Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(2); 2014 > Article
-
Original Article
Incidence and Malignancy Rates of Diagnoses in the Bethesda System for Reporting Thyroid Aspiration Cytology: An Institutional Experience - Ji Hye Park, Sun Och Yoon, Eun Ju Son1, Hye Min Kim, Ji Hae Nahm, SoonWon Hong
-
Korean Journal of Pathology 2014;48(2):133-139.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.2.133
Published online: April 28, 2014
Department of Pathology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
1Department of Radiology, Gangnam Severance Hospital, Yonsei University College of Medicine, Seoul, Korea.
- Corresponding Author: SoonWon Hong, M.D. Department of Pathology, Gangnam Severance Hospital, Yonsei University College of Medicine, 211 Eonju-ro, Gangnam-gu, Seoul 135-720, Korea. Tel: +82-2-2019-3543, Fax: +82-2-3463-2103, soonwonh@yuhs.ac
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
-
Background
- The Bethesda System for Reporting Thyroid Cytopathology (BSRTC) uses six diagnostic categories to standardize communication of thyroid fine-needle aspiration (FNA) interpretations between clinicians and cytopathologists. Since several studies have questioned the diagnostic accuracy of this system, we examined its accuracy in our hospital.
-
Methods
- We calculated the incidences and malignancy rates of each diagnostic category in the BSRTC for 1,730 FNAs that were interpreted by four cytopathologists in Gangnam Severance Hospital between October 1, 2011, and December 31, 2011.
-
Results
- The diagnostic incidences of categories I-VI were as follows: 13.3%, 40.6%, 9.1%, 0.4%, 19.3%, and 17.3%, respectively. Similarly, the malignancy rates of these categories were as follows: 35.3%, 5.6%, 69.0%, 50.0%, 98.7%, and 98.9%, respectively. In categories II, V, and VI, there were no statistically significant differences in the ranges of the malignancy rates among the four cytopathologists. However, there were significant differences in the ranges for categories I and III.
-
Conclusions
- Our findings suggest that institutions that use the BSRTC should regularly update their diagnostic criteria. We also propose that institutions issue an annual report of incidences and malignancy rates to help other clinicians improve the case management of patients with thyroid nodules.
- Thyroid FNA cytology cases
- We retrospectively analyzed 1,538 patients who had thyroid nodules that were diagnosed by FNA between October 1, 2011, and December 31, 2011, in Gangnam Severance Hospital in Korea. This study met criteria for exemption from review from the institutional review board. Each FNA diagnosis was made independently by one of four cytopathologists. Each thyroid aspiration sample was analyzed by using liquid-based preparation or conventional smear. Some FNAs were originally performed by other hospitals; however, in these cases, the slides were re-evaluated by our cytopathologists. If a case was diagnosed by multiple FNA procedures, then we only considered the last diagnosis in the period of 2011. If a patient had more than two thyroid nodules, then we considered each FNA diagnosis as a separate case.
- Follow-up cases
- Among 1,538 patients, we included 1,383 patients who had follow-up data in the same hospital after diagnosis of their thyroid nodules by FNA. The criteria for considering the follow-up data were at least one additional FNA, sonography of the thyroid or thyroid surgery from the date of initial FNA to December 31, 2013. For follow-up cases that were classified as category IV, V, or VI, we only considered the histologic diagnosis of surgical cases. However, for follow-up cases that were classified as category I, II, or III, we considered both the histologic diagnosis of surgical cases (if applicable) and the most recent FNA diagnosis during the follow-up period. The most recent FNA diagnoses that were classified as category I, II, or III were considered to be benign.
- Statistical analysis
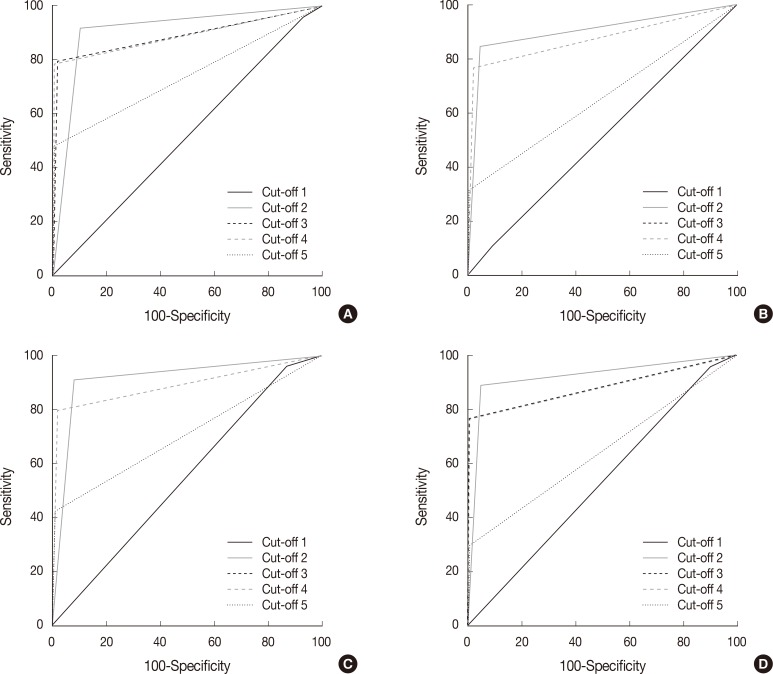
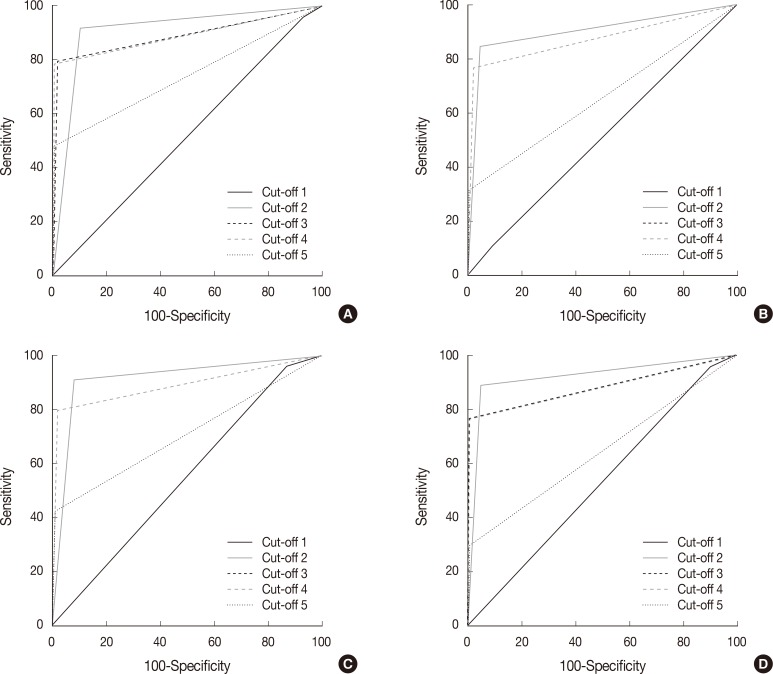
- To determine the sensitivity, specificity, false negative rate, false positive rate, positive predictive value, and negative predictive value of the malignancy rate of individual cytopathologists, we divided the BSRTC categories into two groups: 1) surgery is not recommended (categories I, II, and III) because the suggested malignancy risks of these categories are low, and 2) surgery is recommended (categories IV, V, and VI) because the suggested malignancy risks of these categories are high. The cut-off value for a malignant diagnosis by each cytopathologist was calculated by using a receiver operating characteristic (ROC) curve. ROC curve analysis was performed with MedCalc Statistical Software ver. 12.7.5 (MedCalc Software, Ostend, Belgium). p-values less than .05 were considered to be statistically significant.
