Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(5); 2013 > Article
-
Brief Case Report
Nesidioblastosis and Pancreatic Non-functioning Islet Cell Tumor in an Adult with Type 2 Diabetes Mellitus - Ji Eun Choi, Sang Jae Noh, Jong Jin Sung, Woo Sung Moon
-
Korean Journal of Pathology 2013;47(5):489-491.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.5.489
Published online: October 25, 2013
Department of Pathology, Research Institute for Endocrine Sciences and Research Institute of Clinical Medicine, Chonbuk National University Medical School, Jeonju, Korea.
- Corresponding Author: Woo Sung Moon, M.D. Department of Pathology, Chonbuk National University Medical School, 567 Baekje-daero, Deokjin-gu, Jeonju 561-756, Korea. Tel: +82-63-270-3086, Fax: +82-63-270-3135, mws@chonbuk.ac.kr
• Received: March 4, 2013 • Revised: March 26, 2013 • Accepted: March 27, 2013
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
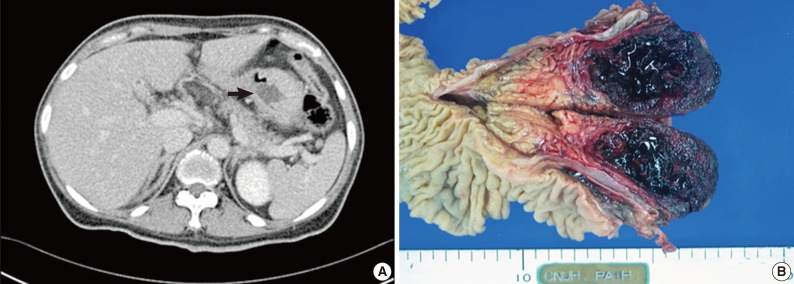
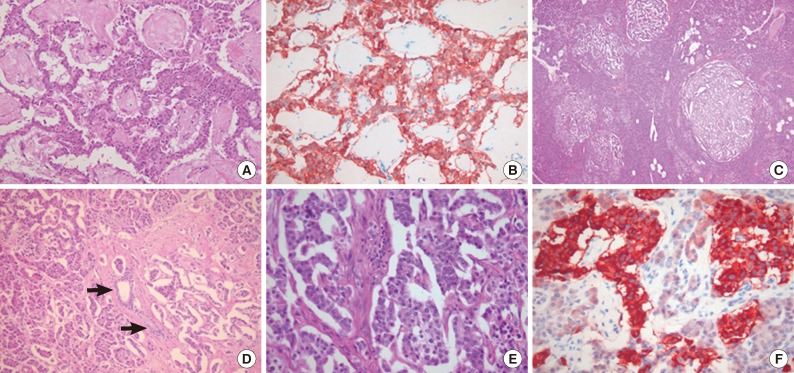
- A 43-year-old woman was hospitalized due to fever and right flank pain with a 2-year history of type 2 DM treated with oral hypoglycemic agents. Physical examination indicated right flank knocking tenderness. All laboratory findings were within normal limits, except for an increased white blood cell count in blood and urine, and elevated blood sugar level (201 mg/dL). Abdominal computed tomography showed a right ureteral stone with pyelonephritis. A 3.6 cm-sized cystic lesion in the pancreatic head was found incidentally (Fig. 1A). After treating the pyelonephritis, the patient underwent a pylorus-preserving pancreatico-duodenectomy and double Roux-en-Y reconstruction based on a pancreatic cystic tumor, such as a solid pseudopapillary neoplasm or serous cystadenoma. Grossly, the cut surface of the pancreas head revealed a well-demarcated, solitary cystic mass that measured 5.6×3.7 cm and was dark red in color, with a soft cut surface and extensive hemorrhage (Fig. 1B). On serial-sectioning, adjacent non-tumor pancreatic tissue appeared normal in gross examination. Histologically, the pancreatic mass was surrounded by a fibrous capsule consisting of nests or trabecular cords of neoplastic cells with extensive hemorrhage and coagulation necrosis (Fig. 2A). The neoplastic cells were relatively uniform, with round or irregular nuclei and abundant eosinophilic cytoplasm, and revealed a centrally located round to oval nucleus. The chromatin pattern was characteristically coarsely clumped. Mitoses were very difficult to find. Lymphovascular invasion of the tumor cells was not observed. The neoplastic cells stained diffusely positive for synaptophysin and chromogranin (Fig. 2B), but were negative for insulin and glucagon. The proliferation index was very low on the Ki-67 immunohistochemistry stain. Based on the histological and immunohistochemical findings, the tumor was diagnosed as a non-functioning pancreatic neuroendocrine tumor. There were a number of irregularly distributed hyperplastic islets throughout the uninvolved pancreatic parenchyma, and their contour and size were markedly variable (Fig. 2C). Many islets were closely associated with pancreatic duct structures (Fig. 2D). Hyperplastic islets were characterized by the presence of islet cells showing enlarged hyperchromatic nuclei with pleomorphism (Fig. 2E). The majority of these dysplastic islet cells were positive for insulin, but negative for glucagon (Fig. 2F). The histology of the non-tumoral pancreatic tissue was compatible with diffuse nesidioblastosis. She remained free of any sign of recurrent tumor and her diabetic symptoms were controlled with oral hypoglycemic drugs for 40 months after surgery.
