Search
- Page Path
- HOME > Search
Review Article
- The evolving role of TRPS1 in dermatopathology: insights from the past 4 years
- Mokhtar H. Abdelhammed, Woo Cheal Cho
- Received September 11, 2025 Accepted November 25, 2025 Published online January 29, 2026
- DOI: https://doi.org/10.4132/jptm.2025.11.25 [Epub ahead of print]
- 376 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - Over the past 4 years, trichorhinophalangeal syndrome type 1 (TRPS1) has rapidly gained attention among practicing pathologists, with numerous studies emerging that both support and question its diagnostic utility. Initially regarded as a highly specific marker for tumors of mammary origin, TRPS1 is now recognized to have broader expression patterns, including in a variety of cutaneous neoplasms. This is likely due to embryologic parallels between breast tissue and skin adnexal structures, an overlap that was underappreciated in early investigations. Although TRPS1 lacks absolute specificity—even among cutaneous neoplasms—it can still offer meaningful diagnostic value when interpreted alongside conventional immunohistochemical markers and within the appropriate morphologic context. Noteworthy diagnostic applications include mammary Paget disease, primary extramammary Paget disease, rare adnexal neoplasms such as endocrine mucin-producing sweat gland carcinoma and primary cutaneous NUT adnexal carcinoma, and cutaneous metastases from breast carcinoma. In this review, we present the most comprehensive and up-to-date evaluation of the utility and limitations of TRPS1 immunohistochemistry in dermatopathology. Our aim is to deepen understanding of this emerging marker and provide practical guidance on its optimal integration with established immunohistochemical panels to enhance diagnostic accuracy in routine practice.
Original Article
- PSMA expression in hepatic colorectal cancer metastasis
- Eundong Park, Michel Kmeid, Xin Wang, Haiyan Qiu, Clifton G. Fulmer, Marcello P. Toscano, Nusret Bekir Subasi, Maciej Gracz, Hwajeong Lee
- J Pathol Transl Med. 2026;60(1):107-123. Published online January 14, 2026
- DOI: https://doi.org/10.4132/jptm.2025.10.20
- 412 View
- 37 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Prostate-specific membrane antigen (PSMA) is expressed in the neovasculature of various malignancies, such as colorectal cancer (CRC) and hepatocellular carcinoma (HCC). However, PSMA expression in hepatic CRC metastasis has not been studied in detail. Methods: The PSMA expression in primary CRC and corresponding hepatic metastasis was evaluated by immunohistochemistry in a metastatic CRC cohort (n = 56), which was divided into subgroups according to treatment history and timing of metastasis. Demographic and histological characteristics of primary CRC were collected and their relationships with PSMA expression were examined. Additionally, the PSMA expression in resected HCC (n = 76) was compared with that of hepatic CRC metastasis. Results: In primary CRC, PSMA level showed a positive association with tumor size. Lower PSMA expression in hepatic metastasis was associated with higher primary CRC grade, advanced pTNM stage at the time of CRC resection, presence of tumor deposit, and unresectability of metastatic lesion. PSMA expression in primary CRC correlated with that in hepatic metastasis only in concurrent and untreated metastasis subgroup. PSMA expression in primary CRC and hepatic metastasis, regardless of treatment history and timing of metastasis, was not significantly different from that of HCC. Conclusions: Several adverse pathological features of primary CRC were associated with a lower PSMA expression in hepatic metastasis. PSMA expression in hepatic metastasis correlated with that of primary CRC only in concurrent and untreated subgroup. Primary HCC and hepatic CRC metastasis show comparable levels of PSMA expression.
Review Article
- A comprehensive review of ossifying fibromyxoid tumor: insights into its clinical, pathological, and molecular landscape
- Kyriakos Chatzopoulos, Antonia Syrnioti, Mohamed Yakoub, Konstantinos Linos
- J Pathol Transl Med. 2026;60(1):6-19. Published online January 14, 2026
- DOI: https://doi.org/10.4132/jptm.2025.10.02
- 490 View
- 48 Download
-
 Abstract
Abstract
 PDF
PDF - Ossifying fibromyxoid tumor (OFMT) is a rare mesenchymal neoplasm first described in 1989. It typically arises in the superficial soft tissues of the extremities as a slow-growing, painless mass. Histologically, it is commonly characterized by a multilobular architecture composed of uniform epithelioid cells embedded in a fibromyxoid matrix, often surrounded by a rim of metaplastic bone. While classic cases are readily identifiable, the tumor's histopathological heterogeneity can mimic a range of benign and malignant neoplasms, posing significant diagnostic challenges. Molecularly, most OFMTs harbor PHF1 rearrangements, commonly involving fusion partners such as EP400, MEAF6, or TFE3. This review underscores the importance of an integrated diagnostic approach- incorporating histopathological, immunohistochemical, and molecular data- to accurately classify OFMT and distinguish it from its mimics. Expanding awareness of its morphologic and molecular spectrum is essential for precise diagnosis, optimal patient management, and a deeper understanding of this enigmatic neoplasm.