MATERIALS AND METHODS
- Patients and distribution of diagnostic categories in all cases
- In this study, we examined 1,538 patients who were 14 to 86 years old (mean, 50 years). The ratio of females to males was 3.8. Among these patients, 201 patients had more than two thyroid nodules, which resulted in a total of 1,730 FNA cases.
- As shown in Table 1, the distribution of all cases in the six BSRTC diagnostic categories were as follows: 230 cases (13.3%) of category I, 702 cases (40.6%) of category II, 157 cases (9.1%) of category III, 7 cases (0.4%) of category IV, 335 cases (19.3%) of category V, and 299 cases (17.3%) of category VI. The total number and distributions of all cases that were analyzed by each cytopathologist is shown in Table 1.
- Patients and distribution of outcomes in follow-up cases
- The patients who met the criteria for follow-up was 1,383. Among these 1,383 patients, 125 had more than two thyroid nodules, rendering a total of 1,547 cases which met the follow-up criteria. Of these 1,547 cases, 213 cases were examined by at least one additional FNA, 485 cases were examined by sonography and the remaining 849 cases were noted by surgery after the initial FNA. The ages of these patients ranged from 14 to 86 years old (mean, 49 years) and the ratio of females to males was 4.0. Their follow-up periods ranged from 2 days to 2 years and 2 months (median, 150 days).
- The distributions of follow-up diagnoses for each initial BSRTC diagnostic classification are shown in Table 2. Specifically, category I diagnoses (116 cases) remained benign in 75 cases (64.7%), but were histologically confirmed as papillary carcinoma in 41 cases (35.3%). Category II diagnoses (702 cases) remained benign in 663 cases (94.5%), but were histologically confirmed as papillary carcinoma in 36 cases (5.1%), follicular carcinoma was present in two cases (0.3%), and poorly differentiated carcinoma occurred in one case (0.1%). Category III diagnoses (126 cases) remained benign in 39 cases (30.9%), but were histologically confirmed as papillary carcinoma in 84 cases (66.7%), follicular carcinoma in two cases (1.6%), and medullary carcinoma in one case (0.8%). Category IV diagnoses (4 cases) were histologically confirmed as follicular carcinoma in two cases (50%) and were histologically confirmed as benign in the other two cases (50%). Category V diagnoses (314 cases) were histologically confirmed as papillary carcinoma in 306 cases (97.4%), medullary carcinoma in three cases (1.0%), and poorly differentiated thyroid carcinoma in one case (0.3%), but were histologically confirmed as benign in three cases (1.1%). Finally, category VI diagnoses (285 cases) were histologically confirmed as papillary carcinoma in 282 cases (98.9%), but were histologically confirmed as benign in three cases (1.1%). The histologically confirmed as benign cases included 53 cases (6.7%) of adenomatous hyperplasia, 13 cases (1.7%) of lymphocytic thyroiditis, nine cases (1.1%) of follicular adenoma, one case (0.1%) of a hyalinizing trabecular tumor, and three cases (0.4%) of a fibrocalcific nodule. The total number and distributions of follow-up cases that were analyzed by each cytopathologist are shown in Table 3. We did not find any significant differences in the malignancy rates for categories II, V, and VI among four cytopathologists, but found considerable difference in the malignancy rates for categories I and III among the cytopathologists. However, the statistical significance of the differences could not be calculated because each FNA diagnosis was made independently by one of four cytopathologists.
- Instead, the cut-off value of malignant diagnosis was analyzed using ROC curves to see if there is a difference in the malignancy-suggesting category among the cytopathologists, and consequently to see if there is a difference in the diagnoses among the cytopathologists. As shown in Fig. 1, we found that all cytopathologists used category III as the cut-off category for differentiating malignant and benign cases (p<.0001).
- The sensitivity, specificity, false negative rate, false positive rate, positive predictive value, and negative predictive value of these malignancy rates for each cytopathologist are shown in Table 4.
