Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(3); 2013 > Article
-
Case Study
Colonic Adenocarcinoma Arising from Gastric Heterotopia: A Case Study - Hyoungsuk Ko, Shin Young Park, Eun Jung Cha, Jang Sihn Sohn
-
Korean Journal of Pathology 2013;47(3):289-292.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.289
Published online: June 25, 2013
Department of Pathology, Konyang University School of Medicine, Daejeon, Korea.
- Corresponding Author: Jang Sihn Sohn, M.D. Department of Pathology, Konyang University School of Medicine, 158 Gwanjeodong-ro, Seo-gu, Daejeon 302-718, Korea. Tel: +82-42-600-9283, Fax: +82-42-600-9280, jsohn@kyuh.ac.kr
• Received: July 11, 2012 • Revised: September 7, 2012 • Accepted: September 11, 2012
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Anorectal gastric heterotopia as a rare cause of constipation: Case report and review of pediatric literature
Kathryn M. Stephenson, Raj P. Kapur, Jeffrey R. Avansino, Lusine Ambartsumyan
JPGN Reports.2025; 6(4): 407. CrossRef - Intussusception of Heterotopic Gastric Mucosa in the Transverse Colon: A Rare Cause of Perforation and Bleeding
Sho Fujiwara, Ryuichi Nishimura, Nozomi Koyamada
Cureus.2024;[Epub] CrossRef - Gastric heterotopia of colon found cancer workup in liver abscess: A case report
Jun Gi Park, Jeong Ill Suh, Yeo Un Kim
World Journal of Clinical Cases.2022; 10(15): 5012. CrossRef - Gastric heterotopia in the ileum mimicking Meckel's diverticulum
Reza Shojaeian, Negar Nekooei, Paria Dehghanian
Journal of Pediatric Surgery Case Reports.2022; 84: 102361. CrossRef - Sometimes Things Are Not Where They Are Supposed to Be: A Case Report of Gastric Heterotopia in the Rectum
Asher Lippe, Scott Lippe
Physician's Journal of Medicine.2022;[Epub] CrossRef - Gastric heterotopia of the rectum
Eduardo Dantas, Diva Yamaguti, Kendi Yamazaki
Gastroenterología y Hepatología.2021; 44(8): 579. CrossRef - Bleeding Gastric Heterotopia of Cecal Diverticulum in an Adolescent: A Case Report
Hyun-Il Seo, Jae-Young Kwak
Advances in Pediatric Surgery.2021; 27(1): 32. CrossRef - Gastric heterotopia of the rectum
Eduardo Dantas, Diva Yamaguti, Kendi Yamazaki
Gastroenterología y Hepatología (English Edition).2021; 44(8): 579. CrossRef - Polypoid Gastric Heterotopia of Colon
Marcela Adriana Duran Alvarez, Carla Noemi Tafur Sanchez
GE - Portuguese Journal of Gastroenterology.2020; 27(1): 65. CrossRef - Heterotopic Respiratory Mucosa in the Rectum: An Unusual Type and Site of Heterotopia in the Gastrointestinal Tract
Caroline Bsirini, Pratyusha Tirumanisetty, Joseph N. Dytoc, Diana Agostini-Vulaj, Christopher Steevens, Asad Ullah, Aaron R. Huber
International Journal of Surgical Pathology.2019; 27(2): 221. CrossRef - Perforation of Heterotopic Gastric Mucosa in ileal duplication in an adult: A case report
