Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 55(4); 2021 > Article
-
Review
Standardization of the pathologic diagnosis of appendiceal mucinous neoplasms -
Dong-Wook Kang1
 , Baek-hui Kim2
, Baek-hui Kim2 , Joon Mee Kim,3
, Joon Mee Kim,3 , Jihun Kim4
, Jihun Kim4 , Hee Jin Chang5
, Hee Jin Chang5 , Mee Soo Chang6
, Mee Soo Chang6 , Jin-Hee Sohn7
, Jin-Hee Sohn7 , Mee-Yon Cho8
, Mee-Yon Cho8 , So-Young Jin9
, So-Young Jin9 , Hee Kyung Chang10
, Hee Kyung Chang10 , Hye Seung Han11
, Hye Seung Han11 , Jung Yeon Kim12
, Jung Yeon Kim12 , Hee Sung Kim13
, Hee Sung Kim13 , Do Youn Park14
, Do Youn Park14 , Ha Young Park15
, Ha Young Park15 , So Jeong Lee16
, So Jeong Lee16 , Wonae Lee17
, Wonae Lee17 , Hye Seung Lee18
, Hye Seung Lee18 , Yoo Na Kang19
, Yoo Na Kang19 , Younghee Choi20
, Younghee Choi20 , The Gastrointestinal Pathology Study Group of the Korean Society of Pathologists
, The Gastrointestinal Pathology Study Group of the Korean Society of Pathologists -
Journal of Pathology and Translational Medicine 2021;55(4):247-264.
DOI: https://doi.org/10.4132/jptm.2021.05.28
Published online: July 8, 2021
1Department of Pathology, Chungnam National University Sejong Hospital, Chungnam National University College of Medicine, Daejeon, Korea
2Department of Pathology, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
3Department of Pathology, Inha University School of Medicine, Incheon, Korea
4Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
5Department of Pathology, Research Institute and Hospital, National Cancer Center, Goyang, Korea
6Department of Pathology, Seoul National University Boramae Hospital, Seoul National University College of Medicine, Seoul, Korea
7Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
8Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea
9Department of Pathology, Soonchunhyang University Seoul Hospital, Seoul, Korea
10Department of Pathology, Kosin University Gospel Hospital, Kosin University College of Medicine, Busan, Korea
11Department of Pathology, Konkuk University School of Medicine, Seoul, Korea
12Department of Pathology, Inje University Sanggye Paik Hospital, Seoul, Korea
13Department of Pathology, Chung-Ang University School of Medicine, Seoul, Korea
14Department of Pathology, St. Maria Pathology, Busan, Korea
15Department of Pathology, Busan Paik Hospital, Inje University College of Medicine, Busan, Korea
16Department of Pathology, Pusan National University Hospital and Pusan National University School of Medicine, Busan, Korea
17Department of Pathology, Dankook University College of Medicine, Cheonan, Korea
18Department of Pathology, Seoul National University College of Medicine, Seoul, Korea
19Department of Forensic Medicine, Kyungpook National University School of Medicine, Daegu, Korea
20Department of Pathology, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
- Corresponding Author: Joon Mee Kim, MD, PhD, Department of Pathology, Inha University School of Medicine, 27 Inhang-ro, Jung-gu, Incheon 22332, Korea Tel: +82-32-890-3987, Fax: +82-32-890-3464, E-mail: jmkpath@inha.ac.kr
© 2021 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- Abstract
- APPENDICEAL MUCINOUS NEOPLASMS
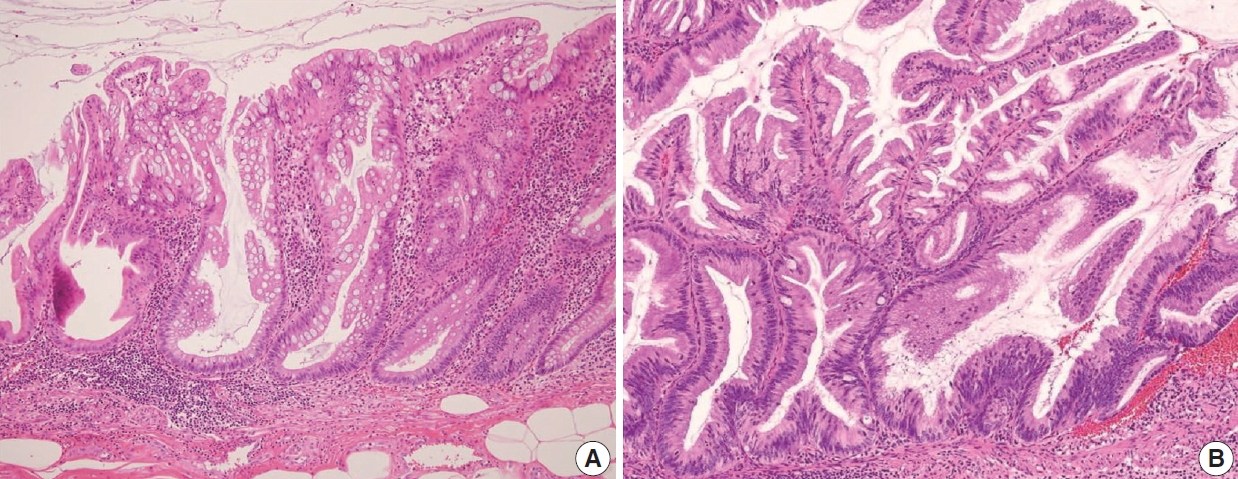
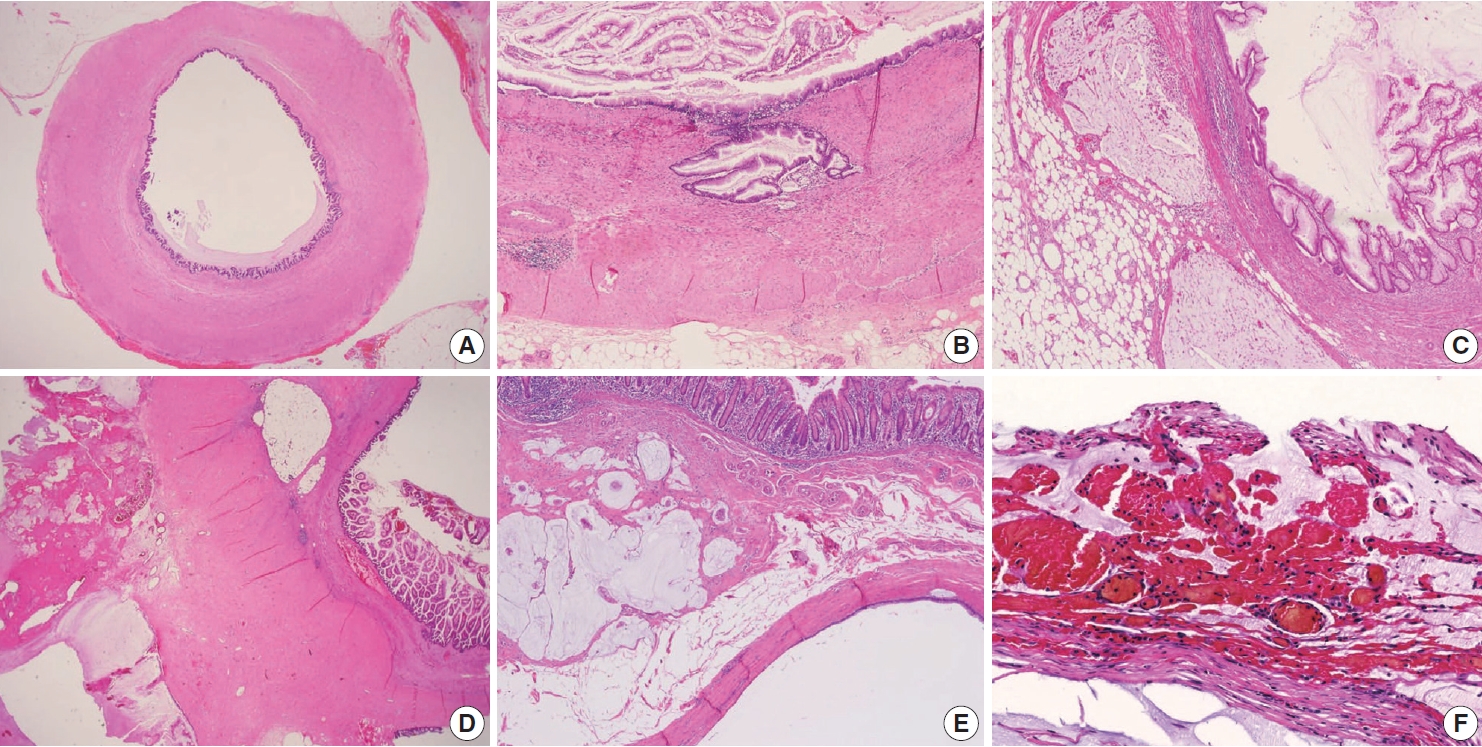
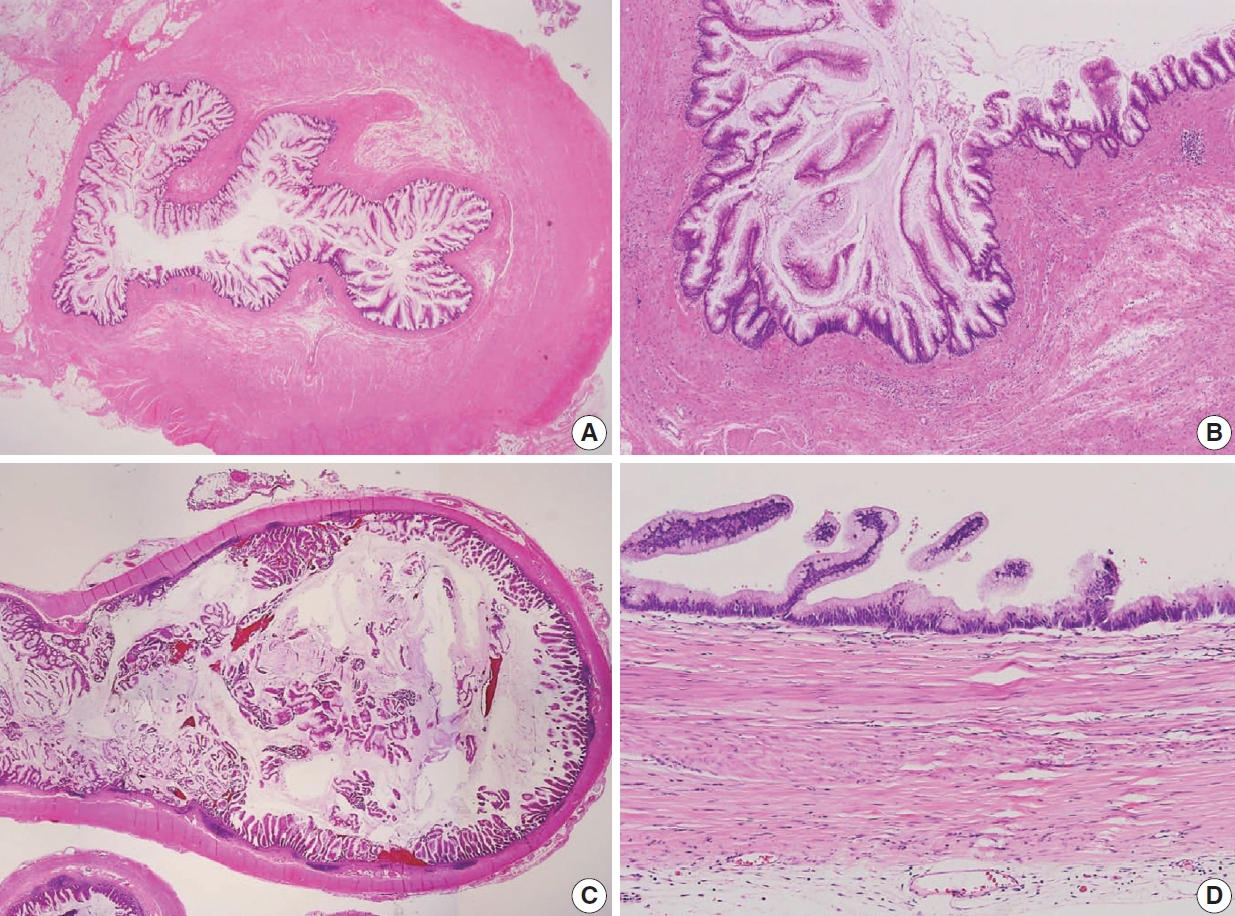
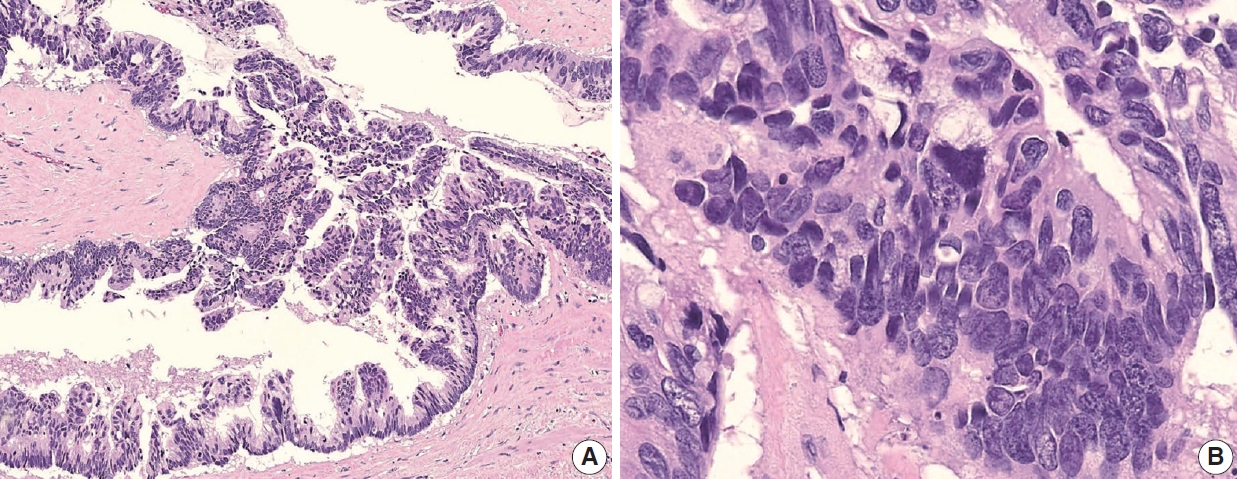
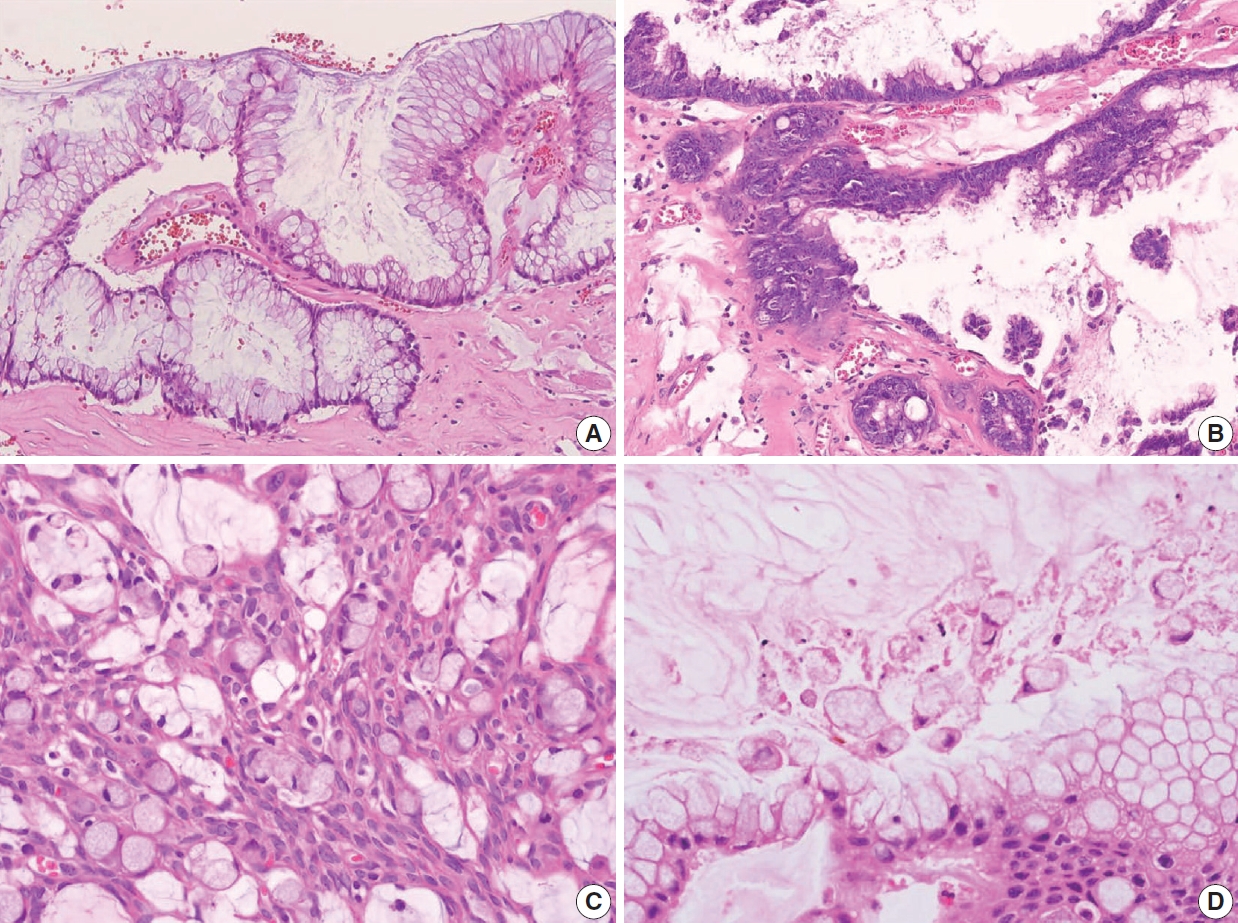
- LOW-GRADE APPENDICEAL MUCINOUS NEOPLASM
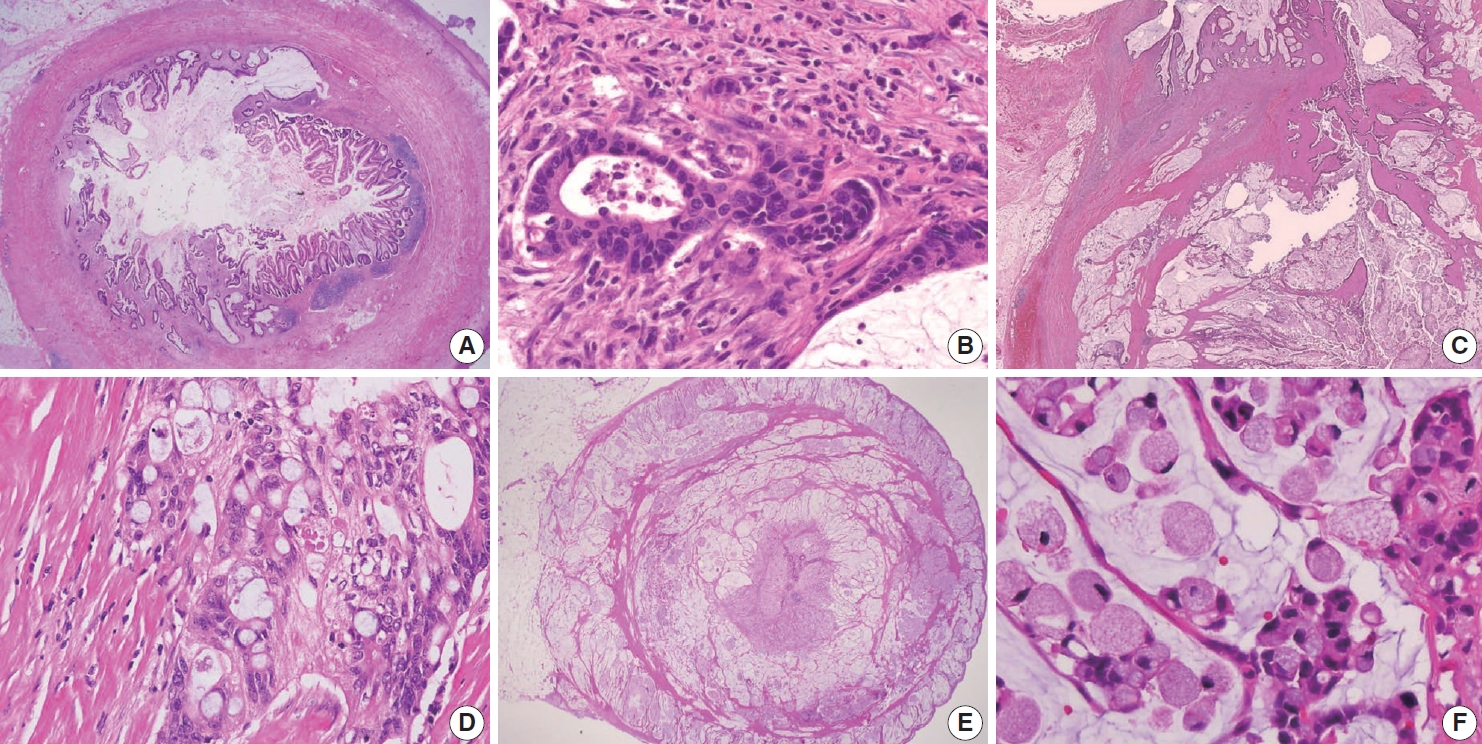
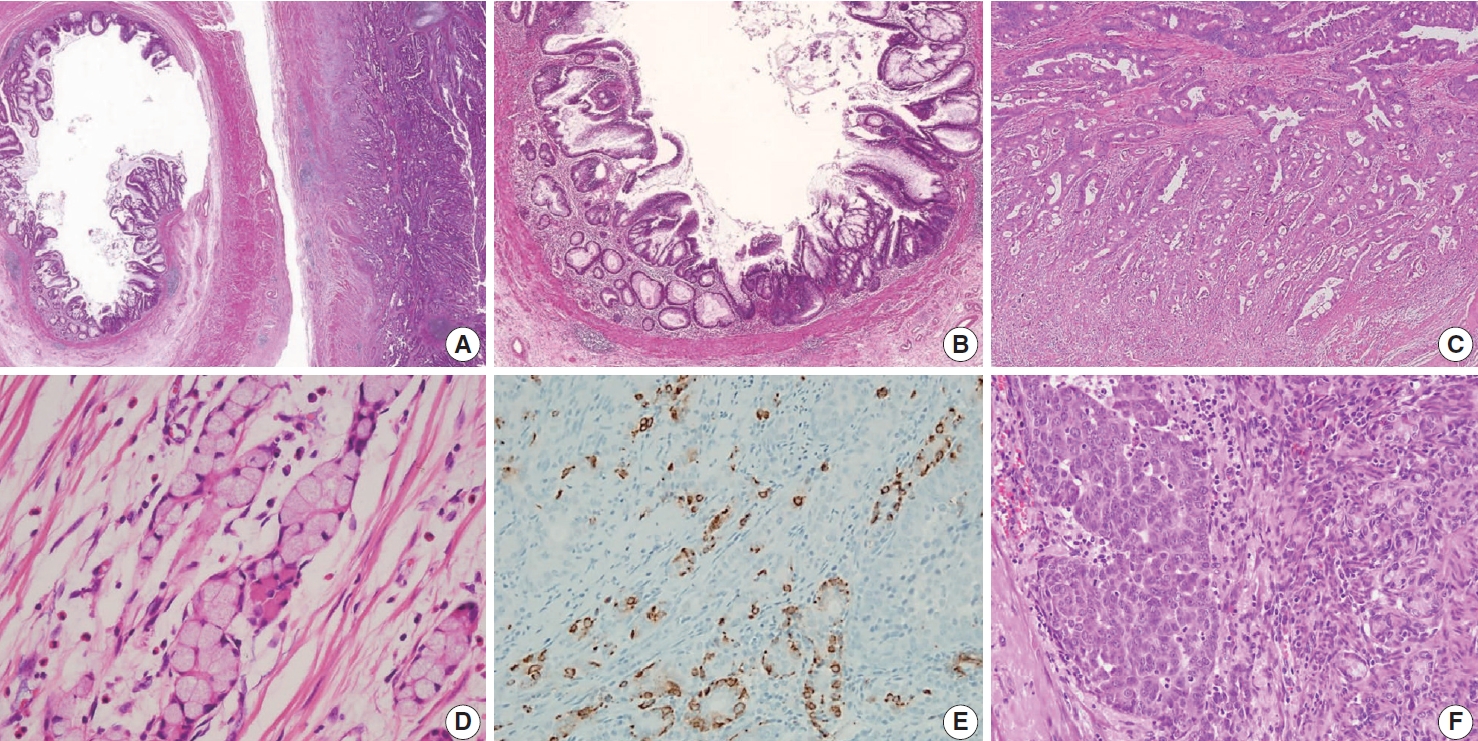
- HIGH-GRADE APPENDICEAL MUCINOUS NEOPLASM
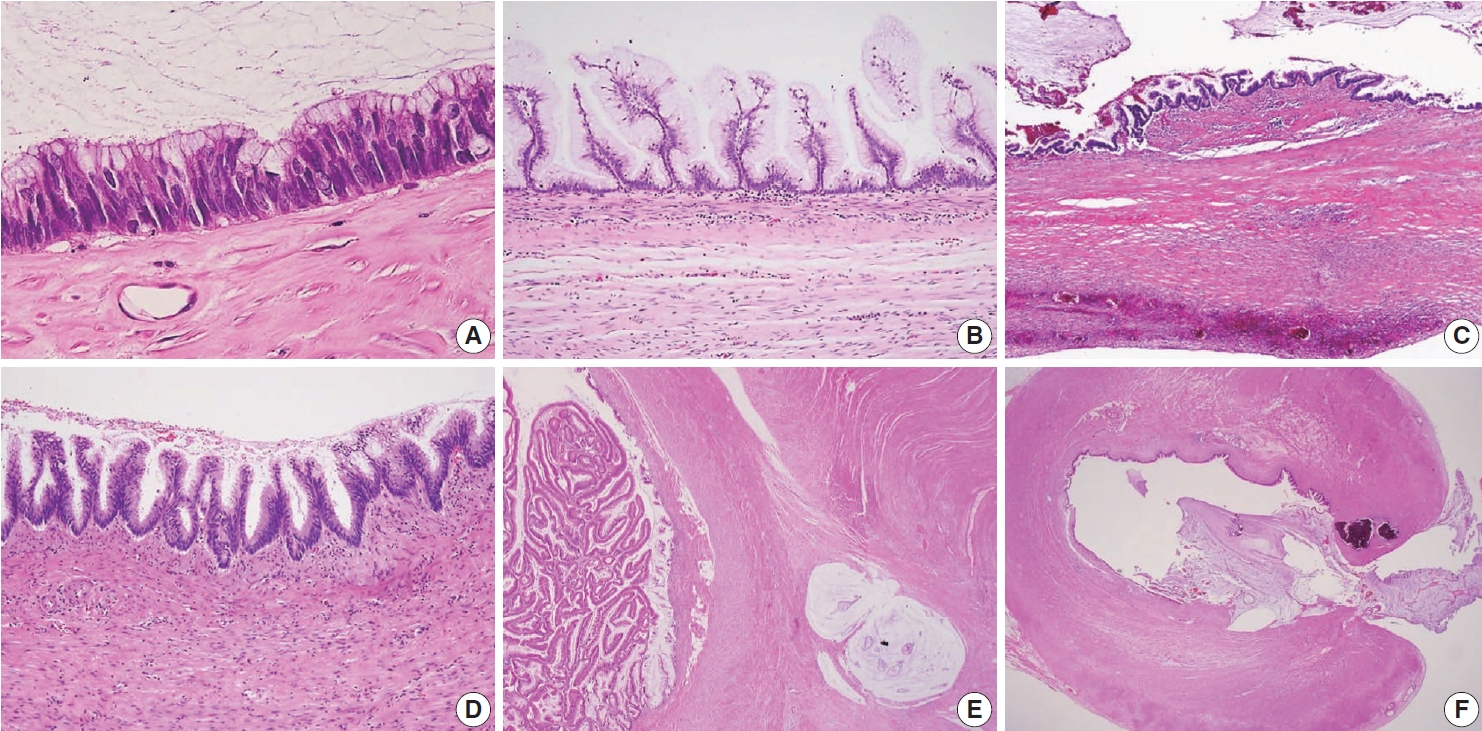
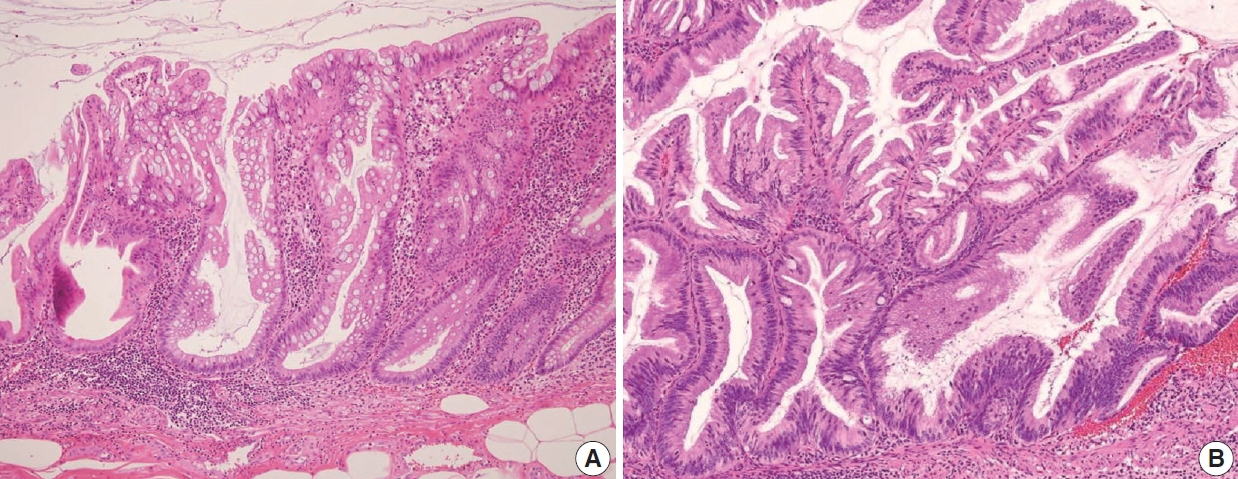
- SERRATED LESIONS
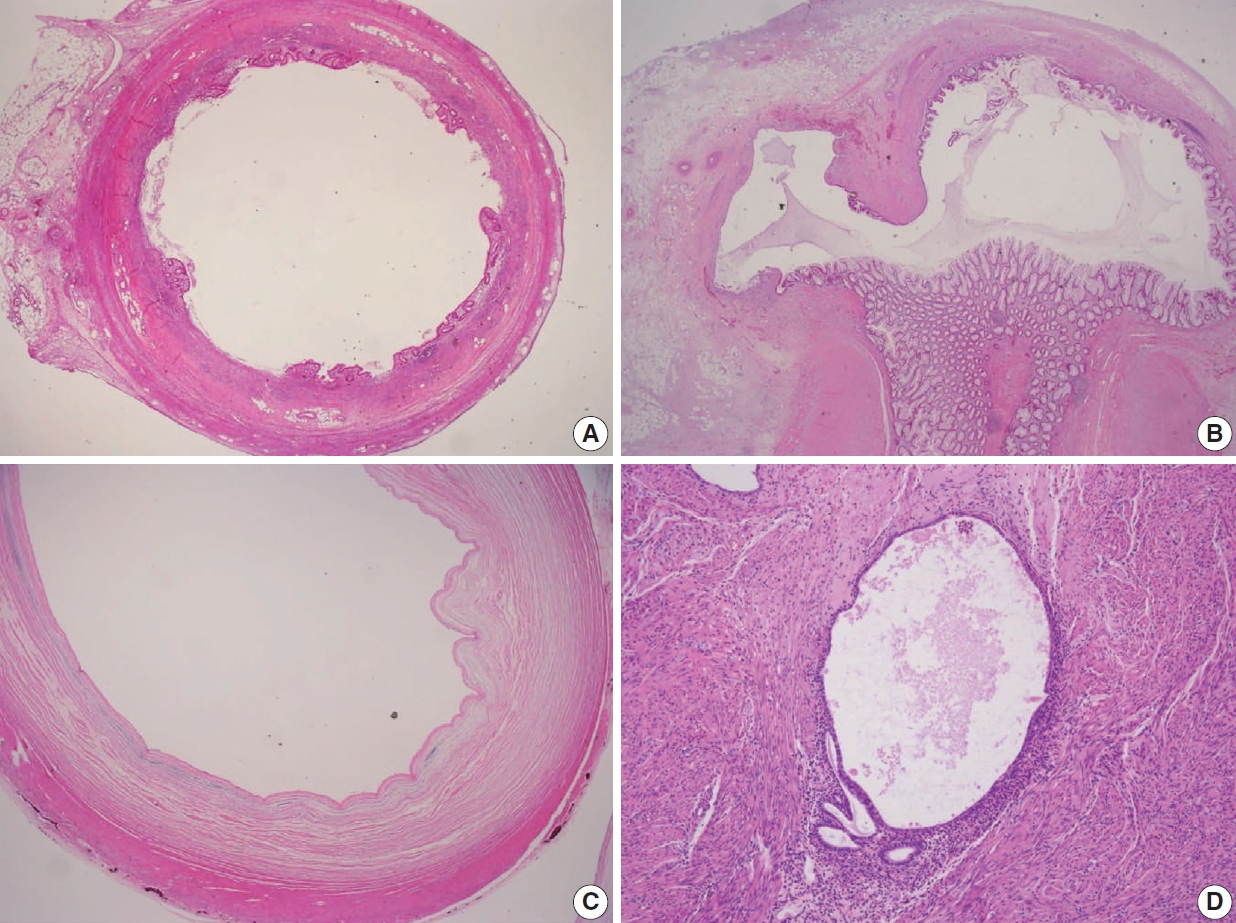
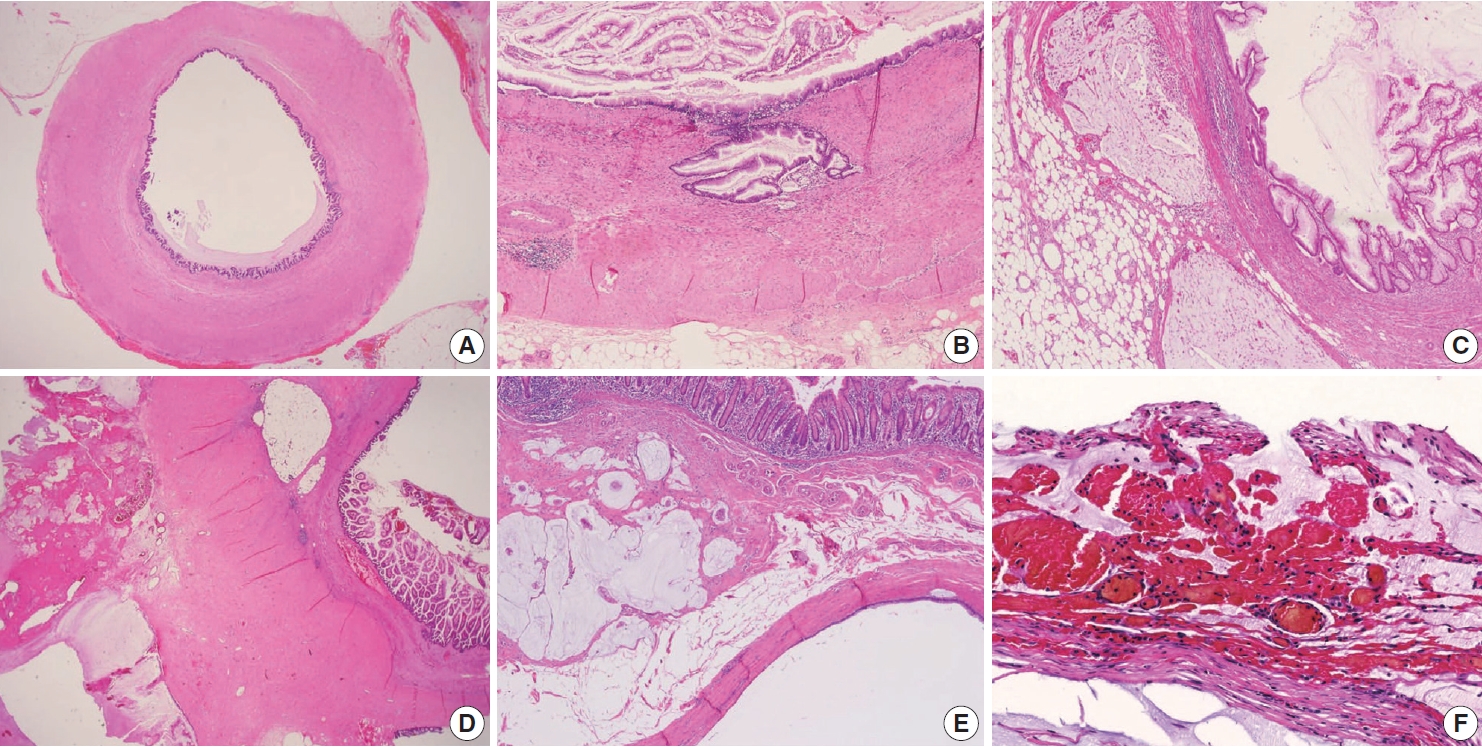
- STAGING OF APPENDICEAL MUCINOUS NEOPLASMS
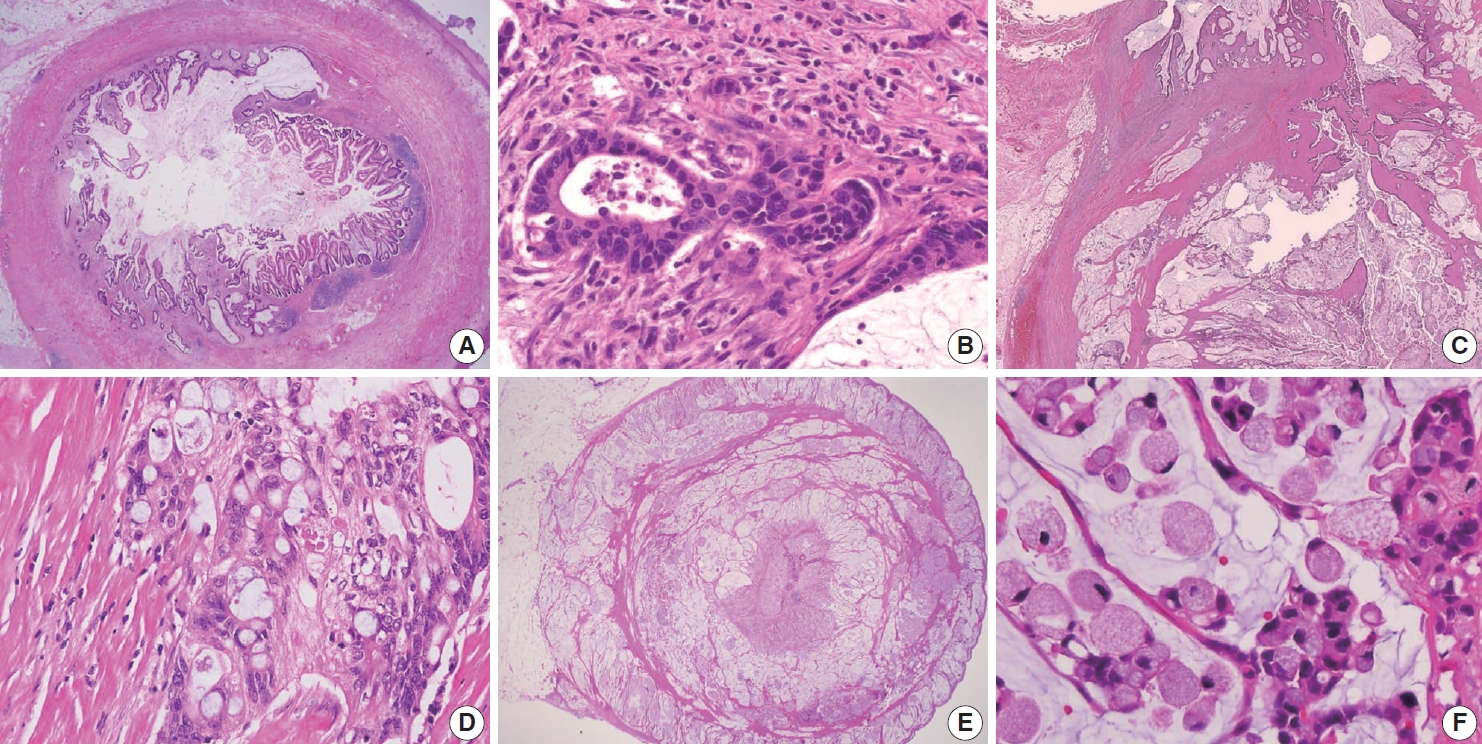
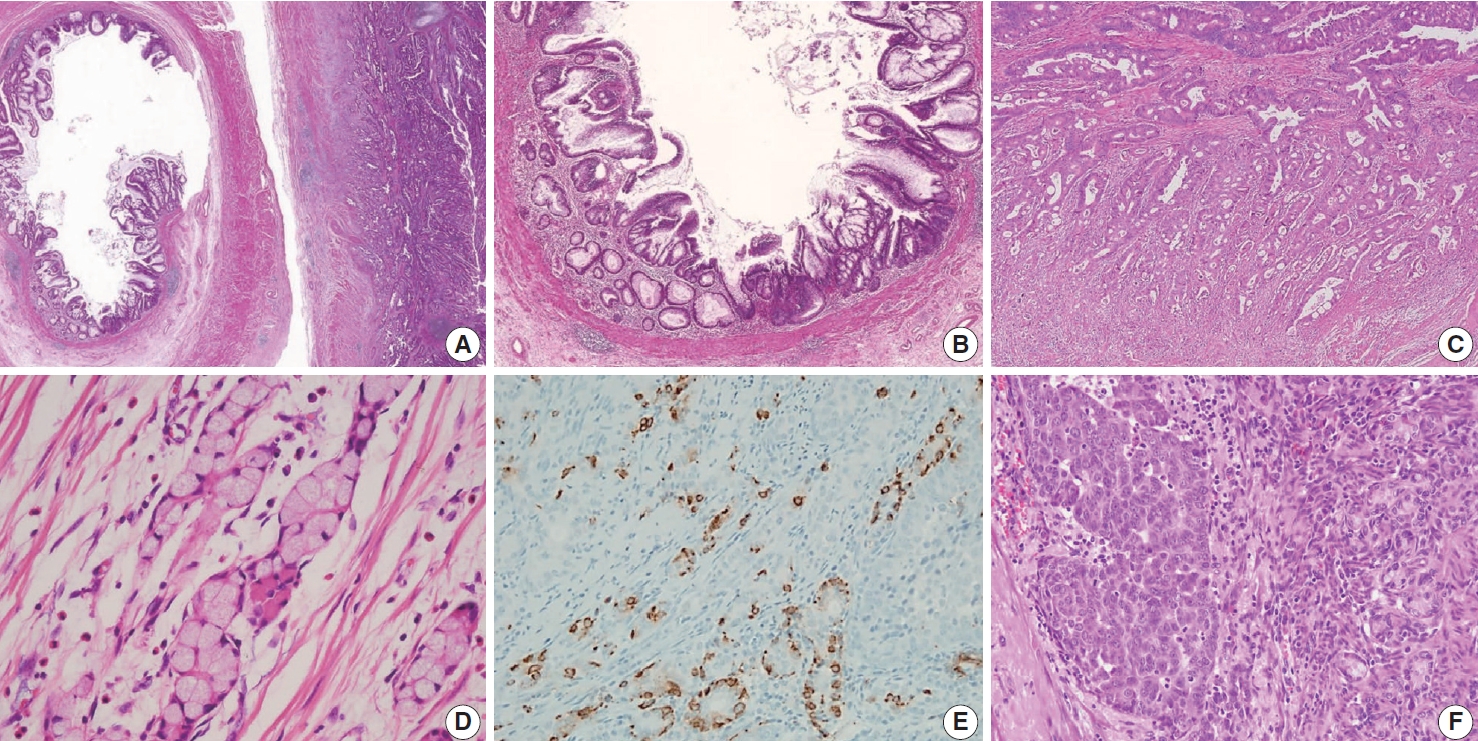
- APPENDICEAL MUCINOUS ADENOCARCINOMA
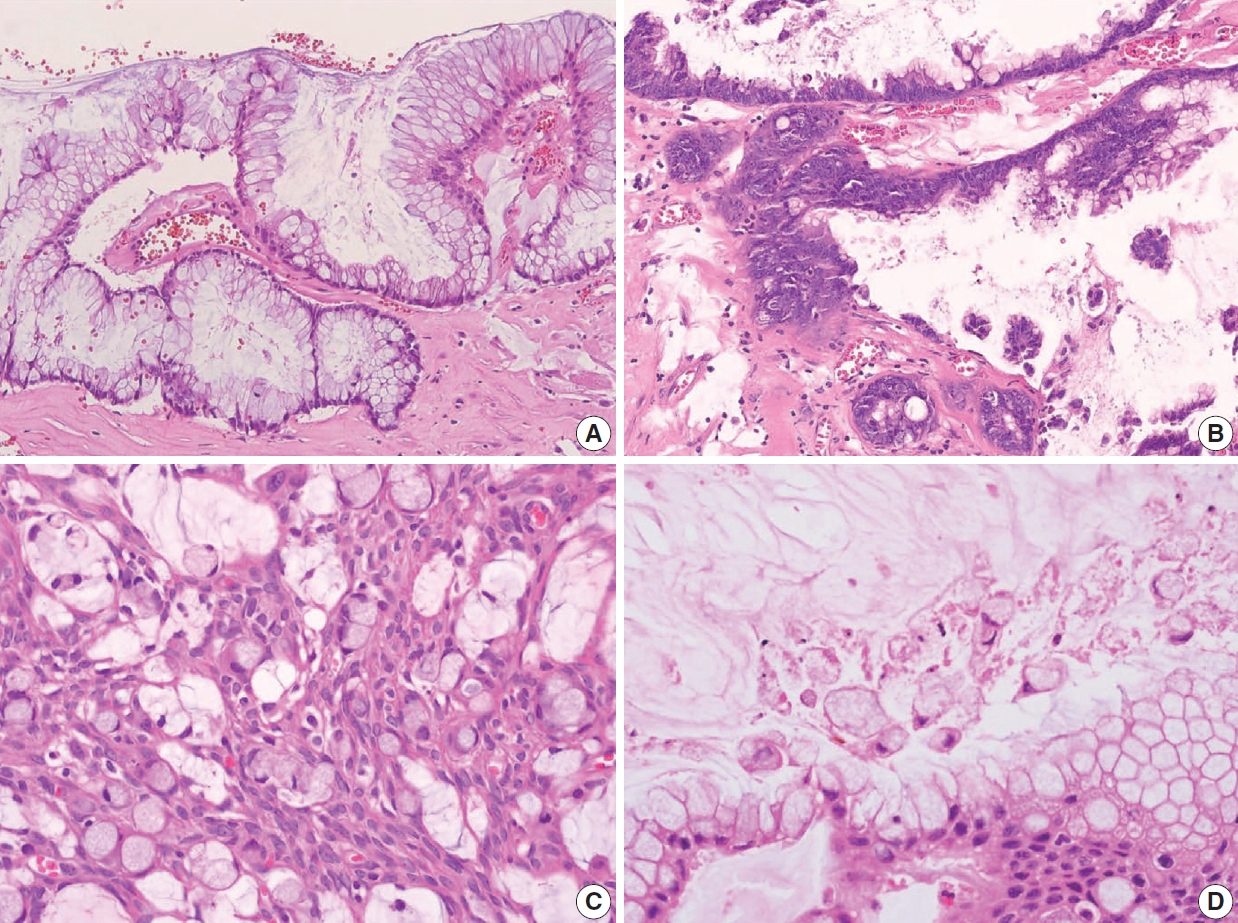
- DISSEMINATED PERITONEAL MUCINOUS DISEASE
- OTHER APPENDICEAL EPITHELIAL TUMORS
- CONCLUSION
- Supplementary Materials
- NOTES
- Acknowledgments
- REFERENCES
Figure & Data
References
Citations

