Articles
- Page Path
- HOME > J Pathol Transl Med > Volume 54(1); 2020 > Article
-
Review
Standardized Pathology Report for Colorectal Cancer, 2nd Edition -
Baek-hui Kim1
 , Joon Mee Kim2
, Joon Mee Kim2 , Gyeong Hoon Kang3
, Gyeong Hoon Kang3 , Hee Jin Chang4
, Hee Jin Chang4 , Dong Wook Kang5
, Dong Wook Kang5 , Jung Ho Kim3
, Jung Ho Kim3 , Jeong Mo Bae3
, Jeong Mo Bae3 , An Na Seo6
, An Na Seo6 , Ho Sung Park7
, Ho Sung Park7 , Yun Kyung Kang8
, Yun Kyung Kang8 , Kyung-Hwa Lee9
, Kyung-Hwa Lee9 , Mee Yon Cho10
, Mee Yon Cho10 , In-Gu Do11
, In-Gu Do11 , Hye Seung Lee12
, Hye Seung Lee12 , Hee Kyung Chang13
, Hee Kyung Chang13 , Do Youn Park14
, Do Youn Park14 , Hyo Jeong Kang15
, Hyo Jeong Kang15 , Jin Hee Sohn11
, Jin Hee Sohn11 , Mee Soo Chang16
, Mee Soo Chang16 , Eun Sun Jung17
, Eun Sun Jung17 , So-Young Jin18
, So-Young Jin18 , Eunsil Yu15
, Eunsil Yu15 , Hye Seung Han19
, Hye Seung Han19 , Youn Wha Kim20
, Youn Wha Kim20 , The Gastrointestinal Pathology Study Group of the Korean Society of Pathologists
, The Gastrointestinal Pathology Study Group of the Korean Society of Pathologists -
Journal of Pathology and Translational Medicine 2020;54(1):1-19.
DOI: https://doi.org/10.4132/jptm.2019.09.28
Published online: November 13, 2019
1Department of Pathology, Korea University Guro Hospital, Seoul, Korea
2Department of Pathology, Inha University School of Medicine, Incheon, Korea
3Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
4Department of Pathology, Research Institute and Hospital, National Cancer Center, Goyang, Korea
5Department of Pathology, Eulji University Hospital, Eulji University School of Medicine, Daejeon, Korea
6Department of Pathology, School of Medicine, Kyungpook National University, Daegu, Korea
7Department of Pathology, Chonbuk National University Medical School, Jeonju, Korea
8Department of Pathology, Seoul Paik Hospital, Inje University College of Medicine, Seoul, Korea
9Department of Pathology, Chonnam National University Medical School, Gwangju, Korea
10Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea
11Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
12Department of Pathology, Seoul National University, Bundang Hospital, Seongnam, Korea
13Department of Pathology, Kosin University College of Medicine, Busan, Korea
14Department of Pathology, Pusan National University Hospital, Pusan National University School of Medicine, Busan, Korea
15Department of Pathology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
16Department of Pathology, Seoul National University Boramae Hospital, Seoul National University College of Medicine, Seoul, Korea
17Department of Hospital Pathology, College of Medicine, The Catholic University of Korea, Seoul, Korea
18Department of Pathology, Soonchunhyang University Seoul Hospital, Soonchunhyang UniversityCollege of Medicine, Seoul, Korea
19Department of Pathology, Konkuk University Medical Center, Konkuk University School of Medicine, Seoul, Korea
20Department of Pathology, Kyung Hee University College of Medicine, Seoul, Korea
- Corresponding Author: Joon Mee Kim, MD, PhD, Department of Pathology, Inha University School of Medicine, 27 Inhang-ro, Jung-gu, Incheon 22332, Korea Tel: +82-32-890-3987, Fax: +82-32-890-3464, E-mail: jmkpath@inha.ac.kr
© 2020 The Korean Society of Pathologists/The Korean Society for Cytopathology
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
- The first edition of the ‘Standardized Pathology Report for Colorectal Cancer,’ which was developed by the Gastrointestinal Pathology Study Group (GIP) of the Korean Society of Pathologists, was published 13 years ago. Meanwhile, there have been many changes in the pathologic diagnosis of colorectal cancer (CRC), pathologic findings included in the pathology report, and immunohistochemical and molecular pathology required for the diagnosis and treatment of colorectal cancer. In order to reflect these changes, we (GIP) decided to make the second edition of the report. The purpose of this standardized pathology report is to provide a practical protocol for Korean pathologists, which could help diagnose and treat CRC patients. This report consists of “standard data elements” and “conditional data elements.” Basic pathologic findings and parts necessary for prognostication of CRC patients are classified as “standard data elements,” while other prognostic factors and factors related to adjuvant therapy are classified as “conditional data elements” so that each institution could select the contents according to the characteristics of the institution. The Korean version is also provided separately so that Korean pathologists can easily understand and use this report. We hope that this report will be helpful in the daily practice of CRC diagnosis.
- All report forms mentioned in this document are shown in Table 1. If there are two or more tumors, the data elements should be listed for each tumor, starting with the tumor that has the deepest level of invasion. ‘Regional lymph node metastasis,’ ‘Associated findings,’ and ‘Separate lesions’ are noted only in the deepest tumor.
- Histopathologic type of invasive carcinoma
- Histologic classification of tumors is based on WHO classification (5th edition) [5]. Although most CRCs are “adenocarcinoma, not otherwise specified (NOS),” if there are other histologic variants, it is recommended to mention them separately. This is because some histologic variants may be associated with specific molecular alteration or patient prognosis [5,7]. Representative histologic types of CRC described in WHO classification and AJCC 8th edition are shown in Table 1 [4,5].
- Mucinous adenocarcinoma and signet ring cell carcinoma can be diagnosed when extracellular mucins are over 50% of tumor areas and signet ring cells are over 50% of tumor component, respectively. At levels of 50% or less, it is recommended to describe the ratio of mucin or signet ring cells along with histologic type [5]. When patients received preoperative neo-adjuvant therapy, which may produce mucin, it is advisable to describe the diagnosis of the preoperative specimen [8]. Medullary carcinoma is a rare histologic type that requires differentiation from undifferentiated carcinoma and it is diagnosed when cancer cells appear as solid or sheet-like structures and lymphocytic infiltration is prominent with intraepithelial (tumor-infiltrating) lymphocytes and neutrophils [5,7]. Tumor cells of medullary carcinoma usually show abundant eosinophilic cytoplasm, vesicular nuclei, and prominent nucleoli [5]. Another rare histologic type, micropapillary adenocarcinoma, can be diagnosed when small tumor cell clusters are surrounded by empty spaces, resembling lymphatic or small vessel invasion [9-11]. Micropapillary adenocarcinoma has a high risk of lymph node metastasis and is frequently accompanied with poor prognostic factors such as lymphatic and vascular invasion [9-13]. However, CRC with pure micropapillary patterns are extremely rare and most micropapillary lesions coexist with another histologic type [5,14]. The WHO classification suggests that tumors consisting of 5% or more micropapillary component should be diagnosed as micropapillary adenocarcinoma [5]. However, the minimal proportion of micropapillary components required for the diagnosis of micropapillary adenocarcinoma is controversial, and our committee could not reach a consensus. Serrated adenocarcinoma is also a special subtype of CRC that is morphologically similar to serrated polyps and is characterized by neoplastic glands with prominent epithelial serrations, low nucleus-to-cytoplasm ratio, eosinophilic and abundant cytoplasm, and vesicular nuclei [5,15,16]. Although some studies have suggested diagnostic criteria for serrated adenocarcinoma [17], a consensus has not yet been reached. Adenosquamous carcinoma is diagnosed when an area of definite squamous differentiation is present in the tumor. Although the WHO classification suggests a greater than 20% and 25% adenocarcinoma component or squamous cell carcinoma component, respectively, for the diagnosis of adenosquamous carcinoma in esophageal and gastric cancer, respectively, there is no standardized diagnostic criteria for adenosquamous carcinoma in terms of the squamous cell carcinoma component [5]. We recommend diagnosing adenosquamous carcinoma when the squamous cell carcinoma component is clearly seen in “more than occasional small foci” as described in the previous report [1]. Undifferentiated carcinoma is diagnosed when the epithelial tumor lacks morphological, immunohistochemical, and molecular evidence of specific differentiation [5]. Adenoma-like adenocarcinoma, also called villous adenocarcinoma, was first introduced as a histological subtype of CRC in the WHO 5th edition [5]. Adenoma-like adenocarcinoma is composed of villous adenoma-like well differentiated tumors in the invasive portion, showing pushing border and minimal desmoplasia [5]. Whether adenoma-like adenocarcinoma should be classified as a specific subtype of CRC is still controversial and has not been added as a subtype in this report.
- Differentiation of tumors is determined by the area ratio of gland or tubule formation by tumor cells [7]. The degree of differentiation of the tumor is applicable to adenocarcinoma, NOS. This is because other histologic types show their own prognosis [7]. Recently, tumor differentiation has been shown to affect the prognosis of patients with mucinous adenocarcinoma [5,18]. However, standardized tumor grading of mucinous adenocarcinoma has not been presented yet. Tumor grading is preferably performed using a two-tiered system with low-grade and high-grade [5]. In the 3-tiered grading system, tumor differentiation is graded as well differentiated (> 95% gland formation), moderately differentiated (50%–95% gland formation), or poorly differentiated (< 50% gland formation). The “well- and moderately differentiated” grades correspond to low-grade, while “poorly differentiated” corresponds to high-grade of the two-tiered grading system [5,19].
- Location
- The location of the tumor follows the ICD-O classification [6]. The length of the cecum is approximately 6 cm and the length of the sigmoid colon is approximately 40 cm. The rectum begins at 1–2 cm above the dentate line and is 12–15 cm long. The upper third of the rectum is covered by peritoneum on the anterior and lateral sides, the middle third is covered by peritoneum on the anterior side, and the lower third is not covered by peritoneum. In this revision, “overlapping lesion of the colon” was removed from the tumor location section because it is practically not used in most institutions. When tumors are involved in two locations of the colon, the tumor epicenter and more involved area should be considered in the determination of tumor location.
- Gross type
- Superficial type is not recommended for describing tumor gross morphology, because superficial type could be defined by microscopic examination. Fungating/polypoid type can substitute most gross morphology of the previously established superficial type. Nevertheless, if superficial type is used, it should be applied to tumors that are confined to mucosa or submucosa and with tumor thickness of no more than two-fold thickness of adjacent mucosa. Other criteria for tumor gross types are the same as in the previous version. Fungating/polypoid, ulcerofungating, ulceroinfiltrative, and infiltrative gross types correspond to the Borrmann classification of gastric cancer.
- Tumor size
- The tumor size is expressed as the product of the longest axis and the length perpendicular to it. The depth of the tumor is measured with a microscope at the thickest point.
- Depth of invasion
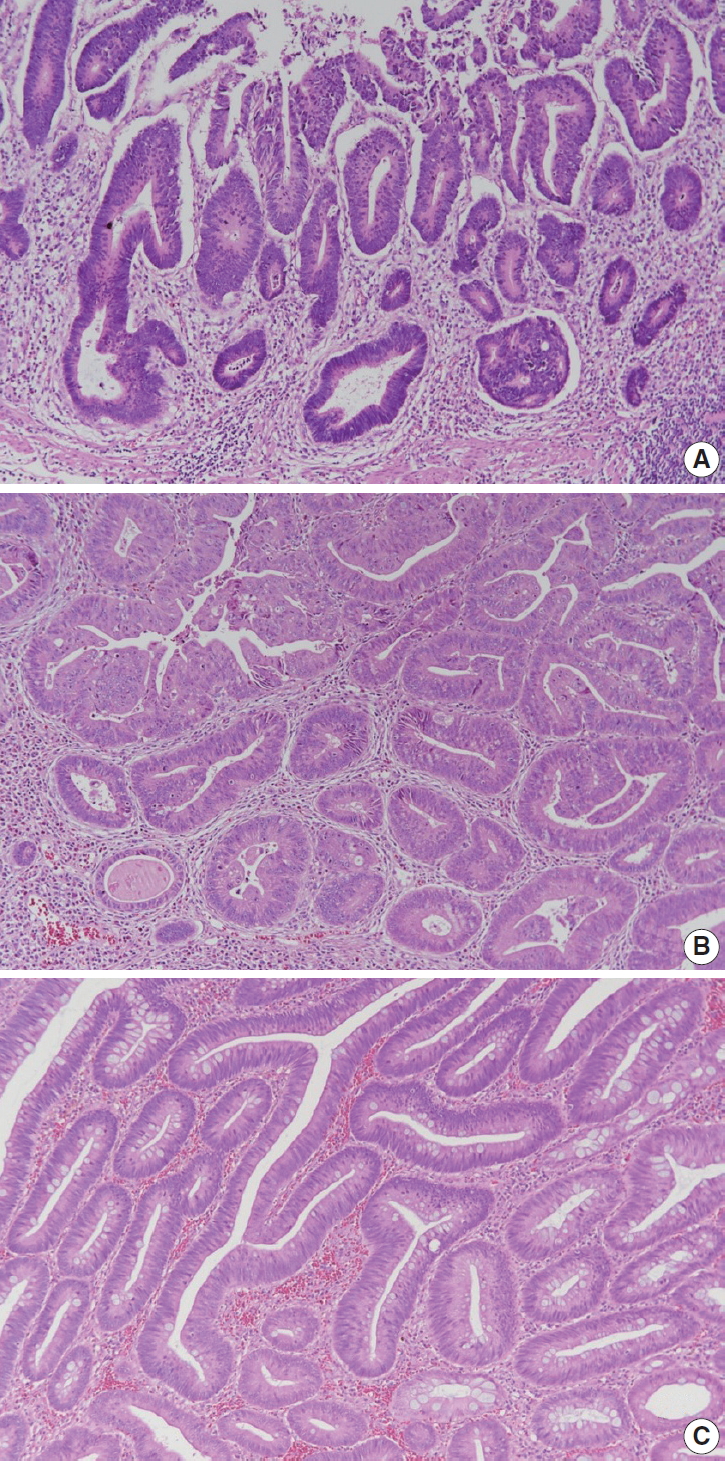
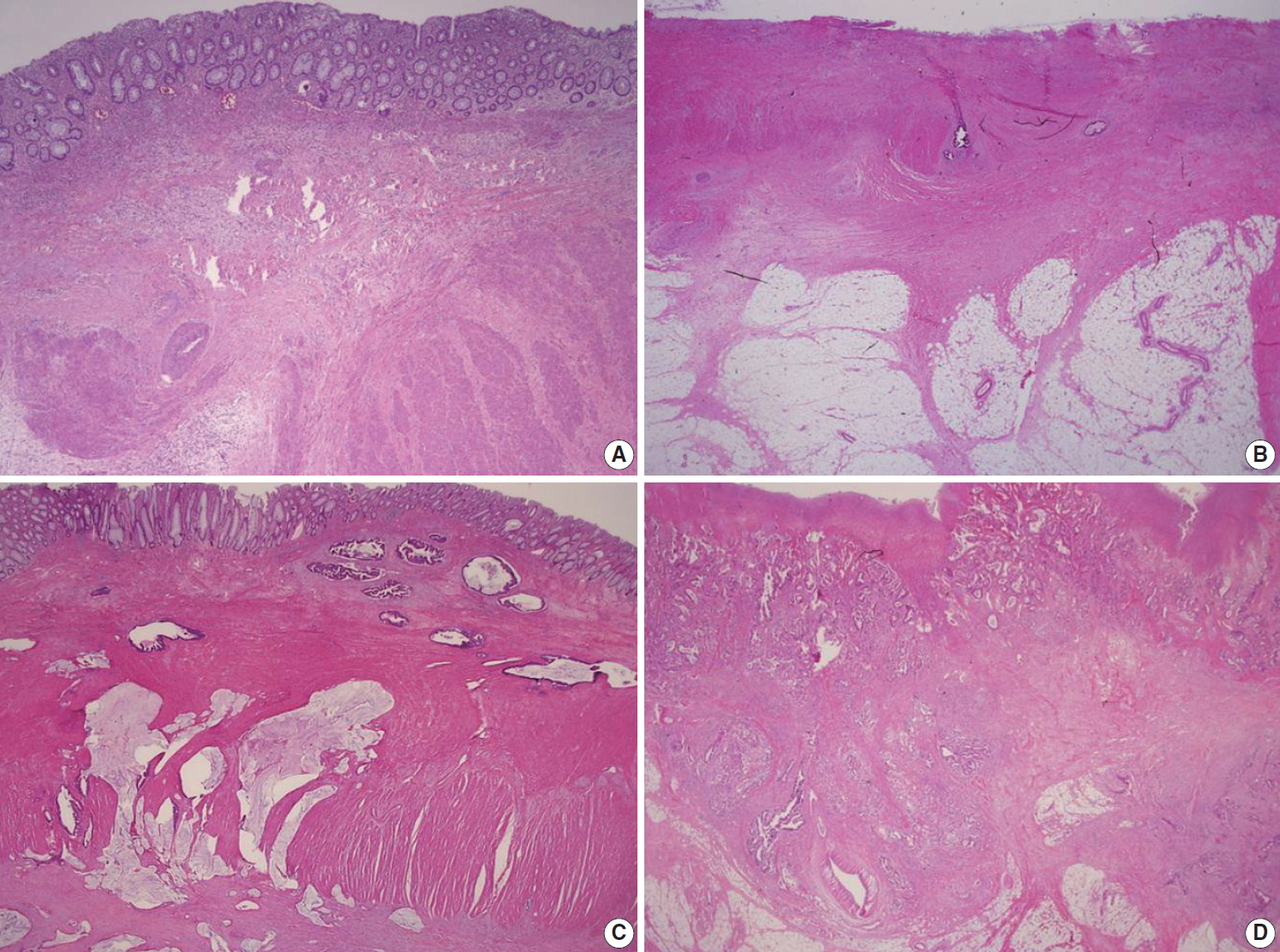
- According to the AJCC 8th edition, “intraepithelial carcinoma” that is confined to the crypt epithelium and lacks invasion beyond the basement membrane is considered synonymous to high-grade dysplasia and is excluded from the pTis category. Intramucosal carcinoma that shows invasion into lamina propria with no penetration through the muscularis mucosae into the submucosa is assigned to pTis considering the negligible risk for metastasis [4]. The histopathologic features of intramucosal carcinoma are defined as follows: (1) infiltration of the stroma by either single or small clusters of tumor cells with basement membrane disruption; (2) a stromal response such as desmoplasia or inflammatory cell infiltrates around the invasion front; (3) definite nuclear anaplasia and severe glandular structural abnormality including marked glandular crowding or excessive branching and budding that endows high suspicion of basement membrane destruction (Fig. 1A, B) [20]. In comparison, high-grade dysplasia is diagnosed when the tumor gland shows (1) nuclear pleomorphism with loss of polarity, (2) architectural complexity of intraluminal cribriforming or necrosis, and (3) back-to-back fusion of multiple glands without lamina propria invasion. Low-grade dysplasia is used when the pseudostratified nucleus is seen without complex architectural change of the glands, regardless of the nuclear ratio to the cell length (Fig. 1C) (refer to ‘Preexisting adenoma’). However, intraepithelial carcinoma of the colorectum had been classified as pTis in the AJCC 7th or earlier editions, while intraepithelial carcinoma of other gastrointestinal tracts except the colorectum is still diagnosed as pTis [4]. Therefore, we recommend minimizing the use of intraepithelial carcinoma or adenocarcinoma in situ in order to reduce confusion and suggest using high-grade dysplasia or intramucosal carcinoma for the diagnosis of mucosal high-grade lesions.