RESULTS
- We compared our findings with those reported in 11 previous studies2,3,4,5,6,7,8,9,10,11,12,13 and found several differences, which we attempt to explain below. The percentage of FNA diagnoses in the BSRTC categories V and VI in our study (19.3% and 17.3%, respectively) was higher than that in other studies (mean, 4.6% and 7.9%, respectively) (Table 5). In addition, the percentage of FNA diagnoses in category II in our study (40.6%) was lower than that in previous studies (mean, 62.7%) (Table 5). One possible reason for these differences may be that our hospital is a referral hospital for thyroid surgery, so many patients who are suspected of having thyroid cancer in other hospitals come here to have their FNA diagnoses confirmed and if possible undergo surgery. Baloch et al.10 also reported a high percentage of FNA diagnoses in BSRTC categories V and VI (19.1% and 21.3%, respectively) in a referral hospital, which is similar to our results. Similarly, Lee et al.13 found that 13.0% of FNA diagnoses in a referral hospital were classified as category VI.
- We also found differences in the malignancy rates of some BSRTC categories in our hospital and those reported in previous studies. For example, the malignancy rates in categories I, III, IV, and V in our study (35.3%, 69.0%, 50.0%, and 98.7%, respectively) were higher than those reported in the original BSRTC guidelines (1-4%, 5-15%, 15-30%, and 60-75%, respectively).1 In addition, the malignancy rates in these categories in our study were higher than those in the other studies that we examined (mean, 24.2%, 33.9%, 37.2%, and 72.6%, respectively) (Table 6).2,3,4,5,6,7,8,9,10,11,12,13 There are two possible reasons for these differences. First, although the BSRTC guidelines recommend that patients with categories I or III diagnoses have a repeat FNA, in Korea, patients who have thyroid nodules that are strongly suspicious for malignancy in a clinical aspect undergo surgery without a repeat FNA, but a frozen section examination may be performed. Second, Korean patients tend to be more concerned about false positive results than false negative results, which may pressure cytopathologists to underdiagnose FNA cases to avoid making false positive diagnoses. Lee et al.13 also reported high malignancy rates for categories III and V (79.0% and 97.6%, respectively), which was similar to our result. However, their explanation was different from ours; they suspected that their cytopathologists did not properly apply the BSRTC classification criteria, which were still relatively new at the time of their study. If our explanation that Korean cytopathologists have a tendency to underdiagnose FNA cases is considerable, then clinicians may need to rely on intraoperative diagnoses in those cases. As a result, we need to refine and adapt to the BSRTC classification criteria or the malignancy rates of the BSRTC diagnostic categories may need to be modified. In addition, we recommend providing clinicians with current institutional data about malignancy rates in these categories to help them improve their management of thyroid nodule cases.
- In this study, we did not find any significant differences in the malignancy rates for categories II, V, and VI among four cytopathologists, but found considerable difference in the malignancy rates for categories I and III among the cytopathologists. However, the large number of patients in these categories who did not undergo surgery may have biased these results. Several previous studies have noted that malignancy rates in the BSRTC categories can differ among cytopathologists both intra- and interinstitutionally. For example, Layfield et al.14 reported that there is wide variation in the malignancy rate for category III diagnoses between different institutions and among cytopathologists within same institution, depending on whether they had received cytopathology fellowship training. Similarly, Wu et al.12 found that differences in thyroid cytopathology diagnoses may arise due to differences in the amount of experience or training that cytopathologists have. Furthermore, Cibas and Ali,1 who wrote the original BSRTC paper, later admitted that "category III may never have good interobserver reproducibility, even after pathologists familiarize themselves with the criteria in the atlas,"15 but they argued that this category was still useful because it provides clinically important distinctions for some cases. Since category III diagnoses may differ significantly among cytopathologists, we recommend that institutions prepare annual reports about the malignancy rates of diagnoses in categories III-VI by individual cytopathologists, so clinicians can improve their case management of patients with thyroid nodules. We also recommend that clinicians consider refining category III in order to better characterize the threshold for differentiating malignant cases from benign ones.
- Our comparison of malignancy rate was difficult because category I, II, and III usually does not require surgery, and distribution of category IV is too small to compare. Other reports also commented on the difficulty in comparing malignancy rates arising from the same cause.16,17,18
- Our comparisons of the malignancy rates of individual cytopathologists may be limited in two ways. First, there are some methodological differences between our study and previous studies that have compared the FNA diagnoses of individual cytopathologists. Specifically, other studies made comparisons among cytopathologists who had all diagnosed the same slides.19,20,21,22,23,24 However, this method was not applicable to our study, because we performed a retrospective data analysis. In addition, such quality control methods are often not practical on a daily basis in hospitals. Second, there were no statistically significant differences in the cut-off value of malignant diagnosis by each cytopathologist. We found that all cytopathologists used category III as the cut-off category for differentiating malignant and benign cases (p<.0001). Therefore, we suggested that there was no difference in the malignancy rates of the diagnoses made by individual cytopathologists. However, an improvement in cut-off value is needed because category III is not appropriate for determining malignancy.
- The sensitivity, specificity, false negative rate, false positive rate, positive predictive value, or negative predictive value of the malignancy rates of individual cytopathologists were not significantly different among cytopathologists. There is some limitation due to the large number of cases that were not treated with surgery.
- Conclusion
- In conclusion, the distribution of diagnostic categories in this institute is shifted towards category V and VI, and the malignancy rates of category I, III, and V were higher than those in other reports. Thus, our findings regarding the distribution of FNA diagnoses in the BSRTC diagnostic categories and their malignancy rates in our hospital suggest the need for future improvements in the BSRTC. Specifically, the determination of the malignancy rate needs to be modified to reduce additional diagnostic procedures, such as intraoperative diagnosis. In addition, we propose that institutions prepare, communicate, and use annual reports of malignancy rates of their cytopathologists' diagnoses to help clinicians practice better case management of patients with thyroid nodules.
