Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(3); 2013 > Article
-
Case Study
A Case of Multifocal Papillary Thyroid Carcinoma Consisting of One Encapsulated Follicular Variant withBRAF K601E Mutation and Three Conventional Types withBRAF V600E Mutation - Wook Youn Kim, Young Sin Ko, Tae Sook Hwang, Hye Seung Han, So Dug Lim, Wan Seop Kim, Seo Young Oh1
-
Korean Journal of Pathology 2013;47(3):293-298.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.293
Published online: June 25, 2013
Department of Pathology, Konkuk University School of Medicine, Seoul, Korea.
1Department of Pathology, Konkuk University Medical Center, Seoul, Korea.
- Corresponding Author: Tae Sook Hwang, M.D. Department of Pathology, Konkuk University School of Medicine, 120-1 Neungdong-ro, Gwangjin-gu, Seoul 143-729, Korea. Tel: +82-2-2030-5641, Fax: +82-2-2030-5629, tshwang@kuh.ac.kr
• Received: June 26, 2012 • Revised: September 27, 2012 • Accepted: October 4, 2012
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- BRAF K601E Mutation in Oncocytic Carcinoma of the Thyroid: A Case Report and Literature Review
Antonio Matrone, Fabrizia Citro, Carla Gambale, Alessandro Prete, Elisa Minaldi, Raffaele Ciampi, Teresa Ramone, Gabriele Materazzi, Liborio Torregrossa, Rossella Elisei
Journal of Clinical Medicine.2023; 12(22): 6970. CrossRef - Case of aggressive metastatic follicular variant papillary thyroid carcinoma with BRAF K601E and BCORL1 mutations
Doaa Attia, Alexander Lurie, Qihui Zhai, Thomas Mesko, Robert Smallridge
BMJ Case Reports.2020; 13(6): e234208. CrossRef - BRAF gene: From human cancers to developmental syndromes
Muhammad Ramzan Manwar Hussain, Mukhtiar Baig, Hussein Sheik Ali Mohamoud, Zaheer Ulhaq, Daniel C. Hoessli, Ghaidaa Siraj Khogeer, Ranem Radwan Al-Sayed, Jumana Yousuf Al-Aama
