Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 46(5); 2012 > Article
-
Case Report
Extraskeletal Mesenchymal Chondrosarcoma in the Axillary Region: Reports of Two Cases - Chang-Young Seo, Sung-Taek Jung, Jae-Wook Byun
-
Korean Journal of Pathology 2012;46(5):483-488.
DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.5.483
Published online: October 25, 2012
Department of Orthopedic Surgery, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea.
- Corresponding Author: Sung-Taek Jung, M.D. Department of Orthopedic Surgery, Chonnam National University Hospital, Chonnam National University Medical School, 42 Jebong-ro, Dong-gu, Gwangju 501-757, Korea. Tel: +82-62-227-1640, Fax: +82-62-225-7794, stjung@chonnam.ac.kr
• Received: March 6, 2011 • Revised: December 1, 2011 • Accepted: December 2, 2011
© 2012 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Extraskeletal Mesenchymal Chondrosarcoma of the Arm: A Rare Case Report with a Review of Literature
Anubhuti Chaturvedi, Nimisha Dhankar, Swapnil Suman, Nita Khurana, Chandra Bhushan Singh, Sapna Singh
Journal of Bone and Joint Diseases.2025; 40(3): 170. CrossRef - Complete surgical excision of a high‐grade extraskeletal mesenchymal chondrosarcoma, resulting in a longer survival than previously reported
Hannah Reeves, Tesh Smalle
Veterinary Record Case Reports.2022;[Epub] CrossRef - Locally recurrent extraskeletal myxoid chondrosarcoma of the shoulder: a case of complete neoadjuvant radiotherapy response
Luca Improta, Sergio Valeri, Rossana Alloni, Chiara Pagnoni, Francesco Mallozzi Santa Maria, Beniamino Brunetti, Carlo Greco, Irene Aprile, Mirella Maselli, Bruno Vincenzi, Alessandro Gronchi
Clinical Sarcoma Research.2020;[Epub] CrossRef - Primary extraskeletal chondrosarcoma in the axillary region of a dog with review of the literature
Catrina Pennington, Josep Monne Rodriguez, Marlene Finck, Ben Walton
Veterinary Record Case Reports.2018;[Epub] CrossRef - Mesenchymal Chondrosarcoma of Bone and Soft Tissue: A Systematic Review of 107 Patients in the Past 20 Years
Jie Xu, Dasen Li, Lu Xie, Shun Tang, Wei Guo, David M Loeb
PLOS ONE.2015; 10(4): e0122216. CrossRef - Management of renal extraskeletal mesenchymal chondrosarcoma
Vitalie Gherman, Ciprian Tomuleasa, Catalina Bungardean, Nicolae Crisan, Victor-Dan Ona, Bogdan Feciche, Alexandru Irimie, Ioan Coman
BMC Surgery.2014;[Epub] CrossRef
Extraskeletal Mesenchymal Chondrosarcoma in the Axillary Region: Reports of Two Cases








Fig. 1 Case 1: (A) Anteroposterior radiographs of the left shoulder. Plain radiography findings are normal. (B) Coronal plane reconstructed computed tomography scan, showing a well-defined soft tissue mass around the left axillary region with no abnormal bony structure. Neither peripheral nor central calcifications are observed.
