Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 58(4); 2024 > Article
-
Case Study
Concurrent intestinal plasmablastic lymphoma and diffuse large B-cell lymphoma with a clonal relationship: a case report and literature review -
Nao Imuta1,2
 , Kosuke Miyai2,3
, Kosuke Miyai2,3 , Motohiro Tsuchiya2,3
, Motohiro Tsuchiya2,3 , Mariko Saito3
, Mariko Saito3 , Takehiro Sone4
, Takehiro Sone4 , Shinichi Kobayashi4
, Shinichi Kobayashi4 , Sho Ogata2,3
, Sho Ogata2,3 , Fumihiko Kimura4
, Fumihiko Kimura4 , Susumu Matsukuma2,3
, Susumu Matsukuma2,3
-
Journal of Pathology and Translational Medicine 2024;58(4):191-197.
DOI: https://doi.org/10.4132/jptm.2024.05.14
Published online: June 25, 2024
1Medical Student, National Defense Medical College, Tokorozawa, Japan
2Department of Pathology and Laboratory Medicine, National Defense Medical College, Tokorozawa, Japan
3Department of Laboratory Medicine, National Defense Medical College Hospital, Tokorozawa, Japan
4Department of Hematology, National Defense Medical College, Tokorozawa, Japan
- Corresponding Author: Kosuke Miyai, MD, PhD, Department of Laboratory Medicine, National Defense Medical College Hospital, 3-2 Namiki, Tokorozawa, Saitama 359-8513, Japan Tel: +81-4-2995-1211, Fax: +81-4-2996-5193, E-mail: mykusu228@nifty.com
© The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
- 4,715 Views
- 222 Download
Abstract
- Herein, we report a case of plasmablastic lymphoma (PBL) and diffuse large B-cell lymphoma (DLBCL) that occurred concurrently in the large intestine. An 84-year-old female presented with a palpable rectal tumor and ileocecal tumor observed on imaging analyses. Endoscopic biopsy of both lesions revealed lymphomatous round cells. Hartmann’s operation and ileocecal resection were performed for regional control. The ileocecal lesion consisted of a proliferation of CD20/CD79a-positive lymphoid cells, indicative of DLBCL. In contrast, the rectal tumor showed proliferation of atypical cells with pleomorphic nuclei and abundant amphophilic cytoplasm, with immunohistochemical findings of CD38/CD79a/MUM1/MYC (+) and CD20/CD3/CD138/PAX5 (–). Tumor cells were positive for Epstein-Barr virus–encoded RNA based on in situ hybridization and MYC rearrangement in fluorescence in situ hybridization analysis. These findings indicated the rectal tumor was most likely a PBL. Sequencing analysis for immunoglobulin heavy variable genes indicated a common B-cell origin of the two sets of lymphoma cells. This case report and literature review provide new insights into PBL tumorigenesis.
- An 84-year-old female with no notable past or familial medical history was admitted to our hospital with a palpable tumor in the lower rectum. The patient experienced chronic diarrhea lasting 2 months after aluminum potassium sulfate and tannic acid sclerotherapy for internal hemorrhoids. Colonoscopy revealed a 50-mm-sized ulcerating localized tumor with 75% luminal circumference in the lower rectum. A complete blood count before surgery showed normocytic anemia with a red blood cell count of 3.54×106/μL, hemoglobin of 10.8 g/dL, and hematocrit of 30.9%. The serum soluble interleukin-2 receptor (sIL-2R) level was 715.7 U/mL. Serum carbohydrate antigen 19-9 and carcinoembryonic antigen levels were within normal limits. Serological test results for HIV were negative. Fluorodeoxyglucose (FDG) positron emission tomography/computed tomography revealed increased FDG uptake from the cecum to the appendix vermiformis as well as the rectal tumor. Secondary endoscopic examination revealed a 20-mm-sized, slightly elevated polypoid lesion in the cecum (appendiceal orifice), and endoscopic biopsy of the ileocecal lesion revealed CD20/CD79a-positive large lymphoid cell proliferation, indicating DLBCL. In contrast, biopsy specimen of the rectal tumor showed diffuse proliferation of discohesive, pleomorphic cells with immunoreaction of CD20 (–), CD79a (+), and CD3 (–); the diagnosis was “malignant lymphoma, suspected.” For regional tumor control, proctosigmoidectomy (Hartmann’s operation) and ileocecal resection were performed simultaneously.
