Search
- Page Path
- HOME > Search
Review
- Interpretation of PD-L1 expression in gastric cancer: summary of a consensus meeting of Korean gastrointestinal pathologists
- Soomin Ahn, Yoonjin Kwak, Gui Young Kwon, Kyoung-Mee Kim, Moonsik Kim, Hyunki Kim, Young Soo Park, Hyeon Jeong Oh, Kyoungyul Lee, Sung Hak Lee, Hye Seung Lee
- J Pathol Transl Med. 2024;58(3):103-116. Published online April 25, 2024
- DOI: https://doi.org/10.4132/jptm.2024.03.15
- 9,450 View
- 580 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Nivolumab plus chemotherapy in the first-line setting has demonstrated clinical efficacy in patients with human epidermal growth factor receptor 2–negative advanced or metastatic gastric cancer, and is currently indicated as a standard treatment. Programmed death-ligand 1 (PD-L1) expression is an important biomarker for predicting response to anti–programmed death 1/PD-L1 agents in several solid tumors, including gastric cancer. In the CheckMate-649 trial, significant clinical improvements were observed in patients with PD-L1 combined positive score (CPS) ≥ 5, determined using the 28-8 pharmDx assay. Accordingly, an accurate interpretation of PD-L1 CPS, especially at a cutoff of 5, is important. The CPS method evaluates both immune and tumor cells and provides a comprehensive assessment of PD-L1 expression in the tumor microenvironment of gastric cancer. However, CPS evaluation has several limitations, one of which is poor interobserver concordance among pathologists. Despite these limitations, clinical indications relying on PD-L1 CPS are increasing. In response, Korean gastrointestinal pathologists held a consensus meeting for the interpretation of PD-L1 CPS in gastric cancer. Eleven pathologists reviewed 20 PD-L1 slides with a CPS cutoff close to 5, stained with the 28-8 pharmDx assay, and determined the consensus scores. The issues observed in discrepant cases were discussed. In this review, we present cases of gastric cancer with consensus PD-L1 CPS. In addition, we briefly touch upon current practices and clinical issues associated with assays used for the assessment of PD-L1 expression in gastric cancer.
-
Citations
Citations to this article as recorded by- Adjuvant immunotherapy in patients with resected gastric and oesophagogastric junction cancer following preoperative chemotherapy with high risk for recurrence (ypN+ and/or R1): European Organisation of Research and Treatment of Cancer (EORTC) 1707 VESTIG
F. Lordick, M.E. Mauer, G. Stocker, C.A. Cella, I. Ben-Aharon, G. Piessen, L. Wyrwicz, G. Al-Haidari, T. Fleitas-Kanonnikoff, V. Boige, R. Lordick Obermannová, U.M. Martens, C. Gomez-Martin, P. Thuss-Patience, V. Arrazubi, A. Avallone, K.K. Shiu, P. Artru
Annals of Oncology.2025; 36(2): 197. CrossRef - PD-L1 as a Biomarker in Gastric Cancer Immunotherapy
Yunjoo Cho, Soomin Ahn, Kyoung-Mee Kim
Journal of Gastric Cancer.2025; 25(1): 177. CrossRef - PD-L1 importance in malignancies comprehensive insights into the role of PD-L1 in malignancies: from molecular mechanisms to therapeutic opportunities
Mojdeh Soltani, Mohammad Abbaszadeh, Hamed Fouladseresht, Mark J. M. Sullman, Nahid Eskandari
Clinical and Experimental Medicine.2025;[Epub] CrossRef - PD-L1 thresholds predict efficacy of immune checkpoint inhibition in first-line treatment of advanced gastroesophageal adenocarcinoma. A systematic review and meta-analysis of seven phase III randomized trials
V. Formica, C. Morelli, L. Fornaro, S. Riondino, M. Rofei, E. Fontana, E.C. Smyth, M. Roselli, H.-T. Arkenau
ESMO Open.2024; 9(11): 103967. CrossRef
- Adjuvant immunotherapy in patients with resected gastric and oesophagogastric junction cancer following preoperative chemotherapy with high risk for recurrence (ypN+ and/or R1): European Organisation of Research and Treatment of Cancer (EORTC) 1707 VESTIG
Original Article
- Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
- Su Hwa Kim, Young Suk Lee, Sung Hak Lee, Yeoun Eun Sung, Ahwon Lee, Jun Kang, Jae-Sung Park, Sin Soo Jeun, Youn Soo Lee
- J Pathol Transl Med. 2023;57(4):217-231. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.10
- 3,233 View
- 161 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The metastatic brain tumor is the most common brain tumor. The aim of this study was to demonstrate the clinicopathological and molecular pathologic features of brain metastases (BM).
