Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(4); 2014 > Article
-
Brief Case Report
Inflammatory Myofibroblastic Tumor of the Thyroid Gland: A Brief Case Report - Hye Jeong Kim, Jong In Na, Ji Shin Lee, Dong Hyeok Cho1, Jin Seong Cho2
-
Korean Journal of Pathology 2014;48(4):319-322.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.4.319
Published online: August 26, 2014
Department of Pathology, Chonnam National University Medical School, Gwangju, Korea.
1Department of Internal Medicine, Chonnam National University Medical School, Gwangju, Korea.
2Department of Surgery, Chonnam National University Medical School, Gwangju, Korea.
- Corresponding Author: Ji Shin Lee, M.D. Department of Pathology, Chonnam National University Hwasun Hospital, 322 Seoyang-ro, Hwasun 519-763, Korea. Tel: +82-61-379-7050, Fax: +82-61-379-7099, jshinlee@hanmail.net
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Novel ALK gene mutation in inflammatory myofibroblastic tumor of the thyroid: a case report
Yang Guangxu, Li Yao, Xie Jing, Liu Hongsheng
Frontiers in Oncology.2025;[Epub] CrossRef - Inflammatory myofibroblastic tumor of the thyroid gland
Yiyang Zhang, Jia Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - ALK-1-positive inflammatory myofibroblastic tumor of the thyroid complicated by Hashimoto’s thyroiditis: report of a rare case and a literature review