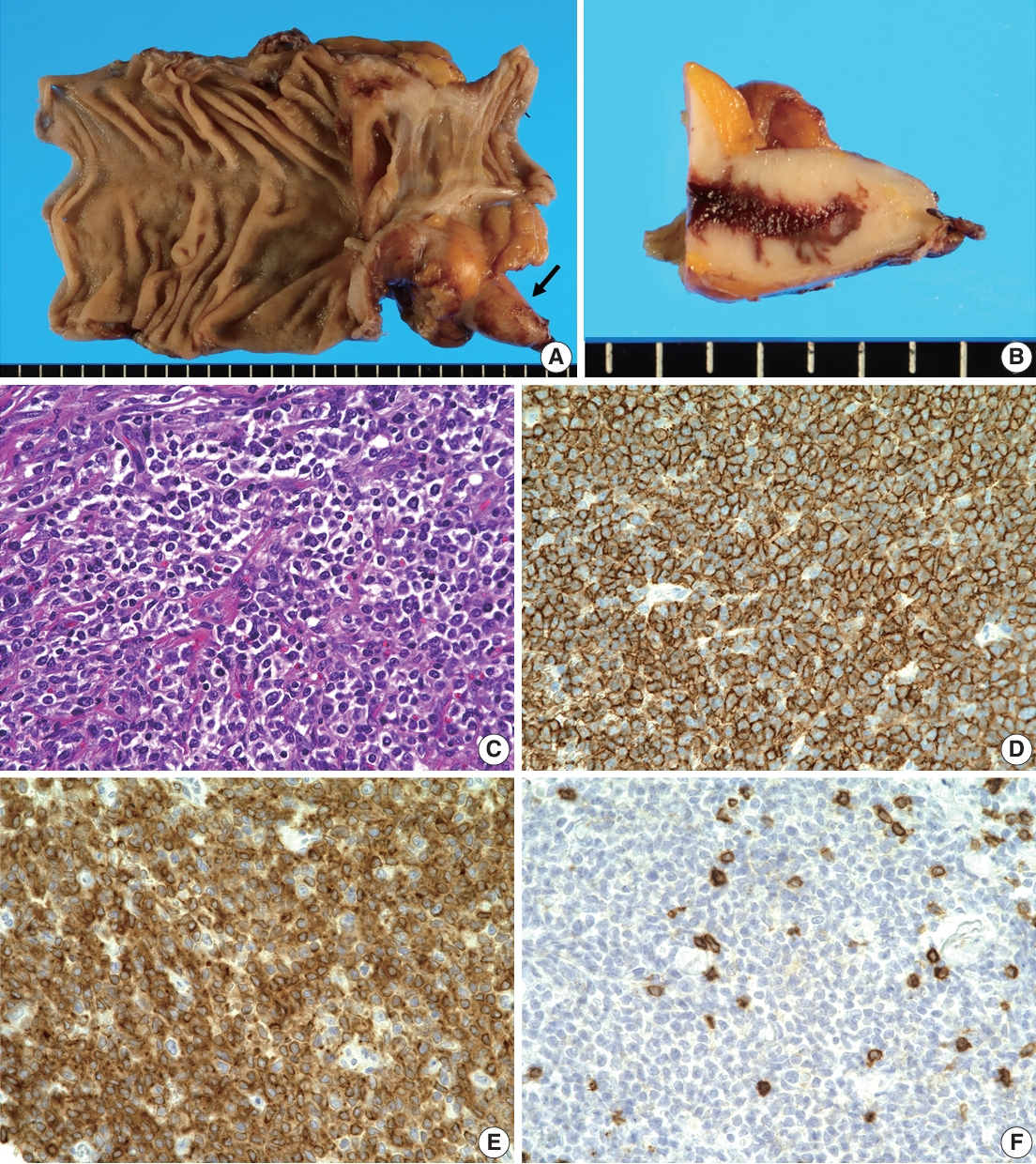
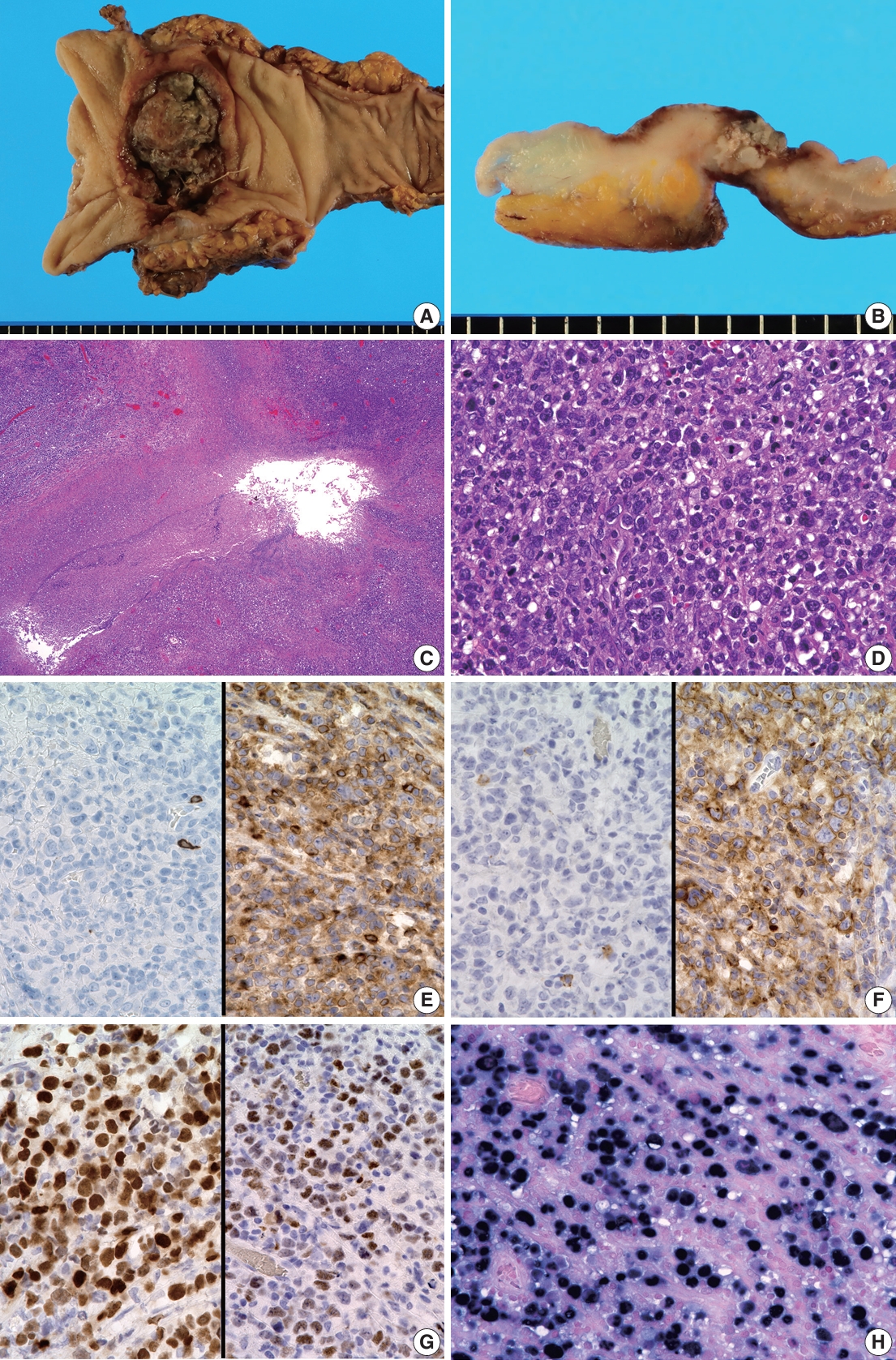
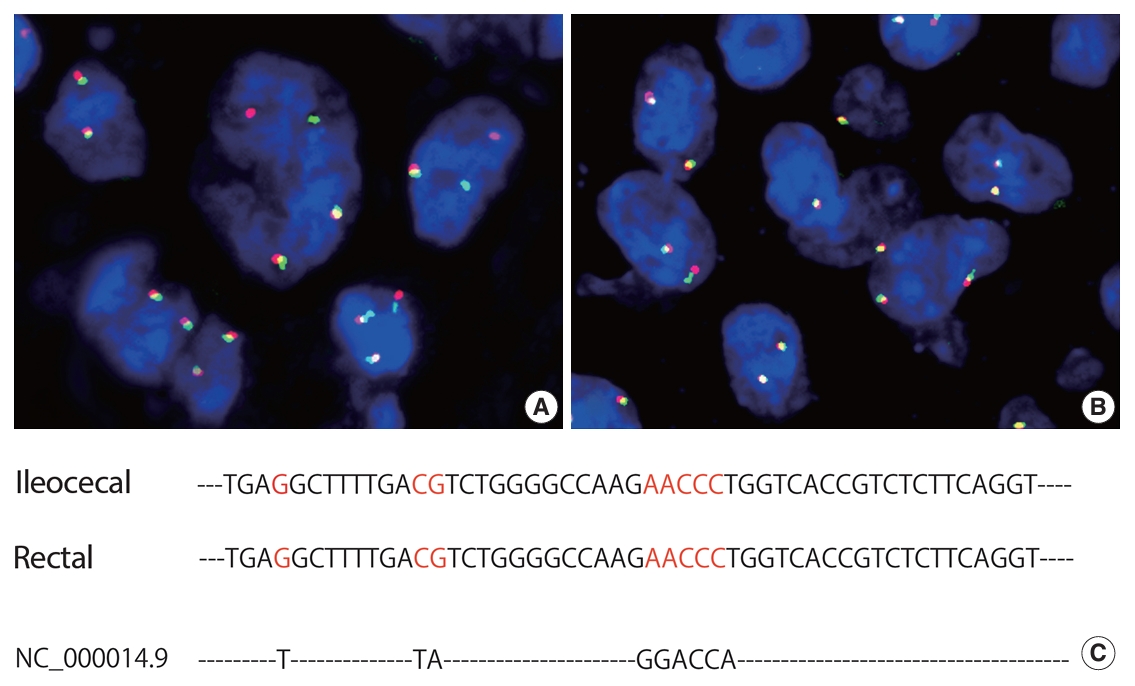
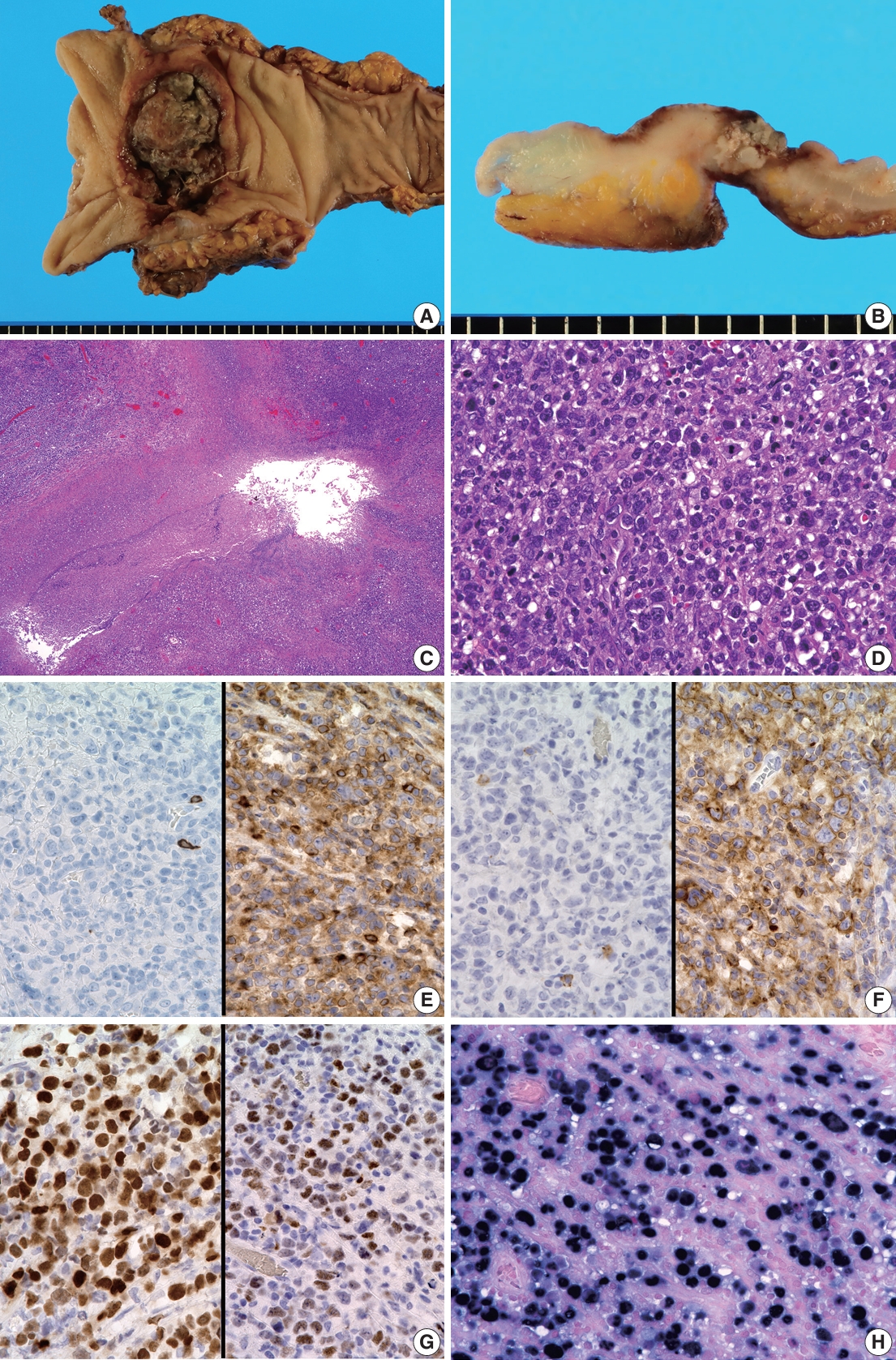
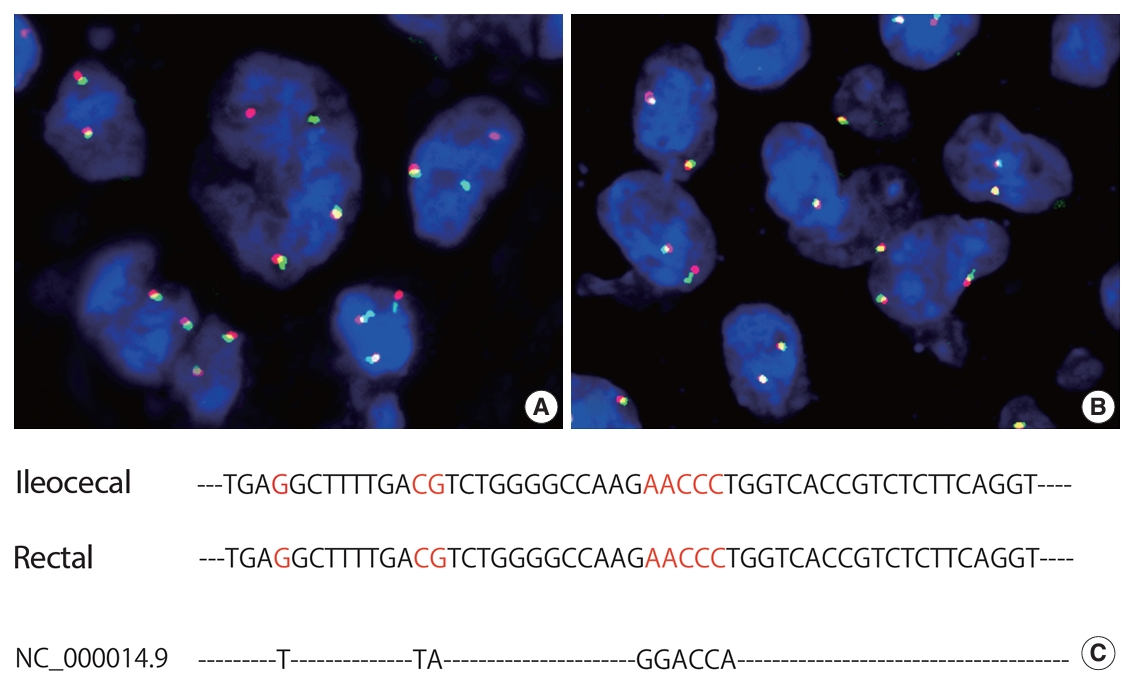
- Grossly, the resected ileocecal specimens showed a 40-mm tumor directly invading and thickening the appendiceal wall (Fig. 1A, B), and the resected rectum exhibited a 55-mm ulcerating localized tumor involving the entire thickness of the rectum (Fig. 2A, B). Both tumors had solid, whitish cut surfaces. Histologically, the ileocecal tumor was comprised of diffusely proliferating medium- to large-sized lymphoid cells with swollen nuclei containing prominent nucleoli (Fig. 1C). These lymphoid cells were diffusely immunoreactive for CD20, CD79a, BCL2, and BCL6 and negative for CD3, CD10, CD30, CD38, CD138, cyclinD1, MYC, and MUM1 (Fig. 1D–F). A few tumor cells tested positive for EBV-encoded RNA (EBER) on in situ hybridization. These findings indicated a possible diagnosis of ileocecal DLBCL, germinal center B-cell type. In contrast, the rectal tumor showed proliferation of atypical lymphoid cells with pleomorphic nuclei and abundant amphophilic cytoplasm (Fig. 2C, D). Multinucleated, bizarre tumor cells were scattered, and geographic coagulative necrosis was