Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(6); 2013 > Article
-
Original Article
Prognostic Significance of Absolute Lymphocyte Count/Absolute Monocyte Count Ratio at Diagnosis in Patients with Multiple Myeloma - Su-Jin Shin, Jin Roh, Misung Kim, Min Jung Jung, Young Wha Koh, Chan-Sik Park, Dok Hyun Yoon1, Cheolwon Suh1, Chan-Jeong Park2, Hyun Sook Chi2, Jooryung Huh
-
Korean Journal of Pathology 2013;47(6):526-533.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.526
Published online: December 24, 2013
Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
1Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
2Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- Corresponding Author: Jooryung Huh, M.D. Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, 88 Olympic-ro 43-gil, Songpa-gu, Seoul 138-736, Korea. Tel: +82-2-3010-4553, Fax: +82-2-472-7898, jrhuh@amc.seoul.kr
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Low peripheral blood B lymphocyte count predicts poor outcome in patients with multiple myeloma
Yuqi Wang, Zhongxin Zheng, Qiaoxi Kang, Linjing Cai, Shanshan Zhang, Huan Chen, Youhai Yuan, Hanzhen Zhang, Xiaolei Wei, Ru Feng, Yongqiang Wei
Immunobiology.2025; 230(4): 153096. CrossRef - Variation of peripheral blood-based biomarkers for response of anti-PD-1 immunotherapy in non-small-cell lung cancer
Xiaoming Wang, Dayu Chen, Yuyan Ma, Dongping Mo, Feng Yan
Clinical and Translational Oncology.2024; 26(8): 1934. CrossRef - Descriptive analysis and prognostic factors in cats with myeloma‐related disorders: A multicenter retrospective study of 50 cases
Lorris Lecot, Isabelle Desmas‐Bazelle, Sarah Benjamin, Pauline De Fornel, Frédérique Ponce, Matthew Kornya, Loïc Desquilbet, Claire Beaudu‐Lange, Catherine Ibisch, David Sayag, Ghita Benchekroun, Jérémy Béguin
Journal of Veterinary Internal Medicine.2024; 38(3): 1693. CrossRef - Clinical features and treatment of newly diagnosed multiple myeloma with secondary myelofibrosis: a retrospective study
Han Xu, Yujie Xu, Mengying Wang, Chunxia Mao, Junxia Huang, Tianlan Li, Yan Gao, Shanshan Liu, Jingjing Zhou, Yi Zhang, Xianqi Feng
Therapeutic Advances in Hematology.2024;[Epub] CrossRef - Definers and drivers of functional high-risk multiple myeloma: insights from genomic, transcriptomic, and immune profiling
