Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(3); 2014 > Article
-
Case Study
Well-Differentiated Papillary Mesothelioma of the Tunica Vaginalis: A Case Study and Review of the Literature - Seyda Erdogan, Arbil Acikalin, Handan Zeren1, Gulfılız Gonlusen, Suzan Zorludemir, Volkan Izol2
-
Korean Journal of Pathology 2014;48(3):225-228.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.3.225
Published online: June 26, 2014
Department of Pathology, School of Medicine, Cukurova University, Adana, Turkey.
1Department of Pathology, School of Medicine, Acibadem University, Adana, Turkey.
2Department of Urology, School of Medicine, Cukurova University, Adana, Turkey.
- Corresponding Author: Seyda Erdogan, M.D. Department of Pathology, School of Medicine, Cukurova University, 01330 Adana, Turkey. Tel: +90-322-3386060 (ext. 3158), Fax: +90-322-3386956, seydaer@cu.edu.tr
• Received: May 7, 2012 • Revised: June 21, 2012 • Accepted: July 23, 2012
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Testicular/paratesticular mesothelial tumours: Uncommon histopathologic entities in a very complex anatomical site
Francesca Pagliuca, Stefano Lucà, Marco De Sio, Davide Arcaniolo, Gaetano Facchini, Marco De Martino, Francesco Esposito, Ferdinando DE Vita, Paolo Chieffi, Renato Franco
Pathology - Research and Practice.2024; 253: 155069. CrossRef - Well-differentiated Papillary Mesothelial Tumour of the Tunica Vaginalis Testis – A Rare Lesion, but one Pathologists Should Know About Two Patient Reports and a Review of the Literature
Johannes Kläger, Felicitas Oberndorfer, Cristophe Brunel, Julian Veser, Eva Compérat
International Journal of Surgical Pathology.2023; 31(6): 1126. CrossRef - A diagnostic approach to paratesticular lesions with tubulopapillary architecture: a series of 16 serous borderline tumors/low-grade serous carcinoma and 14 well-differentiated papillary mesothelial tumors and mesothelioma
Rabia Zafar, Lacey J. Schrader, John C. Cheville, J. Kenneth Schoolmeester, Anja C. Roden, Marie-Christine Aubry, Eunhee S. Yi, Aditya Raghunathan, Loren Herrera-Hernandez, R. Houston Thompson, Stephen A. Boorjian, Bradley C. Leibovich, Gary L. Keeney, Ra
Human Pathology.2022; 128: 31. CrossRef - Mesothelioma subtypes of the tunica vaginalis: a rare case report and review of histological criteria
Cutts Rebecca, Martin J Connor, Luxi Sun, Thomas Johnston, Rachel Gooch, John McLoughlin
Journal of Surgical Case Reports.2019;[Epub] CrossRef - Well‐differentiated papillary mesothelioma of tunica vaginalis testis of unknown malignant potential: Sonographic appearance
