Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(4); 2013 > Article
-
Case Study
A Giant Peritoneal Loose Body - Hyun-Soo Kim, Ji-Youn Sung1, Won Seo Park2, Youn Wha Kim1
-
Korean Journal of Pathology 2013;47(4):378-382.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.378
Published online: August 26, 2013
Department of Experimental Analysis, Aerospace Medical Center, Republic of Korea Air Force, Cheongju, Korea.
1Department of Pathology, Kyung Hee University School of Medicine, Seoul, Korea.
2Department of Surgery, Kyung Hee University School of Medicine, Seoul, Korea.
- Corresponding Author: Youn Wha Kim, M.D. Department of Pathology, Kyung Hee University School of Medicine, 26 Kyunghee-daero, Dongdaemun-gu, Seoul 130-701, Korea. Tel: +82-2-958-8743, Fax: +82-2-958-8730, kimyw@khu.ac.kr
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- A giant peritoneal loose body: A case report and updated literature review and data synthesis
Guo-Le Nie, Shicheng Chu, Song Geng, Hong Jiang, Hao Zhan
Medicine.2025; 104(50): e45956. CrossRef - Unveiling the rarity: A case report of giant peritoneal loose body
Abdudin Heru Mehammed, Natnael Alemu Bezabih, Muluken Yifru Gebresilassie, Yohanna Aregawi Hailu, Mengistu Yismie Semahegn, Misganaw Yigletie Damtie
Radiology Case Reports.2024; 19(11): 5492. CrossRef - A Case of a Fixed Giant Peritoneal Loose Body outside the Peritoneum and near the Rectovesical Excavation
Kotaro Nanno, Seiichi Shinji, Takeshi Yamada, Akihisa Matsuda, Ryo Ohta, Hiromichi Sonoda, Takuma Iwai, Kohki Takeda, Kazuhide Yonaga, Koji Ueda, Sho Kuriyama, Toshimitsu Miyasaka, Hiromasa Komori, Yoshinobu Shioda, Hiroshi Yoshida
Journal of Nippon Medical School.2023; 90(3): 276. CrossRef - A Large Intraperitoneal Free Body in a 69-Year-Old Indian Man: a Case Study
Siddhartha Sankar Bhattacharjee, Promit Chakraborty
Indian Journal of Surgery.2022; 84(1): 206. CrossRef - Peritoneal loose body presenting as a hepatic mass: A case report and review of the literature
Yang Wen, Min-jie Shang, Yan-qing Ma, Song-hua Fang, Yuan Chen
Open Medicine.2021; 16(1): 1356. CrossRef - Peritoneal Loose Body in a Patient With Ampullary Adenocarcinoma
A.V. Pradeep, Abdul Razik, Ankur Goyal, Atin Kumar, Virinder Kumar Bansal, Asuri Krishna
ACG Case Reports Journal.2021; 8(11): e00680. CrossRef - Exploratory laparoscopy as first choice procedure for the diagnosis of giant peritoneal loose body: a case report