Methods
A total of 269 patients were diagnosed with BM through surgical resection at Seoul St. Mary’s Hospital from January 2010 to March 2020. We reviewed the clinicopathological features and molecular status of primary and metastatic brain tissues using immunohistochemistry and molecular pathology results.
Results
Among 269 patients, 139 males and 130 females were included. The median age of primary tumor was 58 years (range, 13 to 87 years) and 86 patients (32.0%) had BM at initial presentation. Median BM free interval was 28.0 months (range, 1 to 286 months). The most frequent primary site was lung 46.5% (125/269), and followed by breast 15.6% (42/269), colorectum 10.0% (27/269). Epidermal growth factor receptor (EGFR) mutation was found in 50.8% (32/63) and 58.0% (40/69) of lung primary and BM, respectively. In both breast primary and breast cancer with BM, luminal B was the most frequent subtype at 37.9% (11/29) and 42.9% (18/42), respectively, followed by human epidermal growth factor receptor 2 with 31.0% (9/29) and 33.3% (14/42). Triple-negative was 20.7% (6/29) and 16.7% (7/42), and luminal A was 10.3% (3/29) and 7.1% (3/42) of breast primary and BM, respectively. In colorectal primary and colorectal cancer with BM, KRAS mutation was found in 76.9% (10/13) and 66.7% (2/3), respectively.
Conclusions
We report the clinicopathological and molecular pathologic features of BM that can provide useful information for understanding the pathogenesis of metastasis and for clinical trials based on the tumor’s molecular pathology.
Review
- A standardized pathology report for gastric cancer: 2nd edition
- Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi, Hee Kyung Chang, Soomin Ahn, Mee Soo Chang, Song-Hee Han, Yoonjin Kwak, An Na Seo, Sung Hak Lee, Mee-Yon Cho
- J Pathol Transl Med. 2023;57(1):1-27. Published online January 15, 2023
- DOI: https://doi.org/10.4132/jptm.2022.12.23
- 18,683 View
- 1,294 Download
- 19 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The first edition of ‘A Standardized Pathology Report for Gastric Cancer’ was initiated by the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists and published 17 years ago. Since then, significant advances have been made in the pathologic diagnosis, molecular genetics, and management of gastric cancer (GC). To reflect those changes, a committee for publishing a second edition of the report was formed within the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists. This second edition consists of two parts: standard data elements and conditional data elements. The standard data elements contain the basic pathologic findings and items necessary to predict the prognosis of GC patients, and they are adequate for routine surgical pathology service. Other diagnostic and prognostic factors relevant to adjuvant therapy, including molecular biomarkers, are classified as conditional data elements to allow each pathologist to selectively choose items appropriate to the environment in their institution. We trust that the standardized pathology report will be helpful for GC diagnosis and facilitate large-scale multidisciplinary collaborative studies.
-
Citations
Citations to this article as recorded by- Spatial and Temporal Tumor Heterogeneity in Gastric Cancer: Discordance of Predictive Biomarkers
Hye Seung Lee
Journal of Gastric Cancer.2025; 25(1): 192. CrossRef - PD-L1 as a Biomarker in Gastric Cancer Immunotherapy
Yunjoo Cho, Soomin Ahn, Kyoung-Mee Kim
Journal of Gastric Cancer.2025; 25(1): 177. CrossRef - Korean Gastric Cancer Association-Led Nationwide Survey on Surgically Treated Gastric Cancers in 2023
Dong Jin Kim, Jeong Ho Song, Ji-Hyeon Park, Sojung Kim, Sin Hye Park, Cheol Min Shin, Yoonjin Kwak, Kyunghye Bang, Chung-sik Gong, Sung Eun Oh, Yoo Min Kim, Young Suk Park, Jeesun Kim, Ji Eun Jung, Mi Ran Jung, Bang Wool Eom, Ki Bum Park, Jae Hun Chung, S
Journal of Gastric Cancer.2025; 25(1): 115. CrossRef - A Comprehensive and Comparative Review of Global Gastric Cancer Treatment Guidelines: 2024 Update
Sang Soo Eom, Keun Won Ryu, Hye Sook Han, Seong-Ho Kong
Journal of Gastric Cancer.2025; 25(1): 153. CrossRef - Korea, Japan, Europe, and the United States: Why are guidelines for gastric cancer different?