CASE REPORT
- Nesidioblastosis is a hyperfunctional disorder of pancreatic insulin-producing cells characterized by hypertrophic β cells, which are present in enlarged or normal-appearing islets.1 The morphological criteria for establishing its diagnosis are the presence of variable-sized islets, often with somewhat irregular outlines, and irregular and poorly-defined endocrine cell clusters scattered in the acinar parenchyma and often intimately connected with small or large ducts. Another feature is distinct islet cell hypertrophy with nuclear enlargement, which often results in the presence of giant and bizarre nuclei.1,3-5 Nesidioblastosis is the most common cause of persistent neonatal hypoglycemia, but it is rare in adults.1,3-7 Since adult nesidioblastosis was first reported in 1980,4 a few cases have been reported in association with pancreatic tumors.3,6 A previous study demonstrated that mice carrying a Moloney murine sarcoma virus-simian virus 40 large T transgene develop nesidioblastosis and islet cell proliferation and finally progress to pancreatic neuroendocrine tumors.2 A patient with a spectrum ranging from nesidioblastosis and islet cell hyperplasia of the pancreas to multiple adenomas with metastases has been reported, suggesting the association of nesidioblastosis with proliferative and neoplastic conditions.4 Islet cell tumors associated with nesidioblastosis are usually insulinoma,2,4 and only a few cases of non-functioning islet cell tumors associated with nesidioblastosis have been reported, as in our case.3,6 Similarly, among 23 developed pancreatic tumors in transgenic mice, 91% of the tumors were insulinoma, and one was a non-functioning neuroendocrine tumor, based on immunohistochemical stain.2
- Sporadic hyperinsulinemic hypoglycemia is the main clinical feature of nesidioblastosis and almost all cases have been detected because of hypoglycemia-related symptoms.1,3-5 However, our case had no symptoms of sporadic hyperinsulinemic hypoglycemia. The pathogenesis of nesidioblastosis and its significance in DM in adults remain elusive. Nesidioblastosis in adults could be a genetic defect like in neonates or a reactive process that occurs in response to metabolic and hormonal changes.7 Indeed, the histologic features of nesidioblastosis also occur in several conditions, such as chronic pancreatitis, in states of insulin resistance, and after gastric-bypass surgery in patients with morbid obesity, all of which are associated with diabetes.7-9 Increased production of a β cell trophic peptide, including insulin-like growth factor (IGF) 2, IGF 1 receptor-α, and transforming growth factor-β receptor 3, may contribute to the development of postgastric bypass nesidioblastosis in adults.9 In fact, there are reported cases of nesidioblastosis associated with pre-existing diabetes in adults.8,10 We speculate that islet hyperplasia and nesidioblastosis in diabetic patients could be a reactive process, reflecting a compensating mechanism for β cell destruction or functional insufficiency.