Original Article
- Correlations and prognostic impacts of tumor spread through airspaces in surgically resected non–small cell lung cancer: a retrospective study from Jordan
- Ola Abu Al Karsaneh, Amani Al-Rousan, Sofian Al Shboul, Mohammed El-Sadoni, Anas Hayajneh, Moath Alrjoub, Sura Al-Rawabdeh, Tareq Saleh
- J Pathol Transl Med. 2026;60(1):92-106. Published online January 9, 2026
- DOI: https://doi.org/10.4132/jptm.2025.10.15
- 672 View
- 50 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Spread through air spaces (STAS) has been identified as an invasion pattern in non–small cell lung cancer (NSCLC). This study evaluated the association between tumor STAS and various clinicopathological parameters of NSCLC, with emphasis on the prognostic role of STAS. Methods: We evaluated 96 cases of NSCLC for STAS. STAS-positive cases were graded according to the distance between the edge of the primary tumor and the furthest STAS, in millimeters, or the number of alveoli separating STAS from the tumor. Results: STAS was observed in 33 patients (34.4%). In 28 cases, STAS was located in airspaces >3 alveoli away from the primary tumor. In 18 cases, STAS was found in airspaces > 2.5 mm away from the edge of the primary tumor. Morphologically, 18 cases of STAS demonstrated a solid nest pattern, eight showed a micropapillary cluster pattern, and seven exhibited a single-cell pattern. In multivariate analysis, only high tumor grade (p = .001) was independently associated with STAS in NSCLC. The presence of STAS (p = .047), lymphovascular invasion (p = .001), positive surgical margin (p = .021), adenocarcinoma histology (p = .020), and postoperative therapy (p = .049) showed a statistically significant lower overall survival (OS). However, multivariate analyses showed that STAS is not an independent predictor of OS in NSCLC. In addition, STAS-positive cases with an extension of >2.5 mm had significantly lower disease-free survival (DFS) (p = .018). Conclusions: The findings demonstrated that STAS is independently associated with a higher tumor grade and appears to have an adverse impact on OS and DFS in the examined subpopulation.
Review Article
- Solitary fibrous tumor: an updated review
- Joon Hyuk Choi
- J Pathol Transl Med. 2026;60(1):20-46. Published online December 29, 2025
- DOI: https://doi.org/10.4132/jptm.2025.10.08
- 573 View
- 79 Download
-
 Abstract
Abstract
 PDF
PDF - Solitary fibrous tumor (SFT) is a fibroblastic neoplasm characterized by a branching, thin-walled dilated staghorn-shaped (hemangiopericytoma-like) vasculature and a NAB2::STAT6 gene fusion. SFTs can occur in almost any anatomical location, including superficial and deep soft tissues, visceral organs, and bone. They most commonly occur in extrapleural locations, equally affect both sexes, and are typically present in adults. Although metastasis is rare, SFTs frequently show local recurrence. The diagnosis of SFTs is difficult because of their broad histological and morphological overlap with other neoplasms. An accurate diagnosis is important for guiding disease management and prognosis. Despite advances in molecular diagnostics and therapeutic strategies, the biological complexity and unpredictable clinical behavior of SFTs present significant challenges. This review provides an updated overview of SFT, with a focus on its molecular genetics, histopathological features, and diagnostic considerations.
Original Articles
- Diagnostic value of cytology in detecting human papillomavirus–independent cervical malignancies: a nation-wide study in Korea
- Hye-Ra Jung, Junyoung Shin, Chong Woo Yoo, Eun Na Kim, Cheol Lee, Kyeongmin Kim, Ho-chang Lee, Yonghee Lee, Ji Hye Kim, Soo Jin Jung, Yumin Chung, Joo Yeon Kim, Hye Eun Park, Tae Hoen Kim, Wonae Lee, Min-Sun Cho, Ran Hong, Yoon Jung Choi, Younghee Choi, Young Sub Lee, Sang-Ryung Lee, Myunghee Kang, Young Jin Seo, Seung-Sook Lee, Yoon-Jung Hwang, Hyun-Jung Kim
- J Pathol Transl Med. 2025;59(6):444-452. Published online November 11, 2025
- DOI: https://doi.org/10.4132/jptm.2025.10.21
- 2,584 View
- 121 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) independent cervical malignancies (HPV-IDCMs) have recently been classified by the World Health Organization (WHO) 5th edition. These malignancies have historically received limited attention due to their rarity and the potential for evasion of HPV-based screening.
Methods
We retrospectively reviewed 5,854 biopsy-confirmed cervical malignancies from 22 institutions over 3 years (July 2020–June 2023). Histologic classification followed the WHO guidelines. HPV independence was confirmed by dual negativity for p16 and HPV; discordant cases (p16-positive/HPV-negative) underwent additional HPV testing using paraffin-embedded tissue. Cytological results were matched sequentially to histological confirmation.
Results
The prevalence of HPV-IDCM was 4.4% (257/5,854) overall and was 3.6% (208/5,805 cases) among primary cervical malignancy. Patient age of HPV-IDCM was 29 to 89 years (median, 57.79). Its histologic subtypes included primary adenocarcinoma (n = 116), endometrial adenocarcinoma (n = 35), squamous cell carcinoma (n = 72), metastatic carcinoma (n = 14), carcinoma, not otherwise specified (n = 10), neuroendocrine carcinoma (n = 3), and others (n = 7). Among 155 cytology-histological matched cases, the overall and primary Pap test detection rates were 85.2% (132/155) and 83.2% (104/125), respectively. The interval between cytology and histologic confirmation extended up to 38 months.