DISCUSSION
- 1. Cibas ES, Ali SZ. NCI Thyroid FNA State of the Science Conference. The Bethesda System For Reporting Thyroid Cytopathology. Am J Clin Pathol 2009; 132: 658-665. ArticlePubMed
- 2. Bongiovanni M, Spitale A, Faquin WC, Mazzucchelli L, Baloch ZW. The Bethesda System for Reporting Thyroid Cytopathology: a meta-analysis. Acta Cytol 2012; 56: 333-339. ArticlePubMedPDF
- 3. Mondal SK, Sinha S, Basak B, Roy DN, Sinha SK. The Bethesda system for reporting thyroid fine needle aspirates: a cytologic study with histologic follow-up. J Cytol 2013; 30: 94-99. ArticlePubMedPMC
- 4. Jo VY, Stelow EB, Dustin SM, Hanley KZ. Malignancy risk for fine-needle aspiration of thyroid lesions according to the Bethesda System for Reporting Thyroid Cytopathology. Am J Clin Pathol 2010; 134: 450-456. ArticlePubMedPDF
- 5. Yassa L, Cibas ES, Benson CB, et al. Long-term assessment of a multidisciplinary approach to thyroid nodule diagnostic evaluation. Cancer 2007; 111: 508-516. ArticlePubMed
- 6. Yang J, Schnadig V, Logrono R, Wasserman PG. Fine-needle aspiration of thyroid nodules: a study of 4,703 patients with histologic and clinical correlations. Cancer 2007; 111: 306-315. ArticlePubMed
- 7. Nayar R, Ivanovic M. The indeterminate thyroid fine-needle aspiration: experience from an academic center using terminology similar to that proposed in the 2007 National Cancer Institute Thyroid Fine Needle Aspiration State of the Science Conference. Cancer 2009; 117: 195-202. PubMed
- 8. Theoharis CG, Schofield KM, Hammers L, Udelsman R, Chhieng DC. The Bethesda thyroid fine-needle aspiration classification system: year 1 at an academic institution. Thyroid 2009; 19: 1215-1223. ArticlePubMed
- 9. Mufti ST, Molah R. The Bethesda System for Reporting Thyroid Cytopathology: a five-year retrospective review of one center experience. Int J Health Sci (Qassim) 2012; 6: 159-173. ArticlePubMedPMC
- 10. Baloch ZW, Hendreen S, Gupta PK, et al. Interinstitutional review of thyroid fine-needle aspirations: impact on clinical management of thyroid nodules. Diagn Cytopathol 2001; 25: 231-234. ArticlePubMed
- 11. Stamataki M, Anninos D, Brountzos E, et al. The role of liquid-based cytology in the investigation of thyroid lesions. Cytopathology 2008; 19: 11-18. ArticlePubMed
- 12. Wu HH, Rose C, Elsheikh TM. The Bethesda System for Reporting Thyroid Cytopathology: an experience of 1,382 cases in a community practice setting with the implication for risk of neoplasm and risk of malignancy. Diagn Cytopathol 2012; 40: 399-403. ArticlePubMed
- 13. Lee K, Jung CK, Lee KY, Bae JS, Lim DJ, Jung SL. Application of Bethesda System for Reporting Thyroid Aspiration Cytology. Korean J Pathol 2010; 44: 521-527. Article
- 14. Layfield LJ, Morton MJ, Cramer HM, Hirschowitz S. Implications of the proposed thyroid fine-needle aspiration category of "follicular lesion of undetermined significance": a five-year multi-institutional analysis. Diagn Cytopathol 2009; 37: 710-714. ArticlePubMed
- 15. Crippa S, Mazzucchelli L, Cibas ES, Ali SZ. The Bethesda system for reporting thyroid fine-needle aspiration specimens. Am J Clin Pathol 2010; 134: 343-344. ArticlePubMed
- 16. Crowe A, Linder A, Hameed O, et al. The impact of implementation of the Bethesda System for Reporting Thyroid Cytopathology on the quality of reporting, "risk" of malignancy, surgical rate, and rate of frozen sections requested for thyroid lesions. Cancer Cytopathol 2011; 119: 315-321. ArticlePubMed
- 17. Marchevsky AM, Walts AE, Bose S, et al. Evidence-based evaluation of the risks of malignancy predicted by thyroid fine-needle aspiration biopsies. Diagn Cytopathol 2010; 38: 252-259. ArticlePubMed
- 18. Renshaw A. An estimate of risk of malignancy for a benign diagnosis in thyroid fine-needle aspirates. Cancer Cytopathol 2010; 118: 190-195. ArticlePubMed
- 19. Gerhard R, da Cunha Santos G. Inter- and intraobserver reproducibility of thyroid fine needle aspiration cytology: an analysis of discrepant cases. Cytopathology 2007; 18: 105-111. ArticlePubMed
- 20. Redman R, Yoder BJ, Massoll NA. Perceptions of diagnostic terminology and cytopathologic reporting of fine-needle aspiration biopsies of thyroid nodules: a survey of clinicians and pathologists. Thyroid 2006; 16: 1003-1008. ArticlePubMed
- 21. Bomeisl PE Jr, Alam S, Wakely PE Jr. Interinstitutional consultation in fine-needle aspiration cytopathology: a study of 742 cases. Cancer 2009; 117: 237-246. PubMed