Emily E. Stroobant, Seong-Ho Kong, Maria Bencivenga, Takahiro Kinoshita, Tae-Han Kim, Takeshi Sano, Giovanni de Manzoni, Han-Kwang Yang, Yuko Kitagawa, Vivian E. Strong
Gastric Cancer.2025; 28(4): 559. CrossRef - Genomic and Transcriptomic Characterization of Gastric Cancer with Bone Metastasis
Sujin Oh, Soo Kyung Nam, Keun-Wook Lee, Hye Seung Lee, Yujun Park, Yoonjin Kwak, Kyu Sang Lee, Ji-Won Kim, Jin Won Kim, Minsu Kang, Young Suk Park, Sang-Hoon Ahn, Yun-Suhk Suh, Do Joong Park, Hyung Ho Kim
Cancer Research and Treatment.2024; 56(1): 219. CrossRef - Microscopic tumor mapping of post-neoadjuvant therapy pancreatic cancer specimens to predict post-surgical recurrence: A prospective cohort study
Yeshong Park, Yeon Bi Han, Jinju Kim, MeeYoung Kang, Boram Lee, Eun Sung Ahn, Saemi Han, Haeryoung Kim, Hee-Young Na, Ho-Seong Han, Yoo-Seok Yoon
Pancreatology.2024; 24(4): 562. CrossRef - Effect of Neoadjuvant Chemotherapy on Tumor-Infiltrating Lymphocytes in Resectable Gastric Cancer: Analysis from a Western Academic Center
Elliott J. Yee, Danielle Gilbert, Jeffrey Kaplan, Sachin Wani, Sunnie S. Kim, Martin D. McCarter, Camille L. Stewart
Cancers.2024; 16(7): 1428. CrossRef - Interpretation of PD-L1 expression in gastric cancer: summary of a consensus meeting of Korean gastrointestinal pathologists
Soomin Ahn, Yoonjin Kwak, Gui Young Kwon, Kyoung-Mee Kim, Moonsik Kim, Hyunki Kim, Young Soo Park, Hyeon Jeong Oh, Kyoungyul Lee, Sung Hak Lee, Hye Seung Lee
Journal of Pathology and Translational Medicine.2024; 58(3): 103. CrossRef - Expression of claudin 18.2 in poorly cohesive carcinoma and its association with clinicopathologic parameters in East Asian patients
Moonsik Kim, Byung Woog Kang, Jihyun Park, Jin Ho Baek, Jong Gwang Kim
Pathology - Research and Practice.2024; 263: 155628. CrossRef - Clinicopathological analysis of claudin 18.2 focusing on intratumoral heterogeneity and survival in patients with metastatic or unresectable gastric cancer
T.-Y. Kim, Y. Kwak, S.K. Nam, D. Han, D.-Y. Oh, S.-A. Im, H.S. Lee
ESMO Open.2024; 9(12): 104000. CrossRef - Pathological Interpretation of Gastric Tumors in Endoscopic Submucosal Dissection
Jung Yeon Kim
Journal of Digestive Cancer Research.2023; 11(1): 15. CrossRef - Histopathology of Gastric Cancer
Baek-hui Kim, Sung Hak Lee
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2023; 23(2): 143. CrossRef - Endoscopic submucosal dissection hands-on training with artificial mucosal layer EndoGEL
Tae-Se Kim, Jun Haeng Lee
Journal of Innovative Medical Technology.2023; 1(1): 5. CrossRef
- Spatial and Temporal Tumor Heterogeneity in Gastric Cancer: Discordance of Predictive Biomarkers
Original Article
- KRAS Mutation Test in Korean Patients with Colorectal Carcinomas: A Methodological Comparison between Sanger Sequencing and a Real-Time PCR-Based Assay
- Sung Hak Lee, Arthur Minwoo Chung, Ahwon Lee, Woo Jin Oh, Yeong Jin Choi, Youn-Soo Lee, Eun Sun Jung
- J Pathol Transl Med. 2017;51(1):24-31. Published online December 25, 2016
- DOI: https://doi.org/10.4132/jptm.2016.10.03
- 10,815 View
- 168 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Mutations in the KRAS gene have been identified in approximately 50% of colorectal cancers (CRCs). KRAS mutations are well established biomarkers in anti–epidermal growth factor receptor therapy. Therefore, assessment of KRAS mutations is needed in CRC patients to ensure appropriate treatment.