Conclusions
HPV-IDCMs comprised 3.6% of primary cervical malignancies with a high detection rate via cytology (83.2%). These findings affirm the value of cytological screening, particularly in patients with limited screening history or at risk for HPV-independent lesions, and may guide future screening protocols.
- Adenomatoid odontogenic tumor: clinicopathological analysis of 34 cases from Karachi, Pakistan
- Summaya Zafar, Sehar Sulaiman, Madeeha Nisar, Poonum Khan, Nasir Ud Din
- J Pathol Transl Med. 2025;59(6):390-397. Published online October 16, 2025
- DOI: https://doi.org/10.4132/jptm.2025.07.11
- 1,818 View
- 134 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Adenomatoid odontogenic tumor (AOT) is a benign slow-growing neoplasm of odontogenic epithelial origin that is relatively uncommon. Only a few studies have described its histological features. Hence, we aimed to describe the clinicopathological features of AOT in a cohort of patients. Methods: AOT cases diagnosed between 2009 and 2024 were searched electronically. Glass slides were retrieved from archives and were reviewed by two pathologists to record the associated morphological features. Other data including patient demographics and tumor site were collected by reviewing histopathology reports. Results: The age of patients ranged from 9 to 44 years (mean, 17.7 years), and most were female (55.9%). The maxilla (44.1%) was the most common tumor site. Histologically, a predominantly solid growth pattern (n = 34) accompanied by ducts with a cuboidal/columnar epithelial lining (n = 31), eosinophilic secretions (n = 31), calcifications (n = 31), lattice work pattern (n = 30), and cystic areas (n = 20) were observed. Less frequent features included calcifying epithelial odontogenic tumor (CEOT)–like areas (n = 13), osteodentin (n = 6), association with impacted tooth (n = 3), mucin in tubules (n = 7), fibrocollagenous stroma (n = 6), mucin in ducts (n = 3) and ossifying fibroma-like areas (n = 6). The association of ducts with a cuboidal/columnar epithelial lining, lattice work pattern, calcifications, and eosinophilic secretions with gingival tumors was statistically significant (p ≤ .05). Additionally, tooth tumors were significantly associated with CEOT-like areas (p = .03). Conclusions: Our study confirms the trends in the clinicopathological features of AOT in previous case reports. Our results suggest that AOTs usually exhibit a predominantly solid pattern with duct-like spaces. Only a few cases with CEOT-like and ossifying fibroma-like areas were observed, similar to infrequent cases reported in the past.
- Evaluation of potential prognostic significance of JUNB in human prostate cancer: a bioinformatic and histopathological study
- Noha R. Noufal, Einas M. Yousef, Mohamed Taha
- J Pathol Transl Med. 2025;59(5):291-305. Published online September 8, 2025
- DOI: https://doi.org/10.4132/jptm.2025.06.06
- 1,433 View
- 116 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Prostate cancer is one of the most common malignancies in males worldwide. Serum prostate-specific antigen is a frequently employed biomarker in the diagnosis and risk stratification of prostate cancer; however, it is known for its low predictive accuracy for disease progression. New prognostic biomarkers are needed to distinguish aggressive prostate cancer from low-risk disease. This study aimed to identify and validate potential prognostic biomarkers of prostate cancer. Methods: Two prostate cancer datasets from the Gene Expression Omnibus were analyzed to identify differentially expressed genes between benign prostatic hyperplasia (BPH) and prostatic carcinoma. Immunohistochemistry was used to evaluate the JUNB proto-oncogene, a subunit of the AP-1 transcription factor (JUNB), in 70 prostate cancer patients and 10 BPH samples. Results: Our findings showed that JUNB was significantly enriched in prostate cancer-related pathways and biological processes. JUNB expression was considerably higher in prostatic adenocarcinoma patients than in BPH patients. Regarding JUNB expression in prostate cancer cases, lower levels of JUNB expression were associated with higher grades of prostatic adenocarcinoma. Lower JUNB expression was associated with a higher risk of prostatic adenocarcinoma progression and shorter overall survival. Conclusions: These results suggest that JUNB is a promising prognostic biomarker and a potential tumor suppressor in prostate cancer.
Review Article
- Central nervous system tumors with BCOR internal tandem duplications: a systematic review of clinical, radiological, and pathological features in 69 cases
- Ji Young Lee, Sung Sun Kim, Hee Jo Baek, Tae-Young Jung, Kyung-Sub Moon, Jae-Hyuk Lee, Kyung-Hwa Lee
- J Pathol Transl Med. 2025;59(5):273-280. Published online September 1, 2025
- DOI: https://doi.org/10.4132/jptm.2025.07.23
- 3,272 View
- 175 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Central nervous system tumors with BCL6 corepressor (BCOR) internal tandem duplications (ITDs) constitute a rare, recently characterized pediatric neoplasm with distinct molecular and histopathological features. To date, 69 cases have been documented in the literature, including our institutional case. These neoplasms predominantly occur in young children, with the cerebellum representing the most frequent anatomical location. Radiologically, these tumors present as large, well-circumscribed masses frequently demonstrating necrosis, hemorrhage, and heterogeneous enhancement. Histologically, they are characterized by a monomorphic cellular population featuring ependymoma-like perivascular pseudorosettes, myxoid stroma, and elevated mitotic activity. Immunohistochemically, these tumors exhibit sparse glial fibrillary acidic protein expression while consistently demonstrating positive staining for vimentin and CD56. The defining molecular hallmark is a heterozygous ITD within exon 15 of the BCOR gene, with insertions ranging from 9 to 42 amino acids in length. BCOR immunohistochemistry reveals nuclear positivity in 97.9% of examined cases, although this finding is not pathognomonic for BCOR ITDs. This comprehensive review synthesizes data from all published cases of this novel tumor entity, providing a detailed analysis of clinical presentation, neuroimaging findings, histopathological features with differential diagnostic considerations, therapeutic approaches, and prognostic outcomes.