observed. Immunohistochemical staining showed these atypical cells to be positive for CD38, CD30, CD79a (focally), MUM1, and MYC (>40%) and negative for CD45, CD20, CD3, CD4, CD8, CD138, BCL2, BCL6, PAX5, and CD56 (Fig. 2E–G). Most tumor cells were positive for EBER on in situ hybridization (Fig. 2H). Fluorescence in situ hybridization (FISH) for detecting MYC rearrangement was performed using ZytoLight SPEC MYC Dual Color Break Apart Probe (ZytoVision GmbH, Bremerhaven, Germany); the split signal was detected in the rectal tumor cells (Fig. 3A) but not in the cecal tumor cells (Fig. 3B), indicating MYC rearrangement in the rectal tumor but not in the cecal tumor. Based on these data, the rectal tumor was most likely PBL. Regional lymph node biopsy at the time of surgery, bone marrow trephine biopsy, and cerebrospinal fluid cytology revealed no lymphoma cell involvement.
- To confirm pathological diagnosis of PBL and identify the cell of origin of these two lymphomas that concurrently occurred in this patient, DNA was extracted from formalin-fixed paraffin-embedded sections for semi-nested polymerase chain reaction (PCR) and the complementarity-determining region (CDR) 3 in the immunoglobulin heavy variable (IGHV) genes sequenced as previously described [9]. Primer sequences were as follows: upstream consensus V region primer (FR2A), 5'-CCGGRAAR RGTCTGGAGTGG-3'; consensus J region primer (LJH, for 1st PCR), 5'-CTTACCTGAGGAGACGGTGACC-3'; and consensus J region primer (VLJH, for 2nd PCR), 5'-GTGAC CAGGGTNCTTGGCCCC-3'. The CDR3 sequences of the ileocecal and rectal tumors matched, indicating that the two emerged from a common clonal B-cell (Fig. 3C). Consequently, a diagnosis of concurrent ileocecal DLBCL and rectal PBL was confirmed.
- The patient was treated with six courses of rituximab, cyclophosphamide, doxorubicin hydrochloride, oncovin, and prednisolone (R-CHOP). The sIL-2R level was within the normal range, and recurrence was not observed on clinical and imaging examinations 1 year after surgery.
CASE REPORT
- The usual immunophenotype of PBL is the expression of plasmacytic markers including CD138, CD38, and MUM1 and the absence of pan B-cell markers including CD20 and PAX5 [15]. Despite the absence of CD138 expression, morphologically and immunohistochemically, the rectal tumor in the present case was most likely PBL. In addition, MYC rearrangement based on FISH analysis was detected only in the rectal PBL. The present case also showed a concurrent ileocecal tumor with features of DLBCL, namely discordant double lymphoma. Sequencing analysis of the CDR3 region in the IGHV genes revealed a common B-cell origin of the tumor cells of the two lymphomas. Based on these findings, the rectal tumor was confidently diagnosed as PBL and showed a clonal relationship with the concurrent ileocecal DLBCL.
- The concomitant occurrence of PBL with other types of lymphoma is extremely rare. Review of the English literature revealed only six case reports in which the histopathological findings of two lymphomas were described [9-14]. The clinicopathological features of these previous cases and the present case are summarized in Table 1. Two patients were in the post-chemotherapeutic state (cases 4 and 5), and no patient was infected with HIV. Histological types concurrent with PBL were CLL/SLL in four cases, DLBCL in two cases, and classical Hodgkin lymphoma and CLL/SLL (concurrent triple lymphoma) in one case. Based on sequencing analysis of the CDR3 region in IGHV genes, the same and different clonality between PBL and other-type lymphomas were detected in three and two cases, respectively. Clonal analysis was not performed in two cases. All patients, except the present case, died of the disease or experienced tumor recurrence, indicating a generally poor patient prognosis.
