Search
- Page Path
- HOME > Search
- Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
- Agnes Stephanie Harahap, Chan Kwon Jung
- J Pathol Transl Med. 2024;58(5):205-213. Published online July 24, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.24
- 4,805 View
- 297 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
While fine needle aspiration cytology (FNAC) plays an essential role in the screening of thyroid nodules, core needle biopsy (CNB) acts as an alternative method to address FNAC limitations. However, diagnosing thyroid CNB samples can be challenging due to variations in background and levels of experience. Effective training is indispensable to mitigate this challenge. We aim to evaluate the impact of an educational program on improving the accuracy of CNB diagnostics.
Methods
The 2-week observational program included a host mentor pathologist with extensive experience and a visiting pathologist. The CNB classification by The Practice Guidelines Committee of the Korean Thyroid Association was used for the report. Two rounds of reviewing the case were carried out, and the level of agreement between the reviewers was analyzed.
Results
The first-round assessment showed a concordance between two pathologists for 247 thyroid CNB specimens by 84.2%, with a kappa coefficient of 0.74 (indicating substantial agreement). This finding was attributed to the discordance in the use of categories III and V. After peer learning, the two pathologists evaluated 30 new cases, which showed an overall improvement in the level of agreement. The percentage of agreement between pathologists on thyroid CNB diagnosis was 86.7%, as measured by kappa coefficient of 0.80.
Conclusions
This educational program, consisting of guided mentorship and peer learning, can substantially enhance the diagnostic accuracy of thyroid CNB. It is useful in promoting consistent diagnostic standards and contributes to the ongoing development of global pathology practices. -
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
- Chan Kwon Jung
- J Pathol Transl Med. 2023;57(4):208-216. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.20
- 7,009 View
- 267 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - As the application of core needle biopsy (CNB) in evaluating thyroid nodules rises in clinical practice, the 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules have officially recognized its value for the first time. CNB procures tissue samples preserving both histologic structure and cytologic detail, thereby supplying substantial material for an accurate diagnosis and reducing the necessity for repeated biopsies or subsequent surgical interventions. The current review introduces the risk of malignancy within distinct diagnostic categories, emphasizing the implications of noninvasive follicular thyroid neoplasm with papillary-like nuclear features on these malignancy risks. Prior research has indicated diagnostic challenges associated with follicular-patterned lesions, resulting in notable variation within indeterminate diagnostic categories. The utilization of mutation-specific immunostaining in CNB enhances the accuracy of lesion classification. This review underlines the essential role of a multidisciplinary approach in diagnosing follicular-patterned lesions and the potential of mutation-specific immunostaining to strengthen diagnostic consensus and inform patient management decisions.
-
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef - Risk Stratification of Thyroid Nodules Diagnosed as Follicular Neoplasm on Core Needle Biopsy
Byeong-Joo Noh, Won Jun Kim, Jin Yub Kim, Ha Young Kim, Jong Cheol Lee, Myoung Sook Shim, Yong Jin Song, Kwang Hyun Yoon, In-Hye Jung, Hyo Sang Lee, Wooyul Paik, Dong Gyu Na
Endocrinology and Metabolism.2025; 40(4): 610. CrossRef - Diagnostic implication of thyroid spherules for cytological diagnosis of thyroid nodules
Heeseung Sohn, Kennichi Kakudo, Chan Kwon Jung
Cytopathology.2024; 35(3): 383. CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - The Diagnostic Role of Repeated Biopsy of Thyroid Nodules with Atypia of Undetermined Significance with Architectural Atypia on Core-Needle Biopsy
Hye Hyeon Moon, Sae Rom Chung, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee, Jung Hwan Baek
Endocrinology and Metabolism.2024; 39(2): 300. CrossRef - Core needle biopsy for thyroid nodules assessment-a new horizon?
David D Dolidze, Serghei Covantsev, Grigorii M Chechenin, Natalia V Pichugina, Anastasia V Bedina, Anna Bumbu
World Journal of Clinical Oncology.2024; 15(5): 580. CrossRef - Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
Agnes Stephanie Harahap, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2024; 58(5): 205. CrossRef - A simplified four-tier classification for thyroid core needle biopsy
M. Paja, J. L. Del Cura, R. Zabala, I. Korta, Mª T. Gutiérrez, A. Expósito, A. Ugalde
Journal of Endocrinological Investigation.2024; 48(4): 895. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Recommendations for pathologic practice using digital pathology: consensus report of the Korean Society of Pathologists
- Yosep Chong, Dae Cheol Kim, Chan Kwon Jung, Dong-chul Kim, Sang Yong Song, Hee Jae Joo, Sang-Yeop Yi
- J Pathol Transl Med. 2020;54(6):437-452. Published online October 8, 2020
- DOI: https://doi.org/10.4132/jptm.2020.08.27
- 12,370 View
- 339 Download
- 24 Web of Science
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Digital pathology (DP) using whole slide imaging (WSI) is becoming a fundamental issue in pathology with recent advances and the rapid development of associated technologies. However, the available evidence on its diagnostic uses and practical advice for pathologists on implementing DP remains insufficient, particularly in light of the exponential growth of this industry. To inform DP implementation in Korea, we developed relevant and timely recommendations. We first performed a literature review of DP guidelines, recommendations, and position papers from major countries, as well as a review of relevant studies validating WSI. Based on that information, we prepared a draft. After several revisions, we released this draft to the public and the members of the Korean Society of Pathologists through our homepage and held an open forum for interested parties. Through that process, this final manuscript has been prepared. This recommendation contains an overview describing the background, objectives, scope of application, and basic terminology; guidelines and considerations for the hardware and software used in DP systems and the validation required for DP implementation; conclusions; and references and appendices, including literature on DP from major countries and WSI validation studies.
-
Citations
Citations to this article as recorded by- Commercially Available Artificial Intelligence Solutions for Gynaecologic Cytology Screening and Their Integration Into Clinical Workflow
Yosep Chong, Andrey Bychkov
Cytopathology.2026; 37(1): 24. CrossRef - The impact of AI on modern oncology from early detection to personalized cancer treatment
Jun Li, Lei Zhang, Zhenglun Yu, Zhiye Bao, Danyang Li, Liming Wang
npj Precision Oncology.2026;[Epub] CrossRef - An equivalency and efficiency study for one year digital pathology for clinical routine diagnostics in an accredited tertiary academic center
Viola Iwuajoku, Kübra Ekici, Anette Haas, Mohammed Zaid Khan, Azar Kazemi, Atsuko Kasajima, Claire Delbridge, Alexander Muckenhuber, Elisa Schmoeckel, Fabian Stögbauer, Christine Bollwein, Kristina Schwamborn, Katja Steiger, Carolin Mogler, Peter J. Schüf
Virchows Archiv.2025; 487(1): 3. CrossRef - An adapted & improved validation protocol for digital pathology implementation
Ying-Han R. Hsu, Iman Ahmed, Juliana Phlamon, Charlotte Carment-Baker, Joyce Yin Tung Chan, Ioannis Prassas, Karen Weiser, Shaza Zeidan, Blaise Clarke, George M. Yousef
Seminars in Diagnostic Pathology.2025; 42(4): 150905. CrossRef - Transforming pathology into digital pathology: highway to hell or stairway to heaven?
Rainer Grobholz, Andrew Janowczyk, Inti Zlobec
Diagnostic Histopathology.2025; 31(7): 410. CrossRef - The Evolution of Digital Pathology in Infrastructure, Artificial Intelligence and Clinical Impact
Chan Kwon Jung
International Journal of Thyroidology.2025; 18(1): 6. CrossRef - Current Trends and Future Directions of Digital Pathology and Artificial Intelligence in Dermatopathology: A Scientometric-Based Review
Iuliu Gabriel Cocuz, Raluca Niculescu, Maria-Cătălina Popelea, Maria Elena Cocuz, Adrian-Horațiu Sabău, Andreea-Cătălina Tinca, Andreea Raluca Cozac-Szoke, Diana Maria Chiorean, Corina Eugenia Budin, Ovidiu Simion Cotoi
Diagnostics.2025; 15(17): 2196. CrossRef - Integration of Digital Cytology in Quality Assurance Programs for Cytopathology
Yosep Chong, Maria Jesús Fernández Aceñero, Zaibo Li, Andrey Bychkov
Acta Cytologica.2025; : 1. CrossRef - Quantitative Assessment of Focus Quality in Whole-Slide Imaging of Thyroid Liquid-Based Cytology Using Laplacian Variance
Chan Kwon Jung, Chankyung Kim, Sora Jeon, Andrey Bychkov
Endocrine Pathology.2025;[Epub] CrossRef - Performance of externally validated machine learning models based on histopathology images for the diagnosis, classification, prognosis, or treatment outcome prediction in female breast cancer: A systematic review
Ricardo Gonzalez, Peyman Nejat, Ashirbani Saha, Clinton J.V. Campbell, Andrew P. Norgan, Cynthia Lokker
Journal of Pathology Informatics.2024; 15: 100348. CrossRef - Swiss digital pathology recommendations: results from a Delphi process conducted by the Swiss Digital Pathology Consortium of the Swiss Society of Pathology
Andrew Janowczyk, Inti Zlobec, Cedric Walker, Sabina Berezowska, Viola Huschauer, Marianne Tinguely, Joel Kupferschmid, Thomas Mallet, Doron Merkler, Mario Kreutzfeldt, Radivoje Gasic, Tilman T. Rau, Luca Mazzucchelli, Isgard Eyberg, Gieri Cathomas, Kirst
Virchows Archiv.2024; 485(1): 13. CrossRef - ChatGPT as an aid for pathological diagnosis of cancer
Shaivy Malik, Sufian Zaheer
Pathology - Research and Practice.2024; 253: 154989. CrossRef - Possible benefits, challenges, pitfalls, and future perspective of using ChatGPT in pathology
Durre Aden, Sufian Zaheer, Sabina Khan
Revista Española de Patología.2024; 57(3): 198. CrossRef - Remote Placental Sign-Out: What Digital Pathology Can Offer for Pediatric Pathologists
Casey P. Schukow, Jacqueline K. Macknis
Pediatric and Developmental Pathology.2024; 27(4): 375. CrossRef - Digital Validation in Breast Cancer Needle Biopsies: Comparison of Histological Grade and Biomarker Expression Assessment Using Conventional Light Microscopy, Whole Slide Imaging, and Digital Image Analysis
Ji Eun Choi, Kyung-Hee Kim, Younju Lee, Dong-Wook Kang
Journal of Personalized Medicine.2024; 14(3): 312. CrossRef - Pathologists light level preferences using the microscope—study to guide digital pathology display use
Charlotte Jennings, Darren Treanor, David Brettle
Journal of Pathology Informatics.2024; 15: 100379. CrossRef - Eye tracking in digital pathology: A comprehensive literature review
Alana Lopes, Aaron D. Ward, Matthew Cecchini
Journal of Pathology Informatics.2024; 15: 100383. CrossRef - Diagnostic Assessment of Deep Learning Algorithms for Frozen Tissue Section Analysis in Women with Breast Cancer
Young-Gon Kim, In Hye Song, Seung Yeon Cho, Sungchul Kim, Milim Kim, Soomin Ahn, Hyunna Lee, Dong Hyun Yang, Namkug Kim, Sungwan Kim, Taewoo Kim, Daeyoung Kim, Jonghyeon Choi, Ki-Sun Lee, Minuk Ma, Minki Jo, So Yeon Park, Gyungyub Gong
Cancer Research and Treatment.2023; 55(2): 513. CrossRef - Recent application of artificial intelligence on histopathologic image-based prediction of gene mutation in solid cancers
Mohammad Rizwan Alam, Kyung Jin Seo, Jamshid Abdul-Ghafar, Kwangil Yim, Sung Hak Lee, Hyun-Jong Jang, Chan Kwon Jung, Yosep Chong
Briefings in Bioinformatics.2023;[Epub] CrossRef - Sustainable development goals applied to digital pathology and artificial intelligence applications in low- to middle-income countries
Sumi Piya, Jochen K. Lennerz
Frontiers in Medicine.2023;[Epub] CrossRef - Diagnostic proficiency test using digital cytopathology and comparative assessment of whole slide images of cytologic samples for quality assurance program in Korea
Yosep Chong, Soon Auck Hong, Hoon Kyu Oh, Soo Jin Jung, Bo-Sung Kim, Ji Yun Jeong, Ho-Chang Lee, Gyungyub Gong
Journal of Pathology and Translational Medicine.2023; 57(5): 251. CrossRef - Real-World Implementation of Digital Pathology: Results From an Intercontinental Survey
Daniel Gomes Pinto, Andrey Bychkov, Naoko Tsuyama, Junya Fukuoka, Catarina Eloy
Laboratory Investigation.2023; 103(12): 100261. CrossRef - National digital pathology projects in Switzerland: A 2023 update
Rainer Grobholz, Andrew Janowczyk, Ana Leni Frei, Mario Kreutzfeldt, Viktor H. Koelzer, Inti Zlobec
Die Pathologie.2023; 44(S3): 225. CrossRef - Understanding the ethical and legal considerations of Digital Pathology
Cheryl Coulter, Francis McKay, Nina Hallowell, Lisa Browning, Richard Colling, Philip Macklin, Tom Sorell, Muhammad Aslam, Gareth Bryson, Darren Treanor, Clare Verrill
The Journal of Pathology: Clinical Research.2022; 8(2): 101. CrossRef - Current Trend of Artificial Intelligence Patents in Digital Pathology: A Systematic Evaluation of the Patent Landscape
Muhammad Joan Ailia, Nishant Thakur, Jamshid Abdul-Ghafar, Chan Kwon Jung, Kwangil Yim, Yosep Chong
Cancers.2022; 14(10): 2400. CrossRef - Recent Applications of Artificial Intelligence from Histopathologic Image-Based Prediction of Microsatellite Instability in Solid Cancers: A Systematic Review
Mohammad Rizwan Alam, Jamshid Abdul-Ghafar, Kwangil Yim, Nishant Thakur, Sung Hak Lee, Hyun-Jong Jang, Chan Kwon Jung, Yosep Chong
Cancers.2022; 14(11): 2590. CrossRef - Automated Hybrid Model for Detecting Perineural Invasion in the Histology of Colorectal Cancer
Jiyoon Jung, Eunsu Kim, Hyeseong Lee, Sung Hak Lee, Sangjeong Ahn
Applied Sciences.2022; 12(18): 9159. CrossRef - Development of quality assurance program for digital pathology by the Korean Society of Pathologists
Yosep Chong, Jeong Mo Bae, Dong Wook Kang, Gwangil Kim, Hye Seung Han
Journal of Pathology and Translational Medicine.2022; 56(6): 370. CrossRef - Improving quality control in the routine practice for histopathological interpretation of gastrointestinal endoscopic biopsies using artificial intelligence
Young Sin Ko, Yoo Mi Choi, Mujin Kim, Youngjin Park, Murtaza Ashraf, Willmer Rafell Quiñones Robles, Min-Ju Kim, Jiwook Jang, Seokju Yun, Yuri Hwang, Hani Jang, Mun Yong Yi, Anwar P.P. Abdul Majeed
PLOS ONE.2022; 17(12): e0278542. CrossRef - What is Essential is (No More) Invisible to the Eyes: The Introduction of BlocDoc in the Digital Pathology Workflow
Vincenzo L’Imperio, Fabio Gibilisco, Filippo Fraggetta
Journal of Pathology Informatics.2021; 12(1): 32. CrossRef
- Commercially Available Artificial Intelligence Solutions for Gynaecologic Cytology Screening and Their Integration Into Clinical Workflow
- HER2 status in breast cancer: changes in guidelines and complicating factors for interpretation
- Soomin Ahn, Ji Won Woo, Kyoungyul Lee, So Yeon Park
- J Pathol Transl Med. 2020;54(1):34-44. Published online November 6, 2019
- DOI: https://doi.org/10.4132/jptm.2019.11.03
- 38,110 View
- 1,323 Download
- 189 Web of Science
- 187 Crossref
-
 Abstract
Abstract
 PDF
PDF - Human epidermal growth factor receptor 2 (HER2) protein overexpression and/or HER2 gene amplification is found in about 20% of invasive breast cancers. It is a sole predictive marker for treatment benefits from HER2 targeted therapy and thus, HER2 testing is a routine practice for newly diagnosed breast cancer in pathology. Currently, HER2 immunohistochemistry (IHC) is used for a screening test, and in situ hybridization is used as a confirmation test for HER2 IHC equivocal cases. Since the American Society of Clinical Oncology (ASCO)/College of American Pathologists (CAP) guidelines on HER2 testing was first released in 2007, it has been updated to provide clear instructions for HER2 testing and accurate determination of HER2 status in breast cancer. During HER2 interpretation, some pitfalls such as intratumoral HER2 heterogeneity and increase in chromosome enumeration probe 17 signals may lead to inaccurate assessment of HER2 status. Moreover, HER2 status can be altered after neoadjuvant chemotherapy or during metastatic progression, due to biologic or methodologic issues. This review addresses recent updates of ASCO/CAP guidelines and factors complicating in the interpretation of HER2 status in breast cancers.