Cheng-fang Li, Xing-long Wu, Jin-jing Wang, Kai Wang, Su-yuan Zhang, Jia-jia Huang, Han-zhong Hu, Hong Zheng
Diagnostic Pathology.2020;[Epub] CrossRef - Plasma Cell Granuloma of the Thyroid: Review of an Uncommon Entity
Pallavi A. Patil, Ronald A. DeLellis
Archives of Pathology & Laboratory Medicine.2018; 142(8): 998. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles



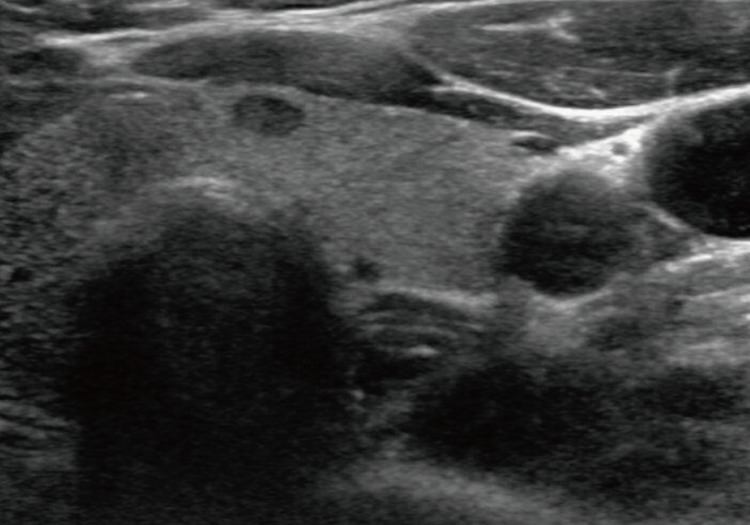
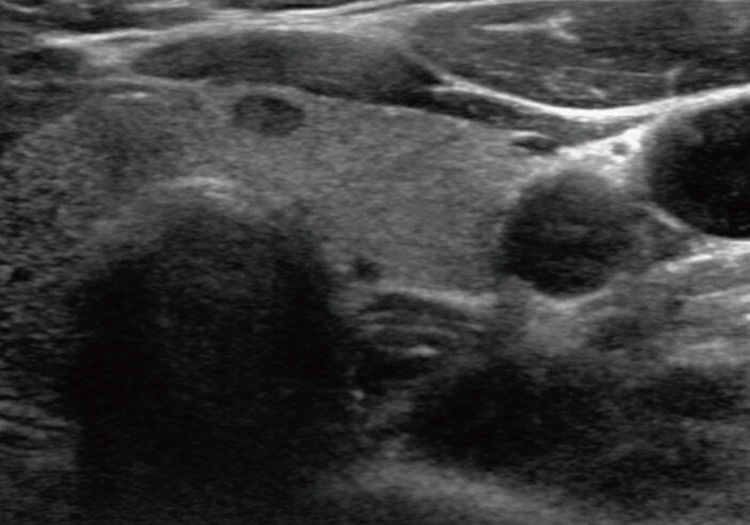
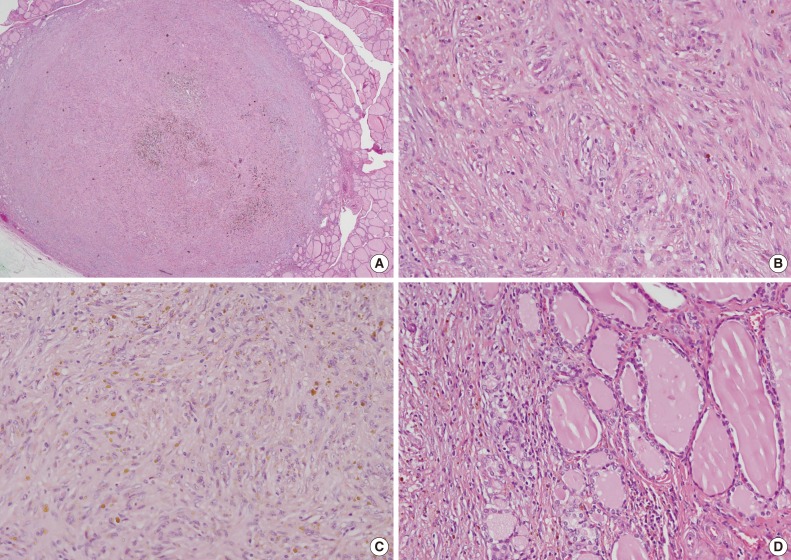
Fig. 1
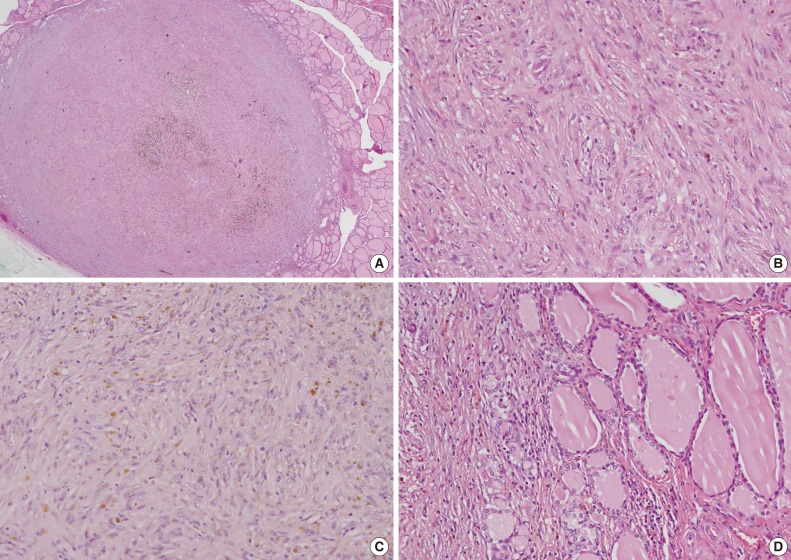
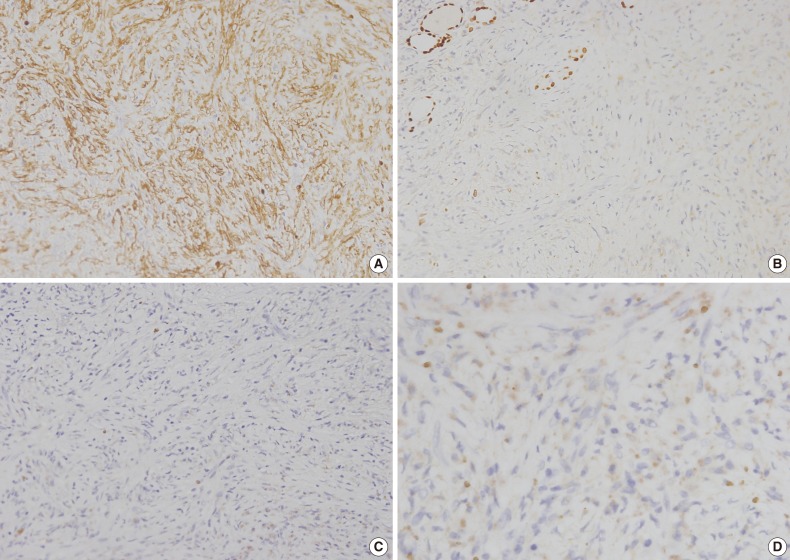
Fig. 2
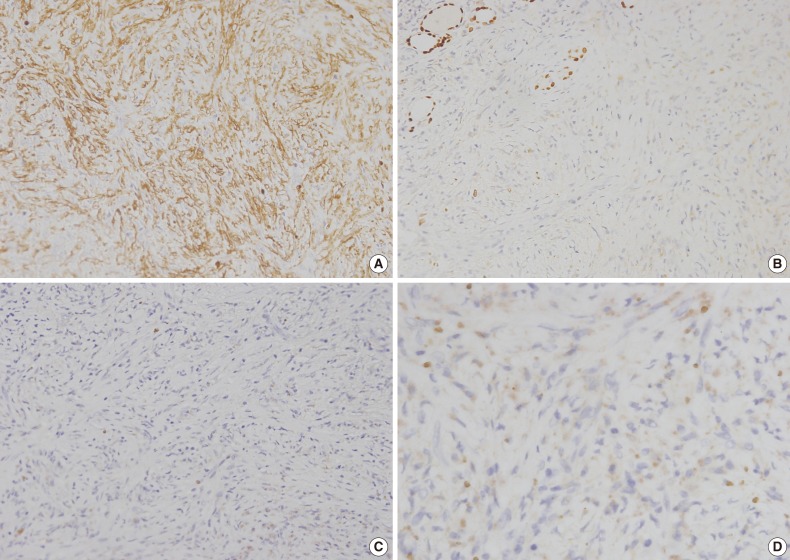
Fig. 3
| Age (yr)/Gender | Histology | Clinical presentation | HT | ALK | Reference | |
|---|---|---|---|---|---|---|
| 1 | 70/F | PCG | 3-cm nodule, difficult breathing | – | NA | - |
| 2 | 61/F | PCG | Symmetric goiter | – | NA | - |
| 3 | 35/F | PCG | 3-cm nodule, trachea compression | – | NA | - |
| 4 | 51/F | PCG | 5-cm painful nodule | – | NA | - |
| 5 | 55/F | PCG | 2.2-cm nodule | – | NA | - |
| 6 | 65/F | PCG | Dyspnea, 5-cm nodule | + | NA | - |
| 7 | 29/M | PCG | Tiredness, fever, sore throat, painful 8-cm nodule, dysphagia | – | NA | - |