- PBLs are assumed to originate from plasmablasts that are precursor plasma cells derived from activated B lymphocytes. Although HIV/EBV infection and MYC rearrangement have been indicated in the disease development, the pathogenesis of PBL remains unclear [3-5]. Using whole-exome sequencing and RNA-sequencing analysis for 33 PBLs, Witte et al. [16] described a significant accumulation of the JAK signal transducer mutations and evidence of frequent perturbances of nuclear factor кB signaling (NFKB2 and BTK), which is distinct from mutational and transcriptomic status of DLBCL and plasmacytic myeloma. Conversely, in the present case, the clonal status of the rectal PBL was the same as that of concurrent ileocecal DLBCL, indicating a developmental relationship of these tumors. Hashimoto et al. [9] reported a case of discordant lymphoma consisting of PBL in the urinary bladder and DLBCL in the nasal cavity and proved the clonality of the two lymphomas using sequencing analysis of the CDR3 region in the IGHV genes. In these two cases, in situ hybridization of EBER was diffusely positive in tumor cells of PBL, and only scattered positive tumor cells were observed in DLBCL. In contrast, in three cases that were analyzed for clonality between concurrent PBL and CLL/SLL, one (case 2) showed the same clonal relationship, while two (cases 4 and 5) harbored different clonal relationships, indicating a case-specific pathogenesis of these tumors [11,13,14]. Gene expression analysis and comprehensive genomic and transcriptomic analyses for each set of tumor cells in such concurrent lymphoma cases would help to elucidate the pathogenesis of PBL.
- The treatment of patients with two concurrent lymphomas is generally challenging. R-CHOP was selected for the present case, similar to a previous case of concurrent DLBCL and PBL that showed recurrence of DLBCL after 4 years [9]. Other cases of PBL co-existing with CLL/SLL were also refractory to R-CHOP and/or vincristine, adriamycin, and dexamethasone (VAD) treatment (Table 1, cases 1–5) [10-14]. Basically, standard treatment for PBL has not been established due to the rarity of the disease and its aggressive clinical course. The National Comprehensive Cancer Network guidelines recommend strong regimens such as dose-adjusted etoposide, vincristine, and doxorubicin with bolus doses of cyclophosphamide and prednisone (DA-EPOCH) based on evidence from other aggressive lymphomas [17,18]. In addition, chemotherapy based on bortezomib, a proteasome inhibitor, was effective as frontline treatment for patients with PBL in several case series [19,20]. However, review of the literature indicates that even bortezomib-based regimens are not effective for PBL concurrent with other lymphomas (Table 1, cases 1 and 3) [10,12]. In the present case, intensified chemotherapy, such as bortezomib plus DA-EPOCH, was necessary due to tumor recurrence.
- In summary, we described a case of concurrent intestinal DLBCL and PBL in which the same clonality was detected on sequencing analysis. Data accumulation and molecular genetic analysis of such concurrent lymphoma cases are essential to elucidate their pathogenesis and could provide primary evidence for a treatment strategy in this challenging clinical situation.
DISCUSSION
Ethics Statement
The Institutional Review Board at National Defense Medical College approved publication of this article (Registration number, 4802). Informed consent from the participant has been waived by Institutional Review Board.
Availability of Data and Material
The datasets generated or analyzed during the study are available from the corresponding author on reasonable request.
Code Availability
Not applicable.
Author Contributions
Conceptualization: NI, KM. Data curation: NI, KM. Formal analysis: KM. Investigation: MT, MS, TS, SK, FK. Methodology: KM, MT, SO. Project administration: KM. Resources: SO, SM. Supervision: SK, SO, FK, SM. Visualization: KM. Writing—original draft: NI, KM. Writing—review & editing: MT, MS, SK, SO, FK, SM. Approval of final manuscript: all authors.
Conflicts of Interest
The authors declare that they have no potential conflicts of interest.
Funding Statement
No funding to declare.
Acknowledgments
| Case No. | Age (yr)/Sex | Immunological status | Location of PBL | Type and location of other tumors | Same clonality of lymphomas | Chemoradiotherapy |
Immunohistochemical analysis of PBL |
Outcome, post diagnosis of PBL | Study | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD20 | CD79a | CD138 | CD38 | MUM1 | MYC | EBER | |||||||||
| 1 | 67/M | Immunocompetent, HIV (–) | Ileocecal valve, left humerus | CLL, bone marrow | N/A | Bortezomib and dexamethasone | - | + | + | + | + | N/A | + | DOD, 2.5 mo | Hatzimichael et al. [10] |
| 2 | 61/M | Immunocompetent, HIV (–), EBV (–), HHV-8 (–) | Lymph node | SLL, the same lymph node as PBL | Detected | Hyper-C-VAD | - | N/A | + | N/A | + | N/A | - | DOD, a couple of months | Ronchi et al. [11] |
| 3 | 48/M | Immunocompetent, HIV (–) | Left supraclavicular area, duodenum | CLL, bone marrow | N/A | R-CHOP, bortezomib, ifosfamide, etoposide, carboplatin, mesna, brentuximab vedotin, and radiation to the neck lesion | N/A | + | + | + | + | N/A | N/A | DOD, N/A | Holderness et al. [12] |
| 4 | 57/F | Postchemotherapy for CLL, HIV (–), CMV IgM (–), CMV IgG (+) | Mandible, bone marrow | CLL, bone marrow | Not detected (different clones) | VAD and CHOP | - | N/A | N/A | N/A | N/A | N/A | N/A | DOD | Robak et al. [13] |
| 6 mo | |||||||||||||||
| 5 | 69/M | Postchemotherapy for CLL, EBV (+) | Nasopharynx | CLL, bone marrow; cHL, left cervical lymph node | Not detected (CLL and PBL) | R-CHOP and radiation to the nasopharynx | - | - | + | N/A | + | N/A | + | DOD | Foo et al. [14] |
| N/A (cHL and PBL) | 9 mo | ||||||||||||||
| 6 | 37/M | EBV (+) | Urinary bladder | DLBCL, right nasal cavity | Detected | R-CHOP, intrathecal infusions of methotrexate, cytarabine, and hydrocortisone | - | - | + | N/A | N/A | + | N/A | Recurrence of DLBCL, 4 yr | Hashimoto et al. [9] |
| 7 | 84/F | Immunocompetent | Rectum | DLBCL, cecum and appendix vermiformis | Detected | R-CHOP | - | + | - | + | + | + | + | No recurrence, 11 mo | Present case |
PBL, plasmablastic lymphoma; EBER, Epstein-Barr virus–encoded RNA; M, male; HIV, human immunodeficiency virus; CLL, chronic lymphocytic leukemia; N/A, not available; DOD, death of disease; EBV, Epstein-Barr virus; HHV-8, human herpes virus-8; SLL, small lymphocytic lymphoma; Hyper-C-PAD, cyclophosphamide, vincristine, adriamycin, and dexamethasone; R-CHOP, rituximab, cyclophosphamide, doxorubicin, oncovin, and prednisolone; CMV, cytomegarovirus; VAD, vincristine, adriamycin, and dexamethasone; cHL, classical Hodgkin lymphoma; DLBCL, diffuse large B-cell lymphoma.