- Intrasplenic metastasis of appendiceal low-grade mucinous neoplasm – A case report and review of the literature
P. Meister, J. Rawitzer, M. Reschke, H.A. Baba, U. Neumann, M. Kaths
Current Problems in Cancer: Case Reports.2025; 18: 100364. CrossRef - Complete laparoscopic resection of giant appendiceal mucinous neoplasm, case report, and literature review
Shatha Awad Althobaiti, Rayan Z. Makeen, Abrar J. Filfilan, Ahmed Abdulaziz Hawsawi
Saudi Surgical Journal.2025; 13(1): 35. CrossRef - Survival Outcomes and Prognostic Factors in Metastatic Unresectable Appendiceal Adenocarcinoma Treated with Palliative Systemic Chemotherapy: A 10-Year Retrospective Analysis from Australia
Jirapat Wonglhow, Hui-Li Wong, Michael Michael, Alexander Heriot, Glen Guerra, Catherine Mitchell, Jeanne Tie
Cancers.2025; 17(20): 3297. CrossRef - Lower Gastrointestinal Bleeding Secondary to Appendiceal Mucinous Neoplasm: A Report of Two Cases and a Review of the Literature
Jesús Omar Soto Llanes, Samanta Kin Dosal Limón, Ana Jimena Iberri Jaime, Mario Zambrano Lara, Billy Jiménez Bobadilla
Cureus.2024;[Epub] CrossRef - Predicting Survival in Mucinous Adenocarcinoma of the Appendix: Demographics, Disease Presentation, and Treatment Methodology
Paul H. McClelland, Stephanie N. Gregory, Shirley K. Nah, Jonathan M. Hernandez, Jeremy L. Davis, Andrew M. Blakely
Annals of Surgical Oncology.2024; 31(9): 6237. CrossRef - Histoséminaire biopsies péritonéales tumorales. Néoplasies mucineuses appendiculaires