Original Article
- AMACR is a highly sensitive and specific immunohistochemical marker for diagnosing prostate cancer on biopsy: a systematic review and meta-analysis
- Johannes Cansius Prihadi, Stevan Kristian Lionardi, Nicolas Daniel Widjanarko, Steven Alvianto, Fransiskus Xaverius Rinaldi, Archie Fontana Iskandar
- J Pathol Transl Med. 2025;59(4):235-248. Published online July 3, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.16
- 6,273 View
- 206 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Alpha-methylacyl-CoA racemase (AMACR) is the preferred biomarker for distinguishing malignant from benign glands in prostate biopsies, showing high sensitivity and specificity for prostate cancer. A meta-analysis of immunohistochemistry (IHC) for AMACR is essential to further assess its diagnostic accuracy across diverse sample sources. Methods: A systematic search of databases including MEDLINE, ScienceDirect, ProQuest, Google Scholar, and the Cochrane Library was performed, focusing on studies of AMACR to diagnose prostate cancer, particularly in biopsy samples analyzed through IHC over the last 20 years. Quality of studies was assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 tool, followed by a meta-analysis of regions and subgroups to calculate summary estimates of diagnostic test accuracy. Results: In the final analysis, 37 studies, with a pooled size of 5,898 samples, were included from the examination of 94 full-text papers. Among them, 27 studies with similar sample sources and testing methodologies underwent meta-analysis, yielding a combined sensitivity estimate of 0.90 (95% confidence interval [CI], 0.86 to 0.93) and specificity of 0.91 (95% CI, 0.83 to 0.95), both with significant heterogeneity (p < .01). The region beneath the hierarchical summary receiver operating characteristic curve was 0.95 (95% CI, 0.93 to 0.97), positive likelihood ratio was 9.6 (95% CI, 5.3 to 17.4), negative likelihood ratio was 0.11 (95% CI, 0.08 to 0.15), and diagnostic odds ratio was 88 (95% CI, 42 to 181). Conclusions: Our meta-analysis findings substantiate AMACR as a highly accurate tool for diagnosing prostate cancer, specifically in biopsy samples, via immunohistochemical staining. Further studies involving diverse samples are needed to enhance our understanding of the AMACR diagnostic accuracy in a range of clinical settings. -
Citations
Citations to this article as recorded by- Pathogenesis-Guided Biomarker Assessment: A Shift in Prostate Cancer Diagnostics
Jessica M. Logan, Victoria Malone, John J. O’Leary, Doug A. Brooks
International Journal of Molecular Sciences.2025; 26(24): 11786. CrossRef
- Pathogenesis-Guided Biomarker Assessment: A Shift in Prostate Cancer Diagnostics
Case Study
- Acquired aberrant partial CD3 expression in recurrent Epstein-Barr virus–negative solitary plasmacytoma of tonsil
- Chenchen Niu, Dong Ren, Truc Tran, Ashley Gamayo, Sherif Rezk, Xiaohui Zhao
- J Pathol Transl Med. 2025;59(4):262-268. Published online May 15, 2025
- DOI: https://doi.org/10.4132/jptm.2025.04.17
- 2,653 View
- 128 Download
-
 Abstract
Abstract
 PDF
PDF - The aberrant expression of specific T-cell maker CD3 in B-cell neoplasms can be a potential diagnostic pitfall leading to a misclassification of cell lineage. Here, we report a case of recurrent solitary plasmacytoma with new aberrant expression of CD3. The neoplastic plasma cells of the recurrent tumor were kappa restricted, positive for CD138, MUM1, negative for CD20, cyclin D1, and Epstein-Barr virus. CD79a was positive in majority of the tumor cells, except for a small focus which was strongly positive for CD3, but negative for other T-cell markers (CD2, CD5, CD7, CD4, and CD8) and CD56. The neoplastic plasma cells of the original tumor were negative for CD3. To the best of our knowledge, only one case of recurrent plasmacytoma with aberrant expression of CD3 has been published, which revealed disease progression in the recurrence. However, we did not observe morphologic evidence of disease progression in our case.
