Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(6); 2014 > Article
-
Brief Case Report
Periductal Stromal Tumor of Breast: A Case Report and A Review of Literature - Salma L. Abbasi, Kate McNamara1, Mohammed S. Absar1, Alison Darlington2, Francene Clucas2, Sami Titi
-
Korean Journal of Pathology 2014;48(6):442-444.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.6.442
Published online: December 31, 2014
Department of Pathology, The Royal Oldham Hospital, Oldham, UK
1Breast Unit, North Manchester General Hospital, Manchester, UK
2Department of Radiology, North Manchester General Hospital, Manchester, UK
- Corresponding Author: Salma L. Abbasi, M.B.B.S., M.Phil. Department of Histopathology, The Royal Oldham Hospital, Oldham OL1 2JH, UK Tel: +44-161-6561768, Fax: +44-161-6278745, E-mail: salma.abbasi@pat.nhs.uk
• Received: May 22, 2013 • Revised: September 5, 2014 • Accepted: September 16, 2014
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
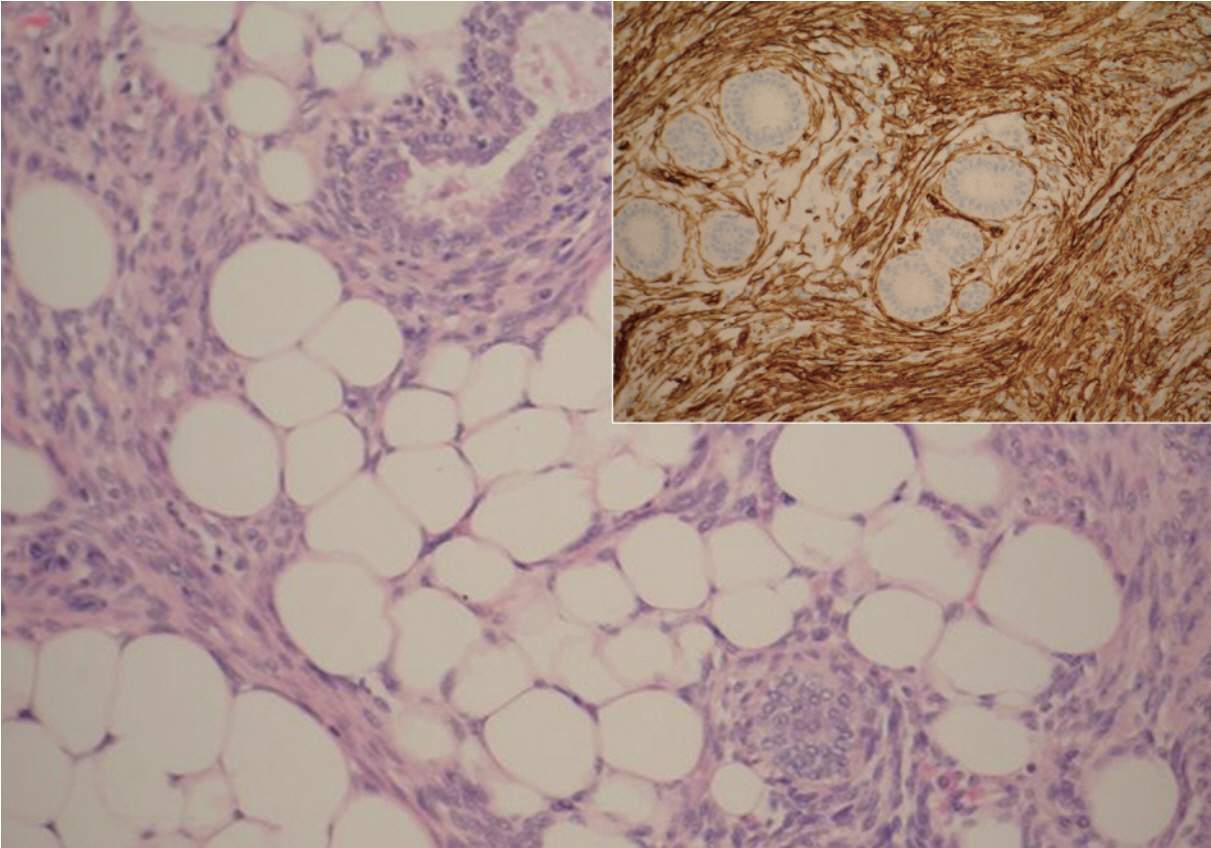
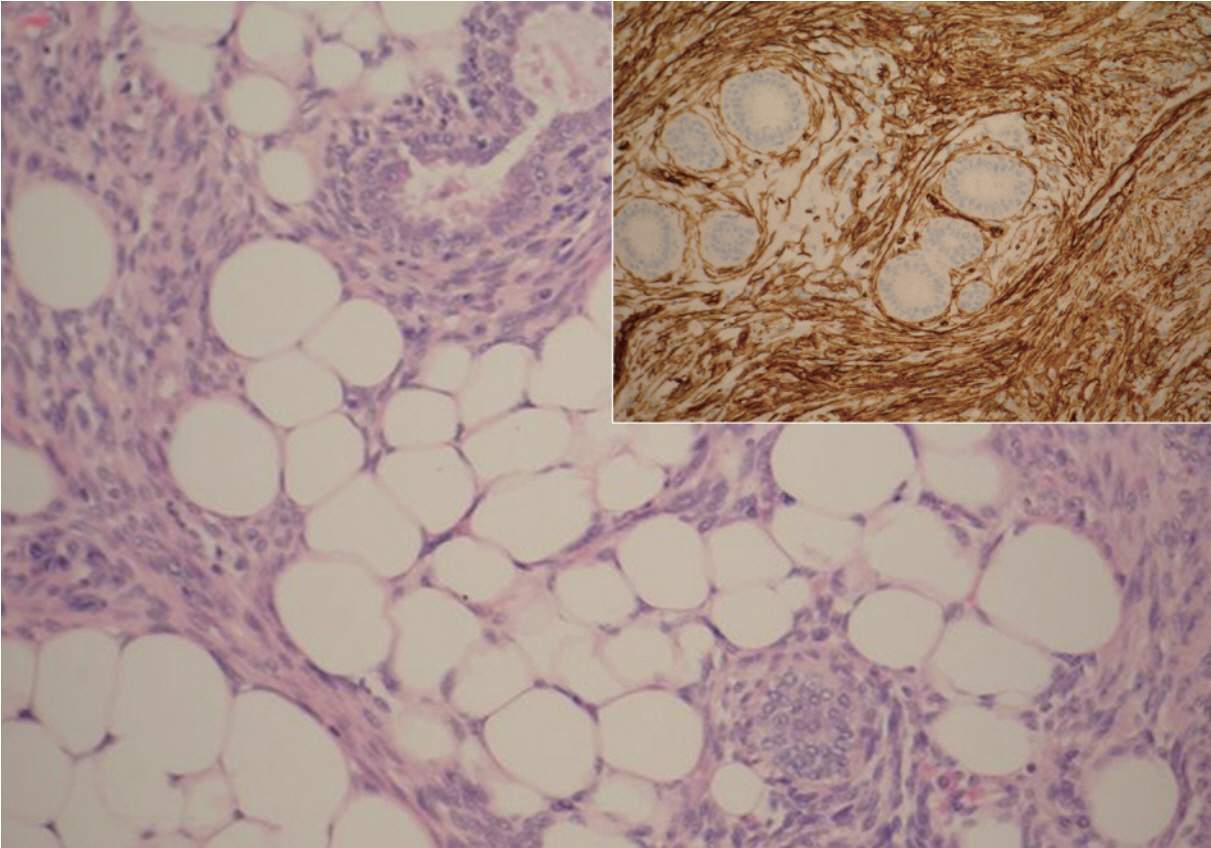
- A 20-year-old female was referred to the breast unit due to a lump in her left breast that had increased in size. On physical examination the tumor was in the 3 o’clock position, well circumscribed, mobile, and non-tender. The patient had no previous history of breast disease herself, or within her family. She underwent an ultrasound scan (USS), which revealed a subtle hypoechoic lesion measuring 17×14×10 mm, and had an