- If there is a tumor at the site where the proper muscle has disappeared by ulceration, it is defined as subserosal infiltration of the tumor (pT3). If tumor cells approach the serosal surface by a gap of ≤ 1 mm with a fibroinflammatory reaction, scrupulous examinations using deeper sections and/or additional tissue blocks are needed to uncover serosal surface involvement [4,21]. In colorectal tumors, similar to other gastrointestinal organs, pT4 is subcategorized into pT4a and pT4b. Although pT4a is basically defined as direct involvement of the serosal surface (visceral peritoneum) by tumor invasion, pT4a encompasses the cases in which tumors with perforation display carcinoma cells running through inflammation to the serosal surface and are accompanied by mesothelial proliferation. The pT4a category is not applicable in nonperitonealized portions of the colorectum, including posterior aspects of the ascending and descending colon and lower portion of the rectum. The pT4b category is assigned when the tumor directly invades the adjacent organs or structures. For distal rectal tumors, tumors with involvement of the external sphincter are assigned to pT3, whereas those with the involvement of the levator ani muscle are assigned to pT4b.
- The presence of tumor cells within the lymphatic or venous vessels is not considered when determining the depth of invasion. The presence of vascular invasion should be recorded in parentheses separately (e.g., invades proper muscle [involvement of subserosa by lymphatic emboli]). The skip metastasis of multiple lesions in mucosa or submucosa of the adjacent bowel is not classified as distant metastasis. The presence of a peritumoral abscess or acellular mucin pool in cancers with preoperative chemoradiotherapy has been known to be unrelated to patients’ prognosis in CRC, and also is not considered in determining the depth of invasion [22-24].
- Endoscopic excision (endoscopic submucosal dissection/polypectomy) or transanal excision
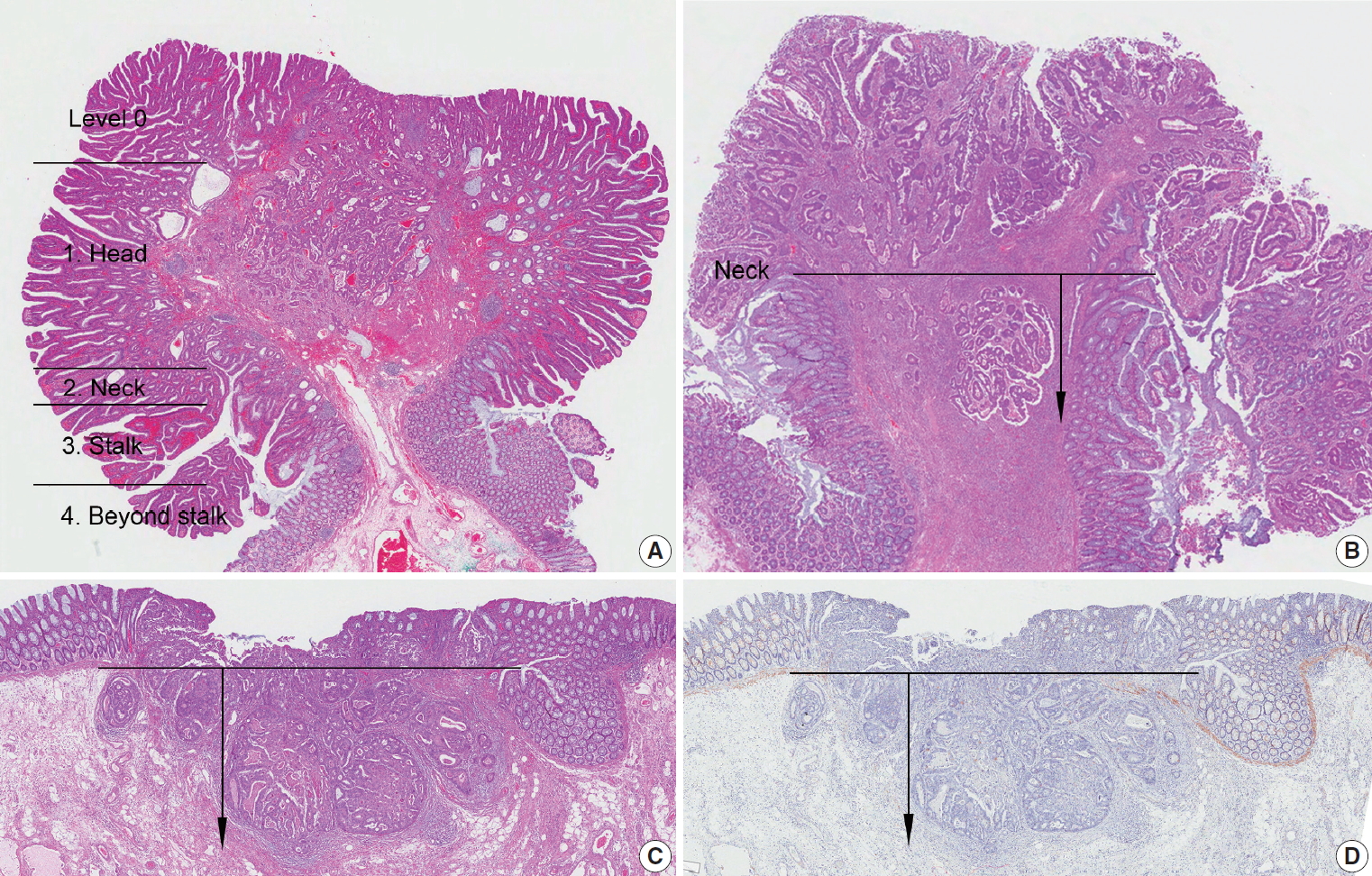
- Invasive adenocarcinomas arising in colorectal adenomas have been called “malignant polyps,” in which tumor cells penetrate through the muscularis mucosae into the submucosa. Independent prognostic factors that prompt further surgical treatment of endoscopically resected polyps are as follows: (1) poorly differentiated carcinoma, (2) tumors at or less than 1 mm from the resection margin, and (3) presence of lymphatic and/or venous vessel involvement. Submucosal invasion depth is also an important factor in determining subsequent surgical treatment, since a submucosal invasion depth of ≥ 1,000 μm in malignant polyps of sessile (non-pedunculated) morphology indicates a significantly increased risk for lymph node metastasis [25,26].
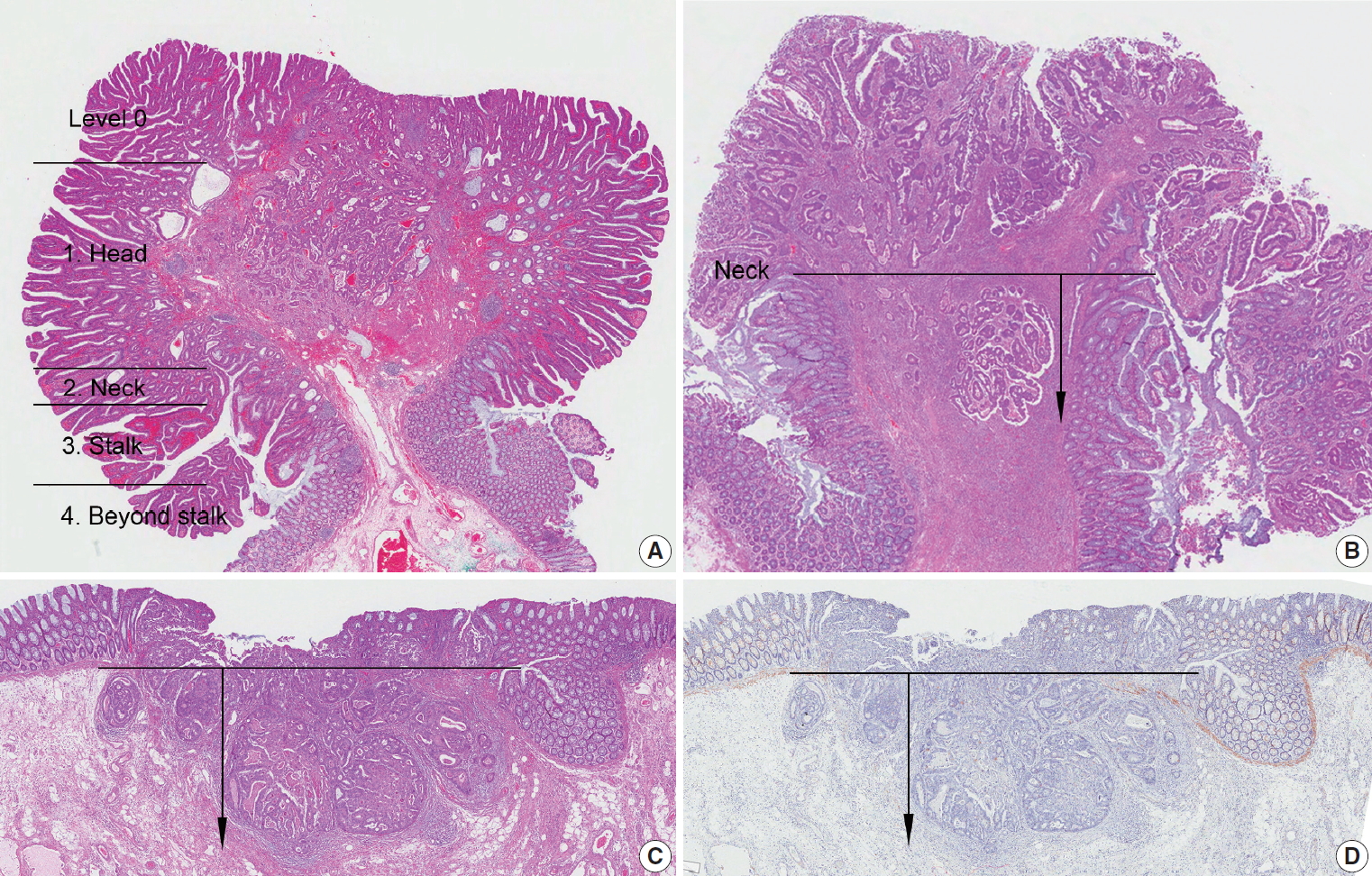
- In this committee, measurement methods were discussed to reduce measurement error in submucosal invasion depth. Polyps are classified into pedunculated and nonpedunculated polyps. For pedunculated polyps, submucosal invasion is classified as ‘head,’ ‘neck,’ ‘stalk,’ and ‘beyond stalk’ according to the Haggitt classification, in which the neck of the polyp (level 2) is the reference point for measuring stalk invasion (Fig. 2A, B) [27,28]. In nonpedunculated polyps, when the muscularis mucosae is preserved, submucosal invasion depth is measured vertically from the lowest part of the muscularis mucosae. When the muscularis mucosae has been disrupted or has disappeared, the depth of submucosa invasion is measured from the imaginary line that is continuous from the residual muscularis mucosae of the neighboring mucosa (Fig. 2C, D) [29].
- Resection margin
- The distance from the proximal and distal resection margins is the length from the edge of the carcinoma to the nearest resection margin. In rectal cancer, the circumferential resection margin should be measured in the areas uncovered by peritoneum. After confirming the circumferential resection margin of the resected specimen, mark the margin with ink, and obtain sections including the site where the tumor is most deeply infiltrated. The involvement of carcinoma in the margin is finally assessed by microscopic examination. If the distance between circumferential resection margin and carcinoma (including lymph node, neural invasion, and intravascular tumor emboli) is 0.1 cm or less than 0.1 cm, the resection margin is regarded as positive [3,4]. Circumferential margins of colon cancers other than rectal cancers can be reported when necessary.
- Endoscopic excision (endoscopic mucosal resection/submucosal dissection/polypectomy) or transanal excision
- This form is applied to the endoscopic resection (polypectomy, mucosal resection, and submucosal dissection) and trans-anal resection. The deep and horizontal margins are examined microscopically. Margin involvement by adenoma is reported in the horizontal margin. When it is impossible to evaluate the resection margins, such as in specimen fragmentation, it shall be marked as ‘not applicable.’
- Regional lymph node metastasis
- Diagnosis of regional lymph node metastasis is made according to the AJCC 8th edition [4]. Although it is recommended to examine 12 or more lymph nodes for determination of accurate prognosis, pN0 can be used if fewer lymph nodes are available, but no lymph node metastasis is observed. Preoperative chemotherapy and radiotherapy can cause fewer lymph nodes to be harvested. Metastasis to lymph nodes other than regional lymph nodes should be diagnosed as distant metastasis and should not be included in lymph node metastasis numbers.
- If the size of the metastatic tumor is less than 2 mm and more than 0.2 mm, it is classified as micrometastasis. If it is less than 0.2 mm, it is classified as isolated tumor cell [4]. A lymph node with micrometastasis is counted as a metastatic lymph node. Although isolated tumor cells are known to be associated with poor prognosis in some stages, pN0 is recommended in AJCC [4]. However, this is controversial and difficult to apply in routine pathologic diagnosis. Thus, we recommend that isolated tumor cells found on hematoxylin and eosin (H&E) slides are considered to be lymph node metastasis and included in the metastatic lymph node numbers, as in the first edition of this report [1].
