Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(3); 2013 > Article
-
Case Study
Multicystic Biliary Hamartoma of the Liver - Ji Soo Song, Sang Jae Noh1, Baik Hwan Cho2, Woo Sung Moon1
-
Korean Journal of Pathology 2013;47(3):275-278.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.275
Published online: June 25, 2013
Department of Radiology, Research Institute of Clinical Medicine and Research Institute for Endocrine Sciences, Chonbuk National University Medical School, Jeonju, Korea.
1Department of Pathology, Research Institute of Clinical Medicine and Research Institute for Endocrine Sciences, Chonbuk National University Medical School, Jeonju, Korea.
2Department of Surgery, Research Institute of Clinical Medicine and Research Institute for Endocrine Sciences, Chonbuk National University Medical School, Jeonju, Korea.
- Corresponding Author: Woo Sung Moon, M.D. Department of Pathology, Chonbuk National University Medical School, 567 Baekje-daero, Deokjin-gu, Jeonju 561-756, Korea. Tel: +82-63-270-3086, Fax: +82-63-270-3135, mws@chonbuk.ac.kr
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- Multicystic biliary hamartoma (MCBH) is a very rare hamartomatous cystic nodule of the liver, which has recently been described as a new entity of a hepatic nodular lesion. We report a unique case of MCBH with a review of the literatures. A hepatic multicystic mass of segment 3 was detected in a 52-year-old male by abdominal computed tomography, and resection of this lesion was performed. Macroscopic examination revealed a 2.7×2.0 cm nodular mass with a multicystic honeycomb cut surface. Histologically, this lesion consisted of multiple dilated cystic ducts lined by biliary type epithelial cells, periductal glands and connective tissue, which included small amounts of hepatic parenchyma and blood vessels. Recognition of this unusual lesion is essential to avoid confusion with other cystic tumors of the liver, and to learn more about its natural history and response to treatment.
