Search
- Page Path
- HOME > Search
- International Academy of Cytology standardized reporting of breast fine-needle aspiration cytology with cyto-histopathological correlation of breast carcinoma
- Shweta Pai
- J Pathol Transl Med. 2024;58(5):241-248. Published online September 13, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.14
- 7,726 View
- 407 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The International Academy of Cytology (IAC) has developed a standardized approach for reporting the findings of breast fine-needle aspiration cytology (FNAC). Accordingly, there are five chief categories of breast lesions, C1 (insufficient material), C2 (benign), C3 (atypical), C4 (suspicious), and C5 (malignant). The prognostication and management of breast carcinoma can be performed readily on the basis of this classification system. The aim of this study was to classify various breast lesions into one of the above-named categories and to further grade the C5 lesions specifically using the Robinson system. The latter grades were then correlated with modified Scarff-Bloom-Richardson (SBR) grades.
Methods
This retrospective study was undertaken in the pathology department of a hospital located in the urban part of the city of Bangalore. All FNAC procedures performed on breast lumps spanning the year 2020 were included in the study.
Results
A total of 205 breast lesions was classified according to the IAC guidelines into C1 (6 cases, 2.9%), C2 (151 cases, 73.7%), C3 (13 cases, 6.3%), C4 (5 cases, 2.5%), and C5 (30 cases, 14.6%) groups. The C5 cases were further graded using Robinson’s system. The latter showed a significant correlation with the SBR system (concordance=83.3%, Spearman correlation=0.746, Kendall’s tau-b=0.736, kappa=0.661, standard error=0.095, p≤.001).
Conclusions
A standardized approach for FNAC reporting of breast lesions, as advocated for by the IAC, improves the quality and clarity of the reports and assures diagnostic reproducibility on a global scale. Further, the cytological grading of C5 lesions provides reliable cyto-prognostic scores that can help assess a tumor’s aggressiveness and predict its histological grade.
- Metastatic choroidal melanoma in the breast: a case report and review of the literature
- Loay Abudalu, Vinisha Malhotra, Nabila Nasir, Sami Titi
- J Pathol Transl Med. 2023;57(4):238-241. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.07
- 4,982 View
- 128 Download
-
 Abstract
Abstract
 PDF
PDF - The breast is an unusual site for metastases, accounting for less than 2% of malignant breast lesions but include those from malignant melanomas, carcinomas, sarcomas, and lymphomas from various organs. We diagnosed a very rare case of metastatic choroidal melanoma for a 67-year-old female who presented with a right breast lump and who had been previously diagnosed with choroidal melanoma-monosomy 3 in 2017. To the best of our knowledge, only five such cases have been published so far, with one in a male patient.
- Fatty acid synthetase expression in triple-negative breast cancer
- Jin Hee Park, Hye Seung Han, So Dug Lim, Wook Youn Kim, Kyoung Sik Park, Young Bum Yoo, Seung Eun Lee, Wan-Seop Kim
- J Pathol Transl Med. 2022;56(2):73-80. Published online January 21, 2022
- DOI: https://doi.org/10.4132/jptm.2021.10.27
- 7,535 View
- 204 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Triple-negative breast cancer (TNBC) has a relatively poor prognosis. Research has identified potential metabolic targets, including fatty acid metabolism, in TNBC. The absence of effective target therapies for TNBC led to exploration of the role of fatty acid synthetase (FASN) as a potential target for TNBC therapy. Here, we analyzed the expression of FASN, a representative lipid metabolism–related protein, and investigated the association between FASN expression and Ki-67 and the programmed death ligand 1 (PD-L1) biomarkers in TNBC.
Methods
Immunohistochemical expression of FASN was analyzed in 166 patients with TNBC. For analytical purposes, patients with 0–1+ FASN staining were grouped as low-grade FASN and patients with 2–3+ FASN staining as high-grade FASN.
Results
FASN expression was observed in 47.1% of TNBC patients. Low and high expression of FASN was identified in 75.9% and 24.1%, respectively, and no statistically significant difference was found in T category, N category, American Joint Committee on Cancer stage, or recurrence rate between the low and high-FASN expression groups. Ki-67 proliferation level was significantly different between the low and high-FASN expression groups. FASN expression was significantly related to Ki-67 as the level increased. There was no significant difference in PD-L1 positivity between the low- and high-FASN expression groups.
Conclusions
We identified FASN expression in 166 TNBC patients. The Ki-67 proliferation index was positively correlated with FASN level, indicating higher proliferation activity as FASN increases. However, there was no statistical association with PD-L1 SP142, the currently FDA-approved assay, or FASN expression level. -
Citations
Citations to this article as recorded by- Lipid metabolism involved in progression and drug resistance of breast cancer
Wenxiang Fu, Aijun Sun, Huijuan Dai
Genes & Diseases.2025; 12(4): 101376. CrossRef - Unveiling the impact of lipid metabolism on triple-negative breast cancer growth and treatment options
Xin-xian Cai, Zhe-zhong Zhang, Xiao-xiao Yang, Wen-rui Shen, Liu-wei Yuan, Xi Ding, Ying Yu, Wen-yu Cai
Frontiers in Oncology.2025;[Epub] CrossRef - Protein biomarkers for diagnosis of breast cancer
Emeka Eze Joshua Iweala, Doris Nnenna Amuji, Faith Chinasaokwu Nnaji
Scientific African.2024; 25: e02308. CrossRef - Microarray analysis points to LMNB1 and JUN as potential target genes for predicting metastasis promotion by etoposide in colorectal cancer
Jiafei Liu, Hongjie Yang, Peng Li, Yuanda Zhou, Zhichun Zhang, Qingsheng Zeng, Xipeng Zhang, Yi Sun
Scientific Reports.2024;[Epub] CrossRef - The signature of extracellular vesicles in hypoxic breast cancer and their therapeutic engineering
Baiheng Zhu, Kehao Xiang, Tanghua Li, Xin Li, Fujun Shi
Cell Communication and Signaling.2024;[Epub] CrossRef - NFYA promotes malignant behavior of triple-negative breast cancer in mice through the regulation of lipid metabolism
Nobuhiro Okada, Chihiro Ueki, Masahiro Shimazaki, Goki Tsujimoto, Susumu Kohno, Hayato Muranaka, Kiyotsugu Yoshikawa, Chiaki Takahashi
Communications Biology.2023;[Epub] CrossRef - Role of EGFR and FASN in breast cancer progression
Suchi Chaturvedi, Mainak Biswas, Sushabhan Sadhukhan, Avinash Sonawane
Journal of Cell Communication and Signaling.2023; 17(4): 1249. CrossRef - Bioinformatics Method Was Used to Analyze the Highly Expressed Gene FAM83A of Breast Cancer in Young Women
Yongzhe Tang, Hao Wang, Qi He, Yuanyuan Chen, Jie Wang, Fahd Abd Algalil
Applied Bionics and Biomechanics.2022; 2022: 1. CrossRef - NCAPH promotes proliferation as well as motility of breast cancer cells by activating the PI3K/AKT pathway
Ting Zhang, Peng Li, Wanying Guo, Qipeng Liu, Weiqiang Qiao, Miao Deng
Physiology International.2022;[Epub] CrossRef
- Lipid metabolism involved in progression and drug resistance of breast cancer
- Potential of AKT2 expression as a predictor of lymph-node metastasis in invasive breast carcinoma of no special type
- Primariadewi Rustamadji, Elvan Wiyarta, Kristina Anna Bethania, Kusmardi Kusmardi
- J Pathol Transl Med. 2021;55(4):271-278. Published online June 14, 2021
- DOI: https://doi.org/10.4132/jptm.2021.04.26
- 5,997 View
- 154 Download
- 3 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Invasive breast carcinoma of no special type (IBC-NST) is the most common type of breast cancer and mainly causes regional lymph-node metastasis (LNM). We investigated the potential for AKT2 expression as a predictive biomarker for LNM in IBC-NST.
Methods
Forty-eight paraffin blocks containing IBC-NST primary tumors were divided into two groups based on presence or absence of LNM. Age, tumor grade, tumor size, lymphovascular invasion (LVI), and AKT expression were assessed. AKT2 expression was assessed based on immunohistochemical staining, while other data were collected from archives.
Results
Multiple logistic regression results showed that AKT2 expression and LVI were significantly associated with LNM (odds ratio [OR], 5.32; 95% confidence interval [CI], 1.42 to 19.93 and OR, 4.46; 95% CI, 1.17 to 16.97, respectively). AKT2 expression was able to discriminate against LNM (area under the receiver operating characteristic, 0.799 ± 0.063; 95% CI, 0.676 to 0.921) at an H-score cutoff of 104.62 (83.3% sensitivity, 62.5% specificity).
Conclusions
AKT2 expression has potential as a predictor of LNM in IBC-NST. The H-score cutoff for AKT2 expression can be used as a classification guide in future studies. -
Citations
Citations to this article as recorded by- Association of Src with Nottingham Prognostic Index in Breast Cancer: Implications for Breast Cancer Prognostication
Primariadewi Rustamadji, Elvan Wiyarta
Journal of Nature and Science of Medicine.2024; 7(2): 90. CrossRef - CD4+ Tumor-infiltrating Lymphocytes in Neoadjuvant Chemotherapy-treated Invasive Breast Cancer of No Special Type
Primariadewi Rustamadji, Elvan Wiyarta, Meike Pramono, Sinta Chaira Maulanisa
Journal of Nature and Science of Medicine.2024; 7(3): 179. CrossRef - Potential of AKNA as a Predictive Biomarker for Ovarian Cancer and Its Relationship to Tumor Grading
P Rustamadji, E Wiyarta, M Miftahuzzakiyah, D Sukmawati, DA Suryandari, R Kodariah
Nigerian Journal of Clinical Practice.2024; 27(9): 1089. CrossRef - Exploring the Expression of Survivin on Neoadjuvant Chemotherapy in Invasive Breast Carcinoma
Primariadewi Rustamadji, Elvan Wiyarta, Ineke Anggreani
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 1440. CrossRef - Effect of Omega-3-Rich Fish Oil on TNF- Expression in Mice's Colonic Tissue Induced with Azoxymethane (AOM) and Dextran Sodium Sulphate (DSS)
Elvan Wiyarta, Kusmardi Kusmardi, Yurnadi Hanafi Midoen
Research Journal of Pharmacy and Technology.2022; : 3179. CrossRef - The potential of lunasin extract for the prevention of breast cancer progression by upregulating E-Cadherin and inhibiting ICAM-1
Kusmardi Kusmardi, Elvan Wiyarta, Numlil Khaira Rusdi, Andi Muh. Maulana, Ari Estuningtyas, Hadi Sunaryo
F1000Research.2021; 10: 902. CrossRef - CD44 Variant Exon 6 Isoform Expression as a Potential Predictor of Lymph Node Metastasis in Invasive Breast Carcinoma of No Special Type
Primariadewi Rustamadji, Elvan Wiyarta, Kristina A. Bethania, Rakesh Sathish Nair
International Journal of Breast Cancer.2021; 2021: 1. CrossRef - Correlation between CD 34 and CD 68 expression in placental malaria with maternal anemia
Primariadewi Rustamadji, Muhammad Takbir, Puspita Eka Wuyung, Kusmardi Kusmardi, Elvan Wiyarta
Tropical Parasitology.2021; 11(2): 92. CrossRef
- Association of Src with Nottingham Prognostic Index in Breast Cancer: Implications for Breast Cancer Prognostication
- Standardized pathology report for breast cancer
- Soo Youn Cho, So Yeon Park, Young Kyung Bae, Jee Yeon Kim, Eun Kyung Kim, Woo Gyeong Kim, Youngmee Kwon, Ahwon Lee, Hee Jin Lee, Ji Shin Lee, Jee Young Park, Gyungyub Gong, Hye Kyoung Yoon
- J Pathol Transl Med. 2021;55(1):1-15. Published online January 11, 2021
- DOI: https://doi.org/10.4132/jptm.2020.11.20
- 15,839 View
- 724 Download
- 8 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Given the recent advances in management and understanding of breast cancer, a standardized pathology report reflecting these changes is critical. To meet this need, the Breast Pathology Study Group of the Korean Society of Pathologists has developed a standardized pathology reporting format for breast cancer, consisting of ‘standard data elements,’ ‘conditional data elements,’ and a biomarker report form. The ‘standard data elements’ consist of the basic pathologic features used for prognostication, while other factors related to prognosis or diagnosis are described in the ‘conditional data elements.’ In addition to standard data elements, all recommended issues are also presented. We expect that this standardized pathology report for breast cancer will improve diagnostic concordance and communication between pathologists and clinicians, as well as between pathologists inter-institutionally.
-
Citations
Citations to this article as recorded by- Adenoid Cystic Carcinoma of Breast Associated With an Incidental Radial Scar: A Cyto‐Histopathology Correlation
Rallapalli Rajyalakshmi, Valasapalli Rajani, Tanuku Sreedhar, Kollabathula Arpitha
Diagnostic Cytopathology.2026;[Epub] CrossRef - Navigating discrepancies: The assessment of residual lymphovascular invasion in breast carcinoma after neoadjuvant treatment
Anikó Kovács, Åsa Rundgren-Sellei, Gunilla Rask, Annette Bauer, Anna Bodén, Johannes van Brakel, Eugenia Colón-Cervantes, Anna Ehinger, Johan Hartman, Balazs Acs
The Breast.2025; 82: 104519. CrossRef - Residual pure intralymphatic carcinoma component only (lymphovascular tumor emboli without invasive carcinoma) after neoadjuvant chemotherapy is associated with poor outcome: Not pathologic complete response
Hyunwoo Lee, Yunjeong Jang, Yoon Ah Cho, Eun Yoon Cho
Human Pathology.2024; 145: 1. CrossRef - Sentinel lymph node biopsy in patients with ductal carcinomain situ: systematic review and meta-analysis
Matthew G. Davey, Colm O’Flaherty, Eoin F. Cleere, Aoife Nohilly, James Phelan, Evan Ronane, Aoife J. Lowery, Michael J. Kerin
BJS Open.2022;[Epub] CrossRef
- Adenoid Cystic Carcinoma of Breast Associated With an Incidental Radial Scar: A Cyto‐Histopathology Correlation
- Imaging features of breast cancer molecular subtypes: state of the art
- Nariya Cho
- J Pathol Transl Med. 2021;55(1):16-25. Published online November 9, 2020
- DOI: https://doi.org/10.4132/jptm.2020.09.03
- 54,797 View
- 402 Download
- 25 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Characterization of breast cancer molecular subtypes has been the standard of care for breast cancer management. We aimed to provide a review of imaging features of breast cancer molecular subtypes for the field of precision medicine. We also provide an update on the recent progress in precision medicine for breast cancer, implications for imaging, and recent observations in longitudinal functional imaging with radiomics.
-
Citations
Citations to this article as recorded by- Prediction of HER2 changes post-neoadjuvant therapy based on fusion of ultrasound radiomics and clinicopathological features empowered by explainable AI: A multicenter study
Yuqi Yan, Xinzheng Xue, Jiayu Xie, Jian Liu, Lin Sui, Tian Jiang, Zhiyan Jin, Di Ou, Zhirui Chuan, Mingjie Jin, Yang Zhang, Vicky Yang Wang, Xiaomao Luo, Shihao Xu, Dong Xu
European Journal of Cancer.2026; 232: 116158. CrossRef - Contrast-Enhanced Mammography and Deep Learning-Derived Malignancy Scoring in Breast Cancer Molecular Subtype Assessment
Antonia O. Ferenčaba, Dora Galić, Gordana Ivanac, Kristina Kralik, Martina Smolić, Justinija Steiner, Ivo Pedišić, Kristina Bojanic
Medicina.2026; 62(1): 115. CrossRef - Radiomics Integration of Mammography and DCE-MRI for Predicting Molecular Subtypes in Breast Cancer Patients
Xianwei Yang, Jing Li, Hang Sun, Jing Chen, Jin Xie, Yonghui Peng, Tao Shang, Tongyong Pan
Breast Cancer: Targets and Therapy.2025; Volume 17: 187. CrossRef - HER2 (2+)/SISH-positive vs. HER2 (3+) Breast Cancer: Pre-treatment MRI Differences and Accuracy of pCR Prediction on Post-treatment MRI
Ga Eun Park, Han Song Mun, Sung Hun Kim, Bong Joo Kang
Academic Radiology.2025; 32(8): 4395. CrossRef - Impact of Prior Mammograms on Radiologists and Radiographers' Detection of Different Breast Cancer Lesion Types
Judith D. Akwo, Phuong Dung (Yun) Trieu, Melissa L. Barron, Tess Reynolds, Sarah J. Lewis
Journal of Medical Radiation Sciences.2025; 72(4): 497. CrossRef - Correlation analysis of multiparametric magnetic resonance imaging features and molecular subtypes of breast cancer
Junping Li, Guanghui Huo, Xiaoye Lei, Guang Li, Mengxing Yu, Ziyang Nie, Zhenhua Guo, Yue Zhang
Journal of Clinical Imaging Science.2025; 15: 37. CrossRef - Intertumoral Heterogeneity in Multifocal Breast Cancer Mimicking a Collision Tumor on Imaging: A Case Report
Yoshika Nagata, Izumi Kinoshita, Toshihiro Saeki, Daiji Uchiyama, Takahisa Fujikawa
Cureus.2025;[Epub] CrossRef - Fractal measures as predictors of histopathological complexity in breast carcinoma mammograms
Abhijeet Das, Ramray Bhat, Mohit Kumar Jolly
Physical Biology.2025; 22(6): 066006. CrossRef - Association of clinicopathologic and molecular factors with the occurrence of positive margins in breast cancer
Anupama Praveen Kumar, Diego Vicente, Jianfang Liu, Praveen-Kumar Raj-Kumar, Brenda Deyarmin, Xiaoying Lin, Craig D. Shriver, Hai Hu
Breast Cancer Research and Treatment.2024; 204(1): 15. CrossRef - The association of magnetic resonance imaging features with five molecular subtypes of breast cancer
Van Thi Nguyen, Duc Huu Duong, Quang Thai Nguyen, Duy Thai Nguyen, Thi Linh Tran, Tra Giang Duong
European Journal of Radiology Open.2024; 13: 100585. CrossRef - The effect of data resampling methods in radiomics
Aydin Demircioğlu
Scientific Reports.2024;[Epub] CrossRef - Treated Primary Cutaneous Malignant Melanoma With Later Metastasis Found in Clinical Presentation of Left Axilla Lymphadenopathy: A Case Report
Brigitte L Cochran, Sara Eliseo, Austin Vaughn, Tamryn L Van Der Horn, Enzo Ferrara, Jamie Edwards
Cureus.2024;[Epub] CrossRef - Pushing the envelope in breast conserving surgery − is multiple-wire localization (3 or more wires) associated with increased risk of compromised margins and long-term recurrence?
