Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(4); 2013 > Article
-
Original Article
Bronchial Schwannomas: Clinicopathologic Analysis of 7 Cases - Yoon Yang Jung,, Min Eui Hong, Joungho Han, Tae Sung Kim1, Jhingook Kim2, Young-Mog Shim2, Hojoong Kim3
-
Korean Journal of Pathology 2013;47(4):326-331.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.326
Published online: August 26, 2013
Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
2Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
3Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- Corresponding Author: Joungho Han, M.D. Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 135-710, Korea. Tel: +82-2-3410-2800, Fax: +82-2-3410-0025, hanjho@skku.edu
- *Present address of Yoon Yang Jung. Department of Pathology, Chung-Ang University Hospital, Seoul, Korea
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Tracheal schwannoma: A pseudo-asthmatic syndrome with successful laser Nd-YAG resection as first-line therapy
Ranim Nakhal, Raneem Ahmad, Bassel Ibrahim, Sultaneh Haddad, Arabi Abbas, Nizar Abbas
International Journal of Surgery Case Reports.2025; 134: 111706. CrossRef - CT-Occult Primary Benign Tracheobronchial Neoplasms: A Single-Center 40-Case Clinicopathologic Series
Qiliang Liu, Yan Hu, Minhui Mei, Xuan Wang, Jun Li, Chao Quan, Peng Liu
International Journal of General Medicine.2025; Volume 18: 5765. CrossRef - Outcomes of Different Surgical Approaches in Tracheal Schwannoma: A Narrative Review
Hassan Fahmi Alkhars, Mohammad Almayouf, Majed Albarrak, Faisal Alzahrani, Naif Fnais, Mohammed Alessa, Khalid Alqahtani, Saleh Aldhahri
Ear, Nose & Throat Journal.2025;[Epub] CrossRef - Video-assisted thoracic surgery for an endobronchial ancient schwannoma obstructing the left main bronchus
Jiyeon Kang, Yeon Soo Kim, Ji-Ye Kim
Journal of Surgical Case Reports.2024;[Epub] CrossRef - Interventional treatment of right lower lobe bronchial schwannoma under bronchoscopy: A case report and literature review
Xiyue Li, Ximiao Yu, Ruiqi Luo, Xun Wang
Science Progress.2024;[Epub] CrossRef - Two cases of large tracheobronchial schwannomas completely resected by rigid bronchoscopy with multiple instruments
Changhwan Kim, Hae‐Seong Nam, Yousang Ko
Respirology Case Reports.2023;[Epub] CrossRef - Tracheobronchial schwannoma: a case report and literature review
Guo Lina, Hou Pengguo, Xiao Zhihua, Wang Jianxin, Bai Baoqin, Zhang Mingyue, Sun Junping
Journal of International Medical Research.2023;[Epub] CrossRef - Malignant and Benign Tracheobronchial Neoplasms: Comprehensive Review with Radiologic, Bronchoscopic, and Pathologic Correlation
Francis Girvin, Alexander Phan, Sharon Steinberger, Eugene Shostak, Jamie Bessich, Fang Zhou, Alain Borczuk, Geraldine Brusca-Augello, Margaret Goldberg, Joanna Escalon
