Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 48(2); 2014 > Article
-
Case Study
Follicular Dendritic Cell Sarcoma of the Inflammatory Pseudotumor-like Variant Presenting as a Colonic Polyp - Shien-Tung Pan1, Chih-Yuan Cheng2, Nie-Sue Lee2, Peir-In Liang3, Shih-Sung Chuang3,4
-
Korean Journal of Pathology 2014;48(2):140-145.
DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.2.140
Published online: April 28, 2014
1Department of Pathology, Miao-Li General Hospital, Miaoli City, Taiwan.
2Department of Surgery, Miao-Li General Hospital, Miaoli City, Taiwan.
3Department of Pathology, Chi-Mei Medical Center, Tainan, Taiwan.
4Department of Pathology, Taipei Medical University, Taipei, Taiwan.
- Corresponding Author: Shih-Sung Chuang, M.D. Department of Pathology, Chi-Mei Medical Center, 901 Chung-Hwa Road, Yung-Kang District, Tainan 710, Taiwan. Tel: +886-6-281-2811 (ext. 53686), Fax: +886-6-251-1235, cmh5301@mail.chimei.org.tw
© 2014 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- The fifth edition of the WHO classification of mature T cell, NK cell and stroma-derived neoplasms
Ayoma D Attygalle, Kennosuke Karube, Yoon Kyung Jeon, Wah Cheuk, Govind Bhagat, John K C Chan, Kikkeri N Naresh
Journal of Clinical Pathology.2025; 78(4): 217. CrossRef - Genomic and Transcriptomic Landscape of Epstein-Barr Virus-Positive Inflammatory Follicular Dendritic Cell Sarcoma: A Multicenter Study
Yan Li, Ze-Lin Weng, Han-Xiao Fei, Hai-Feng Li, Yi-Na Liu, Le-Le Zhang, Qiong Zhang, Xin Weng, Yuan-Yuan Wang, Wen-Yong Huang, Zhi-Xing Cao, Kai-Yan Yang, Xi-Liang Chen, Jie Gao, Wen-Sheng Yang, Fang Liu, Juan-Juan Yong, Jing-Ping Yun, Hua Zhang, Yu-Hua H
Modern Pathology.2025; 38(10): 100864. CrossRef - What is new in the 5th edition of the World Health Organization classification of mature B and T/NK cell tumors and stromal neoplasms?
Ayoma D. Attygalle, John K. C. Chan, Sarah E. Coupland, Ming-Qing Du, Judith A. Ferry, Daphne de Jong, Dita Gratzinger, Megan S. Lim, Alina Nicolae, German Ott, Andreas Rosenwald, Anna Schuh, Reiner Siebert
Journal of Hematopathology.2024; 17(2): 71. CrossRef - Pathologic characteristics of histiocytic and dendritic cell neoplasms
Sun Och Yoon