appearance consistent with fibroadenoma. Fine needle aspiration yielded a C2 benign result with no evidence of atypia. Due to the small size of the lesion and benign cytological diagnosis, the patient was discharged. Eighteen months later she presented again with the same lesion, which had now doubled in size and had become painful. A further USS was carried out which demonstrated that the lesion was still consistent with fibroadenoma and now measured 38×37×19 mm. Due to its rapid growth, excision of the lesion was performed. Macroscopically, the breast lump measured 45 mm in diameter and was poorly circumscribed, exhibiting a yellow and white cut surface. Microscopic examination revealed biphasic proliferation that comprised epithelial and mesenchymal components. The epithelial components composed of benign epithelial ducts but without a leaf-like configuration and were surrounded by mild-to-moderate atypical spindle cells, which infiltrated adjacent adipose tissue in a nodular pattern (Fig. 1). The tumor appeared to be focally present at the inked surgical margin. Stromal overgrowth, variable stromal cellularity, and myxoid background were observed, and the mitotic count was 3/10 high power field in stromal cells (Figs. 2, 3). There were foci of chronic inflammation along with lymphoid aggregates and germinal center formation. Immunocytochemical analysis showed that the neoplastic cells were CD34 positive (Fig. 2) and Ki-67 (a proliferative marker) was 5% to 