Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 57(6); 2023 > Article
-
Newsletter
What’s new in dermatopathology 2023: WHO 5th edition updates -
Jonathan Ho, MD1,2
 , Chico J Collie, MD1
, Chico J Collie, MD1
-
Journal of Pathology and Translational Medicine 2023;57(6):337-340.
DOI: https://doi.org/10.4132/jptm.2023.09.22
Published online: October 17, 2023
1Department of Pathology, The University of the West Indies, Mona Campus, Jamaica W.I.
2Division of Dermatology, Department of Medicine, The University of the West Indies, Mona Campus, Jamaica W.I.
- Corresponding Author: Jonathan D. Ho, MBBS, DSc, Dip Dermpath Departments of Pathology and Medicine, The University of the West Indies, Mona Campus, Jamaica W.I. E-mail: jonathan.ho@uwimona.edu.jm
- This article has been published jointly, with consent, in both Journal of Pathology and Translational Medicine and PathologyOutlines.com.
• Received: July 30, 2023 • Accepted: September 21, 2023
© 2023 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- The 5th edition WHO Classification of Skin Tumors (2022) has introduced changes to nomenclature and diagnostics. Important differences are discussed below. Changes in each category of skin tumor have been detailed, with particular emphasis on meaningful advances in our understanding of the molecular pathogenesis of the skin’s diverse tumor landscape.
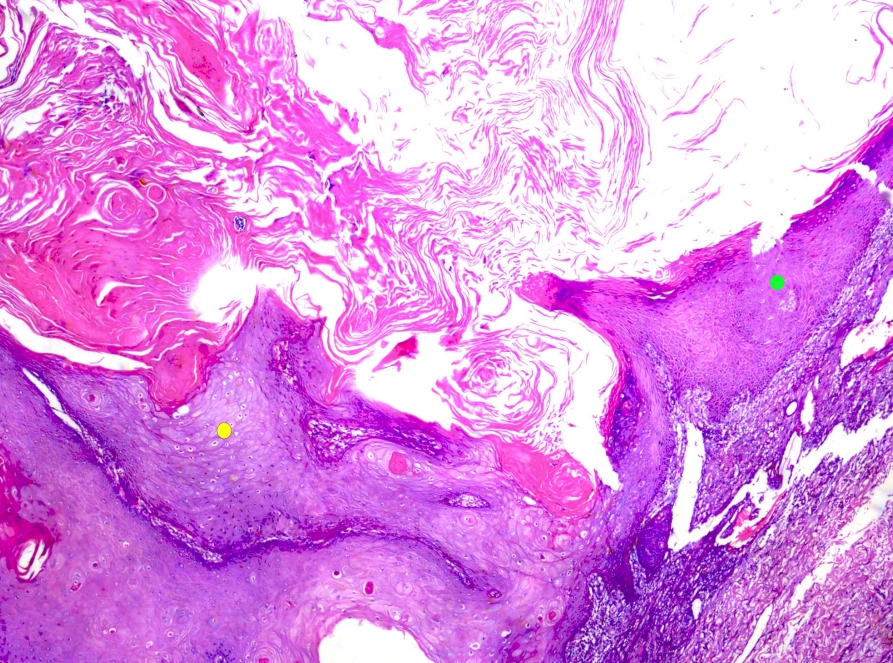
- • Keratoacanthoma is kept separate from squamous cell carcinoma (SCC). Continued recognition that keratoacanthoma likely represents an SCC variant with self-resolving potential (Fig. 1).
- • Adenosquamous carcinoma has been removed as an SCC subtype. It is thought to represent squamoid eccrine ductal carcinoma; discussed with adnexal neoplasms.
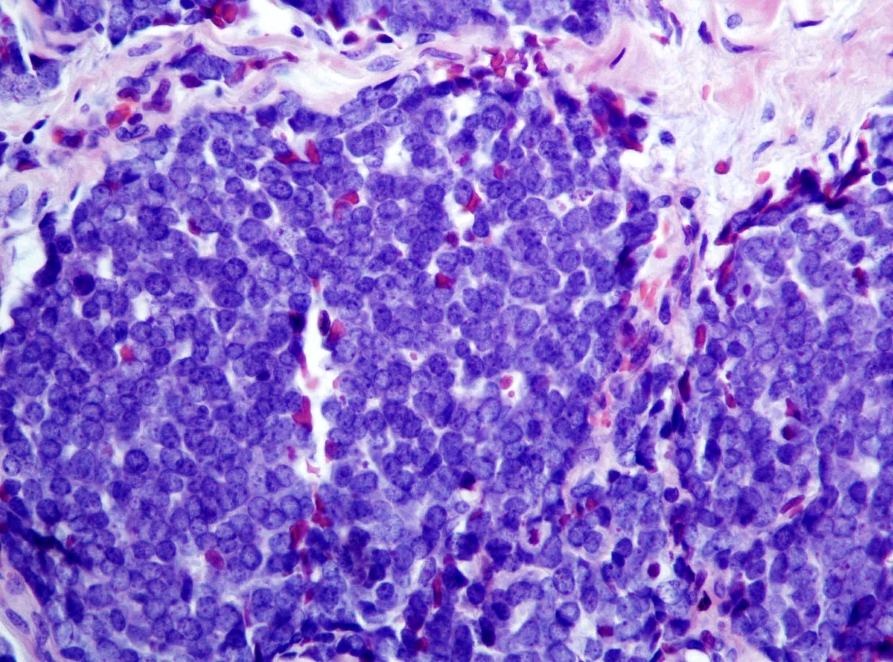
- • Merkel cell carcinoma (Fig. 2) designated a neuroendocrine carcinoma of skin. In non-Merkel cell polyomavirus (MCPyV)-associated cases, TP53 and RB1 mutations seen in other neuroendocrine carcinomas are identified. Origin cell remains unclear.