Blood Research.2024;[Epub] CrossRef - Epstein-barr virus (EBV)-positive inflammatory pseudotumor-like follicular dendritic cell sarcoma (IPT-like FDCS) presenting as thrombocytopenia: A case report and literature review
Jiawei Jin, Xiaolong Zhu, Yi Wan, Yang Shi
Heliyon.2024; 10(12): e32997. CrossRef - EBV-positive inflammatory follicular dendritic cell sarcoma of the colon with clonal immunoglobulin gene rearrangement: A case report and literature review
Xia Xu, Xiuzhen Li, Qun Deng, Kaihang Yu, Jinfan Li
Heliyon.2024; 10(11): e31947. CrossRef - Challenges in the Diagnosis of Epstein-Barr Virus-positive Inflammatory Follicular Dendritic Cell Sarcoma
Yan Li, Xia Yang, Lili Tao, Weimei Zeng, Min Zuo, Shuo Li, Liyan Wu, Yanshong Lin, Ziying Zhang, Jingping Yun, Yuhua Huang
American Journal of Surgical Pathology.2023; 47(4): 476. CrossRef - Epstein-Barr Virus-Positive Inflammatory Follicular Dendritic Cell Sarcoma Presenting as a Colonic Polyp: Report of a Case with a Literature Review
Jiahui Hu, Dongdong Huang, Chengfu Xu, Yi Chen, Han Ma, Zhe Shen
Medicina.2023; 59(7): 1341. CrossRef - A Clinicopathology Review and Update of Epstein–Barr Virus-Associated Mesenchymal Tumors
Oswald Zhao Jian Lee, Noorjehan Omar, Joshua K. Tay, Victor Kwan Min Lee
Cancers.2023; 15(23): 5563. CrossRef - Granulomatous splenic mass with necrosis revealing an EBV-positive inflammatory follicular dendritic cell sarcoma
Irena Antonia Ungureanu, Renato Micelli Lupinacci, Marie Parrens, Jean-François Emile
Journal of Surgical Case Reports.2022;[Epub] CrossRef - Case report: Hepatic inflammatory pseudotumor-like follicular dendritic cell sarcoma: A rare case and minireview of the literature
Fan Ding, Chao Wang, Chi Xu, Hui Tang
Frontiers in Medicine.2022;[Epub] CrossRef - Follicular dendritic cell sarcoma of gastrointestinal tract with two emerging distinct subtypes: a case report and systemic review
Hongxing Gui, Jigisha Chaudhari, Rifat Mannan
Diagnostic Pathology.2022;[Epub] CrossRef - Surgical treatment of liver inflammatory pseudotumor-like follicular dendritic cell sarcoma: A case report
Li-Yue Fu, Jiu-Liang Jiang, Meng Liu, Jun-Jun Li, Kai-Ping Liu, Hai-Tao Zhu
