Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(3); 2014 > Article
-
Brief Case Report
Dedifferentiated Solitary Fibrous Tumor of Thoracic Cavity - Jung Wook Yang1, Dae Hyun Song1, In Seok Jang2,3, Gyung Hyuck Ko1,3
-
Korean Journal of Pathology 2014;48(3):250-253.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.3.250
Published online: June 26, 2014
1Department of Pathology, Gyeongsang National University School of Medicine, Jinju, Korea.
2Department of Thoracic and Cardiovascular Surgery, Gyeongsang National University School of Medicine, Jinju, Korea.
3Institute of Health Sciences, Gyeongsang National University, Jinju, Korea.
- Corresponding Author: Gyung Hyuck Ko, M.D. Department of Pathology, Gyeongsang National University School of Medicine, 15 Jinju-daero 816beon-gil, Jinju 660-751, Korea. Tel: +82-55-772-8061, Fax: +82-55-759-7952, gyunghko@gnu.ac.kr
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
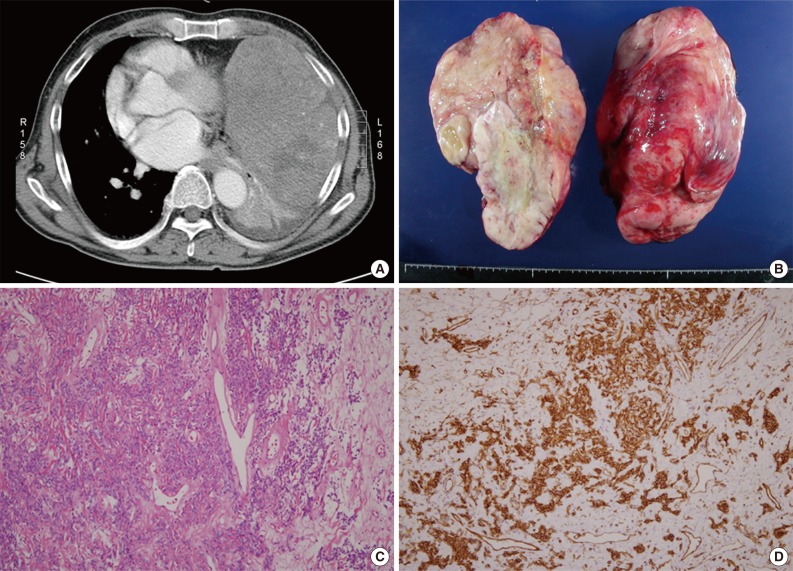
- A 73-year-old male presented with dyspnea for one month. On computerized tomography, a large mass involving the left thoracic cavity and mediastinum was found (Fig. 1A). Sarcoma was suspected upon needle biopsy, based on the large size and mesenchymal features of the tumor cells. During surgery, a 30×25×20-cm-sized well-encapsulated multinodular solid tumor was found. The tumor was divided surgically into two parts and removed (Fig. 1B). Microscopically, the tumor was composed of fibroblast-like tumor cells, collagen fibers and many thin-walled blood vessels, which are characteristics of a SFT (Fig. 1C). The tumor cells were diffusely and strongly positive for CD34 (Fig. 1D) and showed moderate nuclear atypism in focal areas. The mitotic index was generally low, but it was up to 4/10 high-power fields (HPF) in a few areas. Necrosis was absent, and the diagnosis of SFT with malignant potential was made.
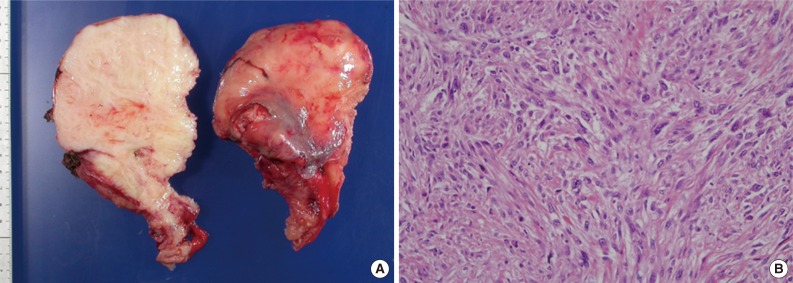
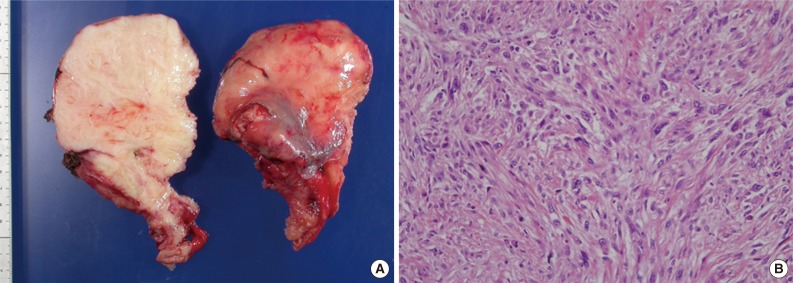
- After 38 months, a computerized tomography showed a 20-cm-sized recurrent mass involving the mediastinum and left thoracic cavity and a separate 4.5-cm-sized mass in the mediastinum. The tumor appeared to have invaded rib bones. The tumor was divided surgically into several parts and removed along with three segments of rib bones (Fig. 2A). The larger mass was composed of highly pleomorphic spindle cells with a mitotic index up to 21/10 HPFs (Fig. 2B). It showed necrosis and invasion to rib bones. The tumor cells were nondistinctive and showed no muscular or osteoid differentiation. They were arranged in a storiform pattern in some areas and were negative for CD34, desmin, S-100, and CD99. Conversely, the smaller mass showed typical microscopic findings of SFT, similar to those seen in the primary tumor. This part of the tumor did not contain any dedifferentiated areas and was positive for CD34.