Original Article
- Characteristics of RET gene mutations in Vietnamese medullary thyroid carcinoma patients: a single-center analysis
- Van Hung Pham, Quoc Thang Pham, Minh Nguyen, Hoa Nhat Ngo, Thao Thi Thu Luu, Nha Dao Thi Minh, Trâm Đặng, Anh Tu Thai, Hoang Anh Vu, Dat Quoc Ngo
- J Pathol Transl Med. 2025;59(2):125-132. Published online March 14, 2025
- DOI: https://doi.org/10.4132/jptm.2025.01.18
- 4,979 View
- 183 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The RET gene point mutation is the main molecular alteration involved in medullary thyroid carcinoma (MTC) tumorigenesis. Previous studies in Vietnam mainly consisted of case reports, with limited data on larger sample sizes. In this study, we investigated RET gene mutations in exons 10, 11, and 16 and analyzed clinicopathological features of a series of Vietnamese MTC patients. Methods: We collected 33 tissue samples from patients with MTC and analyzed RET mutations using the Sanger sequencing method. The relationship between hotspot RET mutations (exons 10, 11, 16) and clinicopathological features were investigated. Results: Among the 33 analyzed cases, 17 tumors (52%) harbored RET mutations in exon 10, 11, or 16. A total of 10 distinct genetic alterations were identified, including eight missense mutations and two short indels. Of these, seven were classified as pathogenic mutations based on previous publications, with p.M918T being the most frequent (4 cases), followed by p.C634R (3 cases) and p.C618R (3 cases). Mutations were significantly associated with specific histological patterns, such as the nested/insular pattern (p=.026), giant cells (p=.007), nuclear pleomorphism (p=.018), stippled chromatin (p=.044), and amyloid deposits (p=.024). No mutations were found in germline analyses, suggesting these were somatic alterations. Conclusions: Our results provided the first comprehensive analysis of RET mutations in Vietnamese MTC patients. The most frequent mutation was p.M918T, followed by p.C634R and p.C618R. Mutations in these three exons were linked to specific histopathological features. Information on mutational profiles of patients with MTC will further aid in the development of targeted therapeutics to ensure effective disease management.
Case Study
- Mucocele of the rectal stump: mucinous cystic neoplasm with low-grade dysplasia simulating low-grade appendiceal mucinous neoplasm
- Hasan Basri Aydin, Maria Faraz, A. David Chismark, Haiyan Qiu, Hwajeong Lee
- J Pathol Transl Med. 2025;59(2):139-146. Published online February 26, 2025
- DOI: https://doi.org/10.4132/jptm.2024.12.27
- 2,771 View
- 170 Download
-
 Abstract
Abstract
 PDF
PDF - Mucoceles, commonly observed in the appendix, are mucin-filled, dilated structures arising from a range of etiologies. Cases associated with dysplastic or neoplastic epithelium can rupture and disseminate within the abdominopelvic cavity. Similar lesions in other parts of the colon are exceedingly rare, with only 16 colonic mucoceles having been reported. The first case of a colonic mucinous neoplasm with dysplasia resembling a low-grade appendiceal mucinous neoplasm involving rectal stump was described in 2016. Here, we present the second such case arising in the rectal stump, identified in a 44-year-old male with extensive surgical history. Microscopic examination revealed low-grade dysplastic epithelium lining the cyst and mucin dissecting into the stroma, without evidence of rupture or extramural mucin. The patient was followed for 16 months without recurrence or peritoneal disease. The exact etiology and outcome of these rare lesions remain unknown, requiring close follow-up.
Original Article
- Association study of TYMS gene expression with TYMS and ENOSF1 genetic variants in neoadjuvant chemotherapy response of gastric cancer
- Khadijeh Arjmandi, Iman Salahshourifar, Shiva Irani, Fereshteh Ameli, Mohsen Esfandbod
- J Pathol Transl Med. 2025;59(2):105-114. Published online February 25, 2025
- DOI: https://doi.org/10.4132/jptm.2024.11.05
- 3,198 View
- 143 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The present research was designed to study the associations between genetic variants of TYMS and ENOSF1 genes with TYMS and ENOSF1 gene expression in neoadjuvant chemotherapy response among patients with gastric cancer. Methods: Formalin-embedded and paraffin-fixed matched tumor and normal gastric cancer tissue samples from patients who received neoadjuvant 5-fluorouracil (5-FU) treatment were obtained. DNA and RNA were extracted for all samples. A 28-bp variable number tandem repeat (VNTR) at the 5' untranslated region of TYMS gene and rs2612091 and rs2741171 variants in the ENOSF1 gene were genotyped for normal tissue samples. The real-time polymerase chain reaction method was used to study the expression of ENOSF1 and TYMS genes in both normal and tumor tissues. Data were analyzed using REST 2000 and SPSS ver. 26.0 software programs. Results: A significant association between TYMS 2R3R VNTR genotypes and 5-FU therapy was found (p = .032). The 3R3R and 2R2R genotypes were significantly associated with increased and decreased survival time, respectively (p = .003). The 3R3R genotype was significantly associated with TYMS overexpression (p < .001). Moreover, a significant association was found between the rs2612091 genotype and treatment outcome (p = .017). Conclusions: This study highlights the impact of TYMS and ENOSF1 genes as predictive indicators for survival and response to 5-FU–based neoadjuvant chemotherapy in gastric cancer patients. -
Citations
Citations to this article as recorded by- Innovative biomaterial strategies for mitigating radiotherapy toxicity: multidimensional mechanistic interventions of nano-microscale materials and hydrogels
Yifan Liu, Fengdi Jiang, Jie Song, Huaijin Qiao, Junlong Dai, Hao Bai, Shuyu Zhang
Coordination Chemistry Reviews.2026; 549: 217313. CrossRef
- Innovative biomaterial strategies for mitigating radiotherapy toxicity: multidimensional mechanistic interventions of nano-microscale materials and hydrogels
Review
- Cervical intraepithelial neoplasia and cervical cytology in pregnancy
- Ji-Young Kim, Jeong Yun Shim
- J Pathol Transl Med. 2024;58(6):283-290. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.17
- 10,236 View
- 440 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Cervical cancer screening during pregnancy presents unique challenges for cytologic interpretation. This review focuses on pregnancy-associated cytomorphological changes and their impact on diagnosis of cervical intraepithelial neoplasia (CIN) and cervical cancer. Pregnancy-induced alterations include navicular cells, hyperplastic endocervical cells, immature metaplastic cells, and occasional decidual cells or trophoblasts. These changes can mimic abnormalities such as koilocytosis, adenocarcinoma in situ, and high-grade squamous intraepithelial lesions, potentially leading to misdiagnosis. Careful attention to nuclear features and awareness of pregnancy-related changes are crucial for correct interpretation. The natural history of CIN during pregnancy shows higher regression rates, particularly for CIN 2, with minimal risk of progression. Management of abnormal cytology follows modified risk-based guidelines to avoid invasive procedures, with treatment typically deferred until postpartum. The findings reported in this review emphasize the importance of considering pregnancy status in cytological interpretation, highlight potential problems, and provide guidance on differentiating benign pregnancy-related changes from true abnormalities. Understanding these nuances is essential for accurate diagnosis and proper management of cervical abnormalities in pregnant women.