Orit Golan, Marian Khatib, Tehillah S. Menes, Vivianne A.R. Freitas, Rivka Kessner, Rina Neeman, Michal Mauda-Havakuk, Diego Mercer, Yoav Amitai
European Journal of Radiology.2024; 176: 111511. CrossRef - A model combining BI-RADS® descriptors from pre-treatment B-mode breast ultrasound with clinicopathological tumor features shows promise in the prediction of residual disease after neoadjuvant chemotherapy
Panagiotis Kapetas, Reena Aggarwal, Basmah Altuwayjiri, Katja Pinker, Paola Clauser, Thomas H. Helbich, Pascal A.T. Baltzer
European Journal of Radiology.2024; 178: 111649. CrossRef - Correlations of Imaging and Therapy in Breast Cancer Based on Molecular Patterns: An Important Issue in the Diagnosis of Breast Cancer
Oana Maria Burciu, Ioan Sas, Tudor-Alexandru Popoiu, Adrian-Grigore Merce, Lavinia Moleriu, Ionut Marcel Cobec
International Journal of Molecular Sciences.2024; 25(15): 8506. CrossRef - Access to prior screening mammograms affects the specificity but not sensitivity of radiologists' performance
J.D. Akwo, P. D. (Yun) Trieu, M.L. Barron, T. Reynolds, S.J. Lewis
Clinical Radiology.2024; 79(12): e1549. CrossRef - Machine learning-based radiomics prognostic model for patients with proximal esophageal cancer after definitive chemoradiotherapy
Linrui Li, Zhihui Qin, Juan Bo, Jiaru Hu, Yu Zhang, Liting Qian, Jiangning Dong
Insights into Imaging.2024;[Epub] CrossRef - LYMPH NODES MORPHOLOGICAL CHANGES AND BREAST CANCER SUBTYPES IN PREDICTION OF METASTASES
J. N. Akhundova, M. F. Amirova
World of Medicine and Biology.2024; 20(90): 15. CrossRef - Axillary lymph node changes in different molecular subtypes of breast cancer
J.N. Akhundova
Український радіологічний та онкологічний журнал.2024; 32(4): 529. CrossRef - Histogram analysis of multi-model high-resolution diffusion-weighted MRI in breast cancer: correlations with molecular prognostic factors and subtypes
Yanjin Qin, Feng Wu, Qilan Hu, Litong He, Min Huo, Caili Tang, Jingru Yi, Huiting Zhang, Ting Yin, Tao Ai
Frontiers in Oncology.2023;[Epub] CrossRef - ASO Author Reflections: Sequence of Treatment in Clinically Node-Negative T1 Triple-Negative Breast Cancer
Kai Huang, James W. Jakub, Sarah A. McLaughlin
Annals of Surgical Oncology.2023; 30(13): 8455. CrossRef - Circulating non-coding RNAs as a diagnostic and management biomarker for breast cancer: current insights
Hamed Hosseinalizadeh, Mehrdad Mahmoodpour, Ammar Ebrahimi
Molecular Biology Reports.2022; 49(1): 705. CrossRef - MRI as a biomarker for breast cancer diagnosis and prognosis
Francesca Galati, Veronica Rizzo, Rubina Manuela Trimboli, Endi Kripa, Roberto Maroncelli, Federica Pediconi
BJR|Open.2022;[Epub] CrossRef - Multiparametric MRI Features of Breast Cancer Molecular Subtypes
Madalina Szep, Roxana Pintican, Bianca Boca, Andra Perja, Magdalena Duma, Diana Feier, Bogdan Fetica, Dan Eniu, Sorin Marian Dudea, Angelica Chiorean
Medicina.2022; 58(12): 1716. CrossRef - Circulating tumor cells as prognostic biomarkers in breast cancer: current status and future prospects
Evagelia Chantzara, Nikolaos Xenidis, Galatea Kallergi, Vassilis Georgoulias, Athanasios Kotsakis
Expert Review of Molecular Diagnostics.2021; 21(10): 1037. CrossRef
- Prediction of HER2 changes post-neoadjuvant therapy based on fusion of ultrasound radiomics and clinicopathological features empowered by explainable AI: A multicenter study
- Clinicopathological characteristics of BRCA-associated breast cancer in Asian patients
- Eun-Kyu Kim, So Yeon Park, Sung-Won Kim
- J Pathol Transl Med. 2020;54(4):265-275. Published online May 14, 2020
- DOI: https://doi.org/10.4132/jptm.2020.04.07
- 11,899 View
- 267 Download
- 16 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF BRCA 1/2 germline mutations account for the majority of hereditary breast cancers. Since the identification of theBRCA genes, several attempts have been made to define the clinicopathological characteristics ofBRCA -associated breast cancer in comparison with sporadic breast cancer. Asians constitute 60% of the world population, and although the incidence of breast cancer in Asia remains low compared to the West, breast cancer is the most prevalent female cancer in the region. The epidemiological aspects of breast cancer are different between Asians and Caucasians. Asian patients present with breast cancer at a younger age than Western patients. The contributions ofBRCA1/2 mutations to breast cancer incidence are expected to differ between Asians and Caucasians, and the different genetic backgrounds among races are likely to influence the breast cancer phenotypes. However, most large-scale studies on the clinicopathological characteristics ofBRCA -associated breast cancer have been on Western patients, while studies on Asian populations were small and sporadic. In this review, we provide an overview of the clinical and pathological characteristics ofBRCA -associated breast cancer, incorporating findings on Asian patients.-
Citations
Citations to this article as recorded by- Harnessing Institutionally Developed Clinical Targeted Sequencing to Improve Patient Survival in Breast Cancer: A Seven-Year Experience
Jiwon Koh, Jinyong Kim, Go-Un Woo, Hanbaek Yi, So Yean Kwon, Jeongmin Seo, Jeong Mo Bae, Jung Ho Kim, Jae Kyung Won, Han Suk Ryu, Yoon Kyung Jeon, Dae-Won Lee, Miso Kim, Tae-Yong Kim, Kyung-Hun Lee, Tae-You Kim, Jee-Soo Lee, Moon-Woo Seong, Sheehyun Kim,
Cancer Research and Treatment.2025; 57(2): 443. CrossRef - Part II: consensus statements and expert recommendations for BRCA-associated breast cancer in the Asia-Pacific region: clinical management
Yeon Hee Park, Soo Chin Lee, Christian F. Singer, Judith Balmaña, Rebecca Alexandra Dent, Veronique Kiak-Mien Tan, Nadia Ayu Mulansari, Mastura Md. Yusof, Frances Victoria F. Que, Yen-Shen Lu, Napa Parinyanitikul, Cam Phuong Pham, Nur Aishah Taib, Sun-You
Frontiers in Oncology.2025;[Epub] CrossRef -
Predicting
BRCA
mutation and stratifying targeted therapy response using multimodal learning: a multicenter study
Yi Li, Xiaomin Xiong, Xiaohua Liu, Mengke Xu, Boping Yang, Xiaoju Li, Yu Li, Bo Lin, Bo Xu
Annals of Medicine.2024;[Epub] CrossRef - BRCA 1–2 Incidence in Synchronous and Metachronous Breast Cancer: a Tertiary Center Study
Ahmet Dağ, Bilal Arslan, Erkan Güler, Serdar Mermer
Indian Journal of Surgery.2023; 85(1): 25. CrossRef - Characteristics of breast cancer patients tested for germline BRCA1/2 mutations by next‐generation sequencing in Ramathibodi Hospital, Mahidol University
Songporn Oranratnachai, Watchalawalee Yamkaew, Atchara Tunteeratum, Thongchai Sukarayothin, Nareenart Iemwimangsa, Ravat Panvichien
Cancer Reports.2023;[Epub] CrossRef - Prognostic and predictive biomarkers with therapeutic targets in breast cancer: A 2022 update on current developments, evidence, and recommendations
Clement Chung, Vanessa T.Y. Yeung, Kenneth C.W. Wong
Journal of Oncology Pharmacy Practice.2023; 29(6): 1343. CrossRef - Mutations of TP53 and genes related to homologous recombination repair in breast cancer with germline BRCA1/2 mutations
Jinyong Kim, Kyeonghun Jeong, Hyeji Jun, Kwangsoo Kim, Jeong Mo Bae, Myung Geun Song, Hanbaek Yi, Songyi Park, Go-un Woo, Dae-Won Lee, Tae-Yong Kim, Kyung-Hun Lee, Seock-Ah Im
Human Genomics.2023;[Epub] CrossRef - Habitat Analysis of Breast Cancer‐Enhanced MRI Reflects BRCA1 Mutation Determined by Immunohistochemistry
Tianming Du, Haidong Zhao, Chen Li
BioMed Research International.2022;[Epub] CrossRef - Prevalence and Factors Associated with BRCA1/2 Gene Mutation in Chinese Populations with Breast Cancer
Guoding Huang, Hongquan Lu, Qizhu Chen, Xinting Huang
International Journal of General Medicine.2022; Volume 15: 6783. CrossRef - Association between fertility treatments and breast cancer risk in women with a family history or BRCA mutations: a systematic review and meta-analysis
Xiaojing Liu, Jing Yue, Ruqiya Pervaiz, Hanwang Zhang, Lan Wang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Relationship between Baseline [18F]FDG PET/CT Semiquantitative Parameters and BRCA Mutational Status and Their Prognostic Role in Patients with Invasive Ductal Breast Carcinoma
Francesco Dondi, Domenico Albano, Pietro Bellini, Luca Camoni, Giorgio Treglia, Francesco Bertagna
Tomography.2022; 8(6): 2662. CrossRef - The clinical and diagnostic characteristics of BRCA-associated breast cancer
M.A. Golotyuk, A.A. Berezhnoy, N.V. Kazantseva, A.V. Dorofeev, S.A. Shevchenko, I.V. Borzunov, N.I. Rozhkova
Onkologiya. Zhurnal imeni P.A.Gertsena.2022; 11(6): 18. CrossRef - The Clinical and Pathological Profile of BRCA1 Gene Methylated Breast Cancer Women: A Meta-Analysis
Ilary Ruscito, Maria Luisa Gasparri, Maria Paola De Marco, Flavia Costanzi, Aris Raad Besharat, Andrea Papadia, Thorsten Kuehn, Oreste Davide Gentilini, Filippo Bellati, Donatella Caserta
Cancers.2021; 13(6): 1391. CrossRef - Changing Patterns in Clinicopathological Characteristics of Breast Cancer and Prevalence of BRCA Mutations: Analysis in a Rural Area of Southern China
Qiuming Wang, Heming Wu, Yongquan Lan, Jinhong Zhang, Jingna Wu, Yunuo Zhang, Liang Li, Donghua Liu, Jinfeng Zhang
International Journal of General Medicine.2021; Volume 14: 7371. CrossRef
- Harnessing Institutionally Developed Clinical Targeted Sequencing to Improve Patient Survival in Breast Cancer: A Seven-Year Experience
- Clinicopathologic characteristics of HER2-positive pure mucinous carcinoma of the breast
- Yunjeong Jang, Hera Jung, Han-Na Kim, Youjeong Seo, Emad Alsharif, Seok Jin Nam, Seok Won Kim, Jeong Eon Lee, Yeon Hee Park, Eun Yoon Cho, Soo Youn Cho
- J Pathol Transl Med. 2020;54(1):95-102. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.24
- 10,690 View
- 293 Download
- 22 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pure mucinous carcinoma (PMC) is a rare type of breast cancer, estimated to represent 2% of invasive breast cancer. PMC is typically positive for estrogen receptors (ER) and progesterone receptors (PR) and negative for human epidermal growth factor receptor 2 (HER2). The clinicopathologic characteristics of HER2-positive PMC have not been investigated.
Methods
Pathology archives were searched for PMC diagnosed from January 1999 to April 2018. Clinicopathologic data and microscopic findings were reviewed and compared between HER2-positive PMC and HER2-negative PMC. We also analyzed the differences in disease-free survival (DFS) and overall survival according to clinicopathologic parameters including HER2 status in overall PMC cases.
Results
There were 21 HER2-positive cases (4.8%) in 438 PMCs. The average tumor size of HER2-positive PMC was 32.21 mm (± 26.55). Lymph node metastasis was present in seven cases. Compared to HER2-negative PMC, HER2-positive PMC presented with a more advanced T category (p < .001), more frequent lymph node metastasis (p = .009), and a higher nuclear and histologic grade (p < .001). Microscopically, signet ring cells were frequently observed in HER2-positive PMC (p < .001), whereas a micropapillary pattern was more frequent in HER2-negative PMC (p = .012). HER2-positive PMC was more frequently negative for ER (33.3% vs. 1.2%) and PR (28.6% vs. 7.2%) than HER2-negative PMC and showed a high Ki-67 labeling index. During follow-up, distant metastasis and recurrence developed in three HER2-positive PMC patients. Multivariate analysis revealed that only HER2-positivity and lymph node status were significantly associated with DFS.
Conclusions
Our results suggest that HER2-positive PMC is a more aggressive subgroup of PMC. HER2 positivity should be considered for adequate management of PMC. -
Citations
Citations to this article as recorded by- Mucin‐producing breast lesions: a practical approach to diagnosis
Sunayana Misra, Mihir Gudi, Kimberly H Allison, Edi Brogi, Cecily Quinn, Hannah Y Wen, Puay Hoon Tan
Histopathology.2026;[Epub] CrossRef - Clinicopathological characteristics of mucinous breast cancer: a retrospective analysis of a 6-years study from national cancer center in Vietnam
Thi Huyen Phung, Thanh Tung Pham, Huu Thang Nguyen, Dinh Thach Nguyen, Thanh Long Nguyen, Thi Hoai Hoang
Breast Cancer Research and Treatment.2025; 209(3): 667. CrossRef - Poor response of HER2-positive mucinous carcinomas of breast to neoadjuvant HER2-targeted therapy: A study of four cases
Min Han, Daniel Schmolze, Javier A. Arias-Stella, Christina H. Wei, Joanne Mortimer, Fang Fan
Annals of Diagnostic Pathology.2025; 74: 152396. CrossRef - Comprehensive Immunohistochemical Analysis of Mesonephric Marker Expression in Low-grade Endometrial Endometrioid Carcinoma
Yurimi Lee, Sangjoon Choi, Hyun-Soo Kim
International Journal of Gynecological Pathology.2024; 43(3): 221. CrossRef - Clinicopathological features and prognosis of mucinous breast carcinoma with a micropapillary structure
Beibei Yang, Menglu Shen, Bo Sun, Jing Zhao, Meng Wang
Thoracic Cancer.2024; 15(36): 2530. CrossRef - Pure Mucinous Carcinoma of the Breast: Radiologic-Pathologic Correlation
Cherie M Kuzmiak, Benjamin C Calhoun
Journal of Breast Imaging.2023;[Epub] CrossRef - Role of circ-FOXO3 and miR-23a in radiosensitivity of breast cancer
Elahe Abdollahi, Hossein Mozdarani, Behrooz Z. Alizadeh
Breast Cancer.2023; 30(5): 714. CrossRef - On Ultrasonographic Features of Mucinous Carcinoma with Micropapillary Pattern
Wei-Sen Yang, Yang Li, Ya Gao
Breast Cancer: Targets and Therapy.2023; Volume 15: 473. CrossRef - Spectrum of Mucin-containing Lesions of the Breast: Multimodality Imaging Review with Pathologic Correlation
Janice N. Thai, Melinda F. Lerwill, Shinn-Huey S. Chou
RadioGraphics.2023;[Epub] CrossRef - Mesonephric-like Adenocarcinoma of the Ovary: Clinicopathological and Molecular Characteristics
Hyun Hee Koh, Eunhyang Park, Hyun-Soo Kim
Diagnostics.2022; 12(2): 326. CrossRef - Alveolar Soft Part Sarcoma of the Uterus: Clinicopathological and Molecular Characteristics
Yurimi Lee, Kiyong Na, Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(5): 1102. CrossRef - Metastasis of the Mucionous adenocarcinoma of breast to the mandibular gingiva: Rare case report
Ivana Mijatov, Aleksandra Fejsa Levakov, Aleksandar Spasić, Jelena Nikolić, Saša Mijatov
Medicine.2022; 101(38): e30732. CrossRef - Endometrioid Carcinomas of the Ovaries and Endometrium Involving Endocervical Polyps: Comprehensive Clinicopathological Analyses
Jihee Sohn, Yurimi Lee, Hyun-Soo Kim
Diagnostics.2022; 12(10): 2339. CrossRef - Serous Carcinoma of the Endometrium with Mesonephric-Like Differentiation Initially Misdiagnosed as Uterine Mesonephric-Like Adenocarcinoma: A Case Report with Emphasis on the Immunostaining and the Identification of Splice Site TP53 Mutation
Sangjoon Choi, Yoon Yang Jung, Hyun-Soo Kim
Diagnostics.2021; 11(4): 717. CrossRef - HER2 positive mucinous carcinoma of breast with micropapillary features: Report of a case and review of literature
Dinesh Chandra Doval, Rupal Tripathi, Sunil Pasricha, Pankaj Goyal, Chaturbhuj Agrawal, Anurag Mehta
Human Pathology: Case Reports.2021; 25: 200531. CrossRef - Carcinoma mucosecretor de mama HER2-positivo, un caso clínico
A.M. González Aranda, E. Martínez Gómez, A. Santana Costa, F. Arnanz Velasco, M.H. González de Diego, A. Zapico Goñi
Clínica e Investigación en Ginecología y Obstetricia.2021; 48(4): 100685. CrossRef - Clinicopathologic features of unexpectedly HER2 positive breast carcinomas: An institutional experience
Carissa LaBoy, Kalliopi P. Siziopikou, Lauren Rosen, Luis Z. Blanco, Jennifer L. Pincus
Pathology - Research and Practice.2021; 222: 153441. CrossRef - Mesonephric-like Differentiation of Endometrial Endometrioid Carcinoma: Clinicopathological and Molecular Characteristics Distinct from Those of Uterine Mesonephric-like Adenocarcinoma
Sujin Park, Go Eun Bae, Jiyoung Kim, Hyun-Soo Kim
Diagnostics.2021; 11(8): 1450. CrossRef - Mesonephric-like Adenocarcinoma of the Uterine Corpus: Comprehensive Immunohistochemical Analyses Using Markers for Mesonephric, Endometrioid and Serous Tumors
Hyunjin Kim, Kiyong Na, Go Eun Bae, Hyun-Soo Kim
Diagnostics.2021; 11(11): 2042. CrossRef
- Mucin‐producing breast lesions: a practical approach to diagnosis
- Analysis of the molecular subtypes of preoperative core needle biopsy and surgical specimens in invasive breast cancer
- Ye Sul Jeong, Jun Kang, Jieun Lee, Tae-Kyung Yoo, Sung Hun Kim, Ahwon Lee
- J Pathol Transl Med. 2020;54(1):87-94. Published online November 13, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.14
- 10,120 View
- 212 Download
- 17 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Accurate molecular classification of breast core needle biopsy (CNB) tissue is important for determining neoadjuvant systemic therapies for invasive breast cancer. The researchers aimed to evaluate the concordance rate (CR) of molecular subtypes between CNBs and surgical specimens.
Methods
This study was conducted with invasive breast cancer patients who underwent surgery after CNB at Seoul St. Mary’s Hospital between December 2014 and December 2017. Estrogen receptor (ER), progesterone receptor (PR), human epidermal growth factor receptor 2 (HER2), and Ki67 were analyzed using immunohistochemistry. ER and PR were evaluated by Allred score (0–8). HER2 was graded from 0 to +3, and all 2+ cases were reflex tested with silver in situ hybridization. The labeling index of Ki67 was counted by either manual scoring or digital image analysis. Molecular subtypes were classified using the above surrogate markers.
Results
In total, 629 patients were evaluated. The CRs of ER, PR, HER2, and Ki67 were 96.5% (kappa, 0.883; p<.001), 93.0% (kappa, 0.824; p<.001), 99.7% (kappa, 0.988; p<.001), and 78.7% (kappa, 0.577; p<.001), respectively. Digital image analysis of Ki67 in CNB showed better concordance with Ki67 in surgical specimens (CR, 82.3%; kappa, 0.639 for digital image analysis vs. CR, 76.2%; kappa, 0.534 for manual counting). The CRs of luminal A, luminal B, HER2, and triple negative types were 89.0%, 70.0%, 82.9%, and 77.2%, respectively.
Conclusions
CNB was reasonably accurate for determining ER, PR, HER2, Ki67, and molecular subtypes. Using digital image analysis for Ki67 in CNB produced more accurate molecular classifications. -
Citations
Citations to this article as recorded by- Predicting the Efficacy of Breast Cancer Neoadjuvant Chemotherapy Using Ultrasonography and Machine Learning
Meihong Jia, Huizhan Li, Wenli Xiao, Jiping Xue, Zhifen Wang, Xia He, Xin Wang, Dianxia Men
Ultrasound in Medicine & Biology.2026;[Epub] CrossRef - Correlation between ultrasonography and elastography parameters and molecular subtypes of breast cancer in young women
Dian-xia Men, Hui-zhan Li, Juan Dong, Meng-hua Xue, Zhi-fen Wang, Wen-li Xiao, Ji-ping Xue, Mei-hong Jia
Annals of Medicine.2025;[Epub] CrossRef - Concordance of Oncotype DX Breast Recurrence Score Assay Results Between Paired Core Needle Biopsy and Surgical Excision Specimens in Hormone Receptor Positive, Human Epidermal Growth Factor Receptor 2 Negative, Early-Stage Breast Cancer
Aziza Nassar, Jodi Carter, Paige Innis, Andrea Pingitore Blacklock, Jennifer Racz, Matthew Petitt, Purva Singla, Helena Hanna, Abigail Lochala, Christy A. Russell, Minetta C. Liu
JCO Precision Oncology.2025;[Epub] CrossRef - Impact of immunohistochemistry staining conditions on the incidence of human epidermal growth factor receptor 2 (HER2)-low breast cancer
Min Chong Kim, Sun Young Kwon, Hye Ra Jung, Young Kyung Bae
Virchows Archiv.2024; 485(6): 1117. CrossRef - Study on Intratumoral Heterogeneity of Expression of Estrogen Receptor, Progesterone Receptor, and Human Epidermal Growth Factor Receptor 2 in Carcinoma Breast
Ragavi Uthayasuriyan, Sheba K Jacob, Saloni Naresh Shah
Apollo Medicine.2024; 21(1): 51. CrossRef - Concordance of HER2 status between core needle biopsy and surgical resection specimens of breast cancer: an analysis focusing on the HER2-low status
Sei Na, Milim Kim, Yujun Park, Hyun Jung Kwon, Hee-Chul Shin, Eun-Kyu Kim, Mijung Jang, Sun Mi Kim, So Yeon Park
Breast Cancer.2024; 31(4): 705. CrossRef - Concordance of immunohistochemistry for predictive and prognostic factors in breast cancer between biopsy and surgical excision: a single-centre experience and review of the literature
Chiara Rossi, Sara Fraticelli, Marianna Fanizza, Alberta Ferrari, Elisa Ferraris, Alessia Messina, Angelica Della Valle, Chiara Annunziata Pasqualina Anghelone, Angioletta Lasagna, Gianpiero Rizzo, Lorenzo Perrone, Maria Grazia Sommaruga, Giulia Meloni, S
Breast Cancer Research and Treatment.2023; 198(3): 573. CrossRef - Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
Su Hwa Kim, Young Suk Lee, Sung Hak Lee, Yeoun Eun Sung, Ahwon Lee, Jun Kang, Jae-Sung Park, Sin Soo Jeun, Youn Soo Lee
Journal of Pathology and Translational Medicine.2023; 57(4): 217. CrossRef - The Role of Diffusion-Weighted Imaging Based on Maximum-Intensity Projection in Young Patients with Marked Background Parenchymal Enhancement on Contrast-Enhanced Breast MRI
Ga-Eun Park, Bong-Joo Kang, Sung-hun Kim, Na-Young Jung
Life.2023; 13(8): 1744. CrossRef - Concordance between core needle biopsy and surgical excision specimens for Ki‐67 in breast cancer – a systematic review of the literature
Jahnavi Kalvala, Ruth M Parks, Andrew R Green, Kwok‐Leung Cheung
Histopathology.2022; 80(3): 468. CrossRef - İnvaziv Meme Kanserinde Preoperatif Kor İğne Biyopsi ile Postoperatif Cerrahi Spesmenler Arasında ER, PR, HER2 ve Ki67 Açısından Karşılaştırma
Pınar CELEPLİ, Pelin Seher ÖZTEKİN, Salih CELEPLİ, İrem BİGAT, Sema HÜCÜMENOĞLU
Akdeniz Medical Journal.2022; : 179. CrossRef - Concordance of breast cancer biomarker testing in core needle biopsy and surgical specimens: A single institution experience
Jessica A. Slostad, Nicole K. Yun, Aimee E. Schad, Surbhi Warrior, Louis F. Fogg, Ruta Rao
Cancer Medicine.2022; 11(24): 4954. CrossRef - N-Cadherin Distinguishes Intrahepatic Cholangiocarcinoma from Liver Metastases of Ductal Adenocarcinoma of the Pancreas
Tiemo S. Gerber, Benjamin Goeppert, Anne Hausen, Hagen R. Witzel, Fabian Bartsch, Mario Schindeldecker, Lisa-Katharina Gröger, Dirk A. Ridder, Oscar Cahyadi, Irene Esposito, Matthias M. Gaida, Peter Schirmacher, Peter R. Galle, Hauke Lang, Wilfried Roth,
Cancers.2022; 14(13): 3091. CrossRef - Association of Ki-67 Change Pattern After Core Needle Biopsy and Prognosis in HR+/HER2− Early Breast Cancer Patients
Shuai Li, Xiaosong Chen, Kunwei Shen
Frontiers in Surgery.2022;[Epub] CrossRef - MRI Features for Prediction Malignant Intra-Mammary Lymph Nodes: Correlations with Mammography and Ultrasound
Meejung Kim, Bong Joo Kang, Ga Eun Park
Investigative Magnetic Resonance Imaging.2022; 26(2): 135. CrossRef - A single centre experience in Turkey for comparison between core needle biopsy and surgical specimen evaluation results for HER2, SISH, estrogen receptors and progesterone receptors in breast cancer patients
Hatice Karaman, Fatma Senel, Arzu Tasdemir, Ipek Özer, Merve Dogan
Journal of Cancer Research and Therapeutics.2022; 18(6): 1789. CrossRef - Meme kanseri trucut ve rezeksiyon materyallerinde yeni moleküler sınıflama, tanı ve hormon reseptörlerinin durumu tutarlı mı?
Yeliz ARMAN KARAKAYA, Sevda YILMAZ, Hande KARABAŞ
Pamukkale Medical Journal.2021;[Epub] CrossRef - What shear wave elastography parameter best differentiates breast cancer and predicts its histologic aggressiveness?