- 1. Sarode SC, Sarode GS, Patil A. Plasmablastic lymphoma of the oral cavity: a review. Oral Oncol 2010; 46: 146-53. ArticlePubMed
- 2. Campo E, Stein H, Harris NL. Plasmablastic lymphoma. In: Swerdlow SH, Campo E, Harris NL, et al., eds. WHO classification of tumours of haematolymphoid and lymphoid tissues. Lyon: IARC Press, 2017; 321-2.
- 3. Kuppers R. The genomic landscape of HIV-associated plasmablastic lymphoma. Blood Cancer Discov 2020; 1: 23-5. ArticlePubMedPMCPDF
- 4. Garcia-Reyero J, Martinez Magunacelaya N, Gonzalez de Villambrosia S, et al. Genetic lesions in MYC and STAT3 drive oncogenic transcription factor overexpression in plasmablastic lymphoma. Haematologica 2021; 106: 1120-8. ArticlePubMedPDF
- 5. Pather S, Mashele T, Willem P, et al. MYC status in HIV-associated plasmablastic lymphoma: dual-colour CISH, FISH and immunohistochemistry. Histopathology 2021; 79: 86-95. ArticlePubMedPDF
- 6. Marvyin K, Tjonnfjord EB, Breland UM, Tjonnfjord GE. Transformation to plasmablastic lymphoma in CLL upon ibrutinib treatment. BMJ Case Rep 2020; 13: e235816. ArticlePubMedPMC
- 7. Ise M, Kageyama H, Ikebe D, Araki A, Kumagai K, Itami M. Transformation of double-hit follicular lymphoma to plasmablastic lymphoma: a partial role of MYC gene rearrangement. J Clin Exp Hematop 2018; 58: 128-35. PubMedPMC
- 8. Wu JZ, Min K, Fan L, et al. Plasmablastic lymphoma following combination treatment with fludarabine and rituximab for nongastric mucosa-associated lymphoid tissue lymphoma: a case report and review of literature. Int J Clin Exp Pathol 2014; 7: 4400-7. PubMedPMC
- 9. Hashimoto N, Ueda T, Hiraiwa S, Tajiri T, Nakamura N, Yokoyama K. Clonally related plasmablastic lymphoma simultaneously occurring with diffuse large B-cell lymphoma. Case Rep Hematol 2020; 2020: 8876567.ArticlePubMedPMCPDF
- 10. Hatzimichael E, Papathanasiou K, Zerdes I, Flindris S, Papoudou-Bai A, Kapsali E. Plasmablastic lymphoma with coexistence of chronic lymphocytic leukemia in an immunocompetent patient: a case report and mini-review. Case Rep Hematol 2017; 2017: 2861596.ArticlePubMedPMCPDF
- 11. Ronchi A, Marra L, Frigeri F, Botti G, Franco R, De Chiara A. Richter syndrome with plasmablastic lymphoma at primary diagnosis: a case report with a review of the literature. Appl Immunohistochem Mol Morphol 2017; 25: e40-5. ArticlePubMed
- 12. Holderness BM, Malhotra S, Levy NB, Danilov AV. Brentuximab vedotin demonstrates activity in a patient with plasmablastic lymphoma arising from a background of chronic lymphocytic leukemia. J Clin Oncol 2013; 31: e197-9. ArticlePubMed
- 13. Robak T, Urbanska-Rys H, Strzelecka B, et al. Plasmablastic lymphoma in a patient with chronic lymphocytic leukemia heavily pretreated with cladribine (2-CdA): an unusual variant of Richter’s syndrome. Eur J Haematol 2001; 67: 322-7. ArticlePubMedPDF
- 14. Foo WC, Huang Q, Sebastian S, Hutchinson CB, Burchette J, Wang E. Concurrent classical Hodgkin lymphoma and plasmablastic lymphoma in a patient with chronic lymphocytic leukemia/small lymphocytic lymphoma treated with fludarabine: a dimorphic presentation of iatrogenic immunodeficiency-associated lymphoproliferative disorder with evidence suggestive of multiclonal transformability of B cells by Epstein-Barr virus. Hum Pathol 2010; 41: 1802-8. ArticlePubMed
- 15. Castillo JJ, Winer ES, Stachurski D, et al. Prognostic factors in chemotherapy-treated patients with HIV-associated plasmablastic lymphoma. Oncologist 2010; 15: 293-9. ArticlePubMedPMCPDF