K.W.S. Ko, K.S. Tse, K.W. Shek, M.N. Hau, S.H. Ting
Journal of Clinical Ultrasound.2018; 46(5): 364. CrossRef - Tunica Vaginalis Thickening, Hemorrhagic Infiltration and Inflammatory Changes in 8 Children with Primary Hydrocele; Reactive Mesothelial Hyperplasia? A Prospective Clinical Study
Ioannis Patoulias, Evangelia Rachmani, Maria Kalogirou, Kyriakos Chatzopoulos, Dimitrios Patoulias
Acta Medica (Hradec Kralove, Czech Republic).2018; 61(2): 41. CrossRef - A 45-year-old man presenting with chest pain
Sheetu Singh, Arpita Jindal
Lung India.2018; 35(2): 171. CrossRef - Two Case Reports of Benign Testicular Mesothelioma and Review of the Literature
Cristobal Ramirez Sevilla, Carme Admella Salvador, Josep Feliu Canaleta, Juan Llopis Manzanera, Miguel Angel Barranco Sanz, Juan Antoni Romero Martin, Sergi Bernal Salguero, Francesco A. Mauri
Case Reports in Oncological Medicine.2017;[Epub] CrossRef - Well-differentiated Papillary Mesothelioma of the Tunica Vaginalis
Wei Keith Tan, Mae-Yen Tan, Hui Meng Tan, Rajadurai Pathmanathan, Wei Phin Tan
Urology.2016; 90: e7. CrossRef - Well-Differentiated Papillary Mesothelioma of the Tunica Vaginalis: Case Report and Systematic Review of Literature
Wei Keith Tan, Mae-Yen Tan, Wei Shen Tan, Soon Ching Gan, Rajadurai Pathmanathan, Hui Meng Tan, Wei Phin Tan
Clinical Genitourinary Cancer.2016; 14(4): e435. CrossRef - The legacy of the F344 rat as a cancer bioassay model (a retrospective summary of three common F344 rat neoplasms)
Robert R. Maronpot, Abraham Nyska, Jennifer E. Foreman, Yuval Ramot
Critical Reviews in Toxicology.2016; 46(8): 641. CrossRef - Malignant Mesothelioma of the Tunica Vaginalis: A Rare Neoplasm—Case Report and Literature Review
Manuel Segura-González, Jorge Urias-Rocha, Jorge Castelán-Pedraza
Clinical Genitourinary Cancer.2015; 13(6): e401. CrossRef - In vivo Optical Coherence Tomography Imaging of the Mesothelium Using Developed Window Models
Yeh-Chan Ahn, Yu-Gyeong Chae, Sang Seok Hwang, Bong-Kwon Chun, Maan Hong Jung, Sung Jin Nam, Hae-Young Lee, Jae Min Chung, Chulho Oak, Eun-Kee Park
Journal of the Optical Society of Korea.2015; 19(1): 69. CrossRef
Well-Differentiated Papillary Mesothelioma of the Tunica Vaginalis: A Case Study and Review of the Literature





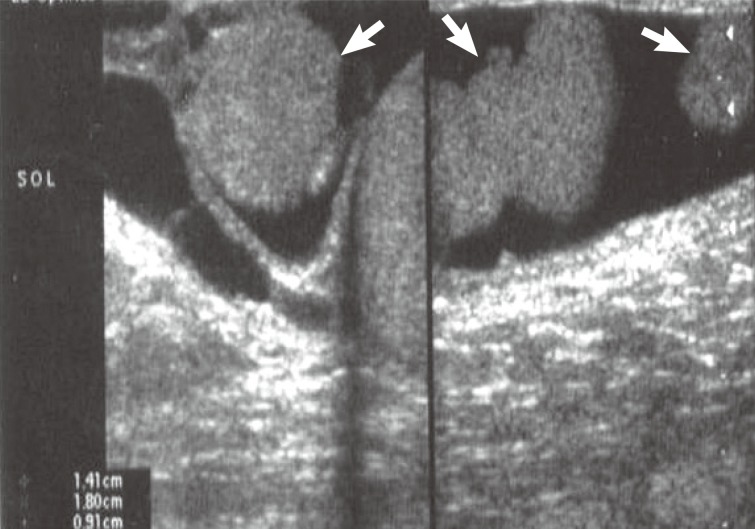
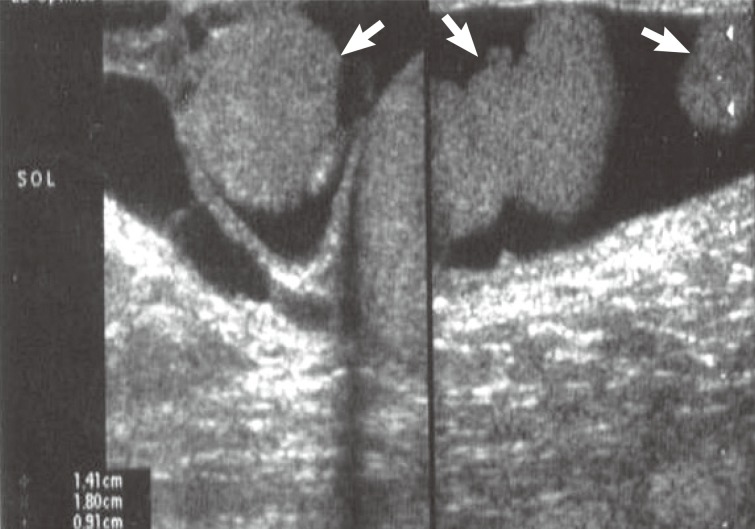
Fig. 1 Ultrasonography shows three hypoechoic nodules measuring 2 cm, 1.4 cm, and 0.9 cm in the wall of hydrocele sac (arrows).