- Tumor deposits are tumor nodules observed separately from the primary tumor in the subserosa, mesentery, and perirectal tissues, regardless of size, shape, and border. Lymph node, vessel, and neural invasions are excluded from tumor deposits [4]. If a blood vessel or nerve structure is observed within the tumor nodule, it should be regarded as a blood vessel invasion or a neural invasion. Elastic stain or immunohistochemical stain (IHC), such as smooth muscle actin, may be helpful in differentiating tumor deposits. pN1c is used when there is no lymph node metastasis, regardless of the invasion depth of the primary tumor, and when there is a tumor deposit. If there are metastatic lymph nodes, tumor deposits are not included in the number of positive lymph nodes. Care should be taken if the patient received preoperative therapy, because regressed residual tumor in subserosa or perirectal soft tissue can be seen as a tumor deposit.
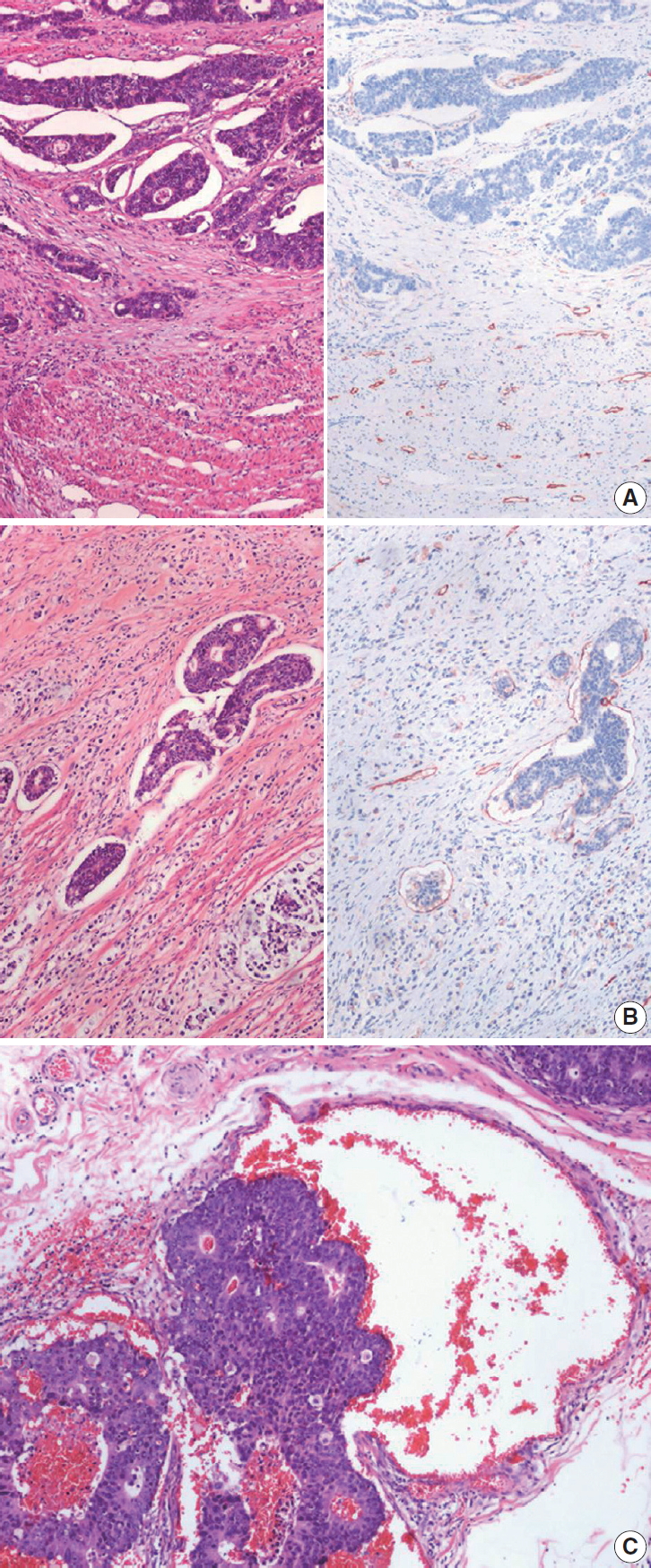
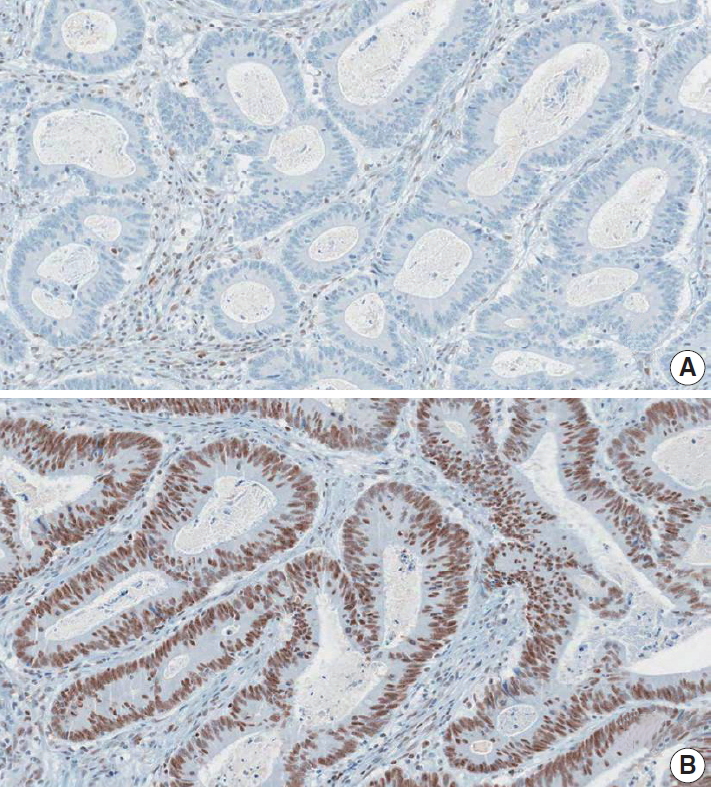
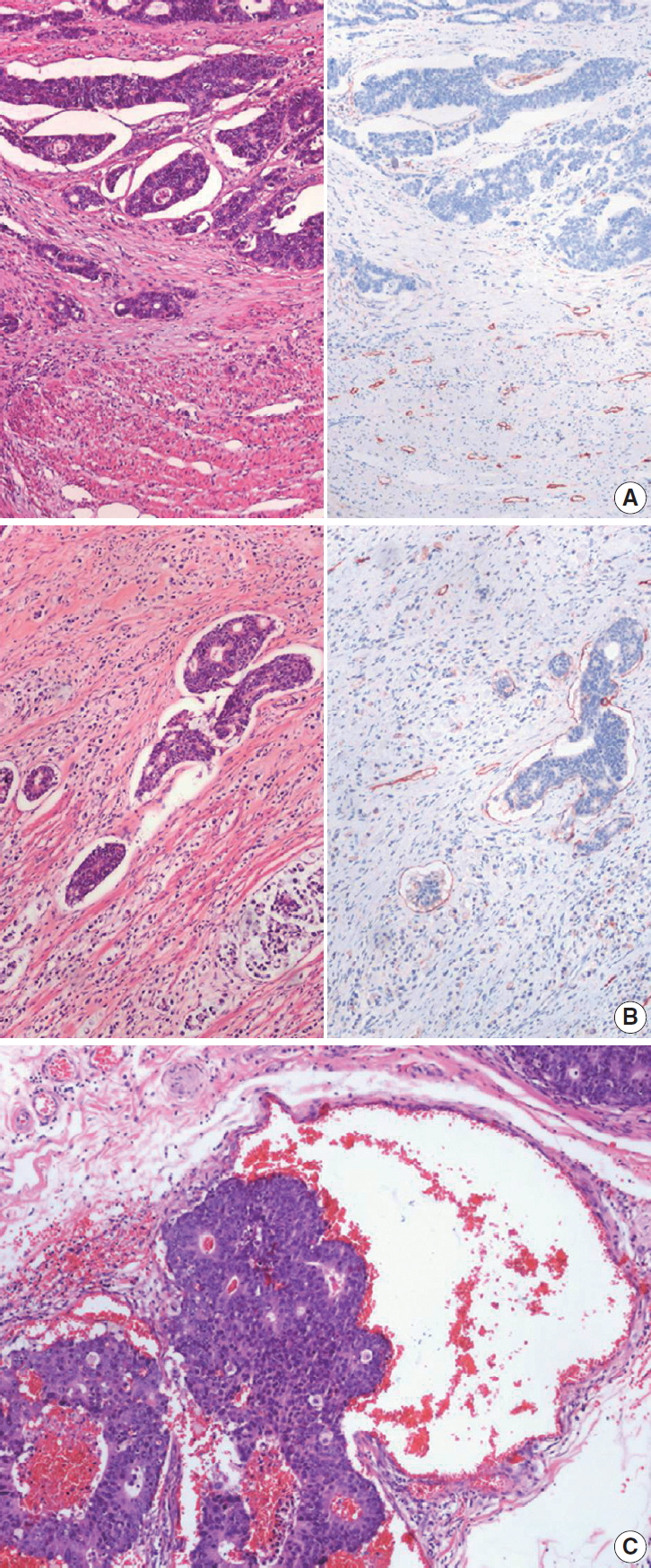
- Lymphatic (small vessel) invasion and venous invasion
- Identification of lymphatic invasion by the tumor has been recognized as a predictor of lymph node metastasis [26], and identification of venous invasion is a well-known independent prognostic indicator [30]. IHC for D2-40 may be performed additionally to identify endothelial cells because it can be difficult to differentiate the lymphatic vessel from retraction artifacts on H&E sections (Fig. 3A). It is commonly difficult to distinguish lymphatic vessels from blood vessels on H&E sections. Thus, it is considered as lymphatic (small vessel) invasion when the tumor cells involve small vessels, such as lymphatics, capillaries, and postcapillary venules (Fig. 3B), whereas venous invasion is when the tumor cells involve large vessels with an identifiable smooth muscle layer or elastic lamina (Fig. 3C) [31]. This should be considered lymphatic (small vessel) invasion if the size of the involved vessel corresponds to that of small vessel, even though there are red blood cells in the involved vessel. Additionally, special stains for elastic fiber or IHCs for CD31, D2-40, and smooth muscle actin can be used if necessary. It is recommended extramural venous invasion be reported separately from the intramural venous invasion, because the former is an adverse prognostic factor and an independent risk factor for liver metastasis [30].
- Perineural invasion
- Perineural invasion has been known as an independent predictor of poor prognosis in CRC [32]. Perineural invasion is an essential element of the pathologic report for CRC and it can be assessed on routine H&E sections. Although there is no clear definition of perineural invasion, it is considered as perineural invasion when the tumor cells invade any of the three layers of nerve sheath, around the nerve, as well as into the nerve [33].
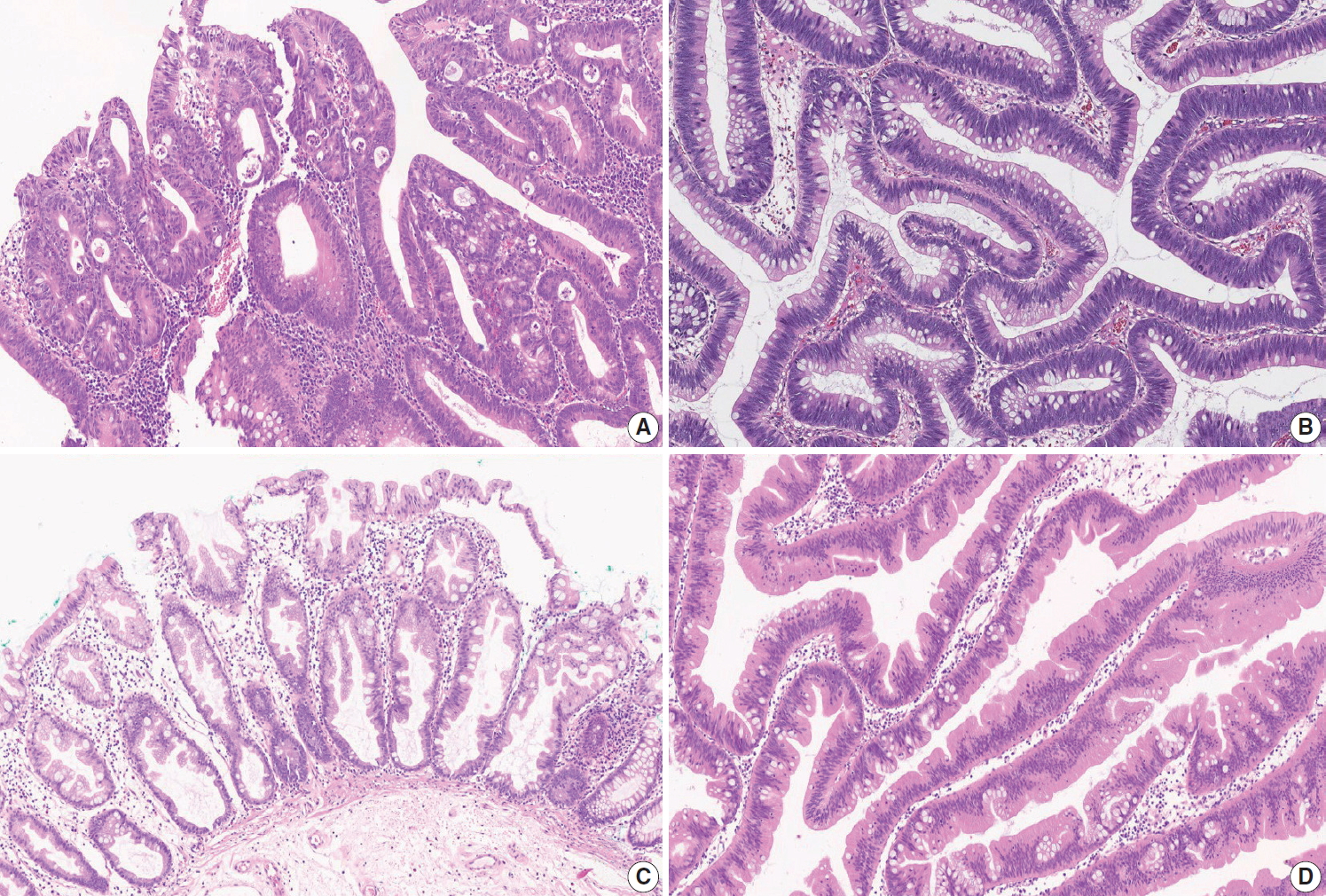
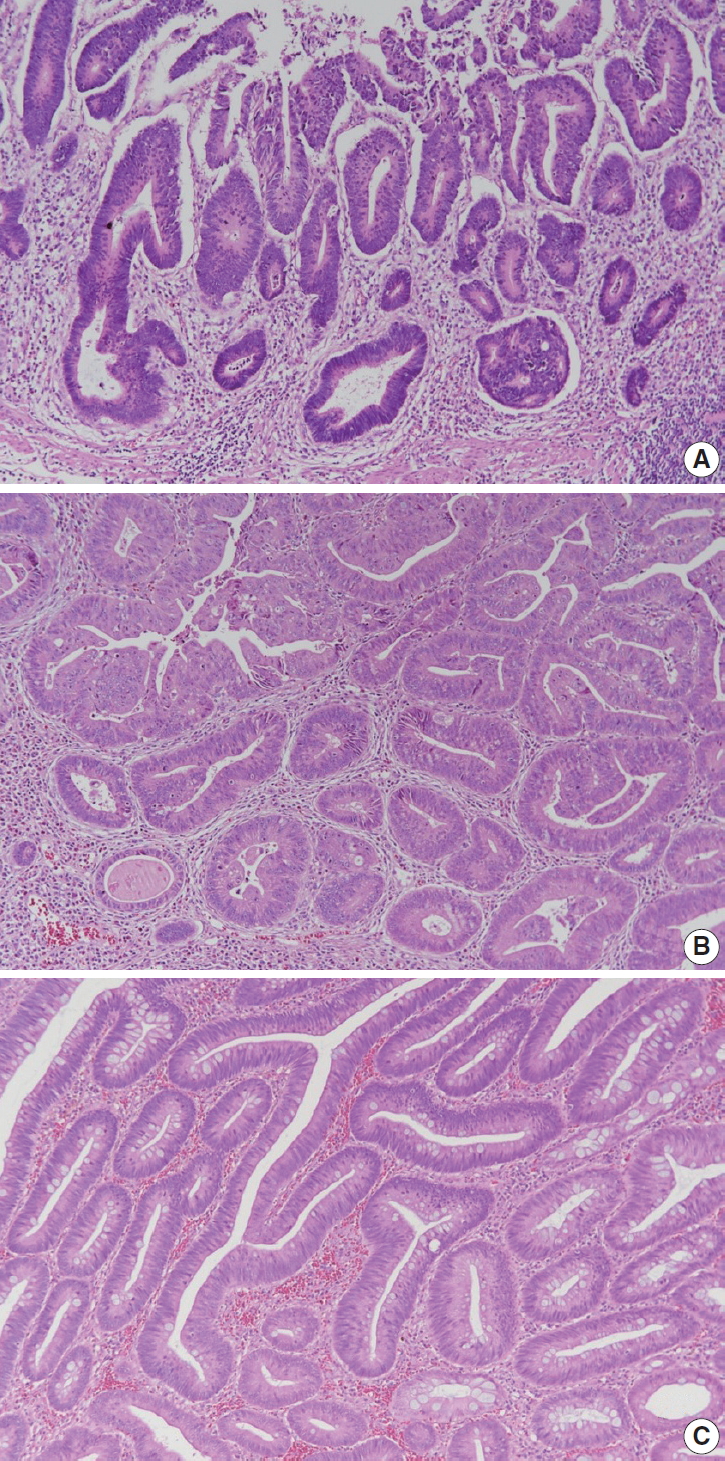
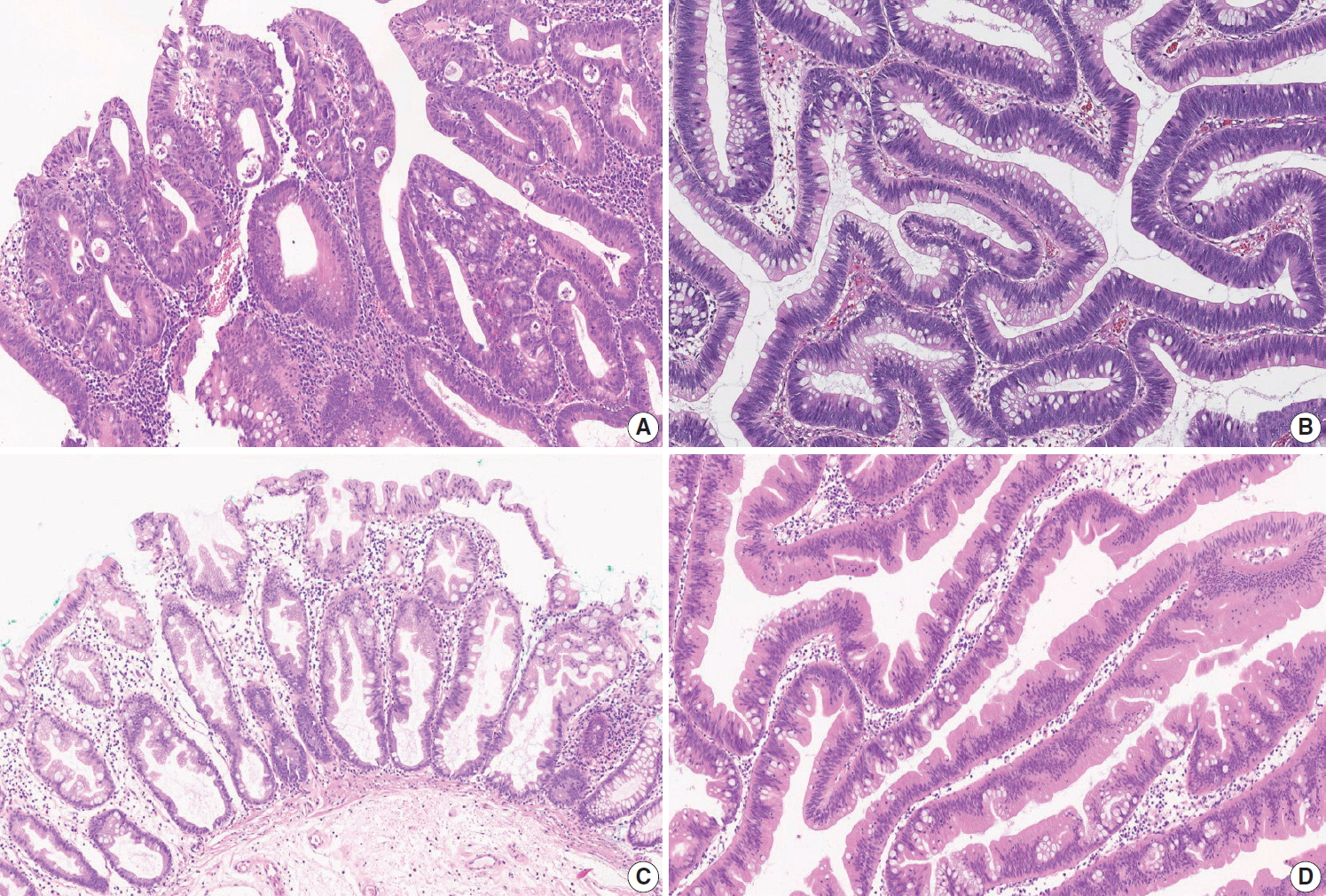
- Pre-existing adenoma
- Two major categories of CRC precursor lesions include conventional adenomas and serrated lesions [34]. According to the latest WHO classification of tumors of the digestive system, conventional adenomas are morphologically classified into tubular (villous component < 25%), tubulovillous (villous component 25%–75%), or villous (villous component > 75%) adenomas based on the proportion of tubular and villous architectures in an adenoma [5]. By definition, all conventional adenomas show dysplastic epithelium, and dysplasia in conventional adenomas can be graded as low-grade or high-grade [5]. High-grade dysplasia is characterized by architectural complexities (e.g., intraluminal cribriforming or necrosis, or back-to-back fusion of multiple glands), nuclear pleomorphisms, loss of nuclear polarity, and increased nuclear-to-cytoplasmic ratio (Fig. 4A). Features of low-grade dysplasia include non-complex architecture, pseudostratified/elongated nuclei with hyperchromasia, and preserved cellular polarization (Fig. 4B). The most important part of the distinction between high-grade and low-grade dysplasia is a complex glandular structure formation of tumor glands without invasion of lamina propria. Dysplastic glands only showing cytologic atypia without complex structural change are not diagnosed as high-grade dysplasia. In the previous edition, we recommended the diagnosis of high-grade dysplasia when there are three contiguous dysplastic gland structures showing high-grade features, which include cytologic atypia. According to the previous edition, there was a tendency to diagnose high-grade dysplasia with only focal cytologic atypia, but tumors with glandular structural abnormalities were sometimes missed as low-grade dysplasia. So, in this edition, complex structural abnormality is described as an essential part of the diagnosis of high-grade dysplasia. When high-grade and low-grade dysplasia components are mixed in a conventional adenoma, the adenoma should be diagnosed as high-grade dysplasia [1].
- Serrated lesions include hyperplastic polyps (HPs), sessile serrated lesions (SSLs, formerly called sessile serrated adenoma/polyp), and traditional serrated adenomas (TSAs), according to the latest WHO classification [5]. However, the classification and diagnostic criteria of serrated lesions have continuously changed [35,36]. Based on a comprehensive review of the latest WHO classification (2019) [5], expert panel recommendations from the US (2012) [35], and UK guidance (2015) [36], we recommend the use of three diagnostic terms for serrated lesions as pre-existing adenomas in CRC: SSL, SSL with dysplasia (SSLD), and TSA. Because HP is regarded as a benign, non-precancerous lesion, it is excluded from serrated lesions as a pre-existing adenoma of CRC.