Rahul Banerjee, Kara I. Cicero, Sarah S. Lee, Andrew J. Cowan
Frontiers in Oncology.2023;[Epub] CrossRef - Normal Absolute Monocyte Count in Combination with Normal/High Absolute Lymphocyte Count at the Time of Relapse is Associated with Improved Survival in Patients with Early Relapsed Acute Myeloid Leukemia
Yu Zhang, Kanchun Dai, Qianying Zhang, Yisha Huang, Yiyun Feng, Deeksha Bhardwaj, Kang Yu, Jianhua Feng
Cancer Investigation.2021; 39(6-7): 550. CrossRef - Real World Experience of Daratumumab: Evaluating Lymphopenia and Adverse Events in Multiple Myeloma Patients
Francesca Cottini, Ying Huang, Nita Williams, Naresh Bumma, Abdullah M. Khan, Maria Chaudhry, Srinivas Devarakonda, Yvonne A. Efebera, Don M. Benson, Ashley E. Rosko
Frontiers in Oncology.2021;[Epub] CrossRef - Are the Derived Indexes of Peripheral Whole Blood Cell Counts (NLR, PLR, LMR/MLR) Clinically Significant Prognostic Biomarkers in Multiple Myeloma? A Systematic Review And Meta-Analysis
Xinwen Zhang, Jialin Duan, Zhenyu Wen, Hao Xiong, Xiaomin Chen, Yang Liu, Kunyu Liao, Chunlan Huang
Frontiers in Oncology.2021;[Epub] CrossRef - Combined immune score of lymphocyte to monocyte ratio and immunoglobulin levels predicts treatment-free survival of multiple myeloma patients after autologous stem cell transplant
Karen Sweiss, Jonathan Lee, Nadim Mahmud, Gregory S. Calip, Youngmin Park, Dolores Mahmud, Damiano Rondelli, Pritesh R. Patel
Bone Marrow Transplantation.2020; 55(1): 199. CrossRef - Low absolute CD4+ T cell counts in peripheral blood predict poor prognosis in patients with newly diagnosed multiple myeloma
Yan Gu, Yuanyuan Jin, Jie Ding, Wu Yujie, Qinglin Shi, Xiaoyan Qu, Sishu Zhao, Jianyong Li, Chen Lijuan
Leukemia & Lymphoma.2020; 61(8): 1869. CrossRef Normal Absolute Monocyte Count at the Time of Relapse is Associated with Improved Survival After First Salvage Therapy in Adult Patients with Early Relapsed B-Lineage Acute Lymphoblastic Leukemia
Yi-fen Shi, Na Wang, Zi-yang Huang, Rong-rong Chen, Yi-sha Huang, Yi-yi Zhu, Chong-yun Xing, Bin Liang, Kang Yu, Jian-hua Feng
Cancer Management and Research.2020; Volume 12: 7097. CrossRef- Peripheral blood biomarkers of early immune reconstitution in newly diagnosed multiple myeloma