- 22. Kocjan G, Chandra A, Cross PA, et al. The interobserver reproducibility of thyroid fine-needle aspiration using the UK Royal College of Pathologists' classification system. Am J Clin Pathol 2011; 135: 852-859. ArticlePubMed
- 23. Clary KM, Condel JL, Liu Y, Johnson DR, Grzybicki DM, Raab SS. Interobserver variability in the fine needle aspiration biopsy diagnosis of follicular lesions of the thyroid gland. Acta Cytol 2005; 49: 378-382. ArticlePubMed
- 24. Stelow EB, Bardales RH, Crary GS, et al. Interobserver variability in thyroid fine-needle aspiration interpretation of lesions showing predominantly colloid and follicular groups. Am J Clin Pathol 2005; 124: 239-244. ArticlePubMed
REFERENCES
| Diagnostic category of Bethesda system | Present study | Mondal et al. [3] | Jo et al. [4] | Yassa et al. [5] | Yang et al. [6] | Nayar and Ivanovic [7] | Theoharis et al. [8] | Mufti and Molah [9] | Baloch et al. [10] | Stamataki et al. [11] | Wu et al. [12] | Lee et al. [13] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | 13.3 | 1.2 | 18.6 | 7.0 | 10.4 | 5.0 | 11.1 | 11.6 | 17.5 | 4.0 | 20.1 | 10.0 |
| II | 40.6 | 87.5 | 59.0 | 66.0 | 64.6 | 64.0 | 73.8 | 77.6 | 15.8 | 74.6 | 39.0 | 67.7 |
| III | 9.1 | 1.0 | 3.4 | 4.0 | 3.2 | 18.0 | 3.0 | 0.8 | 9.8 | 6.7 | 27.2 | 3.1 |
| IV | 0.4 | 4.2 | 9.7 | 9.0 | 11.6 | 6.0 | 5.5 | 4.0 | 16.5 | - | 8.4 | 0.6 |
| V | 19.3 | 1.4 | 2.3 | 9.0 | 2.6 | 2.0 | 1.4 | 2.4 | 19.1 | 2.8 | 2.6 | 5.1 |
| VI | 17.3 | 4.7 | 7.0 | 5.0 | 7.6 | 5.0 | 5.2 | 3.6 | 21.3 | 11.9 | 2.7 | 13.0 |
| Diagnostic category of Bethesda system | Present study | Mondal et al. [3] | Jo et al. [4] | Yassa et al. [5] | Yang et al. [6] | Nayar and Ivanovic [7] | Theoharis et al. [8] | Mufti and Molah [9] | Baloch et al. [10] | Stamataki et al. [11] | Wu et al. [12] | Lee et al. [13] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | 35.3 | 0 | 8.9 | 10.0 | 10.7 | 9.0 | - | 20.0 | 64.0 | 30.0 | 12.0 | 77.8 |
| II | 5.6 | 4.5 | 11.0 | 0.3 | 0.7 | 2.0 | 9.8 | 3.1 | 11.0 | 6.0 | 8.0 | 0 |
| III | 69.0 | 20.0 | 17.0 | 24.0 | 19.2 | 6.0 | 48.0 | 50.0 | 50.0 | 33.0 | 27.0 | 79.0 |
| IV | 50.0 | 30.6 | 25.4 | 28.0 | 32.2 | 14.0 | 34.0 | 20.0 | 63.0 | 67.0 | 33.0 | 61.5 |
| V | 98.7 | 75.0 | 70.0 | 60.0 | 64.8 | 53.0 | 87.0 | 80.0 | 71.0 | - | 68.0 | 97.6 |
| VI | 98.9 | 97.8 | 98.1 | 97.0 | 98.4 | 97.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
Figure & Data
References
Citations

- Assessment of an innovative synthetic matrix for enhanced cell preservation: evaluating its clinical utility and impact on diagnostic precision in thyroid fine-needle aspiration cytology
Diana-Raluca Streinu, Octavian Constantin Neagoe, Andreea Bena, Dana-Liana Stoian
BMC Endocrine Disorders.2026;[Epub] CrossRef - The Malignancy Rates of the Bethesda System for Reporting Thyroid Cytopathology: A 10-year Experience in a Single Asian Institute
Sarah I Liew, Nor S Ahmad, Navarasi R Gopal
World Journal of Endocrine Surgery.2025; 16(2): 42. CrossRef - Assessment of Thyroid Fine-Needle Aspirates Using 2023 Bethesda System
Niti Sureka, Charanjeet Ahluwalia, Sana Ahuja, Neha Kawatra Madan, Meetu Agrawal, Sunil Ranga
Acta Cytologica.2025; 69(3): 280. CrossRef - A Comprehensive Approach to the Thyroid Bethesda Category III (AUS) in the Transition Zone Between 2nd Edition and 3rd Edition of The Bethesda System for Reporting Thyroid Cytopathology: Subcategorization, Nuclear Scoring, and More
Merve Bagıs, Nuray Can, Necdet Sut, Ebru Tastekin, Ezgi Genc Erdogan, Buket Yilmaz Bulbul, Yavuz Atakan Sezer, Osman Kula, Elif Mercan Demirtas, Inci Usta
Endocrine Pathology.2024; 35(1): 51. CrossRef - Evaluation of the Efficacy of Thyroid Imaging Reporting and Data Systems Classification in Risk Stratification and in the Management of Thyroid Swelling by Comparing It With Fine-Needle Aspiration Cytology and Histopathological Examination
Abhishek K Saw, Zenith H Kerketta, Khushboo Rani, Krishna Murari, Kritika Srivastava, Ajay Kumar, Sunny LNU, Anish Baxla, Nabu Kumar, Nusrat Noor
Cureus.2024;[Epub] CrossRef - A COMPARATIVE STUDY BETWEEN CONVENTIONAL METHOD AND THE BETHESDA SYSTEM FOR REPORTING THYROID CYTOPATHOLOGY
Pooja Mangal, Arti Gupta
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2023; : 67. CrossRef - Study of Fine Needle Aspiration Cytology (FNAC) of Thyroid Gland According to the Bethesda System
Keval A Patel, Garima Anandani, Bhawana S Sharma, Riddhi A Parmar
Cureus.2023;[Epub] CrossRef - Correlation of Thyroid Fine Needle Aspiration Biopsy With Histopathological Results
Cemalettin Durgun
Cureus.2023;[Epub] CrossRef - The Bethesda System for Reporting Thyroid Cytopathology: Validating at Tribhuvan University Teaching Hospital