-
Citations
Citations to this article as recorded by- A Comprehensive Model Outperformed the Single Radiomics Model in Noninvasively Predicting the HER2 Status in Patients with Breast Cancer
Weimin Liu, Yiqing Yang, Xiaohong Wang, Chao Li, Chen Liu, Xiaolei Li, Junzhe Wen, Xue Lin, Jie Qin
Academic Radiology.2025; 32(1): 24. CrossRef - Multiparametric MRI Radiomics With Machine Learning for Differentiating HER2-Zero, -Low, and -Positive Breast Cancer: Model Development, Testing, and Interpretability Analysis
Yongxin Chen, Siyi Chen, Wenjie Tang, Qingcong Kong, Zhidan Zhong, Xiaomeng Yu, Yi Sui, Wenke Hu, Xinqing Jiang, Yuan Guo
American Journal of Roentgenology.2025;[Epub] CrossRef - Cervical Lymph Node Metastasis of Unknown Origin and Remote Primary at a Tertiary Cancer Centre in North India: Case Series with Review of Literature
Kriti Grover, Siddharth Arora, Mansi Dey, Deepti Awasthi, Harshad Sharma, Bibhu Prasad Mishra, Nitesh Mohan, Cheena Garg, Arjun Agarwal
Indian Journal of Otolaryngology and Head & Neck Surgery.2025; 77(1): 424. CrossRef - Pooled clinical trial analyses evaluating outcomes of HER2-low vs HER2-0 expression in patients with metastatic breast cancer following chemotherapy
Elizabeth B. Lamont, Emily Stein, Paolo Tarantino, Sara M. Tolaney, Corinne Ahlberg, Krishna Chinnathambu, Jiezhi Qi, Jackie Bilan, Ruthie Davi, Lisa Ensign
Breast Cancer Research and Treatment.2025; 210(1): 11. CrossRef - Insights into AI advances in immunohistochemistry for effective breast cancer treatment: a literature review of ER, PR, and HER2 scoring
Genevieve Chyrmang, Kangkana Bora, Anup Kr. Das, Gazi N. Ahmed, Lopamudra Kakoti
Current Medical Research and Opinion.2025; 41(1): 115. CrossRef - Prediction of Lung Adenocarcinoma Driver Genes Through Protein–Protein Interaction Networks Utilizing GenePlexus
Fei Yuan, Yu‐Hang Zhang, FeiMing Huang, Xiaoyu Cao, Lei Chen, JiaBo Li, WenFeng Shen, KaiYan Feng, YuSheng Bao, Tao Huang, Yu‐Dong Cai
PROTEOMICS.2025;[Epub] CrossRef - Quantitative expression of estrogen, progesterone and human epidermal growth factor receptor-2 and their correlation with immunohistochemistry in breast cancer at Uganda Cancer Institute
Henry Wannume, Nixon Niyonzima, Sam Kalungi, Julius Boniface Okuni, Tonny Okecha, Edward Kakungulu, Steven Mpungu Kiwuwa, Geoffrey Waiswa, Sylvester Kadhumbula, Monica Namayanja, Martin Nabwana, Jackson Orem, Kenji Fujiwara
PLOS ONE.2025; 20(1): e0311185. CrossRef - Automated Quantification of HER2 Amplification Levels Using Deep Learning
Ching-Wei Wang, Kai-Lin Chu, Ting-Sheng Su, Keng-Wei Liu, Yi-Jia Lin, Tai-Kuang Chao
IEEE Journal of Biomedical and Health Informatics.2025; 29(1): 333. CrossRef - CAR-macrophage therapy for HER2-overexpressing advanced solid tumors: a phase 1 trial
Kim A. Reiss, Mathew G. Angelos, E. Claire Dees, Yuan Yuan, Naoto T. Ueno, Paula R. Pohlmann, Melissa L. Johnson, Joseph Chao, Olga Shestova, Jonathan S. Serody, Maggie Schmierer, Madison Kremp, Michael Ball, Rehman Qureshi, Benjamin H. Schott, Poonam Son
Nature Medicine.2025; 31(4): 1171. CrossRef - Human Cytomegalovirus Infection and Breast Cancer: A Literature Review of Clinical and Experimental Data
Rancés Blanco, Juan P. Muñoz
Biology.2025; 14(2): 174. CrossRef - An antibody-photosensitiser bioconjugate overcomes trastuzumab resistance in HER2-positive breast cancer
Mireia Jordà-Redondo, Ana Piqueras, Ana Castillo, Pedro Luis Fernández, Roger Bresolí-Obach, Lidia Blay, Joan Francesc Julián Ibáñez, Santi Nonell
European Journal of Medicinal Chemistry.2025; 290: 117511. CrossRef - Dynamic HER2-low status among patients with triple negative breast cancer (TNBC) and the impact of repeat biopsies
Yael Bar, Geoffrey Fell, Aylin Dedeoglu, Natalie Moffett, Neelima Vidula, Laura Spring, Seth A. Wander, Aditya Bardia, Naomi Ko, Beverly Moy, Leif W. Ellisen, Steven J. Isakoff
npj Breast Cancer.2025;[Epub] CrossRef - Clinical significances of RPL15 gene expression in circulating tumor cells of patients with breast cancer
Ying Zhuang, Keli Su, Shushu Liu, Wei Fan, Huijuan Lv, Wei Zhong
Biomedical Reports.2025; 22(5): 1. CrossRef - Advancing Breast Cancer Treatment: The Role of Immunotherapy and Cancer Vaccines in Overcoming Therapeutic Challenges
Marco Palma
Vaccines.2025; 13(4): 344. CrossRef - Complete preclinical evaluation of the novel antibody mimetic Nanofitin-IRDye800CW for diverse non-invasive diagnostic applications in the management of HER-2 positive tumors
Margherita Iaboni, Federico Crivellin, Francesca Arena, Francesca La Cava, Alessia Cordaro, Francesco Stummo, Daniele Faletto, Simon Huet, Leo Candela, Jessy Pedrault, Eugenia R. Zanella, Andrea Bertotti, Francesco Blasi, Alessandro Maiocchi, Luisa Poggi,
Scientific Reports.2025;[Epub] CrossRef - New insights on Galectin-9 expression in cancer prognosis: An updated systemic review and meta-analysis
Chun Yan So, Yusong Li, Kwan Ting Chow, Xiaosheng Tan
PLOS ONE.2025; 20(3): e0320441. CrossRef - Role of artificial intelligence –based machine learning model in predicting HER2/neu gene status in breast cancer
Ghada Mohamed, Omar Hamdy, Anwar Alkallas, Youssef Tahoun, Mohammed Mohammed Gomaa, Inas Moaz, Ahmed Orabi, Yasmine Hany elzohery, AL-Shimaa Zakaria, Mahitab Ibrahim Eltohamy
Pathology - Research and Practice.2025; 270: 155927. CrossRef - HER2 mRNA Score From Quantitative ERBB2 mRNA Expression of Oncotype Dx
Hyunwoo Lee, Jai Min Ryu, Se Kyung Lee, Byung Joo Chae, Jonghan Yu, Jeong Eon Lee, Seok Won Kim, Seok Jin Nam, Yoon Ah Cho, Eun Yoon Cho
American Journal of Surgical Pathology.2025; 49(8): 807. CrossRef - Neratinib and metformin: A novel therapeutic approach against HER2-Positive Breast Cancer
Hadeel Kheraldine, Arij Fouzat Hassan, Sumayyah Saeed, Maysaloun Merhi, Jericha Miles Mateo, Monika Ulamec, Melita Peric-Balja, Semir Vranic, Hamda Al-Thawadi, Ala-Eddin Al Moustafa
Biomedicine & Pharmacotherapy.2025; 187: 118034. CrossRef - Machine learning prediction of HER2-low expression in breast cancers based on hematoxylin–eosin-stained slides
Jun Du, Jun Shi, Dongdong Sun, Yifei Wang, Guanfeng Liu, Jingru Chen, Wei Wang, Wenchao Zhou, Yushan Zheng, Haibo Wu
Breast Cancer Research.2025;[Epub] CrossRef - Predicting sentinel lymph node metastatic burden with intravoxel incoherent motion diffusion-weighted imaging and dynamic contrast-enhanced magnetic resonance imaging in clinical early-stage breast cancer patients
Mingli Jin, Fang Xiao, Qi Zhao, Ying Jiang, Zhihua Pan, Zhicai Duan, Juxi Jiang, Miaoqi Zhang, Jian Shu
Magnetic Resonance Imaging.2025; 121: 110397. CrossRef - HbA1c levels and breast cancer prognosis in women without diabetes
Jonas Busk Holm, Jens Meldgaard Bruun, Peer Christiansen, Reimar Wernich Thomsen, Jan Frystyk, Deirdre Cronin-Fenton, Signe Borgquist
BMC Cancer.2025;[Epub] CrossRef - Clinical Outcomes in Early-Stage HER2-Low and HER2-Zero Breast Cancer: Single-Center Experience
Jamshid Hamdard, Mehmet Haluk Yücel, Harun Muğlu, Özgür Açıkgöz, Aslı Çakır, Ahmet Bilici, Ömer Fatih Ölmez
Journal of Clinical Medicine.2025; 14(9): 2937. CrossRef - Molecular Mechanism of Breast Cancer and Predisposition of Mouse Mammary Tumor Virus Propagation Cycle
Arya Ghosh, Subash C.B. Gopinath
Current Medicinal Chemistry.2025; 32(12): 2330. CrossRef - ASSESSMENT OF RECEPTOR CONVERSION ROLE FOR ADVANCED BREAST CANCER ON THE CHEMORESISTANCE OCCURRENCE
Oleksii V. Movchan, Ivan I. Smolanka, Andriy O. Lyashenko, Anton D. Loboda, Iryna V. Dosenko, Oksana M. Ivankova
Clinical and Preventive Medicine.2025; (3): 56. CrossRef - Combining conventional magnetic resonance imaging (MRI) parameters with clinicopathologic data for differentiation of the three-tiered human epidermal growth factor receptor 2 (HER2) status in breast cancer
W. Liu, C. Liu, Y. Yang, Y. Chen, A. Muhetaier, Z. Lin, Z. Weng, X. Wang, P. Zhang, J. Qin
Clinical Radiology.2025; 86: 106955. CrossRef - IN SILICO STUDY: THE POTENTIAL OF KILEMO (Litsea cubeba) ENDEMIC PLANT FROM KALIMANTAN AS ANTI-BREAST CANCER THROUGH HER2 INHIBITION
Dwi Utami, Tarisha Elmaningtyas Zahro, Khairun Nisa, Muhammad Farid
JIIS (Jurnal Ilmiah Ibnu Sina): Ilmu Farmasi dan Kesehatan.2025; 10(1): 166. CrossRef - Trastuzumab Deruxtecan in Previously Treated HER2-Low Metastatic Breast Cancer: Real-World Multicentric Study in the Portuguese Population
Luísa Soares Miranda, Maria João Sousa, Miguel Martins Braga, Marisa Couto, Isabel Vieira Fernandes, Francisca Abreu, Inês Eiriz, Catarina Lopes Fernandes, Alice Fonseca Marques, Maria Teresa Marques, Raquel Romão, Fernando Gonçalves, Joana Simões, Antóni
Cancers.2025; 17(12): 1911. CrossRef - Factors influencing pathological complete response to neoadjuvant chemotherapy in resectable breast cancer: A retrospective study
Jian Kang, Huifen Xiong, Xiaoliu Jiang, Zhaohui Huang, Yonghong Guo, Yali Cao, Jingxian Ding
Oncology Letters.2025; 30(1): 1. CrossRef - Association of HER2-low with clinicopathological features in patients with early invasive lobular breast cancer: an international multicentric study
Karen Van Baelen, Ha-Linh Nguyen, François Richard, Gitte Zels, Maria Margarete Karsten, Guilherme Nader-Marta, Peter Vermeulen, Luc Dirix, Adam David Dordevic, Evandro de Azambuja, Denis Larsimont, Marion Maetens, Elia Biganzoli, Hans Wildiers, Ann Smeet
Breast Cancer Research.2025;[Epub] CrossRef - Collagenase type IV improves the quality of HER2 fluorescence in situ hybridization for breast cancers
Shang-En Lee, Sheng-Chi Hsu, Tsai-Hsien Hung, Kwai-Fong Ng, Tse-Ching Chen
American Journal of Clinical Pathology.2025; 164(3): 342. CrossRef - Resonant multi-focal scanning super-resolution microscopy with extended depth and field-of-view
Kidan Tadesse, Keyi Han, Wenhao Liu, Oliver S. Lee, Shu Jia
Cell Reports Physical Science.2025; 6(7): 102680. CrossRef - Scalable Nuclei Detection in HER2-SISH Whole Slide Images via Fine-Tuned Stardist with Expert-Annotated Regions of Interest
Zaka Ur Rehman, Mohammad Faizal Ahmad Fauzi, Wan Siti Halimatul Munirah Wan Ahmad, Fazly Salleh Abas, Phaik-Leng Cheah, Seow-Fan Chiew, Lai-Meng Looi
Diagnostics.2025; 15(13): 1584. CrossRef - Molecular landscape of HER2-mutated non-small cell lung cancer in Northeastern Brazil: Clinical, histopathological, and genomic insights
Cleto Dantas Nogueira, Samuel Frota, Huylmer Lucena Chaves, Juliana Cordeiro de Sousa, Guilherme de Sousa Veloso, Francisco Jonathan dos Santos Araujo, Gabriel Barbosa Silva, Samuel Silva Ferreira, Marclesson Santos Alves, Fabio Nasser, Ezequiel Rangel, F
Oncotarget.2025; 16(1): 467. CrossRef - Correlation between CTMP expression levels and resistance to trastuzumab in HER2 + metastatic breast cancer
Mania Makhoul, Maher Saifo, Fariz Ahmad, Jumana Saleh
Discover Oncology.2025;[Epub] CrossRef - The association between body mass index and neoadjuvant chemotherapy response in patients with breast cancer
Jonas Busk Holm, Stine Blaabjerg Skovbjerg, Hanne Melgaard Nielsen, Peer Christiansen, Jens Meldgaard Bruun, Jan Alsner, Deirdre Cronin-Fenton, Signe Borgquist
Breast Cancer Research.2025;[Epub] CrossRef - An immunohistochemical characterization of basal cell carcinoma in patients below 40 years of age
Vincent Waller, Myriam Boeschen, Thomas Lingscheidt, Mathias Stiller, Lena Eickenscheidt, Thomas Wilhelm, Sonja Grunewald, Mirjana Ziemer, Jan‐Christoph Simon, Hendrik Bläker, Maximilian von Laffert
JDDG: Journal der Deutschen Dermatologischen Gesellschaft.2025; 23(11): 1414. CrossRef - Clinical Relationship Between Serum ApoB, HER2, and Myocardial Ischemia Risk in Breast Cancer Patients
Yeyan Lei, Dongmei Li, Shuang Bai, Xing Zeng, Rongyuan Yang, Qing Liu
Cancer Reports.2025;[Epub] CrossRef - Dual-targeting and steric hindrance resolution in HER2 IHC: a novel approach to improve diagnostic sensitivity
Li Luo, Xi Zhang, Linqiong Chen, Zhuohan Chen, Yuchen Wang, Kaihao Huang, Xiaoyun Lin, Hongxiang Zhu, Wangqi Du
BMC Cancer.2025;[Epub] CrossRef - Time‐Dependent Diffusion MRI‐Based Microstructural Mapping for Characterizing HER2‐Zero, ‐Low, ‐Ultra‐Low, and ‐Positive Breast Cancer
Xiaoxia Wang, Yao Huang, Ying Cao, Huifang Chen, Xueqin Gong, Xiaosong Lan, Jiuquan Zhang, Zhaoxiang Ye
Journal of Magnetic Resonance Imaging.2025; 62(6): 1754. CrossRef - Digital pathology enabling lean management of HER2/neu testing in breast Cancer
Aishwarya Sharma, Prarthna Shah, Manali Ranade, Trupti Pai, Ayushi Sahay, Asawari Patil, Tanuja Shet, Heena Gupta, Devika Chauhan, Puneet Somal, Sankalp Sancheti, Sangeeta Desai
Journal of Pathology Informatics.2025; 19: 100515. CrossRef - Enhancing HER2-low breast cancer detection with quantitative transcriptomics
Maria-Anna Misiakou, Maj-Britt Jensen, Maj-Lis Talman, Bent Ejlertsen, Maria Rossing
npj Breast Cancer.2025;[Epub] CrossRef - Caracterización inmunohistoquímica del cáncer de mama correlacionado con histopatología,estudio realizado en un hospital de Ecuador
María Fernanda Calderón León, Diego Mauricio Cabrera Moyano, Jorge Daniel Cárdenas Rodríguez, Paula Andrea Vásquez Jaramillo, Andrea Alexandra Saltos Román, Maryoli González Sánchez
Journal of the Selva Andina Research Society.2025; 16(2): 116. CrossRef - Relationship of vitamin D receptor expression with hormone receptors and other clinicopathological features in primary breast carcinomas: A retrospective cross-sectional study
Yaşar Ünlü, Ethem Ömeroğlu, Abdülhalim Serden Ay, Meryem İlkay Eren Karanis, Kilinç Ayşe Nur Uğur, Esra Yilmaz
Medicine.2025; 104(35): e44222. CrossRef - Improving HER2 Diagnostics with Digital Real‐Time PCR for Ultrafast, Precise Prediction of Anti‐HER2 Therapy Response in Patients with Breast Cancer
Hee‐Joo Choi, Soo Young Park, Minsik Song, Jinhyuk Chang, YoonSik Kim, Hosub Park, Chihwan David Cha, Sohyeon Yang, Nam Hun Heo, Min Ji Song, Da Sol Kim, Hayeon Kim, Minuk Kim, Jae Eun Park, Yesung Lee, EunChae Ji, Heekyoung Chung, Ilecheon Jeong, Mineui
Small Methods.2025;[Epub] CrossRef - Unveiling Metabolic Signatures as Potential Biomarkers in Common Cancers: Insights from Lung, Breast, Colorectal, Liver, and Gastric Tumours
Kha Wai Hon, Rakesh Naidu
Biomolecules.2025; 15(10): 1376. CrossRef - Validation of ancillary procedures on formalin liquid fixed aspiration cytologic samples: from minimum to maximum
Orsolya Rideg, Tímea Dergez, Arnold Tóth, Tamás Tornóczky, Gábor Pavlovics, Endre Kálmán
American Journal of Clinical Pathology.2025; 164(6): 924. CrossRef - Challenges & recommendations for identification of human epidermal growth factor receptor -2 (HER2)-low metastatic breast cancer in India: Expert opinion statement
Neeraj Arora, Jyoti Bajpai, Amanjit Bal, Atul Batra, Anurag Gupta, Deepak Kumar Mishra, Geetashree Mukherjee, Trupti Pai, Mayur Parihar, Geeta V. Patil Okaly, Shilpa Prabhudesai, Milap Shah, Somashekhar S.P.