Saudi Journal of Biological Sciences.2015; 22(4): 359. CrossRef - Clinical significance of BRAF V600E mutation in 154 patients with thyroid nodules
LINGYING YU, LIZHEN MA, QIAOFENG TU, YI ZHANG, YUEMING CHEN, DAOJUN YU, SHAOYU YANG
Oncology Letters.2015; 9(6): 2633. CrossRef - Clinicopathological Features of Rare BRAF Mutations in Korean Thyroid Cancer Patients
Uiju Cho, Woo Jin Oh, Ja Seong Bae, Sohee Lee, Young Sub Lee, Gyeong Sin Park, Youn Soo Lee, Chan Kwon Jung
Journal of Korean Medical Science.2014; 29(8): 1054. CrossRef - Recurrent Thyroid Papillary Carcinoma in Children Under Ten Years Old: Report of Two Cases and Literature Review
Byeong-Joo Noh, Ji-Youn Sung, Youn-Wha Kim, Yong-Koo Park
Korean Journal of Pathology.2014; 48(4): 297. CrossRef - Anaplastic Transformation of Papillary Thyroid Carcinoma in a Young Man: A Case Study with Immunohistochemical andBRAFAnalysis
Ji Hye Park, Hyeong Ju Kwon, Cheong Soo Park, SoonWon Hong
Korean Journal of Pathology.2014; 48(3): 234. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
A Case of Multifocal Papillary Thyroid Carcinoma Consisting of One Encapsulated Follicular Variant with BRAF K601E Mutation and Three Conventional Types with BRAF V600E Mutation



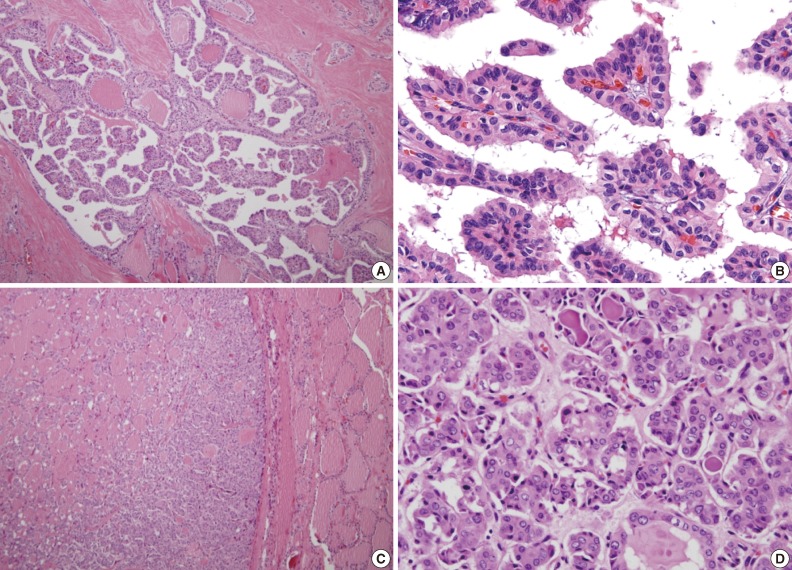
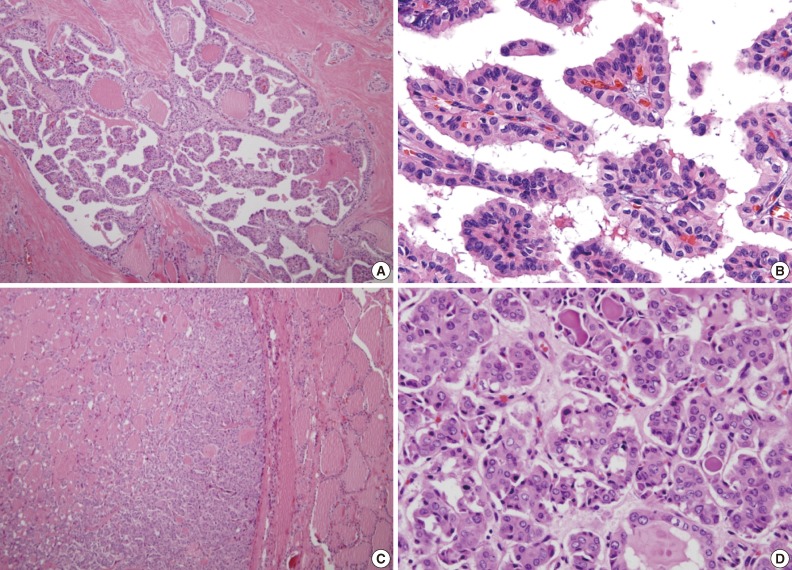
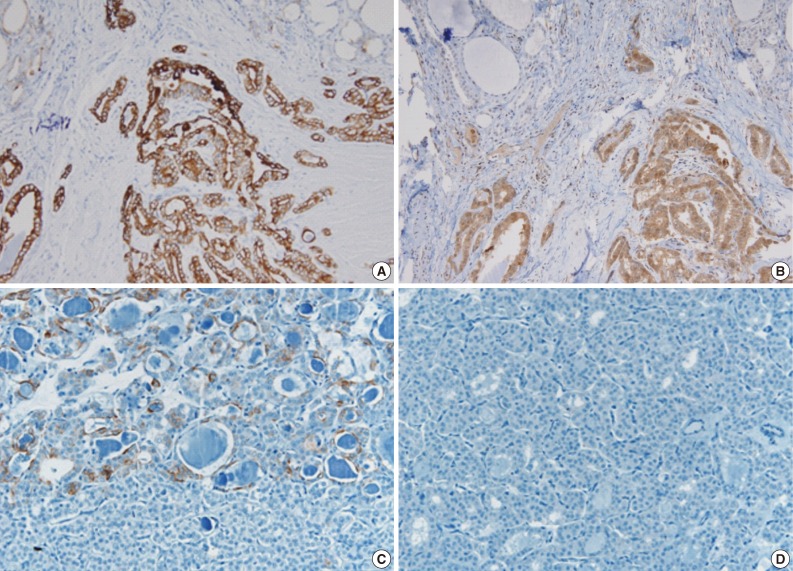
Fig. 1 (A, B) The conventional types in multifocal papillary thyroid carcinoma reveals typical complex and branching papillae with characteristic nuclear features. (C) The follicular variant is encapsulated and composed of small to medium sized, irregularly shaped follicles without papilla formation. (D) Tumor cells of the follicular variant show enlarged, clear nuclei with infrequent nuclear grooves and less irregular nuclear contours compared to conventional foci. Also deeply eosinophilic colloid showing peripheral scalloping is seen within some follicles.