World Journal of Gastrointestinal Oncology.2022; 14(11): 2288. CrossRef - Inflammatory pseudotumor-like follicular/fibroblastic dendritic cell sarcoma: focus on immunohistochemical profile and association with Epstein-Barr virus
Francesca Pagliuca, Andrea Ronchi, Annamaria Auricchio, Eva Lieto, Renato Franco
Infectious Agents and Cancer.2022;[Epub] CrossRef - Recent Advances in Digestive Tract Tumors: Updates From the 5th Edition of the World Health Organization “Blue Book”
Raul S. Gonzalez, Anwar Raza, Robert Propst, Oyedele Adeyi, Justin Bateman, Sabrina C. Sopha, Janet Shaw, Aaron Auerbach
Archives of Pathology & Laboratory Medicine.2021; 145(5): 607. CrossRef - Hepatic inflammatory pseudotumor-like follicular dendritic cell tumor: a case report
Ana Daniela Pascariu, Andreea Ioana Neagu, Andrei Valentin Neagu, Alexandru Băjenaru, Cezar Iulian Bețianu
Journal of Medical Case Reports.2021;[Epub] CrossRef - Inflammatory pseudotumor-like follicular dendritic cell sarcoma: Literature review of 67 cases
Hao Wu, Peng Liu, Xiao-Ran Xie, Jing-Shu Chi, Huan Li, Can-Xia Xu
World Journal of Meta-Analysis.2021; 9(1): 1. CrossRef - New Clinicopathologic Scenarios of EBV+ Inflammatory Follicular Dendritic Cell Sarcoma
Xiang-Nan Jiang, Yan Zhang, Tian Xue, Jie-Yu Chen, Alex C.L. Chan, Wah Cheuk, John K.C. Chan, Xiao-Qiu Li
American Journal of Surgical Pathology.2021; 45(6): 765. CrossRef - Select Epstein-Barr Virus–Associated Digestive Tract Lesions for the Practicing Pathologist
Zainab I. Alruwaii, Elizabeth A. Montgomery
Archives of Pathology & Laboratory Medicine.2021; 145(5): 562. CrossRef - Overview of Gastrointestinal Lymphoproliferative disorders✰
Aaron Auerbach, Nadine S. Aguilera
Seminars in Diagnostic Pathology.2021; 38(4): 1. CrossRef - Follicular dendritic cell sarcoma
Fabio Facchetti, Matteo Simbeni, Luisa Lorenzi
Pathologica.2021; 113(5): 316. CrossRef - Hepatic inflammatory pseudotumor-like follicular dendritic cell tumor with hepatic lymphoma history
Jiang Li, Hai-su Tao, Dong Chen, Zhi-yong Huang, Er-lei Zhang
Medicine.2021; 100(39): e27392. CrossRef - Clinicopathological characteristics of extranodal follicular dendritic cell sarcoma: A report of two cases