RuiBin Li, ZhiHeng Wan, HaoTian Li
Journal of International Medical Research.2020;[Epub] CrossRef - A rare peritoneal egg: Case report with literature review
Nilu Malpani Dhoot, Shivaraj Afzalpurkar, Usha Goenka, Vinay Mahendra, Enam Murshed Khan, Arpita Sutradhar, Mahesh Goenka
Radiology Case Reports.2020; 15(10): 1895. CrossRef - A giant peritoneal loose body impacted in the pelvic cavity, a rare and interesting finding during laparotomy
Ayad A. Mohammed
International Journal of Surgery: Global Health.2020; 3(6): e24. CrossRef - Giant Mobile Intraperitoneal Loose Body
Mohd Ilyas, Mohd Yaqoob Wani, Musaib Ahmad Dar, Feroze A. Shaheen
ACG Case Reports Journal.2019; 6(1): e00006. CrossRef - Giant peritoneal loose body in a patient with end-stage renal disease
Nadejda Cojocari, Leonard David
SAGE Open Medical Case Reports.2018;[Epub] CrossRef - Two giant peritoneal loose bodies were simultaneously found in one patient: A case report and review of the literature
Qingxing Huang, Aihong Cao, Jun Ma, Zhenhua Wang, Jianhong Dong
International Journal of Surgery Case Reports.2017; 36: 74. CrossRef - Laparoscopic extraction of a giant peritoneal loose body: Case report and review of literature
Keiso Matsubara, Yuji Takakura, Takashi Urushihara, Takashi Nishisaka, Toshiyuki Itamoto
International Journal of Surgery Case Reports.2017; 39: 188. CrossRef - Symptomatic giant peritoneal loose body in the pelvic cavity: A case report
Andreas Elsner, Mikolaj Walensi, Maya Fuenfschilling, Robert Rosenberg, Robert Mechera
International Journal of Surgery Case Reports.2016; 21: 32. CrossRef - A Case of a Peritoneal Loose Body with the Maximum Diameter of 50 mm
Yoshihiro MOCHIZUKI, Hiroshi IINO, Michio HARA, Syugo SHIBA, Makoto SUDO, Naoki OISHI, Tetsuo KONDO
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2016; 77(10): 2552. CrossRef - Giant peritoneal loose body in the pelvic cavity confirmed by laparoscopic exploration: a case report and review of the literature
Hong Zhang, Yun-zhi Ling, Ming-ming Cui, Zhi-xiu Xia, Yong Feng, Chun-sheng Chen
World Journal of Surgical Oncology.2015;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


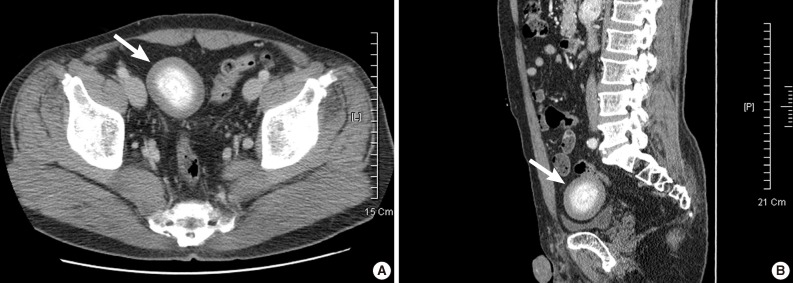
Fig. 1
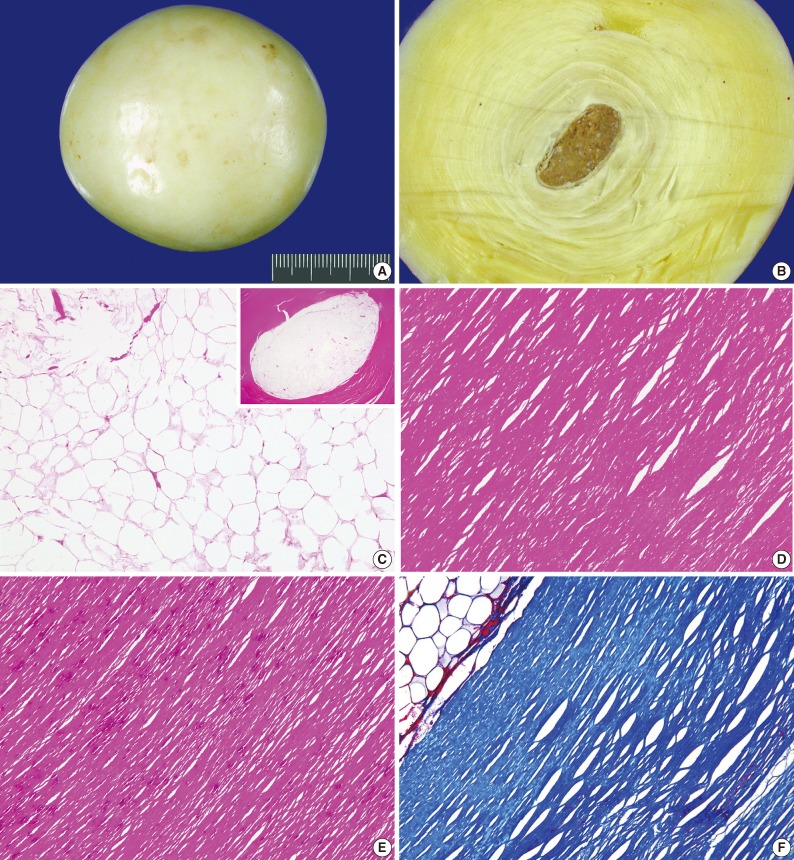
Fig. 2
| Authors | Age/Sex | Presenting symptoms or signs | Imaging findings | Preoperative diagnosis | Maximal diameter (cm) | Location | Surgical approach |