Peggy Dartigues
Annales de Pathologie.2024; 44(4): 274. CrossRef - Histoséminaire biopsies péritonéales tumorales. Cas no 2
Peggy Dartigues
Annales de Pathologie.2024; 44(4): 245. CrossRef - A Case of Low-Grade Appendiceal Mucinous Neoplasm: The Role of Preoperative Imaging and Surgical Technique in Achieving Favorable Outcomes
Daniel A Meza-Martinez, Yeudiel Suro Santos, Samantha J Andrade-Ordoñez, Julio A Palomino-Payan, Brando J Fematt-Rodriguez
Cureus.2024;[Epub] CrossRef - Incidental Appendiceal Mucinous Neoplasm Found During Appendectomy in a 15-Year-Old Patient: A Case Report
Fernando Aguilar-Ruiz, Kevin Joseph Fuentes-Calvo, Sara Fernanda Arechavala-Lopez, Irving Fuentes-Calvo, Luis F Arias-Ruiz
Cureus.2024;[Epub] CrossRef - Uncovering the Hidden Threat: Ileocolic Intussusception in an Adult With Appendicular Tumor
Mrunal Panchal, Shishir Kumar, Khushboo Jha, Kaushik Saha, Abhijit Kundu
Cureus.2024;[Epub] CrossRef - Low-Grade Appendiceal Mucinous Neoplasm vs. Appendiceal Diverticulum: Distinction with Histomorphologic Features
Cevriye Cansiz Ersöz, Siyar Ersöz, Berna Savas, Arzu Ensari
Gastrointestinal Disorders.2024; 6(4): 905. CrossRef - Appendiceal perforation secondary to endometriosis with intestinal metaplasia: A case report
Minghua Wang, Jing Liu, Boxin Hu, Simin Wang, Ping Xie, Ping Li