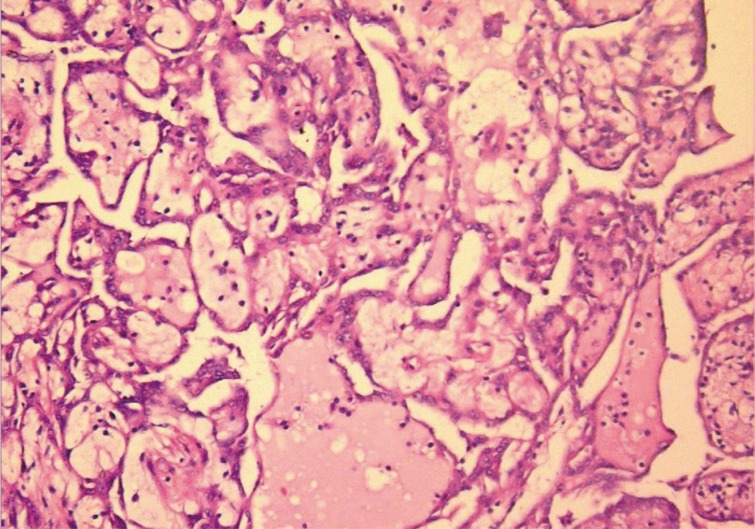
Fig. 2 Tumor mass in the tunica vaginalis is composed of multiple branching, papillary structures with a fibrovascular core.
Fig. 3 Papillary structures are lined by bland-looking cuboidal epithelium.
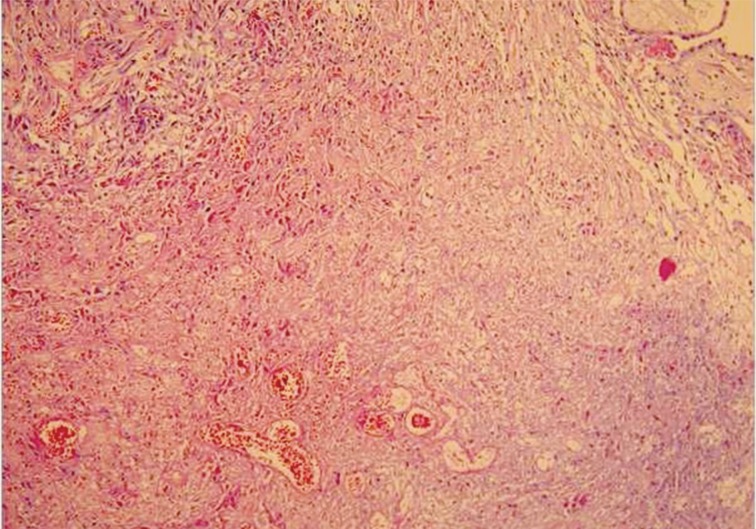
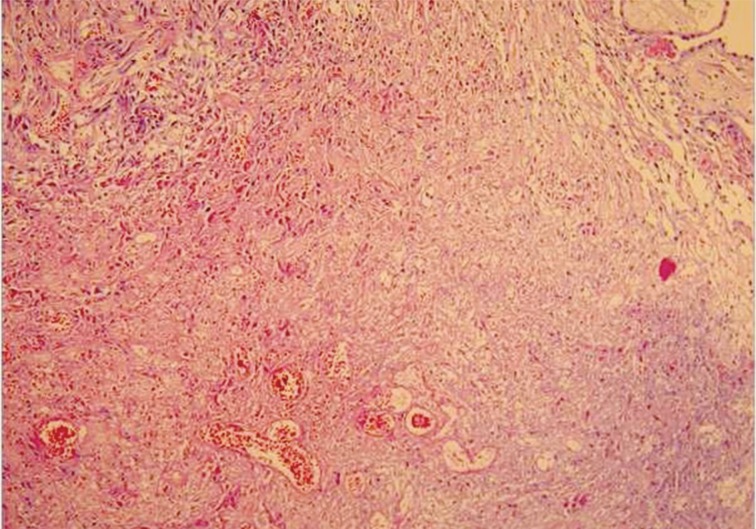
Fig. 4 A focal area of coagulative necrosis is present in the tumor.