KERATINOCYTIC/EPIDERMAL TUMORS
- • Advanced understanding of the molecular pathways in melanocytic lesions have led to definition changes. Restrained proliferation of activated oncogenes by tumor suppressor genes leads to nevi, while additional mutations and escape from tumor suppressor gene control result in intermediate/malignant neoplasms [1].
- • Nevi: clonal neoplasms with a single mutation, no other pathogenic changes, bland cytologic appearance and benign behavior.
- • Melanocytomas: intermediate neoplasms between nevi and melanomas harboring > 1 driver mutation. Display atypical histopathologic features and potential for local recurrence. Second mutations affect specific pathways resulting in reproducible clinical and microscopic features.
- • Some melanocytomas (previously designated “nevi”) have been renamed to reflect respective specific pathway aberrations and their intermediate status.
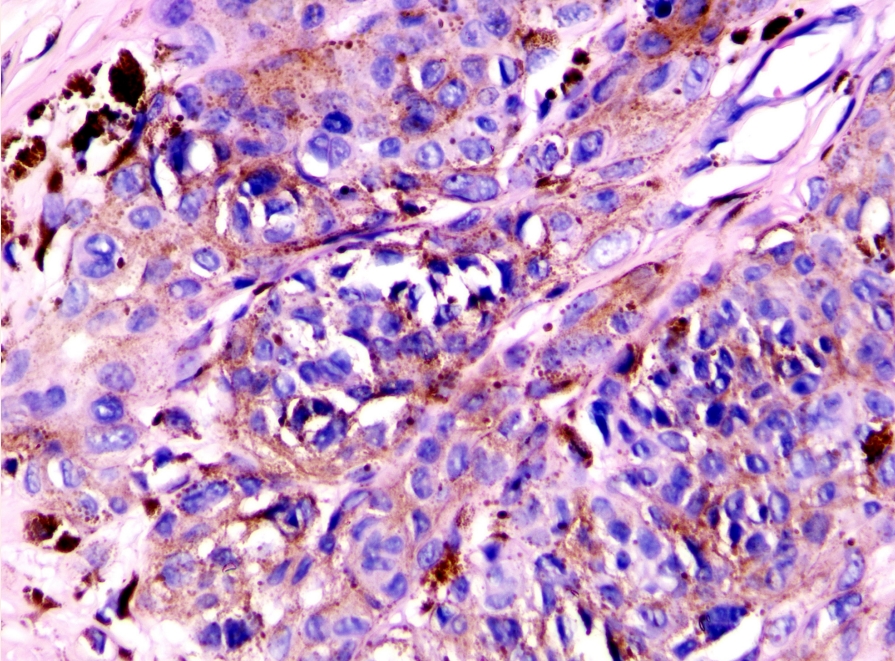
- - Wnt-activated deep penetrating/plexiform melanocytoma (Fig. 3)
- - Pigmented epithelioid melanocytoma (PEM, also known as PRKAR1Ainactivated melanocytoma)
- - BAP1-inactivated melanocytoma
- - Spitz melanocytoma (previously atypical Spitz tumor)
- - Microphthalmia-associated transcription factor (MITF) pathway-activated melanocytic tumors, see below
- • Immunohistochemistry can aid in diagnosis:
- - Loss of expression of PrkAr1a in some PEM
- - Diffuse nuclear β-catenin, nuclear LEF1 in Wnt-activated deep penetrating/plexiform melanocytoma [2].
- - Loss of nuclear BAP1 expression in BAP1-inactivated melanocytoma
- • MITF pathway-activated melanocytic tumors are a newly introduced set of melanocytomas with cytoplasmic clearing and fusion genes resulting in overactive MITF functioning [3,4]. Main differentials include clear cell sarcoma, PEComa, melanoma and carcinomas. Two variants are described
- - Clear cell tumor with melanocytic differentiation and ACTIN::MITF Translocation (CCTMAM)
- ° Cutaneous nodule
- ° Dermal based +/- subcutis. Marked cytoplasmic clearing. Low/high-grade nuclear features but mitoses are inconspicuous and the lesion lacks ulceration or perineural invasion. MART-1, HMB45, S100, MITF positive. Pankeratin negative.
- - Clear cell tumor with melanocytic differentiation and MITF::CREM translocation (CCTMMC)
- ° Cutaneous nodule
- ° Dermal based +/- subcutis
- ° Marked cytoplasmic clearing (high-grade areas may lack clear cell change). Perineural invasion and increased mitotic rate described. No ulceration or vascular invasion reported.
- ° Diffuse MART1, S100, SOX10 and MITF. Patchy HMB45. Pankeratin negative.
- • Language endorsements for lesions lacking clear diagnostic criteria
- - Superficial atypical melanocytic proliferation of uncertain significance (SAMPUS) and intraepidermal atypical melanocytic proliferation of uncertain significance (IAMPUS) for lesions falling short of radial growth phase or in-situ melanoma, respectively. These designations imply virtually no risk of distant spread.
- - Melanocytic tumor of uncertain malignant potential (MELTUMP) for neoplasms where vertical growth phase of melanoma is the main alternative and thus the uncertainty lies in potential metastatic risk.
MELANOCYTIC NEOPLASMS
- • Updates in molecular pathology of adnexal tumors
- - Most poromas and some porocarcinomas harbor gene fusions YAP1::MAML2 or YAP1::NUTM1 [5]. Immunohistochemistry with NUT identifies those with NUTM1 rearrangements
- - Some hidradenomas exhibit CRTC1::MAML2 fusion gene.
- - ALPK1 mutations activating NF-κB pathway in some spiradenomas and spiradenocarcinomas (mutually exclusive from CYLD mutations).
- - ETV6::NTRK3 translocation and NFIX::PKNI fusion in cutaneous secretory carcinoma.
- • Cutaneous NUT carcinoma newly introduced (provisional)
- - Rarely described BRD3::NUTM1 or NSD3::NUTM1 rearranged tumors [6].
- - Dermal, infiltrating neoplasm arranged in islands, cords and/or nests.