-
Citations
Citations to this article as recorded by- The significance of biological samples from pregnant women in cervical intraepithelial neoplasia
Xue Mi, Maharjan Rashmi, Zangyu Pan, Di Wu, Jinwei Miao
Frontiers in Medicine.2025;[Epub] CrossRef - Oncologic and pregnancy outcomes of cervical high-grade intraepithelial lesions and delivery mode
Olga P. Matylevich, Ilya A. Tarasau, Sviatlana Y. Shelkovich, Aliaksandr F. Martsinkevich
Academia Oncology.2025;[Epub] CrossRef
- The significance of biological samples from pregnant women in cervical intraepithelial neoplasia
Original Article
- Fine needle aspiration cytology diagnoses of follicular thyroid carcinoma: results from a multicenter study in Asia
- Hee Young Na, Miyoko Higuchi, Shinya Satoh, Kaori Kameyama, Chan Kwon Jung, Su-Jin Shin, Shipra Agarwal, Jen-Fan Hang, Yun Zhu, Zhiyan Liu, Andrey Bychkov, Kennichi Kakudo, So Yeon Park
- J Pathol Transl Med. 2024;58(6):331-340. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.12
- 5,757 View
- 266 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
This study was designed to compare diagnostic categories of thyroid fine needle aspiration cytology (FNAC) and incidence of thyroid tumors in the multi-institutional Asian series with a special focus on diagnostic category IV (suspicious for a follicular neoplasm) and follicular thyroid carcinomas (FTCs). Methods: Distribution of FNAC categories, incidence of thyroid tumors in resection specimens and cytologic diagnoses of surgically confirmed follicular adenomas (FAs) and FTCs were collected from 10 institutes from five Asian countries and were compared among countries and between FAs and FTCs. Results: The frequency of category IV diagnoses (3.0%) in preoperative FNAC were significantly lower compared to those in Western countries (10.1%). When comparing diagnostic categories among Asian countries, category IV was more frequent in Japan (4.6%) and India (7.9%) than in Taiwan (1.4%), Korea (1.4%), and China (3.6%). Similarly, incidence of FAs and FTCs in surgical resection specimens was significantly higher in Japan (10.9%) and India (10.1%) than in Taiwan (5.5%), Korea (3.0%), and China (2.5%). FTCs were more commonly diagnosed as category IV in Japan (77.5%) than in Korea (33.3%) and China (35.0%). Nuclear pleomorphism, nuclear crowding, microfollicular pattern, and dyshesive cell pattern were more common in FTCs compared with FAs. Conclusions: Our study highlighted the difference in FNAC diagnostic categories of FTCs among Asian countries, which is likely related to different reporting systems and thyroid cancer incidence. Cytologic features such as nuclear pleomorphism, nuclear crowding, microfollicular pattern, and dyshesive cell pattern were found to be useful in diagnosing FTCs more effectively. -
Citations
Citations to this article as recorded by- Misdiagnosed follicular adenoma with 11 year postoperative liver and lung metastases a case report and literature review
Kai-Li Yang, Heng-Tong Han, Shou-Hua Li, Xiao-Xiao Li, Ze Yang, Li-Bin Ma, Yong-Xun Zhao
Discover Oncology.2025;[Epub] CrossRef
- Misdiagnosed follicular adenoma with 11 year postoperative liver and lung metastases a case report and literature review
Review
- Cytologic hallmarks and differential diagnosis of papillary thyroid carcinoma subtypes
- Agnes Stephanie Harahap, Chan Kwon Jung
- J Pathol Transl Med. 2024;58(6):265-282. Published online November 7, 2024
- DOI: https://doi.org/10.4132/jptm.2024.10.11
- 13,907 View
- 597 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - Papillary thyroid carcinoma (PTC) is the most common thyroid malignancy, characterized by a range of subtypes that differ in their cytologic features, clinical behavior, and prognosis. Accurate cytologic evaluation of PTC using fine-needle aspiration is essential but can be challenging due to the morphologic diversity among subtypes. This review focuses on the distinct cytologic characteristics of various PTC subtypes, including the classic type, follicular variant, tall cell, columnar cell, hobnail, diffuse sclerosing, Warthin-like, solid/trabecular, and oncocytic PTCs. Each subtype demonstrates unique nuclear features, architectural patterns, and background elements essential for diagnosis and differentiation from other thyroid lesions. Recognizing these distinct cytologic patterns is essential for identifying aggressive subtypes like tall cell, hobnail, and columnar cell PTCs, which have a higher risk of recurrence, metastasis, and poorer clinical outcomes. Additionally, rare subtypes such as diffuse sclerosing and Warthin-like PTCs present unique cytologic profiles that must be carefully interpreted to avoid diagnostic errors. The review also highlights the cytologic indicators of lymph node metastasis and high-grade features, such as differentiated high-grade thyroid carcinoma. The integration of molecular testing can further refine subtype diagnosis by identifying specific genetic mutations. A thorough understanding of these subtype-specific cytologic features and molecular profiles is vital for accurate diagnosis, risk stratification, and personalized management of PTC patients. Future improvements in diagnostic techniques and standardization are needed to enhance cytologic evaluation and clinical decision-making in thyroid cancer.