Experimental and Therapeutic Medicine.2023;[Epub] CrossRef - Primary and secondary tumors of the peritoneum: key imaging features and differential diagnosis with surgical and pathological correlation
Javier Miguez González, Francesc Calaf Forn, Laura Pelegrí Martínez, Pilar Lozano Arranz, Rafael Oliveira Caiafa, Jordi Català Forteza, Lina Maria Palacio Arteaga, Ferrán Losa Gaspà, Isabel Ramos Bernadó, Pedro Barrios Sánchez, Juan Ramón Ayuso Colella
Insights into Imaging.2023;[Epub] CrossRef - Muzinöse Tumoren des Peritoneums
Anne Kristin Fischer, Andrea Tannapfel, Alexander Quaas
Die Chirurgie.2023; 94(10): 823. CrossRef - Landscape of Genetic Mutations in Appendiceal Cancers
Marian Constantin, Cristina Mătanie, Livia Petrescu, Alexandra Bolocan, Octavian Andronic, Coralia Bleotu, Mihaela Magdalena Mitache, Sorin Tudorache, Corneliu Ovidiu Vrancianu
Cancers.2023; 15(14): 3591. CrossRef - Delivery of an Incidental Appendiceal Mucinous Neoplasm
Madison Bowles, Jessica Y Ng, Hajir Nabi
Cureus.2022;[Epub] CrossRef - Unearthing novel fusions as therapeutic targets in solid tumors using targeted RNA sequencing
Sungbin An, Hyun Hee Koh, Eun Sol Chang, Juyoung Choi, Ji-Young Song, Mi-Sook Lee, Yoon-La Choi
Frontiers in Oncology.2022;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure









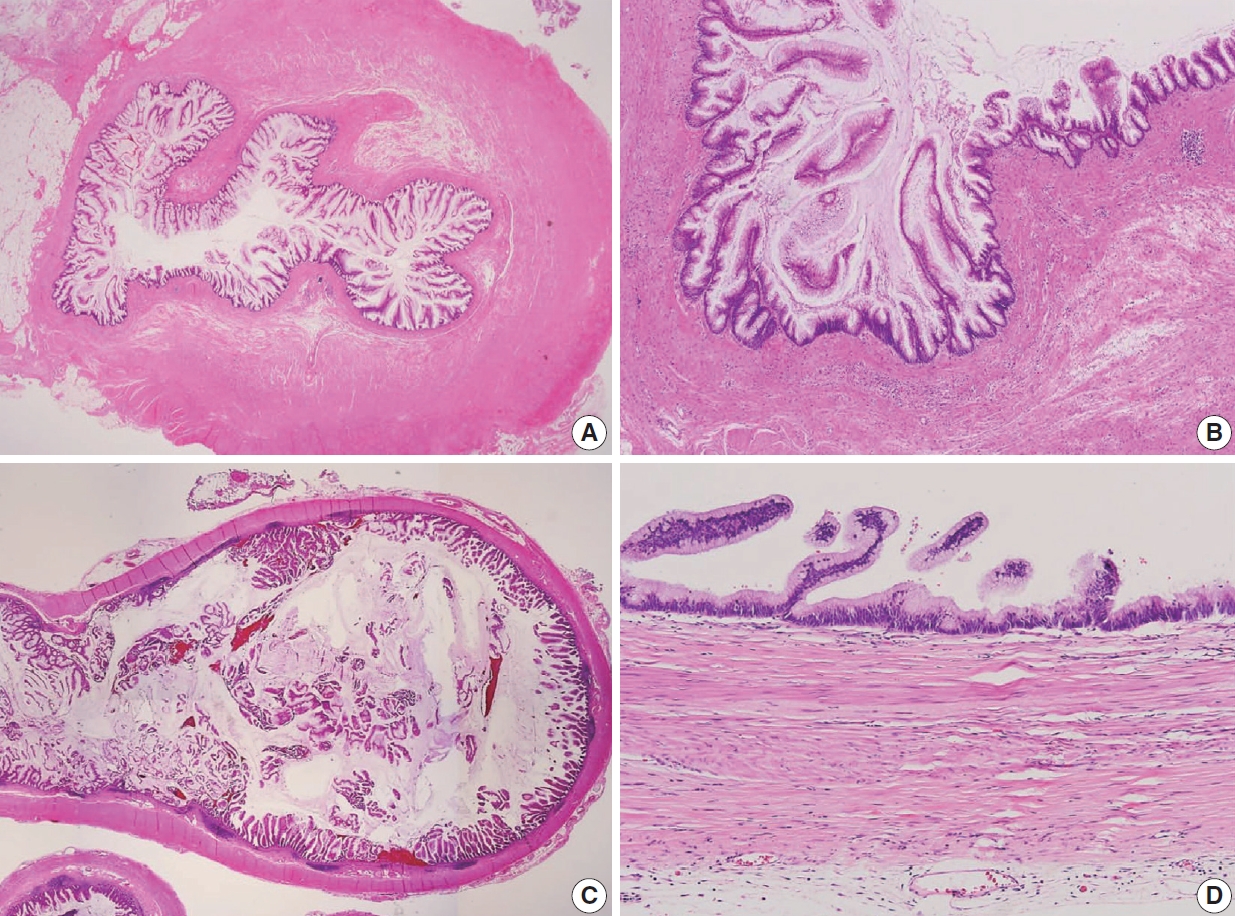
Fig. 1.
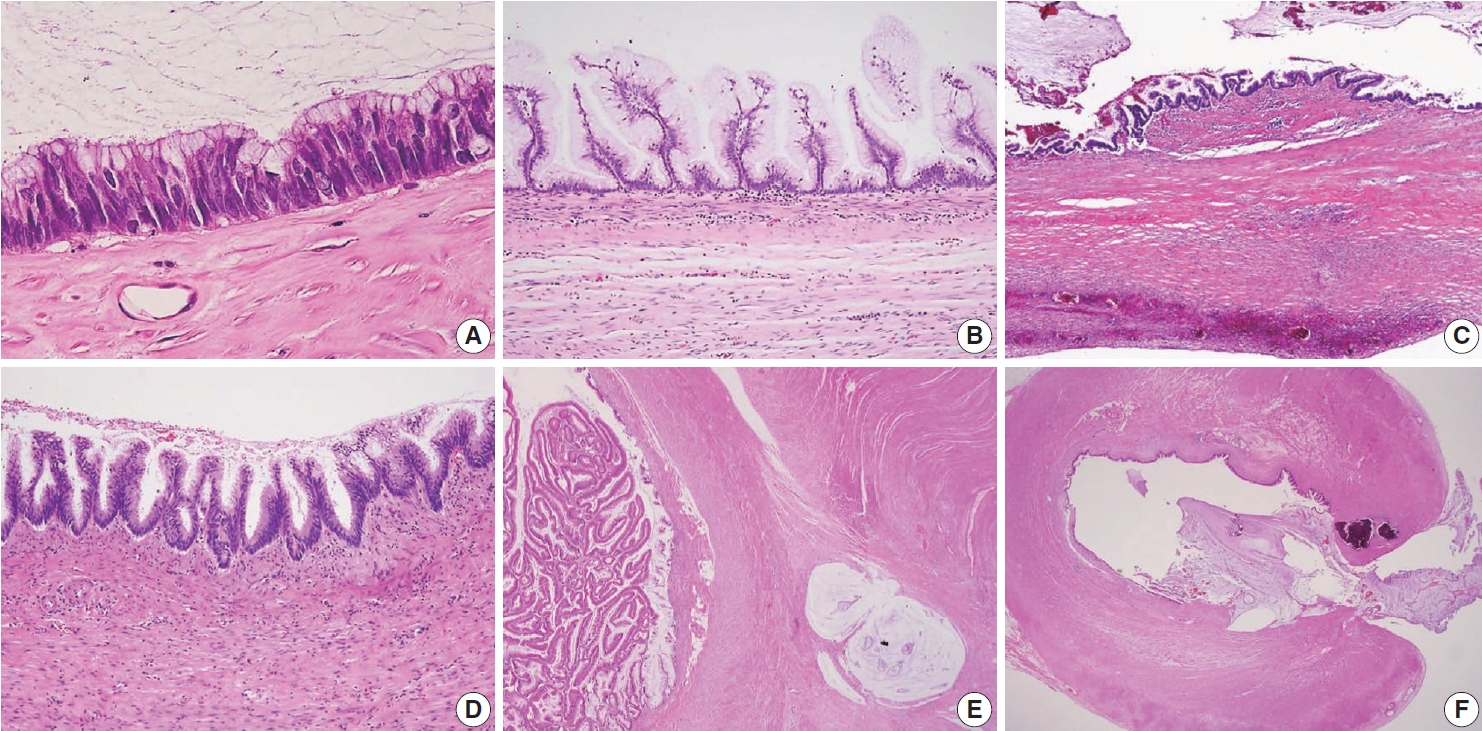
Fig. 2.