- All SSLs are regarded as premalignant lesions, and morphologic dysplasia in SSLs can be present or absent. In comparison to SSL without dysplasia, SSLD is regarded to have a higher risk of progression into carcinoma. SSL is morphologically characterized by crypt luminal serrations extending to the crypt base, horizontal growth of the crypt, and asymmetrical proliferation with typical dilated/branching bases of crypts (Fig 4C). The diagnosis of SSL can be made when there is at least one typical architecturally distorted crypt [5,35]. Morphologic changes in SSLD can be diverse, and multiple morphologic patterns can be seen in a single lesion. Structural changes in SSLD include villous change, elongation of crypts, crowding of crypts, cribriform formation, and excessive decrease of luminal serration. Cytologically, dysplastic cells can show conventional adenoma-like dysplasia (so-called intestinal dysplasia) or round atypical nuclei with prominent nucleoli (serrated dysplasia) [5]. Loss of MLH1 expression is frequently found in SSLD and MLH1 immunohistochemical staining may help to define dysplasia [37]. However, the grading system for SSLD has not been suggested yet. Therefore, we simply recommend the presence or absence of dysplasia, regardless of dysplasia subtype or grade, for the description of SSL as a pre-existing adenoma of CRC.
- All TSAs are regarded as precancerous dysplastic lesions, although classification or grading systems for dysplasia in TSAs have not been established. Thus, we recommend the term TSA without any description of dysplasia as a pre-existing adenoma of CRC. TSA is morphologically characterized by broad-topped, sharplyinvaginated luminal serration, tall columnar cells with abundant eosinophilic cytoplasm, pencillate nuclei, and ectopic crypt formation (Fig. 4D). TSAs can frequently be found as mixed lesions accompanying other serrated lesions or conventional adenomas [37,38].
- In the case of a premalignant lesion consisting of two or more different histologic types of conventional adenomas and/or serrated lesions, the lesion can be referred to as a mixed adenoma.
- Associated findings
- Tumor perforation is associated with a poor outcome in CRC [39]. It is known that perforation of the uninvolved colon proximal to an obstructing tumor can cause peritonitis or sepsis, and is associated with poor prognosis. Distant metastasis is now divided into metastasis to one site or organ (pM1a), or metastasis to two or more sites or organs (pM1b), in the absence of peritoneal surface metastasis according to the AJCC 8th edition. Peritoneal surface metastasis is classified as pM1c [4].
- Separate lesions
- When there are lesions other than colorectal cancer, such as separate adenomas, polyps, gastrointestinal stromal tumors, or inflammatory bowel disease, they can be denoted in this section.
STANDARD DATA ELEMENTS FOR RESECTED COLORECTUM
- Tumor budding
- Tumor budding is a well-known independent adverse prognostic factor of CRC [40]. Tumor budding components in the pathologic report can be potentially helpful in the decision-making process for the management of patients with CRC. First, in patients presenting with endoscopically resected submucosal invasive CRC, the presence of tumor budding is positively correlated with increased risk of lymph node metastases [26,41,42]. Therefore, patients with tumor budding can be potential surgical candidates. Second, stage II CRC patients with high-grade tumor budding show worse disease-free survival than those with no or low-grade tumor budding. Therefore, high-grade tumor budding may be useful for screening patients who need adjuvant therapy [43]. Finally, the presence of tumor budding in pre-operative biopsies can aid in the selection of high-risk rectal cancer patients for neoadjuvant therapy [44,45]. As mentioned above, in endoscopically resected pT1 CRC patients and stage II CRC patients, it is recommended to include tumor budding in the pathologic report.
- The International Tumor Budding Consensus Conference (ITBCC) held in 2016 has recommended the following criteria for evaluation of tumor budding [46]. (1) Tumor budding is defined as a single tumor cell or a cell cluster containing ≤ 4 tumor cells. (2) Tumor budding should be assessed in the hotspot at the invasive tumor front (in a field measuring 0.785 mm2, which corresponds to a 20 × objective lens with an eyepiece having a field number that is 20 mm in diameter) chosen after a review of the available slides. (3) Tumor budding can be assessed on H&E slides. IHC for keratin can be helpful in evaluation of obscure cases showing a peritumoral inflammatory infiltrate on H&E-stained slides, which is difficult to distinguish from reactive stromal cells. In such cases, IHC enables better visualization of tumor budding and superior reproducibility and inter-observer agreement [47]. However, keratin also stains apoptotic bodies and cellular debris, which should not be misinterpreted as tumor budding [46,48].
- We also recommend a 3-tier grading system for reporting of tumor budding. However, this grading system is not an absolute standard. Measuring and reporting the number of tumor buddings could be more beneficial to avoid any loss of information that may occur when applying a cut-off value in borderline cases. In rare histopathological subtypes, such as mucinous, signet-ring cells, micropapillary, and medullary carcinomas, the evaluation of tumor budding should be performed with caution [46]. Therefore, when tumor budding cannot be accurately assessed, it is recommended that the findings be reported as “cannot be assessed” with an explanatory note added to the report.
- Tumor border configuration
- Regarding tumor border configuration, there is currently no recommendation in the AJCC 8th edition, nor in the CAP protocol for CRC, and only a brief mention in the WHO classification [3-5]. Although the assessment of tumor border configuration can be easily carried out using H&E slides, inter-observer reproducibility is lacking due to ambiguous definitions [49]. For these reasons, the tumor border configuration was excluded from this standardization report.
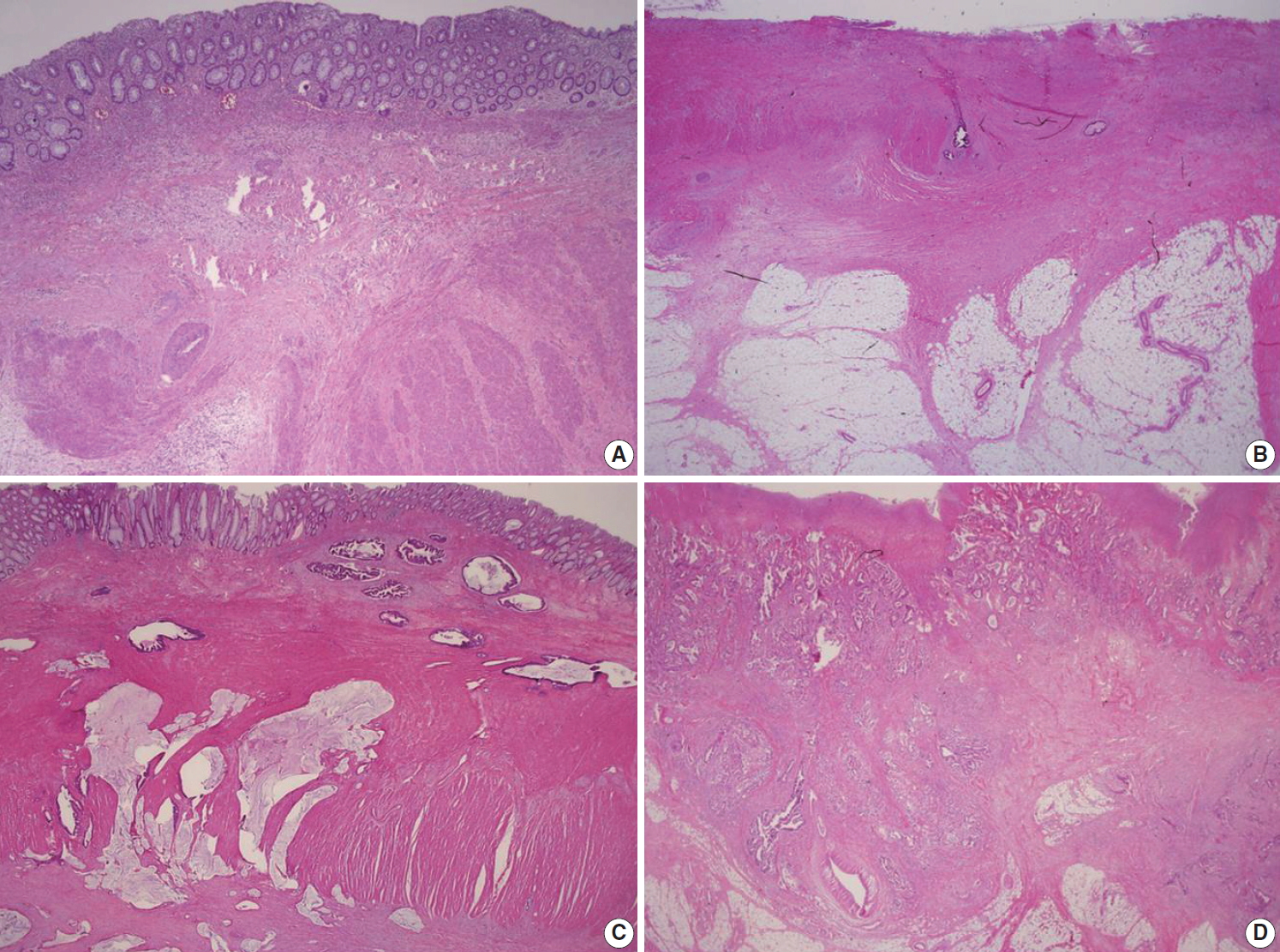
- Completeness of total mesorectal excision
- Total mesorectal excision is a surgical technique that dissects within the areolar plane outside the visceral mesorectal fascia to remove rectum [50]. A large number of non-randomized studies have shown that if total mesorectal excision is appropriately performed, then adequate resection margin is secured, and local recurrence rate is reduced. The surface of the fresh rectal specimen is examined circumferentially, and the completeness of the mesorectal excision is scored according to the worst area, as below [3,4,7].