Kunjan Acharya, Shreya Shrivastav, Prashant Triipathi, Bigyan Raj Gyawali, Bijaya Kharel, Dharma Kanta Baskota, Pallavi Sinha
International Archives of Otorhinolaryngology.2022; 26(01): e097. CrossRef - Validating the ‘CUT score’ risk stratification tool for indeterminate thyroid nodules using the Bethesda system for reporting thyroid cytopathology
Sapir Pinhas, Idit Tessler, Luba Pasherstnik Bizer, Khaled khalilia, Meir Warman, Meital Adi, Doron Halperin, Oded Cohen
European Archives of Oto-Rhino-Laryngology.2022; 279(1): 383. CrossRef - ANALYSIS OF FINE NEEDLE ASPIRATIONS OF THE THYROID: CYTOLOGICAL-HISTOPATHOLOGICAL CORRELATION AND OUTCOMES OF THE BETHESDA SYSTEM
Ayca TAN
SDÜ Tıp Fakültesi Dergisi.2022; 29(2): 213. CrossRef - Reproducibility of Cytomorphological Diagnosis and Assessment of Risk of Malignancy of Thyroid Nodules Based on the Bethesda System for Reporting Thyroid Cytopathology
Sasmita Panda, Mamita Nayak, Lucy Pattanayak, Paresh Kumar Behera, Sagarika Samantaray, Sashibhusan Dash
Journal of Microscopy and Ultrastructure.2022; 10(4): 174. CrossRef - Comparative analysis of cytomorphology of thyroid lesion on conventional cytology versus liquid-based cytology and categorize the lesions according to The Bethesda System for Reporting Thyroid Cytopathology
M Qamar Alam, Pinki Pandey, Megha Ralli, Jitendra Pratap Singh Chauhan, Roopak Aggarwal, Vineet Chaturvedi, Asttha Kapoor, Kapil Trivedi, Savita Agarwal
Journal of Cancer Research and Therapeutics.2022; 18(Suppl 2): S259. CrossRef - Thyroid cytology in Pakistan: An institutional audit of the atypia of undetermined significance/follicular lesion of undetermined significance category
Saira Fatima, Rabia Qureshi, Sumbul Imran, Romana Idrees, Zubair Ahmad, Naila Kayani, Arsalan Ahmed
Cytopathology.2021; 32(2): 205. CrossRef - Outcomes of the Bethesda system for reporting thyroid cytopathology: Real‐life experience
Galit Avior, Or Dagan, Isaac Shochat, Yulia Frenkel, Idit Tessler, Alona Meir, Anat Jaffe, Oded Cohen
Clinical Endocrinology.2021; 94(3): 521. CrossRef - National differences in cost analysis of Afirma Genomic sequencing classifier
Ohad Ronen, Maya Oichman
Clinical Endocrinology.2021; 94(4): 717. CrossRef - Thyroid malignancy rates according to the Bethesda reporting system in Israel - A multicenter study
Ory Madgar, Galit Avior, Isaac Shochat, Ben-Zion Joshua, Lior Baraf, Yuval Avidor, Avi khafif, Niddal Assadi, Eran E. Alon
European Journal of Surgical Oncology.2021; 47(6): 1370. CrossRef - Application of the Bethesda system for reporting thyroid cytopathology for classification of thyroid nodules: A clinical and cytopathological characteristics in Bhutanese population
Sonam Choden, Chimi Wangmo, Sushna Maharjan
Diagnostic Cytopathology.2021; 49(11): 1179. CrossRef - Malignancy rates in thyroid nodules classified as Bethesda categories III and IV; a subcontinent perspective
Adnan Zahid, Waqas Shafiq, Khawaja Shehryar Nasir, Asif Loya, Syed Abbas Raza, Sara Sohail, Umal Azmat
Journal of Clinical & Translational Endocrinology.2021; 23: 100250. CrossRef - The combination of ACR‐Thyroid Imaging Reporting and Data system and The Bethesda System for Reporting Thyroid Cytopathology in the evaluation of thyroid nodules—An institutional experience
Shanmugasundaram Sakthisankari, Sreenivasan Vidhyalakshmi, Sivanandam Shanthakumari, Balalakshmoji Devanand, Udayasankar Nagul
Cytopathology.2021; 32(4): 472. CrossRef - Ultrasound-guided fine needle aspiration cytology and ultrasound examination of thyroid nodules in the UAE: A comparison
Suhail Al-Salam, Charu Sharma, Maysam T. Abu Sa’a, Bachar Afandi, Khaled M. Aldahmani, Alia Al Dhaheri, Hayat Yahya, Duha Al Naqbi, Esraa Al Zuraiqi, Baraa Kamal Mohamed, Shamsa Ahmed Almansoori, Meera Al Zaabi, Aysha Al Derei, Amal Al Shamsi, Juma Al Kaa
PLOS ONE.2021; 16(4): e0247807. CrossRef - Incidence, Clinical Characteristics, and Histopathological Results of Atypia of Undermined Significance in a Tertiary Center in UAE
Maha Osman Shangab, Azza Abdulaziz Khalifa, Fatheya Al Awadi, Mouza Alsharhan, Alaaeldin Bashier
Dubai Diabetes and Endocrinology Journal.2021; 27(1): 1. CrossRef - McGill Thyroid Nodule Score in Differentiating Thyroid Nodules in Total Thyroidectomy Cases of Indeterminate Nodules
Hadi A Al-Hakami, Reem Al-Mohammadi, Rami Al-Mutairi, Haya Al-Subaie, Mohammed A Al Garni
Indian Journal of Surgical Oncology.2020; 11(2): 268. CrossRef - The Bethesda System for Reporting Thyroid Cytopathology: A Cytohistological Study