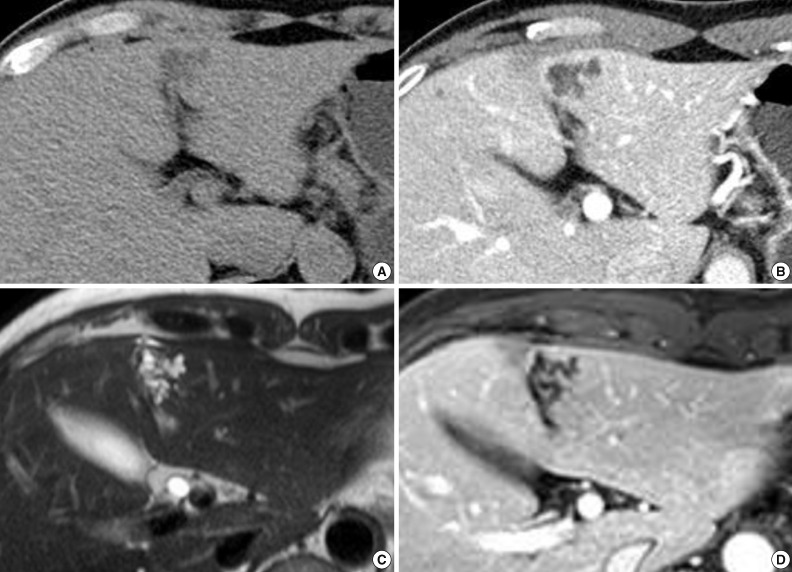
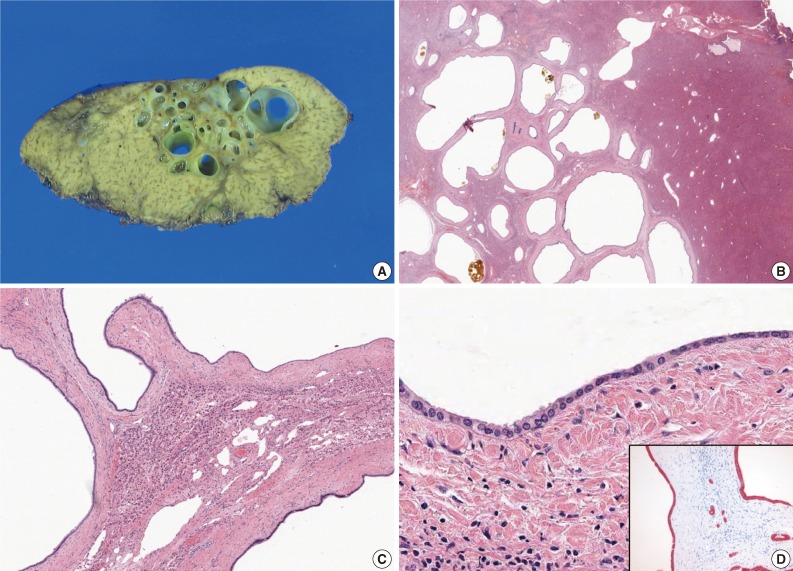
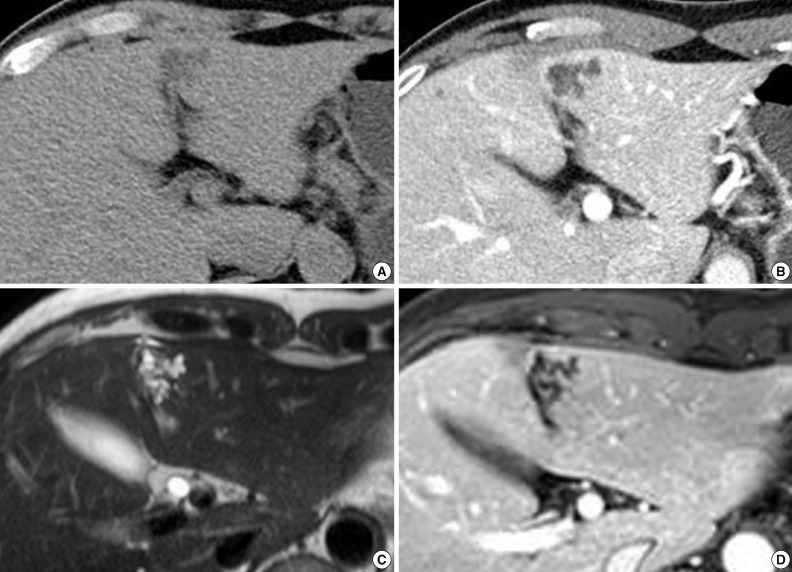
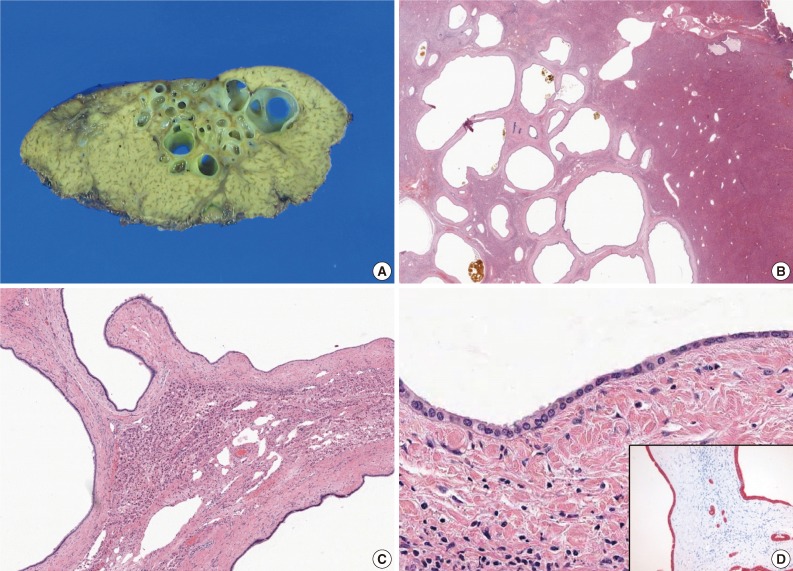
- A 52-year-old male patient was referred to our hospital on February 12, 2012 with a complaint of abdominal discomfort. The physical examination of the patient was unremarkable. The serum levels for alanine aminotransferase (21 IU/L; normal range, 5 to 35 IU/L) and aspartate aminotransferase (23 IU/L; normal range, 12 to 33 IU/L) were normal. Tumor markers (alpha-fetoprotein, carcinoembryonic antigen, and carbohydrate antigen 19-9) were within normal limits. Serological tests for hepatitis B and hepatitis C were negative. All other parameters were normal. An abdominal computed tomography (CT) scan demonstrated an irregularly-shaped low-density lesion measuring 2.7 cm in diameter in segment 3 of the left lobe just beneath the hepatic capsule (Fig. 1A). This lesion was slightly enhanced after contrast medium injection and revealed a multicystic appearance in the portal phase (Fig. 1B). Abdominal magnetic resonance imaging (MRI) more clearly depicted the multicystic nodule in segment 3 of the liver. On T2-weighted MRI, conglomerated multiple cystic nodules with a high signal intensity were seen (Fig. 1C). Thin septae and the wall of the lesion were enhanced on contrast-enhanced, T1-weighted MRI (Fig. 1D). Surgical exploration revealed a 2.7×2.0 cm, relatively well-demarcated nodular mass. The cut surface had a multicystic honeycomb appearance that was composed of a number of cystically dilated ductal structures embedded in the fibrous tissue (Fig. 2A). Histologically, this lesion consisted of dilated cystic