Xing Zhao, Dayong Sun, Gang Zhang
Oncology Letters.2021;[Epub] CrossRef - Inflammatory pseudotumour-like follicular dendritic cell tumour of the colon with plasmacytosis mimicking EBV-positive lymphoproliferative disorder
Ying-Ren Chen, Chi-Lin Lee, Yen-Chien Lee, Kung-Chao Chang
Pathology.2020; 52(4): 484. CrossRef - Beware the inflammatory cell-rich colonic polyp: a rare case of EBV-positive inflammatory pseudotumour-like follicular dendritic cell sarcoma with increased IgG4-positive plasma cells
Lynne Goh, Nan Zun Teo, Lai Mun Wang
Pathology.2020; 52(6): 713. CrossRef - Epstein–Barr virus‐positive inflammatory follicular dendritic cell sarcoma presenting as a solitary colonic mass: two rare cases and a literature review
Xiaokang Ke, Huihua He, Qingping Zhang, Jingping Yuan, Qilin Ao
Histopathology.2020; 77(5): 832. CrossRef - Inflammatory pseudotumor-like follicular dendritic cell sarcoma: A brief report of two cases
Bi-Xi Zhang, Zhi-Hong Chen, Yu Liu, Yuan-Jun Zeng, Yan-Chun Li
World Journal of Gastrointestinal Oncology.2019; 11(12): 1231. CrossRef - Epstein-Barr virus (EBV)–associated lymphoid proliferations, a 2018 update
Sherif A. Rezk, Xiaohui Zhao, Lawrence M. Weiss
Human Pathology.2018; 79: 18. CrossRef - A Rare Case of Epstein-Barr Virus Negative Inflammatory Pseudotumor-like Follicular Dendritic Cell Sarcoma Presenting as a Solitary Colonic Mass in a 53-Year-Old Woman; Case Report and Review of Literature
Rossana Kazemimood, Farid Saei Hamedani, Asma Sharif, Sujata Gaitonde, Elizabeth Wiley, Pier Cristoforo Giulianotti, John Vincent Groth
Applied Immunohistochemistry & Molecular Morphology.2017; 25(5): e30. CrossRef - A Case of Inflammatory Pseudotumor-like Follicular Dendritic Cell Sarcoma of the Lymph Node in the Small Bowel Mesentery Accompanied by Myasthenia Gravis
Daichi KITAGUCHI, Katsuji HISAKURA, Taiki SATO, Masanao KURATA, Tatsuya ODA, Nobuhiro OHKOHCHI
Nihon Rinsho Geka Gakkai Zasshi (Journal of Japan Surgical Association).2017; 78(3): 527. CrossRef - Clinicopathological features of inflammatory pseudotumour‐like follicular dendritic cell tumour of the abdomen
Yanyang Chen, Huijuan Shi, Hui Li, Tiantian Zhen, Anjia Han