The Indian Journal of Medical Research.2025; 162: 279. CrossRef - Eine immunhistologische Charakterisierung des Basalzellkarzinoms bei Patienten unter 40 Jahren
Vincent Waller, Myriam Boeschen, Thomas Lingscheidt, Mathias Stiller, Lena Eickenscheidt, Thomas Wilhelm, Sonja Grunewald, Mirjana Ziemer, Jan‐Christoph Simon, Hendrik Bläker, Maximilian von Laffert
JDDG: Journal der Deutschen Dermatologischen Gesellschaft.2025; 23(11): 1414. CrossRef - Comparison of Immunohistochemical 2 (+) HER2 Gene Status with SISH in Invasive Breast Carcinoma
Alper Sayiner, Hatice Karaman, Fatma Şenel, Arzu Tasdemir, Merve Doğan, İpek Özer
Sakarya Medical Journal.2025; 15(4): 338. CrossRef - Concurrent genomic assessment of circulating tumour cells and ctDNA to guide therapy in metastatic breast cancer
Rebecca C. Allsopp, Karen Page, Evie Wren, Georgios Nteliopoulos, Kelly L. T. Gleason, Gurdeep Matharu Lall, Shradha Bhagani, Emmanuel Acheampong, Marc K. Wadsley, Raoul Charles Coombes, Jacqueline A. Shaw
BMC Cancer.2025;[Epub] CrossRef - Management Strategies and Outcomes in HR+/HER2− Metastatic Breast Cancer Receiving CDK4/6 Inhibitors and Subsequent Therapies
Katarzyna Pogoda, Hubert Pawlik, Anna Balata, Magdalena Czopowicz, Agata Bak, Iwona Twardowska, Malgorzata Meluch, Maria Wojda, Agnieszka Mlodzinska, Ewa Szombara, Renata Sienkiewicz, Aleksandra Konieczna, Elzbieta Brewczynska, Izabela Lemanska, Anna Majs
Breast Cancer: Targets and Therapy.2025; Volume 17: 1307. CrossRef - Identification of novel chemical scaffolds against kinase domain of cancer causing human epidermal growth factor receptor 2: a systemic chemoinformatic approach
Faris Alrumaihi
Journal of Biomolecular Structure and Dynamics.2024; 42(12): 6269. CrossRef - Standardized pathology report for HER2 testing in compliance with 2023 ASCO/CAP updates and 2023 ESMO consensus statements on HER2-low breast cancer
Mariia Ivanova, Francesca Maria Porta, Marianna D’Ercole, Carlo Pescia, Elham Sajjadi, Giulia Cursano, Elisa De Camilli, Oriana Pala, Giovanni Mazzarol, Konstantinos Venetis, Elena Guerini-Rocco, Giuseppe Curigliano, Giuseppe Viale, Nicola Fusco
Virchows Archiv.2024; 484(1): 3. CrossRef - Analytical Performance Evaluation of a 523-Gene Circulating Tumor DNA Assay for Next-Generation Sequencing–Based Comprehensive Tumor Profiling in Liquid Biopsy Samples
Johannes Harter, Eleonora Buth, Janina Johaenning, Florian Battke, Maria Kopp, Henning Zelba, Martin Schulze, Jiri Koedding, Saskia Biskup
The Journal of Molecular Diagnostics.2024; 26(1): 61. CrossRef - Are There More HER2 FISH in the Sea? An Institution’s Experience in Identifying HER2 Positivity Using Fluorescent In Situ Hybridization in Patients with HER2 Negative Immunohistochemistry
Camille Suydam, Fairouz Chibane, Nicole Brown, Madeleine Schlafly, Alicia H. Arnold, Intisar Ghleilib, Melissa Easley, Joseph White
Annals of Surgical Oncology.2024; 31(1): 376. CrossRef - HER2 copy number determination in breast cancer using the highly sensitive droplet digital PCR method
Beate Alinger-Scharinger, Cornelia Kronberger, Georg Hutarew, Wolfgang Hitzl, Roland Reitsamer, Klaassen-Federspiel Frederike, Martina Hager, Thorsten Fischer, Karl Sotlar, Heidi Jaksch-Bogensperger
Virchows Archiv.2024; 485(1): 53. CrossRef - Impact of HER2-low status for patients with early-stage breast cancer and non-pCR after neoadjuvant chemotherapy: a National Cancer Database Analysis
Huiyue Li, Jennifer K. Plichta, Kan Li, Yizi Jin, Samantha M. Thomas, Fei Ma, Li Tang, Qingyi Wei, You-Wen He, Qichen Chen, Yuanyuan Guo, Yueping Liu, Jian Zhang, Sheng Luo
Breast Cancer Research and Treatment.2024; 204(1): 89. CrossRef - Qualification of a multiplexed tissue imaging assay and detection of novel patterns of HER2 heterogeneity in breast cancer
Jennifer L. Guerriero, Jia-Ren Lin, Ricardo G. Pastorello, Ziming Du, Yu-An Chen, Madeline G. Townsend, Kenichi Shimada, Melissa E. Hughes, Siyang Ren, Nabihah Tayob, Kelly Zheng, Shaolin Mei, Alyssa Patterson, Krishan L. Taneja, Otto Metzger, Sara M. Tol
npj Breast Cancer.2024;[Epub] CrossRef - Clinical Utility and Benefits of Comprehensive Genomic Profiling in Cancer
Melissa Yuwono Tjota, Jeremy P Segal, Peng Wang
The Journal of Applied Laboratory Medicine.2024; 9(1): 76. CrossRef - High contrast breast cancer biomarker semi-quantification and immunohistochemistry imaging using upconverting nanoparticles
Sanathana Konugolu Venkata Sekar, Hui Ma, Katarzyna Komolibus, Gokhan Dumlupinar, Matthias J. Mickert, Krzysztof Krawczyk, Stefan Andersson-Engels
Biomedical Optics Express.2024; 15(2): 900. CrossRef - HER2-low breast cancer and response to neoadjuvant chemotherapy: a population-based cohort study
Ximena Baez-Navarro, Mieke R. van Bockstal, Agnes Jager, Carolien H.M. van Deurzen
Pathology.2024; 56(3): 334. CrossRef - Fast-tracking drug development with biomarkers and companion diagnostics
Noreen McBrearty, Devika Bahal, Suso Platero
Journal of Cancer Metastasis and Treatment.2024;[Epub] CrossRef - Emerging Landscape of Targeted Therapy of Breast Cancers With Low Human Epidermal Growth Factor Receptor 2 Protein Expression
Gary Tozbikian, Savitri Krishnamurthy, Marilyn M. Bui, Michael Feldman, David G. Hicks, Shabnam Jaffer, Thaer Khoury, Shi Wei, Hannah Wen, Paula Pohlmann
Archives of Pathology & Laboratory Medicine.2024; 148(2): 242. CrossRef - Treatment Patterns and Health Outcomes among Patients with HER2 IHC0/-Low Metastatic or Recurrent Breast Cancer
Eliya Farah, Chantelle Carbonell, Devon J. Boyne, Darren R. Brenner, Jan-Willem Henning, Daniel Moldaver, Simran Shokar, Winson Y. Cheung
Cancers.2024; 16(3): 518. CrossRef - Clinical Internal Dosimetry and Biodistribution of 177Lu-DOTA-Trastuzumab in HER2-Positive Metastatic and Locally Advanced Breast Carcinoma
Yoga S. Narwadkar, Rahul V. Parghane, Sudeep Sahu, Sangita Lad, Kamal Deep, Gaurav Wanage, Tejal Suralkar, Sharmila Banerjee, Sudeep Gupta, Sandip Basu, Rajendra A. Badwe
Clinical Nuclear Medicine.2024; 49(4): e149. CrossRef - Molecular Classifications in Gastric Cancer: A Call for Interdisciplinary Collaboration
Cristina Díaz del Arco, María Jesús Fernández Aceñero, Luis Ortega Medina
International Journal of Molecular Sciences.2024; 25(5): 2649. CrossRef - The combined immunohistochemical expression of AMBRA1 and SQSTM1 identifies patients with poorly differentiated cutaneous squamous cell carcinoma at risk of metastasis: A proof of concept study
Michael H. Alexander, William J. Cousins, Tom Ewen, Andrew P. South, Penny Lovat, Niki Stefanos
Journal of Cutaneous Pathology.2024; 51(6): 450. CrossRef - Concordance between pathologists and between specimen types in detection of HER2-low breast carcinoma by immunohistochemistry
Jing Wang, Esther Yoon, Savitri Krishnamurthy
Annals of Diagnostic Pathology.2024; 70: 152288. CrossRef - Detection of HER2 expression using 99mTc-NM-02 nanobody in patients with breast cancer: a non-randomized, non-blinded clinical trial
Lingzhou Zhao, Yan Xing, Changcun Liu, Shaofei Ma, Wenhua Huang, Zhen Cheng, Jinhua Zhao
Breast Cancer Research.2024;[Epub] CrossRef - Pyrotinib and Trastuzumab Plus Chemotherapy Serve as an Acceptable Neoadjuvant Regimen Exhibiting Good Efficacy and Tolerance in HER2-Positive Breast Cancer Patients
Yibo Chen, Tianyi Zhang, Rui Zhang, Xuchen Cao
Cancer Biotherapy and Radiopharmaceuticals.2024; 39(6): 435. CrossRef - Clinicopathological and prognostic significance of VEGF, PDGF-B, and HER2/neu expression in gallbladder cancer
Pooja Shukla, Kumudesh Mishra, Ratnakar Shukla, Ruchira Vishwakarma, Niraj Kumari, Narendra Krishnani, Anu Behari, Vinay K. Kapoor
Journal of Cancer Research and Therapeutics.2024; 20(1): 349. CrossRef - Open questions, current challenges, and future perspectives in targeting human epidermal growth factor receptor 2-low breast cancer
G. Curigliano, R. Dent, H. Earle, S. Modi, P. Tarantino, G. Viale, S.M. Tolaney
ESMO Open.2024; 9(4): 102989. CrossRef - Concordance of HER2 status between core needle biopsy and surgical resection specimens of breast cancer: an analysis focusing on the HER2-low status
Sei Na, Milim Kim, Yujun Park, Hyun Jung Kwon, Hee-Chul Shin, Eun-Kyu Kim, Mijung Jang, Sun Mi Kim, So Yeon Park
Breast Cancer.2024; 31(4): 705. CrossRef - Impact of Neoadjuvant Chemotherapy (NAC) on Biomarker Expression in Breast Cancer
Suji Lee, Jee Yeon Kim, So Jeong Lee, Chung Su Hwang, Hyun Jung Lee, Kyung Bin Kim, Jung Hee Lee, Dong Hoon Shin, Kyung Un Choi, Chang Hun Lee, Gi Yeong Huh, Ahrong Kim
Medicina.2024; 60(5): 737. CrossRef - Clinical Use of Molecular Biomarkers in Canine and Feline Oncology: Current and Future
Heike Aupperle-Lellbach, Alexandra Kehl, Simone de Brot, Louise van der Weyden
Veterinary Sciences.2024; 11(5): 199. CrossRef - Clinical Validation of Artificial Intelligence–Powered PD-L1 Tumor Proportion Score Interpretation for Immune Checkpoint Inhibitor Response Prediction in Non–Small Cell Lung Cancer
Hyojin Kim, Seokhwi Kim, Sangjoon Choi, Changhee Park, Seonwook Park, Sergio Pereira, Minuk Ma, Donggeun Yoo, Kyunghyun Paeng, Wonkyung Jung, Sehhoon Park, Chan-Young Ock, Se-Hoon Lee, Yoon-La Choi, Jin-Haeng Chung
JCO Precision Oncology.2024;[Epub] CrossRef - Mesenchymal-epithelial transition factor amplification correlates with adverse pathological features and poor clinical outcome in colorectal cancer
Qiu-Xiao Yu, Ping-Ying Fu, Chi Zhang, Li Li, Wen-Ting Huang
World Journal of Gastrointestinal Surgery.2024; 16(5): 1395. CrossRef - Lipid nanoparticles-based RNA therapies for breast cancer treatment
Luigia Serpico, Yuewen Zhu, Renata Faria Maia, Sumedha Sumedha, Mohammad-Ali Shahbazi, Hélder A. Santos
Drug Delivery and Translational Research.2024; 14(10): 2823. CrossRef - Human epidermal growth factor receptor 2 (HER2) status in breast cancer: practice points and challenges
Natthawadee Laokulrath, Mihir Gudi, Syed Ahmed Salahuddin, Angela Phek Yoon Chong, Cristine Ding, Jabed Iqbal, Wei Qiang Leow, Benjamin Yongcheng Tan, Gary Tse, Emad Rakha, Puay Hoon Tan
Histopathology.2024; 85(3): 371. CrossRef - Comprehensive Immunohistochemical Analysis of Epithelial–Mesenchymal Transition Biomarkers in the Invasive Micropapillary Cancer of the Breast
Ozden Oz, Funda Alkan Tasli, Resmiye Irmak Yuzuguldu, Baha Zengel, Demet Kocatepe Cavdar, Merih Guray Durak, Raika Durusoy, Pranshu Sahgal
International Journal of Breast Cancer.2024;[Epub] CrossRef - Advancing HER2-low breast cancer management: enhancing diagnosis and treatment strategies
Simona Borstnar, Ivana Bozovic-Spasojevic, Ana Cvetanovic, Natalija Dedic Plavetic, Assia Konsoulova, Erika Matos, Lazar Popovic, Savelina Popovska, Snjezana Tomic, Eduard Vrdoljak
Radiology and Oncology.2024; 58(2): 258. CrossRef - Peer‐to‐peer validation of Ki‐67 scoring in a pathology quality circle as a tool to assess interobserver variability: are we better than we thought?
Marit Bernhardt, Leonie Weinhold, Christine Sanders, Oliver Hommerding, Jan‐Frederic Lau, Marieta Toma, Verena Tischler, Matthias Schmid, Tomasz Zienkiewicz, Ralf Hildenbrand, Peter Gerlach, Hui Zhou, Martin Braun, Gunnar Müller, Erich Sieber, Christian M
APMIS.2024; 132(10): 718. CrossRef - Immunohistochemical Expression of Cyclin D1 and p16 in Invasive Breast Carcinoma and Its Association with Clinicopathological Parameters
Shaivy Malik, Shakthivel V., Sana Ahuja, Charanjeet Ahluwalia
Indian Journal of Surgical Oncology.2024; 15(4): 864. CrossRef - Novel engineered HER2 specific recombinant protein nanocages for targeted drug delivery
Javad Kheshti, Mohammad Ahmadyousefi, Meysam Soleimani
Molecular Biology Reports.2024;[Epub] CrossRef - Circulating C-reactive protein levels as a prognostic biomarker in breast cancer across body mass index groups
J. B. Holm, E. Baggesen, D. Cronin-Fenton, J. Frystyk, J. M. Bruun, P. Christiansen, S. Borgquist
Scientific Reports.2024;[Epub] CrossRef - Standardized molecular pathology workflow for ctDNA-based ESR1 testing in HR+/HER2- metastatic breast cancer
Elena Guerini-Rocco, Konstantinos Venetis, Giulia Cursano, Eltjona Mane, Chiara Frascarelli, Francesco Pepe, Mariachiara Negrelli, Edoardo Olmeda, Davide Vacirca, Alberto Ranghiero, Dario Trapani, Carmen Criscitiello, Giuseppe Curigliano, Christian Rolfo,
Critical Reviews in Oncology/Hematology.2024; 201: 104427. CrossRef - The differences between pure and mixed invasive micropapillary breast cancer: the epithelial–mesenchymal transition molecules and prognosis
Ozden Oz, Resmiye Irmak Yuzuguldu, Ayse Yazici, Demet Kocatepe Cavdar, Cengiz Yilmaz, Mucteba Ozturk, Hilal Duzel, Duygu Gurel
Breast Cancer Research and Treatment.2024; 208(1): 41. CrossRef - Best practices for achieving consensus in HER2‐low expression in breast cancer: current perspectives from practising pathologists
Gary Tozbikian, Marilyn M. Bui, David G Hicks, Shabnam Jaffer, Thaer Khoury, Hannah Y Wen, Savitri Krishnamurthy, Shi Wei
Histopathology.2024; 85(3): 489. CrossRef - Consensus Guidelines on Human Epidermal Growth Factor Receptor 2 (HER2)-Low Testing in Breast Cancer in Malaysia
Pathmanathan Rajadurai, Sarala Ravindran, Bang Rom Lee, Suria Hayati Md Pauzi, Seow Fan Chiew, Kean Hooi Teoh, Navarasi S. Raja Gopal, Mastura Md Yusof, Cheng Har Yip
Cancers.2024; 16(13): 2325. CrossRef - Revolutionizing Pathology with Artificial Intelligence: Innovations in Immunohistochemistry
Diana Gina Poalelungi, Anca Iulia Neagu, Ana Fulga, Marius Neagu, Dana Tutunaru, Aurel Nechita, Iuliu Fulga
Journal of Personalized Medicine.2024; 14(7): 693. CrossRef - Interobserver Variability in HER‐2 Immunostaining Interpretation of Metastatic HER2 Low Breast Cancers in Cytology Specimens
Niyati Desai, Courtney F. Connelly, Simon Sung, Adela Cimic, Swikrity U. Baskota
Diagnostic Cytopathology.2024; 52(12): 722. CrossRef - Weakly-supervised deep learning models enable HER2-low prediction from H &E stained slides
Renan Valieris, Luan Martins, Alexandre Defelicibus, Adriana Passos Bueno, Cynthia Aparecida Bueno de Toledo Osorio, Dirce Carraro, Emmanuel Dias-Neto, Rafael A. Rosales, Jose Marcio Barros de Figueiredo, Israel Tojal da Silva
Breast Cancer Research.2024;[Epub] CrossRef - Understanding the spectrum of HER2 status in breast cancer: From HER2-positive to ultra-low HER2
Sana Ahuja, Adil Aziz Khan, Sufian Zaheer
Pathology - Research and Practice.2024; 262: 155550. CrossRef - Systematic review of added immunotherapy in traditional treatment for HER2 positive breast cancer patients
Rohan Choudhari
Innovative Practice in Breast Health.2024; 3-4: 100013. CrossRef - Detecting early-stage breast cancer with GATA3-positive circulating tumor cells
Chun-Hsin Hsieh, Ya-Herng Chang, Pei-Ying Ling, Ying-Tai Jin, Pei-Hsuan Lo, Hei-Jen Jou
Taiwanese Journal of Obstetrics and Gynecology.2024; 63(5): 745. CrossRef - First-in-human study of DP303c, a HER2-targeted antibody-drug conjugate in patients with HER2 positive solid tumors
Jian Zhang, Yiqun Du, Yanchun Meng, Xiaojun Liu, Yuxin Mu, Yunpeng Liu, Yehui Shi, Jufeng Wang, Aimin Zang, Shanzhi Gu, Tianshu Liu, Huan Zhou, Hongqian Guo, Silong Xiang, Xialu Zhang, Suqiong Wu, Huanhuan Qi, Mengke Li, Xichun Hu
npj Precision Oncology.2024;[Epub] CrossRef - Targeting CD276 for T cell-based immunotherapy of breast cancer
Ilona Hagelstein, Laura Wessling, Alexander Rochwarger, Latifa Zekri, Boris Klimovich, Christian M. Tegeler, Gundram Jung, Christian M. Schürch, Helmut R. Salih, Martina S. Lutz
Journal of Translational Medicine.2024;[Epub] CrossRef - Correlation of Androgen Receptor Expression With Ki67 Proliferative Index and Other Clinicopathological Characteristics in Invasive Mammary Carcinomas
D Keerthana Devi, V Pavithra, Leena D Joseph, Chithra Bhanu Challa
Cureus.2024;[Epub] CrossRef - CD81-guided heterologous EVs present heterogeneous interactions with breast cancer cells
Elena Gurrieri, Giulia Carradori, Michela Roccuzzo, Michael Pancher, Daniele Peroni, Romina Belli, Caterina Trevisan, Michela Notarangelo, Wen-Qiu Huang, Agata S. A. Carreira, Alessandro Quattrone, Guido Jenster, Timo L. M. Ten Hagen, Vito Giuseppe D’Agos
Journal of Biomedical Science.2024;[Epub] CrossRef - Deciphering HER2-low breast cancer (BC): insights from real-world data in early stage breast cancer
Anna Pous, Adrià Bernat-Peguera, Assumpció López-Paradís, Beatriz Cirauqui, Vanesa Quiroga, Iris Teruel, Eudald Felip, Angelica Ferrando-Díez, Milana Bergamino, Laia Boronat, Margarita Romeo, Gemma Soler, Christian Mariño, Paula Rodríguez-Martínez, Laura
Therapeutic Advances in Medical Oncology.2024;[Epub] CrossRef - Liquid biopsy-based technologies: a promising tool for biomarker identification in her2-low breast cancer patients for improved therapeutic outcomes
Aldo D’Alessandro, Anca Florentina Deaconu, Sandro Mandolesi, Federico Pio Fabrizio, Massimo Lombardi, Giovanna Liguori, Giovanni Pepe, Nicola Marino, Aureliano Stingi, Alessandro D’Alessandro, Antonio Giordano
Journal of Cancer Metastasis and Treatment.2024;[Epub] CrossRef - SPP1 mRNA Expression Is Associated with M2 Macrophage Infiltration and Poor Prognosis in Triple-Negative Breast Cancer
Yu-Chia Chen, Chia-Ching Chen, Rong-Fu Chen, Hsin-Hung Chen, Po-Ming Chen
Current Issues in Molecular Biology.2024; 46(12): 13499. CrossRef - MicroRNAs and their role in breast cancer metabolism (Review)
Wen Lee, Bann Yeo, Rozi Mahmud, Geok Tan, Mohamed Wahid, Yoke Cheah
International Journal of Oncology.2024;[Epub] CrossRef - CDH1 methylation and expression of E-cadherin and other markers in breast cancer
Luiz Fernando de Queiroz, Marcelo Soares da Mota e Silva, Fernando Colonna Rosman, Siane Lopes Bittencourt Rosas, Heitor Siffert Pereira de Souza, Maria da Glória da Costa Carvalho
Mastology.2024;[Epub] CrossRef - Surgical Management of the Axilla in HR+/HER2– Breast Cancer in the Z1071 Era: A Propensity Score-Matched Analysis of the National Cancer Database
Vayda R. Barker, Samer A. Naffouje, Melissa A. Mallory, Susan A. Hoover, Christine Laronga
Annals of Surgical Oncology.2023; 30(13): 8371. CrossRef - Noninvasive identification of HER2-low-positive status by MRI-based deep learning radiomics predicts the disease-free survival of patients with breast cancer
Yuan Guo, Xiaotong Xie, Wenjie Tang, Siyi Chen, Mingyu Wang, Yaheng Fan, Chuxuan Lin, Wenke Hu, Jing Yang, Jialin Xiang, Kuiming Jiang, Xinhua Wei, Bingsheng Huang, Xinqing Jiang
European Radiology.2023; 34(2): 899. CrossRef - Systemic investigation of inetetamab in combination with small molecules to treat HER2-overexpressing breast and gastric cancers
Lan Deng, Le Zhao, Lifen Liu, Haomin Huang
Open Life Sciences.2023;[Epub] CrossRef - HER2-low expression in patients with advanced or metastatic solid tumors
B. Uzunparmak, C. Haymaker, G. Raso, S. Masciari, L. Wang, H. Lin, A. Gorur, B. Kirby, A.-M. Cimo, A. Kennon, Q. Ding, G. Urschel, Y. Yuan, G. Feng, Y. Rizvi, A. Hussain, C. Zhu, P. Kim, G. Abbadessa, V. Subbiah, T.A. Yap, J. Rodon, S.A. Piha-Paul, F. Mer
Annals of Oncology.2023; 34(11): 1035. CrossRef - Data on 2D culture characterisation of potential markers in human HER2-positive breast cancer cell lines
Son H. Pham, Lyn R. Griffiths, Rachel K. Okolicsanyi, Larisa M. Haupt
Data in Brief.2023; 46: 108880. CrossRef - Determining HER2 Status by Artificial Intelligence: An Investigation of Primary, Metastatic, and HER2 Low Breast Tumors
Christiane Palm, Catherine E. Connolly, Regina Masser, Barbara Padberg Sgier, Eva Karamitopoulou, Quentin Simon, Beata Bode, Marianne Tinguely
Diagnostics.2023; 13(1): 168. CrossRef - Gene amplification mutations originate prior to selective stress in Acinetobacter baylyi
Jennifer A Herrmann, Agata Koprowska, Tesa J Winters, Nancy Villanueva, Victoria D Nikityuk, Feini Pek, Elizabeth M Reis, Constancia Z Dominguez, Daniel Davis, Eric McPherson, Staci R Rocco, Cynthia Recendez, Shyla M Difuntorum, Kelly Faeth, Mario D Lopez
G3.2023;[Epub] CrossRef - Flow Rate-Independent Multiscale Liquid Biopsy for Precision Oncology
Jie Wang, Robert Dallmann, Renquan Lu, Jing Yan, Jérôme Charmet
ACS Sensors.2023; 8(3): 1200. CrossRef - Single-cell HER2 quantification via instant signal amplification in microdroplets
Xiaoxian Liu, Yifan Zhu, Caoxin Li, Yanyun Fang, Jinna Chen, Fei Xu, Yanqing Lu, Perry Ping Shum, Ying Liu, Guanghui Wang
Analytica Chimica Acta.2023; 1251: 340976. CrossRef - Molecular imaging of HER2 receptor: Targeting HER2 for imaging and therapy in nuclear medicine
Daniela Miladinova
Frontiers in Molecular Biosciences.2023;[Epub] CrossRef - CORRELATION BETWEEN DIFFERENT CLINICOPATHOLOGICAL PARAMETERS AND MOLECULAR SUBTYPES OF FEMALE BREAST CARCINOMA IN SOUTH REGION OF IRAQ
Yassir Alaa Muhammed Hassan Shubbar
Wiadomości Lekarskie.2023; 76(1): 97. CrossRef - Pathological identification of HER2-low breast cancer: Tips, tricks, and troubleshooting for the optimal test
Elham Sajjadi, Elena Guerini-Rocco, Elisa De Camilli, Oriana Pala, Giovanni Mazzarol, Konstantinos Venetis, Mariia Ivanova, Nicola Fusco
Frontiers in Molecular Biosciences.2023;[Epub] CrossRef - Protective Effect of HER2 Gene Polymorphism rs24537331 in the Outcome of Canine Mammary Tumors
Ana Canadas-Sousa, Marta Santos, Patrícia Dias-Pereira
Animals.2023; 13(8): 1384. CrossRef - Can Patients with HER2-Low Breast Cancer Benefit from Anti-HER2 Therapies? A Review
Jin Wang, Dongying Liao, Xuemin Zhang, Changhong Miao, Kuang Chen
Breast Cancer: Targets and Therapy.2023; Volume 15: 281. CrossRef - HER2 Low Breast Cancer: A New Subtype or a Trojan for Cytotoxic Drug Delivery?