ducts, periductal glands and connective tissue, which included small amounts of hepatic parenchyma and blood vessels. Bile materials were observed in some of the cystic ducts (Fig. 2B, C). The ducts were lined by a monolayer of low columnar or cuboidal epithelial cells (Fig. 2D). There was no ovarian-like stroma. No mitotic figures were observed in the epithelial cells, and there was no evidence of pleomorphism or nuclear atypia suggesting malignant tumor. Immunohistochemical stainings for mucin core protein (Muc) 1, Muc2, Muc5Ac, Muc6, and biliary type keratin (K) 7 and, K19 were performed. Similar to previous findings,1,3 the duct-lining epithelial cells were diffusely positive for K7, K19 and showed focal Muc1 expression, whereas they were negative for Muc2, Muc5Ac, and Muc6 (Fig. 2D). On the basis of these histologic and immunohistochemical findings, a final diagnosis of MCBH was made.
CASE REPORT
- MCBH is a rare cystic disease of the liver.1 Since the first description of MCBH in 2006, there have only been a eight published cases worldwide.1-4 These publications are shown in Table 1. The reported mean age at the presentation of the disease was 55±12 years (n=9), with a range from 30-70 years. The disease is twice more common in males than in females, with a male-to-female ratio of 6:3. The majority of patients are asymptomatic, and the cyst is found incidentally and most commonly in segment 3 in the left lobe and in segment 6 in the right lobe just beneath the hepatic capsule. The average size of the six lesions for which data are available was 3.35±1.15 cm (n=6) in the greatest dimension (range, 1.8 to 5 cm). The exact size was not reported in three patients. The pathogenesis of MCBH is not clear. Zen et al.1 proposed that MCBHs might be related to developmental abnormalities of the biliary tract or embryonic foregut.