RadioGraphics.2023;[Epub] CrossRef - Clinicopathological Characteristics and Pathogenesis of Granular Cell Tumours of the Airways
Jesús Machuca-Aguado, Fernando Cózar-Bernal, Enrique Rodríguez-Zarco, Juan José Ríos-Martin, Miguel Ángel Idoate Gastearena
Journal of Bronchology & Interventional Pulmonology.2023; 30(4): 390. CrossRef - Treatment of primary tracheal schwannoma with endoscopic resection: A case report
Yong-Shuai Shen, Xiang-Dong Tian, Yi Pan, Hua Li
World Journal of Clinical Cases.2022; 10(28): 10279. CrossRef - Primary bronchial schwannoma: A case report
Yosuke Aoyama, Atsushi Miyamoto, Takeshi Fujii, Sakashi Fujimori, Meiyo Tamaoka, Daiya Takai
Medicine.2022; 101(40): e31062. CrossRef - Endobronchial schwannoma in adult: A case report
Touil Imen, Boudaya Mohamed Sadok, Aloui Raoudha, Souhir Ksissa, Brahem Yosra, Ben Attig Yosr, Ksontini Meriem, Bouchareb Soumaya, Keskes Boudawara Nadia, Boussoffara Leila, Knani Jalel
Respiratory Medicine Case Reports.2021; 33: 101396. CrossRef - Primary intratracheal schwannoma misdiagnosed as severe asthma in an adolescent: A case report
Hui-Rong Huang, Pei-Qiang Li, Yi-Xin Wan
World Journal of Clinical Cases.2021; 9(17): 4388. CrossRef - PD‐1/PD‐L1 negative schwannoma mimicking obstructive bronchial malignancy: A case report
Daibing Zhou, Xiaoyan Xing, Jie Fan, Youzhi Zhang, Jie Liu, Yi Gong
Thoracic Cancer.2020; 11(8): 2335. CrossRef - Case report: A tracheobronchial schwannoma in a child
Li Zhang, Wen Tang, Qing-Shan Hong, Pei-feng Lv, Kui-Ming Jiang, Rui Du
Respiratory Medicine Case Reports.2020; 30: 101047. CrossRef - Recurrent transmural tracheal schwannoma resected by video-assisted thoracoscopic window resection
Huiguo Chen, Kai Zhang, Mingjun Bai, Haifeng Li, Jian Zhang, Lijia Gu, Weibin Wu
Medicine.2019; 98(51): e18180. CrossRef - Primary intratracheal schwannoma resected during bronchoscopy using argon plasma coagulation
Purva V Sharma, Yash B Jobanputra, Tatiana Perdomo Miquel, J Ryan Schroeder, Adam Wellikoff
BMJ Case Reports.2018; 2018: bcr-2018-225140. CrossRef - Dumbbell posterior mediastinal schwannoma invading trachea: Multidisciplinary management – weight off the chest
Abhijeet Singh, VallandramamR Pattabhiraman, Arjun Srinivasan, Sivaramakrishnan Mahadevan
Lung India.2018; 35(3): 269. CrossRef - Primary tracheal schwannoma a review of a rare entity: current understanding of management and followup
Shadi Hamouri, Nathan M. Novotny
Journal of Cardiothoracic Surgery.2017;[Epub] CrossRef - A Case of Primary Tracheal Schwannoma
Sung Min Choi, Ji Hong You, Sang Bae Lee, Seong Han Kim, Yon Soo Kim