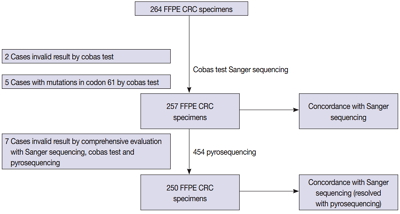
Methods
We compared the analytical performance of the cobas test to Sanger sequencing in 264 CRC cases. In addition, discordant specimens were evaluated by 454 pyrosequencing.
Results
KRAS mutations for codons 12/13 were detected in 43.2% of cases (114/264) by Sanger sequencing. Of 257 evaluable specimens for comparison, KRAS mutations were detected in 112 cases (43.6%) by Sanger sequencing and 118 cases (45.9%) by the cobas test. Concordance between the cobas test and Sanger sequencing for each lot was 93.8% positive percent agreement (PPA) and 91.0% negative percent agreement (NPA) for codons 12/13. Results from the cobas test and Sanger sequencing were discordant for 20 cases (7.8%). Twenty discrepant cases were subsequently subjected to 454 pyrosequencing. After comprehensive analysis of the results from combined Sanger sequencing–454 pyrosequencing and the cobas test, PPA was 97.5% and NPA was 100%.
Conclusions
The cobas test is an accurate and sensitive test for detecting KRAS-activating mutations and has analytical power equivalent to Sanger sequencing. Prescreening using the cobas test with subsequent application of Sanger sequencing is the best strategy for routine detection of KRAS mutations in CRC. -
Citations
Citations to this article as recorded by- Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
Su Hwa Kim, Young Suk Lee, Sung Hak Lee, Yeoun Eun Sung, Ahwon Lee, Jun Kang, Jae-Sung Park, Sin Soo Jeun, Youn Soo Lee
Journal of Pathology and Translational Medicine.2023; 57(4): 217. CrossRef - Assessment of KRAS and NRAS status in metastatic colorectal cancer: Experience of the National Institute of Oncology in Rabat Morocco
Chaimaa Mounjid, Hajar El Agouri, Youssef Mahdi, Abdelilah Laraqui, En-nacer Chtati, Soumaya Ech-charif, Mouna Khmou, Youssef Bakri, Amine Souadka, Basma El Khannoussi
Annals of Cancer Research and Therapy.2022; 30(2): 80. CrossRef - The current understanding on the impact of KRAS on colorectal cancer
Mingjing Meng, Keying Zhong, Ting Jiang, Zhongqiu Liu, Hiu Yee Kwan, Tao Su
Biomedicine & Pharmacotherapy.2021; 140: 111717. CrossRef - Droplet digital PCR revealed high concordance between primary tumors and lymph node metastases in multiplex screening of KRAS mutations in colorectal cancer
Barbora Vanova, Michal Kalman, Karin Jasek, Ivana Kasubova, Tatiana Burjanivova, Anna Farkasova, Peter Kruzliak, Dietrich Busselberg, Lukas Plank, Zora Lasabova
Clinical and Experimental Medicine.2019; 19(2): 219. CrossRef - CRISPR Technology for Breast Cancer: Diagnostics, Modeling, and Therapy
Rachel L. Mintz, Madeleine A. Gao, Kahmun Lo, Yeh‐Hsing Lao, Mingqiang Li, Kam W. Leong
Advanced Biosystems.2018;[Epub] CrossRef
- Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
Case Report
- Systemic Plasmacytosis: A Case Report with a Review of the Literature.
- Sung Hak Lee, Chang Young Yoo, Ji Han Jung, Jin Young Yoo, Suk Jin Kang, Chang Suk Kang
- Korean J Pathol. 2011;45(6):632-638.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.632
- 4,170 View
- 52 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Systemic plasmacytosis is an uncommon disorder characterized by widely disseminated macular skin eruptions composed of polyclonal lymphoplasmacytic infiltrates associated with variable extracutaneous involvement. An aggressive clinical course has been observed in a small number of patients, but most cases have followed chronic and benign clinical course without spontaneous remission. Previously reported cases of this entity have been described almost exclusively in Japanese patients. We recently experienced a case of systemic plasmacytosis in a 48-year-old Korean female patient. Initial skin biopsy specimen revealed patchy perivascular and periadnexal infiltrates of mature plasma cells. Serum immunoelectrophoresis revealed polyclonal hypergammaglobulinemia, and polyclonal plasmacytosis was noted on the subsequent biopsy specimens of left supraclavicular and axillary lymph nodes. Multiple tiny pulmonary nodules appeared six years after the initial cutaneous presentation and were found to be of the same histologic appearance. We herein report a rare case of systemic plasmacytosis with a review of the literature.