Hyunjin Kim, Jeongmin Lee, Bong Joo Kang, Sung Hun Kim
Ultrasonography.2021; 40(2): 265. CrossRef - Risk-based decision-making in the treatment of HER2-positive early breast cancer: Recommendations based on the current state of knowledge
Christian Jackisch, Patricia Cortazar, Charles E. Geyer, Luca Gianni, Joseph Gligorov, Zuzana Machackova, Edith A. Perez, Andreas Schneeweiss, Sara M. Tolaney, Michael Untch, Andrew Wardley, Martine Piccart
Cancer Treatment Reviews.2021; 99: 102229. CrossRef - Factors influencing agreement of breast cancer luminal molecular subtype by Ki67 labeling index between core needle biopsy and surgical resection specimens
Kristina A. Tendl-Schulz, Fabian Rössler, Philipp Wimmer, Ulrike M. Heber, Martina Mittlböck, Nicolas Kozakowski, Katja Pinker, Rupert Bartsch, Peter Dubsky, Florian Fitzal, Martin Filipits, Fanny Carolina Eckel, Eva-Maria Langthaler, Günther Steger, Mich
Virchows Archiv.2020; 477(4): 545. CrossRef
- Predicting the Efficacy of Breast Cancer Neoadjuvant Chemotherapy Using Ultrasonography and Machine Learning
- Association between p53 Expression and Amount of Tumor-Infiltrating Lymphocytes in Triple-Negative Breast Cancer
- Miseon Lee, In Ah Park, Sun-Hee Heo, Young-Ae Kim, Gyungyub Gong, Hee Jin Lee
- J Pathol Transl Med. 2019;53(3):180-187. Published online March 11, 2019
- DOI: https://doi.org/10.4132/jptm.2019.02.08
- 9,628 View
- 205 Download
- 19 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Most triple-negative breast cancers (TNBCs) have a high histologic grade, are associated with high endoplasmic stress, and possess a high frequency of TP53 mutations. TP53 missense mutations lead to the production of mutant p53 protein and usually show high levels of p53 protein expression. Tumor-infiltrating lymphocytes (TILs) accumulate as part of the anti-tumor immune response and have a strong prognostic and predictive significance in TNBC. We aimed to elucidate the association between p53 expression and the amount of TILs in TNBC.
Methods
In 678 TNBC patients, we evaluated TIL levels and expression of endoplasmic stress molecules. Immunohistochemical examination of p53 protein expression was categorized into three groups: no, low, and high expression.
Results
No, low, and high p53 expression was identified in 44.1% (n = 299), 20.1% (n = 136), and 35.8% (n = 243) of patients, respectively. Patients with high p53 expression showed high histologic grade (p < .001), high TIL levels (p = .009), and high expression of endoplasmic reticulum stress-associated molecules (p-eIF2a, p = .013; XBP1, p = .007), compared to patients with low p53 expression. There was no significant difference in disease-free (p = .406) or overall survival rates (p = .444) among the three p53 expression groups.
Conclusions
High p53 expression is associated with increased expression of endoplasmic reticulum stress molecules and TIL influx. -
Citations
Citations to this article as recorded by- The search for a TNBC vaccine: the guardian vaccine
Cory Fines, Helen McCarthy, Niamh Buckley
Cancer Biology & Therapy.2025;[Epub] CrossRef - Correlating p53 immunostaining patterns with somatic TP53 mutation and functional properties of mutant p53 in triple‐negative breast cancer
Meejeong Kim, Miseon Lee, Ahwon Lee, Byung‐Ock Choi, Woo‐Chan Park, Sung Hun Kim, Jieun Lee, Jun Kang
Histopathology.2025; 87(2): 299. CrossRef - GD3 synthase drives resistance to p53-induced apoptosis in breast cancer by modulating mitochondrial function
Vivek Anand, Fouad El-Dana, Natalia Baran, Jenny Borgman, Zheng Yin, Hong Zhao, Stephen T. Wong, Michael Andreeff, V. Lokesh Battula
Oncogene.2025; 44(30): 2646. CrossRef - Topoisomerase Inhibitor Resistance in Breast Cancer: Exploring Alterations in Cellular Metabolism and Properties Driving Drug Insensitivity
Juhong Lee, Youngjoo Kwon
Drug Targets and Therapeutics.2025; 4(2): 185. CrossRef - Updated Austrian treatment algorithm for metastatic triple-negative breast cancer
Rupert Bartsch, Gabriel Rinnerthaler, Edgar Petru, Daniel Egle, Michael Gnant, Marija Balic, Thamer Sliwa, Christian Singer
Wiener klinische Wochenschrift.2024; 136(11-12): 347. CrossRef - Triple negative breast cancer: Immunogenicity, tumor microenvironment, and immunotherapy
Sotiris Loizides, Anastasia Constantinidou
Frontiers in Genetics.2023;[Epub] CrossRef - Prognostic benefit of TILs independent of clinicopathological and molecular factors
Koen Brummel, Anneke L. Eerkens, Marco de Bruyn, Hans W. Nijman
British Journal of Cancer.2023; 129(5): 737. CrossRef - Dihydroartemisinin-Transferrin Adducts Enhance TRAIL-Induced Apoptosis in Triple-Negative Breast Cancer in a P53-Independent and ROS-Dependent Manner
Xinyu Zhou, Abel Soto-Gamez, Fleur Nijdam, Rita Setroikromo, Wim J. Quax
Frontiers in Oncology.2022;[Epub] CrossRef - New Challenges in the Differential Diagnosis of High-Grade Triple-Negative Breast Cancer and Serous Carcinoma
Andrii Puzyrenko, Chandler S Cortina, Julie M Jorns
International Journal of Surgical Pathology.2022; 30(7): 728. CrossRef - Prognostic analysis of cuproptosis-related gene in triple-negative breast cancer
Shengnan Sha, Luyi Si, Xinrui Wu, Yuanbiao Chen, Hui Xiong, Ying Xu, Wangrui Liu, Haijun Mei, Tao Wang, Mei Li
Frontiers in Immunology.2022;[Epub] CrossRef - p53 Missense Mutation is Associated with Immune Cell PD-L1 Expression in Triple-Negative Breast Cancer
Ai-Yan Xing, Long Liu, Ke Liang, Bin Wang
Cancer Investigation.2022; 40(10): 879. CrossRef - Crosstalk between Immune Checkpoint Modulators, Metabolic Reprogramming and Cellular Plasticity in Triple-Negative Breast Cancer
Arpita Poddar, Sushma R. Rao, Prashanth Prithviraj, George Kannourakis, Aparna Jayachandran
Current Oncology.2022; 29(10): 6847. CrossRef - The tumor microenvironment and triple-negative breast cancer aggressiveness: shedding light on mechanisms and targeting
Natsuki Furukawa, Vered Stearns, Cesar A. Santa-Maria, Aleksander S. Popel
Expert Opinion on Therapeutic Targets.2022; 26(12): 1041. CrossRef - Intracellular partners of fibroblast growth factors 1 and 2 - implications for functions
Katarzyna Dominika Sluzalska, Jakub Slawski, Martyna Sochacka, Agata Lampart, Jacek Otlewski, Malgorzata Zakrzewska
Cytokine & Growth Factor Reviews.2021; 57: 93. CrossRef - Targeted Chinese Medicine Delivery by A New Family of Biodegradable Pseudo-Protein Nanoparticles for Treating Triple-Negative Breast Cancer: In Vitro and In Vivo Study
Hiu Yee Kwan, Qinghua Xu, Ruihong Gong, Zhaoxiang Bian, Chih-Chang Chu
Frontiers in Oncology.2021;[Epub] CrossRef - Transcriptomic Properties of HER2+ Ductal Carcinoma In Situ of the Breast Associate with Absence of Immune Cells
Marie Colombe Agahozo, Marcel Smid, Ronald van Marion, Dora Hammerl, Thierry P. P. van den Bosch, Mieke A. M. Timmermans, Chayenne J. Heijerman, Pieter J. Westenend, Reno Debets, John W. M. Martens, Carolien H. M. van Deurzen
Biology.2021; 10(8): 768. CrossRef - With Our Powers Combined
Lawrence Kasherman, Katherine Karakasis, Amit M. Oza
The Cancer Journal.2021; 27(6): 511. CrossRef The Research Progress on the Prognostic Value of the Common Hematological Parameters in Peripheral Venous Blood in Breast Cancer
Li Chen, Xiangyi Kong, Chengrui Yan, Yi Fang, Jing Wang
OncoTargets and Therapy.2020; Volume 13: 1397. CrossRefBiomolecular Factors Represented by Bcl-2, p53, and Tumor-Infiltrating Lymphocytes Predict Response for Adjuvant Anthracycline Chemotherapy in Patients with Early Triple-Negative Breast Cancer
Xenia Elena Bacinschi, Anca Zgura, Inga Safta, Rodica Anghel
Cancer Management and Research.2020; Volume 12: 11965. CrossRef
- The search for a TNBC vaccine: the guardian vaccine
- Loss of Human Leukocyte Antigen Class I Expression Is Associated with Poor Prognosis in Patients with Advanced Breast Cancer
- Hong Sik Park, Uiju Cho, So Young Im, Chang Young Yoo, Ji Han Jung, Young Jin Suh, Hyun Joo Choi
- J Pathol Transl Med. 2019;53(2):75-85. Published online November 14, 2018
- DOI: https://doi.org/10.4132/jptm.2018.10.11
- 9,180 View
- 191 Download
- 33 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Human leukocyte antigen class I (HLA-I) molecules play important roles in regulating immune responses. Loss or reduction of HLA-I expression has been shown to be associated with prognosis in several cancers. Regulatory T-cells (Tregs) also play critical functions in immune response regulation. Evaluation of HLA-I expression status by the EMR8-5 antibody and its clinical impact in breast cancer have not been well studied, and its relationship with Tregs remains unclear.
Methods
We evaluated HLA-I expression and Treg infiltration by immunohistochemistry in 465 surgically resected breast cancer samples. We examined the correlation between HLA-I expression and Treg infiltration and clinicopathologic characteristics and survival analyses were performed.
Results
Total loss of HLA-I expression was found in 84 breast cancer samples (18.1%). Univariate survival analysis revealed that loss of HLA-I expression was significantly associated with worse disease-specific survival (DSS) (p = .029). HLA-I was not an independent prognostic factor in the entire patient group, but it was an adverse independent prognostic factor for DSS in patients with advanced disease (stage II–IV) (p = .031). Treg numbers were significantly higher in the intratumoral stroma of HLA-I–positive tumors than in HLA-I–negative tumors (median 6.3 cells/high power field vs 2.1 cells/high power field, p < .001). However, Tregs were not an independent prognostic factor in our cohort.
Conclusions
Our findings suggest that the loss of HLA-I expression is associated with poor prognosis in breast cancer patients, highlighting the role of HLA-I alterations in immune evasion mechanisms of breast cancer. HLA-I could be a promising marker that enables the application of more effective and precise immunotherapies for patients with advanced breast cancer. -
Citations
Citations to this article as recorded by- Estrogen Signaling in Early-Stage Breast Cancer: Impact on Neoadjuvant Chemotherapy and Immunotherapy
Chiara Corti, Busem Binboğa Kurt, Beyza Koca, Tasnim Rahman, Fabio Conforti, Laura Pala, Giampaolo Bianchini, Carmen Criscitiello, Giuseppe Curigliano, Ana C. Garrido-Castro, Sheheryar K. Kabraji, Adrienne G. Waks, Elizabeth A. Mittendorf, Sara M. Tolaney
Cancer Treatment Reviews.2025; 132: 102852. CrossRef - MHC-I upregulation by macbecin II in the solid tumors potentiates the effect of active immunotherapy
Ravindra Pramod Deshpande, Kerui Wu, Shih-Ying Wu, Abhishek Tyagi, Eleanor C Smith, Jee-Won Kim, Kounosuke Watabe
EMBO Molecular Medicine.2025; 17(4): 797. CrossRef - Programmed Cell Death Ligand 1 (PD-L1) and major Histocompatibility Complex Class I (MHC Class I) Expression Patterns and Their Pathologic Associations in triple-Negative Breast Cancer
Ponkrit Kaewkedsri, Piyapharom Intarawichian, Sirawich Jessadapattarakul, Waritta Kunprom, Supinda Koonmee, Malinee Thanee, Ongart Somintara, Anongporn Wongbuddha, Payia Chadbunchachai, Supajit Nawapun, Chaiwat Aphivatanasiri
Breast Cancer: Targets and Therapy.2025; Volume 17: 123. CrossRef - Comment on “Prognostic and Clinical Significance of Human Leukocyte Antigen Class I Expression in Breast Cancer: A Meta‑Analysis”
Wei Han, Li-zhou Shi, Yu-wei Zhang, Hao-nan Wang
Molecular Diagnosis & Therapy.2024; 28(2): 237. CrossRef - Immunotherapy resistance in solid tumors: mechanisms and potential solutions
Daniel S. Lefler, Steven A. Manobianco, Babar Bashir
Cancer Biology & Therapy.2024;[Epub] CrossRef - Assessment of cancer cell‐expressed HLA class I molecules and their immunopathological implications
Terufumi Kubo, Shiori Asano, Kenta Sasaki, Kenji Murata, Takayuki Kanaseki, Tomohide Tsukahara, Yoshihiko Hirohashi, Toshihiko Torigoe
HLA.2024;[Epub] CrossRef - Human Leukocyte Antigen Class I Expression and Natural Killer Cell Infiltration and Its Correlation with Prognostic Features in Luminal Breast Cancers
Maria Vernet-Tomas, Ivonne Vazquez, Francesc Olivares, David Lopez, Jose Yelamos, Laura Comerma
Breast Cancer: Targets and Therapy.2024; Volume 16: 657. CrossRef - Upregulation of MHC I antigen processing machinery gene expression in breast cancer cells by Trichostatin A
A. H. Murtadha, N. A. Sharudin, I. I.M. Azahar, A. T. Che Has, N. F. Mokhtar
Молекулярная биология.2024; 58(1): 121. CrossRef - HLA-I and breast cancer prognosis: A systematic review and meta-analysis
Francisco Cezar Aquino de Moraes, Jorge Henrique Cavalcanti Orestes Cardoso, Francinny Alves Kelly, Michele Kreuz, Lilianne Rodrigues Fernandes, Maria Cristina Figueroa Magalhães, Rommel Mario Rodríguez Burbano
Human Immunology.2024; 85(6): 111148. CrossRef - Cancer Immunology: Immune Escape of Tumors—Expression and Regulation of HLA Class I Molecules and Its Role in Immunotherapies
Yuan Wang, Simon Jasinski-Bergner, Claudia Wickenhauser, Barbara Seliger
Advances in Anatomic Pathology.2023; 30(3): 148. CrossRef - In Silico Pipeline to Identify Tumor-Specific Antigens for Cancer Immunotherapy Using Exome Sequencing Data
Diego Morazán-Fernández, Javier Mora, Jose Arturo Molina-Mora
Phenomics.2023; 3(2): 130. CrossRef - HLA and tumour immunology: immune escape, immunotherapy and immune-related adverse events
Ning Jiang, Yue Yu, Dawei Wu, Shuhang Wang, Yuan Fang, Huilei Miao, Peiwen Ma, Huiyao Huang, Min Zhang, Yu Zhang, Yu Tang, Ning Li
Journal of Cancer Research and Clinical Oncology.2023; 149(2): 737. CrossRef - Relationship between Systemic Inflammatory Markers, GLUT1 Expression, and Maximum 18F-Fluorodeoxyglucose Uptake in Non-Small Cell Lung Carcinoma and Their Prognostic Significance
Sonya Youngju Park, Deog-Gon Cho, Byoung-Yong Shim, Uiju Cho
Diagnostics.2023; 13(6): 1013. CrossRef - Prognostic and Clinical Significance of Human Leukocyte Antigen Class I Expression in Breast Cancer: A Meta-Analysis
Weiqiang Qiao, Zhiqiang Jia, Wanying Guo, Qipeng Liu, Xiao Guo, Miao Deng
Molecular Diagnosis & Therapy.2023; 27(5): 573. CrossRef - Challenges and solutions for therapeuticTCR‐based agents
Manish Malviya, Zita E. H. Aretz, Zaki Molvi, Jayop Lee, Stephanie Pierre, Patrick Wallisch, Tao Dao, David A. Scheinberg
Immunological Reviews.2023; 320(1): 58. CrossRef - Molecular mechanisms of impaired antigenic presentation as a cause of tumor escape from immune surveillance
A.A. Korotaeva, A.A. Borunova, A.Yu. Kuzevanova, T.N. Zabotina, A.A. Alimov
Russian Journal of Archive of Pathology.2023; 85(6): 76. CrossRef - Immune Escape Mechanism of Cancer
Ayse Caner
Current Molecular Biology Reports.2023; 10(1): 9. CrossRef - Upregulation of MHC I Antigen Processing Machinery Gene Expression in Breast Cancer Cells by Trichostatin A
A. H. Murtadha, N. A. Sharudin, I. I. M. Azahar, A. T. Che Has, N. F. Mokhtar
Molecular Biology.2023; 57(6): 1212. CrossRef - Human Leukocyte Antigen Class I Antigen-Processing Machinery Upregulation by Anticancer Therapies in the Era of Checkpoint Inhibitors
Ananthan Sadagopan, Theodoros Michelakos, Gabriella Boyiadzis, Cristina Ferrone, Soldano Ferrone
JAMA Oncology.2022; 8(3): 462. CrossRef - Mechanisms of MHC-I Downregulation and Role in Immunotherapy Response
Brandie C. Taylor, Justin M. Balko
Frontiers in Immunology.2022;[Epub] CrossRef - Immune Checkpoint Blockade in Hormone Receptor-Positive Breast Cancer: Resistance Mechanisms and Future Perspectives
Ioannis A. Vathiotis, Ioannis Trontzas, Niki Gavrielatou, Georgia Gomatou, Nikolaos K. Syrigos, Elias A. Kotteas
Clinical Breast Cancer.2022; 22(7): 642. CrossRef - Aberrant synaptophysin expression in classic Hodgkin lymphoma
Soyoung Im, Jeong-A. Kim, Gyeongsin Park, Uiju Cho
Diagnostic Pathology.2022;[Epub] CrossRef - Expression of HLA class I is associated with immune cell infiltration and patient outcome in breast cancer
Song-Hee Han, Milim Kim, Yul Ri Chung, Ji Won Woo, Hye Yeon Choi, So Yeon Park
Scientific Reports.2022;[Epub] CrossRef - Immune landscape and therapeutic strategies: new insights into PD-L1 in tumors
Yuan Wei, Xiao Xiao, Xiang-Ming Lao, Limin Zheng, Dong-Ming Kuang
Cellular and Molecular Life Sciences.2021; 78(3): 867. CrossRef - Society for Immunotherapy of Cancer (SITC) clinical practice guideline on immunotherapy for the treatment of breast cancer
Leisha A Emens, Sylvia Adams, Ashley Cimino-Mathews, Mary L Disis, Margaret E Gatti-Mays, Alice Y Ho, Kevin Kalinsky, Heather L McArthur, Elizabeth A Mittendorf, Rita Nanda, David B Page, Hope S Rugo, Krista M Rubin, Hatem Soliman, Patricia A Spears, Sara
Journal for ImmunoTherapy of Cancer.2021; 9(8): e002597. CrossRef - Resistance mechanisms to checkpoint inhibitors
Sarah A Weiss, Mario Sznol
Current Opinion in Immunology.2021; 69: 47. CrossRef - The Immunology of Hormone Receptor Positive Breast Cancer
Jonathan Goldberg, Ricardo G. Pastorello, Tuulia Vallius, Janae Davis, Yvonne Xiaoyong Cui, Judith Agudo, Adrienne G. Waks, Tanya Keenan, Sandra S. McAllister, Sara M. Tolaney, Elizabeth A. Mittendorf, Jennifer L. Guerriero
Frontiers in Immunology.2021;[Epub] CrossRef - B4GALNT2 Gene Promotes Proliferation, and Invasiveness and Migration Abilities of Model Triple Negative Breast Cancer (TNBC) Cells by Interacting With HLA-B Protein
Pu Yu, Lili Zhu, Kang Cui, Yabing Du, Chaojie Zhang, Wang Ma, Jia Guo
Frontiers in Oncology.2021;[Epub] CrossRef - Recurrence biomarkers of triple negative breast cancer treated with neoadjuvant chemotherapy and anti-EGFR antibodies
Nina Radosevic-Robin, Pier Selenica, Yingjie Zhu, Helen H. Won, Michael F. Berger, Lorenzo Ferrando, Emiliano Cocco, Maud Privat, Flora Ponelle-Chachuat, Catherine Abrial, Jean-Marc Nabholtz, Frederique Penault-Llorca, Jorge S. Reis-Filho, Maurizio Scaltr
npj Breast Cancer.2021;[Epub] CrossRef - Immune checkpoint inhibitors in advanced nasopharyngeal carcinoma: Beyond an era of chemoradiation?
Liam Masterson, James Howard, Jazmina Gonzalez‐Cruz, Christopher Jackson, Catherine Barnett, Lewis Overton, Howard Liu, Rahul Ladwa, Fiona Simpson, Margie McGrath, Ben Wallwork, Terry Jones, Christian Ottensmeier, Melvin L.K. Chua, Chris Perry, Rajiv Khan
International Journal of Cancer.2020; 146(8): 2305. CrossRef - Co-expression of HLA-I loci improved prognostication in HER2+ breast cancers
Julia Y. Tsang, Chun-Sing Ho, Yun-Bi Ni, Yan Shao, Ivan K. Poon, Siu-Ki Chan, Sai-Yin Cheung, Ka-Ho Shea, Monalyn Marabi, Gary M. Tse
Cancer Immunology, Immunotherapy.2020; 69(5): 799. CrossRef - Breast cancer patients overall survival depends on a combination of the polymorphisms of tumor necrosis factor gene and HLA-haplotypes
T.F. Malivanova, E.V. Alferova, A.S. Ostashkin, T.A. Astrelina, N.N. Mazurenko
Molecular Genetics Microbiology and Virology (Russian version).2020; 38(1): 40. CrossRef - The Overall Survival of Breast Cancer Patients Depends on a Combination of Polymorphisms of Tumor Necrosis Factor Gene and HLA Haplotypes
T. F. Malivanova, E. V. Alferova, A. S. Ostashkin, T. A. Astrelina, N. N. Mazurenko
Molecular Genetics, Microbiology and Virology.2020; 35(1): 38. CrossRef - The Emergence of Natural Killer Cells as a Major Target in Cancer Immunotherapy
Fernando Souza-Fonseca-Guimaraes, Joseph Cursons, Nicholas D. Huntington
Trends in Immunology.2019; 40(2): 142. CrossRef
- Estrogen Signaling in Early-Stage Breast Cancer: Impact on Neoadjuvant Chemotherapy and Immunotherapy
- The Prognostic Impact of Synchronous Ipsilateral Multiple Breast Cancer: Survival Outcomes according to the Eighth American Joint Committee on Cancer Staging and Molecular Subtype
- Jinah Chu, Hyunsik Bae, Youjeong Seo, Soo Youn Cho, Seok-Hyung Kim, Eun Yoon Cho
- J Pathol Transl Med. 2018;52(6):396-403. Published online October 23, 2018
- DOI: https://doi.org/10.4132/jptm.2018.10.03
- 8,140 View
- 102 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
In the current American Joint Committee on Cancer staging system of breast cancer, only tumor size determines T-category regardless of whether the tumor is single or multiple. This study evaluated if tumor multiplicity has prognostic value and can be used to subclassify breast cancer.
Methods
We included 5,758 patients with invasive breast cancer who underwent surgery at Samsung Medical Center, Seoul, Korea, from 1995 to 2012.