Vaanathi Paulvannan, Seshukumar Bylapudi, Mithun Kumar Ramesh Kumar, Mahesh Nachimuthu, Paulvannan Subramanian
Journal of Surgical Case Reports.2019;[Epub] CrossRef - Mixed adenoneuroendocrine carcinoma of the tongue arising within a congenital enteric cyst
Louis J. Ligthelm, Belinda K. Bunn, Erich J. Raubenheimer, Willie F. P. van Heerden
Head & Neck.2018;[Epub] CrossRef - The outlet patch: gastric heterotopia of the colorectum and anus
Abul A S R Mannan, Michael Vieth, Armen Khararjian, Binny Khandakar, Dora Lam‐Himlin, David Heydt, Feriyl Bhaijee, Henry J Venbrux, Kathleen Byrnes, Lysandra Voltaggio, Norman Barker, Songyang Yuan, Elizabeth A Montgomery
Histopathology.2018; 73(2): 220. CrossRef - Large heterotopic gastric mucosa and a concomitant diverticulum in the rectum: Clinical experience and endoscopic management
Wen-Guo Chen, Hua-Tuo Zhu, Ming Yang, Guo-Qiang Xu, Li-Hua Chen, Hong-Tan Chen
World Journal of Gastroenterology.2018; 24(30): 3462. CrossRef - Gastric heterotopia in the rectum. A rare cause of ectopic gastric tissue
George A. Salem, Javid Fazili, Tauseef Ali
Arab Journal of Gastroenterology.2017; 18(1): 42. CrossRef - Gastric heterotopia in rectum: A literature review and its diagnostic pitfall
Peyman Dinarvand, Ashley A. Vareedayah, Nancy J Phillips, Christine Hachem, Jinping Lai
SAGE Open Medical Case Reports.2017;[Epub] CrossRef - Heterotopic gastric mucosa in the anus and rectum: first case report of endoscopic submucosal dissection and systematic review
Federico Iacopini, Takuji Gotoda, Walter Elisei, Patrizia Rigato, Fabrizio Montagnese, Yutaka Saito, Guido Costamagna, Giampaolo Iacopini
Gastroenterology Report.2016; 4(3): 196. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Colonic Adenocarcinoma Arising from Gastric Heterotopia: A Case Study



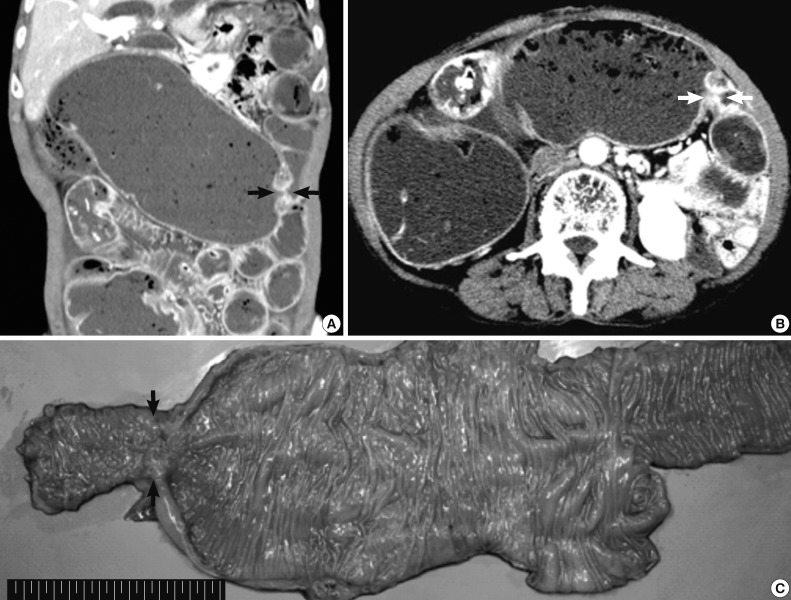
Fig. 1 Preoperative abdominal computed tomography and gross specimen. (A, B) Focal narrowing of the transverse colon (arrows) with proximal intestinal loop dilatation is detected. (C) Gross examination of the resected specimen shows focal erosion and stricture of the transverse colon (arrows).
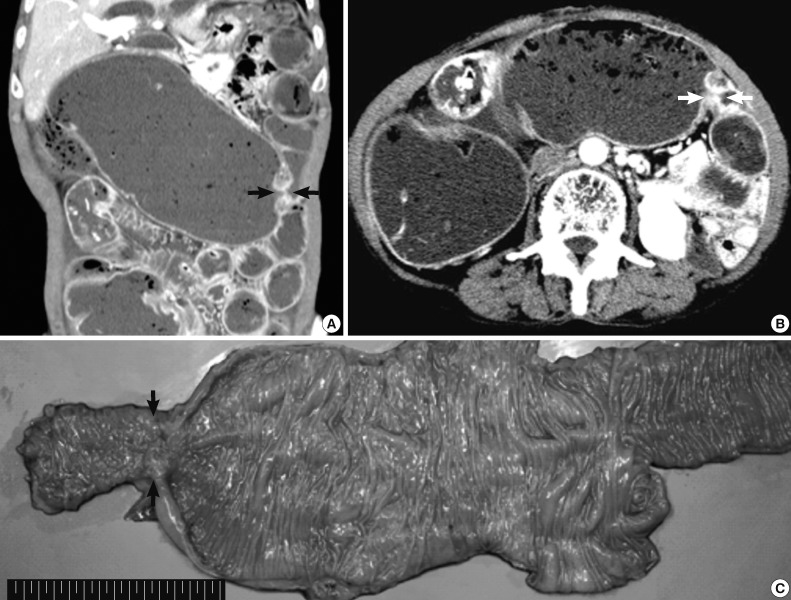
Fig. 2 Histopathologic findings of the resected specimen. (A) Hematoxylin and eosin staining shows normal colonic mucosa adjacent to heterotopic gastric mucosa with cystic dilatation. (B) High magnification view of the tissue in Fig. 2A (arrows). Heterotopic gastric mucosa is immunopositive for cytokeratin (CK) 7 (C) but negative for CK20 (D).
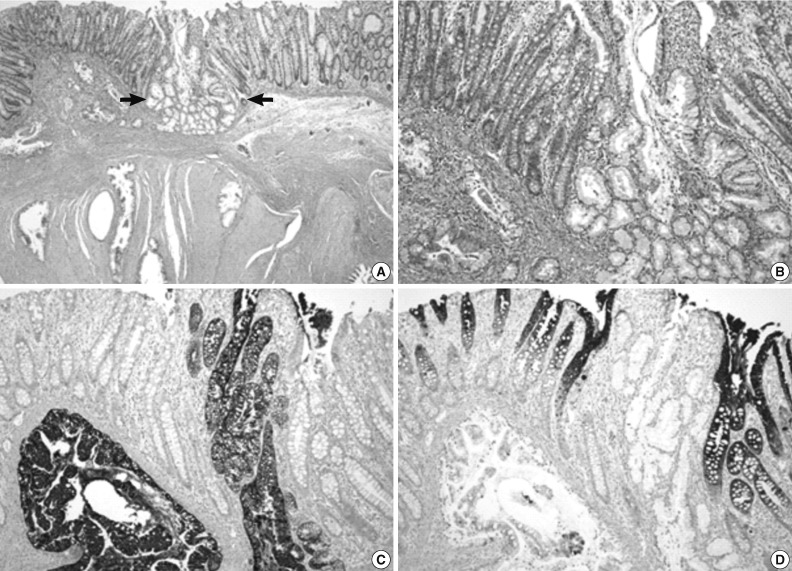
Fig. 3 Microscopic appearance of the adenocarcinoma component. (A-C) Invasive adenocarcinoma is located in an area of gastric heterotopia. Adenocarcinoma is immunopositive for cytokeratin (CK) 7 (D) but negative for CK20 (E).
Fig. 1
Fig. 2
Fig. 3
Colonic Adenocarcinoma Arising from Gastric Heterotopia: A Case Study

 E-submission
E-submission