Moritz Binder, S. Vincent Rajkumar, Martha Q. Lacy, Morie A. Gertz, Francis K. Buadi, Angela Dispenzieri, Yi L. Hwa, Amie Fonder, Miriam Hobbs, Suzanne R. Hayman, Steven R. Zeldenrust, John A. Lust, Stephen J. Russell, Nelson Leung, Prashant Kapoor, Ronal
American Journal of Hematology.2019; 94(3): 306. CrossRef - Effect of absolute monocyte count post-transplant on the outcome of patients with acute myeloid leukemia undergoing myeloablative allogeneic hematopoietic stem cell transplant with busulfan and cyclophosphamide conditioning
Liyuan Tang, Na Wang, Chongyun Xing, Qiang Zhuang, Bin Liang, Lan Sun, Yi Chen, Yan Qian, Zhijian Shen, Songfu Jiang, Kang Yu, Jianhua Feng
Leukemia Research.2018; 69: 60. CrossRef - A lower ALC/AMC ratio is associated with poor prognosis of peripheral T-cell lymphoma-not otherwise specified
Qian Li, Shuang Gao, Jing Ma, Su Liu, Yuanfang Yue, Lin Chen, Han Li, Xue Wang, Dongying Li, Zeng Cao, Zhigang Zhao, Xiaofang Wang, Yong Yu, Yizhuo Zhang, Yafei Wang
Leukemia Research.2018; 73: 5. CrossRef - Peripheral Blood Lymphocyte-to-Monocyte Ratio as a Useful Prognostic Factor in Newly Diagnosed Multiple Myeloma
Ying Tian, Yue Zhang, Wan-Qiu Zhu, Xiao-Lei Chen, He-Bing Zhou, Wen-Ming Chen
BioMed Research International.2018; 2018: 1. CrossRef - Significance of the absolute lymphocyte/monocyte ratio as a prognostic immune biomarker in newly diagnosed multiple myeloma
T Dosani, F Covut, R Beck, J J Driscoll, M de Lima, E Malek
Blood Cancer Journal.2017; 7(6): e579. CrossRef - Lymphocyte-to-monocyte ratio can predict mortality in pancreatic adenocarcinoma
Gurshawn Singh, Ammar Nassri, David Kim, Hong Zhu, Zeeshan Ramzan
World Journal of Gastrointestinal Pharmacology and Therapeutics.2017; 8(1): 60. CrossRef - Bone marrow microenvironmental CD4 + and CD8 + lymphocyte infiltration patterns define overall- and progression free survival in standard risk multiple myeloma – an analysis from the Austrian Myeloma Registry
Wolfgang Willenbacher, Ella Willenbacher, Claudia Zelle-Rieser, Rainer Biedermann, Roman Weger, Karin Jöhrer, Andrea Brunner
Leukemia & Lymphoma.2016; 57(6): 1478. CrossRef - Absolute lymphocyte count as a prognostic marker in newly diagnosed multiple myeloma patients
C. Suriu, L. Akria, D. Azoulay, E. Shaoul, M. Barhoum, A. Braester
International Journal of Laboratory Hematology.2016;[Epub] CrossRef - The Peripheral Blood Mononuclear Cell Count Is Associated With Bone Health in Elderly Men
