Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 47(6); 2013 > Article
-
Case Study
Cystic Benign Phyllodes Tumor in the Inguinal Region - Jai Hyang Go
-
Korean Journal of Pathology 2013;47(6):583-586.
DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.583
Published online: December 24, 2013
Department of Pathology, Dankook University College of Medicine, Cheonan, Korea.
- Corresponding Author: Jai Hyang Go, M.D. Department of Pathology, Dankook University College of Medicine, 119 Dandae-ro, Dongnam-gu, Cheonan 330-997, Korea. Tel: +82-41-550-6972, Fax: +82-41-561-9127, cyjy555@hanmail.net
• Received: November 13, 2012 • Revised: January 21, 2013 • Accepted: January 22, 2013
© 2013 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Benign phyllodes tumor arising from accessory breast tissue of the axilla: An inquisitive rarity
Sonam Sharma
Saudi Surgical Journal.2024; 12(1): 54. CrossRef - Computed tomography and magnetic resonance imaging in diagnosis of metastatic pleural lesion with pleural effusion in patients with breast carcinoma
P. M. Kotlyarov, I. D. Lagkueva, N. I. Sergeev
Russian Pulmonology.2019; 29(1): 112. CrossRef - Mama ectópica en la región inguinal
V.Y. Presas, L.M. Mastronardi, S. Saucedo, E. Rojas Bilbao
Clínica e Investigación en Ginecología y Obstetricia.2017; 44(2): 89. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
Cystic Benign Phyllodes Tumor in the Inguinal Region




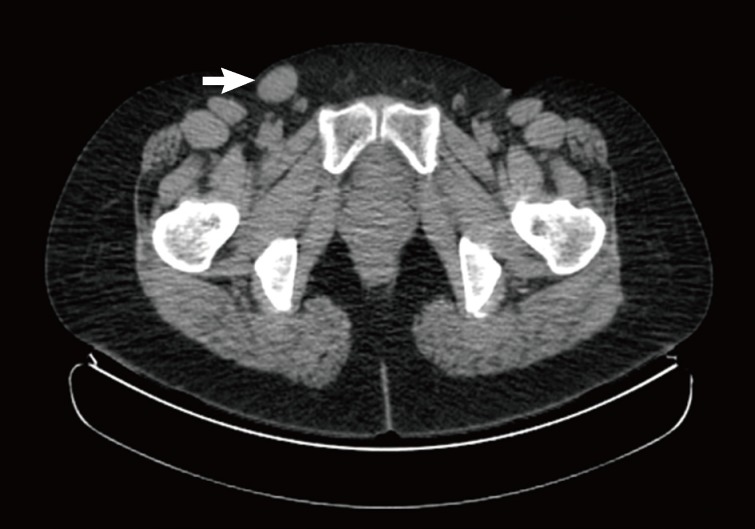
Fig. 1 Positron emission tomography-computed tomography shows a right inguinal mass (27 mm) with low metabolism (arrow).
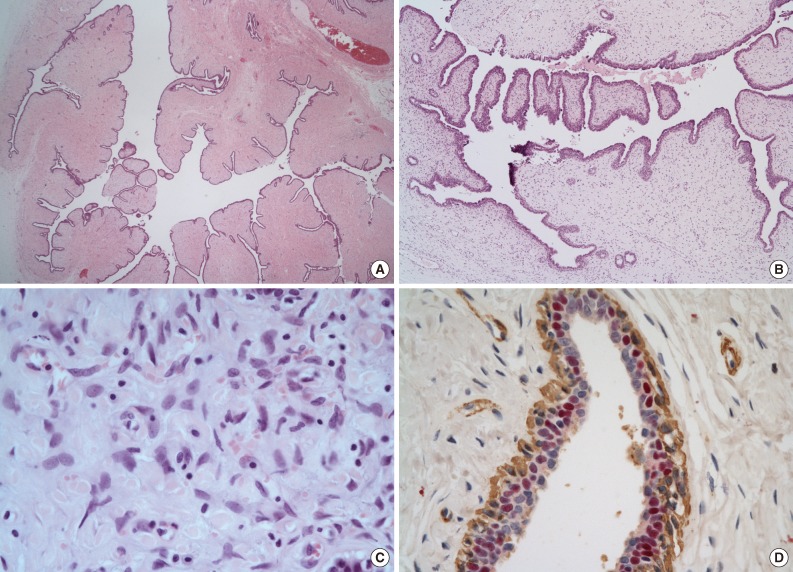
Fig. 2 The tumor is well-circumscribed and showed numerous papillary nodular protrusions into a central cystic cavity (3.5×2.5 cm) (A). Eccentrically, a normal breast tissue (B) is present.
Fig. 3 The microscopic findings show a central elongated cyst with intraluminal projections (A), which is composed of hyperplastic epithelium lined stroma (B). Stromal cells have no mitosis, low-to-moderated cellularity, and mild cytoplasm atypia (C). The lining epithelial cells are diffusely and strongly positive for estrogen receptor. Myoepithelial cells are nonreactive (immunohistochemistry for estrogen receptor [red] and smooth muscle actin [brown]) (D).
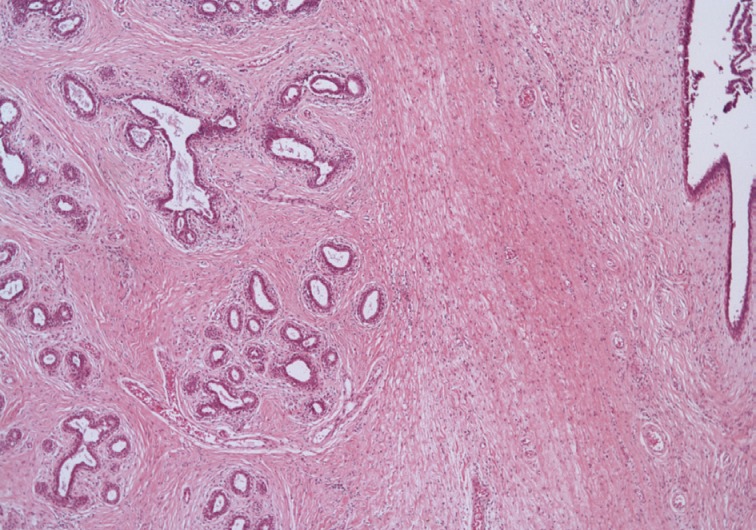
Fig. 4 In the periphery of the mass, normal breast tissue is identified.
Fig. 1
Fig. 2
Fig. 3
Fig. 4
Cystic Benign Phyllodes Tumor in the Inguinal Region
| Case No. | Age (yr) | Location | Size (cm) | Histology | Treatment | Reference |
|---|---|---|---|---|---|---|
| 1 | 20 | Labium majora | 3.0 × 4.0 | Benign | Excision | Tbakhi et al. [9] |
| 2 | 39 | Labium majus | 1.4 × 2.0 | Benign | Excision | Tresserra et al. [10] |
| 3 | 17 | Labium majus and minus | 1.6 × 1.2 | Benign | Excision | Tresserra et al. [10] |
| 4 | 34 | Labium majus | 6.0 × 4.0 | Benign | Excision | Chulia et al. [11] |
| 5 | 31 | Axilla | 1.7 × 1.6 | Benign | Excision | Oshida et al. [3] |
| 6 | 45 | Axilla | 3 × 2 | Low-grade | Wide excision | Saleh and Klein [12] |
Table 1. Summary of the reported cases of ectopic phyllodes tumor

 E-submission
E-submission