| 8 | 46/F | PCG | Asymptomatic neck mass | – | Negative | - |
| 9 | 46/M | PCG | Goiter with dominant left lobe nodule | + | NA | - |
| 10 | 35/F | PCG | Rapid thyroid enlargement with tracheal compression | + | NA | - |
| 11 | 41/M | PCG | Enlarging neck mass, dysphonia, anorexia, weight loss | + | NA | - |
| 12 | 50/M | PCG | Goiter, feeling of narrowness in the neck | + | NA | - |
| 13 | 65/M | PCG | Goiter, large painless neck mass; progressively growing neck mass | – | Negative | - |
| 14 | 44/F | PCG | + | |||
| 15 | 55/F | PCG | Enlarging goiter | + | NA | - |
| 16 | 18/F | IMT | 3-cm firm nodule right lobe | – | Negative | Trimeche et al. [3] |
| 17 | 75/F | IMT | 1.5-cm painless nodule left lobe | – | Negative | Kojima et al. [4] |
| 18 | 89/F | PCG | Large firm irregular mass left lobe | + | NA | Barber et al. [5] |
| 19 | 47/F | PCG | Subhyoid mass, subtotal thyroidectomy 20 years ago | + | NA | Cremonini et al. [2] |
| 20 | 50/F | IMT | 0.6-cm thyroid mass | – | Negative | Present case |
Other reports not sited in this table are based on Cremonini HT, hashimoto’s thyroiditis; ALK, anaplastic lymphoma kinase; F, female; PCG, plasma cell granuloma; NA, not available; M, male; IMT, inflammatory myofibroblastic tumor.

 E-submission
E-submission