- - Glandular and squamoid differentiation with abrupt keratinization.
- - Vesicular nuclei, prominent nucleoli.
- - Positive NUT immunohistochemistry; CEA/EMA highlight ductules.
- - Metastatic potential
- • Cribriform carcinoma is renamed as cribriform tumor; definite malignant potential is unclear.
ADNEXAL TUMORS
- • Newly introduced section encompassing:
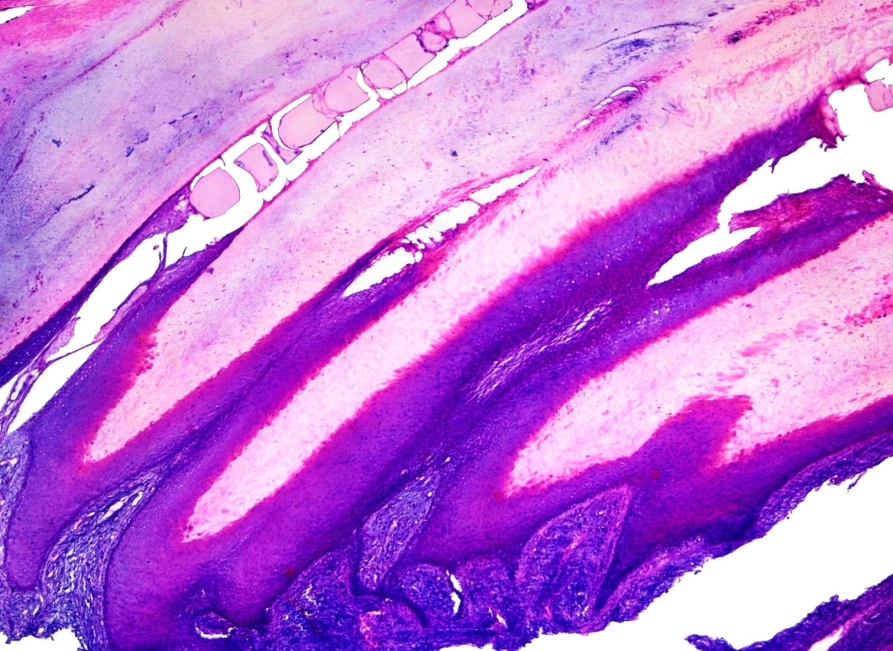
- - Onychomatricoma (Fig. 4)
- - Onychopapilloma
- - Ungual fibrokeratoma
- - Onychocytic matricoma
- - Subungual keratoacanthoma
TUMORS OF THE NAIL UNIT
- • Dendritic cell neoplasms
- - Introduction of mature plasmacytoid dendritic cell proliferation (MPDCP) associated with myeloid neoplasm.
- - MPDCP is a proliferation of plasmacytoid dendritic cells with low-grade cytology occurring in patients with known myeloid neoplasms (most commonly chronic myelomonocytic leukemia and acute myeloid leukemia).
- • Histiocytic neoplasms
- - ALK-positive histiocytosis: A histiocytic neoplasm that may histologically resemble juvenile xanthogranuloma and is characterized by ALK gene rearrangement and positive ALK immunohistochemistry.
- - Indeterminate dendritic cell tumor replaces indeterminate dendritic cell “histiocytosis”. The definitive cell of origin remains unclear.
- - BRAF V600E mutations in Langerhans cell histiocytosis increase risk of relapse, severe clinical manifestations and treatment failure [7]. Patients may benefit from targeted BRAF inhibitor therapy.
- • T-cell and NK-cell lymphoproliferative disorders and neoplasms
- - Primary cutaneous T-cell lymphomas (PCTCL) are all listed as individual entities including those previously labeled “rare subtypes”, i.e., subcutaneous panniculitis-like T-cell lymphoma, extranodal NK/T-cell lymphoma, primary cutaneous CD8+ aggressive epidermotropic cytotoxic T-cell lymphoma, primary cutaneous γ/δ T-cell lymphoma, primary cutaneous CD4-positive small or medium T-cell lymphoproliferative disorder, and primary cutaneous acral CD8- positive lymphoproliferative disorder.
- - Cutaneous CD8-positive acral T-cell lymphoma reclassified as a lymphoproliferative disorder. This entity is indolent with excellent long-term outcomes.
- - “Primary cutaneous peripheral T-cell lymphoma, not otherwise specified (NOS)” should be used for cases that cannot be classified as a known PCTCL subtype.
- - Newly introduced section on inborn error of immunity-associated lymphoproliferative disorders, which are CD8+ T-cell rich dermal infiltrates +/- granulomatous inflammation associated with inborn immunodeficiencies. May present as nodules, papules or ulceronecrotic lesions. EBV in-situ hybridization must be negative.
TUMORS OF HEMATOPOIETIC AND LYMPHOID ORIGIN
- • Introduction of four new entities:
- - CRTC1::TRIM11 cutaneous tumor: dermal-based neoplasm characterized by well-circumscribed proliferation of spindled/epithelioid cells with pale cytoplasm. Arranged in nests/fascicles and may or may not have a vaguely palisaded appearance. Diffuse SOX10 expression; variable positivity for S100 and other melanocytic markers. CRTC1::TRIM11 fusion. Most commonly seen on the extremities. Generally indolent but may recur locally or metastasize [8,9].
- - Superficial CD34-positive fibroblastic tumor: indolent neoplasm occurring in the skin and subcutis with a predilection for the extremities. Characterized by a mixture of spindled and epithelioid cells with moderate pleomorphism, prominent nucleoli, nuclear pseudoinclusions and eosinophilic cytoplasm (granular/glassy). Admixed mixed inflammatory cells are characteristic. Diffuse CD34, PRDM10, and CADM3 expression. AE1/AE3 positivity >50%. PRDM10 rearrangement in >50% of cases [10]. Excision is curative in most cases.