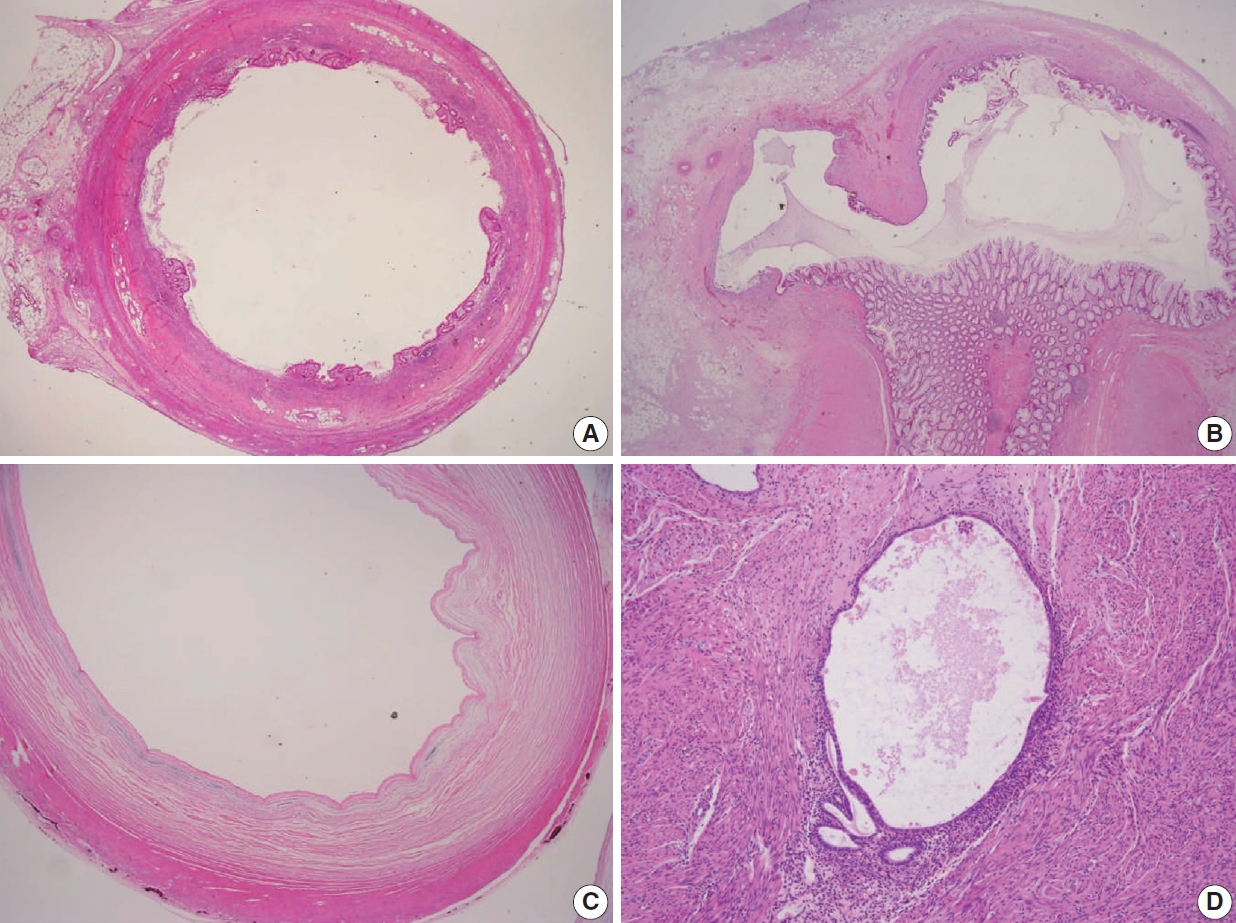
Fig. 3.
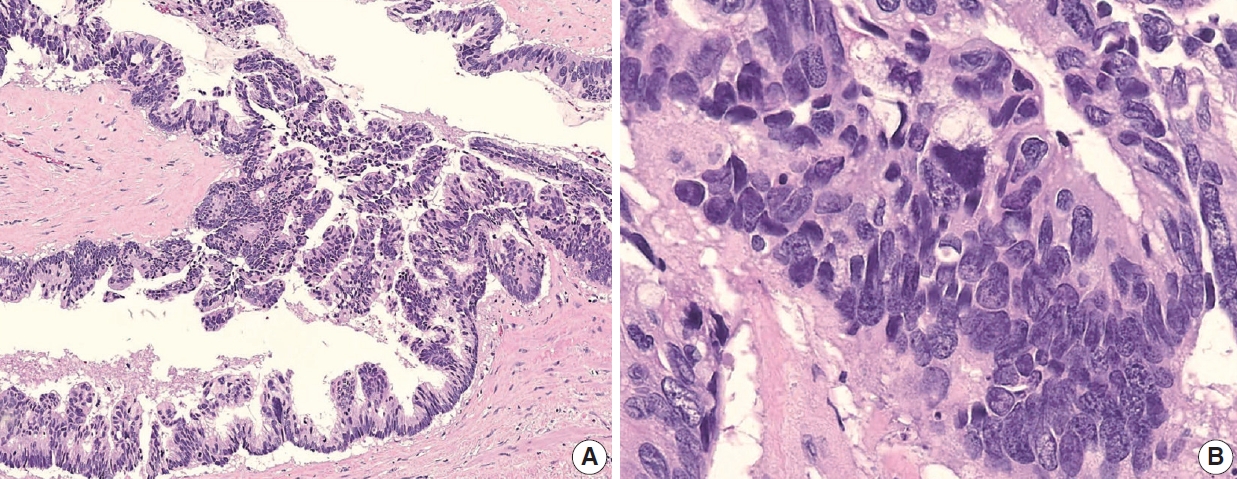
Fig. 4.
Fig. 5.
Fig. 6.
Fig. 7.
Fig. 8.
Fig. 9.