- - Complete: Mesorectum is totally resected. The surface of the specimen is smooth and there is no coning towards the distal margin (there is no surface defect greater than 0.5 cm in depth).
- - Nearly complete: There is irregularity of the mesorectal surface. The surface defect is greater than 0.5 cm, but proper muscle layer is not exposed (except for levator ani muscles).
- - Incomplete: Severe mesorectal defects down to the muscularis propria. Muscularis propria is exposed.
- Preoperative chemoradiotherapy
- Preoperative chemoradiotherapy (CRT) followed by curative resection with TME has been established as a standard treatment for patients with locally advanced rectal cancer [51,52]. Tumor regression after preoperative CRT has an important role that can improve patient outcomes and the potential for achieving no residual tumor status [53-55]. Many studies have been performed to perceive a practical and applicable tumor regression grading (TRG) system [4,53-59]. The tumor regression after CRT was assessed only in the primary tumor and the nodal status was not included in the assessment of the TRG system [4]. The TRG system recommended in the previous edition of the “standardized pathology report for colorectal cancer” used a descriptive 5-tier system and can be easily translated into the Mandard and Dworak TRG scoring system [1]. However, even with a descriptive TRG system there is an inter-observer variation between pathologists, and this descriptive TRG system is not widely used and is often confused with other existing TRG systems. To overcome this, we suggest a new TRG system, which can be widely used in the pathologic practice, based on the AJCC 8th edition and CAP cancer protocol (Fig. 5) [3,4].
- The number of blocks taken is dependent on the size of the residual tumor. If the tumor is grossly visible, a minimum of 4 paraffin blocks should be taken from the tumor, including samples from its closest point to the nearest margin. However, if the tumor is ill-defined and impossible to distinguish from fibrous stromal tissue or the tumor bed size is less than 2.0 cm, the entire embedding of the macroscopically identifiable tumor bed or entire scar area is recommended, orientated from proximal to distal in 0.4-cm levels. Careful examination of the residual tumor cells is essential and is mandatory for assessment of complete response after CRT in CRC patients. Histologically, the tumor bed is characterized by abundant fibrotic stroma with a moderate number of mononuclear inflammatory cells or foamy macrophages. In these areas, there may be edema or mucinous or myxoid changes of the stroma or even areas of necrosis. The presence of mucin lakes without viable tumor cells (acellular mucin) should be defined as a pathologically complete response. If it is difficult to differentiate between giant cells or fibroblast and tumor cells, it may be helpful to perform serial H&E sections, mucin staining, or cytokeratin IHC in TRG grading.
- EGFR immunohistochemistry
- Expression of epidermal growth factor receptor (EGFR) by IHC has been reported in 25% to 90% of patients with CRC [60-64]. In almost all of the initial studies regarding the efficacy of targeted therapies with cetuximab or panitumumab in CRC patients, evidence of EGFR expression by IHC was essential for the application of therapeutic agents [65]. However, subsequent studies have shown no correlation between the degree of EGFR expression and the therapeutic responses to these drugs [66-68]. Thus, immunohistochemical expression of EGFR is not considered a predictor of response to EGFR-targeted drugs, and a number of recent studies do not include EGFR expression in selection criteria for anti-EGFR targeted therapy. However, in Korea, EGFR IHC has been routinely performed on CRC tissues of patients with stage IV CRC who are candidates for EGFR-targeted therapy according to the reimbursement criteria proposed by the Health Insurance Review and Evaluation Center, which mandates patient selection based on EGFR testing prior to application of EGFR-targeted therapy. In conclusion, whether immunohistochemical expression of EGFR accurately predicts the patients who would benefit from EGFR-targeted drugs has not been demonstrated until now.
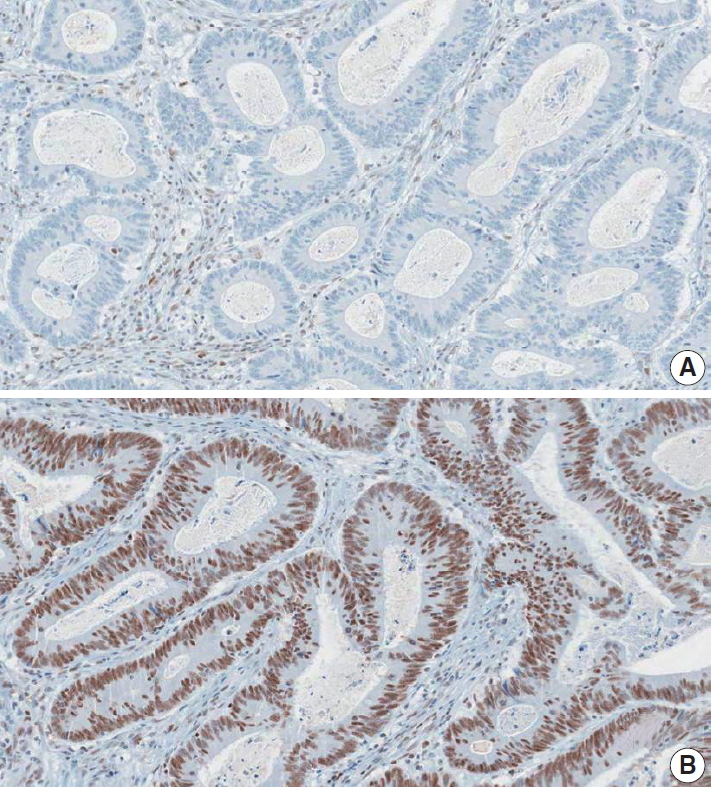
- DNA mismatch repair immunohistochemistry
- IHC for the detection of DNA mismatch repair (MMR) proteins in CRC samples is a simple and useful tool to determine MMR deficiency, which is caused by germline mutation in one of the MMR genes (MLH1, MSH2, MSH6, or PMS2) or promoter CpG island hypermethylation of the MLH1 gene [69-71]. MMR deficiency results in a high level of microsatellite instability (MSI-H) that is characterized by genome-wide length alterations of DNA microsatellite repeat sequences [72]. Because MLH1 dimerizes with PMS2 in order to conduct DNA MMR function, when a mutation or promoter hypermethylation in MLH1 occurs in CRC, IHC expression of both MLH1 and PMS2 is negative in the tumor [69,70]. Similarly, as MSH2 dimerizes with MSH6, MSH2-mutated CRCs show negativity for both MSH2 and MSH6 [69,70]. However, when mutations in PMS2 or MSH6 occur, expression of only PMS2 or MSH6, respectively, is lost, with the expression of MLH1 and MSH2 remaining intact [69,70].
- Nuclear staining should be observed for the IHC detection of MMR positivity. MMR deficiency is determined when the nuclear expression of at least one of the MMR proteins is not observed in tumor cells (Fig. 6).
- MMR IHC is a well-established histopathological screening tool for Lynch syndrome or sporadic MSI-H molecular subtype in CRCs [69-71]. Previous data and meta-analyses have shown that MMR deficiency (or MSI-H) in CRCs is significantly associated with both a better prognosis as well as resistance to 5-fluorouracil-based adjuvant chemotherapy [72-74]. Moreover, recent evidence has indicated that MMR deficiency (or MSI-H) is a significant predictor of a positive response to immunotherapy using immune checkpoint blockade in solid tumors [75,76]. Therefore, the pathologic reporting of MMR or microsatellite instability (MSI) status is strongly recommended for all surgically resected CRC cases.
- Immunoscore
- Tumor-infiltrating lymphocytes (TILs) in tumor tissue has emerged as a strong prognostic factor in CRC. Many previous studies have consistently shown that TIL count is a strong prognostic factor with a high TIL count being significantly associated with a better prognosis in CRC [77]. Several investigations have reported that TIL count can be a strong predictor of patient prognosis in CRC regardless of both TNM staging and MSI [78,79]. The anti-tumor functions of TILs are conducted mainly by cytotoxic T cells. Thus, IHC for CD3+ and CD8+ T cells has been used as one of the major methods for the evaluation of TILs in CRC [78,80].
- Based on the accumulating data, a TIL-based methodology named “immunoscore” has been under development and validation since 2012 by an international consortium led by Dr. Jerome Galon (http://www.immunoscore.org) [80,81]. The steps for determining the immunoscore of a CRC are as follows: (1) selection of a representative tumor section, (2) IHC for CD3 and CD8 on the tumor section, (3) evaluation of CD3+ and CD8+ cell densities at two tumor areas–invasive margin (IM) and tumor center (TC), (4) dichotomous categorization (high vs. low) of each of the four CD3/CD8 variables (CD3+ IM, CD3+ TC, CD8+ IM, and CD8+ TC), (5) determination of the final immunoscore based on the four CD3/CD8 variables (e.g., no “high” variable indicates I0; one “high” variable indicates I1; two “high” variables indicate I2; three “high” variables indicate I3; four “high” variables indicate I4).
- Although there is strong evidence for the prognostic significance of the immunoscore in CRC, there is still a lack of global consensus regarding the application of immunoscore in terms of indication, evaluation, and classification. One of the critical limitations of the current immunoscoring system is the absence of a standard cut-off value for the high versus low categorization of CD3+ or CD8+ cell density. It is expected that a consensus established from digitalized image-based, automated analyses will aid the establishment of a standardized immunoscoring system.
- Microsatellite instability
- MSI is a condition of genome-wide alterations in the number of repeat nucleotide(s) caused by a defective mismatch repair (dMMR) system in the context of germline mutations in mismatch repair genes, including MLH1, MSH2, MSH6, and PMS2, or MLH1 promoter hypermethylation [72]. MSI testing is recommended for all CRC patients for the screening of Lynch syndrome in NCCN guidelines and guidelines from the American Society for Clinical Pathology (ASCP)/College of American Pathologists (CAP)/Association for Molecular Pathology (AMP)/American Society of Clinical Oncology (ASCO) [82]. Moreover, MSI-H is associated with better prognosis but poor therapeutic response to 5-fluorouracil-based cytotoxic chemotherapy [83,84]. Recently, MSI-H is considered as a predictive marker for PD-1 inhibitor-based cancer immunotherapy [75,85].
- The gold standard method to evaluate MSI is the capillary gel electrophoresis, which compares the length in polymerase chain reaction (PCR) products of mono- or di-nucleotide repeats between cancer tissue and normal tissue. The Bethesda panel is composed of two mononucleotide repeat markers (BAT-25 and BAT-26) and three dinucleotide repeat markers (D5S346, D2S123, and D17S250), while the quasimonomorphic mononucleotides panel is composed of five mononucleotide repeat markers (NR-21, NR-24, NR-27 [or Mono-27], BAT-25, and BAT-26) [86,87]. Real-time PCR can be an alternative method for MSI evaluation in quasimonomorphic mononucleotides panel. Cancers classified as MSI-H should undergo immunohistochemistry of mismatch repair genes to screen for Lynch syndrome. If the BRAF V600E mutation is detected in MSI-H CRCs with MLH1 loss, Lynch syndrome can be ruled out [88]. Because MSI corresponds to dMMR, immunohistochemistry of four mismatch repair proteins (MLH1, MSH2, MSH6, and PMS2) could be acceptable for an alternative method to capillary gel electrophoresis. The results of the MSI testing using the Bethesda panel are reported as MSI-H, MSI-low, and MSI-stable (MSS) if the tumor show instability in at least two, only one, and none of the 5 markers, respectively [87]. In determination of MSI using the quasimonomorphic mononucleotide panel, there is a controversy regarding the cut-off of MSI-H (≥ 3/5 or ≥ 2/5) [89,90].
- KRAS and NRAS mutation analysis
- The extended RAS mutation test is a molecular test for the detection of mutations in exons 2 to 4 of KRAS and NRAS genes [82,91]. It is widely known that EGFR blockers improve survival in patients with metastatic CRCs. However, mutations of exons 2 to 4 of KRAS and NRAS genes are associated with resistance to EGFR blockers. Thus, European Society for Medical Oncology (ESMO) guidelines for metastatic CRCs, NCCN guidelines, and ASCP/CAP/AMP/ASCO guidelines recommend extended RAS mutation tests in patients with metastatic CRCs [82,91-93]. Besides, a point mutation of KRAS exon 2 is associated with poor prognosis in CRCs [94-98]. Sanger sequencing, pyrosequencing, and real-time PCR-based methods can be used for extended RAS mutation testing. Next generation sequencing (NGS) panels for solid tumors should include KRAS and NRAS tests in South Korea. The presence or absence of nucleotide and amino acid changes in KRAS and NRAS exons 2–4 should be reported with appropriate nomenclature.
- BRAF mutation analysis
- BRAF V600E mutations are observed in approximately twothirds of MSI-H CRCs caused by MLH1 promoter hypermethylation, however, it never occurs in Lynch syndrome [99]. Thus, if the MSI-H CRCs harbor the BRAF V600E mutation, we can exclude Lynch syndrome. Genetic tests for germline mutation of mismatch repair genes are not indicated in MSI-high CRCs with the BRAF V600E mutation [88].
- Of the molecular subtypes generated by MSI and BRAF/KRAS mutations, MSS CRCs with BRAF V600E mutations were associated with the worst prognosis. However, the association between BRAF V600E mutations and worse prognosis is weakened by the presence of MSI-H, because MSI-H CRCs with BRAF V600E mutations showed no difference in survival compared with MSS CRCs with wild-type KRAS/BRAF [95-98]. Hence, MSI tests and BRAF mutation tests should be performed in CRC patients. Two retrospective studies showed that the BRAF V600E mutation is associated with shorter relapse-free survival and overall survival in metastatic CRC patients that underwent liver resection [98,100].
- Some studies reported that the BRAF V600E mutation is associated with poor therapeutic response to EGFR blockers. However, it is still controversial whether the BRAF V600E mutation is an independent predictive marker for EGFR blockers [101,102]. 2017 National Comprehensive Cancer Network (NCCN) guidelines recommend BRAF V600E mutation testing for metastatic CRC patients; however, ASCP/CAP/AMP/ASCO and ESMO guidelines for metastatic CRCs do not recommend BRAF V600E mutation testing for metastatic CRC [82,91].
- Sanger sequencing, pyrosequencing, and real-time PCR-based methods can be used for BRAF mutation testing. NGS panels for solid tumors should include BRAF tests in South Korea. The presence or absence of nucleotide and amino acid changes in BRAF exon 15 should be reported. Appropriate nomenclature should be used.
CONDITIONAL DATA ELEMENTS FOR RESECTED COLORECTUM
Supplementary Materials
Author contributions
Conceptualization: BHK, JMK, GHK, HJC, DWK, JHK, JMB, ANS, HSP, YKK, KHL, MYC, IGD, HSL, HKC, JHS, MSC, ESJ, SYJ, EY, HSH.