Results
Patients were divided into two groups according to multiplicity (single, n = 4,744; multiple, n = 1,014). Statistically significant differences in lymph node involvement and lymphatic invasion were found between the two groups (p < .001). Patients with multiple masses tended to have luminal A molecular subtype (p < .001). On Kaplan-Meier survival analysis, patients with multiple masses had significantly poorer disease-free survival (DFS) (p = .016). The prognostic significance of multiplicity was seen in patients with anatomic staging group I and prognostic staging group IA (p = .019 and p = .032, respectively). When targeting patients with T1-2 N0 M0, hormone receptor–positive, and human epidermal growth factor receptor 2 (HER2)–negative cancer, Kaplan-Meier survival analysis also revealed significantly reduced DFS with multiple cancer (p = .031). The multivariate analysis indicated that multiplicity was independently correlated with worse DFS (hazard ratio, 1.23; 95% confidence interval, 1.03 to 1.47; p = .025). The results of this study indicate that tumor multiplicity is frequently found in luminal A subtype, is associated with frequent lymph node metastasis, and is correlated with worse DFS.
Conclusions
Tumor multiplicity has prognostic value and could be used to subclassify invasive breast cancer at early stages. Adjuvant chemotherapy would be necessary for multiple masses of T1–2 N0 M0, hormone-receptor-positive, and HER2-negative cancer. -
Citations
Citations to this article as recorded by- The Role of Serum Beta-Human Chorionic Gonadotropin (β-hCG) in Differentiating Benign and Malignant Breast Lesions at a Tertiary Care Center in Jharkhand
Neyaz Ahmad, Khushboo Rani, Zenith Kerketta, Krishna Murari, Anish Baxla, Ujala Murmu, Amit Nishant, Shreya .
Cureus.2025;[Epub] CrossRef - Role of Large Format Histology in Diagnosis of Breast Carcinoma
Hari Shankar Pandey, Sanya Bhasin, Suman Kumari Pandey
NMO Journal.2025; 19(2): 189. CrossRef - Prognostic Impact of Multiple Synchronous T1 Breast Cancer
Hongki Gwak, Sung Hoo Jung, Young Jin Suh, Seok Jin Nam, Jai Hong Han, Se Jeong Oh, Eun Hwa Park, Seong Hwan Kim
Cancers.2024; 16(23): 4019. CrossRef - Deep learning-based system for automatic prediction of triple-negative breast cancer from ultrasound images
Alexandre Boulenger, Yanwen Luo, Chenhui Zhang, Chenyang Zhao, Yuanjing Gao, Mengsu Xiao, Qingli Zhu, Jie Tang
Medical & Biological Engineering & Computing.2023; 61(2): 567. CrossRef - Multicentre prospective cohort study of unmet supportive care needs among patients with breast cancer throughout their cancer treatment trajectory in Penang: a PenBCNeeds Study protocol
Noorsuzana Mohd Shariff, Nizuwan Azman, Rohayu Hami, Noor Mastura Mohd Mujar, Mohammad Farris Iman Leong Bin Abdullah
BMJ Open.2021; 11(3): e044746. CrossRef - The subgross morphology of breast carcinomas: a single-institution series of 2033 consecutive cases documented in large-format histology slides
Tibor Tot, Maria Gere, Syster Hofmeyer, Annette Bauer, Ulrika Pellas
Virchows Archiv.2020; 476(3): 373. CrossRef - Editorial for “Synchronous Breast Cancer: Phenotypic Similarities on MRI”
Uma Sharma
Journal of Magnetic Resonance Imaging.2020; 52(1): 309. CrossRef - Synchronous Multiple Breast Cancers—Do We Need to Reshape Staging?
Minodora Onisâi, Adrian Dumitru, Iuliana Iordan, Cătălin Aliuș, Oana Teodor, Adrian Alexandru, Daniela Gheorghiță, Iulian Antoniac, Adriana Nica, Alexandra-Ana Mihăilescu, Sebastian Grădinaru
Medicina.2020; 56(5): 230. CrossRef - Molecular mechanism of triple‑negative breast cancer‑associated BRCA1 and the identification of signaling pathways
Feng Qi, Wen‑Xing Qin, Yuan‑Sheng Zang
Oncology Letters.2019;[Epub] CrossRef
- The Role of Serum Beta-Human Chorionic Gonadotropin (β-hCG) in Differentiating Benign and Malignant Breast Lesions at a Tertiary Care Center in Jharkhand
- High Cytoplasmic CXCR4 Expression Predicts Prolonged Survival in Triple-Negative Breast Cancer Patients Treated with Adjuvant Chemotherapy
- Bobae Shim, Min‐Sun Jin, Ji Hye Moon, In Ae Park, Han Suk Ryu
- J Pathol Transl Med. 2018;52(6):369-377. Published online October 1, 2018
- DOI: https://doi.org/10.4132/jptm.2018.09.19
- 14,455 View
- 185 Download
- 12 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Chemokine receptor CXC chemokine receptor type 4 (CXCR4) and its ligand CXC motif chemokine 12 (CXCL12; stromal cell-derived factor-1) are implicated in tumor growth, metastasis, and tumor cell-microenvironment interaction. A number of studies have reported that increased CXCR4 expression is associated with worse prognosis in triple-negative breast cancer (TNBC), but its prognostic significance has not been studied in TNBC patients treated with adjuvant chemotherapy.
Methods
Two hundred eighty-three TNBC patients who received adjuvant chemotherapy were retrospectively analyzed. Tissue microarray was constructed from formalinfixed, paraffin-embedded tumor tissue and immunohistochemistry for CXCR4 and CXCL12 was performed. Expression of each marker was compared with clinicopathologic characteristics and outcome.
Results
High cytoplasmic CXCR4 expression was associated with younger age (p = .008), higher histologic grade (p = .007) and lower pathologic stage (p = .045), while high CXCL12 expression was related to larger tumor size (p = .045), positive lymph node metastasis (p = .005), and higher pathologic stage (p = .017). The patients with high cytoplasmic CXCR4 experienced lower distant recurrence (p = .006) and better recurrence-free survival (RFS) (log-rank p = .020) after adjuvant chemotherapy. Cytoplasmic CXCR4 expression remained an independent factor of distant recurrence (p = .019) and RFS (p = .038) after multivariate analysis.
Conclusions
High cytoplasmic CXCR4 expression was associated with lower distant recurrence and better RFS in TNBC patients treated with adjuvant chemotherapy. This is the first study to correlate high CXCR4 expression to better TNBC prognosis, and the underlying mechanism needs to be elucidated in further studies. -
Citations
Citations to this article as recorded by- Bisphenol A-induced cancer-associated adipocytes promotes breast carcinogenesis via CXCL12/AKT signaling
Zhiyuan Dong, Liping He, Jinyi Wu, Chunfeng Xie, Shanshan Geng, Jieshu Wu, Caiyun Zhong, Xiaoting Li
Molecular and Cellular Endocrinology.2025; 599: 112473. CrossRef - Dissecting the tumor microenvironment in primary breast angiosarcoma: insights from single-cell RNA sequencing
Peikai Ding, Shengbin Pei, Yi Zhai, Zheng Qu, Yazhe Yang, Xiaolong Feng, Qiang Liu, Xiangyu Wang, Wenxiang Zhang, Zhongzhao Wang, Xiangyi Kong, Jing Wang, Yi Fang
Breast Cancer Research.2025;[Epub] CrossRef - CXCR4 expression in colorectal cancer and tumor stage correlation
Fang Cao, Yang Zhang, Jianhao Xu, Jiarui Min, Jihao Su, Zhe Chen, Jingfeng Gu, Zijie Xu, Song Xu
Gene Reports.2025; 40: 102281. CrossRef - Distinct profiles of proliferating CD8+/TCF1+ T cells and CD163+/PD-L1+ macrophages predict risk of relapse differently among treatment-naïve breast cancer subtypes
Konstantinos Ntostoglou, Sofia D. P. Theodorou, Tanja Proctor, Ilias P. Nikas, Sinclair Awounvo, Athanasia Sepsa, Vassilis Georgoulias, Han Suk Ryu, Ioannis S. Pateras, Christos Kittas
Cancer Immunology, Immunotherapy.2024;[Epub] CrossRef - Unravelling the CXCL12/CXCR4 Axis in breast cancer: Insights into metastasis, microenvironment interactions, and therapeutic opportunities
Priyanka Garg, Venkateswara Rao Jallepalli, Sonali Verma
Human Gene.2024; 40: 201272. CrossRef - New Emerging Chemokine Receptors: CCR5 or CXCR5 on Tumor Is Associated with Poor Response to Chemotherapy and Poor Prognosis in Locally Advanced Triple-Negative Breast Cancer
Neslihan Cabioglu, Semen Onder, Hüseyin Karatay, Aysel Bayram, Gizem Oner, Mustafa Tukenmez, Mahmut Muslumanoglu, Abdullah Igci, Ahmet Dinccag, Vahit Ozmen, Adnan Aydiner, Pınar Saip, Ekrem Yavuz
Cancers.2024; 16(13): 2388. CrossRef - Cancer-Associated-Fibroblast-Mediated Paracrine and Autocrine SDF-1/CXCR4 Signaling Promotes Stemness and Aggressiveness of Colorectal Cancers
Chao-Yang Chen, Shih-Hsien Yang, Ping-Ying Chang, Su-Feng Chen, Shin Nieh, Wen-Yen Huang, Yu-Chun Lin, Oscar Kuang-Sheng Lee
Cells.2024; 13(16): 1334. CrossRef - Associations of CXCL12 polymorphisms with clinicopathological features in breast cancer: a case-control study
Shuai Lin, Yi Zheng, Meng Wang, Linghui Zhou, Yuyao Zhu, Yujiao Deng, Ying Wu, Dai Zhang, Na Li, Huafeng Kang, Zhijun Dai
Molecular Biology Reports.2022; 49(3): 2255. CrossRef - The clinicopathological and prognostic value of CXCR4 expression in patients with lung cancer: a meta-analysis
Liping Qiu, Yuanyuan Xu, Hui Xu, Biyun Yu
BMC Cancer.2022;[Epub] CrossRef - Demystifying the CXCR4 conundrum in cancer biology: Beyond the surface signaling paradigm
Mushtaq Ahmad Nengroo, Muqtada Ali Khan, Ayushi Verma, Dipak Datta
Biochimica et Biophysica Acta (BBA) - Reviews on Cancer.2022; 1877(5): 188790. CrossRef - Targeted dendrimers for antagonizing the migration and viability of NALM-6 lymphoblastic leukemia cells
Chuda Chittasupho, Chaiyawat Aonsri, Witcha Imaram
Bioorganic Chemistry.2021; 107: 104601. CrossRef - CXCR4 and RANK Combination as a Predictor of Breast Cancer Bone Metastasis in Indonesia
Yulian Erwin D
Journal of Surgery and Surgical Research.2021; : 020. CrossRef - CXCL12/CXCR4 axis in the microenvironment of solid tumors: A critical mediator of metastasis
Keywan Mortezaee
Life Sciences.2020; 249: 117534. CrossRef - Impact of the Chemokine Receptors CXCR4 and CXCR7 on Clinical Outcome in Adrenocortical Carcinoma
Irina Chifu, Britta Heinze, Carmina T. Fuss, Katharina Lang, Matthias Kroiss, Stefan Kircher, Cristina L. Ronchi, Barbara Altieri, Andreas Schirbel, Martin Fassnacht, Stefanie Hahner
Frontiers in Endocrinology.2020;[Epub] CrossRef
- Bisphenol A-induced cancer-associated adipocytes promotes breast carcinogenesis via CXCL12/AKT signaling
- Detection of Human Papillomavirus in Korean Breast Cancer Patients by Real-Time Polymerase Chain Reaction and Meta-Analysis of Human Papillomavirus and Breast Cancer
- Jinhyuk Choi, Chungyeul Kim, Hye Seung Lee, Yoo Jin Choi, Ha Yeon Kim, Jinhwan Lee, Hyeyoon Chang, Aeree Kim
- J Pathol Transl Med. 2016;50(6):442-450. Published online October 10, 2016
- DOI: https://doi.org/10.4132/jptm.2016.07.08
- 14,092 View
- 225 Download
- 15 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) is a well-established oncogenic virus of cervical, anogenital, and oropharyngeal cancer. Various subtypes of HPV have been detected in 0% to 60% of breast cancers. The roles of HPV in the carcinogenesis of breast cancer remain controversial. This study was performed to determine the prevalence of HPV-positive breast cancer in Korean patients and to evaluate the possibility of carcinogenic effect of HPV on breast.
Methods
Meta-analysis was performed in 22 case-control studies for HPV infection in breast cancer. A total of 123 breast cancers, nine intraductal papillomas and 13 nipple tissues of patients with proven cervical HPV infection were tested by real-time polymerase chain reaction to detect 28 subtypes of HPV. Breast cancers were composed of 106 formalin-fixed and paraffin embedded (FFPE) breast cancer samples and 17 touch imprint cytology samples of breast cancers.
Results
The overall odds ratio between breast cancer and HPV infection was 5.43 (95% confidence interval, 3.24 to 9.12) with I2 = 34.5% in meta-analysis of published studies with case-control setting and it was statistically significant. HPV was detected in 22 cases of breast cancers (17.9%) and two cases of intaductal papillomas (22.2%). However, these cases had weak positivity.
Conclusions
These results failed to serve as significant evidence to support the relationship between HPV and breast cancer. Further study with larger epidemiologic population is merited to determine the relationship between HPV and breast cancer. -
Citations
Citations to this article as recorded by- HPV, APOBEC3B, and the origins of breast cancer: a narrative review and perspectives on novel mechanisms
Zhi-yong Liu, Ran Chen
Frontiers in Oncology.2026;[Epub] CrossRef - Advances in human papillomavirus detection for cervical cancer screening and diagnosis: challenges of conventional methods and opportunities for emergent tools
O. Fashedemi, Okoroike C. Ozoemena, Siwaphiwe Peteni, Aderemi B. Haruna, Leshweni J. Shai, Aicheng Chen, Frankie Rawson, Maggie E. Cruickshank, David Grant, Oluwafunmilola Ola, Kenneth I. Ozoemena
Analytical Methods.2025; 17(7): 1428. CrossRef - Bacterial-Viral Interactions in Human Orodigestive and Female Genital Tract Cancers: A Summary of Epidemiologic and Laboratory Evidence
Ikuko Kato, Jilei Zhang, Jun Sun
Cancers.2022; 14(2): 425. CrossRef - Breast cancer association with oncogenic papillomaviruses: papillomaviral DNA detection in breast cancer cells
G. M. Volgareva
Advances in Molecular Oncology.2022; 9(2): 10. CrossRef - Presence of Human Papillomavirus DNA in Malignant Neoplasia and Non-Malignant Breast Disease
Erika Maldonado-Rodríguez, Marisa Hernández-Barrales, Adrián Reyes-López, Susana Godina-González, Perla I. Gallegos-Flores, Edgar L. Esparza-Ibarra, Irma E. González-Curiel, Jesús Aguayo-Rojas, Adrián López-Saucedo, Gretel Mendoza-Almanza, Jorge L. Ayala-
Current Issues in Molecular Biology.2022; 44(8): 3648. CrossRef - Risk Role of Breast Cancer in Association with Human Papilloma Virus among Female Population in Taiwan: A Nationwide Population-Based Cohort Study
Chia-Hsin Liu, Chi-You Liao, Ming-Hsin Yeh, James Cheng-Chung Wei
Healthcare.2022; 10(11): 2235. CrossRef - HPV-Associated Breast Cancer: Myth or Fact?
Erik Kudela, Eva Kudelova, Erik Kozubík, Tomas Rokos, Terezia Pribulova, Veronika Holubekova, Kamil Biringer
Pathogens.2022; 11(12): 1510. CrossRef - Assessment of Human Papillomavirus Infection and Risk Factors in Egyptian Women With Breast Cancer
Nabila El-Sheikh, Nahla O Mousa, Amany M Tawfeik, Alaa M Saleh, Iman Elshikh, Mohamed Deyab, Faten Ragheb, Manar M Moneer, Ahmed Kawashti, Ahmed Osman, Mohamed Elrefaei
Breast Cancer: Basic and Clinical Research.2021;[Epub] CrossRef - Human Papillomavirus (HPV) Detection by Chromogenic In Situ Hybridization (CISH) and p16 Immunohistochemistry (IHC) in Breast Intraductal Papilloma and Breast Carcinoma
Hua Guo, Juan P. Idrovo, Jin Cao, Sudarshana Roychoudhury, Pooja Navale, Louis J. Auguste, Tawfiqul Bhuiya, Silvat Sheikh-Fayyaz
Clinical Breast Cancer.2021; 21(6): e638. CrossRef - Human Papillomavirus in Breast Carcinogenesis: A Passenger, a Cofactor, or a Causal Agent?
Rancés Blanco, Diego Carrillo-Beltrán, Juan P. Muñoz, Alejandro H. Corvalán, Gloria M. Calaf, Francisco Aguayo
Biology.2021; 10(8): 804. CrossRef - Systematic review and meta-analysis of the papillomavirus prevalence in breast cancer fresh tissues
Geilson Gomes de Oliveira, Ana Katherine Gonçalves, José Eleutério, Luiz Gonzaga Porto Pinheiro
Breast Disease.2021; 41(1): 123. CrossRef - Is human papillomavirus associated with breast cancer or papilloma presenting with pathologic nipple discharge?
Fatih Levent Balci, Cihan Uras, Sheldon Marc Feldman
Cancer Treatment and Research Communications.2019; 19: 100122. CrossRef - Is the HPV virus responsible for the development of breast cancer?
Erik Kudela, Marcela Nachajova, Jan Danko
The Breast Journal.2019; 25(5): 1053. CrossRef - Absence of Human Papillomavirus in Benign and Malignant Breast Tissue
Maryam Kazemi Aghdam, Seyed Alireza Nadji, Azadeh Alvandimanesh, Maliheh Khoddami, Yassaman Khademi
Iranian Journal of Pathology.2019; 14(4): 279. CrossRef - Oncogenic Viruses and Breast Cancer: Mouse Mammary Tumor Virus (MMTV), Bovine Leukemia Virus (BLV), Human Papilloma Virus (HPV), and Epstein–Barr Virus (EBV)
James S. Lawson, Brian Salmons, Wendy K. Glenn
Frontiers in Oncology.2018;[Epub] CrossRef - Viral infections and breast cancer – A current perspective
O.M. Gannon, A. Antonsson, I.C. Bennett, N.A. Saunders
Cancer Letters.2018; 420: 182. CrossRef - Prevalence of EBV, HPV and MMTV in Pakistani breast cancer patients: A possible etiological role of viruses in breast cancer
Wasifa Naushad, Orooj Surriya, Hajra Sadia
Infection, Genetics and Evolution.2017; 54: 230. CrossRef
- HPV, APOBEC3B, and the origins of breast cancer: a narrative review and perspectives on novel mechanisms
- Pathologic Evaluation of Breast Cancer after Neoadjuvant Therapy
- Cheol Keun Park, Woo-Hee Jung, Ja Seung Koo
- J Pathol Transl Med. 2016;50(3):173-180. Published online April 11, 2016
- DOI: https://doi.org/10.4132/jptm.2016.02.02
- 17,638 View
- 562 Download
- 33 Web of Science
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF - Breast cancer, one of the most common cancers in women, has various treatment modalities. Neoadjuvant therapy (NAT) has been used in many clinical trials because it is easy to evaluate the treatment response to therapeutic agents in a short time period; consequently, NAT is currently a standard treatment modality for large-sized and locally advanced breast cancers, and its use in early-stage breast cancer is becoming more common. Thus, chances to encounter breast tissue from patients treated with NAT is increasing. However, systems for handling and evaluating such specimens have not been established. Several evaluation systems emphasize a multidisciplinary approach to increase the accuracy of breast cancer assessment. Thus, detailed and systematic evaluation of clinical, radiologic, and pathologic findings is important. In this review, we compare the major problems of each evaluation system and discuss important points for handling and evaluating NAT-treated breast specimens.