Xianfeng Lin, Hejun Yu, Chenchen Zhao, Yu Qian, Dun Hong, Kangmao Huang, Jian Mo, An Qin, Xiangqian Fang, Shunwu Fan
Medicine.2016; 95(15): e3357. CrossRef - Prognostic role of lymphocyte to monocyte ratio for patients with cancer: evidence from a systematic review and meta-analysis
Liangyou Gu, Hongzhao Li, Luyao Chen, Xin Ma, Xintao Li, Yu Gao, Yu Zhang, Yongpeng Xie, Xu Zhang
Oncotarget.2016; 7(22): 31926. CrossRef - Do lymphocytes count in myeloma? Are we absolutely sure?
Tamar Tadmor
Leukemia & Lymphoma.2015; 56(5): 1193. CrossRef - Absolute lymphocyte count is unrelated to overall survival in newly diagnosed elderly patients with multiple myeloma treated with immunomodulatory drugs
Mariasanta Napolitano, Giorgia Saccullo, Roberto Bono, Antonio Branca, Clotilde Cangialosi, Salvatrice Mancuso, Simona Raso, Gerlando Quintini, Maria Grazia Lipari, Francesco Fabbiano, Giorgina Specchia, Alberto Dolce, Francesco Di Raimondo, Sergio Siragu
Leukemia & Lymphoma.2015; 56(5): 1507. CrossRef - Distinct Transcriptional and Anti-Mycobacterial Profiles of Peripheral Blood Monocytes Dependent on the Ratio of Monocytes: Lymphocytes
Vivek Naranbhai, Helen A. Fletcher, Rachel Tanner, Matthew K. O'Shea, Helen McShane, Benjamin P. Fairfax, Julian C. Knight, Adrian V.S. Hill
EBioMedicine.2015; 2(11): 1619. CrossRef - Prognostic value of absolute monocyte count in chronic lymphocytic leukaemia
László Szerafin, János Jakó, Ferenc Riskó
Orvosi Hetilap.2015; 156(15): 592. CrossRef - The lymphocyte to monocyte ratio in peripheral blood represents a novel prognostic marker in patients with pancreatic cancer
Michael Stotz, Joanna Szkandera, Tatjana Stojakovic, Julia Seidel, Hellmut Samonigg, Peter Kornprat, Renate Schaberl-Moser, Fridericke Seggewies, Gerald Hoefler, Armin Gerger, Martin Pichler
Clinical Chemistry and Laboratory Medicine (CCLM).2015;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


Fig. 1
Fig. 2
| Characteristic | ALC < 1,400 cells/µL | ALC ≥ 1,400 cells/µL | p-value | AMC < 490 cells/µL | AMC ≥ 490 cells/µL | p-value | ALC/AMC < 2.9 | ALC/AMC ≥ 2.9 | p-value |
|---|---|---|---|---|---|---|---|---|---|
| Age | 60 (31-81) | 60 (29-84) | .939 |
60 (29-81) | 60 (31-84) | .934 |
62 (31-84) | 59 (29-81) | .130 |
| Sex | .459 |
< .0001 |
.011 |
||||||
| Male | 41 (41.8) | 57 (58.2) | 55 (56.1) | 43 (43.9) | 36 (36.7) | 62 (63.3) | |||