DISCUSSION
- 1. Kaczirek K, Niederle B. Nesidioblastosis: an old term and a new understanding. World J Surg 2004; 28: 1227-1230. ArticlePubMedPDF
- 2. Gotz W, Schucht C, Roth J, Theuring F, Herken R. Endocrine pancreatic tumors in MSV-SV40 large T transgenic mice. Am J Pathol 1993; 142: 1493-1503. PubMedPMC
- 3. Zhao X, Stabile BE, Mo J, Wang J, French SW. Nesidioblastosis coexisting with islet cell tumor and intraductal papillary mucinous hyperplasia. Arch Pathol Lab Med 2001; 125: 1344-1347. ArticlePubMedPDF
- 4. Leong AS, Slavotinek AH, Higgins BA. Nesidioblastosis, islet cell hyperplasia, and adenomatosis in a case of metastasizing insulinoma: contribution to the genesis of the islets of Langerhans. Diabetes Care 1980; 3: 537-542. ArticlePubMedPDF
- 5. Jabri AL, Bayard C. Nesidioblastosis associated with hyperinsulinemic hypoglycemia in adults: review of the literature. Eur J Intern Med 2004; 15: 407-410. ArticlePubMed
- 6. Yu R, Nissen NN, Dhall D, Heaney AP. Nesidioblastosis and hyperplasia of alpha cells, microglucagonoma, and nonfunctioning islet cell tumor of the pancreas: review of the literature. Pancreas 2008; 36: 428-431. PubMed
- 7. Klöppel G, Anlauf M, Raffel A, Perren A, Knoefel WT. Adult diffuse nesidioblastosis: genetically or environmentally induced? Hum Pathol 2008; 39: 3-8. ArticlePubMed
- 8. Kon YC, Loh KC, Chew SP, et al. Hypoglycaemia from islet cell hyperplasia and nesidioblastosis in a patient with type 2 diabetes mellitus: a case report. Ann Acad Med Singapore 2000; 29: 682-687. PubMed
- 9. Rumilla KM, Erickson LA, Service FJ, et al. Hyperinsulinemic hypoglycemia with nesidioblastosis: histologic features and growth factor expression. Mod Pathol 2009; 22: 239-245. ArticlePubMedPDF
- 10. Raffel A, Anlauf M, Hosch SB, et al. Hyperinsulinemic hypoglycemia due to adult nesidioblastosis in insulin-dependent diabetes. World J Gastroenterol 2006; 12: 7221-7224. ArticlePubMedPMC
REFERENCES
Fig. 1(A) An abdominal computed tomography scan reveals a cystic lesion in the pancreatic head (arrow). (B) The cut surface of the pancreas shows a well-circumscribed, dark red color, soft mass with extensive hemorrhage.