Marina Popović, Tajana Silovski, Marija Križić, Natalija Dedić Plavetić
International Journal of Molecular Sciences.2023; 24(9): 8206. CrossRef - HER2-Low Breast Cancer—Diagnostic Challenges and Opportunities for Insights from Ongoing Studies: A Podcast
Aditya Bardia, Giuseppe Viale
Targeted Oncology.2023; 18(3): 313. CrossRef - Histopathological and immunohistochemical analysis of predictive and prognostic markers in spontaneous canine mammary cancer
Vladimír Tancoš, Marcel Kovalik, Martin Levkut, Martina Bobrovská, Petra Kolenčíková, Ľubomír Straka, Zuzana Ševčíková, Ondřej Škor, Martina Antošová, Lukáš Plank, Keith L. Thoday
Acta Veterinaria Brno.2023; 92(2): 143. CrossRef - Dissecting sources of variability in patient response to targeted therapy: anti-HER2 therapies as a case study
Timothy Qi, Yanguang Cao
European Journal of Pharmaceutical Sciences.2023; 186: 106467. CrossRef - The Effect of HER2-Low Status on Pathological Complete Response and Survival in Triple-Negative Breast Cancer: A Systemic Review and Meta-Analysis
Yakup Ergun, Baran Akagunduz, Cengiz Karacin, Sema Turker, Gokhan Ucar
Clinical Breast Cancer.2023; 23(6): 567. CrossRef - Efficacy, toxicity and prognostic factors of pyrotinib‑involved neoadjuvant therapy in HER2‑positive breast cancer: A retrospective study
Hao Wang, Hailing Cao, Zhiyun Guo
Oncology Letters.2023;[Epub] CrossRef - Advancements in clinical aspects of targeted therapy and immunotherapy in breast cancer
Feng Ye, Saikat Dewanjee, Yuehua Li, Niraj Kumar Jha, Zhe-Sheng Chen, Ankush Kumar, Vishakha, Tapan Behl, Saurabh Kumar Jha, Hailin Tang
Molecular Cancer.2023;[Epub] CrossRef - Weakly supervised bilayer convolutional network in segmentation of HER2 related cells to guide HER2 targeted therapies
Ching-Wei Wang, Kun-Lin Lin, Hikam Muzakky, Yi-Jia Lin, Tai-Kuang Chao
Computerized Medical Imaging and Graphics.2023; 108: 102270. CrossRef - Immune Biomarkers in Triple-Negative Breast Cancer: Improving the Predictivity of Current Testing Methods
Francesca Maria Porta, Elham Sajjadi, Konstantinos Venetis, Chiara Frascarelli, Giulia Cursano, Elena Guerini-Rocco, Nicola Fusco, Mariia Ivanova
Journal of Personalized Medicine.2023; 13(7): 1176. CrossRef - HER2 Equivocal (Score = 2+) Breast Carcinoma Cases Identified by Immunohistochemistry at a South African Hospital. What is the Impact of Fluorescent In Situ Hybridization Testing?
Reena Dhansukh Mohanlal, Nikki Bouwer, Pascale Willem
Applied Immunohistochemistry & Molecular Morphology.2023; 31(8): 555. CrossRef - Discordance of HER2 Expression and/or Amplification on Repeat Testing
Timothy P. DiPeri, Kathleen Kong, Kaushik Varadarajan, Daniel D. Karp, Jaffer A. Ajani, Shubham Pant, Michael F. Press, Sarina A. Piha-Paul, Ecaterina E. Dumbrava, Funda Meric-Bernstam
Molecular Cancer Therapeutics.2023; 22(8): 976. CrossRef - Low and Ultra-Low HER2 in Human Breast Cancer: An Effort to Define New Neoplastic Subtypes
Mariausilia Franchina, Cristina Pizzimenti, Vincenzo Fiorentino, Maurizio Martini, Giuseppina Rosaria Rita Ricciardi, Nicola Silvestris, Antonio Ieni, Giovanni Tuccari
International Journal of Molecular Sciences.2023; 24(16): 12795. CrossRef - Genetic analysis of oligo-recurrence breast cancer: correlation with clinical outcomes
Kuikui Jiang, Danyang Zhou, Fei Xu, Wen Xia, Qiufan Zheng, Qianyi Lu, Rongzhen Luo, Ruoxi Hong, Shusen Wang
BMC Cancer.2023;[Epub] CrossRef - Single domain antibodies specific for HER2 dimerization domain effectively disrupts HER2 dimerization
Ahmad Najafi, Reza Valadan, Hossein Asgarian-Omran, Alireza Rafiei, Mohsen Tehrani
International Immunopharmacology.2023; 124: 110999. CrossRef - Récepteur du facteur de croissance épidermique HER2, tests utilisés pour rechercher son amplification dans le cancer du sein : principes et limites
Imane Eliahiai, Mohammed Eljiar, Sanae Chaib, Jinane KHarmoum, Mariame Chraïbi
Bulletin du Cancer.2023; 110(12): 1301. CrossRef - Integrated Molecular Characterization of HER2-Low Breast Cancer Using Next Generation Sequencing (NGS)
Jean-Louis Merlin, Marie Husson, Nassim Sahki, Pauline Gilson, Vincent Massard, Alexandre Harlé, Agnès Leroux
Biomedicines.2023; 11(12): 3164. CrossRef - GLUCOSE LEVELS OF PLEURAL EFFUSION FLUID AND HER2 STATUS IN PLEURAL-METASTATIC BREAST CANCER
Muhammad Dhanny Irawan, Desak Gede Agung Suprabawati, Heru Purwanto
Majalah Biomorfologi.2023; 33(2): 75. CrossRef - Design of a Ratiometric Plasmonic Biosensor for Herceptin Detection in HER2-Positive Breast Cancer
Neda Shahbazi, Rouholah Zare-Dorabei, Seyed Morteza Naghib
ACS Biomaterials Science & Engineering.2022; 8(2): 871. CrossRef - A highly sensitive nanobiosensor based on aptamer-conjugated graphene-decorated rhodium nanoparticles for detection of HER2-positive circulating tumor cells
Mahdi Sadeghi, Soheila Kashanian, Seyed Morteza Naghib, Esfandyar Askari, Fateme Haghiralsadat, Davood Tofighi
Nanotechnology Reviews.2022; 11(1): 793. CrossRef - Anti-HER2 therapy in metastatic breast cancer: many choices and future directions
Carrie S. Wynn, Shou-Ching Tang
Cancer and Metastasis Reviews.2022; 41(1): 193. CrossRef - Electroanalytical overview: screen-printed electrochemical sensing platforms for the detection of vital cardiac, cancer and inflammatory biomarkers
Robert D. Crapnell, Alejandro Garcia-Miranda Ferrari, Nina C. Dempsey, Craig E. Banks
Sensors & Diagnostics.2022; 1(3): 405. CrossRef - FTO genotype was associated with breast cancer in HER2 negative patients
Fateme Montazeri, Hossein Hatami, Soroor Fathi, Naeemeh Hasanpour Ardekanizadeh, Fatemeh Bourbour, Samira Rastgoo, Fatemeh Shafiee, Mohammad Esmail Akbari, Maryam Gholamalizadeh, Seyed Alireza Mosavi Jarrahi, Saeid Doaei
Clinical Nutrition ESPEN.2022; 49: 495. CrossRef - Breast Cancer Human Epidermal Growth Factor Receptor 2 mRNA Molecular Testing Compared to Immunohistochemistry with Correlation to Neoadjuvant Therapy Response
Mahmoud Behairy, Samia Mohamed Gabal, Mohamed Sherif Negm
Open Access Macedonian Journal of Medical Sciences.2022; 10(A): 352. CrossRef - Validity and utility of HER2/ERBB2 copy number variation assessed in liquid biopsies from breast cancer patients: A systematic review
Noortje Verschoor, Teoman Deger, Agnes Jager, Stefan Sleijfer, Saskia M. Wilting, John W.M. Martens
Cancer Treatment Reviews.2022; 106: 102384. CrossRef - RETRACTED: Longitude Variation of the microRNA-497/FGF-23 Axis during Treatment and Its Linkage with Neoadjuvant/Adjuvant Trastuzumab-Induced Cardiotoxicity in HER2-Positive Breast Cancer Patients
Hui Liu, Xiaoyan Hu, Lingyun Wang, Tao Du, Jing Feng, Ming Li, Lei Liu, Xiaofang Liu
Frontiers in Surgery.2022;[Epub] CrossRef - Use of Radionuclide-Based Imaging Methods in Breast Cancer
Betül Altunay, Agnieszka Morgenroth, Felix M. Mottaghy
Seminars in Nuclear Medicine.2022; 52(5): 561. CrossRef - Functional regulations between genetic alteration-driven genes and drug target genes acting as prognostic biomarkers in breast cancer
Li Wang, Lei Yu, Jian Shi, Feng Li, Caiyu Zhang, Haotian Xu, Xiangzhe Yin, Lixia Wang, Shihua Lin, Anastasiia Litvinova, Yanyan Ping, Shangwei Ning, Hongying Zhao
Scientific Reports.2022;[Epub] CrossRef - Human epidermal growth factor receptor-2 and endocrine resistance in hormone-dependent breast cancer
Anastasia Alataki, Mitch Dowsett
Endocrine-Related Cancer.2022; 29(8): R105. CrossRef - The Evolution of Targeted Radionuclide Diagnosis of HER2-Positive Breast Cancer
Olga D. Bragina, Sergei M. Deyev, Vladimir I. Chernov, Vladimir M. Tolmachev
Acta Naturae.2022; 14(2): 4. CrossRef - Deriving tumor purity from cancer next generation sequencing data: applications for quantitative ERBB2 (HER2) copy number analysis and germline inference of BRCA1 and BRCA2 mutations
Stephanie E. Siegmund, Danielle K. Manning, Phani K. Davineni, Fei Dong
Modern Pathology.2022; 35(10): 1458. CrossRef - Current challenges and unmet needs in treating patients with human epidermal growth factor receptor 2-positive advanced breast cancer
Matti Aapro, Fatima Cardoso, Giuseppe Curigliano, Alexandru Eniu, Joseph Gligorov, Nadia Harbeck, Andreas Mueller, Olivia Pagani, Shani Paluch-Shimon, Elzbieta Senkus, Beat Thürlimann, Khalil Zaman
The Breast.2022; 66: 145. CrossRef - [Retracted] Application of Fluorescence In Situ Hybridization Assisted by Fluorescence Microscope in Detection of Her2 Gene in Breast Cancer Patients
Fang Lu, Tingting Zhou, Yan Liu, Liying Song, Bin Zhang, Yuyan Li, Sorayouth Chumnanvej
Contrast Media & Molecular Imaging.2022;[Epub] CrossRef - High sensitivity label-free detection of HER2 using an Al–GaN/GaN high electron mobility transistor-based biosensor
Shivanshu Mishra, Pharyanshu Kachhawa, Amber Kumar Jain, Rajiv Ranjan Thakur, Nidhi Chaturvedi
Lab on a Chip.2022; 22(21): 4129. CrossRef - Indian Data on HER2 Fluorescence In Situ Hybridization in Invasive Breast Cancer with Immunohistochemically Equivocal Results As Per 2018 ASCO/CAP Guidelines
B. R. Nagarjun, Biren Parikh, Manaswi Nareshkumar Patel, Pina J. Trivedi, Dharmesh M. Patel
South Asian Journal of Cancer.2022; 11(04): 281. CrossRef - S‑phase fraction, lymph node status and disease staging as the main prognostic factors to differentiate between young and older patients with invasive breast carcinoma
António Pinto, João Matos, Teresa Pereira, Giovani Silva, Saudade André
Oncology Letters.2022;[Epub] CrossRef - Inferring tumor-specific cancer dependencies through integrating ex vivo drug response assays and drug-protein profiling
Alina Batzilla, Junyan Lu, Jarno Kivioja, Kerstin Putzker, Joe Lewis, Thorsten Zenz, Wolfgang Huber, James Gallo
PLOS Computational Biology.2022; 18(8): e1010438. CrossRef - Clinical possibilities of HER2-positive breast cancer diagnosis using alternative scaffold proteins
O. D. Bragina, V. I. Chernov, S. M. Deyev, V. M. Tolmachev
Bulletin of Siberian Medicine.2022; 21(3): 132. CrossRef - Molecular Pathology of Gastric Cancer
Moonsik Kim, An Na Seo
Journal of Gastric Cancer.2022; 22(4): 264. CrossRef - Loss of NECTIN1 triggers melanoma dissemination upon local IGF1 depletion
Julien Ablain, Amira Al Mahi, Harriet Rothschild, Meera Prasad, Sophie Aires, Song Yang, Maxim E. Dokukin, Shuyun Xu, Michelle Dang, Igor Sokolov, Christine G. Lian, Leonard I. Zon
Nature Genetics.2022; 54(12): 1839. CrossRef - Advanced diagnosis technologies for HER2 breast cancer markers
Mengxue Zhang
Highlights in Science, Engineering and Technology.2022; 14: 44. CrossRef - An Overview of Clinical Development of Agents for Metastatic or Advanced Breast Cancer Without ERBB2 Amplification (HER2-Low)
Aleix Prat, Aditya Bardia, Giuseppe Curigliano, M. Elizabeth H. Hammond, Sibylle Loibl, Sara M. Tolaney, Giuseppe Viale
JAMA Oncology.2022; 8(11): 1676. CrossRef - Development of T-cell engagers selective for cells co-expressing two antigens
Danielle M. Dicara, Sunil Bhakta, Mary Ann Go, James Ziai, Ron Firestein, Bill Forrest, Chen Gu, Steven R. Leong, Genee Lee, Shang-Fan Yu, Andrew G. Polson, Nicholas J. Agard
mAbs.2022;[Epub] CrossRef - The clinical significance of HER2 expression in DCIS
Ioanna Akrida, Francesk Mulita
Medical Oncology.2022;[Epub] CrossRef - Antibody-Drug Conjugates in Breast Cancer: Spotlight on HER2
Rachel Occhiogrosso Abelman, Arielle Medford, Laura Spring, Aditya Bardia
The Cancer Journal.2022; 28(6): 423. CrossRef - The Clinical Utility of Droplet Digital PCR for Profiling Circulating Tumor DNA in Breast Cancer Patients
Ugur Gezer, Abel J. Bronkhorst, Stefan Holdenrieder
Diagnostics.2022; 12(12): 3042. CrossRef - Lapatinib and lapatinib plus trastuzumab therapy versus trastuzumab therapy for HER2 positive breast cancer patients: an updated systematic review and meta-analysis
Ye Yuan, Xumei Liu, Yi Cai, Wenyuan Li
Systematic Reviews.2022;[Epub] CrossRef - Interactions dietary components with expression level of breast cancer-related genes
Fatemeh Bourbour, Azam Pourtaheri, Khadijeh Abbasi, Naeemeh Hasanpour Ardekanizadeh, Maryam Gholamalizadeh, Azadeh Hajipour, Sepideh Abdollahi, Seyedeh Elaheh Bagheri, Mina Ahmadzadeh, Saeid Doaei, Arezoo Haghighian
Egyptian Journal of Medical Human Genetics.2022;[Epub] CrossRef - HER2-directed antibodies, affibodies and nanobodies as drug-delivery vehicles in breast cancer with a specific focus on radioimmunotherapy and radioimmunoimaging
Betül Altunay, Agnieszka Morgenroth, Mohsen Beheshti, Andreas Vogg, Nicholas C. L. Wong, Hong Hoi Ting, Hans-Jürgen Biersack, Elmar Stickeler, Felix M. Mottaghy
European Journal of Nuclear Medicine and Molecular Imaging.2021; 48(5): 1371. CrossRef - Risk-based decision-making in the treatment of HER2-positive early breast cancer: Recommendations based on the current state of knowledge
Christian Jackisch, Patricia Cortazar, Charles E. Geyer, Luca Gianni, Joseph Gligorov, Zuzana Machackova, Edith A. Perez, Andreas Schneeweiss, Sara M. Tolaney, Michael Untch, Andrew Wardley, Martine Piccart
Cancer Treatment Reviews.2021; 99: 102229. CrossRef - Histologic Patterns of Cutaneous Metastases of Breast Carcinoma: A Clinicopathologic Study of 232 Cases
Shira Ronen, David Suster, Wei-Shen Chen, Natali Ronen, Sri Krishna C. Arudra, Celestine Trinidad, Doina Ivan, Victor G. Prieto, Saul Suster
The American Journal of Dermatopathology.2021; 43(6): 401. CrossRef - Standardized pathology report for breast cancer
Soo Youn Cho, So Yeon Park, Young Kyung Bae, Jee Yeon Kim, Eun Kyung Kim, Woo Gyeong Kim, Youngmee Kwon, Ahwon Lee, Hee Jin Lee, Ji Shin Lee, Jee Young Park, Gyungyub Gong, Hye Kyoung Yoon
Journal of Pathology and Translational Medicine.2021; 55(1): 1. CrossRef - The impact of oral contraceptive use on breast cancer risk: State of the art and future perspectives in the era of 4P medicine
R. Bonfiglio, M.L. Di Pietro
Seminars in Cancer Biology.2021; 72: 11. CrossRef - The Co-Expression of Melanoma-Antigen Family a Proteins and New York Esophageal Squamous Cell Carcinoma-1 in Breast Cancer: A Pilot Study
Yu-Xin Wang, Feng-Lian Li, Li-Xin Du, Jun-Fang Liu, Li-Gang Huo, Shu-Qing Li, Bin Tian
Cancer Management and Research.2021; Volume 13: 6123. CrossRef - Targeting HER2 protein in individual cells using ICP-MS detection and its potential as prognostic and predictive breast cancer biomarker
A. Fernández Asensio, M. Corte-Rodríguez, J. Bettmer, L.M. Sierra, M. Montes-Bayón, E. Blanco- González
Talanta.2021; 235: 122773. CrossRef - Development of a 99mTc-Labeled Single-Domain Antibody for SPECT/CT Assessment of HER2 Expression in Breast Cancer
Lingzhou Zhao, Changcun Liu, Yan Xing, Jin He, Jim O’Doherty, Wenhua Huang, Jinhua Zhao
Molecular Pharmaceutics.2021; 18(9): 3616. CrossRef - WITHDRAWN: Nouvelles stratégies thérapeutiques dans les cancers du sein HER2-surexprimé
Benoîte Mery, Philippe Toussaint, Pierre-Etienne Heudel, Armelle Dufresne, Mélodie Carbonnaux, Hélène Vanacker, Thomas Bachelot, Olivier Trédan
Bulletin du Cancer.2021;[Epub] CrossRef - Retrospective observational study of HER2 immunohistochemistry in borderline breast cancer patients undergoing neoadjuvant therapy, with an emphasis on Group 2 (HER2/CEP17 ratio ≥2.0, HER2 copy number <4.0 signals/cell) cases
Emad A. Rakha, Islam M. Miligy, Cecily M. Quinn, Elena Provenzano, Abeer M. Shaaban, Caterina Marchiò, Michael S. Toss, Grace Gallagy, Ciara Murray, Janice Walshe, Ayaka Katayama, Karim Eldib, Nahla Badr, Bruce Tanchel, Rebecca Millican-Slater, Colin Purd
British Journal of Cancer.2021; 124(11): 1836. CrossRef - Loss of HER2‐positivity following neoadjuvant targeted therapy for breast cancer is not associated with inferior oncologic outcomes
Catherine L. Wetzel, Thomas L. Sutton, Stuart Gardiner, Maryam Farinola, Nathalie Johnson, Jennifer R. Garreau
Journal of Surgical Oncology.2021; 124(8): 1224. CrossRef - Clinical and Genetic Predictive Models for the Prediction of Pathological Complete Response to Optimize the Effectiveness for Trastuzumab Based Chemotherapy
Lun Li, Min Chen, Shuyue Zheng, Hanlu Li, Weiru Chi, Bingqiu Xiu, Qi Zhang, Jianjing Hou, Jia Wang, Jiong Wu
Frontiers in Oncology.2021;[Epub] CrossRef - tRNA‐derived fragments: tRF‐Gly‐CCC‐046, tRF‐Tyr‐GTA‐010 and tRF‐Pro‐TGG‐001 as novel diagnostic biomarkers for breast cancer
Yue Zhang, Zhao Bi, Xiaohan Dong, Miao Yu, Kangyu Wang, Xingguo Song, Li Xie, Xianrang Song
Thoracic Cancer.2021; 12(17): 2314. CrossRef - Detection of secondary metastatic breast cancer by measurement of plasma CA 15.3
L. De Cock, J. Heylen, A. Wildiers, K. Punie, A. Smeets, C. Weltens, P. Neven, J. Billen, A. Laenen, H. Wildiers
ESMO Open.2021; 6(4): 100203. CrossRef - Standardized Pathology Report for Breast Cancer
Soo Youn Cho, So Yeon Park, Young Kyung Bae, Jee Yeon Kim, Eun Kyung Kim, Woo Gyeong Kim, Youngmee Kwon, Ahwon Lee, Hee Jin Lee, Ji Shin Lee, Jee Young Park, Gyungyub Gong, Hye Kyoung Yoon
Journal of Breast Cancer.2021; 24(1): 1. CrossRef - Circular RNA circ-ERBB2 promotes HER2-positive breast cancer progression and metastasis via sponging miR-136-5p and miR-198
Jin-xiu Zhong, Yun-yuan Kong, Rong-guang Luo, Guo-jin Xia, Wen-xing He, Xue-zhong Chen, Wei-wei Tan, Qing-jie Chen, Yu-yin Huang, Yan-xing Guan
Journal of Translational Medicine.2021;[Epub] CrossRef - Nouvelles stratégies thérapeutiques dans les cancers du sein HER2-surexprimé
Benoîte Mery, Philippe Toussaint, Pierre-Etienne Heudel, Armelle Dufresne, Mélodie Carbonnaux, Hélène Vanacker, Thomas Bachelot, Olivier Trédan
Bulletin du Cancer.2021; 108(11): 11S8. CrossRef - Association of Estrogen and Progesterone Receptors with Clinicopathological Prognostic Factors in Breast Cancer
Ali Abdul Hadi Abdul-Kareem, Qahtan A. Mahdi
Medical Journal of Babylon.2021; 18(2): 111. CrossRef - HER2 alterations in non-small-cell lung cancer – Druggable or undruggable?