Project administration: BHK, JMK, GHK, HJC, DYP.
Supervision: JMK, GHK, HJC, SYJ, ESJ, YWK, MSC, JHS, EY.
Writing—original draft preparation: HSP, ANS, JHK, IGD, YKK, MYC, JMK, DWK, JMB, BHK, HSL, KHL.
Writing—review & editing: BHK, JMK, GHK, HJC, DWK, JHK, JMB, ANS, HSP, YKK, KHL, MYC, IGD, HSL, HKC, DYP, HJK, JHS, MSC, ESJ, SYJ, EY, HSH, YWK.
Conflicts of Interest
G.H.K., J.H.K., and H.S.L., contributing editors of the Journal of Pathology and Translational Medicine, were not involved in the editorial evaluation or decision to publish this article. All remaining authors have declared no conflicts of interest.
Funding
No funding to declare.
- 1. Chang HJ, Park CK, Kim WH, et al. A standardized pathology report for colorectal cancer. Korean J Pathol 2006; 40: 193-203.
- 2. Ministry of Health and Welfare. Annual report of cancer statistics in Korea in 2015. Sejong: Ministry of Health and Welfare, 2017.
- 3. Kakar S, Shi C, Berho ME, et al. Protocol for the examination of specimens from patients with primary carcinoma of the colon and rectum, version 4.0.0.0. Illinois: College of American Pathologists, 2017.
- 4. Amin MB, Edge S, Greene F, et al. AJCC cancer staging system. 8th ed. New York: Springer, 2017.
- 5. WHO Classification of Tumours Editorial Board. WHO classification of tumours: digestive system tumours. 5th ed. Geneva: World Health Organization, 2019.
- 6. Fritz AG, Percy C, Jack A, et al. International classification of diseases for oncology (ICD-O). 3rd ed. 1st rev. Lyon: International Agency for Research on Cancer, 2013.
- 7. Langman G, Loughrey M, Shepherd N, Quirke P. Association of Coloproctology of Great Britain & Ireland (ACPGBI): guidelines for the management of cancer of the colon, rectum and anus (2017)-pathology standards and datasets. Colorectal Dis 2017; 19 Suppl 1: 74-81. PubMed
- 8. Nagtegaal I, Gaspar C, Marijnen C, Van De Velde C, Fodde R, Van Krieken H. Morphological changes in tumour type after radiotherapy are accompanied by changes in gene expression profile but not in clinical behaviour. J Pathol 2004; 204: 183-92. ArticlePubMed
- 9. Verdu M, Roman R, Calvo M, et al. Clinicopathological and molecular characterization of colorectal micropapillary carcinoma. Mod Pathol 2011; 24: 729-38. ArticlePubMedPDF
- 10. Lee HJ, Eom DW, Kang GH, et al. Colorectal micropapillary carcinomas are associated with poor prognosis and enriched in markers of stem cells. Mod Pathol 2013; 26: 1123-31. ArticlePubMedPDF
- 11. Nassar H. Carcinomas with micropapillary morphology: clinical significance and current concepts. Adv Anat Pathol 2004; 11: 297-303. PubMed
- 12. Xu F, Xu J, Lou Z, et al. Micropapillary component in colorectal carcinoma is associated with lymph node metastasis in T1 and T2 Stages and decreased survival time in TNM stages I and II. Am J Surg Pathol 2009; 33: 1287-92. ArticlePubMed
- 13. Haupt B, Ro JY, Schwartz MR, Shen SS. Colorectal adenocarcinoma with micropapillary pattern and its association with lymph node metastasis. Mod Pathol 2007; 20: 729-33. ArticlePubMedPDF
- 14. Jakubowska K, Guzinska-Ustymowicz K, Pryczynicz A. Invasive micropapillary component and its clinico-histopathological significance in patients with colorectal cancer. Oncol Lett 2016; 12: 1154-8. ArticlePubMedPMC
- 15. Tuppurainen K, Makinen JM, Junttila O, et al. Morphology and microsatellite instability in sporadic serrated and non-serrated colorectal cancer. J Pathol 2005; 207: 285-94. ArticlePubMed
- 16. Patai AV, Molnár B, Tulassay Z, Sipos F. Serrated pathway: alternative route to colorectal cancer. World J Gastroenterol 2013; 19: 607-15. ArticlePubMedPMC
- 17. Mäkinen MJ. Colorectal serrated adenocarcinoma. Histopathology 2007; 50: 131-50. ArticlePubMed
- 18. Barresi V, Reggiani Bonetti L, Ieni A, Domati F, Tuccari G. Prognostic significance of grading based on the counting of poorly differentiated clusters in colorectal mucinous adenocarcinoma. Hum Pathol 2015; 46: 1722-9. ArticlePubMed
- 19. Bosman FT, Carneiro F, Hruban RH, Theise ND. WHO classification of tumours of the digestive system. 4th ed. Lyon: International Agency for Research on Cancer, 2010.
- 20. Kojima M, Shimazaki H, Iwaya K, et al. Intramucosal colorectal carcinoma with invasion of the lamina propria: a study by the Japanese Society for Cancer of the Colon and Rectum. Hum Pathol 2017; 66: 230-7. ArticlePubMed
- 21. Panarelli NC, Schreiner AM, Brandt SM, Shepherd NA, Yantiss RK. Histologic features and cytologic techniques that aid pathologic stage assessment of colonic adenocarcinoma. Am J Surg Pathol 2013; 37: 1252-8. ArticlePubMed
- 22. Uehara K, Nakanishi Y, Shimoda T, Taniguchi H, Akasu T, Moriya Y. Clinicopathological significance of microscopic abscess formation at the invasive margin of advanced low rectal cancer. Br J Surg 2007; 94: 239-43. ArticlePubMedPDF
- 23. Smith KD, Tan D, Das P, et al. Clinical significance of acellular mucin in rectal adenocarcinoma patients with a pathologic complete response to preoperative chemoradiation. Ann Surg 2010; 251: 261-4. ArticlePubMed
- 24. Kang CM, Lim SB, Hong SM, et al. Prevalence and clinical significance of cellular and acellular mucin in patients with locally advanced mucinous rectal cancer who underwent preoperative chemoradiotherapy followed by radical surgery. Colorectal Dis 2016; 18: O10-6. ArticlePubMed
- 25. Kitajima K, Fujimori T, Fujii S, et al. Correlations between lymph node metastasis and depth of submucosal invasion in submucosal invasive colorectal carcinoma: a Japanese collaborative study. J Gastroenterol 2004; 39: 534-43. ArticlePubMedPDF
- 26. Bosch SL, Teerenstra S, de Wilt JH, Cunningham C, Nagtegaal ID. Predicting lymph node metastasis in pT1 colorectal cancer: a systematic review of risk factors providing rationale for therapy decisions. Endoscopy 2013; 45: 827-34. ArticlePubMedPDF
- 27. Haggitt RC, Glotzbach RE, Soffer EE, Wruble LD. Prognostic factors in colorectal carcinomas arising in adenomas: implications for lesions removed by endoscopic polypectomy. Gastroenterology 1985; 89: 328-36. ArticlePubMed
- 28. Kikuchi R, Takano M, Takagi K, et al. Management of early invasive colorectal cancer: risk of recurrence and clinical guidelines. Dis Colon Rectum 1995; 38: 1286-95. PubMed
- 29. Watanabe T, Muro K, Ajioka Y, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2016 for the treatment of colorectal cancer. Int J Clin Oncol 2018; 23: 1-34. ArticlePubMedPDF
- 30. Betge J, Pollheimer MJ, Lindtner RA, et al. Intramural and extramural vascular invasion in colorectal cancer: prognostic significance and quality of pathology reporting. Cancer 2012; 118: 628-38. ArticlePubMed
- 31. Kim WH, Park CK, Kim YB, et al. A standardized pathology report for gastric cancer. Korean J Pathol 2005; 39: 106-13.
- 32. Liebig C, Ayala G, Wilks J, et al. Perineural invasion is an independent predictor of outcome in colorectal cancer. J Clin Oncol 2009; 27: 5131-7. ArticlePubMedPMC
- 33. Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer 2009; 115: 3379-91. ArticlePubMed
- 34. Gibson JA, Odze RD. Pathology of premalignant colorectal neoplasia. Dig Endosc 2016; 28: 312-23. ArticlePubMed
- 35. Rex DK, Ahnen DJ, Baron JA, et al. Serrated lesions of the colorectum: review and recommendations from an expert panel. Am J Gastroenterol 2012; 107: 1315-29. ArticlePubMedPMCPDF
- 36. Bateman AC, Shepherd NA. UK guidance for the pathological reporting of serrated lesions of the colorectum. J Clin Pathol 2015; 68: 585-91. ArticlePubMed
- 37. Liu C, Walker NI, Leggett BA, Whitehall VL, Bettington ML, Rosty C. Sessile serrated adenomas with dysplasia: morphological patterns and correlations with MLH1 immunohistochemistry. Mod Pathol 2017; 30: 1728-38. ArticlePubMedPMCPDF
- 38. Chetty R, Hafezi-Bakhtiari S, Serra S, Colling R, Wang LM. Traditional serrated adenomas (TSAs) admixed with other serrated (socalled precursor) polyps and conventional adenomas: a frequent occurrence. J Clin Pathol 2015; 68: 270-3. ArticlePubMed
- 39. Anwar MA, D'Souza F, Coulter R, Memon B, Khan IM, Memon MA. Outcome of acutely perforated colorectal cancers: experience of a single district general hospital. Surg Oncol 2006; 15: 91-6. ArticlePubMed
- 40. Mitrovic B, Schaeffer DF, Riddell RH, Kirsch R. Tumor budding in colorectal carcinoma: time to take notice. Mod Pathol 2012; 25: 1315-25. ArticlePubMedPDF
- 41. Choi DH, Sohn DK, Chang HJ, Lim SB, Choi HS, Jeong SY. Indications for subsequent surgery after endoscopic resection of submucosally invasive colorectal carcinomas: a prospective cohort study. Dis Colon Rectum 2009; 52: 438-45. PubMed
- 42. Ueno H, Mochizuki H, Hashiguchi Y, et al. Risk factors for an adverse outcome in early invasive colorectal carcinoma. Gastroenterology 2004; 127: 385-94. ArticlePubMed
- 43. Wang LM, Kevans D, Mulcahy H, et al. Tumor budding is a strong and reproducible prognostic marker in T3N0 colorectal cancer. Am J Surg Pathol 2009; 33: 134-41. ArticlePubMed
- 44. Giger OT, Comtesse SC, Lugli A, Zlobec I, Kurrer MO. Intra-tumoral budding in preoperative biopsy specimens predicts lymph node and distant metastasis in patients with colorectal cancer. Mod Pathol 2012; 25: 1048-53. ArticlePubMedPDF
- 45. Rogers AC, Gibbons D, Hanly AM, et al. Prognostic significance of tumor budding in rectal cancer biopsies before neoadjuvant therapy. Mod Pathol 2014; 27: 156-62. ArticlePubMedPDF
- 46. Lugli A, Kirsch R, Ajioka Y, et al. Recommendations for reporting tumor budding in colorectal cancer based on the International Tumor Budding Consensus Conference (ITBCC) 2016. Mod Pathol 2017; 30: 1299-311. PubMedPDF
- 47. Koelzer VH, Zlobec I, Berger MD, et al. Tumor budding in colorectal cancer revisited: results of a multicenter interobserver study. Virchows Arch 2015; 466: 485-93. ArticlePubMedPDF
- 48. Koelzer VH, Assarzadegan N, Dawson H, et al. Cytokeratinbased assessment of tumour budding in colorectal cancer: analysis in stage II patients and prospective diagnostic experience. J Pathol Clin Res 2017; 3: 171-8. ArticlePubMedPMCPDF
- 49. Jass JR, Love SB, Northover JM. A new prognostic classification of rectal cancer. Lancet 1987; 1: 1303-6. ArticlePubMed
- 50. Bosch SL, Nagtegaal ID. The importance of the pathologist’s role in assessment of the quality of the mesorectum. Curr Colorectal Cancer Rep 2012; 8: 90-8. ArticlePubMedPMC
- 51. Aklilu M, Eng C. The current landscape of locally advanced rectal cancer. Nat Rev Clin Oncol 2011; 8: 649-59. ArticlePubMedPDF
- 52. Bibeau F, Rullier A, Jourdan MF, et al. Locally advanced rectal cancer management: which role for the pathologist in 2011? Ann Pathol 2011; 31: 433-41. PubMed
- 53. Dhadda AS, Dickinson P, Zaitoun AM, Gandhi N, Bessell EM. Prognostic importance of Mandard tumour regression grade following pre-operative chemo/radiotherapy for locally advanced rectal cancer. Eur J Cancer 2011; 47: 1138-45. ArticlePubMed
- 54. Mihaylova I, Parvanova V, Velikova C, Kurteva G, Ivanova D. Degree of tumor regression after preoperative chemo-radiotherapy in locally advanced rectal cancer-Preliminary results. Rep Pract Oncol Radiother 2011; 16: 237-42. ArticlePubMedPMC
- 55. Vallböhmer D, Bollschweiler E, Brabender J, et al. Evaluation of histological regression grading systems in the neoadjuvant therapy of rectal cancer: do they have prognostic impact? Int J Colorectal Dis 2012; 27: 1295-301. ArticlePubMedPDF
- 56. Kim SH, Chang HJ, Kim DY, et al. What is the ideal tumor regression grading system in rectal cancer patients after preoperative chemoradiotherapy? Cancer Res Treat 2016; 48: 998-1009. ArticlePubMedPDF
- 57. Mandard AM, Dalibard F, Mandard JC, et al. Pathologic assessment of tumor regression after preoperative chemoradiotherapy of esophageal carcinoma: clinicopathologic correlations. Cancer 1994; 73: 2680-6. ArticlePubMed
- 58. Dworak O, Keilholz L, Hoffmann A. Pathological features of rectal cancer after preoperative radiochemotherapy. Int J Colorectal Dis 1997; 12: 19-23. ArticlePubMedPDF
- 59. Ryan R, Gibbons D, Hyland JM, et al. Pathological response following long-course neoadjuvant chemoradiotherapy for locally advanced rectal cancer. Histopathology 2005; 47: 141-6. ArticlePubMed
- 60. Krasinskas AM. EGFR Signaling in Colorectal Carcinoma. Patholog Res Int 2011; 2011: 932932.ArticlePubMedPMCPDF
- 61. Goldstein NS, Armin M. Epidermal growth factor receptor immunohistochemical reactivity in patients with American Joint Committee on Cancer Stage IV colon adenocarcinoma: implications for a standardized scoring system. Cancer 2001; 92: 1331-46. ArticlePubMed
- 62. McKay JA, Murray LJ, Curran S, et al. Evaluation of the epidermal growth factor receptor (EGFR) in colorectal tumours and lymph node metastases. Eur J Cancer 2002; 38: 2258-64. ArticlePubMed
- 63. Spano JP, Fagard R, Soria JC, Rixe O, Khayat D, Milano G. Epidermal growth factor receptor signaling in colorectal cancer: preclinical data and therapeutic perspectives. Ann Oncol 2005; 16: 189-94. ArticlePubMedPDF
- 64. Resnick MB, Routhier J, Konkin T, Sabo E, Pricolo VE. Epidermal growth factor receptor, c-MET, beta-catenin, and p53 expression as prognostic indicators in stage II colon cancer: a tissue microarray study. Clin Cancer Res 2004; 10: 3069-75. PubMed
- 65. de Castro-Carpeno J, Belda-Iniesta C, Casado Saenz E, Hernandez Agudo E, Feliu Batlle J, Gonzalez Baron M. EGFR and colon cancer: a clinical view. Clin Transl Oncol 2008; 10: 6-13. ArticlePubMedPDF