Bakiarathana Anand, Anita Ramdas, Marie Moses Ambroise, Nirmal P. Kumar
Journal of Thyroid Research.2020; 2020: 1. CrossRef - Differences in cytopathologist thyroid nodule malignancy rate
Ohad Ronen, Hector Cohen, Eyal Sela, Mor Abu
Cytopathology.2020; 31(4): 315. CrossRef - Thyroid Multimodal Ultrasound Evaluation—Impact on Presurgical Diagnosis of Intermediate Cytology Cases
Andreea Borlea, Dana Stoian, Laura Cotoi, Ioan Sporea, Fulger Lazar, Ioana Mozos
Applied Sciences.2020; 10(10): 3439. CrossRef - Fine-needle aspiration cytology of nodular thyroid lesions: A 1-year experience of the thyroid cytopathology in a large regional and a University Hospital, with histological correlation
Kaumudi Konkay, Radhika Kottu, Mutheeswaraiah Yootla, Narendra Hulikal
Thyroid Research and Practice.2019; 16(2): 60. CrossRef - Review of a single institution's fine needle aspiration results for thyroid nodules: Initial observations and lessons for the future
Ohad Ronen, Hector Cohen, Mor Abu
Cytopathology.2019; 30(5): 468. CrossRef - Strain Elastography as a Valuable Diagnosis Tool in Intermediate Cytology (Bethesda III) Thyroid Nodules
Dana Stoian, Florin Borcan, Izabella Petre, Ioana Mozos, Flore Varcus, Viviana Ivan, Andreea Cioca, Adrian Apostol, Cristina Adriana Dehelean
Diagnostics.2019; 9(3): 119. CrossRef - Improvement of diagnostic performance of pathologists by reducing the number of pathologists responsible for thyroid fine needle aspiration cytology: An institutional experience
Jae Yeon Seok, Jungsuk An, Hyun Yee Cho
Diagnostic Cytopathology.2018; 46(7): 561. CrossRef - Bethesda Classification and Cytohistological Correlation of Thyroid Nodules in a Brazilian Thyroid Disease Center
Kassia B. Reuters, Maria C.O.C. Mamone, Elsa S. Ikejiri, Cleber P. Camacho, Claudia C.D. Nakabashi, Carolina C.P.S. Janovsky, Ji H. Yang, Danielle M. Andreoni, Rosalia Padovani, Rui M.B. Maciel, Felipe A.B. Vanderlei, Rosa P.M. Biscolla
European Thyroid Journal.2018; 7(3): 133. CrossRef - The impact of rapid on‐site evaluation on thyroid fine‐needle aspiration biopsy: A 2‐year cancer center institutional experience
Ricardo G. Pastorello, Camila Destefani, Pedro H. Pinto, Caroline H. Credidio, Rafael X. Reis, Thiago de A. Rodrigues, Maryane C. de Toledo, Louise De Brot, Felipe de A. Costa, Antonio G. do Nascimento, Clóvis A. L. Pinto, Mauro A. Saieg
Cancer Cytopathology.2018; 126(10): 846. CrossRef - The Use of the Bethesda System for Reporting Thyroid Cytopathology in Korea: A Nationwide Multicenter Survey by the Korean Society of Endocrine Pathologists
Mimi Kim, Hyo Jin Park, Hye Sook Min, Hyeong Ju Kwon, Chan Kwon Jung, Seoung Wan Chae, Hyun Ju Yoo, Yoo Duk Choi, Mi Ja Lee, Jeong Ja Kwak, Dong Eun Song, Dong Hoon Kim, Hye Kyung Lee, Ji Yeon Kim, Sook Hee Hong, Jang Sihn Sohn, Hyun Seung Lee, So Yeon Pa
Journal of Pathology and Translational Medicine.2017; 51(4): 410. CrossRef - Thyroid FNA cytology in Asian practice—Active surveillance for indeterminate thyroid nodules reduces overtreatment of thyroid carcinomas
K. Kakudo, M. Higuchi, M. Hirokawa, S. Satoh, C. K. Jung, A. Bychkov
Cytopathology.2017; 28(6): 455. CrossRef - Thyroid Fine-Needle Aspiration Cytology Practice in Korea
Yoon Jin Cha, Ju Yeon Pyo, SoonWon Hong, Jae Yeon Seok, Kyung-Ju Kim, Jee-Young Han, Jeong Mo Bae, Hyeong Ju Kwon, Yeejeong Kim, Kyueng-Whan Min, Soonae Oak, Sunhee Chang
Journal of Pathology and Translational Medicine.2017; 51(6): 521. CrossRef - Bethesda System for Reporting Thyroid Cytopathology: A three-year study at a tertiary care referral center in Saudi Arabia
Mohamed Abdulaziz Al Dawish, Asirvatham Alwin Robert, Aljuboury Muna, Alkharashi Eyad, Abdullah Al Ghamdi, Khalid Al Hajeri, Mohammed A Thabet, Rim Braham
World Journal of Clinical Oncology.2017; 8(2): 151. CrossRef - A meta‐analytic review of the Bethesda System for Reporting Thyroid Cytopathology: Has the rate of malignancy in indeterminate lesions been underestimated?
Patrizia Straccia, Esther Diana Rossi, Tommaso Bizzarro, Chiara Brunelli, Federica Cianfrini, Domenico Damiani, Guido Fadda
Cancer Cytopathology.2015; 123(12): 713. CrossRef - Value of TIRADS, BSRTC and FNA-BRAFV600E mutation analysis in differentiating high-risk thyroid nodules
Yu-zhi Zhang, Ting Xu, Dai Cui, Xiao Li, Qing Yao, Hai-yan Gong, Xiao-yun Liu, Huan-huan Chen, Lin Jiang, Xin-hua Ye, Zhi-hong Zhang, Mei-ping Shen, Yu Duan, Tao Yang, Xiao-hong Wu
Scientific Reports.2015;[Epub] CrossRef - A study of malignancy rates in different diagnostic categories of the Bethesda system for reporting thyroid cytopathology: An institutional experience