| Female | 33 (36.3) | 58 (63.7) | 77 (84.6) | 14 (15.4) | 18 (19.8) | 73 (80.2) | |||
| International Staging System (ISS) | .004 |
.195 |
.142 |
||||||
| I | 8 (22.9) | 27 (77.1) | 27 (77.1) | 8 (22.9) | 7 (20.0) | 28 (80.0) | |||
| II | 29 (33.3) | 58 (66.7) | 62 (71.3) | 25 (28.7) | 23 (26.4) | 64 (73.6) | |||
| III | 33 (54.1) | 28 (45.9) | 37 (60.7) | 24 (39.3) | 23 (37.7) | 38 (62.3) | |||
| Durie-Salmon stage | .745 |
.641 |
.263 |
||||||
| I | 6 (28.6) | 15 (71.4) | 15 (71.4) | 6 (28.6) | 8 (38.1) | 13 (61.9) | |||
| II | 22 (42.3) | 30 (57.7) | 37 (71.2) | 15 (28.8) | 12 (23.1) | 40 (76.9) | |||
| IIIA | 35 (39.3) | 54 (60.7) | 64 (71.9) | 25 (28.1) | 23 (25.8) | 66 (74.2) | |||
| IIIB | 11 (40.7) | 16 (59.3) | 16 (59.3) | 11 (40.7) | 11 (40.7) | 16 (59.3) | |||
| Morphology | .027 |
.112 |
.008 |
||||||
| Plasmablastic | 29 (50.9) | 28 (49.1) | 33 (57.9) | 24 (42.1) | 26 (45.6) | 31 (54.4) | |||
| Plasmacytic | 32 (32.3) | 67 (67.7) | 71 (71.7) | 28 (28.3) | 24 (24.2) | 75 (75.8) | |||
| Bone lesion | .233 |
1.000 |
.873 |
||||||
| ≥ 3 lytic bone lesions | 42 (43.8) | 54 (56.3) | 67 (69.8) | 29 (30.2) | 28 (29.2) | 68 (70.8) | |||
| < 3 lytic bone lesions | 32 (34.4) | 61 (65.6) | 65 (69.9) | 28 (30.1) | 26 (28.0) | 67 (72.0) | |||
| β2m (mg/L) | 8.98 (0.89-82.50) | 7.80 (1.40-65.80) | .122 |
6.47 (0.89-48.40) | 12.20 (1.60-82.50) | .015 |
10.96 (0.89-82.50) | 7.14 (1.00-63.80) | .087 |
| Albumin (g/dL) | 3.00 (0.90-10.70) | 3.22 (1.10-4.60) | .004 |
3.12 (0.90-10.70) | 3.17 (0.90-4.60) | .316 |
2.99 (0.90-4.50) | 3.19 (0.90-10.70) | .265 |
| Cr (mg/dL) | 1.70 (0.50-14.40) | 1.75 (0.39-18.70) | .976 |
1.50 (0.50-14.40) | 2.27 (0.39-18.70) | .014 |
2.22 (0.39-18.70) | 1.53 (0.50-8.50) | .282 |
| Hb (g/dL) | 9.81 (6.40-14.80) | 10.68 (5.50-15.40) | .005 |
10.17 (5.50-15.40) | 10.74 (6.30-15.00) | .085 |
10.48 (6.30-14.80) | 10.29 (5.50-15.40) | .510 |
| Ca (mg/dL) | 9.13 (4.00-14.60) | 9.35 (6.70-15.10) | .131 |
9.14 (4.00-14.10) | 9.56 (7.10–15.10) | .098 |
9.57 (7.10-15.10) | 9.14 (4.00-13.80) | .928 |
| Serum protein (g/dL) | 8.22 (3.90-17.00) | 8.17 (4.70-13.60) | .453 |
8.30 (3.90-17.00) | 7.93 (4.70-12.50) | .280 |
7.90 (4.60-12.50) | 8.30 (3.90-17.00) | .373 |
| 24 hr urine protein (mg/day) | 2,092 (11-13,947) | 2,123 (9-14,286) | .912 |
2,049 (9-14,286) | 2,261 (11-13,947) | .793 |