- 16. Witte HM, Kunstner A, Hertel N, et al. Integrative genomic and transcriptomic analysis in plasmablastic lymphoma identifies disruption of key regulatory pathways. Blood Adv 2022; 6: 637-51. ArticlePubMedPMCPDF
- 17. Zelenetz AD, Gordon LI, Abramson JS, et al. NCCN Guidelines(R) Insights: B-cell lymphomas, version 6.2023. J Natl Compr Canc Netw 2023; 21: 1118-31. PubMed
- 18. Bailly J, Jenkins N, Chetty D, Mohamed Z, Verburgh ER, Opie JJ. Plasmablastic lymphoma: an update. Int J Lab Hematol 2022; 44 Suppl 1: 54-63. ArticlePubMedPDF
- 19. Guerrero-Garcia TA, Mogollon RJ, Castillo JJ. Bortezomib in plasmablastic lymphoma: a glimpse of hope for a hard-to-treat disease. Leuk Res 2017; 62: 12-6. ArticlePubMed
- 20. Castillo JJ, Guerrero-Garcia T, Baldini F, et al. Bortezomib plus EPOCH is effective as frontline treatment in patients with plasmablastic lymphoma. Br J Haematol 2019; 184: 679-82. ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure



Fig. 1.
Fig. 2.
Fig. 3.
| Case No. | Age (yr)/Sex | Immunological status | Location of PBL | Type and location of other tumors | Same clonality of lymphomas | Chemoradiotherapy | Immunohistochemical analysis of PBL |
Outcome, post diagnosis of PBL | Study | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD20 | CD79a | CD138 | CD38 | MUM1 | MYC | EBER | |||||||||
| 1 | 67/M | Immunocompetent, HIV (–) | Ileocecal valve, left humerus | CLL, bone marrow | N/A | Bortezomib and dexamethasone | - | + | + | + | + | N/A | + | DOD, 2.5 mo | Hatzimichael et al. [10] |
| 2 | 61/M | Immunocompetent, HIV (–), EBV (–), HHV-8 (–) | Lymph node | SLL, the same lymph node as PBL | Detected | Hyper-C-VAD | - | N/A | + | N/A | + | N/A | - | DOD, a couple of months | Ronchi et al. [11] |
| 3 | 48/M | Immunocompetent, HIV (–) | Left supraclavicular area, duodenum | CLL, bone marrow | N/A | R-CHOP, bortezomib, ifosfamide, etoposide, carboplatin, mesna, brentuximab vedotin, and radiation to the neck lesion | N/A | + | + | + | + | N/A | N/A | DOD, N/A | Holderness et al. [12] |
| 4 | 57/F | Postchemotherapy for CLL, HIV (–), CMV IgM (–), CMV IgG (+) | Mandible, bone marrow | CLL, bone marrow | Not detected (different clones) | VAD and CHOP | - | N/A | N/A | N/A | N/A | N/A | N/A | DOD | Robak et al. [13] |
| 6 mo | |||||||||||||||
| 5 | 69/M | Postchemotherapy for CLL, EBV (+) | Nasopharynx | CLL, bone marrow; cHL, left cervical lymph node | Not detected (CLL and PBL) | R-CHOP and radiation to the nasopharynx | - | - | + | N/A | + | N/A | + | DOD | Foo et al. [14] |
| N/A (cHL and PBL) | 9 mo | ||||||||||||||
| 6 | 37/M | EBV (+) | Urinary bladder | DLBCL, right nasal cavity | Detected | R-CHOP, intrathecal infusions of methotrexate, cytarabine, and hydrocortisone | - | - | + | N/A | N/A | + | N/A | Recurrence of DLBCL, 4 yr | Hashimoto et al. [9] |
| 7 | 84/F | Immunocompetent | Rectum | DLBCL, cecum and appendix vermiformis | Detected | R-CHOP | - | + | - | + | + | + | + | No recurrence, 11 mo | Present case |
PBL, plasmablastic lymphoma; EBER, Epstein-Barr virus–encoded RNA; M, male; HIV, human immunodeficiency virus; CLL, chronic lymphocytic leukemia; N/A, not available; DOD, death of disease; EBV, Epstein-Barr virus; HHV-8, human herpes virus-8; SLL, small lymphocytic lymphoma; Hyper-C-PAD, cyclophosphamide, vincristine, adriamycin, and dexamethasone; R-CHOP, rituximab, cyclophosphamide, doxorubicin, oncovin, and prednisolone; CMV, cytomegarovirus; VAD, vincristine, adriamycin, and dexamethasone; cHL, classical Hodgkin lymphoma; DLBCL, diffuse large B-cell lymphoma.

 E-submission
E-submission