CASE REPORT
- Although most cases of SFT are benign, about 10% are aggressive.1 Most, but not all, tumors that show malignant behavior (malignant SFT, MSFT) are hypercellular and show cytological atypia, necrosis, numerous mitoses and infiltrative margins.7 Rarely, SFT is accompanied by an overgrowth of a high-grade component, morphologically mimicking a high-grade pleomorphic spindle or small cell sarcoma, as seen in dedifferentiated liposarcoma.
- Patients of DSFT are middle-to-old-aged (Table 1), and males and females are equally affected. These age and sex distributions are similar to those of typical SFT. However, the sites of DSFT seem to be slightly different from those of SFT. Although our case occurred in the thoracic cavity, DSFT occurs more frequently in the retroperitoneum or pelvic cavity than in the pleura, in comparison to SFT. In the report by Collini et al.,2 7 out of 10 DSFT cases occurred in the retroperitoneum or pelvic cavity. The tumor size of DSFT appears to be larger than that of typical SFT and similar to that of MSFT.
- Histologically, DSFT is composed of two portions; one is an area of typical SFT, and the other is a high-grade sarcomatous dedifferentiated area. The dedifferentiated area shows a very high-mitotic rate, with an average of 30/10 HPFs. In the dedifferentiated area, there are no morphologic features that would suggest a diagnosis of SFT. This is in contrast to MSFT, in which even the atypical portion contains some features of typical SFT. The dedifferentiated area in our case was a nondistinctive undifferentiated high-grade pleomorphic sarcoma. However, in other reports,2,3 Ewing-like undifferentiated small round cell sarcomas were seen more frequently. In several cases, rhabdomyosarcomatous2 or osteosarcomatous4 features were seen in the dedifferentiated areas. As in our case, the dedifferentiated area is usually negative for CD34,2,3 in contrast to the area of typical SFT, which is positive for CD34.
- The five-year survival rate of DSFT is approximately 50% to 60%.2 The prognosis of DSFT is worse than that of SFT or even that of MSFT, although an accurate evaluation is difficult because of the limited number of cases.
- Collini et al.2 demonstrated that activated (phosphorylated) ribosomal protein 6 (S6) and activated eukaryotic initiation factor 4E-binding protein 1 (4E-BP1) are strongly expressed in the dedifferentiated area. In contrast to DSFT, MSFT weakly expresses these proteins, while typical SFT does not. S6 and 4E-BP1 control transcription and protein synthesis and have been reported to be associated with malignant progression.
- Collini et al.2 used the term "evoluted SFT" to describe the cases showing a gradual transition from classic SFT/MSFT to a high-grade sarcomatous component or when the tumor consisted of a high-grade sarcomatous component without any trace of SFT/MSFT at a site of local relapse or metastasis. They used the term DSFT only to describe cases with evidence of an abrupt synchronous transition from the classic SFT/MSFT to the high-grade sarcomatous component. According to their criteria, our case corresponds to DSFT because the recurrent tumor was composed of two separate masses, with one showing classic SFT component only and the other showing high-grade sarcomatous component only. However, we do not think this distinction between evoluted and DSFT has a significant meaning because there seems to be no difference in clinical significance, including prognosis, between the two subtypes.
DISCUSSION
- 1. Fletcher CD, Bridge JA, Hogendoorn P, Mertens F. WHO classification of tumours of soft tissue and bone. Lyon: IARC Press, 2013; 80-82.