1,749 (11-13,947) | 2,250 (9-14,286) | .238 |
| WBC count (× 109/L) | 5.72 (2.40-12.70) | 6.86 (2.90-17.40) | .001 |
5.55 (2.40-16.00) | 8.40 (4.40-17.40) | < .0001 |
7.44 (2.40-17.00) | 5.99 (2.40-17.40) | .003 |
| Platelets (× 109/L) | 176 (23-461) | 225 (39-663) | .001 |
194 (31-523) | 231 (23-663) | .028 |
199 (23-663) | 208 (38-584) | .448 |
| Factor | HR | 95% CI | p-value | |
|---|---|---|---|---|
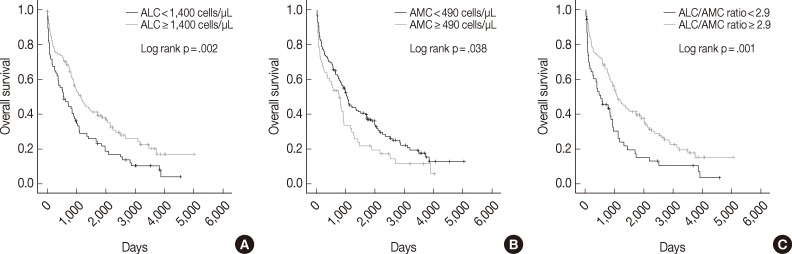
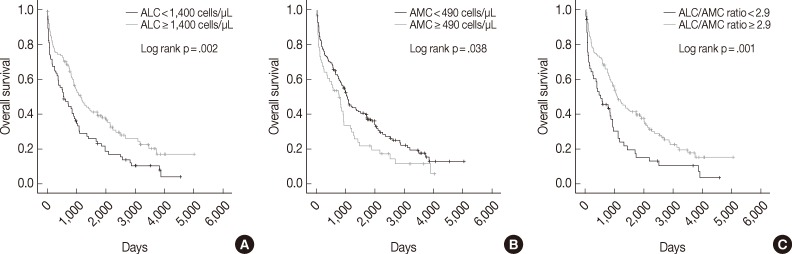
| ALC (cells/µL) | ≥ 1,400 vs < 1,400 | 1.649 | 1.189-2.286 | .002 |
| AMC (cells/µL) | < 490 vs ≥ 490 | 1.443 | 1.018-2.045 | .038 |
| ALC/AMC ratio | ≥ 2.9 vs < 2.9 | 1.772 | 1.249-2.514 | .001 |
| Morphology | Plasmacytic vs plasmablastic | 1.552 | 1.081-2.228 | .016 |
| Age (yr) | < 65 vs ≥ 65 | 1.793 | 1.279-2.513 | .001 |
| ISS | I | 1 | ||
| II | 2.148 | 1.258-3.670 | .005 | |
| III | 4.360 | 2.526-7.523 | < .0001 | |
| D-S stage | I | 1 | ||
| II | 1.982 | 1.061-3.702 | .032 | |
| IIIA | 1.403 | 0.769-2.560 | .270 | |
| IIIB | 3.368 | 1.712-6.627 | < .0001 | |
| β2-Microglobulin (mg/L) | < 3.5 vs ≥ 3.5 | 2.128 | 1.468-3.084 | < .0001 |
| Albumin (g/dL) | < 3.5 vs ≥ 3.5 | 1.573 | 1.115-2.219 | .009 |
| Bone lesion (lytic bone lesions) | < 3 vs ≥ 3 | 1.108 | 0.799-1.535 | .539 |
| Treatment type | ASCT vs no ASCT | 2.345 | 1.637-3.359 | < .0001 |
| Factors | HR | 95% CI | p-value | HR | 95% CI | p-value | |
|---|---|---|---|---|---|---|---|
| ALC (cells/µL) | ≥ 1,400 vs < 1,400 | 1.389 | 0.933-2.069 | .106 | |||
| AMC (cells/µL) | < 490 vs ≥ 490 | 1.415 | 0.928-2.157 | .107 | |||
| ALC/AMC ratio | ≥ 2.9 vs < 2.9 | 1.511 | 1.006-2.272 | .047 | |||
| Morphology | Plasmacytic vs plasmablastic | 1.396 | 0.940-2.074 | .099 | 1.366 | 0.917-2.033 | .125 |
| Age (yr) | < 65 vs ≥ 65 | 1.441 | 0.949-2.189 | .087 | 1.388 | 0.910-2.116 | .128 |
| ISS | I | 1 | 1 | ||||
| II | 1.129 | 0.543-2.348 | .745 | 1.122 | 0.540-2.331 | .757 | |
| III | 1.799 | 0.824-3.925 | .140 | 2.048 | 0.947-4.429 | .069 | |
| D-S stage | I | 1 | 1 | ||||
| II | 1.089 | 0.454-2.611 | .849 | 1.151 | 0.482-2.750 | .751 | |
| IIIA | 0.997 | 0.427-2.326 | .994 | 1.099 | 0.479-2.520 | .824 | |
| IIIB | 1.786 | 0.681-4.683 | .239 | 1.899 | 0.725-4.975 | .192 | |
| Treatment type | ASCT vs no ASCT | 2.252 | 1.405-3.610 | .001 | 2.131 | 1.337-3.396 | .001 |