Suresh Kumar Bondili, Ravindra Nandhana, Vanita Noronha, Swayamprabha Pawar, Nandini Menon, Omshree Shetty, Anuradha Chougule, Abhishek Mahajan, Rajiv Kumar, Vijay M. Patil, Amit Joshi, Kumar Prabhash
Cancer Research, Statistics, and Treatment.2021; 4(2): 374. CrossRef - UCNP-based Photoluminescent Nanomedicines for Targeted Imaging and Theranostics of Cancer
Evgenii L. Guryev, Anita S. Smyshlyaeva, Natalia Y. Shilyagina, Evgeniya A. Sokolova, Samah Shanwar, Alexey B. Kostyuk, Alexander V. Lyubeshkin, Alexey A. Schulga, Elena V. Konovalova, Quan Lin, Indrajit Roy, Irina V. Balalaeva, Sergey M. Deyev, Andrei V.
Molecules.2020; 25(18): 4302. CrossRef - Impact of the Updated Guidelines on Human Epidermal Growth Factor Receptor 2 (HER2) Testing in Breast Cancer
Min Chong Kim, Su Hwan Kang, Jung Eun Choi, Young Kyung Bae
Journal of Breast Cancer.2020; 23(5): 484. CrossRef
- A Comprehensive Model Outperformed the Single Radiomics Model in Noninvasively Predicting the HER2 Status in Patients with Breast Cancer
- Good Laboratory Standards for Clinical Next-Generation Sequencing Cancer Panel Tests
- Jihun Kim, Woong-Yang Park, Nayoung K. D. Kim, Se Jin Jang, Sung-Min Chun, Chang-Ohk Sung, Jene Choi, Young-Hyeh Ko, Yoon-La Choi, Hyo Sup Shim, Jae-Kyung Won
- J Pathol Transl Med. 2017;51(3):191-204. Published online May 10, 2017
- DOI: https://doi.org/10.4132/jptm.2017.03.14
- 29,164 View
- 1,118 Download
- 36 Web of Science
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF - Next-generation sequencing (NGS) has recently emerged as an essential component of personalized cancer medicine due to its high throughput and low per-base cost. However, no sufficient guidelines for implementing NGS as a clinical molecular pathology test are established in Korea. To ensure clinical grade quality without inhibiting adoption of NGS, a taskforce team assembled by the Korean Society of Pathologists developed laboratory guidelines for NGS cancer panel testing procedures and requirements for clinical implementation of NGS. This consensus standard proposal consists of two parts: laboratory guidelines and requirements for clinical NGS laboratories. The laboratory guidelines part addressed several important issues across multistep NGS cancer panel tests including choice of gene panel and platform, sample handling, nucleic acid management, sample identity tracking, library preparation, sequencing, analysis and reporting. Requirements for clinical NGS tests were summarized in terms of documentation, validation, quality management, and other required written policies. Together with appropriate pathologist training and international laboratory standards, these laboratory standards would help molecular pathology laboratories to successfully implement NGS cancer panel tests in clinic. In this way, the oncology community would be able to help patients to benefit more from personalized cancer medicine.
-
Citations
Citations to this article as recorded by- Tumour purity assessment with deep learning in colorectal cancer and impact on molecular analysis
Lydia A Schoenpflug, Aikaterini Chatzipli, Korsuk Sirinukunwattana, Susan Richman, Andrew Blake, James Robineau, Kirsten D Mertz, Clare Verrill, Simon J Leedham, Claire Hardy, Celina Whalley, Keara Redmond, Philip Dunne, Steven Walker, Andrew D Beggs, Ult
The Journal of Pathology.2025; 265(2): 184. CrossRef - Clinical Validation of Local Versus Commercial Genomic Testing in Cancer: A Comparison of Tissue and Plasma Concordance
Lucy G. Faulkner, Lynne Howells, Susann Lehman, Caroline Cowley, Zahirah Sidat, Jacqui Shaw, Anne L. Thomas
Cancer Investigation.2025; 43(2): 119. CrossRef - Diagnostic Implications of NGS-Based Molecular Profiling in Mature B-Cell Lymphomas with Potential Bone Marrow Involvement
Bernhard Strasser, Sebastian Mustafa, Josef Seier, Erich Wimmer, Josef Tomasits
Diagnostics.2025; 15(6): 727. CrossRef - Pragmatic nationwide master observational trial based on genomic alterations in advanced solid tumors: KOrean Precision Medicine Networking Group Study of MOlecular profiling guided therapy based on genomic alterations in advanced Solid tumors (KOSMOS)-II
Sun Young Kim, Jee Hyun Kim, Tae-Yong Kim, Sook Ryun Park, Shinkyo Yoon, Soohyeon Lee, Se-Hoon Lee, Tae Min Kim, Sae-Won Han, Hye Ryun Kim, Hongseok Yun, Sejoon Lee, Jihun Kim, Yoon-La Choi, Kui Son Choi, Heejung Chae, Hyewon Ryu, Gyeong-Won Lee, Dae Youn
BMC Cancer.2024;[Epub] CrossRef - Reporting of somatic variants in clinical cancer care: recommendations of the Swiss Society of Molecular Pathology
Yann Christinat, Baptiste Hamelin, Ilaria Alborelli, Paolo Angelino, Valérie Barbié, Bettina Bisig, Heather Dawson, Milo Frattini, Tobias Grob, Wolfram Jochum, Ronny Nienhold, Thomas McKee, Matthias Matter, Edoardo Missiaglia, Francesca Molinari, Sacha Ro
Virchows Archiv.2024; 485(6): 1033. CrossRef - Acute myeloid leukemia and myelodysplastic neoplasms: clinical implications of myelodysplasia-related genes mutations and TP53 aberrations
Hyunwoo Kim, Ja Young Lee, Shinae Yu, Eunkyoung Yoo, Hye Ran Kim, Sang Min Lee, Won Sik Lee
Blood Research.2024;[Epub] CrossRef - Validation and Clinical Application of ONCOaccuPanel for Targeted Next-Generation Sequencing of Solid Tumors
Moonsik Kim, Changseon Lee, Juyeon Hong, Juhee Kim, Ji Yun Jeong, Nora Jee-Young Park, Ji-Eun Kim, Ji Young Park
Cancer Research and Treatment.2023; 55(2): 429. CrossRef - Establishing molecular pathology curriculum for pathology trainees and continued medical education: a collaborative work from the Molecular Pathology Study Group of the Korean Society of Pathologists
Jiwon Koh, Ha Young Park, Jeong Mo Bae, Jun Kang, Uiju Cho, Seung Eun Lee, Haeyoun Kang, Min Eui Hong, Jae Kyung Won, Youn-La Choi, Wan-Seop Kim, Ahwon Lee
Journal of Pathology and Translational Medicine.2023; 57(5): 265. CrossRef - Clinical applications of next-generation sequencing in the diagnosis of genetic disorders in Korea: a narrative review
Jihoon G. Yoon, Man Jin Kim, Yong Jin Kwon, Jong-Hee Chae
Journal of the Korean Medical Association.2023; 66(10): 613. CrossRef - Obtaining spatially resolved tumor purity maps using deep multiple instance learning in a pan-cancer study
Mustafa Umit Oner, Jianbin Chen, Egor Revkov, Anne James, Seow Ye Heng, Arife Neslihan Kaya, Jacob Josiah Santiago Alvarez, Angela Takano, Xin Min Cheng, Tony Kiat Hon Lim, Daniel Shao Weng Tan, Weiwei Zhai, Anders Jacobsen Skanderup, Wing-Kin Sung, Hwee
Patterns.2022; 3(2): 100399. CrossRef - Update on Molecular Diagnosis in Extranodal NK/T-Cell Lymphoma and Its Role in the Era of Personalized Medicine
Ka-Hei (Murphy) Sun, Yin-Ting (Heylie) Wong, Ka-Man (Carmen) Cheung, Carmen (Michelle) Yuen, Yun-Tat (Ted) Chan, Wing-Yan (Jennifer) Lai, Chun (David) Chao, Wing-Sum (Katie) Fan, Yuen-Kiu (Karen) Chow, Man-Fai Law, Ho-Chi (Tommy) Tam
Diagnostics.2022; 12(2): 409. CrossRef - Defining Novel DNA Virus-Tumor Associations and Genomic Correlates Using Prospective Clinical Tumor/Normal Matched Sequencing Data
Chad M. Vanderbilt, Anita S. Bowman, Sumit Middha, Kseniya Petrova-Drus, Yi-Wei Tang, Xin Chen, Youxiang Wang, Jason Chang, Natasha Rekhtman, Klaus J. Busam, Sounak Gupta, Meera Hameed, Maria E. Arcila, Marc Ladanyi, Michael F. Berger, Snjezana Dogan, Ahm
The Journal of Molecular Diagnostics.2022; 24(5): 515. CrossRef - Performance Evaluation of Three DNA Sample Tracking Tools in a Whole Exome Sequencing Workflow
Gertjan Wils, Céline Helsmoortel, Pieter-Jan Volders, Inge Vereecke, Mauro Milazzo, Jo Vandesompele, Frauke Coppieters, Kim De Leeneer, Steve Lefever
Molecular Diagnosis & Therapy.2022; 26(4): 411. CrossRef - Clinical Quality Considerations when Using Next-Generation Sequencing (NGS) in Clinical Drug Development
Timothé Ménard, Alaina Barros, Christopher Ganter
Therapeutic Innovation & Regulatory Science.2021; 55(5): 1066. CrossRef - Fast Healthcare Interoperability Resources (FHIR)–Based Quality Information Exchange for Clinical Next-Generation Sequencing Genomic Testing: Implementation Study
Donghyeong Seong, Sungwon Jung, Sungchul Bae, Jongsuk Chung, Dae-Soon Son, Byoung-Kee Yi
Journal of Medical Internet Research.2021; 23(4): e26261. CrossRef - Status of Next-Generation Sequencing-Based Genetic Diagnosis in Hematologic Malignancies in Korea (2017-2018)
JinJu Kim, Ja Young Lee, Jungwon Huh, Myung-Hyun Nam, Myungshin Kim, Young-Uk Cho, Sun-Young Kong, Seung-Tae Lee, In-Suk Kim
Laboratory Medicine Online.2021; 11(1): 25. CrossRef - MSI-Testung
Josef Rüschoff, Gustavo Baretton, Hendrik Bläker, Wolfgang Dietmaier, Manfred Dietel, Arndt Hartmann, Lars-Christian Horn, Korinna Jöhrens, Thomas Kirchner, Ruth Knüchel, Doris Mayr, Sabine Merkelbach-Bruse, Hans-Ulrich Schildhaus, Peter Schirmacher, Mark
Der Pathologe.2021; 42(4): 414. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - MSI testing
Josef Rüschoff, Gustavo Baretton, Hendrik Bläker, Wolfgang Dietmaier, Manfred Dietel, Arndt Hartmann, Lars-Christian Horn, Korinna Jöhrens, Thomas Kirchner, Ruth Knüchel, Doris Mayr, Sabine Merkelbach-Bruse, Hans-Ulrich Schildhaus, Peter Schirmacher, Mark
Der Pathologe.2021; 42(S1): 110. CrossRef - 16S rDNA microbiome composition pattern analysis as a diagnostic biomarker for biliary tract cancer
Huisong Lee, Hyeon Kook Lee, Seog Ki Min, Won Hee Lee
World Journal of Surgical Oncology.2020;[Epub] CrossRef - Risk Stratification Using a Novel Genetic Classifier IncludingPLEKHS1Promoter Mutations for Differentiated Thyroid Cancer with Distant Metastasis
Chan Kwon Jung, Seung-Hyun Jung, Sora Jeon, Young Mun Jeong, Yourha Kim, Sohee Lee, Ja-Seong Bae, Yeun-Jun Chung
Thyroid.2020; 30(11): 1589. CrossRef - Biomarker testing for advanced lung cancer by next-generation sequencing; a valid method to achieve a comprehensive glimpse at mutational landscape
Anurag Mehta, Smreti Vasudevan, Sanjeev Kumar Sharma, Manoj Panigrahi, Moushumi Suryavanshi, Mumtaz Saifi, Ullas Batra
Applied Cancer Research.2020;[Epub] CrossRef - Application Areas of Traditional Molecular Genetic Methods and NGS in relation to Hereditary Urological Cancer Diagnosis
Dmitry S. Mikhaylenko, Alexander S. Tanas, Dmitry V. Zaletaev, Marina V. Nemtsova
Journal of Oncology.2020; 2020: 1. CrossRef - Assembling and Validating Bioinformatic Pipelines for Next-Generation Sequencing Clinical Assays
Jeffrey A SoRelle, Megan Wachsmann, Brandi L. Cantarel
Archives of Pathology & Laboratory Medicine.2020; 144(9): 1118. CrossRef - Standard operating procedure for somatic variant refinement of sequencing data with paired tumor and normal samples
Erica K. Barnell, Peter Ronning, Katie M. Campbell, Kilannin Krysiak, Benjamin J. Ainscough, Lana M. Sheta, Shahil P. Pema, Alina D. Schmidt, Megan Richters, Kelsy C. Cotto, Arpad M. Danos, Cody Ramirez, Zachary L. Skidmore, Nicholas C. Spies, Jasreet Hun
Genetics in Medicine.2019; 21(4): 972. CrossRef - A DNA pool of FLT3-ITD positive DNA samples can be used efficiently for analytical evaluation of NGS-based FLT3-ITD quantitation - Testing several different ITD sequences and rates, simultaneously
Zoltán A. Mezei, Dávid Tornai, Róza Földesi, László Madar, Andrea Sümegi, Mária Papp, Péter Antal-Szalmás
Journal of Biotechnology.2019; 303: 25. CrossRef - Pharmacogenomic Testing: Clinical Evidence and Implementation Challenges
Catriona Hippman, Corey Nislow
Journal of Personalized Medicine.2019; 9(3): 40. CrossRef - Cancer Panel Assay for Precision Oncology Clinic: Results from a 1-Year Study
Dohee Kwon, Binnari Kim, Hyeong Chan Shin, Eun Ji Kim, Sang Yun Ha, Kee-Taek Jang, Seung Tae Kim, Jeeyun Lee, Won Ki Kang, Joon Oh Park, Kyoung-Mee Kim
Translational Oncology.2019; 12(11): 1488. CrossRef - Analytical Evaluation of an NGS Testing Method for Routine Molecular Diagnostics on Melanoma Formalin-Fixed, Paraffin-Embedded Tumor-Derived DNA
Irene Mancini, Lisa Simi, Francesca Salvianti, Francesca Castiglione, Gemma Sonnati, Pamela Pinzani
Diagnostics.2019; 9(3): 117. CrossRef - Benchmark Database for Process Optimization and Quality Control of Clinical Cancer Panel Sequencing
Donghyeong Seong, Jongsuk Chung, Ki-Wook Lee, Sook-Young Kim, Byung-Suk Kim, Jung-Keun Song, Sungwon Jung, Taeseob Lee, Donghyun Park, Byoung-Kee Yi, Woong-Yang Park, Dae-Soon Son
Biotechnology and Bioprocess Engineering.2019; 24(5): 793. CrossRef - Use of the Ion PGM and the GeneReader NGS Systems in Daily Routine Practice for Advanced Lung Adenocarcinoma Patients: A Practical Point of View Reporting a Comparative Study and Assessment of 90 Patients
Simon Heeke, Véronique Hofman, Elodie Long-Mira, Virginie Lespinet, Salomé Lalvée, Olivier Bordone, Camille Ribeyre, Virginie Tanga, Jonathan Benzaquen, Sylvie Leroy, Charlotte Cohen, Jérôme Mouroux, Charles Marquette, Marius Ilié, Paul Hofman
Cancers.2018; 10(4): 88. CrossRef - Use of the Ion AmpliSeq Cancer Hotspot Panel in clinical molecular pathology laboratories for analysis of solid tumours: With emphasis on validation with relevant single molecular pathology tests and the Oncomine Focus Assay
Ahwon Lee, Sung-Hak Lee, Chan Kwon Jung, Gyungsin Park, Kyo Young Lee, Hyun Joo Choi, Ki Ouk Min, Tae Jung Kim, Eun Jung Lee, Youn Soo Lee
Pathology - Research and Practice.2018; 214(5): 713. CrossRef - Recent Advancement of the Molecular Diagnosis in Pediatric Brain Tumor
Jeong-Mo Bae, Jae-Kyung Won, Sung-Hye Park
Journal of Korean Neurosurgical Society.2018; 61(3): 376. CrossRef - The long tail of molecular alterations in non-small cell lung cancer: a single-institution experience of next-generation sequencing in clinical molecular diagnostics
Caterina Fumagalli, Davide Vacirca, Alessandra Rappa, Antonio Passaro, Juliana Guarize, Paola Rafaniello Raviele, Filippo de Marinis, Lorenzo Spaggiari, Chiara Casadio, Giuseppe Viale, Massimo Barberis, Elena Guerini-Rocco
Journal of Clinical Pathology.2018; 71(9): 767. CrossRef - Clinical laboratory utilization management and improved healthcare performance
Christopher Naugler, Deirdre L. Church
Critical Reviews in Clinical Laboratory Sciences.2018; 55(8): 535. CrossRef - Development of HLA-A, -B and -DR Typing Method Using Next-Generation Sequencing
Dong Hee Seo, Jeong Min Lee, Mi Ok Park, Hyun Ju Lee, Seo Yoon Moon, Mijin Oh, So Young Kim, Sang-Heon Lee, Ki-Eun Hyeong, Hae-Jin Hu, Dae-Yeon Cho
The Korean Journal of Blood Transfusion.2018; 29(3): 310. CrossRef - Value-based genomics
Jun Gong, Kathy Pan, Marwan Fakih, Sumanta Pal, Ravi Salgia
Oncotarget.2018; 9(21): 15792. CrossRef
- Tumour purity assessment with deep learning in colorectal cancer and impact on molecular analysis
- Molecular Testing of Lung Cancers
- Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
- J Pathol Transl Med. 2017;51(3):242-254. Published online April 21, 2017
- DOI: https://doi.org/10.4132/jptm.2017.04.10
- 18,031 View
- 616 Download
- 28 Web of Science
- 28 Crossref
-
 Abstract
Abstract
 PDF
PDF - Targeted therapies guided by molecular diagnostics have become a standard treatment of lung cancer. Epidermal growth factor receptor (EGFR) mutations and anaplastic lymphoma kinase (ALK) rearrangements are currently used as the best predictive biomarkers for EGFR tyrosine kinase inhibitors and ALK inhibitors, respectively. Besides EGFR and ALK, the list of druggable genetic alterations has been growing, including ROS1 rearrangements, RET rearrangements, and MET alterations. In this situation, pathologists should carefully manage clinical samples for molecular testing and should do their best to quickly and accurately identify patients who will benefit from precision therapeutics. Here, we grouped molecular biomarkers of lung cancers into three categories—mutations, gene rearrangements, and amplifications—and propose expanded guidelines on molecular testing of lung cancers.