- 66. Saltz LB, Meropol NJ, Loehrer PJ Sr, Needle MN, Kopit J, Mayer RJ. Phase II trial of cetuximab in patients with refractory colorectal cancer that expresses the epidermal growth factor receptor. J Clin Oncol 2004; 22: 1201-8. ArticlePubMed
- 67. Vallböhmer D, Zhang W, Gordon M, et al. Molecular determinants of cetuximab efficacy. J Clin Oncol 2005; 23: 3536-44. ArticlePubMed
- 68. Ogino S, Meyerhardt JA, Cantor M, et al. Molecular alterations in tumors and response to combination chemotherapy with gefitinib for advanced colorectal cancer. Clin Cancer Res 2005; 11: 6650-6. ArticlePubMedPDF
- 69. Geiersbach KB, Samowitz WS. Microsatellite instability and colorectal cancer. Arch Pathol Lab Med 2011; 135: 1269-77. ArticlePubMedPDF
- 70. Pino MS, Chung DC. Microsatellite instability in the management of colorectal cancer. Expert Rev Gastroenterol Hepatol 2011; 5: 385-99. ArticlePubMed
- 71. Samowitz WS. Evaluation of colorectal cancers for Lynch syndrome: practical molecular diagnostics for surgical pathologists. Mod Pathol 2015; 28 Suppl 1: S109-13. ArticlePubMedPDF
- 72. Boland CR, Goel A. Microsatellite instability in colorectal cancer. Gastroenterology 2010; 138: 2073-87. ArticlePubMedPMC
- 73. Guastadisegni C, Colafranceschi M, Ottini L, Dogliotti E. Microsatellite instability as a marker of prognosis and response to therapy: a meta-analysis of colorectal cancer survival data. Eur J Cancer 2010; 46: 2788-98. ArticlePubMed
- 74. Pritchard CC, Grady WM. Colorectal cancer molecular biology moves into clinical practice. Gut 2011; 60: 116-29. ArticlePubMed
- 75. Le DT, Uram JN, Wang H, et al. PD-1 blockade in tumors with mismatch-repair deficiency. N Engl J Med 2015; 372: 2509-20. PubMedPMC
- 76. Le DT, Durham JN, Smith KN, et al. Mismatch repair deficiency predicts response of solid tumors to PD-1 blockade. Science 2017; 357: 409-13. PubMedPMC
- 77. Roxburgh CS, McMillan DC. The role of the in situ local inflammatory response in predicting recurrence and survival in patients with primary operable colorectal cancer. Cancer Treat Rev 2012; 38: 451-66. ArticlePubMed
- 78. Kirilovsky A, Marliot F, El Sissy C, Haicheur N, Galon J, Pages F. Rational bases for the use of the Immunoscore in routine clinical settings as a prognostic and predictive biomarker in cancer patients. Int Immunol 2016; 28: 373-82. ArticlePubMedPMCPDF
- 79. Mlecnik B, Bindea G, Angell HK, et al. Integrative analyses of colorectal cancer show immunoscore is a stronger predictor of patient survival than microsatellite instability. Immunity 2016; 44: 698-711. ArticlePubMed
- 80. Galon J, Mlecnik B, Bindea G, et al. Towards the introduction of the ‘Immunoscore’ in the classification of malignant tumours. J Pathol 2014; 232: 199-209. ArticlePubMedPDF
- 81. Galon J, Pagès F, Marincola FM, et al. Cancer classification using the Immunoscore: a worldwide task force. J Transl Med 2012; 10: 205.PubMedPMCPDF
- 82. Sepulveda AR, Hamilton SR, Allegra CJ, et al. Molecular biomarkers for the evaluation of colorectal cancer: guideline from the American Society for Clinical Pathology, College of American Pathologists, Association for Molecular Pathology, and the American Society of Clinical Oncology. J Clin Oncol 2017; 35: 1453-86. ArticlePubMed
- 83. Zaanan A, Shi Q, Taieb J, et al. Role of deficient DNA mismatch repair status in patients with stage III colon cancer treated with FOLFOX adjuvant chemotherapy: a pooled analysis from 2 randomized clinical trials. JAMA Oncol 2018; 4: 379-83. ArticlePubMed
- 84. Sargent DJ, Marsoni S, Monges G, et al. Defective mismatch repair as a predictive marker for lack of efficacy of fluorouracil-based adjuvant therapy in colon cancer. J Clin Oncol 2010; 28: 3219-26. PubMedPMC
- 85. Overman MJ, McDermott R, Leach JL, et al. Nivolumab in patients with metastatic DNA mismatch repair-deficient or microsatellite instability-high colorectal cancer (CheckMate 142): an open-label, multicentre, phase 2 study. Lancet Oncol 2017; 18: 1182-91. ArticlePubMedPMC
- 86. Umar A, Boland CR, Terdiman JP, et al. Revised Bethesda Guidelines for hereditary nonpolyposis colorectal cancer (Lynch syndrome) and microsatellite instability. J Natl Cancer Inst 2004; 96: 261-8. PubMedPMCPDF
- 87. Boland CR, Thibodeau SN, Hamilton SR, et al. A National Cancer Institute Workshop on Microsatellite Instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 1998; 58: 5248-57. PubMed
- 88. Adar T, Rodgers LH, Shannon KM, et al. A tailored approach to BRAF and MLH1 methylation testing in a universal screening program for Lynch syndrome. Mod Pathol 2017; 30: 440-7. ArticlePDF
- 89. Buhard O, Cattaneo F, Wong YF, et al. Multipopulation analysis of polymorphisms in five mononucleotide repeats used to determine the microsatellite instability status of human tumors. J Clin Oncol 2006; 24: 241-51. ArticlePubMed
- 90. Goel A, Nagasaka T, Hamelin R, Boland CR. An optimized pentaplex PCR for detecting DNA mismatch repair-deficient colorectal cancers. PLoS One 2010; 5: e9393. ArticlePubMedPMC
- 91. Van Cutsem E, Cervantes A, Adam R, et al. ESMO consensus guidelines for the management of patients with metastatic colorectal cancer. Ann Oncol 2016; 27: 1386-422. PubMedPDF
- 92. Amado RG, Wolf M, Peeters M, et al. Wild-type KRAS is required for panitumumab efficacy in patients with metastatic colorectal cancer. J Clin Oncol 2008; 26: 1626-34. ArticlePubMed
- 93. Douillard JY, Oliner KS, Siena S, et al. Panitumumab-FOLFOX4 treatment and RAS mutations in colorectal cancer. N Engl J Med 2013; 369: 1023-34. ArticlePubMed
- 94. Rui Y, Wang C, Zhou Z, Zhong X, Yu Y. K-Ras mutation and prognosis of colorectal cancer: a meta-analysis. Hepatogastroenterology 2015; 62: 19-24. PubMed
- 95. Phipps AI, Limburg PJ, Baron JA, et al. Association between molecular subtypes of colorectal cancer and patient survival. Gastroenterology 2015; 148: 77-87. ArticlePubMed
- 96. Sinicrope FA, Shi Q, Smyrk TC, et al. Molecular markers identify subtypes of stage III colon cancer associated with patient outcomes. Gastroenterology 2015; 148: 88-99. ArticlePubMed
- 97. Taieb J, Le Malicot K, Shi Q, et al. Prognostic value of BRAF and KRAS mutations in MSI and MSS stage III colon cancer. J Natl Cancer Inst 2017; 109: djw272.ArticlePubMed
- 98. Schirripa M, Bergamo F, Cremolini C, et al. BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. Br J Cancer 2015; 112: 1921-8. ArticlePubMedPMCPDF
- 99. Wang L, Cunningham JM, Winters JL, et al. BRAF mutations in colon cancer are not likely attributable to defective DNA mismatch repair. Cancer Res 2003; 63: 5209-12. PubMed
- 100. Loes IM, Immervoll H, Sorbye H, et al. Impact of KRAS, BRAF, PIK3CA, TP53 status and intraindividual mutation heterogeneity on outcome after liver resection for colorectal cancer metastases. Int J Cancer 2016; 139: 647-56. PubMedPMC
- 101. Di Nicolantonio F, Martini M, Molinari F, et al. Wild-type BRAF is required for response to panitumumab or cetuximab in metastatic colorectal cancer. J Clin Oncol 2008; 26: 5705-12. ArticlePubMed
- 102. Pietrantonio F, Petrelli F, Coinu A, et al. Predictive role of BRAF mutations in patients with advanced colorectal cancer receiving cetuximab and panitumumab: a meta-analysis. Eur J Cancer 2015; 51: 587-94. ArticlePubMed
REFERENCES
Figure & Data
References
Citations

- Proteogenomic profiling predicts outcomes of adjuvant chemotherapy in extrahepatic cholangiocarcinoma
Hyehyun Jeong, Ji-Hye Oh, Hee-Sung Ahn, Baek-Yeol Ryoo, Kyu-pyo Kim, Jae Ho Jeong, Inkeun Park, Dae Wook Hwang, Jae Hoon Lee, Ki Byung Song, Woohyung Lee, Ki-Hun Kim, Deog-Bog Moon, Gi Won Song, Dong-Hwan Jung, Seung-Mo Hong, Chae Won Park, In-Pyo Baek, Y
Journal of Hepatology.2026; 84(1): 122. CrossRef - A study on the effect of CBSM-based psychological intervention on self-management ability and quality of life in colorectal cancer patients from the perspective of benefit finding: A quasi-experimental study
Linzhi Jiang, Zhouyuan Peng, Rongrong Liu, Lei Chen, Yang Wu, Xingqun Tan, Fan Wang, Liyuan Sun, Chong-Chi Chiu
PLOS One.2026; 21(1): e0339472. CrossRef - Impact of gross tumor morphology on the clinical outcomes of colon cancer: multicenter retrospective cohort study
So Jung Han, Hyun Seok Lee, Byung Ik Jang, Jae Hyun Kim, Hyun Gun Kim, Il Hyun Baek, Jun Lee, Bun Kim, Dae Bum Kim, Jae Jun Park
International Journal of Colorectal Disease.2026;[Epub] CrossRef - Diagnostic accuracy and pitfalls of MRI for restaging locally advanced rectal cancer in patients following anti-PD1 therapy plus neoadjuvant chemoradiotherapy: a multicenter study
Lixue Xu, Liting Sun, Yuhuan Fu, Guangyong Chen, Hongwei Yao, Zhenchang Wang, Zhenghan Yang, Jie Zhang
Abdominal Radiology.2025; 51(1): 14. CrossRef - Unraveling the role of perineural invasion in cancer progression across multiple tumor types
Muqtada Shaikh, Sanket Shirodkar, Gaurav Doshi
Medical Oncology.2025;[Epub] CrossRef - MALT lymphoma affecting the oral cavity: a clinical, pathologic and genetic study of MALT1 gene translocation
Juan Manuel Arteaga Legarrea, Mauro Lima dos Santos, Nathalia Gomes Rodrigues, Ricardo Santiago Gomez, Ricardo Alves Mesquita, Silvia Ferreira de Sousa, Cinthia Verónica Bardález López de Cáceres, Hélder Antônio Rebelo Pontes, Pablo Agustin Vargas, Luiz A
Oral Surgery, Oral Medicine, Oral Pathology and Oral Radiology.2025; 140(6): 740. CrossRef - Additional staining for lymphovascular invasion is associated with increased estimation of lymph node metastasis in patients with T1 colorectal cancer: Systematic review and meta‐analysis
Jun Watanabe, Katsuro Ichimasa, Yuki Kataoka, Atsushi Miki, Hidehiro Someko, Munenori Honda, Makiko Tahara, Takeshi Yamashina, Khay Guan Yeoh, Shigeo Kawai, Kazuhiko Kotani, Naohiro Sata
Digestive Endoscopy.2024; 36(5): 533. CrossRef - The use of core descriptors from the ENiGMA code study in recent literature: a systematic review
Saher‐Zahra Khan, Andrea Arline, Kate M. Williams, Matthew J. Lee, Emily Steinhagen, Sharon L. Stein
Colorectal Disease.2024; 26(3): 428. CrossRef - Efficacy and safety of PD-1 blockade plus long-course chemoradiotherapy in locally advanced rectal cancer (NECTAR): a multi-center phase 2 study
Zhengyang Yang, Jiale Gao, Jianyong Zheng, Jiagang Han, Ang Li, Gang Liu, Yi Sun, Jie Zhang, Guangyong Chen, Rui Xu, Xiao Zhang, Yishan Liu, Zhigang Bai, Wei Deng, Wei He, Hongwei Yao, Zhongtao Zhang
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Diagnostic Accuracy of Highest-Grade or Predominant Histological Differentiation of T1 Colorectal Cancer in Predicting Lymph Node Metastasis: A Systematic Review and Meta-Analysis
Jun Watanabe, Katsuro Ichimasa, Yuki Kataoka, Shoko Miyahara, Atsushi Miki, Khay Guan Yeoh, Shigeo Kawai, Fernando Martínez de Juan, Isidro Machado, Kazuhiko Kotani, Naohiro Sata
Clinical and Translational Gastroenterology.2024; 15(3): e00673. CrossRef - Comparative evaluation of CT and MRI in the preoperative staging of colon cancer
Effrosyni Bompou, Aikaterini Vassiou, Ioannis Baloyiannis, Konstantinos Perivoliotis, Ioannis Fezoulidis, George Tzovaras
Scientific Reports.2024;[Epub] CrossRef - Pathologic Implications of Magnetic Resonance Imaging-detected Extramural Venous Invasion of Rectal Cancer
Hyun Gu Lee, Chan Wook Kim, Jong Keon Jang, Seong Ho Park, Young Il Kim, Jong Lyul Lee, Yong Sik Yoon, In Ja Park, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Clinical Colorectal Cancer.2023; 22(1): 129. CrossRef - A standardized pathology report for gastric cancer: 2nd edition
Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi,
Journal of Pathology and Translational Medicine.2023; 57(1): 1. CrossRef - IGFL2-AS1, a Long Non-Coding RNA, Is Associated with Radioresistance in Colorectal Cancer
Jeeyong Lee, Da Yeon Kim, Younjoo Kim, Ui Sup Shin, Kwang Seok Kim, Eun Ju Kim
International Journal of Molecular Sciences.2023; 24(2): 978. CrossRef - A Standardized Pathology Report for Gastric Cancer: 2nd Edition
Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi,
Journal of Gastric Cancer.2023; 23(1): 107. CrossRef - Incremental Detection Rate of Dysplasia and Sessile Serrated Polyps/Adenomas Using Narrow-Band Imaging and Dye Spray Chromoendoscopy in Addition to High-Definition Endoscopy in Patients with Long-Standing Extensive Ulcerative Colitis: Segmental Tandem End
Ji Eun Kim, Chang Wan Choi, Sung Noh Hong, Joo Hye Song, Eun Ran Kim, Dong Kyung Chang, Young-Ho Kim
Diagnostics.2023; 13(3): 516. CrossRef - Prognostic Impact of Extramural Lymphatic, Vascular, and Perineural Invasion in Stage II Colon Cancer: A Comparison With Intramural Invasion
Sang Sik Cho, Ji Won Park, Gyeong Hoon Kang, Jung Ho Kim, Jeong Mo Bae, Sae-Won Han, Tae-You Kim, Min Jung Kim, Seung-Bum Ryoo, Seung-Yong Jeong, Kyu Joo Park
Diseases of the Colon & Rectum.2023; 66(3): 366. CrossRef - Towards targeted colorectal cancer biopsy based on tissue morphology assessment by compression optical coherence elastography
Anton A. Plekhanov, Marina A. Sirotkina, Ekaterina V. Gubarkova, Elena B. Kiseleva, Alexander A. Sovetsky, Maria M. Karabut, Vladimir E. Zagainov, Sergey S. Kuznetsov, Anna V. Maslennikova, Elena V. Zagaynova, Vladimir Y. Zaitsev, Natalia D. Gladkova
Frontiers in Oncology.2023;[Epub] CrossRef - Is High-Grade Tumor Budding an Independent Prognostic Factor in Stage II Colon Cancer?
