor, appendicitis or inflammatory bowel disease
| Case | Study | Age (yr)/Sex | Symptom | Radiologic or colonoscopic finding | Initial diagnosis | Pathologic feature | Treatment |
|---|---|---|---|---|---|---|---|
| 1 | Atalaia-Martins et al. (2018) [8] | 66/F | Abdominal pain | Subepithelial luminal protrusion in the region of the appendiceal orifice with a whitish liquid material discharge | Uncertain | Polymorphic cell infiltrate and erosion with appendiceal fibrosis | Right hemicolectomy |
| 2 | Gomez-Torres et al. (2017) [5] | 39/M | Abdominal pain, fever, nausea, and vomiting | Non compressible enlarged cecal appendix (58 mm) with peri-appendiceal edema | Appendicitis | Chronic fistulized appendicitis with transmural lymphoid infiltration | Appendectomy |
| 3 | Liu et al. (2016) [7] | 53/M | Abdominal pain, fever | Distended appendix (9 mm) with surrounding mesenteric stranding | Appendicitis | Lymphoid hyperplasia and chronic inflammatory cells in muscularis propria and serosa | Appendectomy with IV/oral antibiotics (6 months) |
| 4 | Liu et al. (2016) [7] | 54/F | Abdominal pain, fever | Markedly thickened appendix (18 mm) with periappendiceal fat stranding | Appendicitis | Suppurative granulomatous inflammation | Preoperative antibiotics and drainage with elective appendectomy |
| 5 | Ng et al. (2014) [12] | 19/F | Abdominal pain, nausea, and vomiting | Markedly swollen appendix (2.3 cm) with a calcified appendicolith | Uncertain | Extensive chronic inflammation and eosinophilic infiltration within the wall of appendix | Ileocecectomy |
| 6 | Karakus et al. (2014) [13] | 14/M | Abdominal pain and vomiting | Increased (10 mm) thickness of the appendix with nonperistaltic ileocecal region on ultrasonography | Appendicitis | Vermiform appendix with neutrophilic infiltration | Appendectomy |
| 7 | Lee et al. (2010) [1] | 50/F | Incidental finding (routine screening) | Well defined mass (2 cm) at the origin of appendix | Appendiceal neoplasm of mucosal origin | Localized abscess formation of the appendiceal wall | Appendectomy |
| 8 | Nissotakis et al. (2008) [9] | 31/M | Abdominal pain | No sign of appendicitis on X-ray and ultrasonography | Appendicitis | Transmural inflammatory cell infiltrate with lymphoid hyperplasia and fibrosis | Appendectomy with oral antibiotics (6 months) |
| 9 | Karagulle et al. (2008) [10] | 51/F | Abdominal pain, fever and vomiting | 3 × 2-cm-sized enhancing mass near cecum | Appendicitis | Chronic active inflammation around sulfur granules | Appendectomy with IV/oral antibiotics (3 months) |
| 10 | Koren et al. (2002) [11] | 83/F | Abdominal pain | Lobular mass (5 m) attached to the cecum | Uncertain | Dense inflammatory cell infiltration within muscularis and fibro- purulent reaction over the serosa | Right hemicolectomy with IV/oral antibiotics (6 months) |
Table 1. Clinicopathologic features of reported cases of appendiceal actinomycosis

 E-submission
E-submission