- - EWSR1::SMAD3 rearranged fibroblastic tumor: well-demarcated superficial tumor exhibiting intersecting fascicles of bland fibroblastic spindle cells peripherally and relatively acellular, hyalinized collagen centrally (may lack clear zones). Diffuse nuclear ERG positivity; negative for SMA, EMA, SOX10, CD34, S100. EWSR1::SMAD3 fusion present. Benign tumor; may have local recurrence.
- - NTRK-rearranged spindle cell neoplasm: group of spindle cell lesions with frequent NTRK rearrangements, most commonly seen in children. Involves the dermis and subcutis with a spectrum of appearances, including bland spindle cells in fibrous septa entrapping mature fat to highly cellular lesions with sheets/fascicles of spindle cells. Foci of high-grade atypia is possible. Variable CD34, SMA, S100 positivity. Diffuse panTRK positivity if NTRK fusion present.
- • Atypical intradermal smooth muscle neoplasm remains the preferred terminology for smooth muscle tumors with cytologic atypia limited to the dermis. Lesions have limited metastatic potential and an excellent prognosis once completely excised.
- • Epithelioid fibrous histiocytoma is classified as being of uncertain differentiation rather than a dermatofibroma subtype.
SOFT TISSUE TUMORS
- Newly introduced section detailing tumor syndromes with cutaneous neoplasms including:
- • Familial melanoma
- • BAP1 tumor predisposition syndrome
- • Xeroderma pigmentosum
- • Nevoid basal cell carcinoma syndrome (Gorlin syndrome)
- • Carney complex
- • Muir-Torre syndrome
- • Brooke-Spiegler and related syndromes
GENETIC TUMOR SYNDROMES ASSOCIATED WITH SKIN MALIGNANCIES
- Dr. Jonathan Ho has been an author for PathologyOutlines.com since 2021 and the Deputy Editor for Dermatopathology since January 2023. He is currently a Lecturer at The University of the West Indies, Mona Campus, Jamaica where he practices dermatopathology and dermatology and is the CoDirector of the dermatology residency program.
- Dr. Chico Collie has been a resident author for PathologyOutlines.com since 2021. He is the Chief Resident in Pathology at the University of the West Indies, Mona Campus, Jamaica. He is passionate about surgical pathology, with a subspecialty interest in dermatopathology.
Meet the Authors
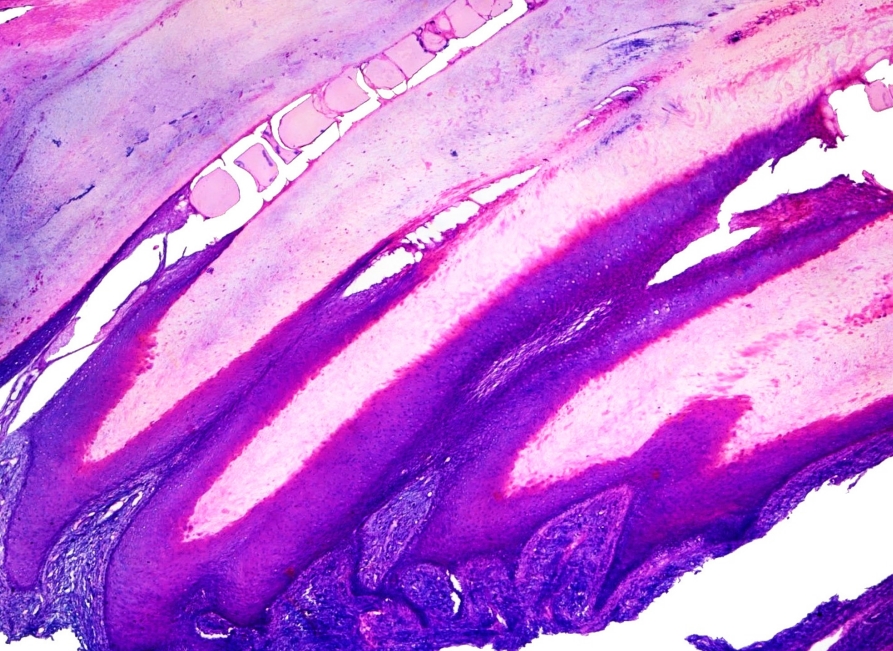
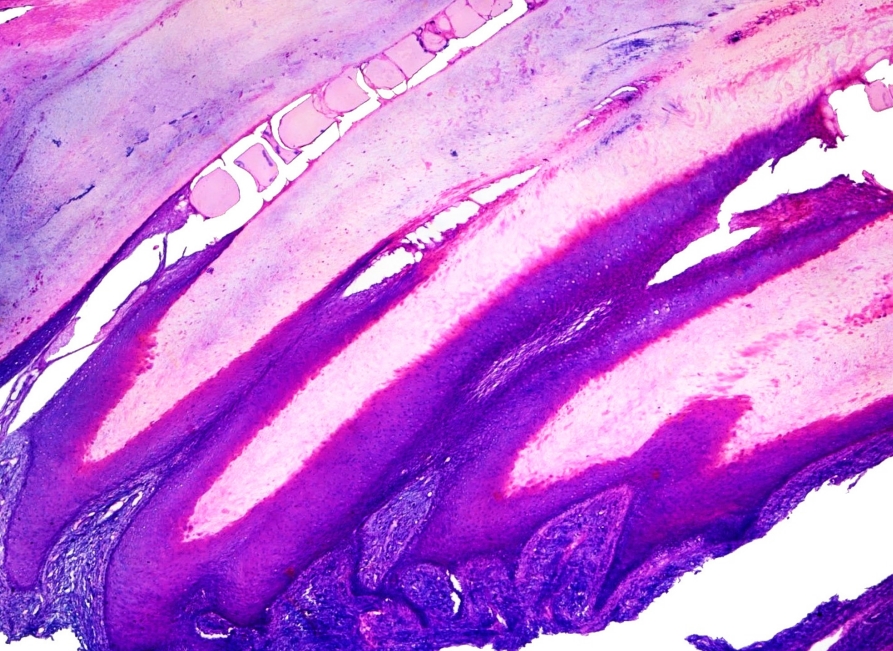
Fig. 1.Keratoacanthoma. This crateriform squamous cell carcinoma variant possesses self-resolving potential. Thick glassy epithelium (yellow dot) may regress via thinner basophilic epithelium (green dot) as shown in the image.