-
Citations
Citations to this article as recorded by- Association between PD-L1 expression with EGFR, ALK, and ROS1 driver oncogene mutations in non-small cell lung cancer
Dülger Onur, Yaylım İlhan, Öz Büge
Indian Journal of Pathology and Microbiology.2025; 68(1): 36. CrossRef - Evidence-based Approach to Transthoracic Needle Biopsy: Procedural Techniques, Risks, and Controversies
Shravan Sridhar, Hannah G. Ahn, Sayedomid Ebrahimzadeh, Felicia Tang, Brett Elicker
RadioGraphics.2025;[Epub] CrossRef - Enhancing Lung Cancer Care in Portugal: Bridging Gaps for Improved Patient Outcomes
Raquel Ramos, Conceição Souto Moura, Mariana Costa, Nuno Jorge Lamas, Renato Correia, Diogo Garcez, José Miguel Pereira, Carlos Sousa, Nuno Vale
Journal of Personalized Medicine.2024; 14(5): 446. CrossRef - Evolution of therapy for ALK-positive lung carcinomas: Application of third-generation ALK inhibitors in real clinical practice
A. F. Nasretdinov, A. V. Sultanbaev, Sh. I. Musin, K. V. Menshikov, R. T. Ayupov, A. A. Izmailov, G. A. Serebrennikov, V. E. Askarov, D. V. Feoktistov
Meditsinskiy sovet = Medical Council.2024; (10): 74. CrossRef - Cost-effectiveness of next-generation sequencing for advanced EGFR/ALK-negative non-small cell lung cancer
Dong-Won Kang, Sun-Kyeong Park, Sokbom Kang, Eui-Kyung Lee
Lung Cancer.2024; 197: 107970. CrossRef - miR-92a-3p regulates cisplatin-induced cancer cell death
Romain Larrue, Sandy Fellah, Nihad Boukrout, Corentin De Sousa, Julie Lemaire, Carolane Leboeuf, Marine Goujon, Michael Perrais, Bernard Mari, Christelle Cauffiez, Nicolas Pottier, Cynthia Van der Hauwaert
Cell Death & Disease.2023;[Epub] CrossRef - Diagnostic Approach of Lung Cancer: A Literature Review
Jesi Hana, Novia Nurul Faizah
Jurnal Respirasi.2023; 9(2): 141. CrossRef - Molecular Pathology of Lung Cancer
James J. Saller, Theresa A. Boyle
Cold Spring Harbor Perspectives in Medicine.2022; 12(3): a037812. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - TM4SF4 and LRRK2 Are Potential Therapeutic Targets in Lung and Breast Cancers through Outlier Analysis
Kyungsoo Jung, Joon-Seok Choi, Beom-Mo Koo, Yu Jin Kim, Ji-Young Song, Minjung Sung, Eun Sol Chang, Ka-Won Noh, Sungbin An, Mi-Sook Lee, Kyoung Song, Hannah Lee, Ryong Nam Kim, Young Kee Shin, Doo-Yi Oh, Yoon-La Choi
Cancer Research and Treatment.2021; 53(1): 9. CrossRef - The promises and challenges of early non‐small cell lung cancer detection: patient perceptions, low‐dose CT screening, bronchoscopy and biomarkers
Lukas Kalinke, Ricky Thakrar, Sam M. Janes
Molecular Oncology.2021; 15(10): 2544. CrossRef - Cost-effectiveness analyses of targeted therapy and immunotherapy for advanced non-small cell lung cancer in the United States: a systematic review
Anthony Yu, Eva Huang, Momoka Abe, Kang An, Sun-Kyeong Park, Chanhyun Park
Expert Review of Pharmacoeconomics & Outcomes Research.2021; 21(3): 381. CrossRef - The expanding capability and clinical relevance of molecular diagnostic technology to identify and evaluate EGFR mutations in advanced/metastatic NSCLC
Parth Shah, Jacob Sands, Nicola Normanno
Lung Cancer.2021; 160: 118. CrossRef - Testing for EGFR Mutations and ALK Rearrangements in Advanced Non-Small-Cell Lung Cancer: Considerations for Countries in Emerging Markets
Mercedes L Dalurzo, Alejandro Avilés-Salas, Fernando Augusto Soares, Yingyong Hou, Yuan Li, Anna Stroganova, Büge Öz, Arif Abdillah, Hui Wan, Yoon-La Choi
OncoTargets and Therapy.2021; Volume 14: 4671. CrossRef - Treatment of Patients With Non–Small-Cell Lung Cancer Harboring Rare Oncogenic Mutations
Melina E. Marmarelis, Corey J. Langer
Clinical Lung Cancer.2020; 21(5): 395. CrossRef - Detection of Targetable Genetic Alterations in Korean Lung Cancer Patients: A Comparison Study of Single-Gene Assays and Targeted Next-Generation Sequencing
Eunhyang Park, Hyo Sup Shim
Cancer Research and Treatment.2020; 52(2): 543. CrossRef - High prevalence of ROS1 gene rearrangement detected by FISH in EGFR and ALK negative lung adenocarcinoma
Yuyin Xu, Heng Chang, Lijing Wu, Xin Zhang, Ling Zhang, Jing Zhang, Yuan Li, Lei Shen, Xiaoli Zhu, Xiaoyan Zhou, Qianming Bai
Experimental and Molecular Pathology.2020; 117: 104548. CrossRef - An All-In-One Transcriptome-Based Assay to Identify Therapy-Guiding Genomic Aberrations in Nonsmall Cell Lung Cancer Patients
Jiacong Wei, Anna A. Rybczynska, Pei Meng, Martijn Terpstra, Ali Saber, Jantine Sietzema, Wim Timens, Ed Schuuring, T. Jeroen N. Hiltermann, Harry. J.M. Groen, Anthonie van der Wekken, Anke van den Berg, Klaas Kok
Cancers.2020; 12(10): 2843. CrossRef - Immunotherapy in EGFR-Mutant and ALK-Positive Lung Cancer
Alexander Gavralidis, Justin F. Gainor
The Cancer Journal.2020; 26(6): 517. CrossRef - Role of Immunocytochemistry in the Cytological Diagnosis of Pulmonary Tumors
Jasna Metovic, Luisella Righi, Luisa Delsedime, Marco Volante, Mauro Papotti
Acta Cytologica.2020; 64(1-2): 16. CrossRef - Molecular Diagnostic Assays and Clinicopathologic Implications of MET Exon 14 Skipping Mutation in Non–small-cell Lung Cancer
Eun Kyung Kim, Kyung A. Kim, Chang Young Lee, Sangwoo Kim, Sunhee Chang, Byoung Chul Cho, Hyo Sup Shim
Clinical Lung Cancer.2019; 20(1): e123. CrossRef - PD‐L1 expression in ROS1‐rearranged non‐small cell lung cancer: A study using simultaneous genotypic screening of EGFR, ALK, and ROS1
Jongmin Lee, Chan Kwon Park, Hyoung‐Kyu Yoon, Young Jo Sa, In Sook Woo, Hyo Rim Kim, Sue Youn Kim, Tae‐Jung Kim
Thoracic Cancer.2019; 10(1): 103. CrossRef - Human Leukocyte Antigen Class I and Programmed Death-Ligand 1 Coexpression Is an Independent Poor Prognostic Factor in Adenocarcinoma of the Lung
Yeon Bi Han, Hyun Jung Kwon, Soo Young Park, Eun-Sun Kim, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2019; 53(2): 86. CrossRef - Molecular testing for advanced non-small cell lung cancer in Malaysia: Consensus statement from the College of Pathologists, Academy of Medicine Malaysia, the Malaysian Thoracic Society, and the Malaysian Oncological Society
Pathmanathan Rajadurai, Phaik Leng Cheah, Soon Hin How, Chong Kin Liam, Muhammad Azrif Ahmad Annuar, Norhayati Omar, Noriah Othman, Nurhayati Mohd Marzuki, Yong Kek Pang, Ros Suzanna Ahmad Bustamam, Lye Mun Tho
Lung Cancer.2019; 136: 65. CrossRef - Somatic mutations and immune checkpoint biomarkers
Brielle A. Parris, Eloise Shaw, Brendan Pang, Richie Soong, Kwun Fong, Ross A. Soo
Respirology.2019; 24(3): 215. CrossRef - Adverse Event Management in Patients with BRAF V600E-Mutant Non-Small Cell Lung Cancer Treated with Dabrafenib plus Trametinib
Anna Chalmers, Laura Cannon, Wallace Akerley
The Oncologist.2019; 24(7): 963. CrossRef - Genetic and clinicopathologic characteristics of lung adenocarcinoma with tumor spread through air spaces
Jae Seok Lee, Eun Kyung Kim, Moonsik Kim, Hyo Sup Shim
Lung Cancer.2018; 123: 121. CrossRef
- Association between PD-L1 expression with EGFR, ALK, and ROS1 driver oncogene mutations in non-small cell lung cancer
- Pathology Reporting of Thyroid Core Needle Biopsy: A Proposal of the Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group
- Chan Kwon Jung, Hye Sook Min, Hyo Jin Park, Dong Eun Song, Jang Hee Kim, So Yeon Park, Hyunju Yoo, Mi Kyung Shin, Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group
- J Pathol Transl Med. 2015;49(4):288-299. Published online June 17, 2015
- DOI: https://doi.org/10.4132/jptm.2015.06.04
- 20,864 View
- 492 Download
- 108 Web of Science
- 103 Crossref
-
 Abstract
Abstract
 PDF
PDF - In recent years throughout Korea, the use of ultrasound-guided core needle biopsy (CNB) has become common for the preoperative diagnosis of thyroid nodules. However, there is no consensus on the pathology reporting system for thyroid CNB. The Korean Endocrine Pathology Thyroid Core Needle Biopsy Study Group held a conference on thyroid CNB pathology and developed guidelines through contributions from the participants. This article discusses the outcome of the discussions that led to a consensus on the pathology reporting of thyroid CNB.
-
Citations
Citations to this article as recorded by- Predictive US findings for differentiating between malignant and benign thyroid nodules: Doppler and microvascular imaging according to the TI-RADS and pathologic subtypes of malignancy
Younghee Yim, Hye Shin Ahn, Min Ji Hong, Hyun Jeong Park, Sung Bin Park
Ultrasonography.2026; 45(1): 38. CrossRef - Risk Stratification of Thyroid Nodules Diagnosed as Follicular Neoplasm on Core Needle Biopsy
Byeong-Joo Noh, Won Jun Kim, Jin Yub Kim, Ha Young Kim, Jong Cheol Lee, Myoung Sook Shim, Yong Jin Song, Kwang Hyun Yoon, In-Hye Jung, Hyo Sang Lee, Wooyul Paik, Dong Gyu Na
Endocrinology and Metabolism.2025; 40(4): 610. CrossRef - Diagnostic performances of five US risk stratification systems for malignancy in focal [18F]FDG-PET/CT thyroid incidentalomas
Chae Young Shin, Hye Shin Ahn, Dong Gyu Na, Hyo Sang Lee, Eon-Woo Shin
European Radiology.2025; 35(12): 7701. CrossRef - Malignancy risk in AUS thyroid lesions: comparison between FNA and CNB with implications for NIFTP diagnosis
Yeseul Kim, Jae Ho Shin, You-Na Sung, Dawon Park, Harim Oh, Hyo Seon Ryu, Kyeong Jin Kim, Hyun Joo Kim, Sin Gon Kim, Hoon Yub Kim, Kwang Yoon Jung, Seung-Kuk Baek, Sangjeong Ahn
Frontiers in Endocrinology.2025;[Epub] CrossRef - The Diagnostic Role of Repeated Biopsy of Thyroid Nodules with Atypia of Undetermined Significance with Architectural Atypia on Core-Needle Biopsy
Hye Hyeon Moon, Sae Rom Chung, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee, Jung Hwan Baek
Endocrinology and Metabolism.2024; 39(2): 300. CrossRef - Core needle biopsy for thyroid nodules assessment-a new horizon?
David D Dolidze, Serghei Covantsev, Grigorii M Chechenin, Natalia V Pichugina, Anastasia V Bedina, Anna Bumbu
World Journal of Clinical Oncology.2024; 15(5): 580. CrossRef - Ultrasonographic features and diagnostic accuracy of FNA and CNB in secondary thyroid malignancies: A retrospective study
Zhen Xia, Xiaochen Huang, Ting Zhang, Zhigang Gao, Xiuliang Tang, Wei Zhang, Qing Miao
Heliyon.2024; 10(16): e36305. CrossRef - Current role of interventional radiology in thyroid nodules
Onur Taydas, Erbil Arik, Omer Faruk Sevinc, Ahmet Burak Kara, Mustafa Ozdemir, Hasret Cengiz, Zulfu Bayhan, Mehmet Halil Ozturk
Frontiers in Endocrinology.2024;[Epub] CrossRef - A simplified four-tier classification for thyroid core needle biopsy
M. Paja, J. L. Del Cura, R. Zabala, I. Korta, Mª T. Gutiérrez, A. Expósito, A. Ugalde
Journal of Endocrinological Investigation.2024; 48(4): 895. CrossRef - Follow-up of benign thyroid nodules confirmed by ultrasound-guided core needle biopsy after inconclusive cytology on fine-needle aspiration biopsy
Yoon Ji Hwang, Hye Ryoung Koo, Jeong Seon Park
Ultrasonography.2023; 42(1): 121. CrossRef - Subcategorization of intermediate suspicion thyroid nodules based on suspicious ultrasonographic findings
Haejung Kim, Jung Hee Shin, Ka Eun Kim, Myoung Kyoung Kim, Jiyun Oh, Soo Yeon Hahn
Ultrasonography.2023; 42(2): 307. CrossRef - Preoperative Risk Stratification of Follicular-patterned Thyroid Lesions on Core Needle Biopsy by Histologic Subtyping and RAS Variant-specific Immunohistochemistry
Meejeong Kim, Sora Jeon, Chan Kwon Jung
Endocrine Pathology.2023; 34(2): 247. CrossRef - Cytological and Ultrasound Features of Thyroid Nodules Correlate With Histotypes and Variants of Thyroid Carcinoma
Daniele Sgrò, Alessandro Brancatella, Giuseppe Greco, Liborio Torregrossa, Paolo Piaggi, Nicola Viola, Teresa Rago, Fulvio Basolo, Riccardo Giannini, Gabriele Materazzi, Rossella Elisei, Ferruccio Santini, Francesco Latrofa
The Journal of Clinical Endocrinology & Metabolism.2023; 108(11): e1186. CrossRef - Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
Chan Kwon Jung
Journal of Pathology and Translational Medicine.2023; 57(4): 208. CrossRef - Contrast Enhancement Ultrasound Improves Diagnostic Accuracy for Thyroid Nodules: A Prospective Multicenter Study
Jianming Li, Jianping Dou, Huarong Li, Fan Xiao, Jie Yu, Mingxing Xie, Ping Zhou, Lei Liang, Guiming Zhou, Ying Che, Cun Liu, Zhibin Cong, Fangyi Liu, Zhiyu Han, Ping Liang
Journal of the Endocrine Society.2023;[Epub] CrossRef - Core needle biopsy and ultrasonography are superior to fine needle aspiration in the management of follicular variant papillary thyroid carcinomas
Ji-Ye Kim, Sunhee Chang, Ah-Young Kwon, Eun Young Park, Tae Hyuk Kim, Sangjoon Choi, Minju Lee, Young Lyun Oh
Endocrine.2022; 75(2): 437. CrossRef - Fine Needle Aspiration Cytology vs. Core Needle Biopsy for Thyroid Nodules: A Prospective, Experimental Study Using Surgical Specimen
Hyuk Kwon, Jandee Lee, Soon Won Hong, Hyeong Ju Kwon, Jin Young Kwak, Jung Hyun Yoon
Journal of the Korean Society of Radiology.2022; 83(3): 645. CrossRef - Diagnostic efficacy, performance and safety of side-cut core needle biopsy for thyroid nodules: comparison of automated and semi-automated biopsy needles
Ji Yeon Park, Seong Yoon Yi, Soo Heui Baek, Yu Hyun Lee, Heon-Ju Kwon, Hee Jin Park
Endocrine.2022; 76(2): 341. CrossRef - Approach to Bethesda system category III thyroid nodules according to US-risk stratification
Jieun Kim, Jung Hee Shin, Young Lyun Oh, Soo Yeon Hahn, Ko Woon Park
Endocrine Journal.2022; 69(1): 67. CrossRef - Quantitative analysis of vascularity for thyroid nodules on ultrasound using superb microvascular imaging
Min Ji Hong, Hye Shin Ahn, Su Min Ha, Hyun Jeong Park, Jiyun Oh
Medicine.2022; 101(5): e28725. CrossRef - Diagnostic Performance of Thyroid Core Needle Biopsy Using the Revised Reporting System: Comparison with Fine Needle Aspiration Cytology
Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, So Lyung Jung, Chan Kwon Jung
Endocrinology and Metabolism.2022; 37(1): 159. CrossRef - A Matched-Pair Analysis of Nuclear Morphologic Features Between Core Needle Biopsy and Surgical Specimen in Thyroid Tumors Using a Deep Learning Model
Faridul Haq, Andrey Bychkov, Chan Kwon Jung
Endocrine Pathology.2022; 33(4): 472. CrossRef - Role of echogenic foci in ultrasonographic risk stratification of thyroid nodules: Echogenic focus scoring in the American College of Radiology Thyroid Imaging Reporting and Data System
Renxu Li, Zhenwei Liang, Xiangyu Wang, Luzeng Chen
Frontiers in Oncology.2022;[Epub] CrossRef - Ultrasonographic characteristics of medullary thyroid carcinoma according to nodule size: application of the Korean Thyroid Imaging Reporting and Data System and American Thyroid Association guidelines
Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Ko Woon Park
Acta Radiologica.2021; 62(4): 474. CrossRef - Malignancy risk of thyroid nodules with nonshadowing echogenic foci
Yu-Mee Sohn, Dong Gyu Na, Wooyul Paik, Hye Yun Gwon, Byeong-Joo Noh
Ultrasonography.2021; 40(1): 115. CrossRef - Assessing the diagnostic performance of thyroid biopsy with recommendations for appropriate interpretation
Su Min Ha, Jung Hwan Baek, Dong Gyu Na, Chan-Kwon Jung, Chong Hyun Suh, Young Kee Shong, Tae Yon Sung, Dong Eun Song, Jeong Hyun Lee
Ultrasonography.2021; 40(2): 228. CrossRef - Usage and Diagnostic Yield of Fine-Needle Aspiration Cytology and Core Needle Biopsy in Thyroid Nodules: A Systematic Review and Meta-Analysis of Literature Published by Korean Authors
Soon-Hyun Ahn
Clinical and Experimental Otorhinolaryngology.2021; 14(1): 116. CrossRef - Comparison of the Efficacy and Safety of the American Thyroid Association Guidelines and American College of Radiology TI-RADS
Jinghua Liu, Yajun Guo, Jiangxi Xiao, Luzeng Chen, Zhenwei Liang
Endocrine Practice.2021; 27(7): 661. CrossRef - Malignancy Rate of Bethesda Class III Thyroid Nodules Based on the Presence of Chronic Lymphocytic Thyroiditis in Surgical Patients
Yoon Young Cho, Yun Jae Chung, Hee Sung Kim
Frontiers in Endocrinology.2021;[Epub] CrossRef - Efficacy of Differential Diagnosis of Thyroid Nodules by Shear Wave Elastography—the Stiffness Map
Myung Hi Yoo, Hye Jeong Kim, In Ho Choi, Suyeon Park, Sumi Yun, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh
Journal of the Endocrine Society.2021;[Epub] CrossRef - The relationship of thyroid nodule size on malignancy risk according to histological type of thyroid cancer
Sae Rom Chung, Jung Hwan Baek, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee
Acta Radiologica.2020; 61(5): 620. CrossRef - Concordance of Three International Guidelines for Thyroid Nodules Classified by Ultrasonography and Diagnostic Performance of Biopsy Criteria
Younghee Yim, Dong Gyu Na, Eun Ju Ha, Jung Hwan Baek, Jin Yong Sung, Ji-hoon Kim, Won-Jin Moon
Korean Journal of Radiology.2020; 21(1): 108. CrossRef - 2019 Practice guidelines for thyroid core needle biopsy: a report of the Clinical Practice Guidelines Development Committee of the Korean Thyroid Association
Chan Kwon Jung, Jung Hwan Baek, Dong Gyu Na, Young Lyun Oh, Ka Hee Yi, Ho-Cheol Kang
Journal of Pathology and Translational Medicine.2020; 54(1): 64. CrossRef - Core-Needle Biopsy Does Not Show Superior Diagnostic Performance to Fine-Needle Aspiration for Diagnosing Thyroid Nodules
Ilah Shin, Eun-Kyung Kim, Hee Jung Moon, Jung Hyun Yoon, Vivian Youngjean Park, Si Eun Lee, Hye Sun Lee, Jin Young Kwak
Yonsei Medical Journal.2020; 61(2): 161. CrossRef - Ultrasound‐guided fine‐needle aspiration or core needle biopsy for diagnosing follicular thyroid carcinoma?