Kosin Medical Journal.2017; 32(2): 258. CrossRef - Bronchial schwannoma: a singular lesion as a cause of obstructive pneumonia
Rui Caetano Oliveira, Tiago Nogueira, Vítor Sousa, Lina Carvalho
BMJ Case Reports.2016; 2016: bcr2016217300. CrossRef - Endobronchial Neurilemmoma Mimicking a Bronchial Polyp
Ryoung Eun Ko, Seung Yong Park, Yeong Hun Choe, So Ri Kim, Heung Bum Lee, Yong Chul Lee, Seoung Ju Park
Soonchunhyang Medical Science.2015; 21(2): 176. CrossRef - Optimal treatment for primary benign intratracheal schwannoma: A case report and review of the literature
XIAHUI GE, FENGFENG HAN, WENBIN GUAN, JINYUAN SUN, XUEJUN GUO
Oncology Letters.2015; 10(4): 2273. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
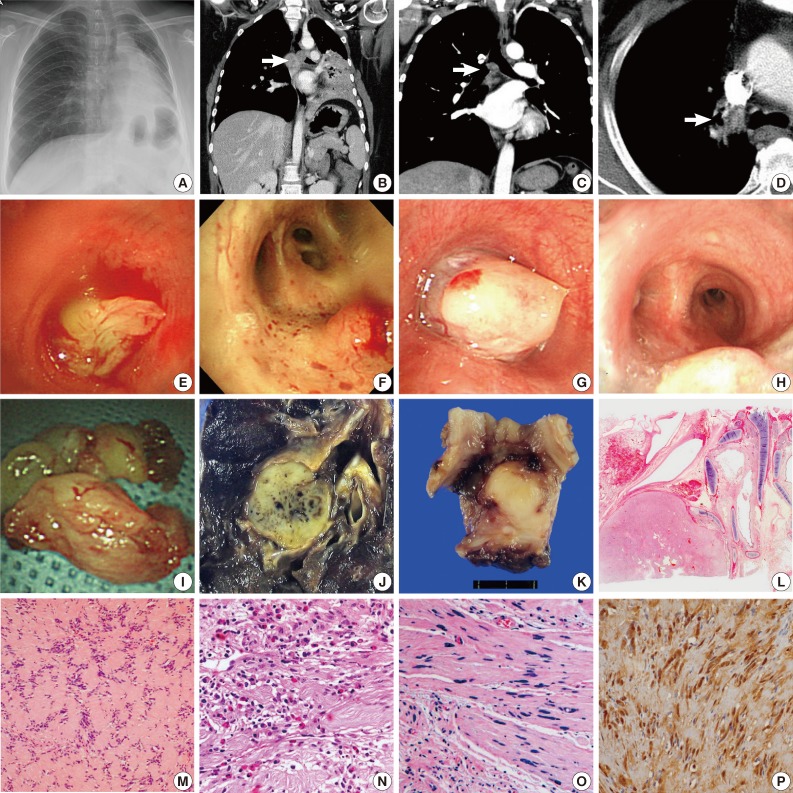
- Figure

Fig. 1
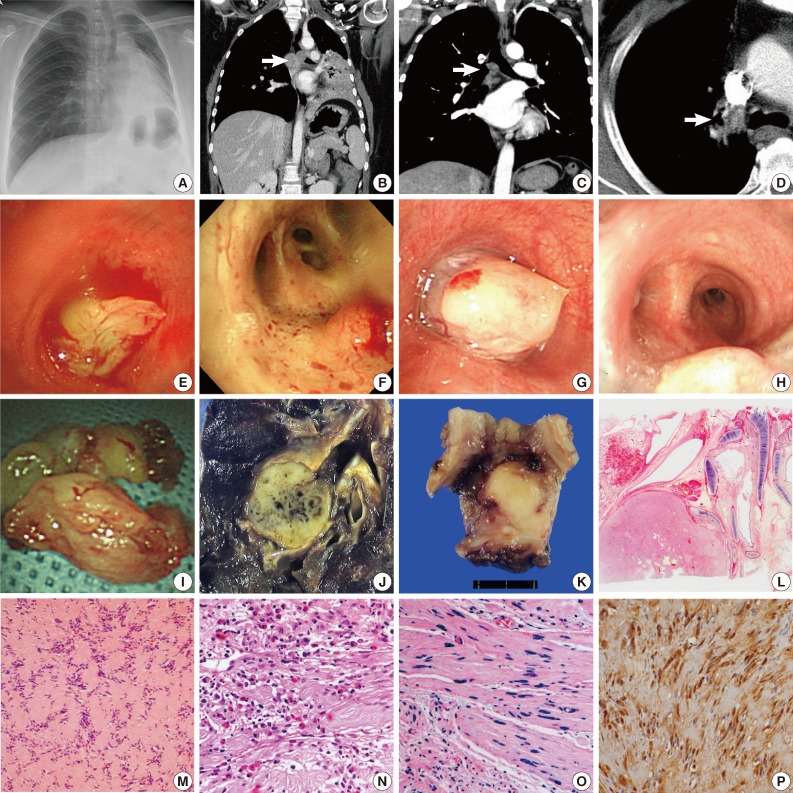
| Case No. | Sex/Age(yr) | Size (cm) | Location | Clinical presentation | Duration of symptom (mo) | Clinical/Radiologic impression (differential diagnosis list) | Bronchoscopic findings | Treatment | Histology |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F/81 | 4.0 | Left main bronchus | Dyspnea | 19 | Tumor, not otherwise specified | Complete narrowing of left main bronchus by lobulated mass | Rigid bronchoscopy for mass removal | |
| 2 | F/52 | 3.0 | Carina | Dyspnea, hemoptysis | 9 | Malignant tumor such as squamous cell carcinoma or carcinoid tumor | Carinal mass with total obstruction of distal trachea and right and left main bronchus | Rigid bronchoscopic tumor removal (initial), surgical resection for recurred tumor | |
| 3 | F/21 | 2.1 | Left main bronchus | Cough, fever | 1 | Adenoid cystic carcinoma, leiomyoma, mucoepidermoid carcinoma, cylindroma, schwannoma | Complete obstruction of proximal left main bronchus by round beefy mass | Bronchoscopic tumor excision | Eosinophilic infiltration |
| 4 | F/50 | 2.8 | Carina and right main bronchus | Recurrent cough, dyspnea | 4 | Metastatic breast cancer (history of breast cancer) | 50% obstruction of distal trachea by white tumor | Rigid bronchoscopic mass excision | Ancient change |
| 5 | F/58 | 1.5 | Bronchus intermedius | Pleuritic chest pain | 2 | Peripheral organizing pneumonia | Well-circumscribed raised lesion on the lateral wall side of bronchus intermedius | Bronchoscopic tumor excision | Ancient change |
| 6 | M/16 | 2.3 | Anterior segmental brochus of left lower lobe | Asymptomatic | - | Atypical carcinoid | Smooth surfaced mass with visible vessels on the surface | Lobectomy, left lower lobe | |
| 7 | M/36 | 3.0 | Right main bronchus | Dyspnea | 7 | Inflammatory pseudotumor (diagnosis of previous biopsy at outside hospital) | Almost complete obstruction of right main bronchus by beefy mass | Bronchoscopic tumor excision |
F, female; M, male.

 E-submission
E-submission