-
Citations
Citations to this article as recorded by- Application of Multimodal Radiomics in Assessing Neoadjuvant Therapeutic Efficacy for Breast Cancer
聪 刘
Journal of Clinical Personalized Medicine.2026; 05(01): 324. CrossRef - Evaluating the Tumor Burden, Histological Changes, and Immune Landscape of Breast Cancer Post-neoadjuvant Chemotherapy: Insights From 50 Cases
Arasi Rajesh, Dharma Saranya Gurusamy, Rajalakshmi Manikkam
Cureus.2025;[Epub] CrossRef - Prognostic value of residual cancer burden after neoadjuvant chemotherapy in breast cancer: a comprehensive subtype-specific analysis
Soo-Young Lee, Tae-Kyung Yoo, Sae Byul Lee, Jisun Kim, Il Yong Chung, Beom Seok Ko, Hee Jeong Kim, Jong Won Lee, Byung Ho Son
Scientific Reports.2025;[Epub] CrossRef - Comparison of Tru-Cut and Surgical Biopsy Specimens in Breast Carcinoma Cases Undergoing Neoadjuvant Chemotherapy
Tuba Devrim, Gamze Erkılınç, Saniye Sevim Tuncer, Helin Tinas Abacı, Fazilet Uğur Duman, Eyup Kebapçı
Dicle Tıp Dergisi.2025; 52(4): 827. CrossRef - Good practice: The experiences with the utilization of residual cancer burden—A single institution study
Anita Sejben, Fanni Hegedűs, Szintia Almási, Márton Berta, Orsolya Oláh‐Németh, Tamás Zombori
Thoracic Cancer.2023; 14(11): 963. CrossRef - Assessing the Correlation of Rate of Pathological Complete Response and Outcome in Post Neoadjuvant Chemotherapy Setting and Molecular Subtypes of Breast Cancer
Ahmad Omair, Abdulmohsen Alkushi, Ghaida Alamri, Talal Almojel, Sara Alsadun, Emad Masuadi, Haitham Arabi, Amin E Mohamed, Omalkhair A Abulkhair
Cureus.2023;[Epub] CrossRef - Compression OCT-elastography combined with speckle-contrast analysis as an approach to the morphological assessment of breast cancer tissue
Anton A. Plekhanov, Ekaterina V. Gubarkova, Marina A. Sirotkina, Alexander A. Sovetsky, Dmitry A. Vorontsov, Lev A. Matveev, Sergey S. Kuznetsov, Alexandra Y. Bogomolova, Alexey Y. Vorontsov, Alexander L. Matveyev, Sergey V. Gamayunov, Elena V. Zagaynova,
Biomedical Optics Express.2023; 14(6): 3037. CrossRef - Ambiguity-aware breast tumor cellularity estimation via self-ensemble label distribution learning
Xiangyu Li, Xinjie Liang, Gongning Luo, Wei Wang, Kuanquan Wang, Shuo Li
Medical Image Analysis.2023; 90: 102944. CrossRef - Concurrent Chemo-radiation As a Means of Achieving Pathologic Complete Response in Triple Negative Breast Cancer
Maryam Nemati Shafaee, Shalini Makawita, Bora Lim, Matthew J Ellis, Michelle S Ludwig
Clinical Breast Cancer.2022; 22(4): e536. CrossRef - Pathology after neoadjuvant treatment – How to assess residual disease
Giuseppe Viale, Nicola Fusco
The Breast.2022; 62: S25. CrossRef - Efficacy Evaluation of Neoadjuvant Chemotherapy in Breast Cancer by MRI
Yongguang Liu, Mingxiang Wu, Wenyong Tan, Jingshan Gong, Jie Ma, Mohammad Farukh Hashmi
Contrast Media & Molecular Imaging.2022;[Epub] CrossRef - Predictive Role of Soluble IL-6R, TNF-R1/2, and Cell Adhesion Molecules Serum Levels in the Preoperative and Adjuvant Therapy in Women with Nonmetastatic Breast Cancer: A Preliminary Study
Weronika Bulska-Będkowska, Paulina Czajka-Francuz, Sylwia Cisoń-Jurek, Aleksander J. Owczarek, Tomasz Francuz, Jerzy Chudek
Journal of Interferon & Cytokine Research.2022; 42(11): 557. CrossRef - The prognostic role of lymph node ratio in breast cancer patients received neoadjuvant chemotherapy: A dose-response meta-analysis
Jinzhao Liu, Yifei Li, Weifang Zhang, Chenhui Yang, Chao Yang, Liang Chen, Mingjian Ding, Liang Zhang, Xiaojun Liu, Guozhong Cui, Yunjiang Liu
Frontiers in Surgery.2022;[Epub] CrossRef - The Role of miR-375-3p, miR-210-3p and Let-7e-5p in the Pathological Response of Breast Cancer Patients to Neoadjuvant Therapy
Lorena Alexandra Lisencu, Andrei Roman, Simona Visan, Eduard-Alexandru Bonci, Andrei Pașca, Emilia Grigorescu, Elena Mustea, Andrei Cismaru, Alexandru Irimie, Cosmin Lisencu, Loredana Balacescu, Ovidiu Balacescu, Oana Tudoran
Medicina.2022; 58(10): 1494. CrossRef - Post-Neoadjuvant Treatment Strategies for Patients with Early Breast Cancer
Elisa Agostinetto, Flavia Jacobs, Véronique Debien, Alex De Caluwé, Catalin-Florin Pop, Xavier Catteau, Philippe Aftimos, Evandro de Azambuja, Laurence Buisseret
Cancers.2022; 14(21): 5467. CrossRef - Tumor Microenvironment in Breast Cancer—Updates on Therapeutic Implications and Pathologic Assessment
Joshua J. Li, Julia Y. Tsang, Gary M. Tse
Cancers.2021; 13(16): 4233. CrossRef - SPIE-AAPM-NCI BreastPathQ challenge: an image analysis challenge for quantitative tumor cellularity assessment in breast cancer histology images following neoadjuvant treatment
Nicholas Petrick, Shazia Akbar, Kenny H. Cha, Sharon Nofech-Mozes, Berkman Sahiner, Marios A. Gavrielides, Jayashree Kalpathy-Cramer, Karen Drukker, Anne L. Martel, for the BreastPathQ Challenge Group
Journal of Medical Imaging.2021;[Epub] CrossRef - Diagnostic performance of digital breast tomosynthesis for predicting response to neoadjuvant systemic therapy in breast cancer patients: A comparison with magnetic resonance imaging, ultrasound, and full-field digital mammography
Ryusuke Murakami, Hitomi Tani, Shinichiro Kumita, Nachiko Uchiyama
Acta Radiologica Open.2021;[Epub] CrossRef - Los márgenes
Laia Bernet, María Angeles Montero Fernández
Revista de Senología y Patología Mamaria.2021; 34: S25. CrossRef - Neoadjuvant chemotherapy in non‐metastatic breast cancer: a study on practice trends in a regional cancer treatment service
Edmond Ang, Navin Wewala, Rebecca Carroll, Garry Forgeson, Malcolm Anderson, Jennifer Fernando, Jody Jordan, Richard Isaacs
Internal Medicine Journal.2020; 50(3): 315. CrossRef - Examination of Tumor Regression Grading Systems in Breast Cancer Patients Who Received Neoadjuvant Therapy
Anita Sejben, Renáta Kószó, Zsuzsanna Kahán, Gábor Cserni, Tamás Zombori
Pathology & Oncology Research.2020; 26(4): 2747. CrossRef - Integrating evolutionary dynamics into cancer therapy
Robert A. Gatenby, Joel S. Brown
Nature Reviews Clinical Oncology.2020; 17(11): 675. CrossRef - Assessing the accuracy of conventional gadolinium‐enhanced breast MRI in measuring the nodal response to neoadjuvant chemotherapy (NAC) in breast cancer
Lisa Christine Murphy, Edel Marie Quinn, Zeeshan Razzaq, Claire Brady, Vicki Livingstone, Lorna Duddy, Josephine Barry, Henry Paul Redmond, Mark Anthony Corrigan
The Breast Journal.2020; 26(11): 2151. CrossRef - Early prediction of neoadjuvant chemotherapy response for advanced breast cancer using PET/MRI image deep learning
Joon Ho Choi, Hyun-Ah Kim, Wook Kim, Ilhan Lim, Inki Lee, Byung Hyun Byun, Woo Chul Noh, Min-Ki Seong, Seung-Sook Lee, Byung Il Kim, Chang Woon Choi, Sang Moo Lim, Sang-Keun Woo
Scientific Reports.2020;[Epub] CrossRef - Patterns of Regression in Breast Cancer after Primary Systemic Treatment
Tamás Zombori, Gábor Cserni
Pathology & Oncology Research.2019; 25(3): 1153. CrossRef - The Role of Neutrophil-lymphocyte Ratio and Platelet-lymphocyte Ratio in Predicting Neoadjuvant Chemotherapy Response in Breast Cancer
Hee Yeon Kim, Tae Hyun Kim, Hye Kyoung Yoon, Anbok Lee
Journal of Breast Cancer.2019; 22(3): 425. CrossRef - Higher underestimation of tumour size post-neoadjuvant chemotherapy with breast magnetic resonance imaging (MRI)—A concordance comparison cohort analysis
Wen-Pei Wu, Hwa-Koon Wu, Chih-Jung Chen, Chih-Wie Lee, Shou-Tung Chen, Dar-Ren Chen, Chen-Te Chou, Chi Wei Mok, Hung-Wen Lai, Pascal A. T. Baltzer
PLOS ONE.2019; 14(10): e0222917. CrossRef - Multimodal image-guided surgery of HER2-positive breast cancer using [111In]In-DTPA-trastuzumab-IRDye800CW in an orthotopic breast tumor model
Marion M. Deken, Desirée L. Bos, Willemieke S. F. J. Tummers, Taryn L. March, Cornelis J. H. van de Velde, Mark Rijpkema, Alexander L. Vahrmeijer
EJNMMI Research.2019;[Epub] CrossRef - Mammographic density is a potential predictive marker of pathological response after neoadjuvant chemotherapy in breast cancer
Ida Skarping, Daniel Förnvik, Hanna Sartor, Uffe Heide-Jørgensen, Sophia Zackrisson, Signe Borgquist
BMC Cancer.2019;[Epub] CrossRef - ALDH1 and tumor infiltrating lymphocytes as predictors for neoadjuvant chemotherapy response in breast cancer
Anbok Lee, Kyu Yeoun Won, Sung-Jig Lim, Sun Young Cho, Sang-Ah Han, SaeGwang Park, Jeong-Yoon Song
Pathology - Research and Practice.2018; 214(5): 619. CrossRef - Early Prediction of Response to Neoadjuvant Chemotherapy Using Dynamic Contrast-Enhanced MRI and Ultrasound in Breast Cancer
Yunju Kim, Sung Hun Kim, Byung Joo Song, Bong Joo Kang, Kwang-il Yim, Ahwon Lee, Yoonho Nam
Korean Journal of Radiology.2018; 19(4): 682. CrossRef - Outcomes of neoadjuvant and adjuvant chemotherapy in stage 2 and 3 non-small cell lung cancer: an analysis of the National Cancer Database
Matthew MacLean, Xin Luo, Shidan Wang, Kemp Kernstine, David E. Gerber, Yang Xie
Oncotarget.2018; 9(36): 24470. CrossRef - Automatic cellularity assessment from post‐treated breast surgical specimens
Mohammad Peikari, Sherine Salama, Sharon Nofech‐Mozes, Anne L. Martel
Cytometry Part A.2017; 91(11): 1078. CrossRef - The importance of tissue confirmation of metastatic disease in patients with breast cancer: lesson from a brain metastasis case
Jingxian Ding, Pinghua Hu, Jun Chen, Xiaobo Wu, Yali Cao
Oncoscience.2016; 3(9-10): 268. CrossRef
- Application of Multimodal Radiomics in Assessing Neoadjuvant Therapeutic Efficacy for Breast Cancer
- Interobserver Variability of Ki-67 Measurement in Breast Cancer
- Yul Ri Chung, Min Hye Jang, So Yeon Park, Gyungyub Gong, Woo-Hee Jung, The Korean Breast Pathology Ki- Study Group
- J Pathol Transl Med. 2016;50(2):129-137. Published online February 15, 2016
- DOI: https://doi.org/10.4132/jptm.2015.12.24
- 12,941 View
- 130 Download
- 29 Web of Science
- 29 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
As measurement of Ki-67 proliferation index is an important part of breast cancer diagnostics, we conducted a multicenter study to examine the degree of concordance in Ki-67 counting and to find factors that lead to its variability. Methods: Thirty observers from thirty different institutions reviewed Ki-67–stained slides of 20 different breast cancers on whole sections and tissue microarray (TMA) by online system. Ten of the 20 breast cancers had hot spots of Ki-67 expression. Each observer scored Ki-67 in two different ways: direct counting (average vs. hot spot method) and categorical estimation. Intraclass correlation coefficient (ICC) of Ki-67 index was calculated for comparative analysis. Results: For direct counting, ICC of TMA was slightly higher than that of whole sections using average method (0.895 vs 0.858). The ICC of tumors with hot spots was lower than that of tumors without (0.736 vs 0.874). In tumors with hot spots, observers took an additional counting from the hot spot; the ICC of whole sections using hot spot method was still lower than that of TMA (0.737 vs 0.895). In categorical estimation, Ki-67 index showed a wide distribution in some cases. Nevertheless, in tumors with hot spots, the range of distribution in Ki-67 categories was decreased with hot spot method and in TMA platform. Conclusions: Interobserver variability of Ki-67 index for direct counting and categorical estimation was relatively high. Tumors with hot spots showed greater interobserver variability as opposed to those without, and restricting the measurement area yielded lower interobserver variability. -
Citations
Citations to this article as recorded by- Comparative analysis of Ki-67 labeling index morphometry using deep learning, conventional image analysis, and manual counting
Mohammad Rizwan Alam, Kyung Jin Seo, Kwangil Yim, Phoebe Liang, Joe Yeh, Chifu Chang, Yosep Chong
Translational Oncology.2025; 51: 102159. CrossRef - Machine Learning-Based Approaches for Breast Density Estimation from Mammograms: A Comprehensive Review
Khaldoon Alhusari, Salam Dhou
Journal of Imaging.2025; 11(2): 38. CrossRef - Letter re: A critical appraisal of the DATA trial analysis on the prognostic and predictive value of the luminal-like subtype
M. Rizk, K. Mokbel
ESMO Open.2025; 10(5): 105067. CrossRef - Clinico-Histomorphological and Mib-1 Analysis of Recurrent Meningiomas: A Retrospective Study
Sujata Sarangi, Asha Shenoy, Ashvini Kolhe, Kanchan Kothari
Asian Journal of Neurosurgery.2025; 20(04): 785. CrossRef - Emerging Diagnostics and Therapies in Neuroendocrine Neoplasms: A Critical Review
Jorge H. Hernandez-Felix, Monica Isabel Meneses-Medina, Rachel Riechelmann, Jonathan Strosberg, Rocio Garcia-Carbonero, Jaydira del Rivero
Cancers.2025; 17(22): 3632. CrossRef - Ki-67 Testing in Breast Cancer: Assessing Variability With Scoring Methods and Specimen Types and the Potential Subsequent Impact on Therapy Eligibility
Therese Bocklage, Virgilius Cornea, Caylin Hickey, Justin Miller, Jessica Moss, Mara Chambers, S. Emily Bachert
Applied Immunohistochemistry & Molecular Morphology.2024; 32(3): 119. CrossRef - Interobserver agreement and diagnostic challenges of Congo red staining for amyloid detection on fat pad aspiration biopsies
Levent Trabzonlu, T. Leif Helland, Melanie C. Kwan, Nathalie Kumiega, M. Lisa Zhang, Ivan Chebib, Vanda F. Torous
Journal of the American Society of Cytopathology.2024; 13(5): 359. CrossRef - Assessment of the Predictive Role of Ki-67 in Breast Cancer Patients’ Responses to Neoadjuvant Chemotherapy
Ghizlane Rais, Rania Mokfi, Farah Boutaggount, Meryem Maskrout, Soundouss Bennour, Chaymae Senoussi, Fadoua Rais
European Journal of Breast Health.2024; : 199. CrossRef - Improving the accuracy of reporting Ki-67 IHC by using an AI tool
Sahil Ajit Saraf, Aahan Singh, Wai Po Kevin Teng, Sencer Karakaya, M. Logaswari, Kaveh Taghipour, Rajasa Jialdasani, Li Yan Khor, Kiat Hon Lim, Sathiyamoorthy Selvarajan, Vani Ravikumar, Md Ali Osama, Priti Chatterjee, Santosh KV
Heliyon.2024; 10(22): e40193. CrossRef - Predictive Value of Ki-67 Index in Evaluating Sporadic Vestibular Schwannoma Recurrence: Systematic Review and Meta-analysis
Kunal Vakharia, Hirotaka Hasegawa, Christopher Graffeo, Mohammad H. A. Noureldine, Salomon Cohen-Cohen, Avital Perry, Matthew L. Carlson, Colin L. W. Driscoll, Maria Peris-Celda, Jamie J. Van Gompel, Michael J. Link
Journal of Neurological Surgery Part B: Skull Base.2023; 84(02): 119. CrossRef - Venous invasion and lymphatic invasion are correlated with the postoperative prognosis of pancreatic neuroendocrine neoplasm
Sho Kiritani, Junichi Arita, Yuichiro Mihara, Rihito Nagata, Akihiko Ichida, Yoshikuni Kawaguchi, Takeaki Ishizawa, Nobuhisa Akamatsu, Junichi Kaneko, Kiyoshi Hasegawa
Surgery.2023; 173(2): 365. CrossRef - Automated Molecular Subtyping of Breast Carcinoma Using Deep Learning Techniques
S. Niyas, Ramya Bygari, Rachita Naik, Bhavishya Viswanath, Dhananjay Ugwekar, Tojo Mathew, J Kavya, Jyoti R Kini, Jeny Rajan
IEEE Journal of Translational Engineering in Health and Medicine.2023; 11: 161. CrossRef - Grade Progression and Intrapatient Tumor Heterogeneity as Potential Contributors to Resistance in Gastroenteropancreatic Neuroendocrine Tumors
Diana Grace Varghese, Jaydira Del Rivero, Emily Bergsland
Cancers.2023; 15(14): 3712. CrossRef - Diagnostic Role and Prognostic Impact of PSAP Immunohistochemistry: A Tissue Microarray Study on 31,358 Cancer Tissues
Laura Sophie Tribian, Maximilian Lennartz, Doris Höflmayer, Noémi de Wispelaere, Sebastian Dwertmann Rico, Clara von Bargen, Simon Kind, Viktor Reiswich, Florian Viehweger, Florian Lutz, Veit Bertram, Christoph Fraune, Natalia Gorbokon, Sören Weidemann, C
Diagnostics.2023; 13(20): 3242. CrossRef - AI-Powered Segmentation of Invasive Carcinoma Regions in Breast Cancer Immunohistochemical Whole-Slide Images
Yiqing Liu, Tiantian Zhen, Yuqiu Fu, Yizhi Wang, Yonghong He, Anjia Han, Huijuan Shi
Cancers.2023; 16(1): 167. CrossRef - Expression of estrogen and progesterone receptors, HER2 protein and Ki-67 proliferation index in breast carcinoma in both tumor tissue and tissue microarray
UP Hacısalihoğlu, MA Dogan
Biotechnic & Histochemistry.2022; 97(4): 298. CrossRef - Diffusive Ki67 and vimentin are associated with worse recurrence-free survival of upper tract urothelial carcinoma: A retrospective cohort study from bench to bedside
Che Hsueh Yang, Wei Chun Weng, Yen Chuan Ou, Yi Sheng Lin, Li Hua Huang, Chin Heng Lu, Tang Yi Tsao, Chao Yu Hsu, Min Che Tung
Urologic Oncology: Seminars and Original Investigations.2022; 40(3): 109.e21. CrossRef - Should Ki-67 be adopted to select breast cancer patients for treatment with adjuvant abemaciclib?
P. Tarantino, H.J. Burstein, N.U. Lin, I.E. Krop, E.P. Winer, S.J. Schnitt, E.P. Hamilton, S.A. Hurvitz, H.S. Rugo, G. Curigliano, S.M. Tolaney
Annals of Oncology.2022; 33(3): 234. CrossRef - A novel deep classifier framework for automated molecular subtyping of breast carcinoma using immunohistochemistry image analysis
Tojo Mathew, S. Niyas, C.I. Johnpaul, Jyoti R. Kini, Jeny Rajan
Biomedical Signal Processing and Control.2022; 76: 103657. CrossRef - Deep learning for the standardized classification of Ki-67 in vulva carcinoma: A feasibility study
Matthias Choschzick, Mariam Alyahiaoui, Alexander Ciritsis, Cristina Rossi, André Gut, Patryk Hejduk, Andreas Boss
Heliyon.2021; 7(7): e07577. CrossRef - Oncotype DX Predictive Nomogram for Recurrence Score Output: The Novel System ADAPTED01 Based on Quantitative Immunochemistry Analysis
Fabio Marazzi, Roberto Barone, Valeria Masiello, Valentina Magri, Antonino Mulè, Angela Santoro, Federica Cacciatori, Luca Boldrini, Gianluca Franceschini, Francesca Moschella, Giuseppe Naso, Silverio Tomao, Maria Antonietta Gambacorta, Giovanna Mantini,
Clinical Breast Cancer.2020; 20(5): e600. CrossRef - Study of Ki-67 index in the molecular subtypes of breast cancer: Inter-observer variability and automated scoring
Divya Meermira, Meenakshi Swain, Swarnalata Gowrishankar
Indian Journal of Cancer.2020; 57(3): 289. CrossRef - Improving the accuracy of gastrointestinal neuroendocrine tumor grading with deep learning
Darshana Govind, Kuang-Yu Jen, Karen Matsukuma, Guofeng Gao, Kristin A. Olson, Dorina Gui, Gregory. E. Wilding, Samuel P. Border, Pinaki Sarder
Scientific Reports.2020;[Epub] CrossRef - Practical approaches to automated digital image analysis of Ki-67 labeling index in 997 breast carcinomas and causes of discordance with visual assessment
Ah-Young Kwon, Ha Young Park, Jiyeon Hyeon, Seok Jin Nam, Seok Won Kim, Jeong Eon Lee, Jong-Han Yu, Se Kyung Lee, Soo Youn Cho, Eun Yoon Cho, Irina V. Lebedeva
PLOS ONE.2019; 14(2): e0212309. CrossRef - Evaluation of Ki-67 Index in Core Needle Biopsies and Matched Breast Cancer Surgical Specimens
Soomin Ahn, Junghye Lee, Min-Sun Cho, Sanghui Park, Sun Hee Sung
Archives of Pathology & Laboratory Medicine.2018; 142(3): 364. CrossRef - Assessment of Ki-67 for Predicting Effective Prognosis in Breast Cancer Subtypes
Sangjung Park, Sunyoung Park, Jungho Kim, Sungwoo Ahn, Kwang Hwa Park, Hyeyoung Lee
Biomedical Science Letters.2018; 24(1): 9. CrossRef - Quantitative tumor heterogeneity assessment on a nuclear population basis
Anne‐Sofie Wessel Lindberg, Knut Conradsen, Rasmus Larsen, Michael Friis Lippert, Rasmus Røge, Mogens Vyberg
Cytometry Part A.2017; 91(6): 574. CrossRef - A comparison of Ki-67 counting methods in luminal Breast Cancer: The Average Method vs. the Hot Spot Method
Min Hye Jang, Hyun Jung Kim, Yul Ri Chung, Yangkyu Lee, So Yeon Park, William B. Coleman
PLOS ONE.2017; 12(2): e0172031. CrossRef - A Novel Breast Cancer Index for Prediction of Distant Recurrence in HR+ Early-Stage Breast Cancer with One to Three Positive Nodes
Yi Zhang, Brock E. Schroeder, Piiha-Lotta Jerevall, Amy Ly, Hannah Nolan, Catherine A. Schnabel, Dennis C. Sgroi
Clinical Cancer Research.2017; 23(23): 7217. CrossRef
- Comparative analysis of Ki-67 labeling index morphometry using deep learning, conventional image analysis, and manual counting
- Current Issues and Clinical Evidence in Tumor-Infiltrating Lymphocytes in Breast Cancer
- Sung Gwe Ahn, Joon Jeong, SoonWon Hong, Woo Hee Jung
- J Pathol Transl Med. 2015;49(5):355-363. Published online August 17, 2015
- DOI: https://doi.org/10.4132/jptm.2015.07.29
- 16,170 View
- 244 Download
- 45 Web of Science
- 37 Crossref
-
 Abstract
Abstract
 PDF
PDF - With the advance in personalized therapeutic strategies in patients with breast cancer, there is an increasing need for biomarker-guided therapy. Although the immunogenicity of breast cancer has not been strongly considered in research or practice, tumor-infiltrating lymphocytes (TILs) are emerging as biomarkers mediating tumor response to treatments. Earlier studies have provided evidence that the level of TILs has prognostic value and the potential for predictive value, particularly in triple-negative and human epidermal growth factor receptor 2–positive breast cancer. Moreover, the level of TILs has been associated with treatment outcome in patients undergoing neoadjuvant chemotherapy. To date, no standardized methodology for measuring TILs has been established. In this article, we review current issues and clinical evidence for the use of TILs in breast cancer.