-
Citations
Citations to this article as recorded by- Cutaneous plasmacytosis with mast cell infiltration
Sarina Jain, RohitV Hede, UdayS Khopkar
Indian Journal of Dermatology, Venereology and Leprology.2020; 86(1): 91. CrossRef - Plasmocitosis cutánea en un varón de raza blanca
A. López-Gómez, T. Salas-García, A. Ramírez-Andreo, E. Poblet-Martínez
Actas Dermo-Sifiliográficas.2015; 106(6): 520. CrossRef - Cutaneous Plasmacytosis in a White Man
A. López-Gómez, T. Salas-García, A. Ramírez-Andreo, E. Poblet-Martínez
Actas Dermo-Sifiliográficas (English Edition).2015; 106(6): 520. CrossRef
- Cutaneous plasmacytosis with mast cell infiltration
Original Articles
- Detection Limit of Monoclonal B-Cells Using Multiplex PCR and Laser-Induced Fluorescence Capillary Electrophoresis.
- Sung Hak Lee, Yeonsook Moon, Byunghoo Song, Hyung Nam Lee, Ahwon Lee, Eun Sun Jung, Yeong Jin Choi, Kyo Young Lee, Chang Suk Kang, Gyeongsin Park
- Korean J Pathol. 2011;45(6):582-588.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.582
- 3,603 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The identification of monoclonality has been widely used for making diagnoses of lymphoproliferative lesions. Awareness of the sensitivity and detection limit of the technique used would be important for the data to be convincing.
METHODS
We investigated the minimum requirement of cells and sensitivity of gel electrophoresis (GE) and laser-induced fluorescence capillary electrophoresis (LFCE) for identifying IgH gene rearrangement using BIOMED-2 protocols. DNA extracted from Raji cells were diluted serially with peripheral blood mononuclear cells (PBMNCs) DNA. DNA from mixtures of diffuse large B-cell lymphoma (DLBCL) and reactive lymph nodes were also serially diluted.
RESULTS
For Raji cells, the detection limit was 62 and 16 cell-equivalents for GE and LFCE, respectively. In the condition with PBMNCs mixture, 2.5% and 1.25% of clonal cells was the minimum requirement for GE and LFCE, respectively. In 23% of DLBCL cells in tissue section, the detection limit was 120 and 12 cell-equivalents for GE and LFCE, respectively. In 3.2% of DLBCL cells, that was 1,200 and 120 cell-equivalents for GE and LFCE, respectively.
CONCLUSIONS
These results show that LFCE method is more sensitive than GE and the sensitivity of clonality detection can be influenced by the amount of admixed normal lymphoid cells. -
Citations
Citations to this article as recorded by- Molecular pathology diagnosis of diffuse large B cell lymphoma using BIOMED-2 clonal gene rearrangements
Saeid Ghorbian
Annals of Diagnostic Pathology.2017; 29: 28. CrossRef
- Molecular pathology diagnosis of diffuse large B cell lymphoma using BIOMED-2 clonal gene rearrangements
- Copy Number Alterations of BCAS1 in Squamous Cell Carcinomas.
- Yu Im Kim, Ahwon Lee, Jennifer Kim, Bum Hee Lee, Sung Hak Lee, Suk Woo Nam, Sug Hyung Lee, Won Sang Park, Nam Jin Yoo, Jung Young Lee, Sang Ho Kim, Su Young Kim
- Korean J Pathol. 2011;45(3):271-275.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.271
- 3,887 View
- 34 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Breast carcinoma amplified sequence 1 (BCAS1), located in 20q13, is amplified and overexpressed in breast cancers. Even though BCAS1 is expected to be an oncogene candidate, its contribution to tumorigenesis and copy number status in other malignancies is not reported. To elucidate the role of BCAS1 in squamous cell carcinomas, we investigated the copy number status and expression level of BCAS1 in several squamous cell carcinoma cell lines, normal keratinocytes and primary tumors.