-
Citations
Citations to this article as recorded by- Oncocytic Thyroid Tumours With Pathogenic FLCN Mutations Mimic Oncocytic Papillary Thyroid Carcinoma on Fine‐Needle Aspiration
Adeel M. Ashraf, Faisal Hassan, Adrian A. Dawkins, Julie C. Dueber, Derek B. Allison, Thèrése J. Bocklage
Cytopathology.2026; 37(1): 108. CrossRef - Using a new type of visible light-based emission fluorescence microscope to identify the benign and malignant nature of thyroid tissue during the surgical process: Analysis of diagnostic results
Yu Miao, Liu Xiaowei, Li Muyang, Gao Jian, Chen Lu
Photodiagnosis and Photodynamic Therapy.2026; 57: 105324. CrossRef - Nuclear pseudoinclusion is associated with BRAFV600E mutation: Analysis of nuclear features in papillary thyroid carcinoma
Agnes Stephanie Harahap, Dina Khoirunnisa, Salinah, Maria Francisca Ham
Annals of Diagnostic Pathology.2025; 75: 152434. CrossRef - 2025 Korean Thyroid Association Clinical Management Guideline on Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Eun Kyung Lee, Min Joo Kim, Seung Heon Kang, Bon Seok Koo, Kyungsik Kim, Mijin Kim, Bo Hyun Kim, Ji-hoon Kim, Shin Je Moon, Kyorim Back, Young Shin Song, Jong-hyuk Ahn, Hwa Young Ahn, Ho-Ryun Won, Won Sang Yoo, Min Kyoung Lee, Jeongmin Lee, Ji Ye Lee, Kyo
International Journal of Thyroidology.2025; 18(1): 30. CrossRef - Structure-based molecular screening and dynamic simulation of phytocompounds targeting VEGFR-2: a novel therapeutic approach for papillary thyroid carcinoma
Shuai Wang, Lingqian Zhang, Wenjun Zhang, Xiong Zeng, Jie Mei, Weidong Xiao, Lijie Yang
Frontiers in Pharmacology.2025;[Epub] CrossRef - 2025 Korean Thyroid Association Clinical Management Guideline on Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Eun Kyung Lee, Min Joo Kim, Seung Heon Kang, Bon Seok Koo, Kyungsik Kim, Mijin Kim, Bo Hyun Kim, Ji-hoon Kim, Shinje Moon, Kyorim Back, Young Shin Song, Jong-hyuk Ahn, Hwa Young Ahn, Ho-Ryun Won, Won Sang Yoo, Min Kyoung Lee, Jeongmin Lee, Ji Ye Lee, Kyon
Endocrinology and Metabolism.2025; 40(3): 307. CrossRef - A Case of Warthin-Like Variant of Papillary Thyroid Cancer
Amy Chow, Israa Laklouk
Cureus.2025;[Epub] CrossRef - Propensity score-matched analysis of the ‘2+2’ parathyroid strategy in total thyroidectomy with central neck dissection
Hao Gong, Simei Yao, Tianyuchen Jiang, Yi Yang, Yuhan Jiang, Zhujuan Wu, Anping Su
Frontiers in Endocrinology.2025;[Epub] CrossRef
- Oncocytic Thyroid Tumours With Pathogenic FLCN Mutations Mimic Oncocytic Papillary Thyroid Carcinoma on Fine‐Needle Aspiration
Original Articles
- The combination of CDX2 expression status and tumor-infiltrating lymphocyte density as a prognostic factor in adjuvant FOLFOX-treated patients with stage III colorectal cancers
- Ji-Ae Lee, Hye Eun Park, Hye-Yeong Jin, Lingyan Jin, Seung Yeon Yoo, Nam-Yun Cho, Jeong Mo Bae, Jung Ho Kim, Gyeong Hoon Kang
- J Pathol Transl Med. 2025;59(1):50-59. Published online October 24, 2024
- DOI: https://doi.org/10.4132/jptm.2024.09.26
- 3,629 View
- 281 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Colorectal carcinomas (CRCs) with caudal-type homeobox 2 (CDX2) loss are recognized to pursue an aggressive behavior but tend to be accompanied by a high density of tumor-infiltrating lymphocytes (TILs). However, little is known about whether there is an interplay between CDX2 loss and TIL density in the survival of patients with CRC.