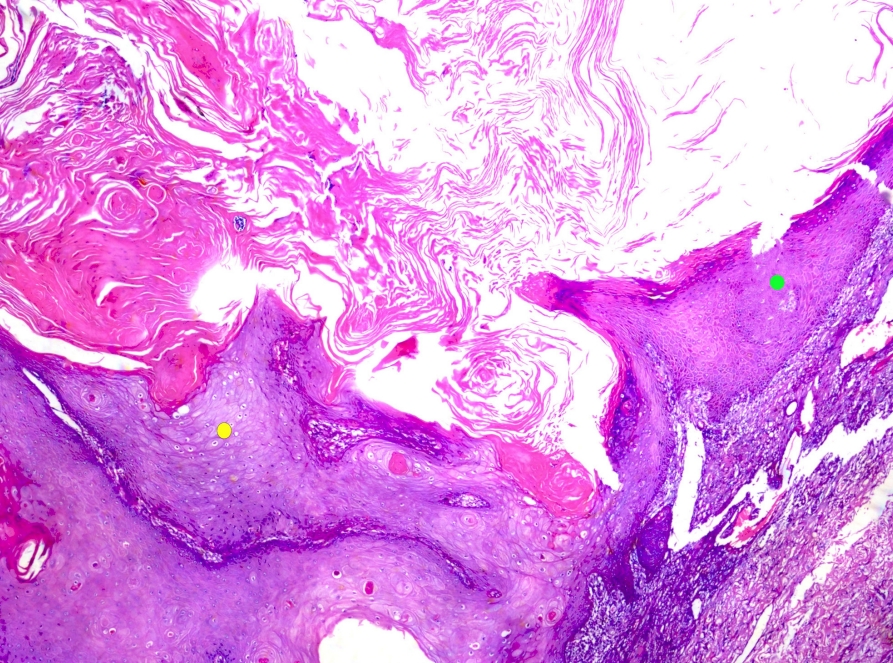
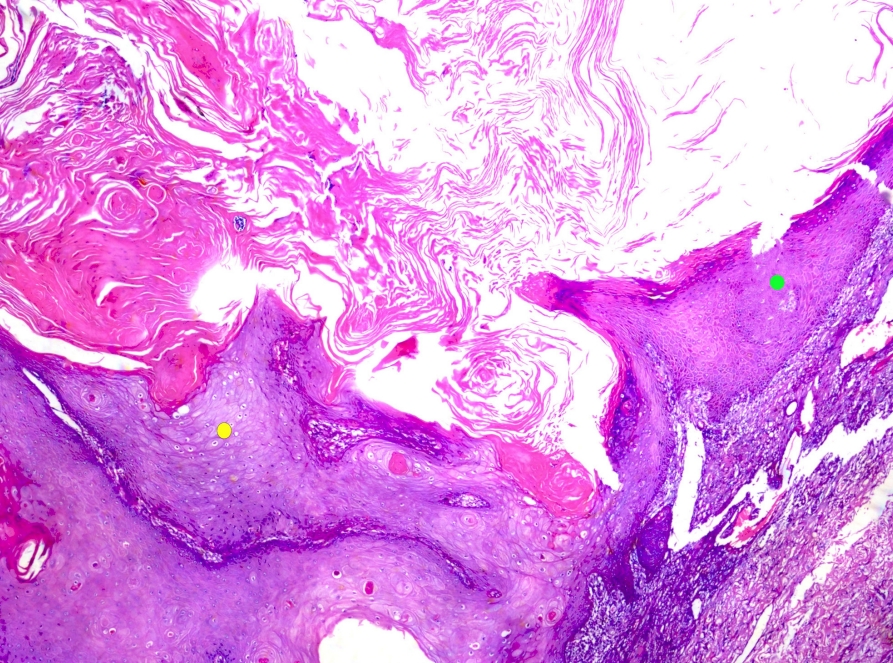
Fig. 2.Merkel cell carcinoma (primary cutaneous neuroendocrine carcinoma of skin). The tumor demonstrates round blue cells with a characteristic finely dispersed “salt and pepper” chromatin pattern. Both Merkel cell polyomavirus associated and non-associated cases exist.