METHODS
We quantitated BCAS1 gene by real-time polymerase chain reaction (PCR). Expression level of BCAS1 was measured by real-time reverse transcription-PCR and immunoblot.
RESULTS
Seven (88%) of 8 squamous cell carcinoma cell lines showed copy number gain of BCAS1 with various degrees. BCAS1 gene in primary tumors (73%) also showed copy number gain. However, expression level did not show a linear correlation with copy number changes.
CONCLUSIONS
We identified copy number gain of BCAS1 in squamous cell carcinomas. Due to lack of linear correlation between copy numbers of BCAS1 and its expression level, we could not confirm that the overexpression of BCAS1 is a common finding in squamous cell carcinoma cell lines. However, this study shows that the copy number gain of BCAS1 is a common finding in squamous cell carcinomas. -
Citations
Citations to this article as recorded by- Electrochemical Approaches for Preparation of Tailor-Made Amino Acids
Nana Wang, Jingcheng Xu, Haibo Mei, Hiroki Moriwaki, Kunisuke Izawa, Vadim A. Soloshonok, Jianlin Han
Chinese Journal of Organic Chemistry.2021; 41(8): 3034. CrossRef
- Electrochemical Approaches for Preparation of Tailor-Made Amino Acids
- Comparison of Detecting Methods of BK Virus Infection in Patients with Renal Allograft Recipients.
- Sung Hak Lee, Youn Jun Park, Chul Woo Yang, Yong Soo Kim, In Sung Moon, Chang Suk Kang, Yeong Jin Choi
- Korean J Pathol. 2010;44(6):636-641.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.6.636
- 3,900 View
- 25 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
BK virus nephropathy (BKVN) is an emerging problem as a consequence of the use of potent immunosuppressive agents. Because optimal detection methods for the diagnosis of BKVN are required clinically, we compared the results of renal allograft biopsy, urine cytology, and urine and blood viral loads.
METHODS
Four hundred sixty two case notes from 2004 to 2009 at Seoul St. Mary's Hospital were reviewed. During that period, 286 cases of urine cytology for decoy cells, 938 cases of urine BKV reverse transcription-polymerase chain reaction (RT-PCR), and 1,029 cases of blood BKV RT-PCR were performed. All diagnostic methods were performed in 85 cases.
RESULTS
A histological diagnosis of BKVN was made in 2.4% of cases (11/462). Urine cytology for decoy cells was positive in 26.2% (75/286). BKV RT-PCR revealed viruria in positivity of 22.1% (207/938) and viremia in 5.2% (54/1,029). In cases of BKVN, the sensitivities of urine and blood BKV RT-PCR were all 100% and the specificities were 69% and 94.5%, respectively. In cases with positive urine decoy cells, the sensitivities of urine and blood BKV RT-PCR were 50% and 27.7%, with specificities of 77.7% and 100%, respectively.
CONCLUSIONS
BKV screening by RT-PCR assays may be a clinically useful noninvasive test to identify renal recipients with concurrent BKVN. -
Citations
Citations to this article as recorded by- Prevalence of BK Virus among Iranian Renal Transplant Recipients: A Systematic Review and Meta-Analysis
Mohsen Ebrahimi, Alireza Mohebbi, Mohammad Mostakhdem Hashemi, Mobina Ashrafi Shahmirzadi
Journal of Clinical and Basic Research.2020; 4(4): 50. CrossRef - Asymptomatic hematuria associated with urinary polyomavirus infection in immunocompetent patients
Sung Hak Lee, Sung Hoo Hong, Ji Youl Lee, Tae Kon Hwang, Kyoung Suk Kim, Hyoungnam Lee, Yeong Jin Choi
Journal of Medical Virology.2014; 86(2): 347. CrossRef
- Prevalence of BK Virus among Iranian Renal Transplant Recipients: A Systematic Review and Meta-Analysis
- Mutation and Expression of DNA2 Gene in Gastric and Colorectal Carcinomas.
- Sung Hak Lee, Yoo Ri Kim, Nam Jin Yoo, Sug Hyung Lee
- Korean J Pathol. 2010;44(4):354-359.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.4.354
- 4,229 View
- 35 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Deregulation of DNA repair and replication are involved in cancer development. DNA2 is a nuclease/helicase that plays roles in DNA repair and replication. The aim of this study was to explore DNA2 mutation and DNA2 protein expression in gastric cancers (GCs) and colorectal cancers (CRCs).