10%. The tumor was negative for S100, estrogen receptor (ER), progesterone receptor (PR), MNF116, BCL2, β-catenin, AE1/AE3, cytokeratin 5/6, smooth muscle actin (SMA), desmin, and CD117. This immunoprofile together with histomorphology results confirmed the diagnosis of PDST. No adjuvant treatment was administered, but re-excision of the cavity was performed due to the positive surgical margin, and was free from tumor on subsequent histology examination. During a follow-up period of 12 months, USS showed a well-circumscribed lesion (U2) and a normal/benign (B1/B2) histological diagnosis was made after two further core biopsies. The patient has not shown any symptoms or signs of local or distant recurrence for approximately 38 months.
CASE REPORT
- PDST is a biphasic tumor of the breast characterized by proliferation of spindle cells surrounding benign ductal elements and infiltrating surrounding fatty tissue [1,2]. PDST is the preferred ‘neutral’ term for this entity [2], which most commonly occurs in adult women, usually perimenopausal or postmenopausal; however, it has also been described in a 14-year-old boy [3]. PDST on gross examination usually appears as an ill-defined white/grey or yellow mass. There may also be minute, scattered cysts. Our patient was a 20-year-old female with no previous history of breast disease. The breast lesion in the current case was poorly circumscribed with a solid, yellow/white cut surface, but no cystic changes were observed.