Ko Woon Park, Jung Hee Shin, Soo Yeon Hahn, Young Lyun Oh, Sun Wook Kim, Tae Hyuk Kim, Jae Hoon Chung
Clinical Endocrinology.2020; 92(5): 468. CrossRef - Distribution and malignancy risk of six categories of the pathology reporting system for thyroid core-needle biopsy in 1,216 consecutive thyroid nodules
Hye Min Son, Ji-hoon Kim, Soo Chin Kim, Roh-Eul Yoo, Jeong Mo Bae, Hyobin Seo, Dong Gyu Na
Ultrasonography.2020; 39(2): 159. CrossRef - CT features of thyroid nodules with isolated macrocalcifications detected by ultrasonography
Wooyul Paik, Dong Gyu Na, Hye Yun Gwon, Jinna Kim
Ultrasonography.2020; 39(2): 130. CrossRef - Contribution of cytologic examination to diagnosis of poorly differentiated thyroid carcinoma
Na Rae Kim, Jae Yeon Seok, Yoo Seung Chung, Joon Hyop Lee, Dong Hae Chung
Journal of Pathology and Translational Medicine.2020; 54(2): 171. CrossRef - Comparison Between Fine Needle Aspiration and Core Needle Biopsy for the Diagnosis of Thyroid Nodules: Effective Indications According to US Findings
Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Ko Woon Park, Yaeji Lim
Scientific Reports.2020;[Epub] CrossRef - Thyroid Nodules with Isolated Macrocalcifications: Malignancy Risk of Isolated Macrocalcifications and Postoperative Risk Stratification of Malignant Tumors Manifesting as Isolated Macrocalcifications
Hye Yun Gwon, Dong Gyu Na, Byeong-Joo Noh, Wooyul Paik, So Jin Yoon, Soo-Jung Choi, Dong Rock Shin
Korean Journal of Radiology.2020; 21(5): 605. CrossRef - Diagnostic Efficacy and Safety of Core Needle Biopsy as a First-Line Diagnostic Method for Thyroid Nodules: A Prospective Cohort Study
Min Ji Hong, Dong Gyu Na, Hunkyung Lee
Thyroid.2020; 30(8): 1141. CrossRef - Re: The 2019 core-needle biopsy practice guidelines
Ji-hoon Kim
Ultrasonography.2020; 39(3): 313. CrossRef - Cytopathologic criteria and size should be considered in comparison of fine-needle aspiration vs. core-needle biopsy for thyroid nodules: results based on large surgical series
Jung Hyun Yoon, Hye Sun Lee, Eun-Kyung Kim, Hee Jung Moon, Vivian Youngjean Park, Jin Young Kwak
Endocrine.2020; 70(3): 558. CrossRef - Preoperative diagnostic categories of fine needle aspiration cytology for histologically proven thyroid follicular adenoma and carcinoma, and Hurthle cell adenoma and carcinoma: Analysis of cause of under- or misdiagnoses
Hee Young Na, Jae Hoon Moon, June Young Choi, Hyeong Won Yu, Woo-Jin Jeong, Yeo Koon Kim, Ji-Young Choe, So Yeon Park, Paula Soares
PLOS ONE.2020; 15(11): e0241597. CrossRef - The Role of Core Needle Biopsy for the Evaluation of Thyroid Nodules with Suspicious Ultrasound Features
Sae Rom Chung, Jung Hwan Baek, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee
Korean Journal of Radiology.2019; 20(1): 158. CrossRef - Pathological diagnosis of thyroid nodules based on core needle biopsies: comparative study between core needle biopsies and resected specimens in 578 cases
Yan Xiong, Limin Yan, Lin Nong, Yalin Zheng, Ting Li
Diagnostic Pathology.2019;[Epub] CrossRef - The Current Histologic Classification of Thyroid Cancer
Sylvia L. Asa
Endocrinology and Metabolism Clinics of North America.2019; 48(1): 1. CrossRef - Core-needle biopsy in thyroid nodules: performance, accuracy, and complications
Miguel Paja, Jose Luis del Cura, Rosa Zabala, Igone Korta, Aitziber Ugalde, José I. López
European Radiology.2019; 29(9): 4889. CrossRef - Ultrasound‐guided needle biopsy of large thyroid nodules: Core needle biopsy yields more reliable results than fine needle aspiration
Hyeon Jin Lee, Young Joong Kim, Hye Yeon Han, Jae Young Seo, Cheol Mog Hwang, KeumWon Kim
Journal of Clinical Ultrasound.2019; 47(5): 255. CrossRef - Tumor Volume Doubling Time in Active Surveillance of Papillary Thyroid Carcinoma
Hye-Seon Oh, Hyemi Kwon, Eyun Song, Min Ji Jeon, Tae Yong Kim, Jeong Hyun Lee, Won Bae Kim, Young Kee Shong, Ki-Wook Chung, Jung Hwan Baek, Won Gu Kim
Thyroid.2019; 29(5): 642. CrossRef - Role of Immunohistochemistry in Fine Needle Aspiration and Core Needle Biopsy of Thyroid Nodules
Seulki Song, Hyojin Kim, Soon-Hyun Ahn
Clinical and Experimental Otorhinolaryngology.2019; 12(2): 224. CrossRef - Echogenic foci in thyroid nodules: diagnostic performance with combination of TIRADS and echogenic foci
Su Min Ha, Yun Jae Chung, Hye Shin Ahn, Jung Hwan Baek, Sung Bin Park
BMC Medical Imaging.2019;[Epub] CrossRef - Risk of Malignancy According to the Sub-classification of Atypia of Undetermined Significance and Suspicious Follicular Neoplasm Categories in Thyroid Core Needle Biopsies
Sae Rom Chung, Jung Hwan Baek, Jeong Hyun Lee, Yu-Mi Lee, Tae-Yon Sung, Ki-Wook Chung, Suck Joon Hong, Min Ji Jeon, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Won Gu Kim, Dong Eun Song
Endocrine Pathology.2019; 30(2): 146. CrossRef - Thyroid core needle biopsy: patients’ pain and satisfaction compared to fine needle aspiration
Hyo Jin Kim, Yeo Koon Kim, Jae Hoon Moon, June Young Choi, Sang Il Choi
Endocrine.2019; 65(2): 365. CrossRef - Does Radiofrequency Ablation Induce Neoplastic Changes in Benign Thyroid Nodules: A Preliminary Study
Su Min Ha, Jun Young Shin, Jung Hwan Baek, Dong Eun Song, Sae Rom Chung, Young Jun Choi, Jeong Hyun Lee
Endocrinology and Metabolism.2019; 34(2): 169. CrossRef - Differential Diagnosis of Thyroid Follicular Neoplasm from Nodular Hyperplasia by Shear Wave Elastography
Myung Hi Yoo, Hye Jeong Kim, In Ho Choi, Ji-Oh Mok, Hyeong Kyu Park, Dong Won Byun, Kyoil Suh
Soonchunhyang Medical Science.2019; 25(1): 10. CrossRef - Ultrasound-Guided Core Needle Biopsy Techniques for Intermediate or Low Suspicion Thyroid Nodules: Which Method is Effective for Diagnosis?
Soo Yeon Hahn, Jung Hee Shin, Young Lyun Oh, Ko Woon Park
Korean Journal of Radiology.2019; 20(10): 1454. CrossRef - Preoperative Diagnostic Categories of Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features in Thyroid Core Needle Biopsy and Its Impact on Risk of Malignancy
Hee Young Na, Ji Won Woo, Jae Hoon Moon, June Young Choi, Woo-Jin Jeong, Yeo Koon Kim, Ji-Young Choe, So Yeon Park
Endocrine Pathology.2019; 30(4): 329. CrossRef - Utility of a formatted pathologic reporting system in thyroid core needle biopsy: A validation study of 1998 consecutive cases
Ji‐Young Choe, Yoonjin Kwak, Mimi Kim, Yul Ri Chung, Hyun Jeong Kim, Yeo Koon Kim, So Yeon Park
Clinical Endocrinology.2018; 88(1): 96. CrossRef - Nuclear features of papillary thyroid carcinoma: Comparison of Core needle biopsy and thyroidectomy specimens
Jae Yeon Seok, Jungsuk An, Hyun Yee Cho, Younghye Kim, Seung Yeon Ha
Annals of Diagnostic Pathology.2018; 32: 35. CrossRef - Prevention of total thyroidectomy in noninvasive follicular thyroid neoplasm with papillary‐like nuclear features (NIFTP) based on combined interpretation of ultrasonographic and cytopathologic results
Sung‐Hye You, Kyu Eun Lee, Roh‐Eul Yoo, Hye Jeong Choi, Kyeong Cheon Jung, Jae‐Kyung Won, Koung Mi Kang, Tae Jin Yoon, Seung Hong Choi, Chul‐Ho Sohn, Ji‐hoon Kim
Clinical Endocrinology.2018; 88(1): 114. CrossRef - Statement and Recommendations on Interventional Ultrasound as a Thyroid Diagnostic and Treatment Procedure
Christoph F. Dietrich, Thomas Müller, Jörg Bojunga, Yi Dong, Giovanni Mauri, Maija Radzina, Manjiri Dighe, Xin-Wu Cui, Frank Grünwald, Andreas Schuler, Andre Ignee, Huedayi Korkusuz
Ultrasound in Medicine & Biology.2018; 44(1): 14. CrossRef - Core needle biopsy of thyroid nodules: outcomes and safety from a large single-center single-operator study
Jooae Choe, Jung Hwan Baek, Hye Sun Park, Young Jun Choi, Jeong Hyun Lee
Acta Radiologica.2018; 59(8): 924. CrossRef - Improvement of diagnostic performance of pathologists by reducing the number of pathologists responsible for thyroid fine needle aspiration cytology: An institutional experience
Jae Yeon Seok, Jungsuk An, Hyun Yee Cho
Diagnostic Cytopathology.2018; 46(7): 561. CrossRef - Comparison of Immunohistochemistry and Direct Sanger Sequencing for Detection of theBRAFV600EMutation in Thyroid Neoplasm
Hye-Seon Oh, Hyemi Kwon, Suyeon Park, Mijin Kim, Min Ji Jeon, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Jene Choi, Won Gu Kim, Dong Eun Song
Endocrinology and Metabolism.2018; 33(1): 62. CrossRef - Comparison of the Diagnostic Efficacy of Ultrasound‐Guided Core Needle Biopsy With 18‐ Versus 20‐Gauge Needles for Thyroid Nodules
Hye Shin Ahn, Mirinae Seo, Su Min Ha, Hee Sung Kim
Journal of Ultrasound in Medicine.2018; 37(11): 2565. CrossRef - Impact of Nodule Size on Malignancy Risk Differs according to the Ultrasonography Pattern of Thyroid Nodules
Min Ji Hong, Dong Gyu Na, Jung Hwan Baek, Jin Yong Sung, Ji-Hoon Kim
Korean Journal of Radiology.2018; 19(3): 534. CrossRef - Web‐based thyroid imaging reporting and data system: Malignancy risk of atypia of undetermined significance or follicular lesion of undetermined significance thyroid nodules calculated by a combination of ultrasonography features and biopsy results
Young Jun Choi, Jung Hwan Baek, Jung Hee Shin, Woo Hyun Shim, Seon‐Ok Kim, Won‐Hong Lee, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jeong Hyun Lee
Head & Neck.2018; 40(9): 1917. CrossRef - Thyroid Incidentalomas Detected on18F-Fluorodeoxyglucose Positron Emission Tomography with Computed Tomography: Malignant Risk Stratification and Management Plan
Sae Rom Chung, Young Jun Choi, Chong Hyun Suh, Hwa Jung Kim, Jong Jin Lee, Won Gu Kim, Tae Yon Sung, Yu-mi Lee, Dong Eun Song, Jeong Hyun Lee, Jung Hwan Baek
Thyroid.2018; 28(6): 762. CrossRef - The role of core needle biopsy in the diagnosis of initially detected thyroid nodules: a systematic review and meta-analysis
Sae Rom Chung, Chong Hyun Suh, Jung Hwan Baek, Young Jun Choi, Jeong Hyun Lee
European Radiology.2018; 28(11): 4909. CrossRef - The History of Korean Thyroid Pathology
Soon Won Hong, Chan Kwon Jung
International Journal of Thyroidology.2018; 11(1): 15. CrossRef - Ultrasonographic Echogenicity and Histopathologic Correlation of Thyroid Nodules in Core Needle Biopsy Specimens
Ji-hoon Kim, Dong Gyu Na, Hunkyung Lee
Korean Journal of Radiology.2018; 19(4): 673. CrossRef - Evaluation of Modified Core-Needle Biopsy in the Diagnosis of Thyroid Nodules
Soomin Ahn, Sejin Jung, Ji-Ye Kim, Jung Hee Shin, Soo Yeon Hahn, Young Lyun Oh
Korean Journal of Radiology.2018; 19(4): 656. CrossRef - Role of core needle biopsy as a first-line diagnostic tool for thyroid nodules: a retrospective cohort study
Min Ji Hong, Dong Gyu Na, Soo Jin Kim, Dae Sik Kim
Ultrasonography.2018; 37(3): 244. CrossRef - Active Surveillance of Low-Risk Papillary Thyroid Microcarcinoma: A Multi-Center Cohort Study in Korea
Hye-Seon Oh, Jeonghoon Ha, Hye In Kim, Tae Hyuk Kim, Won Gu Kim, Dong-Jun Lim, Tae Yong Kim, Sun Wook Kim, Won Bae Kim, Young Kee Shong, Jae Hoon Chung, Jung Hwan Baek
Thyroid.2018; 28(12): 1587. CrossRef - Risk of malignancy according to sub‐classification of the atypia of undetermined significance or follicular lesion of undetermined significance (AUS/FLUS) category in the Bethesda system for reporting thyroid cytopathology
S. J. Kim, J. Roh, J. H. Baek, S. J. Hong, Y. K. Shong, W. B. Kim, D. E. Song
Cytopathology.2017; 28(1): 65. CrossRef - Fine-needle aspiration versus core needle biopsy for diagnosis of thyroid malignancy and neoplasm: a matched cohort study
Soo-Yeon Kim, Hye Sun Lee, Jieun Moon, Eun-Kyung Kim, Hee Jung Moon, Jung Hyun Yoon, Jin Young Kwak
European Radiology.2017; 27(2): 801. CrossRef - Follicular variant of papillary thyroid carcinoma: comparison of ultrasound-guided core needle biopsy and ultrasound-guided fine needle aspiration in a multicentre study
Soo Yeon Hahn, Jung Hee Shin, Hyun Kyung Lim, So Lyung Jung
Clinical Endocrinology.2017; 86(1): 113. CrossRef - Core‐needle biopsy versus repeat fine‐needle aspiration for thyroid nodules initially read as atypia/follicular lesion of undetermined significance
Young Jun Choi, Jung Hwan Baek, Chong Hyun Suh, Woo Hyun Shim, Boseul Jeong, Jae Kyun Kim, Dong Eun Song, Tae Yong Kim, Ki‐Wook Chung, Jeong Hyun Lee
Head & Neck.2017; 39(2): 361. CrossRef - Preoperative differentiation between noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP) and non-NIFTP
Soo Yeon Hahn, Jung Hee Shin, Hyun Kyung Lim, So Lyung Jung, Young Lyun Oh, In Ho Choi, Chan Kwon Jung
Clinical Endocrinology.2017; 86(3): 444. CrossRef - Core Needle Biopsy of the Thyroid: 2016 Consensus Statement and Recommendations from Korean Society of Thyroid Radiology
Dong Gyu Na, Jung Hwan Baek, So Lyung Jung, Ji-hoon Kim, Jin Yong Sung, Kyu Sun Kim, Jeong Hyun Lee, Jung Hee Shin, Yoon Jung Choi, Eun Ju Ha, Hyun Kyung Lim, Soo Jin Kim, Soo Yeon Hahn, Kwang Hwi Lee, Young Jun Choi, Inyoung Youn, Young Joong Kim, Hye Sh
Korean Journal of Radiology.2017; 18(1): 217. CrossRef - First-Line Use of Core Needle Biopsy for High-Yield Preliminary Diagnosis of Thyroid Nodules
H.C. Kim, Y.J. Kim, H.Y. Han, J.M. Yi, J.H. Baek, S.Y. Park, J.Y. Seo, K.W. Kim
American Journal of Neuroradiology.2017; 38(2): 357. CrossRef - Ultrasound-Pathology Discordant Nodules on Core-Needle Biopsy: Malignancy Risk and Management Strategy
Sae Rom Chung, Jung Hwan Baek, Hye Sun Park, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee
Thyroid.2017; 27(5): 707. CrossRef - Current status of core needle biopsy of the thyroid
Jung Hwan Baek
Ultrasonography.2017; 36(2): 83. CrossRef - Cytology-Ultrasonography Risk-Stratification Scoring System Based on Fine-Needle Aspiration Cytology and the Korean-Thyroid Imaging Reporting and Data System
Min Ji Hong, Dong Gyu Na, Jung Hwan Baek, Jin Yong Sung, Ji-Hoon Kim
Thyroid.2017; 27(7): 953. CrossRef - Preoperative clinicopathological characteristics of patients with solitary encapsulated follicular variants of papillary thyroid carcinomas
Hyemi Kwon, Min Ji Jeon, Jong Ho Yoon, Suck Joon Hong, Jeong Hyun Lee, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Won Gu Kim, Dong Eun Song
Journal of Surgical Oncology.2017; 116(6): 746. CrossRef - Active Surveillance for Patients With Papillary Thyroid Microcarcinoma: A Single Center’s Experience in Korea
Hyemi Kwon, Hye-Seon Oh, Mijin Kim, Suyeon Park, Min Ji Jeon, Won Gu Kim, Won Bae Kim, Young Kee Shong, Dong Eun Song, Jung Hwan Baek, Ki-Wook Chung, Tae Yong Kim
The Journal of Clinical Endocrinology & Metabolism.2017; 102(6): 1917. CrossRef - Comparison of Consecutive Results from Fine Needle Aspiration and Core Needle Biopsy in Thyroid Nodules
Soon-Hyun Ahn, So-Yeon Park, Sang Il Choi
Endocrine Pathology.2017; 28(4): 332. CrossRef - Efficacy and safety of core-needle biopsy in initially detected thyroid nodules via propensity score analysis
Chong Hyun Suh, Jung Hwan Baek, Young Jun Choi, Tae Yong Kim, Tae Yon Sung, Dong Eun Song, Jeong Hyun Lee
Scientific Reports.2017;[Epub] CrossRef - Comparison of Core-Needle Biopsy and Fine-Needle Aspiration for Evaluating Thyroid Incidentalomas Detected by 18F-Fluorodeoxyglucose Positron Emission Tomography/Computed Tomography: A Propensity Score Analysis
Chong Hyun Suh, Young Jun Choi, Jong Jin Lee, Woo Hyun Shim, Jung Hwan Baek, Han Cheol Chung, Young Kee Shong, Dong Eun Song, Tae Yon Sung, Jeong Hyun Lee
Thyroid.2017; 27(10): 1258. CrossRef - Thyroid Fine-Needle Aspiration Cytology Practice in Korea
Yoon Jin Cha, Ju Yeon Pyo, SoonWon Hong, Jae Yeon Seok, Kyung-Ju Kim, Jee-Young Han, Jeong Mo Bae, Hyeong Ju Kwon, Yeejeong Kim, Kyueng-Whan Min, Soonae Oak, Sunhee Chang
Journal of Pathology and Translational Medicine.2017; 51(6): 521. CrossRef - Recent Advances in Core Needle Biopsy for Thyroid Nodules
Chan Kwon Jung, Jung Hwan Baek
Endocrinology and Metabolism.2017; 32(4): 407. CrossRef - Core-needle biopsy for the preoperative diagnosis of follicular neoplasm in thyroid nodule screening: A validation study
Sung Hak Lee, Gyeong Sin Park, So Lyung Jung, Min-Hee Kim, Ja Seong Bae, Dong Jun Lim, Chan Kwon Jung
Pathology - Research and Practice.2016; 212(1): 44. CrossRef - The Role of Core-Needle Biopsy as a First-Line Diagnostic Tool for Initially Detected Thyroid Nodules
Chong Hyun Suh, Jung Hwan Baek, Jeong Hyun Lee, Young Jun Choi, Jae Kyun Kim, Tae-Yon Sung, Jong Ho Yoon, Young Kee Shong
Thyroid.2016; 26(3): 395. CrossRef - Thyroid nodules with minimal cystic changes have a low risk of malignancy
Dong Gyu Na, Ji-hoon Kim, Dea Sik Kim, Soo Jin Kim
Ultrasonography.2016; 35(2): 153. CrossRef - Thyroid nodules with isolated macrocalcification: malignancy risk and diagnostic efficacy of fine-needle aspiration and core needle biopsy
Dong Gyu Na, Dae Sik Kim, Soo Jin Kim, Jae Wook Ryoo, So Lyung Jung
Ultrasonography.2016; 35(3): 212. CrossRef - Thyroid Imaging Reporting and Data System Risk Stratification of Thyroid Nodules: Categorization Based on Solidity and Echogenicity
Dong Gyu Na, Jung Hwan Baek, Jin Yong Sung, Ji-Hoon Kim, Jae Kyun Kim, Young Jun Choi, Hyobin Seo
Thyroid.2016; 26(4): 562. CrossRef - Fine‐needle aspiration and core needle biopsy: An update on 2 common minimally invasive tissue sampling modalities
Paul A. VanderLaan
Cancer Cytopathology.2016; 124(12): 862. CrossRef - The role of core-needle biopsy in the diagnosis of thyroid malignancy in 4580 patients with 4746 thyroid nodules: a systematic review and meta-analysis
Chong Hyun Suh, Jung Hwan Baek, Jeong Hyun Lee, Young Jun Choi, Kyung Won Kim, Jayoun Lee, Ki-Wook Chung, Young Kee Shong
Endocrine.2016; 54(2): 315. CrossRef - The Role of Core-Needle Biopsy for Thyroid Nodules with Initially Nondiagnostic Fine-Needle Aspiration Results: A Systematic Review and Meta-Analysis
Chong Hyun Suh, Jung Hwan Baek, Kyung Won Kim, Tae Yon Sung, Tae Yong Kim, Dong Eun Song, Young Jun Choi, Jeong Hyun Lee
Endocrine Practice.2016; 22(6): 679. CrossRef - Should Core Needle Biopsy be Used in the Evaluation of Thyroid Nodules?