- On ultrasonography, the most consistent findings in MCBHs are a conglomerate of hypoechoic irregular masses with hyperechoic cystic walls.2 CT usually displays these lesions at as low density with enhancing septae, as in our case. On MRI, MCBHs are hypointense on T1-weighted imaging. T2-weighted imaging reveals a multicystic, honeycomb-like lesion with bright, high signal intensity. Although most MCBHs have some typical imaging features, radiology alone is non-diagnostic. The radiologic features of biliary mucinous cystic neoplasm, echinococcosis, and hepatic lymphangioma resemble those of MCBH.2
- The key histological features of MCBH include the following: location around the hepatic capsule close to the fissure of the falciform ligament; protrusion from the liver; composition of ductal structures, periductal glands, and fibrous connective tissue; presence of bile-like materials in the ducts; and positivity for biliary type keratins on the cyst lining-epithelium.1 All these features, except for liver protrusion, were observed in the present case; five of the eight previously reported MCBHs also did not protrude from the liver.1-4 Previous reports additionally showed that MCBH occurs not only on the liver's surface but also in the intrahepatic portion.3 Therefore, we ultimately diagnosed this lesion as MCBH. Histologically, the differential diagnoses of MCBH included ciliated hepatic foregut cyst (CHFC), Caroli's disease, mucinous cystic neoplasm, and von Meyenburg's complex (biliary microhamartoma). The histological features of CHFC are the presence of a four-layered cyst wall, which consists of a mostly inner lining of pseudostratified ciliated columnar epithelium followed by a layer of loose subepithelial connective tissue, a smooth muscle layer and an outer layer of dense fibrous tissue.5 No characteristic pathological features of CHFC, such as ciliated cells and a smooth muscle layer were observed in the present case. Caroli's disease is characterized by segmental or multiple dilatations of the intrahepatic ducts. Ductal structures in Caroli's disease are cystically dilated preexisting bile ducts, whereas ducts in MCBH derive from hamartomaous or abnormal ducts.6 Moreover, Caroli's disease is often accompanied by congenital hepatic fibrosis. Mucinous cystic neoplasm should always be included in the differential diagnosis, because mucinous cystic neoplasm is a true neoplasm with the potential for progression to biliary cystadenocarcinoma. The presence of ovarian-like stroma in addition to mucinous lining epithelium in the wall of the cyst defines the mucinous cystic neoplasm.7 We excluded mucinous cystic neoplasm because there was no ovarian-like stroma or mucinous cells, which are necessary for the diagnosis of mucinous cystic neoplasm. Biliary microhamartomas appear as a focal disorderly collection of bile ducts and ductules surrounded by abundant fibrous stoma. They are usually multiple and located adjacent to a portal region.8 Contrary to the relatively larger size of MCBH (1.8-5.0 cm),1-4 biliary microhamartomas usually range from 2 to 5 mm in diameter.8
- The clinical course of MCBH is benign.1-4 After three months of follow-up, the patient is in good health without any evidence of recurrence. Because only a small number of cases have been documented in the literature, it is essential to be able to recognize MCBH to learn more about its natural history and response to treatment.
DISCUSSION
Acknowledgments
Acknowledgments
- 1. Zen Y, Terahata S, Miyayama S, et al. Multicystic biliary hamartoma: a hitherto undescribed lesion. Hum Pathol 2006; 37: 339-344. PubMed
- 2. Ryu Y, Matsui O, Zen Y, et al. Multicystic biliary hamartoma: imaging findings in four cases. Abdom Imaging 2010; 35: 543-547. ArticlePubMedPDF
- 3. Kai K, Takahashi T, Miyoshi A, Yasui T, Tokunaga O, Miyazaki K. Intrahepatic multicystic biliary hamartoma: report of a case. Hepatol Res 2008; 38: 629-634. ArticlePubMed
- 4. Kobayashi A, Takahashi S, Hasebe T, et al. Solitary bile duct hamartoma of the liver. Scand J Gastroenterol 2005; 40: 1378-1381. ArticlePubMed
- 5. Yang JD, Moon WS. Ciliated hepatic foregut cyst. Korean J Hepatol 2012; 18: 98-100. ArticlePubMedPMC
- 6. Yonem O, Bayraktar Y. Clinical characteristics of Caroli's disease. World J Gastroenterol 2007; 13: 1930-1933. ArticlePubMedPMC
- 7. Tsui WM, Adsay NV, Crawford JM, Hruban R, Kloppel G, Wee A. Mucinous cystic neoplasms of the liver. In: Bosman FT, Carneiro F, Hruban RH, Theise ND, eds. WHO classification of tumours of the digestive system. 4th ed. Lyon: IARC Press, 2010; 236-238.