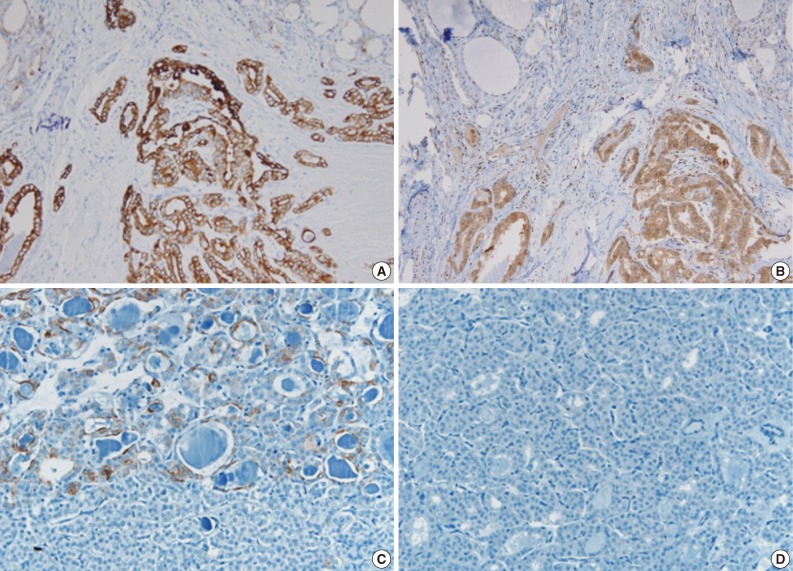
Fig. 2 The tumor cells of the conventional papillary thyroid carcinoma (A, B) show strong, diffusely positive immunoreactivity to cytokeratin 19 (A) and galectin 3 (B), whereas the tumor cells of the follicular variant reveal focal, weak positivity to cytokeratin 19 (C), and no reactivity to galectin 3 (D).
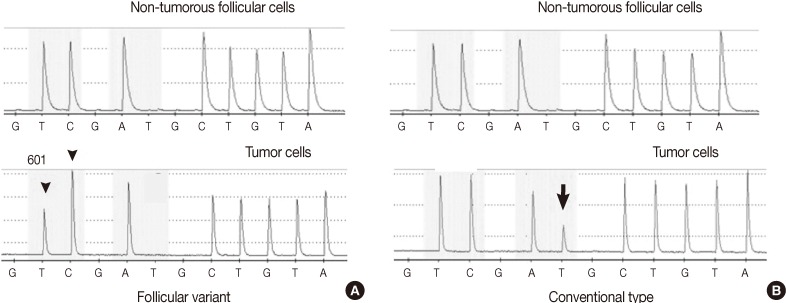
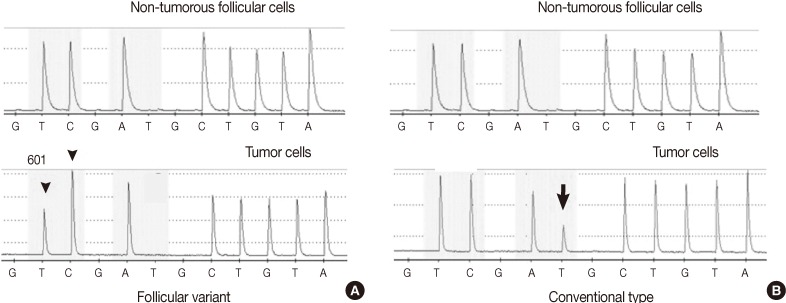
Fig. 3 The pyrosequencing analysis of the BRAF mutation shows the BRAF K601E (A1801G) mutation in one follicular variant (A) and the BRAF V600E (T1799A) mutation in three conventional types (B) of multifocal papillary thyroid carcinoma. (A) When the substitution of thymine to cytosine occurs at nucleotide 1801 of exon 15 in the reverse strand, an additional cytosine peak is fused to the next cytosine peak (arrowhead) at nucleotide 1800 with a decrease of the thymine peak at nucleotide 1801 in mutational analysis of the follicular variant. (B) In the three conventional types, the additional thymine peak (arrow) is shown with a decrease of the adenine peak at nucleotide 1799 in reading along the reverse strand.
Fig. 1
Fig. 2
Fig. 3
A Case of Multifocal Papillary Thyroid Carcinoma Consisting of One Encapsulated Follicular Variant with BRAF K601E Mutation and Three Conventional Types with BRAF V600E Mutation

 E-submission
E-submission