METHODS
We analyzed two mononucleotide repeats in DNA2 in 27 GCs with high microsatellite instability (MSI-H), 34 GCs with stable MSI (MSS), 29 CRCs with MSI-H and 35 CRCs with MSS by single-strand conformation polymorphism. We also analyzed DNA2 expression in GCs and CRCs either with MSI-H or MSS.
RESULTS
We found DNA2 mutations in two GCs (7.1%) and two CRCs with MSI-H (6.9%), but not in cancers with MSS. The mutations consisted of three cases of a c.2593delT and one of a c.2592_2593delTT, which would result in premature stopping of amino acid synthesis (p.Ser865Hisfsx6 and p.Ser865Thrfsx20, respectively). DNA2 expression was observed in 16 (80%) of the GCs and 15 (75%) of the CRCs with MSI-H, but all of the cancers with DNA2 frameshift mutations were weak or negative for DNA2.
CONCLUSIONS
Our data indicate that DNA2 mutation and loss of DNA2 expression occur in GCs and CRCs, and suggest that these alterations may contribute to cancer pathogenesis by deregulating DNA repair and replication. -
Citations
Citations to this article as recorded by- Multiple roles of DNA2 nuclease/helicase in DNA metabolism, genome stability and human diseases
Li Zheng, Yuan Meng, Judith L Campbell, Binghui Shen
Nucleic Acids Research.2020; 48(1): 16. CrossRef - Integration of multiple networks and pathways identifies cancer driver genes in pan-cancer analysis
Claudia Cava, Gloria Bertoli, Antonio Colaprico, Catharina Olsen, Gianluca Bontempi, Isabella Castiglioni
BMC Genomics.2018;[Epub] CrossRef - Replication intermediates that escape Dna2 activity are processed by Holliday junction resolvase Yen1
Gizem Ölmezer, Maryna Levikova, Dominique Klein, Benoît Falquet, Gabriele Alessandro Fontana, Petr Cejka, Ulrich Rass
Nature Communications.2016;[Epub] CrossRef
- Multiple roles of DNA2 nuclease/helicase in DNA metabolism, genome stability and human diseases
Case Report
- Primary Malignant Melanoma of the Urinary Bladder: A Case Report.
- Sung Hak Lee, Eun Deok Chang, Eun Jung Lee, Chang Suk Kang
- Korean J Pathol. 2010;44(2):216-219.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.216
- 3,801 View
- 43 Download
-
 Abstract
Abstract
 PDF
PDF - Primary malignant melanoma in the bladder is very rare, with only 18 cases having been currently reported. A 65-year-old male patient presented with a 5-month history of gross hematuria. On ultrasonography, an 8.1 x 6.1 cm mass was revealed on the bladder wall. A partial cystectomy was performed. Microscopically, the tumor was composed of atypical, pigmented melanocytes that were positive for S-100 protein and they were negative for human melanoma black-45. Although he underwent supportive therapy, an 8.7 x 5.9 cm mass occupying the prevesical space was noted on a follow-up computed tomography scan 4 months later. Two nodules of the left lower lung and multiple enlarged lymph nodes in the left external iliac chain were also revealed. The patient declined any further treatment. The histogenesis of primary bladder melanoma is uncertain, but an origin from neural crest cells has been proposed. The prognosis for patients with this tumor is still poor despite the availability of several therapeutic options.
Short Case Report
- Pneumocystis jirovecii Pneumonia Accompanied with Fat Embolism: A Case Report.
- Sung Hak Lee, Ok Ran Shin, Eun Jung Lee, Kyo Young Lee
- Korean J Pathol. 2009;43(4):355-357.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.355
- 2,961 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Pneumocystis jirovecii is an atypical fungus that causes severe pneumonia in immune compromised patients. While Pneumocystis jirovecii pneumonia (PCP) is more commonly diagnosed in individuals who have HIV infection, it can occur in individuals with other forms of immunosuppression. Fat embolism most commonly develops after orthopedic injuries, but it has also been reported after other forms of trauma such as severe burns, closed-chest cardiac massage, and liposuction. Overlap in the clinical presentation of these diseases has not yet been reported. We report here on a case of PCP with fat embolism in 52-year-old female patient who had no obvious risk factors for HIV infection. Even if risk factors for HIV or other forms of immunosuppression are not present, PCP can also be seen in patients who present with fat embolism, and the clinical presentation of both conditions can overlap.

 E-submission
E-submission




 First
First Prev
Prev