- Microscopically PDST is composed of periductal spindle cell proliferation of variable cellularity and atypia around open ducts that lacks the leaf-like pattern typical of phyllodes tumors [1]. There are usually multiple nodules, often separated by fat. The main differential diagnosis includes phyllodes tumor, myxoid fibroadenoma, low-grade sarcoma, and fibromatosis. We used the criteria established by the Armed Forces Institute of Pathology (AFIP) of PDST: 1) a predominantly spindle-cell stromal proliferation of variable cellularity and atypia around open tubules and ducts devoid of a phyllodes pattern; 2) one or, more often, multiple nodules separated by adipose tissue; 3) stromal mitotic activity of ≥3/10 high-power fields; and 4) infiltration into surrounding mammary fibroadipose tissue [1]. The use of extensive tumor sampling and a broad panel of immunocytochemistry may help to establish the final diagnosis [4,5]. PDST is positive for CD34, some cases have been reported to be positive for CD117 and very few were positive for actin (HHF35), while it is negative for ER and PR. In the current case, stromal cells were diffusely positive for CD34, but negative for CD117, SMA, ER, and PR. The lack of the leaf-like architecture typical of phyllodes tumors is the main feature distinguishing PDST, as both lesions can have a similar immunoprofile. The characteristic pattern of atypical spindle cell proliferation around the open ducts can easily discriminate PDST from other lesions like myxoid fibroadenoma, low-grade sarcoma, and fibromatosis. β-Catenin is also often positive in fibromatosis and negative in PDST.
- PDST is a low-grade malignancy of intermediate behavior that may progress to phyllodes tumor or another form of soft-tissue sarcoma [1,5]. The number of reported cases of PDST in the literature is limited; hence, the optimal means of management and prognosis have yet to be accurately established. The main