-
Citations
Citations to this article as recorded by- Cytokine Networks in Triple-Negative Breast Cancer: Mechanisms, Therapeutic Targets, and Emerging Strategies
María Rosado-Sanz, Nuria Martínez-Alarcón, Adrián Abellán-Soriano, Raúl Golfe, Eva M. Trinidad, Jaime Font de Mora
Biomedicines.2025; 13(8): 1945. CrossRef - Unveiling Metabolic Signatures as Potential Biomarkers in Common Cancers: Insights from Lung, Breast, Colorectal, Liver, and Gastric Tumours
Kha Wai Hon, Rakesh Naidu
Biomolecules.2025; 15(10): 1376. CrossRef - Systemic chemotherapy in metastatic TNBC polarizes effector T cell differentiation
Hye-Yeon Ju, Hyundong Yoon, Seungpil Jung, Serk In Park, Tae Kon Kim, Mi-Ryung Han
Cancer Cell International.2025;[Epub] CrossRef - Immune characteristics and clinical significance of peripheral blood lymphocytes in breast cancer
Hongyu Gao, Dengjie Ouyang, Xinyu Guan, Jiachi Xu, Qitong Chen, Liyun Zeng, Jian Pang, Qiongyan Zou, Ke Qian, Wenjun Yi
BMC Cancer.2024;[Epub] CrossRef - Precision unveiled: Synergistic genomic landscapes in breast cancer—Integrating single‐cell analysis and decoding drug toxicity for elite prognostication and tailored therapeutics
Chenglu Jiang, Shengke Zhang, Lai Jiang, Zipei Chen, Haiqing Chen, Jinbang Huang, Jingyi Tang, Xiufang Luo, Guanhu Yang, Jie Liu, Hao Chi
Environmental Toxicology.2024; 39(6): 3448. CrossRef - Exploring histological predictive biomarkers for immune checkpoint inhibitor therapy response in non–small cell lung cancer
Uiju Cho, Soyoung Im, Hyung Soon Park
Journal of Pathology and Translational Medicine.2024; 58(2): 49. CrossRef - Review: Merging from traditional to potential novel breast cancer biomarkers
Hanan Alismail
Journal of King Saud University - Science.2024; 36(11): 103551. CrossRef - A non-inferiority, phase III trial of gemcitabine plus capecitabine versus gemcitabine plus carboplatin as first-line therapy and tumor-infiltrating lymphocytes as a prognostic biomarker in patients with advanced triple-negative breast cancer
Xiaodong Liu, Weipeng Zhao, Yongsheng Jia, Yehui Shi, Xu Wang, Shufen Li, Pin Zhang, Chen Wang, Chunfang Hao, Zhongsheng Tong
Therapeutic Advances in Medical Oncology.2024;[Epub] CrossRef - Predictive and Prognostic Role of Tumor‐Infiltrating Lymphocytes in Patients with Advanced Breast Cancer Treated with Primary Systemic Therapy
Gaurav Agarwal, K. M. M. Vishvak Chanthar, Shweta Katiyar, Niraj Kumari, Narendra Krishnani, M. Sabaretnam, Gyan Chand, Anjali Mishra, Punita Lal
World Journal of Surgery.2023; 47(5): 1238. CrossRef - The role of tumor-infiltrating lymphocytes in triple-negative breast cancer and the research progress of adoptive cell therapy
Ruonan Li, Lili Cao
Frontiers in Immunology.2023;[Epub] CrossRef - Using Self-Assembling ADDomer Platform to Display B and T Epitopes of Type O Foot-and-Mouth Disease Virus
Chaowei Luo, Quanhui Yan, Juncong Huang, Jiameng Liu, Yuwan Li, Keke Wu, Bingke Li, Mingqiu Zhao, Shuangqi Fan, Hongxing Ding, Jinding Chen
Viruses.2022; 14(8): 1810. CrossRef - Modification of the Tumor Microenvironment Enhances Anti-PD-1 Immunotherapy in Metastatic Melanoma
Guilan Shi, Megan Scott, Cathryn G. Mangiamele, Richard Heller
Pharmaceutics.2022; 14(11): 2429. CrossRef - Assessment of Immune Status in Dynamics for Patients with Cancer Undergoing Immunotherapy
Bacinschi Xenia Elena, Laurentia Nicoleta Gales, Anca Florina Zgura, Laura Iliescu, Rodica Maricela Anghel, Bogdan Haineala, Xiaosheng Wang
Journal of Oncology.2021; 2021: 1. CrossRef - Differences in immune-related gene expressions and tumor-infiltrating lymphocytes according to chemotherapeutic response in ovarian high-grade serous carcinoma
Kyung Un Choi, Ahrong Kim, Jee Yeon Kim, Ki Hyung Kim, Chungsu Hwang, So Jung Lee, Won Young Park, Sejin Jung, Hye Jeong Choi, Kyungbin Kim
Journal of Ovarian Research.2020;[Epub] CrossRef Predictors of Neoadjuvant Chemotherapy Response in Breast Cancer: A Review
Weilin Xu, Xiu Chen, Fei Deng, Jian Zhang, Wei Zhang, Jinhai Tang
OncoTargets and Therapy.2020; Volume 13: 5887. CrossRef- Immune phenotype of patients with stage IV metastatic inflammatory breast cancer
Sandra V. Fernandez, Alexander W. MacFarlane, Mowafaq Jillab, Maria F. Arisi, Jennifer Yearley, Lakshmanan Annamalai, Yulan Gong, Kathy Q. Cai, R. Katherine Alpaugh, Massimo Cristofanilli, Kerry S. Campbell
Breast Cancer Research.2020;[Epub] CrossRef - Infiltrating stromal immune cells in inflammatory breast cancer are associated with an improved outcome and increased PD-L1 expression
C. Van Berckelaer, C. Rypens, P. van Dam, L. Pouillon, M. Parizel, K. A. Schats, M. Kockx, W. A. A. Tjalma, P. Vermeulen, S. van Laere, F. Bertucci, C. Colpaert, L. Dirix
Breast Cancer Research.2019;[Epub] CrossRef - The composition of T cell infiltrates varies in primary invasive breast cancer of different molecular subtypes as well as according to tumor size and nodal status
Anna Glajcar, Joanna Szpor, Diana Hodorowicz-Zaniewska, Katarzyna Ewa Tyrak, Krzysztof Okoń
Virchows Archiv.2019; 475(1): 13. CrossRef - Retinoid X receptor agonist LG100268 modulates the immune microenvironment in preclinical breast cancer models
Ana S. Leal, Kayla Zydeck, Sarah Carapellucci, Lyndsey A. Reich, Di Zhang, Jessica A. Moerland, Michael B. Sporn, Karen T. Liby
npj Breast Cancer.2019;[Epub] CrossRef - Stromal tumor‑infiltrating lymphocytes evaluated on H&E‑stained slides are an independent prognostic factor in epithelial ovarian cancer and ovarian serous carcinoma
Chungsu Hwang, So Lee, Jung Lee, Ki Kim, Dong Suh, Byung‑Su Kwon, Kyung Choi
Oncology Letters.2019;[Epub] CrossRef - The therapeutic candidate for immune checkpoint inhibitors elucidated by the status of tumor-infiltrating lymphocytes (TILs) and programmed death ligand 1 (PD-L1) expression in triple negative breast cancer (TNBC)
Nobumoto Tomioka, Manabu Azuma, Mayuko Ikarashi, Mitsugu Yamamoto, Masako Sato, Ken-ichi Watanabe, Katsushige Yamashiro, Masato Takahashi
Breast Cancer.2018; 25(1): 34. CrossRef - Triple negative breast cancer – prognostic role of immune-related factors: a systematic review
Elisabeth Specht Stovgaard, Dorte Nielsen, Estrid Hogdall, Eva Balslev
Acta Oncologica.2018; 57(1): 74. CrossRef - Lack of effective translational regulation of PLD expression and exosome biogenesis in triple-negative breast cancer cells
Julian Gomez-Cambronero
Cancer and Metastasis Reviews.2018; 37(2-3): 491. CrossRef - Expression of Myxovirus Resistance A (MxA) Is Associated with Tumor-Infiltrating Lymphocytes in Human Epidermal Growth Factor Receptor 2 (HER2)–Positive Breast Cancers
So Jeong Lee, Cheong-Soo Hwang, Young-Keum Kim, Hyun Jung Lee, Sang-Jeong Ahn, Nari Shin, Jung Hee Lee, Dong Hoon Shin, Kyung Un Choi, Do Youn Park, Chang Hun Lee, Gi Young Huh, Mi Young Sol, Hee Jin Lee, Gyungyub Gong, Jee Yeon Kim, Ahrong Kim
Cancer Research and Treatment.2017; 49(2): 313. CrossRef - Glutaminase expression is a poor prognostic factor in node-positive triple-negative breast cancer patients with a high level of tumor-infiltrating lymphocytes
Joo Young Kim, Sun-Hee Heo, Seul Ki Choi, In Hye Song, In Ah Park, Young-Ae Kim, Hye Seon Park, Suk Young Park, Won Seon Bang, Gyungyub Gong, Hee Jin Lee
Virchows Archiv.2017; 470(4): 381. CrossRef - Whole Slide Imaging for Analytical Anatomic Pathology and Telepathology: Practical Applications Today, Promises, and Perils
Alton Brad Farris, Cynthia Cohen, Thomas E. Rogers, Geoffrey H. Smith
Archives of Pathology & Laboratory Medicine.2017; 141(4): 542. CrossRef - Tumor-infiltrating lymphocytes and breast cancer: Beyond the prognostic and predictive utility
Andrea Ravelli, Giandomenico Roviello, Daniele Cretella, Andrea Cavazzoni, Alessandra Biondi, Maria Rosa Cappelletti, Laura Zanotti, Giuseppina Ferrero, Marco Ungari, Fabrizio Zanconati, Alberto Bottini, Roberta Alfieri, Pier Giorgio Petronini, Daniele Ge
Tumor Biology.2017; 39(4): 101042831769502. CrossRef - Predictive Value of Tertiary Lymphoid Structures Assessed by High Endothelial Venule Counts in the Neoadjuvant Setting of Triple-Negative Breast Cancer
In Hye Song, Sun-Hee Heo, Won Seon Bang, Hye Seon Park, In Ah Park, Young-Ae Kim, Suk Young Park, Jin Roh, Gyungyub Gong, Hee Jin Lee
Cancer Research and Treatment.2017; 49(2): 399. CrossRef - Lymphocyte count or percentage: which can better predict the prognosis of advanced cancer patients following palliative care?
Weiwei Zhao, Peng Wang, Huixun Jia, Menglei Chen, Xiaoli Gu, Minghui Liu, Zhe Zhang, Wenwu Cheng, Zhenyu Wu
BMC Cancer.2017;[Epub] CrossRef - Programmed death-ligand 1 (PD-L1) expression in tumour cell and tumour infiltrating lymphocytes of HER2-positive breast cancer and its prognostic value
Ahrong Kim, So Jeong Lee, Young Keum Kim, Won Young Park, Do Youn Park, Jee Yeon Kim, Chang Hun Lee, Gyungyub Gong, Gi Yeong Huh, Kyung Un Choi
Scientific Reports.2017;[Epub] CrossRef - Negative association between GATA3 and fascin could predict relapse-free and overall survival in patients with breast cancer
Kyueng-Whan Min, Dong-Hoon Kim, Sung-Im Do, Seoung Wan Chae, Kyungeun Kim, Jin Hee Sohn, Jung-Soo Pyo, Hyun Joo Lee, Dong Hyun Kim, Sukjoong Oh, Seon Hyeong Choi, Yong Lai Park, Chan Heun Park, Eun-Kyung Kim, Mi Jung Kwon, Jinwon Seo, Kyoung Min Moon
Virchows Archiv.2016; 468(4): 409. CrossRef - Cytoplasmic expression of high mobility group B1 (HMGB1) is associated with tumor‐infiltrating lymphocytes (TILs) in breast cancer
Hee Jin Lee, Ahrong Kim, In Hye Song, In Ah Park, Jong Han Yu, Jin Hee Ahn, Gyungyub Gong
Pathology International.2016; 66(4): 202. CrossRef - Clinical pharmacologic aspects of immune checkpoint inhibitors in cancer therapy
Kyu-pyo Kim, Hun Jung
Translational and Clinical Pharmacology.2016; 24(1): 7. CrossRef - The next level of 3D tumour models: immunocompetence
Agata Nyga, Joana Neves, Katerina Stamati, Marilena Loizidou, Mark Emberton, Umber Cheema
Drug Discovery Today.2016; 21(9): 1421. CrossRef - An Examination of the Local Cellular Immune Response to Examples of Both Ductal Carcinoma In Situ (DCIS) of the Breast and DCIS With Microinvasion, With Emphasis on Tertiary Lymphoid Structures and Tumor Infiltrating Lymphoctytes
Ahrong Kim, Sun-Hee Heo, Young-Ae Kim, Gyungyub Gong, Hee Jin Lee
American Journal of Clinical Pathology.2016; 146(1): 137. CrossRef - High Ki67/BCL2 index is associated with worse outcome in early stage breast cancer
Kyueng-Whan Min, Dong-Hoon Kim, Sung-Im Do, Jung-Soo Pyo, Seoung Wan Chae, Jin Hee Sohn, Kyungeun Kim, Hyun Joo Lee, Dong Hyun Kim, Sukjoong Oh, Seon Hyeong Choi, Yong Lai Park, Chan Heun Park, Mi Jung Kwon, Kyoung Min Moon
Postgraduate Medical Journal.2016; 92(1094): 707. CrossRef - Expression of T-Lymphocyte Markers in Human Epidermal Growth Factor Receptor 2-Positive Breast Cancer
Changro Lee, Seho Park, Joo Heung Kim, Sung Mook Lim, Hyung Seok Park, Seung Il Kim, Byeong-Woo Park
Journal of Breast Cancer.2016; 19(4): 385. CrossRef
- Cytokine Networks in Triple-Negative Breast Cancer: Mechanisms, Therapeutic Targets, and Emerging Strategies
- Microtubule-Associated Protein Tau, α-Tubulin and βIII-Tubulin Expression in Breast Cancer
- Soyoung Im, Changyoung Yoo, Ji-Han Jung, Ye-Won Jeon, Young Jin Suh, Youn Soo Lee, Hyun Joo Choi
- Korean J Pathol. 2013;47(6):534-540. Published online December 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.6.534
- 9,062 View
- 62 Download
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The microtubule-associated protein Tau binds to both inner and outer surfaces of microtubules, leading to tubulin assembly and microtubule stabilization. The aim of this study was to evaluate the significance of Tau, α-tubulin, and βIII-tubulin expression in breast carcinoma and to assess their relationships with disease progression in the context of taxane treatment.
Methods Immunohistochemical expressions of Tau, α-tubulin, and βIII-tubulin were assessed in 183 breast cancer cases. Expression was correlated with clinicopathologic parameters, disease progression and overall survival.
Results Tau expression was correlated with lymph node metastasis and estrogen receptor (ER) positivity (p=.003 and p<.001, respectively). Loss of α-tubulin was significantly correlated with distant metastasis (p=.034). Loss of βIII-tubulin was correlated with lymph node metastasis and ER positivity (p=.004 and p<.001, respectively). In taxane-treated cases, Tau expression and loss of α-tubulin and βIII-tubulin expression were related to disease progression (p=.001, p=.028, and p=.030, respectively). Tau expression was associated with a worse survival rate in taxane-treated patients (p=.049).
Conclusions Tau expression and loss of α-tubulin and βIII-tubulin expression were correlated with aggressive behavior in taxane-treated breast cancer. Further evaluation of Tau, α-tubulin and βIII-tubulin may be useful in predicting clinical behavior and seeking therapeutic measures in taxane-based chemotherapy for breast cancer.
-
Citations
Citations to this article as recorded by- Cytoskeletal dynamics in breast cancer: mechanistic insights and therapeutic opportunities
RamaRao Malla, Anshu Tumbali, Pavani Chode, Krithika Manda, Anuveda Sree Samudrala, Yerusha Nuthalapati, Charanteja Mangam, Priyamvada Bhamidipati, Mundla Srilatha, Ganji Purnachandra Nagaraju
Journal of the National Cancer Center.2025;[Epub] CrossRef - Genes Related to Motility in an Ionizing Radiation and Estrogen Breast Cancer Model
Tania Koning, Gloria M. Calaf
Biology.2024; 13(11): 849. CrossRef - Tubulin Isotypes: Emerging Roles in Defining Cancer Stem Cell Niche
Tessy Thomas Maliekal, Dhrishya Dharmapal, Suparna Sengupta
Frontiers in Immunology.2022;[Epub] CrossRef - RAD6 inhibition enhances paclitaxel sensitivity of triple negative breast cancer cells by aggravating mitotic spindle damage
Brittany M. Haynes, Kristen Cunningham, Malathy P. V. Shekhar
BMC Cancer.2022;[Epub] CrossRef - Influence of Paclitaxel and Doxorubicin Therapy of ßIII-Tubulin, Carbonic Anhydrase IX, and Survivin in Chemically Induced Breast Cancer in Female Rat
Alena Pastornická, Silvia Rybárová, Slávka Drahošová, Jozef Mihalik, Andrea Kreheľová, Andriana Pavliuk-Karachevtseva, Ingrid Hodorová
International Journal of Molecular Sciences.2021; 22(12): 6363. CrossRef - Intelligently thermoresponsive flower-like hollow nano-ruthenium system for sustained release of nerve growth factor to inhibit hyperphosphorylation of tau and neuronal damage for the treatment of Alzheimer's disease
Hui Zhou, Youcong Gong, Yanan Liu, Anlian Huang, Xufeng Zhu, Jiawei Liu, Guanglong Yuan, Li Zhang, Ji-an Wei, Jie Liu
Biomaterials.2020; 237: 119822. CrossRef - HE4 promotes collateral resistance to cisplatin and paclitaxel in ovarian cancer cells
J. R. Ribeiro, C. Schorl, N. Yano, N. Romano, K. K. Kim, R. K. Singh, R. G. Moore
Journal of Ovarian Research.2016;[Epub] CrossRef - A strategy to identify housekeeping genes suitable for analysis in breast cancer diseases
Tatiana M. Tilli, Cláudio da Silva Castro, Jack A. Tuszynski, Nicolas Carels
BMC Genomics.2016;[Epub] CrossRef - Increased expression of αTubulin is associated with poor prognosis in patients with pancreatic cancer after surgical resection
Chao Lin, Guo-chao Zhao, Ya-dong Xu, Dan-song Wang, Da-yong Jin, Yuan Ji, Wen-hui Lou, Wen-chuan Wu
Oncotarget.2016; 7(37): 60657. CrossRef - Oblongifolin C inhibits metastasis by up-regulating keratin 18 and tubulins
Xiaoyu Wang, Yuanzhi Lao, Naihan Xu, Zhichao Xi, Man Wu, Hua Wang, Xiyi Li, Hongsheng Tan, Menghong Sun, Hongxi Xu
Scientific Reports.2015;[Epub] CrossRef - Regulation of human MAPT gene expression
Marie-Laure Caillet-Boudin, Luc Buée, Nicolas Sergeant, Bruno Lefebvre
Molecular Neurodegeneration.2015;[Epub] CrossRef
- Cytoskeletal dynamics in breast cancer: mechanistic insights and therapeutic opportunities
- Hedgehog Related Protein Expression in Breast Cancer: Gli-2 Is Associated with Poor Overall Survival
- Soyoung Im, Hyun Joo Choi, Changyoung Yoo, Ji-Han Jung, Ye-Won Jeon, Young Jin Suh, Chang Suk Kang
- Korean J Pathol. 2013;47(2):116-123. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.116
- 9,668 View
- 98 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The hedgehog (Hh) signaling pathway is known to play a critical role in various malignancies, but its clinicopathologic role in breast cancer is yet to be established.
Methods Tissue microarray blocks from 334 cases of breast cancer were prepared. The expression of six Hh signaling proteins including sonic hedgehog (Shh), patched (Ptch), smoothened (Smo), and the glioma-associated oncogene (Gli)-1, Gli-2, and Gli-3 were analyzed immunohistochemically.
Results The expression of Hh signaling proteins was significantly correlated with some prognostic factors including the correlation of lymph node metastasis with the expression of Shh (p=0.001) and Ptch (p=0.064), the correlation of the stages with Shh and Gli-3 expression (p=0.007 and p=0.024, respectively), the correlation of the nuclear grade with the Smo (p=0.004) and Gli-3 (p=0.000), and the correlation of the histologic grade with the Ptch (p=0.016), Smo (p=0.007), and Gli-3 (p=0.000). The Shh, Ptch, Smo, Gli-1, and Gli-2 expression was significantly different between the phenotypes (p=0.000, p=0.001, p=0.004, p=0.039, and p=0.031, respectively). Gli-2 expression was correlated with a worse overall survival outcome (p=0.012).
Conclusions Hh pathway activation is correlated with a more aggressive clinical behavior in breast carcinomas. The comparison of phenotypes suggested that the Hh pathway may be a useful therapeutic target for breast carcinoma. Patients with Gli-2 expression had a significantly lower overall survival rate and, therefore, it showed promise as a prognostic marker.