- 8. Yeh MM. Benign and malignant tumors of bile ducts. In: Saxena R, ed. Practical hepatic pathology: a diagnostic approach. Philadelphia: Saunders-Elsevier, 2011; 504-505.
REFERENCES
| Case No. | Author | Age/Sex | Location | Size (cm) | Clinical symptoms | Treatments |
|---|---|---|---|---|---|---|
| 1 | Zen et al. [1] | 59/M | Segment 4 | 4.2 | Abdominal pain | Left hepatectomy |
| 2 | Zen et al. [1] | 70/F | Segment 3 | 1.8 | Liver dysfunction | Segmentectomy |
| 3 | Zen et al. [1] | 69/F | Segment 3 | 2.8 | Elevation of liver enzyme | Segmentectomy |
| 4 | Kai et al. [3] | 55/M | Segment 6 | 5.0 | Incidental | Partial resection |
| 5 | Ryu et al. [2] | 45/M | Segment 7 | 2.0-3.5 (case nos. 5-7) | Incidental | Partial resection |
| 6 | Ryu et al. [2] | 58/M | Segment 3 | - | Incidental | Partial resection |
| 7 | Ryu et al. [2] | 55/F | Segment 6/7 | - | Incidental | Partial resection |
| 8 | Kobayashi et al. [4] | 30/M | Segment 6 | 3.6 | Incidental | Partial resection |
| Present case | 52/M | Segment 3 | 2.7 | Abdominal discomfort | Partial resection |
Figure & Data
References
Citations

- Multicystic biliary hamartoma with long-term gradual enlargement treated by laparoscopic partial hepatectomy
Satoshi Nishiwada, Tetsuya Tanaka, Yuki Kirihataya, Takeshi Takei, Tomomi Sadamitsu, Masato Takano, Masayoshi Sawai, Atsushi Yoshimura
Clinical Journal of Gastroenterology.2025; 18(3): 527. CrossRef - Technical Considerations in EEG Source Imaging
Benjamin H. Brinkmann
Journal of Clinical Neurophysiology.2024; 41(1): 2. CrossRef - A Case of Multicystic Biliary Hamartoma with a Marked Peribiliary Gland Component Successfully Treated by Purely Laparoscopic Anatomical Liver Resection
Keita Kai, Takao Ide, Tomokazu Tanaka, Kumpei Yukimoto, Hiroyuki Irie, Hirokazu Noshiro, Shinichi Aishima
Journal of Gastrointestinal Cancer.2023; 54(3): 996. CrossRef - Characteristics of multicystic biliary hamartoma: A case report
Jia Lian, Lixia Sun, Yankai Yang, Jun Li, Ye Zhang, Guiqiu Liu, Weijuan Hu
Frontiers in Surgery.2023;[Epub] CrossRef - Recurrent sepsis in a patient with biliary hamartomas
Maria Beatriz Santos, Magda Ponta Garça, Bárbara Vieira, Paulo Ávila, Alexandra Freitas
European Journal of Case Reports in Internal Medicine.2023;[Epub] CrossRef - Hamartoma multiquístico de vías biliares
Victoria Carmona, Iago Justo, Yolanda Rodríguez-Gil, Alberto Marcacuzco, Carmelo Loinaz, Carlos Jiménez
Cirugía Española.2022; 100(12): 800. CrossRef - Multicystic Biliary Hamartoma With Xanthogranulomatous Inflammation on 18F-FDG PET/CT
Nahomi Shono, Yoichi Otomi, Hideki Otsuka, Takayoshi Shinya, Masafumi Harada
Clinical Nuclear Medicine.2022; 47(10): 882. CrossRef - Intrahepatic multicystic biliary hamartoma: A case report
Chen-Yu Wang, Fu-Yang Shi, Wei-Feng Huang, Yan Tang, Ting Li, Guo-Lin He
World Journal of Clinical Cases.2022; 10(26): 9361. CrossRef - A Case of Multicystic Biliary Hamartoma Treated with Left Medial Sectionectomy
Naomi KUROKI, Tomoaki TANAKA, Takanobu SUGASE, Syoji TANIGUCHI, Takashi GOTO, Rintaro KOGA, Takumi KIWAKI, Hiroyuki TANAKA