therapeutic management of PDST is based on wide local excision with free surgical margins; neither axillary clearance nor adjuvant therapy is required [1]. In one series, 2 of 10 women experienced either recurrence or metastases within 12 months: one of these women had local recurrence with leaf-like formations, suggesting progression to a phyllodes tumor [6]. In our case the patient was treated with surgical resection and has been recurrence-free approximately 38 months. PDST may occasionally exhibit intraepithelial changes ranging from hyperplasia to intraductal carcinoma, and therefore close follow-up has been recommended [1,4]. The epithelial component in the current tumor demonstrated usual epithelial hyperplasia and there was no evidence of ductal carcinoma in situ or invasive carcinoma. Complete excision with tumor-free margins is the current recommended treatment; however, there has been little clinical experience of this disease and, hence, its management remains controversial. The prognosis in patients with PDST is unclear; thus, more studies with longer follow-up of patients are needed to determine the optimal management and the clinical behavior of this unusual breast neoplasm.
DISCUSSION
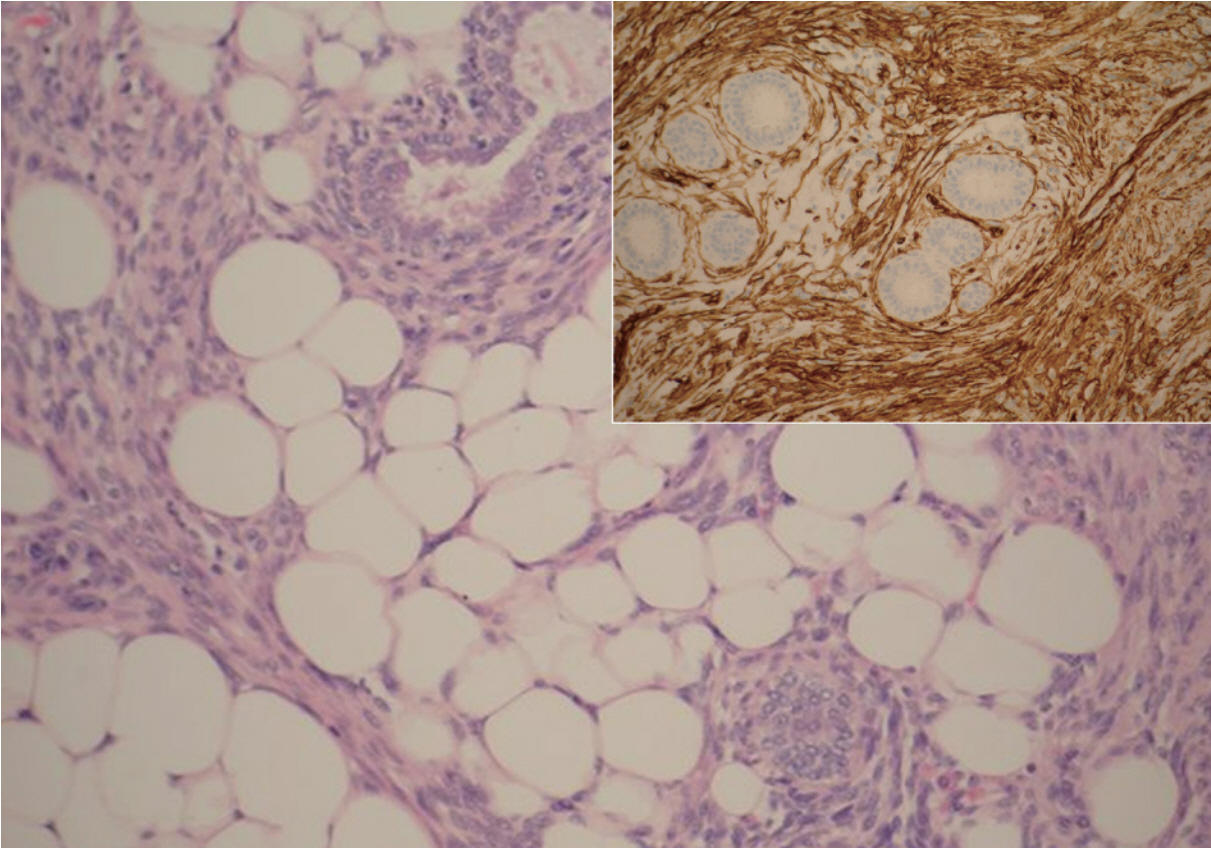
Fig. 2.Periductal stromal tumor exhibiting benign ducts surrounded by atypical spindle cells, which appear to infiltrate adjacent adipose tissue. The spindle cells are diffusely positive for CD34 (inset).
- 1. Burga AM, Tavassoli FA. Periductal stromal tumor: a rare lesion with low-grade sarcomatous behavior. Am J Surg Pathol 2003; 27: 343-8. PubMed
- 2. Lakhani SR, Ellis IO, Schnitt SJ, et al. Phyllodes tumors. WHO classification of tumors of the breast. Lyon: IARC Press, 2012; 145.
- 3. Masbah O, Lalya I, Mellas N, et al. Periductal stromal sarcoma in a child: a case report. J Med Case Rep 2011; 5: 249.ArticlePubMedPMCPDF