-
Citations
Citations to this article as recorded by- Dysregulation of deubiquitination in breast cancer
Lili Kong, Xiaofeng Jin
Gene.2024; 902: 148175. CrossRef - siRNA treatment targeting integrin α11 overexpressed via EZH2-driven axis inhibits drug-resistant breast cancer progression
Prakash Chaudhary, Kiran Yadav, Ho Jin Lee, Keon Wook Kang, Jongseo Mo, Jung-Ae Kim
Breast Cancer Research.2024;[Epub] CrossRef - Implicating clinical utility of altered expression of PTCH1 & SMO in oral squamous cell carcinoma
Hitarth V. Patel, Jigna S. Joshi, Franky D. Shah
Journal of Molecular Histology.2024; 55(4): 379. CrossRef - A clinicopathological exploration of Hedgehog signaling: implications in oral carcinogenesis
Hitarth V. Patel, Jigna S. Joshi, Franky D. Shah
Journal of Cancer Research and Clinical Oncology.2023; 149(18): 16525. CrossRef - GLI3 and androgen receptor are mutually dependent for their malignancy-promoting activity in ovarian and breast cancer cells
Min Lin, Haiyan Zhu, Qi Shen, Lu-Zhe Sun, Xueqiong Zhu
Cellular Signalling.2022; 92: 110278. CrossRef - Persistent Properties of a Subpopulation of Cancer Cells Overexpressing the Hedgehog Receptor Patched
Álvaro Javier Feliz Morel, Anida Hasanovic, Aurélie Morin, Chloé Prunier, Virginie Magnone, Kevin Lebrigand, Amaury Aouad, Sarah Cogoluegnes, Judith Favier, Claude Pasquier, Isabelle Mus-Veteau
Pharmaceutics.2022; 14(5): 988. CrossRef - Case Report: Submucosal gastroblastoma with a novel PTCH1::GLI2 gene fusion in a 58-year-old man
Cuimin Chen, Junliang Lu, Huanwen Wu
Frontiers in Oncology.2022;[Epub] CrossRef - Higher Expressions of SHH and AR Are Associated with a Positive Receptor Status and Have Impact on Survival in a Cohort of Croatian Breast Cancer Patients
Ivan Budimir, Čedna Tomasović-Lončarić, Kristina Kralik, Josipa Čonkaš, Domagoj Eljuga, Rado Žic, Božo Gorjanc, Hrvoje Tucaković, Doroteja Caktaš, Josip Jaman, Valentino Lisek, Zlatko Vlajčić, Krešimir Martić, Petar Ozretić
Life.2022; 12(10): 1559. CrossRef - New insight into the role of PTCH1 protein in serous ovarian carcinomas
Valentina Karin‑Kujundzic, Adriana Covarrubias‑Pinto, Anita Skrtic, Semir Vranic, Ljiljana Serman
International Journal of Oncology.2022;[Epub] CrossRef - Hedgehog gene expression patterns among intrinsic subtypes of breast cancer: Prognostic relevance
Araceli García-Martínez, Ariadna Pérez-Balaguer, Fernando Ortiz-Martínez, Eloy Pomares-Navarro, Elena Sanmartín, Marta García-Escolano, Yoel G. Montoyo-Pujol, Elena Castellón-Molla, Gloria Peiró
Pathology - Research and Practice.2021; 223: 153478. CrossRef - Coexpression of Epha10 and Gli3 Promotes Breast Cancer Cell Proliferation, Invasion and Migration
Jing Peng, Danhua Zhang
Journal of Investigative Medicine.2021; 69(6): 1215. CrossRef - The Role of Smoothened-Dependent and -Independent Hedgehog Signaling Pathway in Tumorigenesis
Jian Yi Chai, Vaisnevee Sugumar, Mohammed Abdullah Alshawsh, Won Fen Wong, Aditya Arya, Pei Pei Chong, Chung Yeng Looi
Biomedicines.2021; 9(9): 1188. CrossRef - HER2-mediated GLI2 stabilization promotes anoikis resistance and metastasis of breast cancer cells
Parul Gupta, Nehal Gupta, Neel M. Fofaria, Alok Ranjan, Sanjay K. Srivastava
Cancer Letters.2019; 442: 68. CrossRef - Role of Hedgehog Signaling in Breast Cancer: Pathogenesis and Therapeutics
Natalia Riobo-Del Galdo, Ángela Lara Montero, Eva Wertheimer
Cells.2019; 8(4): 375. CrossRef - Carbonic anhydrase XII expression is linked to suppression of Sonic hedgehog ligand expression in triple negative breast cancer cells
G. Guerrini, J. Durivault, I. Filippi, M. Criscuoli, S. Monaci, J. Pouyssegur, A. Naldini, F. Carraro, S.K. Parks
Biochemical and Biophysical Research Communications.2019; 516(2): 408. CrossRef - Sonic hedgehog and Wnt/β-catenin pathways mediate curcumin inhibition of breast cancer stem cells
Xiaoting Li, Xiaoqian Wang, Chunfeng Xie, Jianyun Zhu, Yu Meng, Yue Chen, Yuan Li, Ye Jiang, Xue Yang, Shijia Wang, Jiaqi Chen, Qi Zhang, Shanshan Geng, Jieshu Wu, Caiyun Zhong, Yu Zhao
Anti-Cancer Drugs.2018; 29(3): 208. CrossRef - Glioma-Associated Oncogene Homolog Inhibitors Have the Potential of Suppressing Cancer Stem Cells of Breast Cancer
Kuo-Shyang Jeng, Chi-Juei Jeng, I-Shyan Sheen, Szu-Hua Wu, Ssu-Jung Lu, Chih-Hsuan Wang, Chiung-Fang Chang
International Journal of Molecular Sciences.2018; 19(5): 1375. CrossRef - Cancer Stem Cell Metabolism and Potential Therapeutic Targets
Vusala Snyder, Tamika C. Reed-Newman, Levi Arnold, Sufi Mary Thomas, Shrikant Anant
Frontiers in Oncology.2018;[Epub] CrossRef - Targeting the Multidrug Transporter Ptch1 Potentiates Chemotherapy Efficiency
Anida Hasanovic, Isabelle Mus-Veteau
Cells.2018; 7(8): 107. CrossRef - Combined inhibition of GLI and FLT3 signaling leads to effective anti-leukemic effects in human acute myeloid leukemia
Emily-Marie Latuske, Hauke Stamm, Marianne Klokow, Gabi Vohwinkel, Jana Muschhammer, Carsten Bokemeyer, Manfred Jücker, Maxim Kebenko, Walter Fiedler, Jasmin Wellbrock
Oncotarget.2017; 8(17): 29187. CrossRef - Prognostic role of Gli1 expression in breast cancer: a meta-analysis
Bilan Wang, Ting Yu, Yuzhu Hu, Mengmeng Xiang, Haoning Peng, Yunzhu Lin, Lu Han, Lingli Zhang
Oncotarget.2017; 8(46): 81088. CrossRef - Inhibition of Ciliogenesis Promotes Hedgehog Signaling, Tumorigenesis, and Metastasis in Breast Cancer
Nadia B. Hassounah, Martha Nunez, Colleen Fordyce, Denise Roe, Ray Nagle, Thomas Bunch, Kimberly M. McDermott
Molecular Cancer Research.2017; 15(10): 1421. CrossRef - The sonic hedgehog signaling pathway contributes to the development of salivary gland neoplasms regardless of perineural infiltration
Manuela Torres Andion Vidal, Sílvia Vanessa Lourenço, Fernando Augusto Soares, Clarissa Araújo Gurgel, Eduardo J. B. Studart, Ludmila de Faro Valverde, Iguaracyra Barreto de Oliveira Araújo, Eduardo Antônio Gonçalves Ramos, Flávia Caló de Aquino Xavier, J
Tumor Biology.2016; 37(7): 9587. CrossRef - Cancer stem cells and HER2 positive breast cancer: The story so far
Deep Shah, Clodia Osipo
Genes & Diseases.2016; 3(2): 114. CrossRef - Tamoxifen Resistance: Emerging Molecular Targets
Milena Rondón-Lagos, Victoria Villegas, Nelson Rangel, Magda Sánchez, Peter Zaphiropoulos
International Journal of Molecular Sciences.2016; 17(8): 1357. CrossRef - The Hedgehog signaling pathway is associated with poor prognosis in breast cancer patients with the CD44+/CD24− phenotype
Haishan Zhao, Hongtao Tang, Qinghuan Xiao, Miao He, Lin Zhao, Yingzi Fu, Huizhe Wu, Zhaojin Yu, Qian Jiang, Yuanyuan Yan, Feng Jin, Minjie Wei
Molecular Medicine Reports.2016; 14(6): 5261. CrossRef - Significance of the hedgehog pathway-associated proteins Gli-1 and Gli-2 and the epithelial-mesenchymal transition-associated proteins Twist and E-cadherin in hepatocellular carcinoma
Hyung Wook Chun, Ran Hong
Oncology Letters.2016; 12(3): 1753. CrossRef - Taxane‐induced hedgehog signaling is linked to expansion of breast cancer stem‐like populations after chemotherapy
Jennifer Sims‐Mourtada, Lynn M. Opdenaker, Joshua Davis, Kimberly M. Arnold, Daniel Flynn
Molecular Carcinogenesis.2015; 54(11): 1480. CrossRef - Loss of Tumor Suppressor ARID1A Protein Expression Correlates with Poor Prognosis in Patients with Primary Breast Cancer
Hyun Deuk Cho, Jong Eun Lee, Hae Yoen Jung, Mee-Hye Oh, Ji-Hye Lee, Si-Hyong Jang, Kyung-Ju Kim, Sun Wook Han, Sung Yong Kim, Han Jo Kim, Sang Byung Bae, Hyun Ju Lee
Journal of Breast Cancer.2015; 18(4): 339. CrossRef - Prognostic impact of the expression of Hedgehog proteins in cervical carcinoma FIGO stages I–IV treated with radiotherapy or chemoradiotherapy
Louise Bohr Mordhorst, Cecilia Ahlin, Bengt Sorbe
Gynecologic Oncology.2014; 135(2): 305. CrossRef - Sonic hedgehog signaling may promote invasion and metastasis of oral squamous cell carcinoma by activating MMP-9 and E-cadherin expression
Hai-Xia Fan, Shan Wang, Hong Zhao, Nian Liu, Dong Chen, Miao Sun, Jin-Hua Zheng
Medical Oncology.2014;[Epub] CrossRef
- Dysregulation of deubiquitination in breast cancer
EGFR Gene Amplification and Protein Expression in Invasive Ductal Carcinoma of the Breast- Won Hwangbo, Jeong Hyeon Lee, Sangjeong Ahn, Seojin Kim, Kyong Hwa Park, Chul Hwan Kim, Insun Kim
- Korean J Pathol. 2013;47(2):107-115. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.107
- 14,041 View
- 82 Download
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The epidermal growth factor receptor (EGFR) is a surrogate marker for basal-like breast cancer. A recent study suggested that EGFR may be used as a target for breast cancer treatment.
Methods A total of 706 invasive ductal carcinomas (IDC) of the breast were immunophenotyped, and 82 cases with EGFR protein expression were studied for
EGFR gene amplification.Results EGFR protein was expressed in 121 of 706 IDCs (17.1%); 5.9% were of luminal type, 25.3% of epidermal growth factor receptor 2 (HER-2) type, and 79.3% of basal-like tumors.
EGFR gene amplification and high polysomy (fluorescentin situ hybridization [FISH]-positive) were found in 18 of 82 cases (22.0%); 41.2% of the HER-2+, EGFR+, cytokeratin 5/6- (CK5/6-) group, 11.2% of the HER-2-, EGFR+, CK5/6- group, and 19.1% of the HER-2-, EGFR+, CK5/6+ group. FISH-positive cases were detected in 8.3% of the EGFR protein 1+ expression cases, 15.9% of 2+ expression cases, and 38.5% of 3+ expression cases. In group 2, the tumors had a high Ki-67 labeling (>60%), but the patients showed better disease-free survival than those with tumors that co-expressed HER-2 or CK5/6.Conclusions EGFR-directed therapy can be considered in breast cancer patients with EGFR protein overexpression and gene amplification, and its therapeutic implication should be determined in HER-2 type breast cancer patients.
-
Citations
Citations to this article as recorded by- An overview of phenylsulfonylfuroxan-based nitric oxide donors for cancer treatment
Chao Gao, Xingyu Li, Tong Liu, Wanning Wang, Jianhui Wu
Bioorganic Chemistry.2025; 154: 108020. CrossRef - Identification of a cross-talk between EGFR and Wnt/beta-catenin signaling pathways in HepG2 liver cancer cells
Gurjinder Singh, Md Mehedi Hossain, Aadil Qadir Bhat, Mir Owais Ayaz, Nasima Bano, Rafiqa Eachkoti, Mohd Jamal Dar
Cellular Signalling.2021; 79: 109885. CrossRef - Blocking c-MET/ERBB1 Axis Prevents Brain Metastasis in ERBB2+ Breast Cancer
Shailendra K. Gautam, Ranjana K. Kanchan, Jawed A. Siddiqui, Shailendra K. Maurya, Sanchita Rauth, Naveenkumar Perumal, Pranita Atri, Ramakanth C. Venkata, Kavita Mallya, Sameer Mirza, Moorthy P. Ponnusamy, Vimla Band, Sidharth Mahapatra, Maneesh Jain, Su
Cancers.2020; 12(10): 2838. CrossRef - Evaluation of lapatinib cytotoxicity and genotoxicity on MDA-MB-231 breast cancer cell line
Mona A.M. Abo-Zeid, Mahmoud T. Abo-Elfadl, Amira M. Gamal-Eldeen
Environmental Toxicology and Pharmacology.2019; 71: 103207. CrossRef - Improved characterization of the relationship between long intergenic non‐coding RNA Linc00152 and the occurrence and development of malignancies
Jiasheng Xu, Jingjing Guo, Yangkai Jiang, Yujun Liu, Kaili Liao, Zhonghua Fu, Zhenfang Xiong
Cancer Medicine.2019; 8(10): 4722. CrossRef - Relationship between EGFR expression and subcellular localization with cancer development and clinical outcome
Ge Yan, Mohamed E.M. Saeed, Sebastian Foersch, Jose Schneider, Wilfried Roth, Thomas Efferth
Oncotarget.2019; 10(20): 1918. CrossRef - A novel matrine derivative WM622 inhibits hepatocellular carcinoma by inhibiting PI3K/AKT signaling pathways
Xiao Sun, Xiao-bin Zhuo, Yi-ping Hu, Xuan Zheng, Qing-jie Zhao
Molecular and Cellular Biochemistry.2018; 449(1-2): 47. CrossRef - lncRNA LINC00152 knockdown had effects to suppress biological activity of lung cancer via EGFR/PI3K/AKT pathway
Yan Zhang, Cheng Xiang, Yuling Wang, Yuanyuan Duan, Ci Liu, Yongli Jin, Yajing Zhang
Biomedicine & Pharmacotherapy.2017; 94: 644. CrossRef - Copy Number Profiling of MammaPrint™ Genes Reveals Association with the Prognosis of Breast Cancer Patients
Areej Fatima, Fomaz Tariq, Muhammad Faraz Arshad Malik, Muhammad Qasim, Farhan Haq
Journal of Breast Cancer.2017; 20(3): 246. CrossRef - Evaluation of serum epidermal growth factor receptor (EGFR) in correlation to circulating tumor cells in patients with metastatic breast cancer
Malgorzata Banys-Paluchowski, Isabell Witzel, Sabine Riethdorf, Brigitte Rack, Wolfgang Janni, Peter A. Fasching, Erich-Franz Solomayer, Bahriye Aktas, Sabine Kasimir-Bauer, Klaus Pantel, Tanja Fehm, Volkmar Müller
Scientific Reports.2017;[Epub] CrossRef - EGFR Is Regulated by TFAP2C in Luminal Breast Cancer and Is a Target for Vandetanib
James P. De Andrade, Jung M. Park, Vivian W. Gu, George W. Woodfield, Mikhail V. Kulak, Allison W. Lorenzen, Vincent T. Wu, Sarah E. Van Dorin, Philip M. Spanheimer, Ronald J. Weigel
Molecular Cancer Therapeutics.2016; 15(3): 503. CrossRef - Prognostic and predictive values of EGFR overexpression and EGFR copy number alteration in HER2-positive breast cancer
H J Lee, A N Seo, E J Kim, M H Jang, Y J Kim, J H Kim, S-W Kim, H S Ryu, I A Park, S-A Im, G Gong, K H Jung, H J Kim, S Y Park
British Journal of Cancer.2015; 112(1): 103. CrossRef - Epidermal growth factor receptor protein overexpression and gene amplification are associated with aggressive biological behaviors of esophageal squamous cell carcinoma
GANG LIN, XIAO-JIANG SUN, QIAN-BO HAN, ZHUN WANG, YA-PING XU, JIA-LEI GU, WEI WU, GU ZHANG, JIN-LIN HU, WEN-YONG SUN, WEI-MIN MAO
Oncology Letters.2015; 10(2): 901. CrossRef - Immunohistochemical Classification of Primary and Secondary Glioblastomas
Kyu Sang Lee, Gheeyoung Choe, Kyung Han Nam, An Na Seo, Sumi Yun, Kyung Ju Kim, Hwa Jin Cho, Sung Hye Park
Korean Journal of Pathology.2013; 47(6): 541. CrossRef - A Comparison of Tumor Biology in Primary Ductal CarcinomaIn SituRecurring as Invasive Carcinoma versus a NewIn Situ
Wenjing Zhou, Christine Johansson, Karin Jirström, Anita Ringberg, Carl Blomqvist, Rose-Marie Amini, Marie-Louise Fjallskog, Fredrik Wärnberg
International Journal of Breast Cancer.2013; 2013: 1. CrossRef
- An overview of phenylsulfonylfuroxan-based nitric oxide donors for cancer treatment
- Expressional Difference of RHEB, HDAC1, and WEE1 Proteins in the Stromal Tumors of the Breast and Their Significance in Tumorigenesis
- Minseob Eom, Airi Han, Mi Jeong Lee, Kwang Hwa Park
- Korean J Pathol. 2012;46(4):324-330. Published online August 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.324
- 9,476 View
- 56 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Fibroadenoma (FA) and phyllodes tumor (PT) are stromal tumors of breast and are histologically similar. There are no established differences in tumorigenesis and oncogene expression among them. Ras homolog enriched in brain (RHEB) plays an important role in cell growth and cell-cycle control, histone deacetylase 1 (HDAC1) is an important factor in breast tumor progression and prognosis, and WEE1 homolog (WEE1) functions as a tumor suppressor. No studies on the expressional differences of these proteins in FA and PT have been reported to date.
Methods The expression of these proteins in FA, PT, and normal breast was compared. We used 102 cases of FA and 25 cases of benign PT.
Results In epithelial cells, the expression of RHEB, HDAC1, and WEE1 was lowest in PT, higher in FA, and most enhanced in normal breast. In addition, the expression of RHEB and HDAC1 was higher in the stromal cells of PT than in FA and normal breast.
Conclusions Both epithelial and stromal cells of FA and PT express these proteins, which indicates that epithelial cells play an important role in the development of stromal tumors. In addition, the expressional differences of these proteins may be associated with the tumorigenesis of breast stromal tumors.
-
Citations
Citations to this article as recorded by- Gut microbiota-derived 3-phenylpropionic acid promotes intestinal epithelial barrier function via AhR signaling
Jun Hu, Jianwei Chen, Xiaojian Xu, Qiliang Hou, Jing Ren, Xianghua Yan
Microbiome.2023;[Epub] CrossRef - Genome-scale meta-analysis of breast cancer datasets identifies promising targets for drug development
Reem Altaf, Humaira Nadeem, Mustafeez Mujtaba Babar, Umair Ilyas, Syed Aun Muhammad
Journal of Biological Research-Thessaloniki.2021;[Epub] CrossRef - Wee1 Kinase: A Potential Target to Overcome Tumor Resistance to Therapy
Francesca Esposito, Raffaella Giuffrida, Gabriele Raciti, Caterina Puglisi, Stefano Forte
International Journal of Molecular Sciences.2021; 22(19): 10689. CrossRef - MiR-503 enhances the radiosensitivity of laryngeal carcinoma cells via the inhibition of WEE1
Huimin Ma, Rong Lian, Zhiyan Wu, Xiao Li, Wenfa Yu, Yun Shang, Xixia Guo
Tumor Biology.2017; 39(10): 101042831770622. CrossRef - Rheb phosphorylation is involved in p38-regulated/activated protein kinase-mediated tumor suppression in liver cancer
MIN ZHENG, SHENGBING ZANG, LINNA XIE, XUETING FANG, YU ZHANG, XIAOJIE MA, JINGFENG LIU, DEXIN LIN, AIMIN HUANG
Oncology Letters.2015; 10(3): 1655. CrossRef - Expression of CDK1Tyr15, pCDK1Thr161, Cyclin B1 (Total) and pCyclin B1Ser126 in Vulvar Squamous Cell Carcinoma and Their Relations with Clinicopatological Features and Prognosis
Zhihui Wang, Ana Slipicevic, Mette Førsund, Claes G. Trope, Jahn M. Nesland, Ruth Holm, Xin-Yuan Guan
PLOS ONE.2015; 10(4): e0121398. CrossRef - High expression of wee1 is associated with malignancy in vulvar squamous cell carcinoma patients
Gry Irene Magnussen, Ellen Hellesylt, Jahn M Nesland, Claes G Trope, Vivi Ann Flørenes, Ruth Holm
BMC Cancer.2013;[Epub] CrossRef
- Gut microbiota-derived 3-phenylpropionic acid promotes intestinal epithelial barrier function via AhR signaling
- The Clinicopathologic Features of Molecular Apocrine Breast Cancer
- Yoon Jin Cha, Woo-Hee Jung, Ja Seung Koo
- Korean J Pathol. 2012;46(2):169-176. Published online April 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.2.169
- 8,369 View
- 52 Download
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Background To elucidate the clinicopathologic features and their implications on the immunohistochemistry in cases of molecular apocrine breast cancer (MABC).
Methods Immunohistochemical (IHC) staining for estrogen receptor (ER), human epidermal growth factor receptor 2 (HER-2), cytokeratin (CK) 5/6, epidermal growth factor receptor (EGFR), androgen receptor (AR), gamma-glutamyltrasferase 1 (GGT1) and Ki-67 was performed on tissue microarray breast cancer samples from 204 patients. Phenotypes of breast cancer were divided based on the IHC status of ER, AR and GGT1 into the following: luminal type, ER positive and AR and/or GGT1 positive; basal type, ER, AR, and GGT1 negative; non-basal type, ER positive and AR and GGT1 negative; and MABC type, ER negative and AR and/or GGT1 positive.
Results In our series of patients (n=204), there were 26 cases of MABC. Besides, there were 18, 60, and 100 cases of luminal type, basal type and non-basal type, respectively. The MABC demonstrated apocrine histology and a higher prevalence of HER-2 positivity than other phenotypes. With the basal type, the MABC manifested a more frequent expression of CK5/6 and EGFR and a higher Ki-67 index than other phenotypes (p<0.001). There were no significant differences in patient prognosis between the phenotypes of breast cancer.
Conclusions MABC are distinguishable from other phenotypes based on the apocrine histology and a higher expression rate of HER-2.
-
Citations
Citations to this article as recorded by- The role of histopathologic testing on apocrine carcinoma of the breast
Burak Ilhan, Selman Emiroğlu, Rustu Türkay, Rıdvan Ilhan
Current Problems in Cancer.2020; 44(2): 100501. CrossRef - Cancer du sein triple négatif exprimant le récepteur aux androgènes : de la biologie à la thérapeutique
Thomas Grellety
Bulletin du Cancer.2020; 107(4): 506. CrossRef - Triple‐negative apocrine carcinoma: A rare pathologic subtype with a better prognosis than other triple‐negative breast cancers
Cletus A. Arciero, Albert H. Diehl, Yuan Liu, Qin Sun, Theresa Gillespie, Xiaoxian Li, Preeti Subhedar
Journal of Surgical Oncology.2020; 122(6): 1232. CrossRef - Apocrine lesions of the breast: part 2 of a two-part review. Invasive apocrine carcinoma, the molecular apocrine signature and utility of immunohistochemistry in the diagnosis of apocrine lesions of the breast
Clare D'Arcy, Cecily M Quinn
Journal of Clinical Pathology.2019; 72(1): 7. CrossRef - Enhancing Abiraterone Acetate Efficacy in Androgen Receptor–positive Triple-negative Breast Cancer: Chk1 as a Potential Target
Thomas Grellety, Celine Callens, Elodie Richard, Adrien Briaux, Valérie Vélasco, Marina Pulido, Anthony Gonçalves, Pierre Gestraud, Gaetan MacGrogan, Hervé Bonnefoi, Bruno Cardinaud
Clinical Cancer Research.2019; 25(2): 856. CrossRef - A clinicopathologic study of invasive apocrine carcinoma of the breast: A single-center experience
Denira Imamovic, Nurija Bilalovic, Faruk Skenderi, Vanesa Beslagic, Timur Ceric, Berisa Hasanbegovic, Semir Beslija, Semir Vranic
The Breast Journal.2018; 24(6): 1105. CrossRef - Dose invasive apocrine adenocarcinoma has worse prognosis than invasive ductal carcinoma of breast: evidence from SEER database
Ning Zhang, Hanwen Zhang, Tong Chen, Qifeng Yang
Oncotarget.2017; 8(15): 24579. CrossRef - Pure Apocrine Carcinomas Represent a Clinicopathologically Distinct Androgen Receptor–Positive Subset of Triple-Negative Breast Cancers
Anne M. Mills, Chelsea E. Gottlieb, Scott M. Wendroth, Christiana M. Brenin, Kristen A. Atkins
American Journal of Surgical Pathology.2016; 40(8): 1109. CrossRef - Androgen Receptor: A Complex Therapeutic Target for Breast Cancer
Ramesh Narayanan, James Dalton
Cancers.2016; 8(12): 108. CrossRef - Early versus late distant metastasis and adjuvant chemotherapy alone versus both radiotherapy and chemotherapy in molecular apocrine breast cancer
Xiaozhen Liu, Yang Yang, Xiaolong Feng, Honghong Shen, Jian Liu, Xia Liu, Yun Niu
Oncotarget.2016; 7(31): 48905. CrossRef - Molecular and diagnostic features of apocrine breast lesions
Pavel Gromov, Jaime A Espinoza, Irina Gromova
Expert Review of Molecular Diagnostics.2015; 15(8): 1011. CrossRef - Prevalencia de receptores androgénicos en el cáncer de mama
Claudia Janeth Rodríguez-Silva, José Luis González-Vela, Ascary Alcides Velázquez-Pacheco
Gaceta Mexicana de Oncología.2015; 14(3): 135. CrossRef
- The role of histopathologic testing on apocrine carcinoma of the breast
- Mimicry of Minute Pulmonary Meningothelial-like Nodules to Metastatic Deposits in a Patient with Infiltrating Lobular Carcinoma: A Case Report and Review of the Literature
- Hala Kfoury, Maria A. Arafah, Maha M. Arafah, Sami Alnassar, Waseem Hajjar
- Korean J Pathol. 2012;46(1):87-91. Published online February 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.1.87
- 10,172 View
- 66 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Minute pulmonary meningothelial-like nodules (MPMNs) are incidentally found lesions in lung resection specimens and autopsies. MPMNs have been associated with neoplastic and non-neoplastic pulmonary conditions and occasionally with extrapulmonary diseases. We report a case of a female patient presenting with invasive lobular carcinoma of the breast and MPMNs, masquerading as metastatic deposits. We describe the morphological, immunohistochemical and ultrastructural features of MPMNs and emphasize the importance of their recognition for proper staging and treatment of patients. To our knowledge, this is the first case in the English literature describing this coexistence.