Histopathology.2016; 68(6): 858. CrossRef - A Rare Case of Follicular Dendritic Cell Sarcoma with Pseudochylous Effusion and Review of Literature From India
Kamal Kant Sahu, Gaurav Prakash, Sandeep Rao, Amanjit Bal, Pankaj Malhotra, Jasmina Ahluwalia, Rakesh K. Vashistha
Indian Journal of Hematology and Blood Transfusion.2015; 31(2): 307. CrossRef - Epstein-Barr virus–associated inflammatory pseudotumor presenting as a colonic mass
Shunyou Gong, Iwona Auer, Rajan Duggal, Stefania Pittaluga, Mark Raffeld, Elaine S. Jaffe
Human Pathology.2015; 46(12): 1956. CrossRef - Response of follicular dendritic cell sarcoma to gemcitabine and docetaxel: report of two cases and literature review
Robert M Conry
Clinical Sarcoma Research.2014;[Epub] CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure


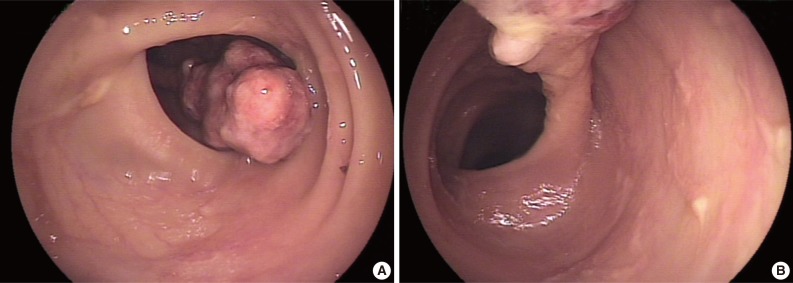
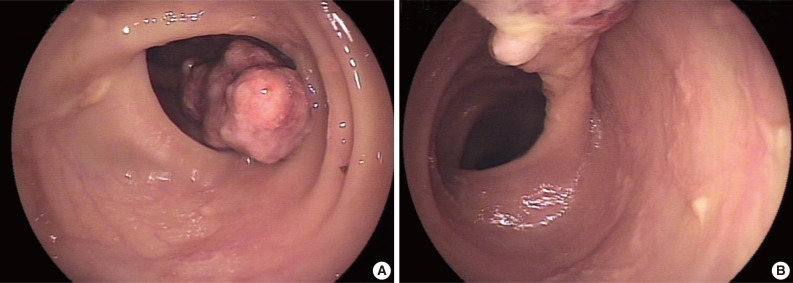
Fig. 1
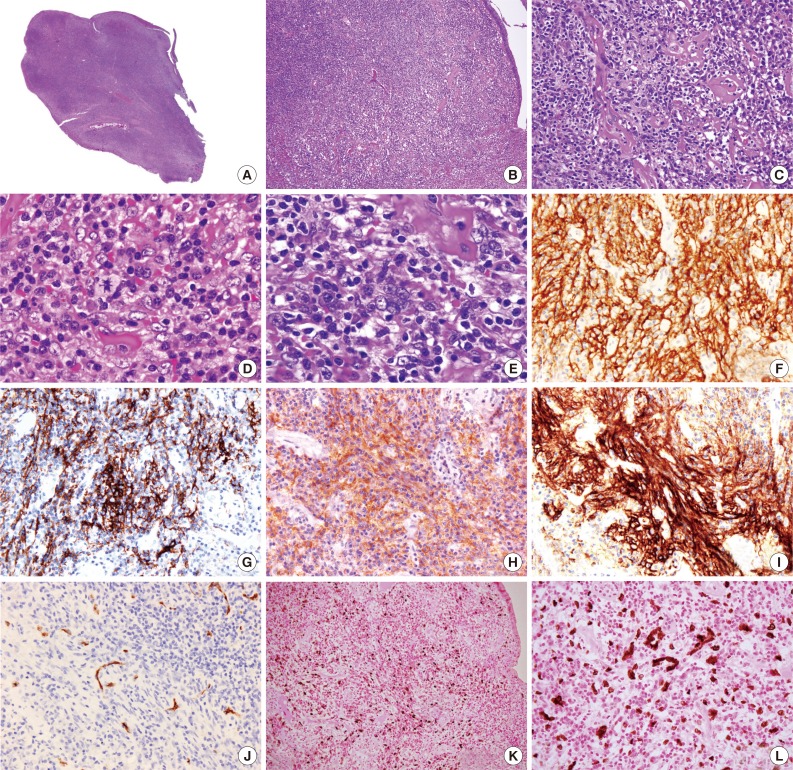
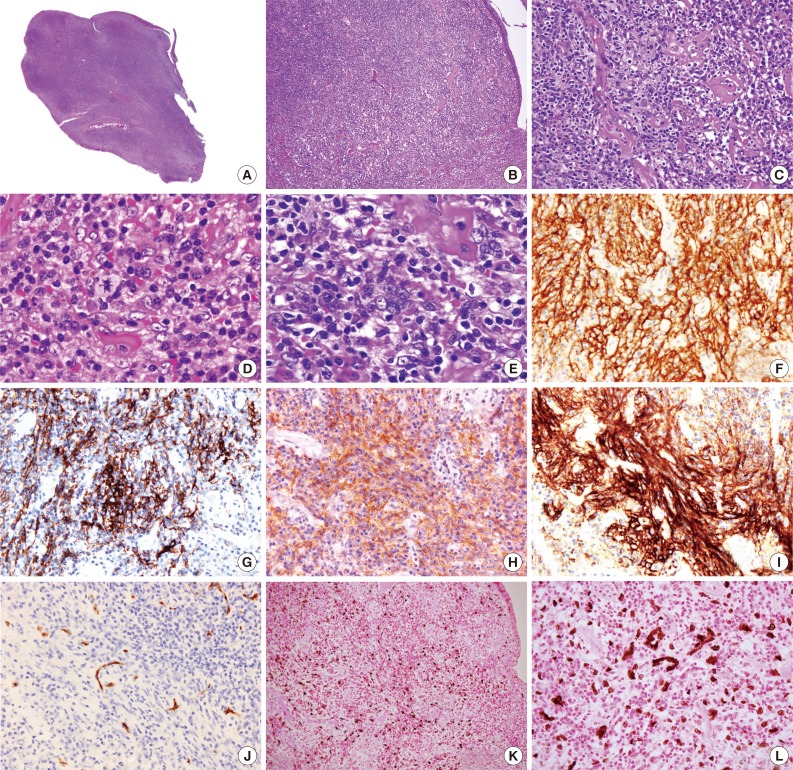
Fig. 2
| Case No. | Sex/Age (yr) | Site | Size (cm) | Immunohistochemistry |
EBER | Tx | Outcome (yr) | Reference | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CD21 | CD23 | CD35 | CNA.42 | Other | LMP1 | ||||||||
| 1 | M/70 | Spleen | 5.5 | ND | ND | ND | ND | FDC+ | ND | + | Surgery | NR | Arber et al. [7] |
| SMA- | |||||||||||||
| 2 | F/68 | Liver | 12 | + | ND | + | ND | R4/23+ | + | + | Surgery | NR | Selves et al. [8] |
| CT | |||||||||||||
| 3 | F/35 | Liver | 20 | + | - | + | ND | R4/23+ | + | + | Surgery | Recurrence | Shek et al. [9] |
| SMA+ | NED, 2.5 | ||||||||||||
| 4 | M/37 | Liver | 15 | + | + | + | ND | ND | + | Surgery | NED, 2 | Shek et al. [10] | |
| 5 | F/19 | Liver | 12 | -/+ |
- | -/+ |
+ | HHF-35+ | +/- | + | Surgery | NED, 3.5 | Cheuk et al. [3] |
| 6 | F/56 | Liver | 15 | + |
+ | + |
+ | HHF-35- | + | + | Surgery | Recurrence, alive | Cheuk et al. [3] |
| with disease, 4.5 | |||||||||||||
| 7 | F/40 | Liver | 12.5 | -/+ |
- | -/+ |
+ | HHF-35- | + | + | Surgery | Recurrence, 9 | Cheuk et al. [3] |
| 8 | F/49 | Liver | 4.2 | + |
+ | + |
+ | +/- | + | Surgery | NED, 0.75 | Cheuk et al. [3] | |
| 9 | M/37 | Liver | 15 | + |
+/- | + |
+ | HHF-35+/- | - | + | Surgery | NED, 3.5 | Cheuk et al. [3] |