- 4. Tomas D, Janković D, Marusić Z, Franceschi A, Mijić A, Kruslin B. Low-grade periductal stromal sarcoma of the breast with myxoid features: immunohistochemistry. Pathol Int 2009; 59: 588-91. ArticlePubMed
- 5. Chen CM, Chen CJ, Chang CL, Shyu JS, Hsieh HF, Harn HJ. CD34, CD117, and actin expression in phyllodes tumor of the breast. J Surg Res 2000; 94: 84-91. ArticlePubMed
- 6. Rao AC, Geetha V, Khurana A. Periductal stromal sarcoma of breast with lipoblast-like cells: a case report with review of literature. Indian J Pathol Microbiol 2008; 51: 252-4. ArticlePubMed
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Genetic profiling of mammary periductal stromal tumors with histologic correlation highlights high-grade and low-grade groups and similarities to phyllodes tumors
Gregor Krings, Gregory R. Bean, Elizabeth M. Hosfield, J.J. Rowe, Joseph Geradts, Yunn-Yi Chen
Modern Pathology.2026; : 100961. CrossRef - Survey of recurrent diagnostic challenges in breast phyllodes tumours
Benjamin Yongcheng Tan, Stephen B Fox, Sunil R Lakhani, Puay Hoon Tan
Histopathology.2023; 82(1): 95. CrossRef - Management of a periductal stromal tumor in a young woman: Our breast unit experience
Irene Valente, Adela Ristani, Cristina Mancini, Eugenia Martella, Leonardo Quartieri, Cecilia D'Aloia
The Breast Journal.2020; 26(7): 1375. CrossRef - A Diagnostic Approach to Fibroepithelial Breast Lesions
Benjamin Yongcheng Tan, Puay Hoon Tan
Surgical Pathology Clinics.2018; 11(1): 17. CrossRef - A case of local recurrence of periductal stromal sarcoma of the breast
Kana TERAMOTO, Yasuro DOI, Kayo YAMAMOTO, Kaname MATSUKAWA, Hisaka IWAIHARA, Rumi MOTOSHIMA, Noboru TAKATA, Ichiro YOSHINAKA, Kazunori HARADA
Choonpa Igaku.2018; 45(1): 61. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Periductal Stromal Tumor of Breast: A Case Report and A Review of Literature



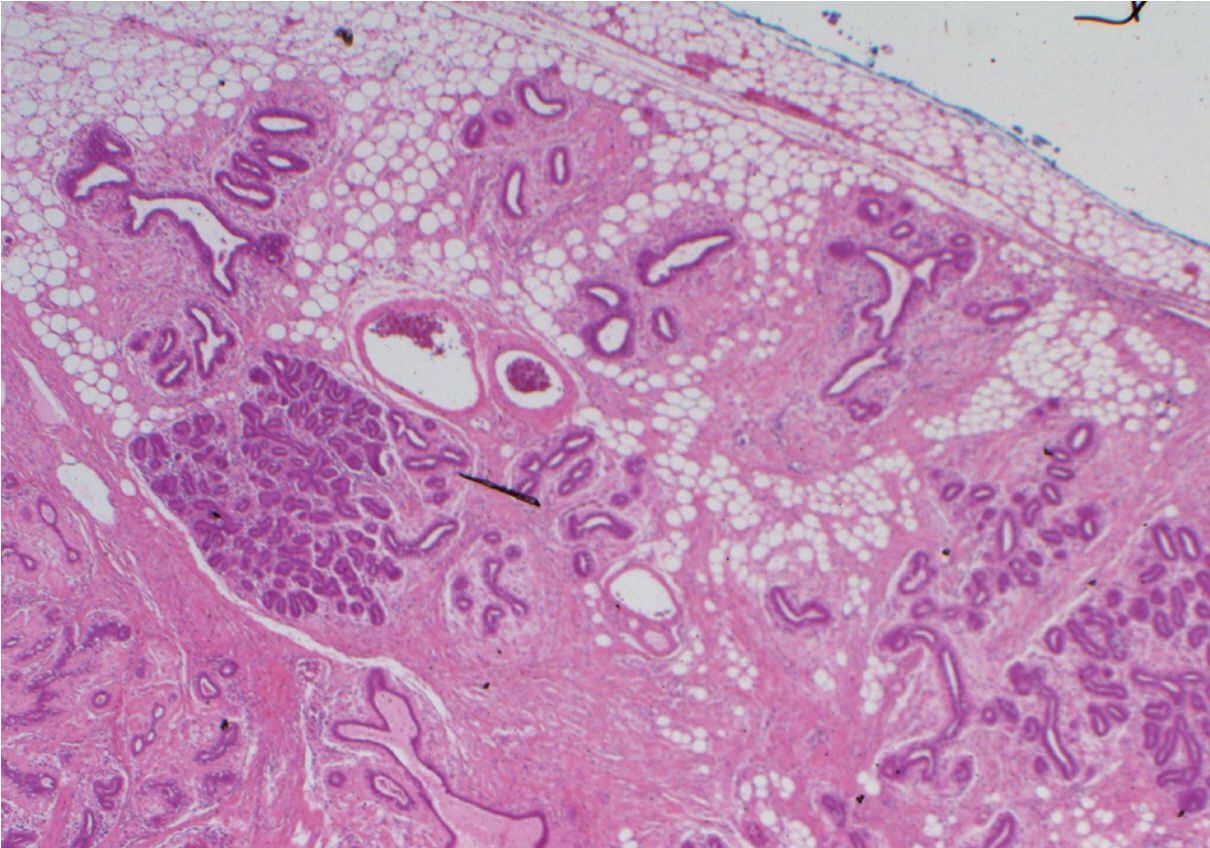
Fig. 1. Periductal stromal tumor exhibiting a multinodular growth pattern separated by fat.