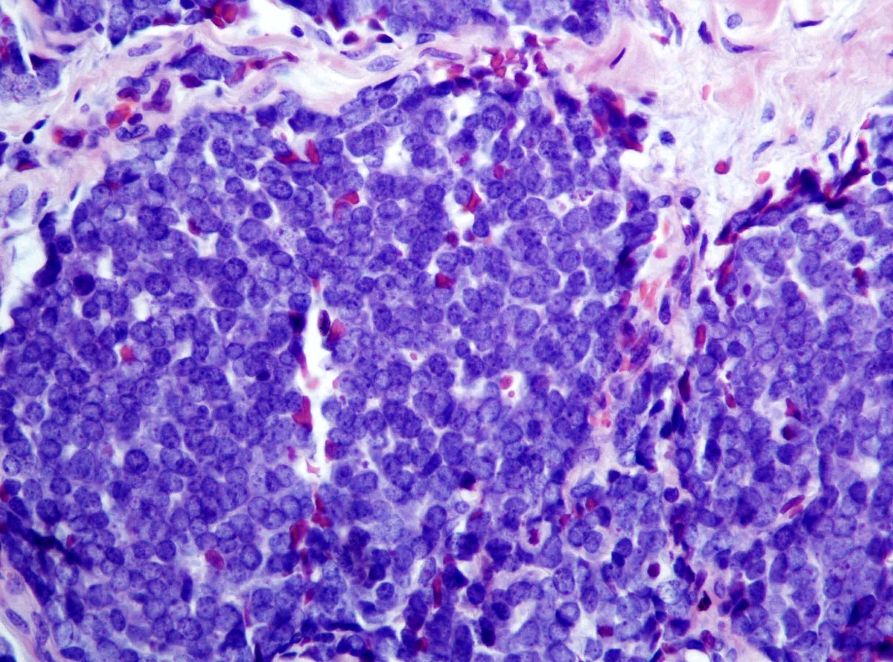
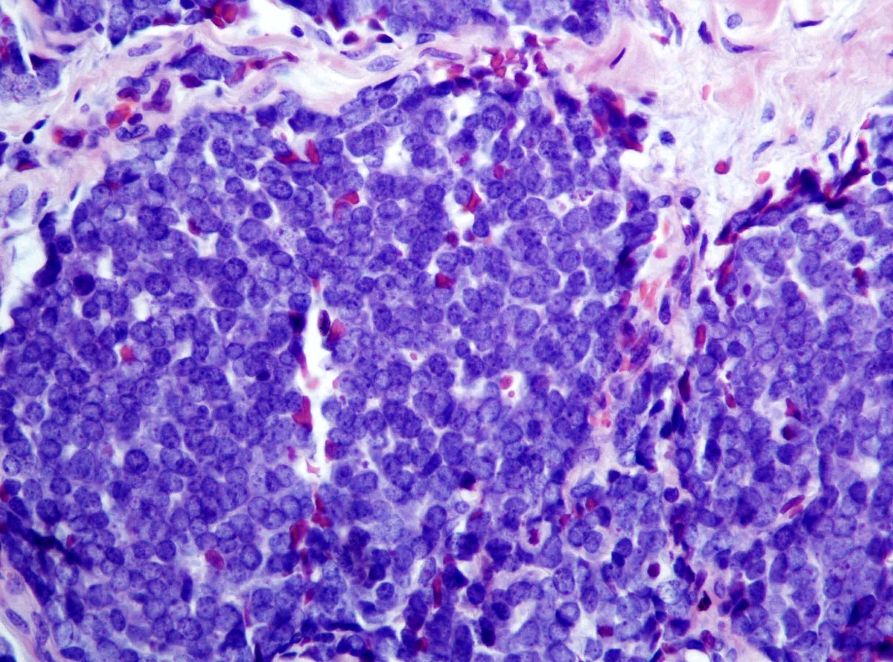
Fig. 3.Wnt-activated deep penetrating/plexiform melanocytoma. This tumor lacks maturation with descent, displays nested/plexiform melanocytes with visible nucleoli, some nuclear pleomorphism, nuclear pseudoinclusions, and melanophages. Expresses nuclear β-catenin and LEF1.
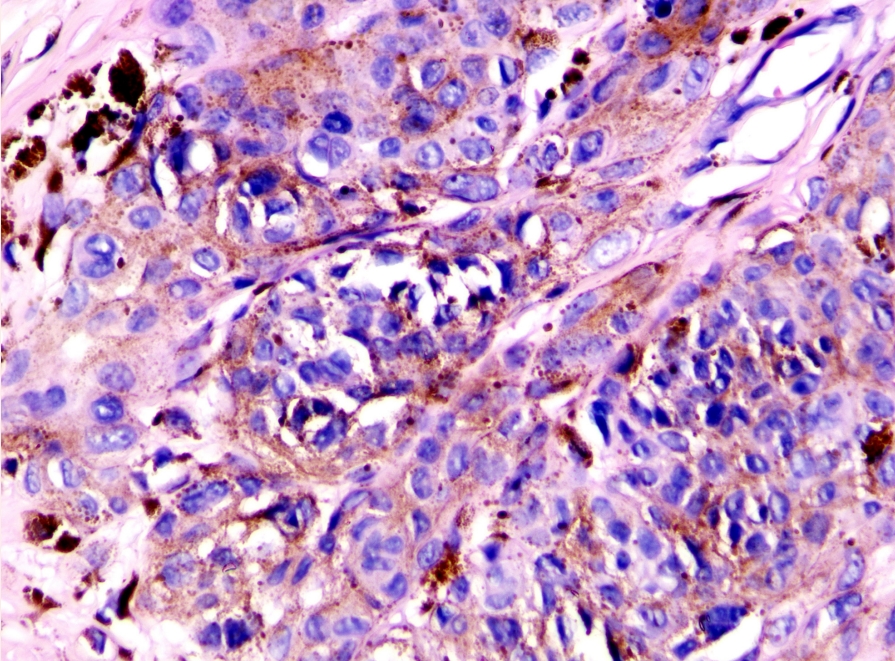
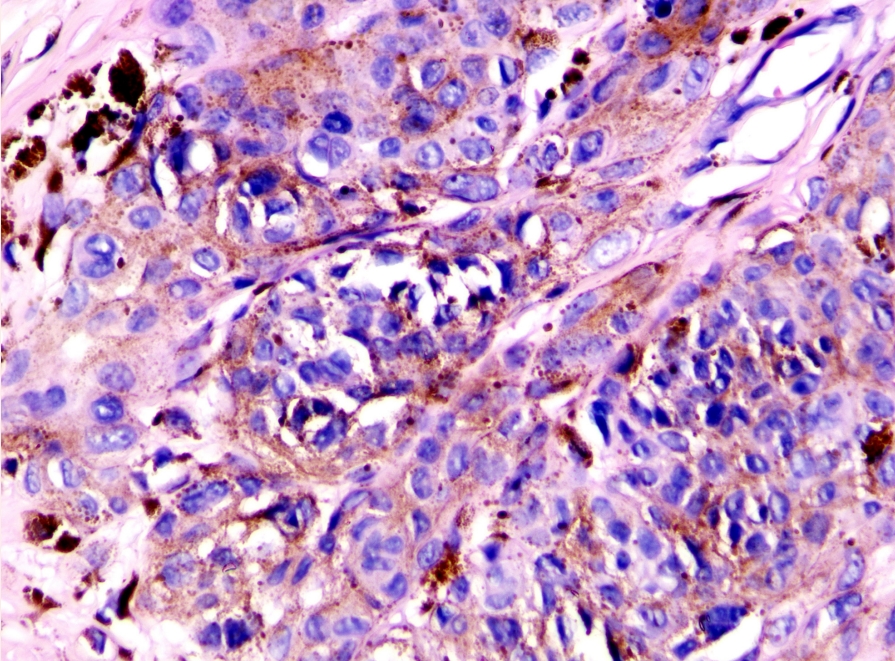
Fig. 4.Onychomatricoma. Note typical papillomatous projections of matrical-type epithelium with deep V-shaped invaginations. Subjacent spindle cell proliferation expresses CD34.