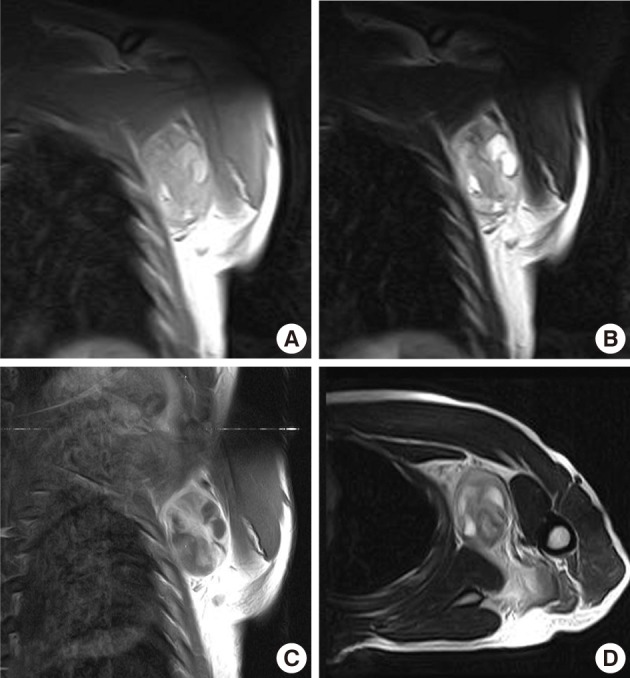
Fig. 2 Case 1: Preoperative magnetic resonance imaging. (A) A coronal plane T1-weighted (T1W) image. (B) A coronal plane T2-weighted (T2W) image. (C) A coronal plane Gd-enhanced image. (D) An axial plane T2W image. A well-defined soft tissue mass between the pectoralis major and subscapularis muscles without vascular encasement. The peripheral area shows high intensity in both T1W and T2W images, whereas the central area exhibits heterogenous intensity in T1W and T2W images. The tumor shows peripheral enhancement on Gd-enhanced images.
Fig. 3 Case 1: Gross appearance of the tumor. (A) The mass appears well-encapsulated and has an elastic-hard consistency. (B) Longitudinal section of the resected mass reveals a yellowish-white, glistening surface. The mass is homogenous except for a few small focal cystic and necrotic changes.
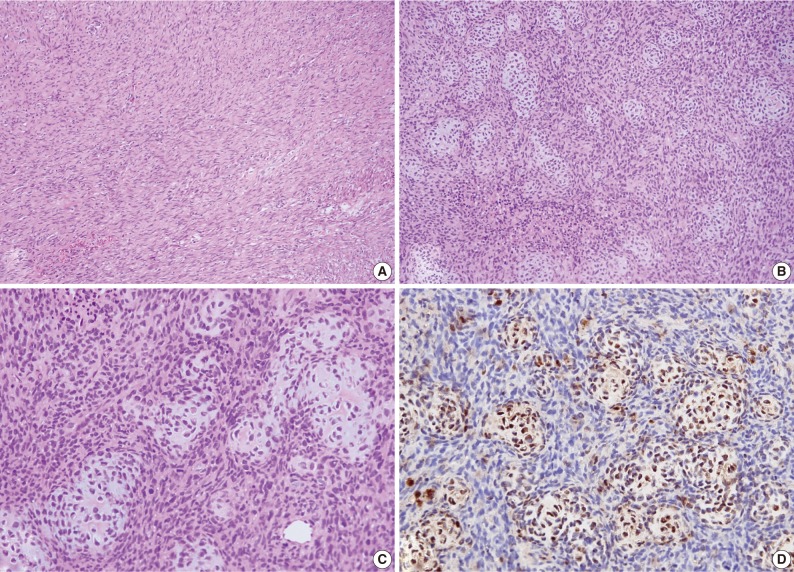
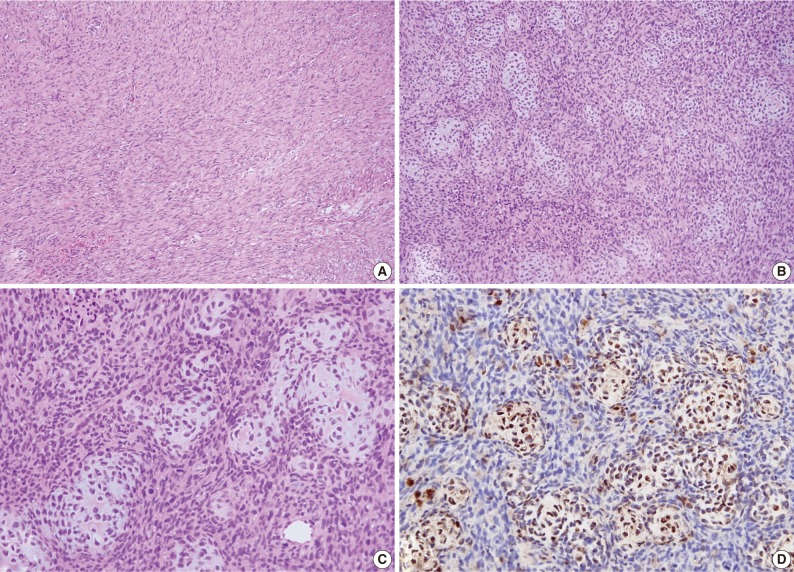
Fig. 4 Case 1: Histologic examination. (A) Histologic features showing scattered patterns with undifferentiated cells and focal areas of well-differentiated cartilaginous tissue. (B,C) Intimate admixture of islands of cartilaginous tissue and undifferentiated small neoplastic cells. (D) Immunohistochemically, the cartilaginous portion of the tumor shows strong S-100 protein positivity.