|---|---|---|---|---|---|---|---|
| Burns and Rogers [14] | 33 yr/F | Pelvic pain | Calcified mass | Not available | 1.8 | LUQ | Open |
| Bhandarwar et al. [5] | 65 yr/M | Acute uninary retention | Concentric radio-opaque shadow | Not available | 9.0 | RVP | Open |
| Takada et al. [2] | 79 yr/M | Incidental | Calcified mass | Leiomyoma | 7.0 | RVP | Open |
| Nomura et al. [12] | 63 yr/M | Incidental | Egg-shaped mass with calcification | Leiomyoma | 5.0 | PC | Laparoscopy |
| Asabe et al. [15] | 2 mo/F | Uninary tract infection | Cystic mass with calcification | Not available | 3.0 | PC | Laparoscopy |
| Ooyagi et al. [16] | 65 yr/M | Abdominal discomfort | Egg-shaped mass with calcification | Not available | 4.0 | RLQ | Not available |
| Takabe et al. [3] | 68 yr/M | Small bowel obstruction | Oval-shaped stone with calcification | Gallstone ileus | 4.2 | RLQ | Open |
| Ghosh et al. [4] | 63 yr/M | Small bowel obstruction | Oval-shaped stone with calcification | Gallstone ileus | 5.8 | PC | Open |
| Mohri et al. [8] | 73 yr/M | Abdominal pain | Oval-shaped stone with calcification | Peritoneal loose body | 9.5 | RVP | Open |
| Takayama et al. [11] | 63 yr/M | Abdominal discomfort | Egg-shaped mass with central low-intensity area | Not available | 4.5 | PC | Laparoscopy |
| Koga et al. [17] | 33 yr/F | Infertility | Oval-shaped filling detect | Not available | 3.0 | VUP | Laparoscopy |
| Hedawoo and Wagh [13] | 65 yr/M | Intermittent constipation | Heterogeneously enhancing mass with calcification | Duplication cyst | 9.5 | RLQ | Open |
| Gayer and Petrovitch [10] | 59 yr/M | Incidental | Round mass with calcification | Metastatic tumor | 3.0 | PC | Not available |
| Sewkani et al. [9] | 64 yr/M | Small bowel obstruction | Not available | Not available | 7.0 | PC | Open |
| Jang et al. [18] | 60 yr/M | Incidental | Oval-shaped mass with calcification | Leiomyoma | 4.5 | PC | Laparoscopy |
| Nozu and Okamura [19] | 67 yr/M | Incidental | Well-defined mass with a central low-intensity area | Pancreatic cancer | 4.0 | PC | Not available |
| Present case | 50 yr/M | Incidental | Oval-shaped mass with calcification | Calcifying fibrous pseudotumor | 7.5 | PC | Laparoscopy |
F, female; LUQ, left upper quadrant; M, male; RVP, rectovesical pouch; PC, pelvic cavity; VUP, vesicouterine pouch; RLQ, right lower quadrant.

 E-submission
E-submission