- 1. Bastian BC. The molecular pathology of melanoma: an integrated taxonomy of melanocytic neoplasia. Annu Rev Pathol 2014; 9: 239-71. ArticlePubMedPMC
- 2. Raghavan SS, Saleem A, Wang JY, Rieger KE, Brown RA, Novoa RA. Diagnostic utility of LEF1 immunohistochemistry in differentiating deep penetrating nevi from histologic mimics. Am J Surg Pathol 2020; 44: 1413-8. ArticlePubMed
- 3. de la Fouchardiere A, Pissaloux D, Tirode F, Karanian M, Fletcher CDM, Hanna J. Clear cell tumor with melanocytic differentiation and ACTIN-MITF translocation: report of 7 cases of a novel entity. Am J Surg Pathol 2021; 45: 962-8. PubMed
- 4. de la Fouchardiere A, Pissaloux D, Tirode F, Hanna J. Clear cell tumor with melanocytic differentiation and MITF-CREM translocation: a novel entity similar to clear cell sarcoma. Virchows Arch 2021; 479: 841-6. ArticlePubMedPDF
- 5. Sekine S, Kiyono T, Ryo E, et al. Recurrent YAP1- MAML2 and YAP1-NUTM1 fusions in poroma and porocarcinoma. J Clin Invest 2019; 129: 3827-32. ArticlePubMedPMC
- 6. Nishimura Y, Ryo E, Yamazaki N, Yatabe Y, Mori T. Cutaneous primary NUT carcinoma With BRD3- NUTM1 Fusion. Am J Surg Pathol 2021; 45: 1582-4. ArticlePubMed
- 7. Héritier S, Emile JF, Barkaoui MA, et al. BRAF mu- tation correlates with high-risk langerhans cell histiocytosis and increased resistance to first-line therapy. J Clin Oncol 2016; 34: 3023-30. ArticlePubMedPMC
- 8. Bontoux C, Baroudjian B, Le Maignan C, et al. CRTC1-TRIM11 fusion in a case of metastatic clear cell sarcoma: are CRTC1-TRIM11 fusion-bearing tumors melanocytomas or clear cell sarcomas? Am J Surg Pathol 2019; 43: 861-3. PubMed
- 9. Yang L, Yin Z, Wei J, et al. Cutaneous melanocytic tumour with CRTC1::TRIM11 fusion in a case with recurrent local lymph node and distant pulmonary metastases at early stage: aggressive rather than indolent? Histopathology 2023; 82: 368-71. ArticlePubMedPDF
- 10. Puls F, Carter JM, Pillay N, et al. Overlapping morphological, immunohistochemical and genetic features of superficial CD34-positive fibroblastic tumor and PRDM10-rearranged soft tissue tumor. Mod Pathol 2022; 35: 767-76. ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Primary cutaneous cribriform tumor: A case report and literature review
Doukou Jiang, Yongzhen Tian, Jiabin Tian, Hui Liu, Yang Guan
Journal of Cutaneous Pathology.2025; 52(1): 9. CrossRef - Pediatric Cutaneous T‐Cell Neoplasms: Clinical and Pathological Features, Updated Classifications, and Critical Differential Diagnoses
Jinjun Cheng, Birte Wistinghausen, A. Yasmine Kirkorian
Pediatric Dermatology.2025; 42(1): 11. CrossRef - Histologic and Immunohistochemical Patterns in Lymphomatoid Papulosis: A Systematic Review of Published Cases
Torben Fricke, Werner Kempf, Michael P. Schön, Christina Mitteldorf
Dermatopathology.2025; 12(1): 6. CrossRef - Unveiling cutaneous adenosquamous carcinoma: A systematic review and case analysis of a rare cutaneous malignancy
Adam Christie, Jessica Falon, Jennifer Kim, Julie Howle
EJC Skin Cancer.2025; 3: 100733. CrossRef - Merkel Cell Carcinoma: An Updated Review Focused on Bone and Bone Marrow Metastases
Biagio Scotti, Elisabetta Broseghini, Costantino Ricci, Barbara Corti, Costanza Viola, Cosimo Misciali, Carlotta Baraldi, Sabina Vaccari, Martina Lambertini, Federico Venturi, Elisabetta Magnaterra, Aurora Alessandrini, Tiziano Ferrari, Massimo Lepri, Gab
Cancers.2025; 17(13): 2253. CrossRef - Melanoma
Mette Mogensen, Terese von Knorring, Lisbet Rosenkrantz Hölmich, Torben Steiniche, Johanne Lade-Keller, Katrine Karmisholt, Silje Haukali Omland
Ugeskrift for Læger.2025; : 1. CrossRef - Prognosis and Follow‐Up Recommendations for Subcutaneous and Dermal Leiomyosarcoma: Local Recurrence, Metastasis, and Overall Survival in a Danish Nationwide Cohort of 661 Patients
Kiya Abebe, Mathias Ørholt, Erik E. F. Bak, Andreas Larsen, Anne Lene Wagenblast, Grethe Schmidt, David Hebbelstrup Jensen, Michael M. Petersen, Anand C. Loya, Søren Daugaard, Mikkel Herly, Jason L. Hornick, Thomas Mentzel, Peter Vester‐Glowinski
Journal of Surgical Oncology.2025; 132(6): 1076. CrossRef - Diagnostic and prognostic value of immunohistochemical markers HMB-45, Melan-A/MART-1, and S100 in different histological subtypes of melanoma
Kirill A. Silakov, Ekaterina Yu. Demenkova, Vladimir I. Shchekin, Maksim A. Bobrov, Grigory A. Demyashkin