Jung Kyong Shin, Yoon Ah Park, Jung Wook Huh, Seong Hyeon Yun, Hee Cheol Kim, Woo Yong Lee, Seok Hyung Kim, Sang Yun Ha, Yong Beom Cho
Diseases of the Colon & Rectum.2023; 66(8): e801. CrossRef - Detection of Human cytomegalovirus UL55 Gene and IE/E Protein Expression in Colorectal Cancer Patients in Egypt
May Raouf, Ahmed A. Sabry, Mahinour A. Ragab, Samar El Achy, Amira Amer
BMC Cancer.2023;[Epub] CrossRef - Polo-like kinase 4 as a potential predictive biomarker of chemoradioresistance in locally advanced rectal cancer
Hyunseung Oh, Soon Gu Kim, Sung Uk Bae, Sang Jun Byun, Shin Kim, Jae-Ho Lee, Ilseon Hwang, Sun Young Kwon, Hye Won Lee
Journal of Pathology and Translational Medicine.2022; 56(1): 40. CrossRef - A Prediction Model for Tumor Recurrence in Stage II–III Colorectal Cancer Patients: From a Machine Learning Model to Genomic Profiling
Po-Chuan Chen, Yu-Min Yeh, Bo-Wen Lin, Ren-Hao Chan, Pei-Fang Su, Yi-Chia Liu, Chung-Ta Lee, Shang-Hung Chen, Peng-Chan Lin
Biomedicines.2022; 10(2): 340. CrossRef - Rationale and design of a prospective, multicenter, phase II clinical trial of safety and efficacy evaluation of long course neoadjuvant chemoradiotherapy plus tislelizumab followed by total mesorectal excision for locally advanced rectal cancer (NCRT-PD1
Zhengyang Yang, Xiao Zhang, Jie Zhang, Jiale Gao, Zhigang Bai, Wei Deng, Guangyong Chen, Yongbo An, Yishan Liu, Qi Wei, Jiagang Han, Ang Li, Gang Liu, Yi Sun, Dalu Kong, Hongwei Yao, Zhongtao Zhang
BMC Cancer.2022;[Epub] CrossRef - Potential of DEK proto‑oncogene as a prognostic biomarker for colorectal cancer: An evidence‑based review
Muhammad Habiburrahman, Muhammad Wardoyo, Stefanus Sutopo, Nur Rahadiani
Molecular and Clinical Oncology.2022;[Epub] CrossRef - Reproducibility and Feasibility of Classification and National Guidelines for Histological Diagnosis of Canine Mammary Gland Tumours: A Multi-Institutional Ring Study
Serenella Papparella, Maria Crescio, Valeria Baldassarre, Barbara Brunetti, Giovanni Burrai, Cristiano Cocumelli, Valeria Grieco, Selina Iussich, Lorella Maniscalco, Francesca Mariotti, Francesca Millanta, Orlando Paciello, Roberta Rasotto, Mariarita Roma
Veterinary Sciences.2022; 9(7): 357. CrossRef - Composite scoring system and optimal tumor budding cut-off number for estimating lymph node metastasis in submucosal colorectal cancer
Jeong-ki Kim, Ye-Young Rhee, Jeong Mo Bae, Jung Ho Kim, Seong-Joon Koh, Hyun Jung Lee, Jong Pil Im, Min Jung Kim, Seung-Bum Ryoo, Seung-Yong Jeong, Kyu Joo Park, Ji Won Park, Gyeong Hoon Kang
BMC Cancer.2022;[Epub] CrossRef - Automated Hybrid Model for Detecting Perineural Invasion in the Histology of Colorectal Cancer
Jiyoon Jung, Eunsu Kim, Hyeseong Lee, Sung Hak Lee, Sangjeong Ahn
Applied Sciences.2022; 12(18): 9159. CrossRef - Clinical Implication of Perineural and Lymphovascular Invasion in Rectal Cancer Patients Who Underwent Surgery After Preoperative Chemoradiotherapy
Young Il Kim, Chan Wook Kim, Jong Hoon Kim, Jihun Kim, Jun-Soo Ro, Jong Lyul Lee, Yong Sik Yoon, In Ja Park, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Diseases of the Colon & Rectum.2022; 65(11): 1325. CrossRef - Molecular Pathology of Gastric Cancer
Moonsik Kim, An Na Seo
Journal of Gastric Cancer.2022; 22(4): 264. CrossRef - Selective approach to arterial ligation in radical sigmoid colon cancer surgery with D3 lymph node dissection: A multicenter comparative study
Sergey Efetov, Albina Zubayraeva, Cüneyt Kayaalp, Alisa Minenkova, Yusuf Bağ, Aftandil Alekberzade, Petr Tsarkov
Turkish Journal of Surgery.2022; 38(4): 382. CrossRef - Evaluation of lncRNA FOXD2-AS1 Expression as a Diagnostic Biomarker in Colorectal Cancer
Hooman Shalmashi, Sahar Safaei, Dariush Shanehbandi, Milad Asadi, Soghra Bornehdeli, Abdolreza Mehdi Navaz
Reports of Biochemistry and Molecular Biology.2022; 11(3): 471. CrossRef - Improvement in the Assessment of Response to Preoperative Chemoradiotherapy for Rectal Cancer Using Magnetic Resonance Imaging and a Multigene Biomarker
Eunhae Cho, Sung Woo Jung, In Ja Park, Jong Keon Jang, Seong Ho Park, Seung-Mo Hong, Jong Lyul Lee, Chan Wook Kim, Yong Sik Yoon, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Cancers.2021; 13(14): 3480. CrossRef - Addition of V-Stage to Conventional TNM Staging to Create the TNVM Staging System for Accurate Prediction of Prognosis in Colon Cancer: A Multi-Institutional Retrospective Cohort Study
Jung Hoon Bae, Ji Hoon Kim, Jaeim Lee, Bong-Hyeon Kye, Sang Chul Lee, In Kyu Lee, Won Kyung Kang, Hyeon-Min Cho, Yoon Suk Lee
Biomedicines.2021; 9(8): 888. CrossRef - Gene Expression Profiles Associated with Radio-Responsiveness in Locally Advanced Rectal Cancer
Jeeyong Lee, Junhye Kwon, DaYeon Kim, Misun Park, KwangSeok Kim, InHwa Bae, Hyunkyung Kim, JoonSeog Kong, Younjoo Kim, UiSup Shin, EunJu Kim
Biology.2021; 10(6): 500. CrossRef - A Patient-Derived Organoid-Based Radiosensitivity Model for the Prediction of Radiation Responses in Patients with Rectal Cancer
Misun Park, Junhye Kwon, Joonseog Kong, Sun Mi Moon, Sangsik Cho, Ki Young Yang, Won Il Jang, Mi Sook Kim, Younjoo Kim, Ui Sup Shin
Cancers.2021; 13(15): 3760. CrossRef - Comparison between Local Excision and Radical Resection for the Treatment of Rectal Cancer in ypT0-1 Patients: An Analysis of the Clinicopathological Factors and Survival Rates
Soo Young Oh, In Ja Park, Young IL Kim, Jong-Lyul Lee, Chan Wook Kim, Yong Sik Yoon, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Cancers.2021; 13(19): 4823. CrossRef - Comparison of Vascular Invasion With Lymph Node Metastasis as a Prognostic Factor in Stage I-III Colon Cancer: An Observational Cohort Study
Jung Hoon Bae, Ji Hoon Kim, Bong-Hyeon Kye, Abdullah Al-Sawat, Chul Seung Lee, Seung-Rim Han, In Kyu Lee, Sung Hak Lee, Yoon Suk Lee
Frontiers in Surgery.2021;[Epub] CrossRef - Clinicopathological significance of Ki67 expression in colorectal cancer
Jing Li, Zhi-ye Liu, Hai-bo Yu, Qing Xue, Wen-jie He, Hai-tao Yu
Medicine.2020; 99(20): e20136. CrossRef - Lateral lymph node and its association with distant recurrence in rectal cancer: A clue of systemic disease
Young Il Kim, Jong Keon Jang, In Ja Park, Seong Ho Park, Jong Beom Kim, Jin-Hong Park, Tae Won Kim, Jun-Soo Ro, Seok-Byung Lim, Chang Sik Yu, Jin Cheon Kim
Surgical Oncology.2020; 35: 174. CrossRef - Transformation of Pathology Reports Into the Common Data Model With Oncology Module: Use Case for Colon Cancer
Borim Ryu, Eunsil Yoon, Seok Kim, Sejoon Lee, Hyunyoung Baek, Soyoung Yi, Hee Young Na, Ji-Won Kim, Rong-Min Baek, Hee Hwang, Sooyoung Yoo
Journal of Medical Internet Research.2020; 22(12): e18526. CrossRef
 PubReader
PubReader ePub Link
ePub Link-
 Cite this Article
Cite this Article
- Cite this Article
-
- Close
- Download Citation
- Close
- Figure
- Related articles






Fig. 1.
Fig. 2.
Fig. 3.
Fig. 4.
Fig. 5.
Fig. 6.
| Standard data elements | |||
|---|---|---|---|
| Specimen type | |||
| □ Right hemicolectomy | |||
| □ Transverse hemicolectomy | |||
| □ Left hemicolectomy | |||
| □ Anterior resection | |||
| □ Low anterior resection | |||
| □ Abdominoperineal resection | |||
| □ Subtotal/total colectomy | |||
| □ Total proctocolectomy | |||
| □ Transanal excision | |||
| □ Endoscopic mucosal resection | |||
| □ Other: (specify: ) | |||
| Histopathologic type of invasive carcinoma | |||
| □ Adenocarcinoma, NOS | |||
| □ Low-grade (well differentiated and moderately differentiated) | |||
| □ High-grade (poorly differentiated) | |||
| □ Mucinous adenocarcinoma | |||
| □ Signet ring cell carcinoma | |||
| □ Medullary carcinoma | |||
| □ Serrated adenocarcinoma | |||
| □ Micropapillary adenocarcinoma | |||
| □ Squamous cell (epidermoid) carcinoma (excluding upwardly spreading anal tumors) | |||
| □ Adenosquamous carcinoma | |||
| □ Small cell neuroendocrine carcinoma | |||
| □ Large cell neuroendocrine carcinoma | |||
| □ Mixed neuroendocrine-non-neuroendocrine neoplasm | |||
| □ Undifferentiated carcinoma | |||
| □ Other: (specify: ) | |||
| Location | |||
| □ Cecum | |||
| □ Ascending colon | |||
| □ Hepatic flexure | |||
| □ Transverse colon | |||
| □ Splenic flexure | |||
| □ Descending colon | |||
| □ Sigmoid colon | |||
| □ Rectosigmoid junction | |||
| □ Rectum | |||
| □ Other: (specify: ) | |||
| Gross type | |||
| □ Fungating/polypoid | |||
| □ Ulcerofungating | |||
| □ Ulceroinfiltrative | |||
| □ Infiltrative | |||
| □ Unclassifiable | |||
| Tumor size | |||
| × × cm | |||
| Depth of invasion | |||
| □ Intramucosal carcinoma (pTis) | |||
| □ Tumor invades the submucosa (pT1) | |||
| □ Tumor invades the muscularis propria (pT2) | |||
| □ Tumor invades through the muscularis propria into pericolorectal tissue (pT3) | |||
| □ Tumor invades through the visceral peritoneum (pT4a) | |||
| □ Tumor directly invades or adheres to adjacent organs or structures (pT4b) | |||
| - [Endoscopic excision (Endoscopic submucosal dissection/polypectomy) or transanal excision] | |||
| □ Tumor invades the lamina propria with no extension through muscularis mucosae (pTis) | |||
| □ Tumor invades the submucosa (pT1) | |||
| For sessile lesion: | |||
| Distance of tumor from muscularis mucosae: mm | |||
| For pedunculated lesion: | |||
| Haggitt level (head, neck, stalk, beyond stalk) | |||
| Distance of tumor invasion in stalk: mm | |||
| Resection margin | |||
| Proximal margin | |||
| □ Free from carcinoma | |||
| □ Involved by carcinoma | |||
| Distal margin | |||
| □ Free from carcinoma | |||
| □ Involved by carcinoma | |||
| Circumferential margin (rectum only) | |||
| □ Free from carcinoma | |||
| □ Involved by carcinoma | |||
| Safety margin: proximal cm, distal cm, circumferential cm | |||
| - [Endoscopic excision (Endoscopic mucosal resection/submucosal dissection/polypectomy) or transanal excision] | |||
| Deep margin | |||
| □ Free from carcinoma | |||
| □ Involved by carcinoma | |||
| □ Not applicable | |||
| Horizontal margin | |||
| □ Free from carcinoma | |||
| □ Involved by carcinoma | |||
| □ Involved by adenoma: (specify grade: ) | |||
| □ Not applicable | |||
| Safety margin: deep cm, horizontal cm | |||
| Regional lymph node metastasis | |||
| □ No metastasis in all regional lymph nodes (pN0) | |||
| □ Metastasis to out of regional lymph nodes pN | |||
| Lymphatic (small vessel) invasion | |||
| □ Not identified | |||
| □ Present | |||
| Venous invasion | |||
| □ Not identified | |||
| □ Present | |||
| □ Intramural | |||
| □ Extramural | |||
| Perineural invasion | |||
| □ Not identified | |||
| □ Present | |||
| Pre-existing adenoma | |||
| □ Absent | |||
| □ Tubular/Tubulovillous/Villous adenoma | |||
| Low grade dysplasia/High grade dysplasia | |||
| □ Sessile serrated lesion (sessile serrated adenoma/polyp) | |||
| □ Sessile serrated lesion (sessile serrated adenoma/polyp) with dysplasia | |||
| □ Traditional serrated adenoma | |||
| □ Other (specify: ) | |||
| Associated findings | |||
| □ Absent | |||
| □ Tumor perforation (pT4a) | |||
| □ Perforation (non-tumor perforation) | |||
| □ Metastasis to one site or organ without peritoneal metastasis (pM1a) | |||
| □ Metastasis to two or more sites or organs without peritoneal metastasis (pM1b) | |||
| □ Metastasis to the peritoneal surface with or without other site or organ metastasis (pM1c) | |||
| Specify metastatic sites or organs: | |||
| Separate lesions | |||
| □ Absent | |||
| □ Adenoma | |||
| □ Polyp | |||
| □ GIST | |||
| □ Ulcerative colitis/Crohn’s disease | |||
| □ Others | |||
| Specify: | |||
Conditional data elements |
|||
| Tumor budding | |||
| □ Not identified | |||
| □ Present | |||
| □ ≤ 4 buds (low) | |||
| □ 5–9 buds (intermediate) | |||
| □ ≥ 10 buds (high) | |||
| □ Cannot be assessed (specify: ) | |||
| Completeness of total mesorectal excision | |||
| □ Complete | |||
| □ Nearly complete | |||
| □ Incomplete | |||
| □ Cannot be determined | |||
| Preoperative chemoradiotherapy | |||
| □ Yes □ No □ Not known | |||
| If yes) Tumor regression grade | |||
| □ Grade 0: No viable cancer cells (complete response) | |||
| □ Grade 1: Single cells or rare small groups of cancer cells (near-complete response) | |||
| □ Grade 2: Residual cancer with evident tumor regression, but more than single cells or rare small groups of cancer cells (partial response) | |||
| □ Grade 3: Extensive residual cancer with no evident tumor regression (poor or no response) | |||
| DNA mismatch repair immunohistochemistry | |||
| MLH1: | □ Positive (retained expression) | ||
| □ Negative (loss of expression) | |||
| MSH2: | □ Positive (retained expression) | ||
| □ Negative (loss of expression) | |||
| PMS2: | □ Positive (retained expression) | ||
| □ Negative (loss of expression) | |||
| MSH6: | □ Positive (retained expression) | ||
| □ Negative (loss of expression) | |||
| Summary: DNA mismatch repair deficiency (was/was not) observed | |||
| Microsatellite instability (MSI) | |||
| Summary: | □ MSI-stable (MSS) | ||
| □ MSI-low (MSI-L) | |||
| □ MSI-high (MSI-H) | |||
| KRAS mutation analysis | |||
| □ No mutation detected | |||
| □ Mutation detected (specify: example: c.35G > A, p.Gly12Asp ) | |||
| NRAS mutation analysis | |||
| □ No mutation detected | |||
| □ Mutation detected (specify: example: c.35G>A, p.Gly12Asp ) | |||
| BRAF mutation analysis | |||
| □ No mutation detected | |||
| □ BRAF V600E (c.1799T > A) mutation | |||
| □ Other BRAF mutation (specify: ) | |||
Comment: This report is intended to be applicable to endoscopic resection or transanal excision specimens as well as surgical resection of CRC. NOS, not otherwise specified; CRC, colorectal cancer.

 E-submission
E-submission