-
Citations
Citations to this article as recorded by- Diffuse pulmonary meningotheliomatosis with pan-TRK expression by immunohistochemistry: a novel finding and potential pitfall
Cansu Karakas, Michael A. Nead, Moises J. Velez
Diagnostic Pathology.2023;[Epub] CrossRef - Diffuse Pulmonary Meningotheliomatosis: Clinic-Pathologic Entity or Indolent Metastasis from Meningioma (or Both)?
Laura Melocchi, Giulio Rossi, Mirca Valli, Maria Cecilia Mengoli, Michele Mondoni, Luigi Lazzari-Agli, Giacomo Santandrea, Fabio Davoli, Chiara Baldovini, Alberto Cavazza, Thomas V. Colby
Diagnostics.2023; 13(4): 802. CrossRef - Pathological diagnosis and immunohistochemical analysis of minute pulmonary meningothelial-like nodules: A case report
Xin Ruan, Liu-Sheng Wu, Zheng-Yang Fan, Qi Liu, Jun Yan, Xiao-Qiang Li
World Journal of Clinical Cases.2023; 11(33): 8022. CrossRef - Benign disease prone to be misdiagnosed as malignant pulmonary nodules: Minute meningothelioid nodules
Xiao‐Xiao Peng, Li‐Xu Yan, Chao Liu, Si‐Yun Wang, Wen‐Feng Li, Xing Gao, Xue‐Wu Wei, Qing Zhou
Thoracic Cancer.2019; 10(5): 1182. CrossRef - Atypical finding of meningothelial-like inclusions in cervical lymph nodes
Rebecca Donkin, Andrew Dettrick, Penelope Wyche, Sarah Grigg
Pathology.2018; 50(7): 785. CrossRef - Minute Pulmonary Meningothelial-Like Nodules Simulating Hematogenous Lung Metastasis: A Case Report
Sang Kook Lee, Gi Jeong Kim, Young Jae Kim, Ah Young Leem, Eu Dong Hwang, Se Kyu Kim, Joon Chang, Young Ae Kang, Song Yee Kim
Tuberculosis and Respiratory Diseases.2013; 75(2): 67. CrossRef - Diffuse Pulmonary Meningotheliomatosis Diagnosed by Transbronchial Lung Biopsy
Roberto Bernabeu Mora, Juan Miguel Sánchez Nieto, Chunshao Hu, Eduardo Alcaraz Mateos, Alberto Giménez Bascuñana, Manuel Rodríguez Rodríguez
Respiration.2013; 86(2): 145. CrossRef
- Diffuse pulmonary meningotheliomatosis with pan-TRK expression by immunohistochemistry: a novel finding and potential pitfall
- HER2-Positive Breast Carcinomas with Co-amplification or Gain of Chromosome 17 Centromere Locus: Report of Three Cases and an Impact on HER2 Testing.
- Hyeong Chan Shin, Young Kyung Bae, Aeri Kim, Seok Ju Park
- Korean J Pathol. 2011;45(6):665-669.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.6.665
- 3,429 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - Recently we experienced three cases of human epidermal growth factor receptor 2 (HER2)-amplified invasive breast carcinomas associated with co-amplification or gain of chromosome 17 centromere (CEP17) in silver-enhanced in situ hybridization (SISH) analysis. These cases revealed 2+ or 3+ staining for HER2 immunohistochemistry and >6 HER2 copies per cell on SISH analyses. However, the calculated HER2/CEP17 ratios were low (<2.2) and did not fit within the HER2-positive category. We interpreted those cases as HER2-positive tumors based on the number of HER2 copies per cell. There is a potential for misinterpretation of SISH analysis in cases showing increased CEP17 copy number, based on the criterion used for HER2 positivity (HER2 copies >6 per cell vs HER2/CEP17 ratio>2.2). We recommend reporting raw SISH or fluorescence in situ hybridization data, including number of cells counted, average numbers of HER2 and CEP17 signals, and the calculated HER2/CEP17 ratio to prevent underreporting of HER2 amplification.
- The Significance of MicroRNA Let-7b, miR-30c, and miR-200c Expression in Breast Cancers.
- Sung Min Chun, Hee Jung Park, Chul Hwan Kim, Insun Kim
- Korean J Pathol. 2011;45(4):354-360.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.354
- 4,294 View
- 50 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
MicroRNA (miRNA) is a class of noncoding protein RNA as a promising biomarker for various diseases. In this study, the expression of let-7b, miR-30c, and miR-200c was studied in breast cancer tissues to evaluate the potential relationship with known clinicopathological parameters.
METHODS
Quantitative real-time polymerase chain reaction was performed to determine the expression level of three miRNAs in 37 pairs of noncancerous normal and cancer tissues and an additional 38 cancer tissues from patients with invasive ductal carcinoma.
RESULTS
miR-200c expression was higher in cancer tissues compared to noncancerous normal tissues, and its ratio was correlated with patient age at surgery, type of surgery, and Ki-67 expression. The expression level of let-7b in cancer tissues was inversely correlated with lymph node metastasis, histological grade, and Ki-67 expression but positively correlated with estrogen and progesterone receptor expression. miR-200c expression level was positively correlated with Her-2 expression. The miR-30c expression level in breast cancer was not correlated with any parameters.
CONCLUSIONS
miR-200c and let-7b could be used as biomarkers in patients with breast cancer, but its pathological mechanism should be determined. -
Citations
Citations to this article as recorded by- Evaluating MicroRNAs as diagnostic tools for lymph node metastasis in breast cancer: Findings from a systematic review and meta-analysis
Coral González Martínez, Stavros Therapontos, Jose A. Lorente, Miriam Alcaide Lucena, F.Gabriel Ortega, M.Jose Serrano
Critical Reviews in Oncology/Hematology.2025; 207: 104598. CrossRef - High DRC Levels Are Associated with Let-7b Overexpression in Women with Breast Cancer
Jarline Encarnación, Carmen Ortiz, Ralphdy Vergne, Wanda Vargas, Domenico Coppola, Jaime Matta
International Journal of Molecular Sciences.2016; 17(6): 865. CrossRef
- Evaluating MicroRNAs as diagnostic tools for lymph node metastasis in breast cancer: Findings from a systematic review and meta-analysis
- Prognostic Implications of the Expression of CXCL16 in Breast Carcinoma.
- Dong Youl Choi, Ran Hong, Sung Churl Lim, Keun Hong Kee, Chae Hong Suh, Mija Lee
- Korean J Pathol. 2011;45(1):15-20.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.15
- 4,921 View
- 32 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Of the many prognostic factors for breast cancer, the relationship between an infiltration of inflammatory cells and the prognosis is debatable. Of the chemokines affecting cancer's inflammatory reactions, chemokine (C-X-C motif) ligand 16 (CXCL16) has attracted attention for its prognostic value in many cancers, including colorectal cancer and renal cell carcinoma. But the situation for breast carcinoma is unknown. The aim of this study was to examine the relationship between the prognostic factors and the CXCL16 expression in patients with breast carcinoma.
METHODS
The patients (n=106) diagnosed with invasive ductal cancer of the breast were enrolled. We reviewed the clinicopathological factors of these patients, hematoxylin and eosin stains were prepared and estrogen receptor (ER), human epidermal growth factor receptor 2 (HER2/neu) and CXCL16 immunostaining was performed.
RESULTS
The ER expression was significantly correlated with age and inflammation. A CXCL16 expression was noted in 81.1% of the cases. No association was evident between a CXCL16 expression and any other parameter, including the survival rate. Multivariate analysis did not implicate ER, HER2/neu or CXCL16 as an independent prognostic factor, but the tumor size was independent predictive factor for the patient outcome.
CONCLUSIONS
An inflammatory reaction mediated by CXCL16 is not associated with the prognosis of breast cancer or any clinicopathological factors. -
Citations
Citations to this article as recorded by- The Emerging Role of CXC Chemokines And Their Receptors in Cancer
Victoria Vinader, Kamyar Afarinkia
Future Medicinal Chemistry.2012; 4(7): 853. CrossRef
- The Emerging Role of CXC Chemokines And Their Receptors in Cancer
- Automated Silver-enhanced In Situ Hybridization for Evaluation of HER2 Gene Status in Breast Carcinoma: Comparison with Fluorescence In Situ Hybridization and Immunohistochemistry.
- Woo Jung Sung, Seok Ju Park, Mi Jin Gu, Young Kyung Bae
- Korean J Pathol. 2010;44(1):28-34.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.28
- 4,795 View
- 64 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The human epidermal growth factor receptor 2 (HER2) is amplified in 20-25% of breast cancers. HER2 overexpression or amplification is associated with a worse clinical outcome and it can predict the benefit from anthracycline and anti-HER2 therapies. The HER2 status has usually been assessed by immunohistochemistry (IHC) or fluorescence in situ hybridization (FISH) in clinical samples. A new silver-enhanced in situ hybridization (SISH) technique was recently introduced. Therefore we evaluated the usefulness of SISH for detecting HER2 amplification.
METHODS
Tissue microarrays (TMAs) were constructed with 144 invasive breast cancer tissue samples. We performed IHC, FISH and SISH for HER2 on the tissue sections from the TMAs and we interpreted the results according to the American Society of Clinical Oncology/College of American Pathologists (ASCO/CAP) guidelines. The concordant rates between the two different tests were calculated.
RESULTS
HER2 was overexpressed and amplified in 16.9%, 16.9%, and 18% of the cases by IHC, FISH and SISH, respectively. The concordant rates between IHC and FISH, IHC and SISH, and FISH and SISH were 95.1%, 95.7%, and 97.8%, respectively.
CONCLUSIONS
SISH can be an alternative test for evaluating HER2 amplification because the 97.8% concordance with FISH satisfies the ASCO/CAP requirement of > 95% concordance with an alternative validated method. -
Citations
Citations to this article as recorded by- HER2 assessment by silverin situhybridization: where are we now?
Francesca Sanguedolce, Pantaleo Bufo
Expert Review of Molecular Diagnostics.2015; 15(3): 385. CrossRef - Diagnostic Effectiveness of PCR-based Tests DetectingBRAFMutation for Treating Malignant Melanoma: A Systematic Review
Hae-Won Shin, Ryeo-Jin Ko, Min Lee, Hee-Young Bang, Kye-Chul Kwon, Jong-Woo Park, Sun-Hoe Koo
Laboratory Medicine Online.2014; 4(4): 203. CrossRef - Effectiveness of Silver-enhanced In Situ Hybridization for Evaluating HER2 Gene Status in Invasive Breast Carcinoma: A Comparative Study
Youngseok Lee, Youngjoon Ryu, Hoiseon Jeong, Hyeyoon Chang, Younghye Kim, Aeree Kim
Archives of Medical Research.2012; 43(2): 139. CrossRef - HER2 Status by Standardized Immunohistochemistry and Silver-EnhancedIn SituHybridization in Korean Breast Cancer
Young Kyung Bae, Gyungyub Gong, Jun Kang, Ahwon Lee, Eun Yoon Cho, Ji Shin Lee, Kwang-Sun Suh, Dong Wha Lee, Woo Hee Jung
Journal of Breast Cancer.2012; 15(4): 381. CrossRef - Multiplication of Chromosome 17 Centromere Is Associated with Prognosis in Patients with Invasive Breast Cancers Exhibiting NormalHER2andTOP2AStatus
Aeri Kim, Hyung Chan Shin, Young Kyung Bae, Min Kyoung Kim, Su Hwan Kang, Soo Jung Lee, Eun Hee Lee
Journal of Breast Cancer.2012; 15(1): 24. CrossRef - HER2-Positive Breast Carcinomas with Co-amplification or Gain of Chromosome 17 Centromere Locus: Report of Three Cases and an Impact on HER2 Testing
Hyeong Chan Shin, Young Kyung Bae, Aeri Kim, Seok Ju Park
The Korean Journal of Pathology.2011; 45(6): 665. CrossRef - The Effectiveness of SilverIn SituHybridization in Patients with Breast Cancer: A Systematic Review
Sunyoung Jang, Seon-Heui Lee, Soojin Kim, You-Kyoung Lee, Young-Hyuck Im, Wonshik Han, Hee-Sook Park
Journal of Breast Cancer.2011; 14(Suppl 1): S1. CrossRef - Clinical and health economic outcomes of alternative HER2 test strategies for guiding adjuvant trastuzumab therapy
James A Lee, Megan Shaheen, Thomas Walke, Matt Daly
Expert Review of Pharmacoeconomics & Outcomes Research.2011; 11(3): 325. CrossRef - HER2 expression in breast cancer: Comparisons of fluorescence in situ hybridization and silver in situ hybridization, and immunohistochemical staining using monoclonal antibody and polyclonal antibody
Jung Sik Jang, Eun Jeong Jang, Ji‐Young Park
Basic and Applied Pathology.2010; 3(4): 115. CrossRef - HER2Status in Gastric Adenocarcinomas Assessed by Immunohistochemistry, Automated Silver-EnhancedIn SituHybridization and FluorescenceIn SituHybridization
Aeri Kim, Jung Min Bae, Se Won Kim, Mi Jin Gu, Young Kyung Bae
The Korean Journal of Pathology.2010; 44(5): 493. CrossRef
- HER2 assessment by silverin situhybridization: where are we now?
- The Loss of E-cadherin is Associated with the Epigenetic Alteration of CDH1 in Breast Cancer and it is also Associated with an Abnormal beta-catenin Expression in Lobular Carcinoma.
- Gwangil Kim, Ji Young Kim, Hee Jung An, Haeyoun Kang, Tae Heon Kim, Jung Yon Shim, Jin Hyung Heo, Hai Lin Park, Young Kil Choi
- Korean J Pathol. 2009;43(5):400-407.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.5.400
- 4,372 View
- 41 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
APC and E-cadherin are the key molecules in the Wnt/beta-catenin pathway. We attempted to define the epigenetic alteration of APC and CDH1 (the E-cadherin gene) and the expression of Wnt-related molecules in human mammary carcinomas.
METHODS
Sixty-four mammary carcinomas, including 52 invasive ductal carcinomas (IDCs) and 12 invasive lobular carcinomas (ILCs), were evaluated using methylation-specific PCR and immunohistochemistry. We performed immunohistochemistry for E-cadherin, beta-catenin, APC, Wnt1, cyclin D1, ER, PR and C-erb B2.
RESULTS
Hypermethylation of APC and CDH1 was observed in 38 (59%) and 28 (44%) cases, respectively. CDH1 hypermethylation in ILCs was increased compared to that in IDCs (p=0.002) and it was associated with the loss of E-cadherin (p=0.02) and beta-catenin (p=0.042). APC methylation was positively correlated with the ER expression (p=0.021). Abnormal cytoplasmic localization of beta-catenin was found in 10 cases and any expression was not detected in six cases. In ILCs, the E-cadherin or beta-catenin expression was markedly decreased compared to that in IDCs (p<0.001 in both).
CONCLUSIONS
Methylation of APC or CDH1 was relatively frequent in mammary carcinomas. The loss of E-cadherin in mammary carcinoma was associated with CDH1 methylation, and abnormal beta-catenin expression was related to the loss of E-cadherin in ILC. -
Citations
Citations to this article as recorded by- Wnt/β-catenin signaling pathway activation reverses gemcitabine resistance by attenuating Beclin1-mediated autophagy in the MG63 human osteosarcoma cell line
Hao Tao, Feng Chen, Haifei Liu, Yanling Hu, Yingzhen Wang, Haiyan Li
Molecular Medicine Reports.2017; 16(2): 1701. CrossRef
- Wnt/β-catenin signaling pathway activation reverses gemcitabine resistance by attenuating Beclin1-mediated autophagy in the MG63 human osteosarcoma cell line
- Intraductal Cystic Hypersecretory Carcinoma of the Breast: A case report.
- Jin Haeng Chung, Seung Sook Lee, Jae Soo Koh, Kyung Ja Cho, Jong Inn Lee
- Korean J Pathol. 1999;33(2):137-140.
- 2,066 View
- 10 Download
-
 Abstract
Abstract
- The cystic hypersecretory duct carcinoma of the breast was first described in 1984 by Rosen and Scott and warrants separate discussion because of its unusual pathological features. It is morphologically distinguishable from juvenile (secretory) carcinoma and from mucinous (colloid) carcinoma or mucocele-like tumor. We present a case report of intraductal cystic hypersecretory carcinoma of the breast with hormone receptor and oncogene study. The histologic differential diagnosis, with an emphasis on benign lesions that may have a predominant cystic component, is also discussed.
- E-cadherin Expression in Distinguishing Ductal and Lobular Carcinomas of the Breast.
- Eun Deok Chang, An Hi Lee, Eun Jung Lee, Seok Jin Kang, Chang Suk Kang
- Korean J Pathol. 2002;36(5):323-327.
- 2,465 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Most breast carcinomas are easily categorized as ductal or lobular. However, in some cases the distinction can be difficult since some tumors may have intermediate features of these two. Prior studies suggest that E-cadherin is useful to classify tumors as ductal or lobular, as it is lost in lobular but not in ductal carcinomas.
METHODS
We studied the histologic features and E-cadherin expression by immunohistochemistry in 57 cases of breast carcinomas, which were divided into three groups based on histology. Group 1 included 4 cases of infiltrating lobular carcinoma (IFL) and 1 case of lobular carcinoma in situ (LCIS) (n=5). Group 2 included infiltrating ductal carcinoma (IFD) with some features of IFL (n=48). Group 3 included a solid type of intraductal carcinoma (DCIS) (n=4). E-cadherin staining was scored as negative or positive.
RESULTS
All 5 cases from group 1 were E-cadherin negative, and all 4 DCIS cases were positive. Only 2 (0.04%) of the 48 cases from group 2 were E-cadherin negative.
CONCLUSIONS
Our findings suggest that the majority of cases with morphologically IFD with some IFL features are ductal. E-cadherin immunostaining is of value in helping to characterize breast carcinomas with indeterminate morphologic features.
- Expression of p21, p53 and bcl-2 Proteins in Invasive Ductal Carcinoma of the Breast.
- Hyang Jeong Jo, Ki Jung Yun, Hyung Bae Moon
- Korean J Pathol. 2003;37(6):393-399.
- 2,017 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was designed to investigate the prognostic significance of p21, p53, and bcl-2 proteins in invasive ductal carcinoma of the breast.
METHODS
Seventy-two cases of invasive ductal carcinoma were examined by immunohistochemical staining for p21, p53 and bcl-2 proteins. The results were correlated with clinicopathological variables, including age, tumor size, histologic grade, nuclear grade, lymph node status, estrogen receptor (ER) and progesterone receptor (PR) expression.
RESULTS
Of 72 cases, p21, p53 and bcl-2 proteins were positive in 25 (34.8%), 35 (50.0%) and 27 (37.5%), respectively. There were no statistically significant correlations between the p21 protein expression and the other clinicopathological variables. The expression of p53 protein, however, showed a significant relation to ER expression, and that of bcl-2 was positively correlated with tumor size. In survival analysis, p21, p53, and bcl-2 proteins, nuclear grade and lymph node status were associated with survival rate.
CONCLUSIONS
These results indicate that p21, p53, and bcl-2 proteins might play a role in tumorigenesis of breast carcinoma. In addition, the increased expression of p21, p53, and bcl-2 proteins could be used as factors suggesting poor prognosis in breast carcinomas.
- Expression of MMP-2, MT1-MMP, and TIMP-2 mRNA in Breast Carcinomas.
- Dong Won Kim, So Young Jin, Dong Wha Lee
- Korean J Pathol. 2003;37(6):400-406.
- 2,145 View
- 66 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The activation of proMMP-2 is induced by membrane type 1-matrix metalloproteinase (MT1-MMP), but inhibited by tissue inhibitors of matrix metalloproteinase type 2 (TIMP-2). This study was carried out to establish the pattern of mRNA expression of MMP-2, MT1-MMP, and TIMP-2 in breast carcinomas.
METHODS
Seventy-nine cases of invasive ductal carcinoma, 10 of ductal carcinoma in situ, and 10 of fibrocystic disease as a control were analysed for the expression of MMP-2, MT1-MMP, and TIMP-2 mRNA, using in situ hybridization. Correlations of the results with the clinical stage, tumor size, nodal status, and nuclear grade were analysed.
RESULTS
The expression rates of MMP-2, MT1-MMP, and TIMP-2 mRNA in invasive ductal carcinoma were 68%, 73%, and 56%, respectively. They were localized to both stromal and tumor cells, but mainly in the latter. The MMP-2 mRNA expression was significantly correlated with the clinical stage (p < 0.05), while the expression of TIMP-2 mRNA was inversely correlated with clinical stage and tumor size(p < 0.05). Significant positive correlations between MMP-2 and MT1-MMP expressions, along with inverse relationships between MMP-2 and TIMP-2, and between TIMP-2 and MT1-MMP, were also found. CONCLUSIONS: MMP-2 and TIMP-2 mRNA expressions might be useful as one of a range of prognostic parameters in breast carcinoma patients.

 E-submission
E-submission








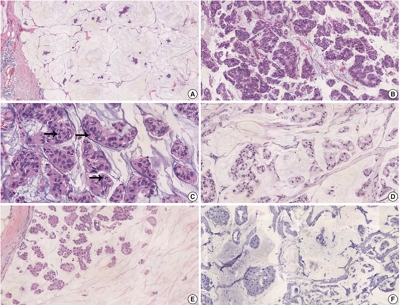

 First
First Prev
Prev