Fig. 2. Periductal stromal tumor exhibiting benign ducts surrounded by atypical spindle cells, which appear to infiltrate adjacent adipose tissue. The spindle cells are diffusely positive for CD34 (inset).
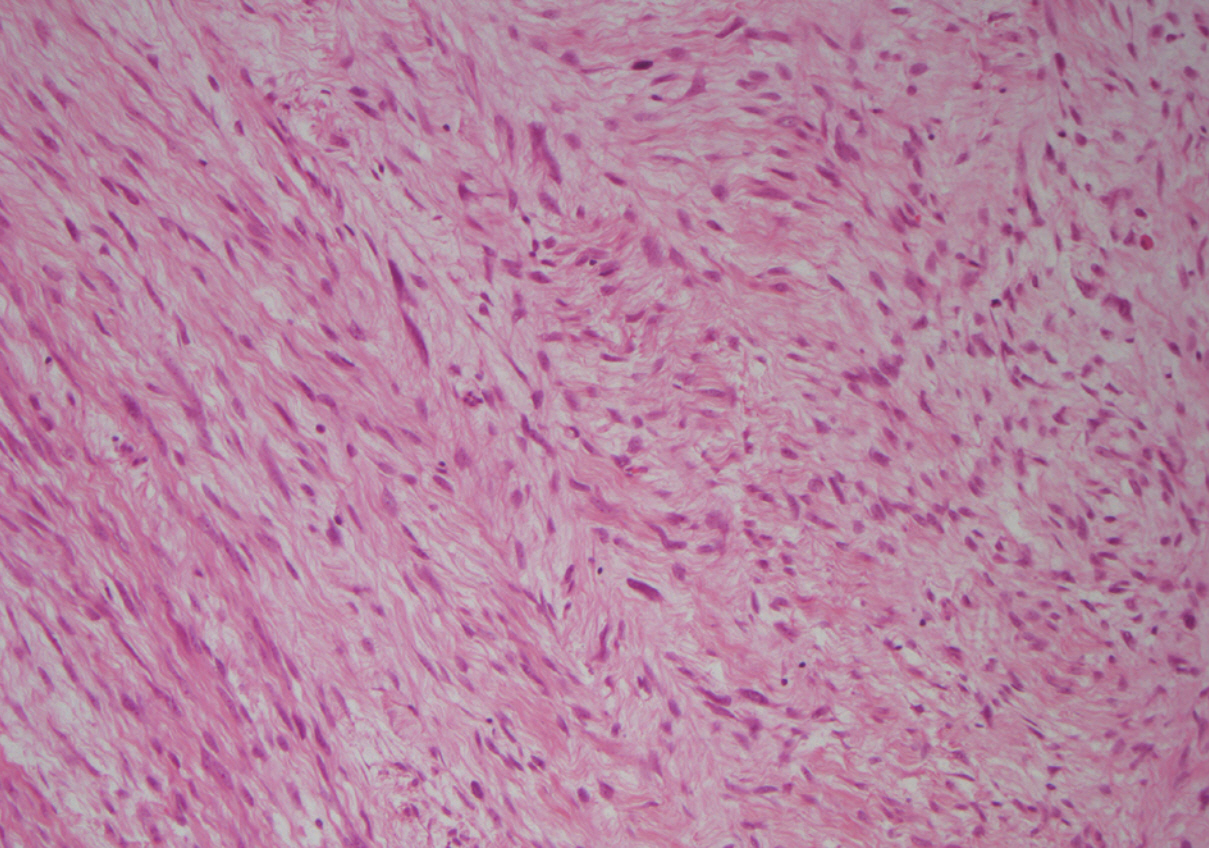