P. Arul, C. Akshatha, Suresh Masilamani
Biomedical Journal.2015; 38(6): 517. CrossRef - Diagnostic accuracy of Bethesda system for reporting thyroid cytopathology: an institutional perspective
Samreen Naz, Atif Hashmi, Amna khurshid, Naveen Faridi, Muhammad Edhi, Anwar Kamal, Mehmood Khan
International Archives of Medicine.2014; 7(1): 46. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure

Fig. 1
| Diagnostic category of Bethesda system | Cytopathologists |
Total (n = 1,730) | |||
|---|---|---|---|---|---|
| A (n = 348) | B (n = 330) | C (n = 382) | D (n = 670) | ||
| I | 28 (8.0) | 50 (15.1) | 63 (16.5) | 89 (13.3) | 230 (13.3) |
| II | 128 (36.8) | 151 (45.8) | 122 (31.9) | 301 (44.9) | 702 (40.6) |
| III | 41 (11.8) | 18 (5.5) | 40 (10.5) | 58 (8.7) | 157 (9.1) |
| IV | 5 (1.4) | 0 (0) | 1 (0.3) | 1 (0.1) | 7 (0.4) |
| V | 57 (16.4) | 66 (20.0) | 75 (19.6) | 137 (20.5) | 335 (19.3) |
| VI | 89 (25.6) | 45 (13.6) | 81 (21.2) | 84 (12.5) | 299 (17.3) |
| Diagnostic category of Bethesda system | Follow-up diagnosis |
|||||
|---|---|---|---|---|---|---|
| BN | PTC | MTC | FC | PD | Malignancy | |
| I (n = 116) | 75 (64.7) | 41 (35.3) | 0 (0) | 0 (0) | 0 (0) | 41 (35.3) |
| II (n = 702) | 663 (94.5) | 36 (5.1) | 0 (0) | 2 (0.3) | 1 (0.1) | 39 (5.6) |
| III (n = 126) | 39 (30.9) | 84 (66.7) | 1 (0.8) | 2 (1.6) | 0 (0) | 87 (69.0) |
| IV (n = 4) | 2 (50.0) | 2 (50.0) | 0 (0) | 0 (0) | 0 (0) | 2 (50.0) |
| V (n = 314) | 4 (1.3) | 306 (97.4) | 3 (1.0) | 0 (0) | 1 (0.3) | 310 (98.7) |
| VI (n = 285) | 3 (1.1) | 282 (98.9) | 0 (0) | 0 (0) | 0 (0) | 282 (98.9) |
| Diagnostic category of Bethesda system | Cytopathologists |
|||
|---|---|---|---|---|
| A (M/T) | B (M/T) | C (M/T) | D (M/T) | |
| I | 41.2 (7/17) | 48.4 (15/31) | 28.0 (7/25) | 27.9 (12/43) |
| II | 4.7 (6/128) | 4.0 (6/151) | 7.4 (9/122) | 6.0 (18/301) |
| III | 63.6 (21/33) | 73.3 (11/15) | 70.0 (21/30) | 70.8 (34/48) |
| IV | 33.3 (1/3) | 0 (0/0) | 0 (0/0) | 100.0 (1/1) |
| V | 100.0 (51/51) | 95.4 (62/65) | 100.0 (68/68) | 99.2 (129/130) |
| VI | 98.8 (80/81) | 100.0 (43/43) | 98.7 (78/79) | 98.8 (81/82) |
| Total | 53.0 (166/313) | 44.9 (137/305) | 56.5 (183/324) | 45.5 (275/605) |
| Cytopathologists |
||||
|---|---|---|---|---|
| A | B | C | D | |
| Sensitivity | 79.5 | 76.6 | 79.8 | 76.7 |
| Specificity | 98.0 | 98.2 | 99.3 | 99.4 |
| False negative rate | 20.5 | 23.4 | 20.2 | 23.3 |
| False positive rate | 2.0 | 1.8 | 0.7 | 0.6 |
| Positive predictive value | 97.8 | 97.2 | 99.3 | 99.1 |
| Negative predictive value | 80.9 | 83.8 | 79.1 | 83.7 |
| Diagnostic category of Bethesda system | Present study | Mondal et al. [3] | Jo et al. [4] | Yassa et al. [5] | Yang et al. [6] | Nayar and Ivanovic [7] | Theoharis et al. [8] | Mufti and Molah [9] | Baloch et al. [10] | Stamataki et al. [11] | Wu et al. [12] | Lee et al. [13] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | 13.3 | 1.2 | 18.6 | 7.0 | 10.4 | 5.0 | 11.1 | 11.6 | 17.5 | 4.0 | 20.1 | 10.0 |
| II | 40.6 | 87.5 | 59.0 | 66.0 | 64.6 | 64.0 | 73.8 | 77.6 | 15.8 | 74.6 | 39.0 | 67.7 |
| III | 9.1 | 1.0 | 3.4 | 4.0 | 3.2 | 18.0 | 3.0 | 0.8 | 9.8 | 6.7 | 27.2 | 3.1 |
| IV | 0.4 | 4.2 | 9.7 | 9.0 | 11.6 | 6.0 | 5.5 | 4.0 | 16.5 | - | 8.4 | 0.6 |
| V | 19.3 | 1.4 | 2.3 | 9.0 | 2.6 | 2.0 | 1.4 | 2.4 | 19.1 | 2.8 | 2.6 | 5.1 |
| VI | 17.3 | 4.7 | 7.0 | 5.0 | 7.6 | 5.0 | 5.2 | 3.6 | 21.3 | 11.9 | 2.7 | 13.0 |
| Diagnostic category of Bethesda system | Present study | Mondal et al. [3] | Jo et al. [4] | Yassa et al. [5] | Yang et al. [6] | Nayar and Ivanovic [7] | Theoharis et al. [8] | Mufti and Molah [9] | Baloch et al. [10] | Stamataki et al. [11] | Wu et al. [12] | Lee et al. [13] |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | 35.3 | 0 | 8.9 | 10.0 | 10.7 | 9.0 | - | 20.0 | 64.0 | 30.0 | 12.0 | 77.8 |
| II | 5.6 | 4.5 | 11.0 | 0.3 | 0.7 | 2.0 | 9.8 | 3.1 | 11.0 | 6.0 | 8.0 | 0 |
| III | 69.0 | 20.0 | 17.0 | 24.0 | 19.2 | 6.0 | 48.0 | 50.0 | 50.0 | 33.0 | 27.0 | 79.0 |
| IV | 50.0 | 30.6 | 25.4 | 28.0 | 32.2 | 14.0 | 34.0 | 20.0 | 63.0 | 67.0 | 33.0 | 61.5 |
| V | 98.7 | 75.0 | 70.0 | 60.0 | 64.8 | 53.0 | 87.0 | 80.0 | 71.0 | - | 68.0 | 97.6 |
| VI | 98.9 | 97.8 | 98.1 | 97.0 | 98.4 | 97.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 | 100.0 |
BN, benign; PTC, papillary carcinoma; MTC, medullary carcinoma; FC, follicular carcinoma; PD, poorly differentiated carcinoma.
M, case number of malignancy; T, total case number.

 E-submission
E-submission