Beril Guler, Tugce Kiran, Dilek Sema Arici, Erhan Aysan, Fatma Cavide Sonmez
Endocrine Pathology.2016; 27(4): 352. CrossRef - A Multicenter Prospective Validation Study for the Korean Thyroid Imaging Reporting and Data System in Patients with Thyroid Nodules
Eun Ju Ha, Won-Jin Moon, Dong Gyu Na, Young Hen Lee, Nami Choi, Soo Jin Kim, Jae Kyun Kim
Korean Journal of Radiology.2016; 17(5): 811. CrossRef - Impact of Reclassification on Thyroid Nodules with Architectural Atypia: From Non-Invasive Encapsulated Follicular Variant Papillary Thyroid Carcinomas to Non-Invasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features
Min Ji Jeon, Dong Eun Song, Chan Kwon Jung, Won Gu Kim, Hyemi Kwon, Yu-Mi Lee, Tae-Yon Sung, Jong Ho Yoon, Ki-Wook Chung, Suck Joon Hong, Jung Hwan Baek, Jeong Hyun Lee, Tae Yong Kim, Young Kee Shong, Won Bae Kim, Rafael Rosell
PLOS ONE.2016; 11(12): e0167756. CrossRef
- Predictive US findings for differentiating between malignant and benign thyroid nodules: Doppler and microvascular imaging according to the TI-RADS and pathologic subtypes of malignancy
- Guideline Recommendations for Testing of
ALK Gene Rearrangement in Lung Cancer: A Proposal of the Korean Cardiopulmonary Pathology Study Group - Hyojin Kim, Hyo Sup Shim, Lucia Kim, Tae-Jung Kim, Kun Young Kwon, Geon Kook Lee, Jin-Haeng Chung
- Korean J Pathol. 2014;48(1):1-9. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.1
- 16,128 View
- 130 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Rearrangement of anaplastic lymphoma kinase (
ALK ) gene is the best predictor of response to crizotinib, an ALK tyrosine kinase inhibitor. However, the prevalence of theALK fusion is low, so accurate patient identification is crucial for successful treatment using ALK inhibitors. Furthermore, most patients with lung cancer present with advanced-stage disease at the time of diagnosis, so it is important for pathologists to detectALK -rearranged patients while effectively maximizing small biopsy or cytology specimens. In this review, we propose a guideline recommendation for ALK testing approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.-
Citations
Citations to this article as recorded by- Molecular Characteristics of Radon Associated Lung Cancer Highlights MET Alterations
Gabriele Gamerith, Marcel Kloppenburg, Finn Mildner, Arno Amann, Sabine Merkelbach-Bruse, Carina Heydt, Janna Siemanowski, Reinhard Buettner, Michael Fiegl, Claudia Manzl, Georg Pall
Cancers.2022; 14(20): 5113. CrossRef -
ALK Translocation in ALK-Positive Mesenchymal Tumors: Diagnostic and Therapeutic Insights
Minsun Jung, Kyung Chul Moon, Jeongmo Bae, Tae Min Kim, Miso Kim, Yoon Kyung Jeon, Cheol Lee
Archives of Pathology & Laboratory Medicine.2022; 146(12): 1460. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Testing for EGFR Mutations and ALK Rearrangements in Advanced Non-Small-Cell Lung Cancer: Considerations for Countries in Emerging Markets
Mercedes L Dalurzo, Alejandro Avilés-Salas, Fernando Augusto Soares, Yingyong Hou, Yuan Li, Anna Stroganova, Büge Öz, Arif Abdillah, Hui Wan, Yoon-La Choi
OncoTargets and Therapy.2021; Volume 14: 4671. CrossRef - Molecular testing for advanced non-small cell lung cancer in Malaysia: Consensus statement from the College of Pathologists, Academy of Medicine Malaysia, the Malaysian Thoracic Society, and the Malaysian Oncological Society
Pathmanathan Rajadurai, Phaik Leng Cheah, Soon Hin How, Chong Kin Liam, Muhammad Azrif Ahmad Annuar, Norhayati Omar, Noriah Othman, Nurhayati Mohd Marzuki, Yong Kek Pang, Ros Suzanna Ahmad Bustamam, Lye Mun Tho
Lung Cancer.2019; 136: 65. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H. Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benj
Journal of Thoracic Oncology.2018; 13(3): 323. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H. Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benj
The Journal of Molecular Diagnostics.2018; 20(2): 129. CrossRef - Updated Molecular Testing Guideline for the Selection of Lung Cancer Patients for Treatment With Targeted Tyrosine Kinase Inhibitors: Guideline From the College of American Pathologists, the International Association for the Study of Lung Cancer, and the
Neal I. Lindeman, Philip T. Cagle, Dara L. Aisner, Maria E. Arcila, Mary Beth Beasley, Eric H Bernicker, Carol Colasacco, Sanja Dacic, Fred R. Hirsch, Keith Kerr, David J. Kwiatkowski, Marc Ladanyi, Jan A. Nowak, Lynette Sholl, Robyn Temple-Smolkin, Benja
Archives of Pathology & Laboratory Medicine.2018; 142(3): 321. CrossRef - 5′/ 3′ imbalance strategy to detect ALK fusion genes in circulating tumor RNA from patients with non-small cell lung cancer
Yongqing Tong, Zhijun Zhao, Bei Liu, Anyu Bao, Hongyun Zheng, Jian Gu, Mary McGrath, Ying Xia, Bihua Tan, Chunhua Song, Yan Li
Journal of Experimental & Clinical Cancer Research.2018;[Epub] CrossRef - Molecular testing and treatment patterns for patients with advanced non-small cell lung cancer: PIvOTAL observational study
Dae Ho Lee, Ming-Sound Tsao, Karl-Otto Kambartel, Hiroshi Isobe, Ming-Shyan Huang, Carlos H. Barrios, Adnan Khattak, Filippo de Marinis, Smita Kothari, Ashwini Arunachalam, Xiting Cao, Thomas Burke, Amparo Valladares, Javier de Castro, Aamir Ahmad
PLOS ONE.2018; 13(8): e0202865. CrossRef - Microfluidics-based immunofluorescence for fast staining of ALK in lung adenocarcinoma
Saška Brajkovic, Benjamin Pelz, Maria-Giuseppina Procopio, Anne-Laure Leblond, Grégoire Repond, Ariane Schaub-Clerigué, Diego G Dupouy, Alex Soltermann
Diagnostic Pathology.2018;[Epub] CrossRef - Expanded Circulating Tumor Cells from a Patient with ALK- Positive Lung Cancer Present with EML4-ALK Rearrangement Along with Resistance Mutation and Enable Drug Sensitivity Testing: A Case Study
Zhuo Zhang, Hiroe Shiratsuchi, Nallasivam Palanisamy, Sunitha Nagrath, Nithya Ramnath
Journal of Thoracic Oncology.2017; 12(2): 397. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Novel ALK fusion partners in lung cancer
Aglaya G. Iyevleva, Grigory A. Raskin, Vladislav I. Tiurin, Anna P. Sokolenko, Natalia V. Mitiushkina, Svetlana N. Aleksakhina, Aigul R. Garifullina, Tatiana N. Strelkova, Valery O. Merkulov, Alexandr O. Ivantsov, Ekatherina Sh. Kuligina, Kazimir M. Pozha
Cancer Letters.2015; 362(1): 116. CrossRef - Strategic management of transthoracic needle aspirates for histological subtyping and EGFR testing in patients with peripheral lung cancer: An institutional experience
Choonhee Son, Eun‐Ju Kang, Mee Sook Roh
Diagnostic Cytopathology.2015; 43(7): 532. CrossRef - Current and future molecular diagnostics in non-small-cell lung cancer
Chun Man Li, Wing Ying Chu, Di Lun Wong, Hin Fung Tsang, Nancy Bo Yin Tsui, Charles Ming Lok Chan, Vivian Wei Wen Xue, Parco Ming Fai Siu, Benjamin Yat Ming Yung, Lawrence Wing Chi Chan, Sze Chuen Cesar Wong
Expert Review of Molecular Diagnostics.2015; 15(8): 1061. CrossRef - Role of biopsy sampling for diagnosis of early and progressed hepatocellular carcinoma
Haeryoung Kim, Young Nyun Park
Best Practice & Research Clinical Gastroenterology.2014; 28(5): 813. CrossRef - Molecular Pathology of Lung Cancer: Current Status and Future Directions
Mee Sook Roh
Tuberculosis and Respiratory Diseases.2014; 77(2): 49. CrossRef - Epidermal growth factor receptor mutations and anaplastic lymphoma kinase rearrangements in lung cancer with nodular ground-glass opacity
Sung-Jun Ko, Yeon Joo Lee, Jong Sun Park, Young-Jae Cho, Ho Il Yoon, Jin-Haeng Chung, Tae Jung Kim, Kyung Won Lee, Kwhanmien Kim, Sanghoon Jheon, Hyojin Kim, Jae Ho Lee, Choon-Taek Lee
BMC Cancer.2014;[Epub] CrossRef
- Molecular Characteristics of Radon Associated Lung Cancer Highlights MET Alterations
- Guideline Recommendations for
EGFR Mutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group - Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
- Korean J Pathol. 2013;47(2):100-106. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.100
- 12,523 View
- 100 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Mutations of the epidermal growth factor receptor (
EGFR ) are the strongest predictive factor for response to EGFR tyrosine kinase inhibitors (TKIs), such as gefitinib and erlotinib. EGFR TKIs are approved in Korea as a first-line treatment for lung cancer patients with mutatedEGFR . Rapid and accurateEGFR mutation testing is essential for patient selection and establishing targeted therapies with EGFR TKIs. Thus, a standard set of guideline recommendations forEGFR mutation testing suitable for the Korean medical community is necessary. In this article, we propose a set of guideline recommendations forEGFR mutation testing that was discussed and approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.-
Citations
Citations to this article as recorded by- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
Cheng-Yu Chang, Chia-Chun Tu, Shian-Ren Lin, Chih-Hao Fang, Po-Wei Tseng, Wan-En Liao, Li-Yun Huang, Shiu-Lan Wang, Wan-Yu Lai, Yee Chao, Yen-Ling Chiu, Jan-Mou Lee
Diseases.2025; 13(12): 406. CrossRef - Favorable Conditions for the Detection of EGFR T790M Mutation Using Plasma Sample in Patients with Non-Small-Cell Lung Cancer
Insu Kim, Hee Yun Seol, Soo Han Kim, Mi-Hyun Kim, Min Ki Lee, Jung Seop Eom
Cancers.2023; 15(5): 1445. CrossRef - Novel Targets, Novel Treatments: The Changing Landscape of Non-Small Cell Lung Cancer
Dorine de Jong, Jeeban P. Das, Hong Ma, Jacienta Pailey Valiplackal, Conor Prendergast, Tina Roa, Brian Braumuller, Aileen Deng, Laurent Dercle, Randy Yeh, Mary M. Salvatore, Kathleen M. Capaccione
Cancers.2023; 15(10): 2855. CrossRef - Coordination games in cancer
Péter Bayer, Robert A. Gatenby, Patricia H. McDonald, Derek R. Duckett, Kateřina Staňková, Joel S. Brown, Jun Tanimoto
PLOS ONE.2022; 17(1): e0261578. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Primary HHV-8 (-) Effusion-Based Non-Germinal Center B Cell Diffuse Large B Cell Lymphoma Successfully Treated with Standard Anthracycline-Based Chemoimmunotherapy
Justin J Kuhlman, Muhamad Alhaj Moustafa, Liuyan Jiang, Han W Tun
Journal of Blood Medicine.2021; Volume 12: 833. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Strategic management of transthoracic needle aspirates for histological subtyping and EGFR testing in patients with peripheral lung cancer: An institutional experience
Choonhee Son, Eun‐Ju Kang, Mee Sook Roh
Diagnostic Cytopathology.2015; 43(7): 532. CrossRef - Ultrasonography-Guided Core Biopsy of Supraclavicular Lymph Nodes for Diagnosis of Metastasis and Identification of Epidermal Growth Factor Receptor (EGFR) Mutation in Advanced Lung Cancer
Jooae Choe, Mi Young Kim, Jung Hwan Baek, Chang-Min Choi, Hwa Jung Kim
Medicine.2015; 94(29): e1209. CrossRef - Reliable EGFR mutation testing in ultrasound-guided supraclavicular lymph node fine-needle aspirates: a cohort study with diagnostic performance analysis
Amir Awwad, Sandeep Tiwari, Vishakha Sovani, David R Baldwin, Maruti Kumaran
BMJ Open Respiratory Research.2015; 2(1): e000075. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Molecular Pathology of Lung Cancer: Current Status and Future Directions
Mee Sook Roh
Tuberculosis and Respiratory Diseases.2014; 77(2): 49. CrossRef
- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
- Guidelines for Pathologic Study of Gastric Cancer.
- Korean J Pathol. 1992;26(2):154-163.
- 2,138 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF - Gastric cancer is the most common malignant neoplasm among Koreans, and the pathologists's daily diagnostic competency on gastric cancer at any hospital setting plays a critical implication not only in the quality of clinical service but also to the determination of patient's prognosis. Thus, adoption of a unified assessment system based on comprehensive understanding of pathologic features together with their active participation has been crucially demanded. Nevertheless, a considerable difference in handling procedures and diagnostic approach on gastric cancer among institutions apparently resulted in an extreme difficulty in exchange of clinicopathologic informations and in the nationwide survey. It is, therefore, essential and be the first step to develop a practical but scientific and reproducible classification of gastric cancer with its diverse gross and histologic findings. Based on the following basic principles, the Subcommittee on Gastric Cancer under the Gastrointestinal Study Group of the Korean Society of Pathologists has been requested to develop the guidelines of future pathologic study of gastric cancer to meet the above needs and be efficiently used with ease among the society members. 1) The prerequisite for pathologic classification of gastric cancer starts with consistency in handling of the resected stomach before its further examination. Thus, the guideline shall limits its scope only with the minimum agreement. 2) The classification should be simple and practical so that all pathologists can use with ease and with high reproducibility. 3) All the gross and microscopic findings which have been considered to be the prognosis-related factors should be included in every pathologic procedures to help future information exchange among pathologists and clinicians and to provide a meaningful role in determination of patient's prognosis. 4) The classification should be interchangeable and stand with compatibility among WHO and other internationally accepted classifications. 5) The guideline accepts in part the staging system of American Joint Commitee on Cancer, classification of early gastric cancer proposed by the Japanese Society of Gastrointestinal Endoscopy, and the General Rules of Stomach Cancer Study by Japanese Research Society of Gastric Cancer, until otherwise developed and accepted by the Korean Society of Pathologists. 6) The guideline should not interfere with each institution-based special study. The details of the handling procedures of the resected stomach cancer, its gross and histologic classifications and descriptive methods of prognostic factors are supplemented with illustrations.

 E-submission
E-submission



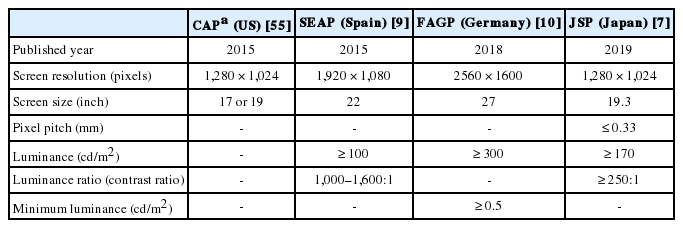
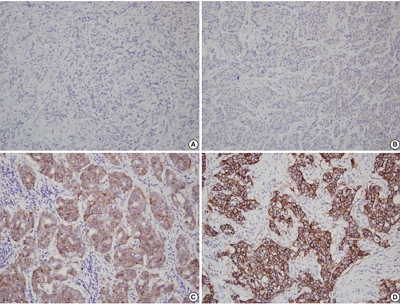
 First
First Prev
Prev