| ICD-O3 | Epithelial tumors | |
|---|---|---|
| - | Hyperplastic polyp | |
| - | Sessile serrated lesion without dysplasia | |
| 8213/0 | Serrated dysplasia, low grade | |
| 8213/2 | Serrated dysplasia, high grade | |
| 8480/1 | Low-grade appendiceal mucinous neoplasm | |
| 8480/2 | High-grade appendiceal mucinous neoplasm | |
| 8140/3 | Adenocarcinoma, NOS | |
| 8480/3 | Mucinous adenocarcinoma (> 50% mucin) | |
| 8490/3 | Signet-ring cell carcinoma (> 50% signet-ring cells) | |
| 8020/3 | Carcinoma, undifferentiated, NOS | |
| 8243/3 | Goblet cell adenocarcinoma | |
| 8240/3 | Neuroendocrine tumor, NOS | |
| 8240/3 | Neuroendocrine tumor, grade 1 | |
| 8249/3 | Neuroendocrine tumor, grade 2 | |
| 8249/3 | Neuroendocrine tumor, grade 3 | |
| 8152/3 | L-cell tumor | |
| 8152/3 | Glucagon-like peptide producing tumor | |
| 8152/3 | PP/PYY-producing tumor | |
| 8241/3 | Enterochromaffin-cell carcinoid | |
| 8241/3 | Serotonin-producing carcinoid | |
| 8246/3 | Neuroendocrine carcinoma | |
| 8013/3 | Large cell neuroendocrine carcinoma | |
| 8041/3 | Small cell neuroendocrine carcinoma | |
| 8154/3 | Mixed neuroendocrine-non-neuroendocrine carcinoma (MiNEN) | |
| Classification | Grading |
ICD-O3 | KCD-8 | Diagnostic criteria and microscopic features [3,12] | |
|---|---|---|---|---|---|
| Low-grade appendiceal mucinous neoplasm | Low/G1 | 8480/1 | D37.3 | Mucinous neoplasm with low-grade cytology and any of the following (by PSOGI criteria) | |
| Loss of muscularis mucosae | |||||
| Fibrosis of submucosa | |||||
| “Pushing invasion” (expansile or diverticulum-like growth) | |||||
| Dissection of acellular mucin in wall | |||||
| Undulating or flattened epithelial growth | |||||
| Rupture of appendix | |||||
| Mucin and/or cells outside appendix | |||||
| High-grade appendiceal mucinous neoplasm | High/G2 | 8480/2 | D01.7 | Mucinous neoplasm with the architectural features of LAMN and no infiltrative invasion, but with high-grade cytologic atypia | |
| Mucinous adenocarcinoma | High/G2 | 8480/3 | C18.1 | Malignant glandular neoplasm, comprising of > 50% extracellular mucin, characterized by infiltrative invasion. The pattern of infiltrative invasion as follows: Infiltrative glands, or single infiltrative tumor cells associated with extracellular mucin and desmoplastic stroma | |
| Small dissecting mucin pools containing floating nests, glands, or single neoplastic cells | |||||
| Mucinous adenocarcinoma with signet-ring cells | High/G3 | 8480/3 | C18.1 | Mucinous adenocarcinoma, comprising of ≤ 50% signet-ring cells | |
| Signet-ring cell carcinoma | High/G3 | 8490/3 | C18.1 | Adenocarcinoma, comprising up to > 50% signet-ring cells | |
| pT stage | Definition and lesions | Prognostic significances |
|---|---|---|
| pTis(LAMN) | LAMN confined to the appendiceal wall after histologic examination of the entire appendix. | pTis(LAMN) has essentially no risk of recurrence. pTis(LAMN) designation requires correlation with the intraoperative findings and an evaluation by the operator. |
| Acellular mucin or mucinous epithelium may interrupt the muscle propria. | ||
| pT3(LAMN) | LAMN with acellular mucin or mucinous epithelium extending into the subserosa or mesoappendix but no involvement of the serosa after histologic examination of the entire appendix. | Unknown risk of peritoneal recurrence. |
| Long-term follow-up for 10 yr is suggested until additional data on recurrence risk becomes available. | ||
| pT4(LAMN) | LAMN invades the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of the appendix or mesoappendix (pT4a), and/or directly invades adjacent organs or structures (pT4b). | Low risk (acellular mucin) and high risk (mucinous epithelium) of peritoneal recurrence. |
| Long-term follow-up for 10 yr with periodic imaging is required. | ||
| Additional surgery or CRS-HIPEC is uncertain but is used in some centers. |
| Lesion | Grade | Behavior codes |
Terminology |
Criteria | Treatment | ||
|---|---|---|---|---|---|---|---|
| ICD-O3 | KCD-8 | PSOGI/Carr [12] | AJCC/Misdraji [10] | ||||
| Mucin without tumor cells | - | 8480/6 | C78.6 | Acellular mucin | Acellular mucin | Mucin within the peritoneal cavity without neoplastic epithelial cells | CRS-HIPEC |
| Mucinous tumor with low-grade histologic features | G1 | 8480/6 | C78.6 | Low-grade mucinous carcinoma peritonei | LAMN with peritoneal involvement | Scanty (≤ 20% cellularity) | CRS-HIPEC |
| Strips, gland-like or small clusters | |||||||
| Low-grade cytological atypia | |||||||
| Not more than occasional mitosis | |||||||
| Pushing invasion | |||||||
| Mucinous tumor with high-grade histologic features | G2 | 8480/6 | C78.6 | High-grade mucinous carcinoma peritonei | Mucinous adenocarcinoma, moderately differentiated | More cellular (> 20% cellularity) | Systemic chemotherapy ± CRS-HIPEC |
| Cribriform growth | |||||||
| Mixed but mostly high-grade cytological atypia | |||||||
| Numerous mitoses | |||||||
| Destructive infiltrative invasion | |||||||
| Mucinous tumor with signet-ring cells | G3 | 8480/6 | C78.6 | High-grade mucinous carcinoma peritonei with signet-ring cells | Mucinous adenocarcinoma, poorly differentiated | Any lesion with signet-ring cells (degenerating cells within mucin that mimic signet-ring cells should be discounted) | Systemic chemotherapy ± CRS-HIPEC |
| Specimen type | ||
|---|---|---|
| □ Appendectomy | ||
| □ Appendectomy and right colectomy | ||
| □ Other: (specify: ) | ||
| Tumor size | ||
| × × cm | ||
| Tumor site | ||
| □ Proximal half of appendix | ||
| □ Distal half of appendix | ||
| □ Diffusely involving appendix | ||
| □ Other: (specify: ) | ||
| Histologic types (WHO 5th Digestive System Tumors) [1] | ||
| □ Low-grade appendiceal mucinous neoplasm (LAMN) | ||
| □ High-grade appendiceal mucinous neoplasm (HAMN) | ||
| □ Mucinous adenocarcinoma | ||
| □ Non-mucinous adenocarcinoma | ||
| □ Signet-ring cell carcinoma | ||
| □ Goblet cell adenocarcinoma | ||
| □ Large cell neuroendocrine carcinoma | ||
| □ Small cell neuroendocrine carcinoma | ||
| □ Mixed neuroendocrine-non-neuroendocrine carcinoma (MiNEN) | ||
| □ Medullary carcinoma | ||
| □ Adenosquamous carcinoma | ||
| □ Undifferentiated carcinoma | ||
| □ Other histologic type not listed (specify: ) | ||
| Histologic grade | ||
| □ G1: Well differentiated | ||
| □ G2: Moderately differentiated | ||
| □ G3: Poorly differentiated | ||
| □ GX: Cannot be assessed | ||
| □ Other: (specify: ) | ||
| Disseminated peritoneal mucinous disease | ||
| □ Not identified | ||
| □ Present | ||
| □ Low-grade mucinous carcinoma peritonei/LAMN (G1) with peritoneal involvement | ||
| □ High-grade mucinous carcinoma peritonei/Mucinous adenocarcinoma, moderately differentiated (G2) | ||
| □ High-grade mucinous carcinoma peritonei with signet-ring cells / Mucinous adenocarcinoma, poorly differentiated (G3) | ||
| Resection margins including proximal and mesenteric margins | ||
| □ Cannot be assessed | ||
| □ Uninvolved by tumor | ||
| □ Distance of tumor from the closest margin: mm | ||
| □ Involved by tumor | ||
| □ Involved by invasive carcinoma (□ Proximal margin, □ Mesenteric margin) | ||
| □ Involved by appendiceal mucinous neoplasm (□ Proximal margin, □ Mesenteric margin) | ||
| □ Involved by acellular mucin (□ Proximal margin, □ Mesenteric margin) | ||
| Lympho-vascular invasion | ||
| □ Not identified □ Present □ Cannot be determined | ||
| Perineural invasion | ||
| □ Not identified □ Present □ Cannot be determined | ||
| Tumor deposits | ||
| □ Not identified □ Present □ Cannot be determined | ||
| Regional lymph nodes | ||
| □ No lymph nodes submitted or found | ||
| □ Total number of lymph nodes examined: | ||
| □ Number of lymph nodes involved with metastases: | ||
| Pathologic stage classification (pTNM, AJCC 8th edition) [13] | ||
| TNM Descriptors: □ m (multiple) □ r (recurrent) □ y (post-neoadjuvant therapy) | ||
| Primary tumor (pT) | ||
| □ pTX: Primary tumor cannot be assessed | ||
| □ pTX0: No evidence of primary tumor | ||
| □ pTis: Carcinoma in situ (high-grade dysplasia); intraepithelial carcinoma; invasion of lamina propria (intramucosal carcinoma) | ||
| □ pTis(LAMN): LAMN confined to the appendix (defined as involvement by acellular mucin or mucinous epithelium that may extend into the muscularis propria) | ||
| □ pT1: Tumor invades submucosa (does not apply to LAMN) | ||
| □ pT2: Tumor invades muscularis propria (does not apply to LAMN) | ||
| □ pT3: Tumor invades through the muscularis propria into the subserosa or mesoappendix | ||
| □ pT4: Tumor invades the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of the appendix or mesoappendix, and/or directly invades adjacent organs or structures | ||
| □ pT4a: Tumor invades the visceral peritoneum, including the acellular mucin or mucinous epithelium involving the serosa of appendix or serosa of mesoappendix | ||
| □ pT4b: Tumor directly invades other organs or structures | ||
| Regional lymph nodes (pN) | ||
| □ pNX: Regional lymph nodes cannot be assessed | ||
| □ pN0: No regional nodal metastasis | ||
| □ pN1: One to three regional lymph nodes are positive (tumor in lymph nodes measuring ≥ 0.2 mm), or any number of tumor deposits is present, and all identifiable lymph nodes are negative | ||
| □ pN1a: One regional lymph node is positive | ||
| □ pN1b: Two or three regional lymph nodes are positive | ||
| □ pN1c: No regional lymph node metastasis, but tumor deposits in the subserosa or mesentery | ||
| □ pN2: Metastasis in 4 or more regional nodes | ||
| Distant metastasis (pM) | ||
| □ Not applicable | ||
| □ pM1: Distant metastasis | ||
| □ pM1a: Intraperitoneal acellular mucin only | ||
| □ pM1b: Intraperitoneal metastasis only, including mucinous epithelium | ||
| □ pM1c: Non-peritoneal metastasis | ||
| Additional pathologic findings or pre-existing lesions | ||
| □ None | ||
| □ Other: (specify: ) | ||
| Ancillary studies | ||
| □ Specify: | ||
WHO, World Health Organization; ICD-O3, International Classification of Diseases for Oncology, 3rd edition; NOS, not otherwise specified.
ICD-O3, International Classification of Diseases for Oncology, 3rd edition; KCD-8, Korean Classification of Disease, 8th edition; PSOGI, Peritoneal Surface Oncology Group International; LAMN, low-grade appendiceal mucinous neoplasm. Grading divide into low- and high-grade by the two-tier system and G1 to G3 by three-tiered system.
Note that pT1 and pT2 do not apply to LAMN. LAMN, low-grade appendiceal mucinous neoplasm; AJCC, American Joint Committee on Cancer; CRS-HIPEC, cytoreductive surgery with hyperthermic intraperitoneal chemotherapy.
Note that ICD-O3 and KCD-8 codes of primary or unknown origin disseminated peritoneal mucinous disease are 8480/3 and C80.0, respectively. ICD-O3, International Classification of Diseases for Oncology, 3rd edition; KCD-8, Korean Classification of Disease, 8th edition; PSOGI, Peritoneal Surface Oncology Group International; AJCC, American Joint Committee on Cancer; CRS-HIPEC, cytoreductive surgery with hyperthermic intraperitoneal chemotherapy; LAMN, low-grade appendiceal mucinous neoplasm.

 E-submission
E-submission