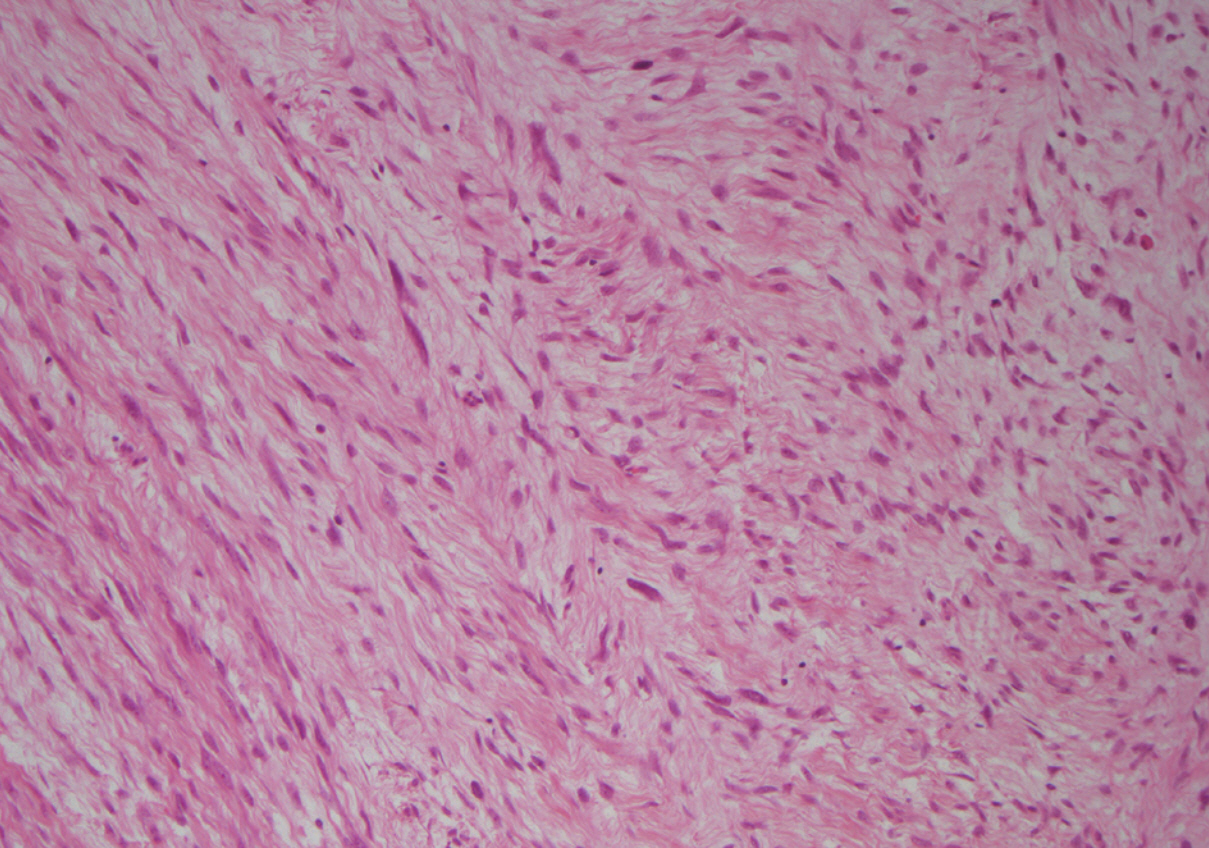
Fig. 3. Periductal stromal tumor showing stromal overgrowth.
Fig. 1.
Fig. 2.
Fig. 3.
Periductal Stromal Tumor of Breast: A Case Report and A Review of Literature

 E-submission
E-submission