| 10 | F/35 | Liver | 20 | +* | + | +* | + | HHF-35+/- | +/- | + | Surgery | Recurrence | Cheuk et al. [3] |
| DOD, 7.9 | |||||||||||||
| 11 | F/31 | Liver | 15 | -/+ |
- | -/+ |
+ | HHF-35+/- | - | + | Surgery | NED, 5 | Cheuk et al. [3] |
| 12 | F/58 | Spleen | 22 | + |
- | + |
+ | +/- | + | Surgery | NED, 0.3 | Cheuk et al. [3] | |
| 13 | F/39 | Spleen | 7.5 | + |
+ | + |
+ | + | + | Surgery | NED, 0.2 | Cheuk et al. [3] | |
| 14 | F/61 | Spleen | 3.5 | + |
+ | + |
+ | HHF-35+/- | +/- | + | Surgery | NR | Cheuk et al. [3] |
| 15 | F/49 | Peripancreas | 9.5 | + |
+ | + |
+ | HHF-35- | +/- | + | Surgery | NR | Cheuk et al. [3] |
| 16 | F/51 | Liver | 15 | + | + | - | ND | ND | + | Surgery | NED, 3 | Chen et al. [11] | |
| 17 | F/57 | Liver | 12 | + | + | - | ND | ND | + | Surgery | NED, 1 | Chen et al. [11] | |
| 18 | M/54 | Spleen | 12 | + | + | ND | ND | SMA+ | +/- | + | Surgery | NED, 4 | Brittig et al. [12] |
| 19 | F/77 | Spleen | 11 | ND | ND | ND | + | + | + | Surgery | NED, 3 | Horiguchi et al. [13] | |
| 20 | F/30 | Liver | 5.5 | + | ND | + | ND | ND | + | Surgery | NED, 2 | Bai et al. [14] | |
| 21 | F/50 | Spleen | 5 | + | ND | + | + | SMA+ | ND | + | Surgery | NED, 0.3 | Laurent et al. [15] |
| 22 | F/57 | Liver | 13 | + | + | ND | ND | ND | + | Surgery | NED, 2 | Granados et al. [16] | |
| 23 | M/45 | Liver | 14.5 | + | + | - | ND | ND | + | Surgery | NED | Li et al. [5] | |
| 24 | F/78 | Colon | 3.9 | + | + | + | ND | ND | + | Polypectomy | NED, 0.5 | Present case | |
| Subtotal (%) | NA | NA | 11/11 (100) | 13/18 (72) | 6/9 (67) | 13/13 (100) | 6/8 (75) | 24/24 (100) | NA | NA | NA | ||
NACase 1-3 and 11 are reported as inflammatory pseudotumor. IPT, inflammatory pseudotumor; FDC, follicular dendritic cell; LMP-1, latent membrane protein 1; EBER, Epstein-Barr virus-encoded mRNA; Tx, treatment; M, male; ND, not done; SMA, smooth muscle actin; NR, not recorded; F, female; CT, chemotherapy; NED, no evidence of disease; DOD, die of disease; NA, not applicable. Staining results from using combined CD21 and CD35 antibodies. These cases are not included in the calculation for the percentage of markers expressed by IPT-like FDC sarcomas.

 E-submission
E-submission