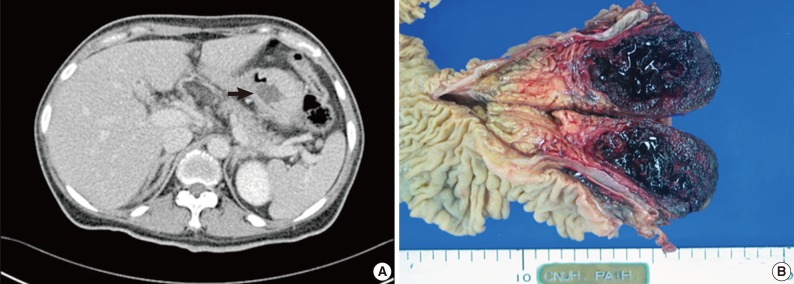
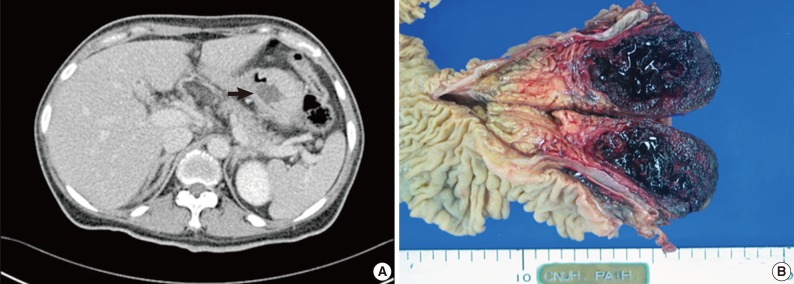
Fig. 2(A) The tumor is composed of cells showing neuroendocrine features. (B) The tumor cells that show neuroendocrine features are positive for neuroendocrine markers (chromogranin). (C) Low-power magnification of pancreatic tissue shows an increased number of irregular-shaped hyperplastic islets scattered randomly in the pancreas. (D) Irregular-shaped islets in close approximation to pancreatic exocrine ductal structures (arrows). (E) The hyperplastic islets contain cells with enlarged hyperchromatic nuclei and of different sizes. (F) Approximately half of cells within the hyperplastic islets are stained with insulin.
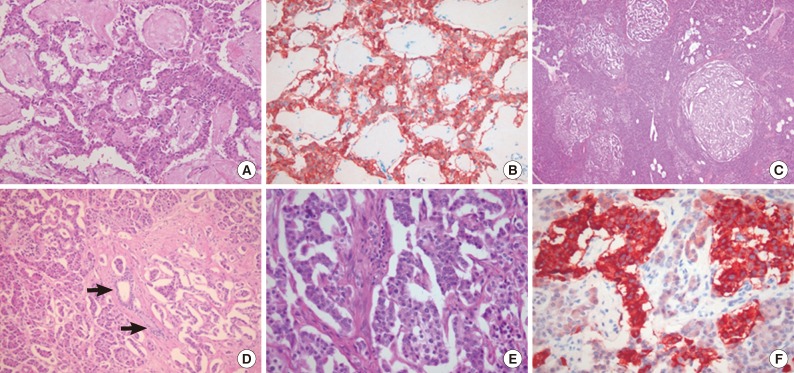
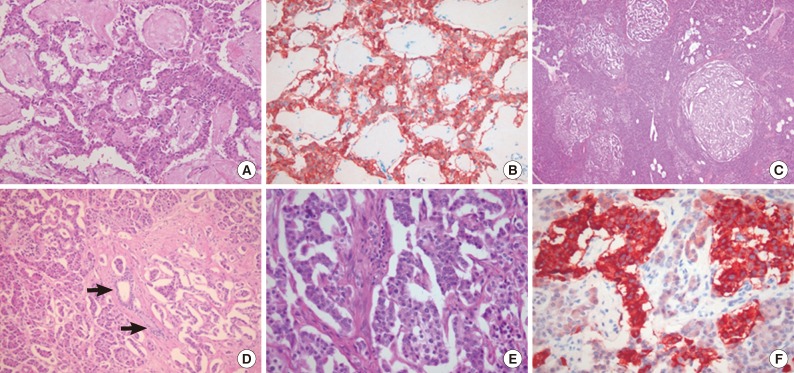
Figure & Data
References
Citations
Citations to this article as recorded by 

- Diffuse, Adult-Onset Nesidioblastosis/Non-Insulinoma Pancreatogenous Hypoglycemia Syndrome (NIPHS): Review of the Literature of a Rare Cause of Hyperinsulinemic Hypoglycemia
Martin Philipp Dieterle, Ayman Husari, Sophie Nicole Prozmann, Hendrik Wiethoff, Albrecht Stenzinger, Manuel Röhrich, Uwe Pfeiffer, Wolfgang Rüdiger Kießling, Helena Engel, Harald Sourij, Thorsten Steinberg, Pascal Tomakidi, Stefan Kopf, Julia Szendroedi
Biomedicines.2023; 11(6): 1732. CrossRef - Postprandial hypoglycemia after upper gastrointestinal tract surgery: prevalence and pathophysiology (part 1)
M. Yu. Yukina, M. O. Chernova, E. A. Troshina, V. V. Evdoshenko, N. M. Platonova
Almanac of Clinical Medicine.2021; 49(4): 285. CrossRef - Nésidioblastose traitée par pasiréotide LAR : à propos d’un cas
Alexia Rouland, Benjamin Bouillet, Pauline Legris, Isabelle Simoneau, Jean-Michel Petit, Bruno Vergès
Médecine des Maladies Métaboliques.2021; 15(6): 619. CrossRef - Concurrent Adult-Onset Diffuse β-Cell Nesidioblastosis and Pancreatic Neuroendocrine Tumor: A Case Report and Review of the Literature
Mushfig Orujov, Keith K. Lai, Catherine L. Forse
International Journal of Surgical Pathology.2019; 27(8): 912. CrossRef - Nesidioblastosis in an Adult with Short Gut Syndrome and Type 2 Diabetes
Mimi Wong, Luke Conway, Caroline Cooper, Ashim Sinha, Nirjhar Nandi