- 2. Collini P, Negri T, Barisella M, et al. High-grade sarcomatous overgrowth in solitary fibrous tumors: a clinicopathologic study of 10 cases. Am J Surg Pathol 2012; 36: 1202-1215. PubMed
- 3. Mosquera JM, Fletcher CD. Expanding the spectrum of malignant progression in solitary fibrous tumors: a study of 8 cases with a discrete anaplastic component: is this dedifferentiated SFT? Am J Surg Pathol 2009; 33: 1314-1321. PubMed
- 4. Thway K, Hayes A, Ieremia E, Fisher C. Heterologous osteosarcomatous and rhabdomyosarcomatous elements in dedifferentiated solitary fibrous tumor: further support for the concept of dedifferentiation in solitary fibrous tumor. Ann Diagn Pathol 2013; 17: 457-463. ArticlePubMed
- 5. Subramaniam MM, Lim XY, Venkateswaran K, Shuen CS, Soong R, Petersson F. Dedifferentiated solitary fibrous tumour of the nasal cavity: the first case reported with molecular characterization of a TP53 mutation. Histopathology 2011; 59: 1269-1274. ArticlePubMed
- 6. Moritani S, Ichihara S, Hasegawa M, et al. Dedifferentiation and progression of an intracranial solitary fibrous tumor: autopsy case of a Japanese woman with a history of radiation therapy of the head during infancy. Pathol Int 2011; 61: 143-149. ArticlePubMed
- 7. Demicco EG, Park MS, Araujo DM, et al. Solitary fibrous tumor: a clinicopathological study of 110 cases and proposed risk assessment model. Mod Pathol 2012; 25: 1298-1306. ArticlePubMedPDF
REFERENCES
| All SFTa | Benign SFTa | Malignant SFTa | Dedifferentiated SFTb | |
|---|---|---|---|---|
| Age (median, yr) | 53 | 51 | 61 | 51 |
| Sex (male:female) | 1:1 | - | - | 2:3 |
| Site | Abdomen, pelvis; 33/101 (32%) | - | - | Retroperitoneum, pelvic cavity; 7/10 (70%) |
| Size (cm) | 10.3 | 8.7 | 16.2 | 13.2 |
| 5YSR (%) | 89 | - | 60-93c | 50-60 |
Figure & Data
References
Citations

- Dedifferentiated Solitary Fibrous Tumor
Adrian Georg Simon, Adrian Mariño-Enríquez, Jason L. Hornick, Christopher D. M. Fletcher, William J. Anderson
American Journal of Surgical Pathology.2025; 49(10): 1015. CrossRef - A case of slow-growing dedifferentiated solitary fibrous tumor of the pleura over a 7-year period
Madoka Goto, Rio Takada, Yasuhisa Ichikawa, Hideki Tsubouchi, Yuta Kawasumi, Shoichi Mori
The Journal of the Japanese Association for Chest Surgery.2022; 36(7): 821. CrossRef - A Comprehensive Review on Solitary Fibrous Tumor: New Insights for New Horizons
Javier Martin-Broto, Jose L. Mondaza-Hernandez, David S. Moura, Nadia Hindi
Cancers.2021; 13(12): 2913. CrossRef - An intrathoracic giant tumour and vanishing lung cyst after tumour resection
Masashi Nishimura, Shinichiro Ota, Sumitaka Yamanaka, Kanako Shinada, Masaharu Shinkai
Respirology Case Reports.2021;[Epub] CrossRef - Molecular changes in solitary fibrous tumor progression
Hyung Kyu Park, Dan Bi Yu, Minjung Sung, Ensel Oh, Mingi Kim, Ji-Young Song, Mi-Sook Lee, Kyungsoo Jung, Ka-Won Noh, Sungbin An, Kyoung Song, Do-Hyun Nam, Yu Jin Kim, Yoon-La Choi
Journal of Molecular Medicine.2019; 97(10): 1413. CrossRef - A Case Report of Solitary Fibrous Tumor in the Axilla of a 4-year-old Girl with Additional Marker Chromosome
Ji Hye Park, Eun Jeong Kim, O Kyu Noh, Hyun Ju Jung, Jun Eun Park
Clinical Pediatric Hematology-Oncology.2015; 22(2): 171. CrossRef


Fig. 1
Fig. 2
| All SFT |
Benign SFT |
Malignant SFT |
Dedifferentiated SFT |
|
|---|---|---|---|---|
| Age (median, yr) | 53 | 51 | 61 | 51 |
| Sex (male:female) | 1:1 | - | - | 2:3 |
| Site | Abdomen, pelvis; 33/101 (32%) | - | - | Retroperitoneum, pelvic cavity; 7/10 (70%) |
| Size (cm) | 10.3 | 8.7 | 16.2 | 13.2 |
| 5YSR (%) | 89 | - | 60-93 |
50-60 |
5YSR, 5-year survival rate. Data extracted from Demicco Data extracted from Collini 93% for moderate-risk group, 60% for high-risk group.

 E-submission
E-submission
 PubReader
PubReader Cite this Article
Cite this Article