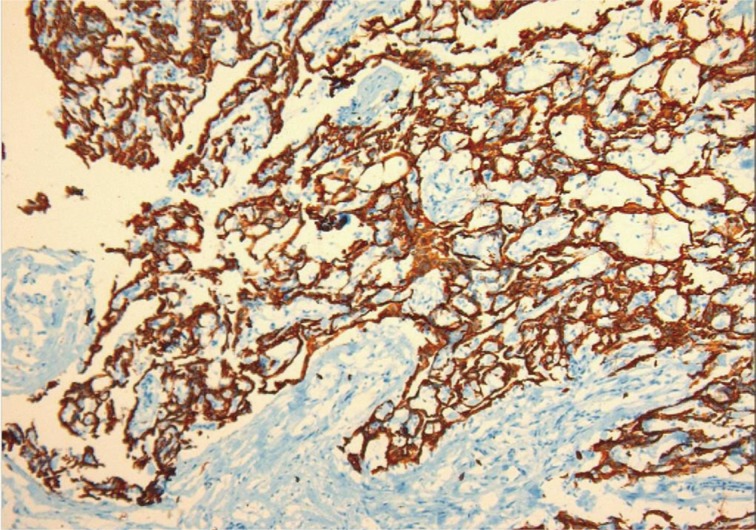
Fig. 5 Mesothelial cells show diffuse calretinin positivity in the tumor.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Fig. 5
Well-Differentiated Papillary Mesothelioma of the Tunica Vaginalis: A Case Study and Review of the Literature
| Author | Age (yr) | Presentation | Location | Focality | Size | Follow-up | Asbestosis | SV40 |
|---|---|---|---|---|---|---|---|---|
| Chetty [3] | 18 | Hydrocele | NA | Multifocal | 1 cm | 1 yr | - | NA |
| Fujii et al. [11] | 56 | Hydrocele | Left | Solitary | 15 mm | 10 yr | - | NA |
| Xiao et al. [1] | 69 | Hydrocele | Right | Solitary | 1.5 cm | 3 yr | - | - |
| Butnor et al. [7] | 32 | Hydrocele | NA | NA | NA | 2 yr | Family contact | NA |
| Tolhurst et al. [2] | 35 | Hydrocele | Right | Multifocal | 9 mm | NA | NA | NA |
| Cabay et al. [4] | 52 | Hydrocele | Right | Solitary | 2 cm | 3 mo | + | NA |
| Fukunaga [5] | 70 | Hydrocele | Right | Solitary | 1.2 cm | 18 mo | - | NA |
| Chollet et al. [10] | 18 | Hydrocele | Left | Solitary | NA | 18 mo | NA | NA |
| Brimo et al. [8] (8 cases) | 52.5 (mean) | 7/8 hydrocele | NA | 6/8 solitary | Mean 1 cm | 3 yr | NA | NA |
| 1/8 mass | 1/8 multifocal | 3 yr | ||||||
| 1/8 plaque | 1.5 yr | |||||||
| 1.5 yr | ||||||||
| 2 mo | ||||||||
| Trpkov et al. [6] | 57 | Hydrocele | NA | Multifocal | 1.5 cm | 6 yr | _ | NA |
| Present case | 48 | Hydrocele | Left | Multifocal | 2 cm | 3 yr | - | - |
Table 1. The review of paratesticular WDPM cases in the literature
WDPM, well-differentiated papillary mesothelioma; SV40, simian virus 40; NA, not available.

 E-submission
E-submission

 PubReader
PubReader Cite this Article
Cite this Article