AACE Clinical Case Reports.2019; 5(6): e375. CrossRef - Superimposed effect of ovariectomy on type 2 diabetes mellitus in Wistar rats
Minerva K. Fahmy, Hayam G. Sayyed, Eman A. Abd Elrahim, Rana T.A. Farag
Alexandria Journal of Medicine.2018; 54(2): 129. CrossRef - Diagnostic Performance of 48-Hour Fasting Test and Insulin Surrogates in Patients With Suspected Insulinoma
Keijiro Ueda, Ken Kawabe, Lingaku Lee, Yuichi Tachibana, Nao Fujimori, Hisato Igarashi, Yoshinao Oda, Robert T. Jensen, Ryoichi Takayanagi, Tetsuhide Ito
Pancreas.2017; 46(4): 476. CrossRef - Nesidioblastosis (diagnosis, surgical treatment)
A. G. Kriger, A. V. Smirnov, D. V. Kalinin, A. V. Glotov, S. V. Berelavichus, G. I. Konyaeva, A. N. Lebedeva, N. A. Karel’skaya, V. N. Tsygankov
Khirurgiya. Zhurnal im. N.I. Pirogova.2015; (10): 16. CrossRef - A Rare Complication of Gastric Bypass (Weight Loss) Surgery
Betül Ünal, Özlem Ceren Uzun, Cumhur İbrahim Başsorgun, Okan Erdoğan, Gülsüm Özlem Elpek
International Journal of Surgical Pathology.2015; 23(1): 68. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Nesidioblastosis and Pancreatic Non-functioning Islet Cell Tumor in an Adult with Type 2 Diabetes Mellitus


Fig. 1 (A) An abdominal computed tomography scan reveals a cystic lesion in the pancreatic head (arrow). (B) The cut surface of the pancreas shows a well-circumscribed, dark red color, soft mass with extensive hemorrhage.
Fig. 2 (A) The tumor is composed of cells showing neuroendocrine features. (B) The tumor cells that show neuroendocrine features are positive for neuroendocrine markers (chromogranin). (C) Low-power magnification of pancreatic tissue shows an increased number of irregular-shaped hyperplastic islets scattered randomly in the pancreas. (D) Irregular-shaped islets in close approximation to pancreatic exocrine ductal structures (arrows). (E) The hyperplastic islets contain cells with enlarged hyperchromatic nuclei and of different sizes. (F) Approximately half of cells within the hyperplastic islets are stained with insulin.
Fig. 1
Fig. 2
Nesidioblastosis and Pancreatic Non-functioning Islet Cell Tumor in an Adult with Type 2 Diabetes Mellitus

 E-submission
E-submission