Morphology.2025; 163(4): 353. CrossRef - Rethinking Melanocytic Tumors: A Critical Appraisal of the WHO Classification and the Myth of Nevus-to-Melanoma Progression
Giuseppe Argenziano, Giulia Briatico, Eugenia Veronica Di Brizzi, Camila Scharf, Gabriella Brancaccio, Elvira Moscarella, Maria Maddalena Nicoletti, Pasquale Verolino, Aimilios Lallas, Harald Kittler
Dermatology Practical & Conceptual.2025; 15(4): 6994. CrossRef - Translating Features to Findings: Deep Learning for Melanoma Subtype Prediction
Dorra Guermazi, Sarina Khemchandani, Samer Wahood, Cuong Nguyen, Elie Saliba
Dermatopathology.2025; 12(4): 42. CrossRef - Multiple Onychopapillomas and BAP1 Tumor Predisposition Syndrome
Alexandra Lebensohn, Azam Ghafoor, Luke Bloomquist, Michael C. Royer, Leslie Castelo-Soccio, Kelli Karacki, Olanda Hathaway, Tenin Maglo, Cathy Wagner, Maria G. Agra, Andrew M. Blakely, David S. Schrump, Raffit Hassan, Edward W. Cowen
JAMA Dermatology.2024; 160(8): 838. CrossRef - Molecular and Histopathological Characterization of Metastatic Cutaneous Squamous Cell Carcinomas: A Case–Control Study
Alessia Paganelli, Marco Zaffonato, Benedetta Donati, Federica Torricelli, Veronica Manicardi, Michela Lai, Marco Spadafora, Simonetta Piana, Alessia Ciarrocchi, Caterina Longo
Cancers.2024; 16(12): 2233. CrossRef - The Gray Zone of Melanocytic Tumors - A Clinical Point of View
Camila Scharf, Giulia Briatico, Gabriella Brancaccio, Elvira Moscarella, Andrea Ronchi, Giuseppe Argenziano
Dermatology Practical & Conceptual.2024; 14(2): e2024153. CrossRef - Biologic Gray Zone of Melanocytic Tumors, Fiction or Reality?
Harald Kittler
Dermatology Practical & Conceptual.2024; 14(2): e2024148. CrossRef - Minimally Invasive Plasma Device Management of Multiple Benign Skin Cancers Associated with Rare Genodermatoses—Case Series and Review of the Therapeutic Methods
Anna Płatkowska, Monika Słowińska, Joanna Zalewska, Zbigniew Swacha, Anna Szumera-Ciećkiewicz, Michał Wągrodzki, Janusz Patera, Katarzyna Łapieńska-Rey, Małgorzata Lorent, Iwona Ługowska, Piotr Rutkowski, Witold Owczarek
Journal of Clinical Medicine.2024; 13(15): 4377. CrossRef - Clinical Variables Influencing Outcomes in Patients with Atypical Intradermal Smooth Muscle Neoplasms (Formerly Cutaneous Leiomyosarcomas): Single-Institution Study of 95 Surgical Patients
Alicia Gingrich, Sintawat Wangsiricharoen, Madeline B. Torres, Vinod Ravi, Ravin Ratan, Emily Z. Keung, Christopher P. Scally, Alexander J. Lazar, Wei-Lien Wang, Christina L. Roland, Kelly K. Hunt, Wendong Yu, Keila E. Torres
Annals of Surgical Oncology.2024; 31(12): 7950. CrossRef - A Narrative Review of Molecular, Immunohistochemical and In-Situ Techniques in Dermatopathology
J. A. Gabriel, N. Weerasinghe, P. Balachandran, R. Salih, G. E. Orchard
British Journal of Biomedical Science.2024;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles
-
- What’s new in hematopathology 2025: myeloid neoplasms in the WHO 5th edition and ICC
- What’s new in neuropathology 2024: CNS WHO 5th edition updates
- What’s new in adrenal gland pathology: WHO 5th edition for adrenal cortex
- What’s new in genitourinary pathology 2023: WHO 5th edition updates for urinary tract, prostate, testis, and penis
- What’s new in hematopathology 2023: updates on mature T-cell neoplasms in the 5th edition of the WHO classification
What’s new in dermatopathology 2023: WHO 5th edition updates




Fig. 1. Keratoacanthoma. This crateriform squamous cell carcinoma variant possesses self-resolving potential. Thick glassy epithelium (yellow dot) may regress via thinner basophilic epithelium (green dot) as shown in the image.
Fig. 2. Merkel cell carcinoma (primary cutaneous neuroendocrine carcinoma of skin). The tumor demonstrates round blue cells with a characteristic finely dispersed “salt and pepper” chromatin pattern. Both Merkel cell polyomavirus associated and non-associated cases exist.
Fig. 3. Wnt-activated deep penetrating/plexiform melanocytoma. This tumor lacks maturation with descent, displays nested/plexiform melanocytes with visible nucleoli, some nuclear pleomorphism, nuclear pseudoinclusions, and melanophages. Expresses nuclear β-catenin and LEF1.
Fig. 4. Onychomatricoma. Note typical papillomatous projections of matrical-type epithelium with deep V-shaped invaginations. Subjacent spindle cell proliferation expresses CD34.
Fig. 1.
Fig. 2.
Fig. 3.
Fig. 4.
What’s new in dermatopathology 2023: WHO 5th edition updates

 E-submission
E-submission