| Characteristics | ALC < 1,400 cells/µL |
AMC ≥ 490 cells/µL |
ALC/AMC < 2.9 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| HR | 95% CI | p-value | HR | 95% CI | p-value | HR | 95% CI | p-value | |
| Treatment | |||||||||
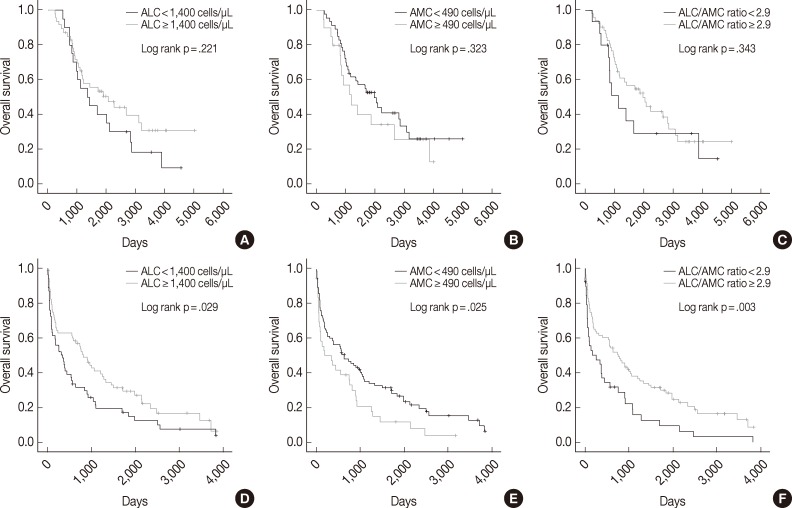
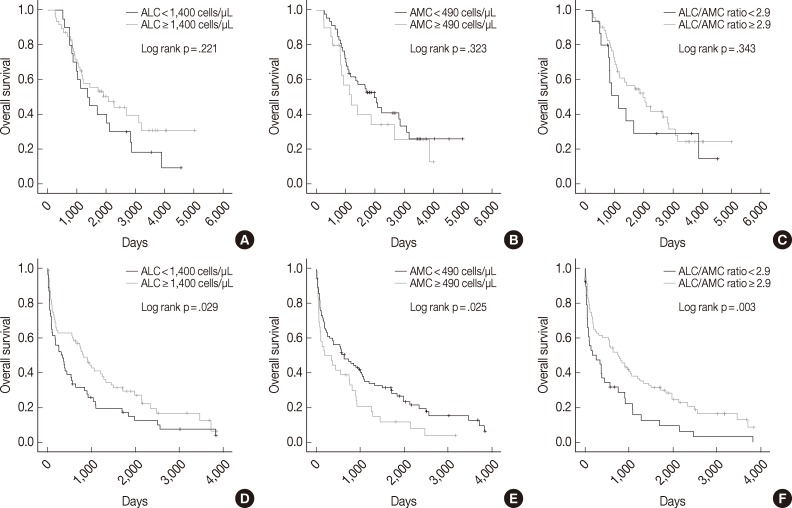
| ASCT (n = 67) | 1.459 | 0.794-2.679 | .221 | 1.376 | 0.728-2.600 | .323 | 1.393 | 0.700-2.769 | .343 |
| No ASCT (n = 122) | 1.542 | 1.043-2.281 | .029 | 1.613 | 1.058-2.457 | .025 | 1.850 | 1.227-2.789 | .003 |
| Age (yr) | |||||||||
| < 65 (n = 121) | 1.728 | 1.139-2.622 | .009 | 1.517 | 0.971-2.369 | .065 | 1.843 | 1.163-2.920 | .008 |
| ≥ 65 (n = 68) | 1.606 | 0.934-2.762 | .084 | 1.323 | 0.752-2.327 | .330 | 1.408 | 0.812-2.442 | .221 |
| Sex | |||||||||
| Male (n = 98) | 2.112 | 1.351-3.301 | .001 | 1.259 | 0.806-1.967 | .310 | 1.719 | 1.091-2.708 | .018 |
| Female (n = 91) | 1.245 | 0.764-2.028 | .379 | 1.433 | 0.748-2.744 | .276 | 1.559 | 0.873-2.784 | .130 |
| ISS | |||||||||
| I (n = 35) | 1.303 | 0.451-3.761 | .624 | 6.865 | 2.408-19.576 | < .0001 | 3.169 | 1.166-8.617 | .017 |
| II (n = 87) | 1.720 | 1.044-2.834 | .031 | 0.982 | 0.563-1.712 | .949 | 1.209 | 0.693-2.110 | .504 |
| III (n = 61) | 0.936 | 0.554-1.580 | .804 | 1.171 | 0.683-2.005 | .566 | 2.011 | 1.172-3.450 | .010 |
Values are presencted as mean (range) or number (%). ALC, absolute lymphocyte count; AMC, absolute monocyte count; β2m, β2-microglobulin; Cr, creatinine; Hb, hemoglobin; Ca, calcium; WBC, white blood cell. Mann-Whitney U test; Two-sided Fisher’s exact test; Two-sided Pearson’s chi-square test.
ALC, absolute lymphocyte count; AMC, absolute monocyte count; OS, overall survival; HR, hazard ratio; CI, confidence interval; ISS, International Staging System; D-S stage, Durie-Salmon stage; ASCT, autologous stem cell transplantation.
ALC, absolute lymphocyte count; AMC, absolute monocyte count; OS, overall survival; HR, hazard ratio; CI, confidence interval; ISS, International Staging System; D-S stage, Durie-Salmon stage; ASCT, autologous stem cell transplantation.
OS, overall survival; ALC, absolute lymphocyte count; AMC, absolute monocyte count; HR, hazard ratio; CI, confidence interval; ASCT, autologous stem cell transplantation; ISS, International Staging System.

 E-submission
E-submission