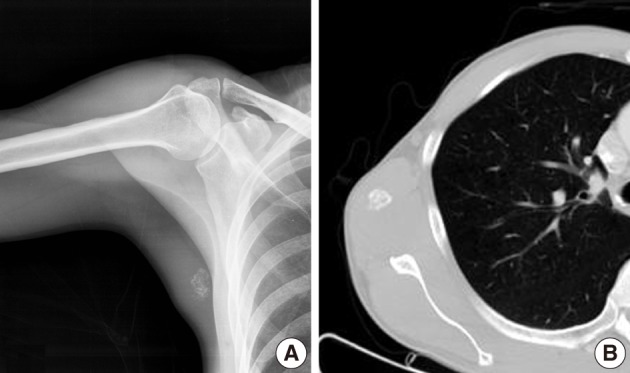
Fig. 5 Case 2: (A) Anteroposterior radiographs of right medial axilla. Plain radiograph showing stippled calcification. (B) Axial computed tomography image showing calcification but no bony abnormality.
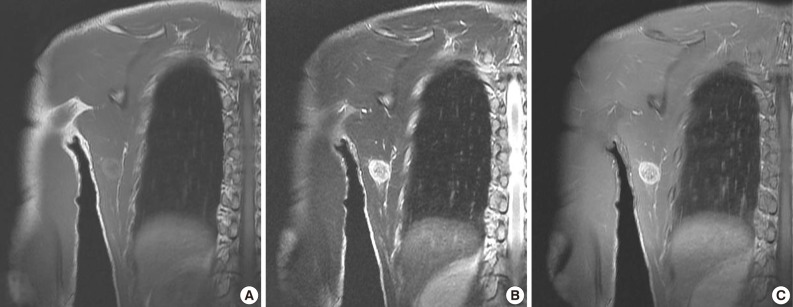
Fig. 6 Case 2: Preoperative magnetic resonance images. (A) Coronal plane T1-weighted (T1W) image. (B) Coronal T2-weighted (T2W) image. (C) Coronal plane Gd-enhanced image. The peripheral area has high intensity in T1W and T2W images and enhancement in Gd-enhanced images, whereas the central area has lower intensity.
Fig. 7 Case 2: Gross appearance of the tumor. Longitudinal section shows tan-white tissue with focal hemorrhage and necrosis.
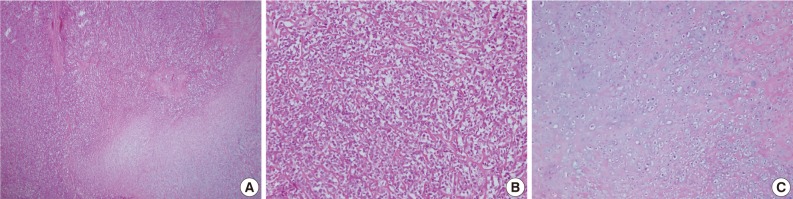
Fig. 8 Case 2: Histologic findings. Histologic features showing (A) gradual transition between hypercellular stroma and focal areas of well-differentiated cartilaginous tissue, (B) tumors consisted of undifferentiated small neoplastic cells, (C) the coexistence of nests of well-defined cartilaginous tissue.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Fig. 6
Fig. 7
Fig. 8
Extraskeletal Mesenchymal Chondrosarcoma in the Axillary Region: Reports of Two Cases

 E-submission
E-submission






 PubReader
PubReader Cite this Article
Cite this Article