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2022; 83(2): 395. CrossRef - Multicystic biliary hamartoma
Victoria Carmona, Iago Justo, Yolanda Rodríguez-Gil, Alberto Marcacuzco, Carmelo Loinaz, Carlos Jiménez
Cirugía Española (English Edition).2022; 100(12): 800. CrossRef - Case Report: Incidentally Discovered a Rare Cystic Lesion of Liver: Multicystic Biliary Hamartoma
Wentao Mu, Peng Su, Shanglei Ning
Pathology and Oncology Research.2021;[Epub] CrossRef - Bile Duct Hamartoma Mimicking Liver Metastasis in Suspected Porcelain Gallbladder: a Case Report
Gautham Krishnamurthy, Harjeet Singh, Sravya Deepika Ganti, Ganga Ram Verma
Journal of Gastrointestinal Cancer.2019; 50(4): 1022. CrossRef - A variant of multicystic biliary hamartoma presenting as an intrahepatic cystic neoplasm
Tetsuro Tominaga, Takafumi Abo, Naoe Kinoshita, Tomonori Murakami, Yasunori Sato, Yasuni Nakanuma, Kenich Harada, Junichi Masuda, Takeshi Nagayasu, Atsushi Nanashima
Clinical Journal of Gastroenterology.2015; 8(3): 162. CrossRef - Hamartoma biliar multiquístico intrahepático: presentación de un caso clínico
María Jezabel Fernández-Carrión, Ricardo Robles Campos, Asunción López Conesa, Roberto Brusadín, Pascual Parrilla Paricio
Cirugía Española.2015; 93(9): e103. CrossRef - Intrahepatic Multicystic Biliary Hamartoma: Presentation of a Case Report
María Jezabel Fernández-Carrión, Ricardo Robles Campos, Asunción López Conesa, Roberto Brusadín, Pascual Parrilla Paricio
Cirugía Española (English Edition).2015; 93(9): e103. CrossRef - Multicystic biliary hamartoma: A report of a rare entity and a review of the literature
Rachel E. Beard, Eric U. Yee, Koenraad J. Mortele, Khalid Khwaja
International Journal of Surgery Case Reports.2014; 5(12): 919. CrossRef - Multicystic biliary hamartoma mimicking intrahepatic cholangiocarcinoma: report of a case
Tomoaki Yoh, Ryuji Okamura, Hiroyuki Nakayama, Xue Lin, Yuya Nakamura, Tatsushi Kato
Clinical Journal of Gastroenterology.2014; 7(5): 418. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


Fig. 1
Fig. 2
| Case No. | Author | Age/Sex | Location | Size (cm) | Clinical symptoms | Treatments |
|---|---|---|---|---|---|---|
| 1 | Zen et al. [1] | 59/M | Segment 4 | 4.2 | Abdominal pain | Left hepatectomy |
| 2 | Zen et al. [1] | 70/F | Segment 3 | 1.8 | Liver dysfunction | Segmentectomy |
| 3 | Zen et al. [1] | 69/F | Segment 3 | 2.8 | Elevation of liver enzyme | Segmentectomy |
| 4 | Kai et al. [3] | 55/M | Segment 6 | 5.0 | Incidental | Partial resection |
| 5 | Ryu et al. [2] | 45/M | Segment 7 | 2.0-3.5 (case nos. 5-7) | Incidental | Partial resection |
| 6 | Ryu et al. [2] | 58/M | Segment 3 | - | Incidental | Partial resection |
| 7 | Ryu et al. [2] | 55/F | Segment 6/7 | - | Incidental | Partial resection |
| 8 | Kobayashi et al. [4] | 30/M | Segment 6 | 3.6 | Incidental | Partial resection |
| Present case | 52/M | Segment 3 | 2.7 | Abdominal discomfort | Partial resection |
M, male; F, female.

 E-submission
E-submission