Methods
Stage III CRC tissues were assessed for CDX2 loss using immunohistochemistry and analyzed for their densities of CD8 TILs in both intraepithelial (iTILs) and stromal areas using a machine learning-based analytic method.
Results
CDX2 loss was significantly associated with a higher density of CD8 TILs in both intraepithelial and stromal areas. Both CDX2 loss and a high CD8 iTIL density were found to be prognostic parameters and showed hazard ratios of 2.314 (1.050–5.100) and 0.378 (0.175–0.817), respectively, for cancer-specific survival. A subset of CRCs with retained CDX2 expression and a high density of CD8 iTILs showed the best clinical outcome (hazard ratio of 0.138 [0.023–0.826]), whereas a subset with CDX2 loss and a high density of CD8 iTILs exhibited the worst clinical outcome (15.781 [3.939–63.230]).
Conclusions
Altogether, a high density of CD8 iTILs did not make a difference in the survival of patients with CRC with CDX2 loss. The combination of CDX2 expression and intraepithelial CD8 TIL density was an independent prognostic marker in adjuvant chemotherapy-treated patients with stage III CRC.
- International Academy of Cytology standardized reporting of breast fine-needle aspiration cytology with cyto-histopathological correlation of breast carcinoma
- Shweta Pai
- J Pathol Transl Med. 2024;58(5):241-248. Published online September 13, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.14
- 7,776 View
- 412 Download
-
 Abstract
Abstract
 PDF
PDF - Background
The International Academy of Cytology (IAC) has developed a standardized approach for reporting the findings of breast fine-needle aspiration cytology (FNAC). Accordingly, there are five chief categories of breast lesions, C1 (insufficient material), C2 (benign), C3 (atypical), C4 (suspicious), and C5 (malignant). The prognostication and management of breast carcinoma can be performed readily on the basis of this classification system. The aim of this study was to classify various breast lesions into one of the above-named categories and to further grade the C5 lesions specifically using the Robinson system. The latter grades were then correlated with modified Scarff-Bloom-Richardson (SBR) grades.
Methods
This retrospective study was undertaken in the pathology department of a hospital located in the urban part of the city of Bangalore. All FNAC procedures performed on breast lumps spanning the year 2020 were included in the study.
Results
A total of 205 breast lesions was classified according to the IAC guidelines into C1 (6 cases, 2.9%), C2 (151 cases, 73.7%), C3 (13 cases, 6.3%), C4 (5 cases, 2.5%), and C5 (30 cases, 14.6%) groups. The C5 cases were further graded using Robinson’s system. The latter showed a significant correlation with the SBR system (concordance=83.3%, Spearman correlation=0.746, Kendall’s tau-b=0.736, kappa=0.661, standard error=0.095, p≤.001).
Conclusions
A standardized approach for FNAC reporting of breast lesions, as advocated for by the IAC, improves the quality and clarity of the reports and assures diagnostic reproducibility on a global scale. Further, the cytological grading of C5 lesions provides reliable cyto-prognostic scores that can help assess a tumor’s aggressiveness and predict its histological grade.
- Diagnostic challenges in the assessment of thyroid neoplasms using nuclear features and vascular and capsular invasion: a multi-center interobserver agreement study
- Agnes Stephanie Harahap, Mutiah Mutmainnah, Maria Francisca Ham, Dina Khoirunnisa, Abdillah Hasbi Assadyk, Husni Cangara, Aswiyanti Asri, Diah Prabawati Retnani, Fairuz Quzwain, Hasrayati Agustina, Hermawan Istiadi, Indri Windarti, Krisna Murti, Muhammad Takbir, Ni Made Mahastuti, Nila Kurniasari, Nungki Anggorowati, Pamela Abineno, Yulita Pundewi Setyorini, Kennichi Kakudo
- J Pathol Transl Med. 2024;58(6):299-309. Published online September 12, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.25
- Correction in: J Pathol Transl Med 2025;59(3):201
- 5,028 View
- 406 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The diagnosis of thyroid neoplasms necessitates the identification of distinct histological features. Various education/hospital centers located in cities across Indonesia likely result in discordances among pathologists when diagnosing thyroid neoplasms.
Methods
This study examined the concordance among Indonesian pathologists in assessing nuclear features and capsular and vascular invasion of thyroid tumors. Fifteen pathologists from different centers independently assessed the same 14 digital slides of thyroid tumor specimens. All the specimens were thyroid neoplasms with known BRAFV600E and RAS mutational status, from a single center. We evaluated the pre- and post-training agreement using the Fleiss kappa. The significance of the training was evaluated using a paired T-test.
Results
Baseline agreement on nuclear features was slight to fair based on a 3-point scoring system (k = 0.14 to 0.28) and poor to fair based on an eight-point system (k = –0.02 to 0.24). Agreements on vascular (κ = 0.35) and capsular invasion (κ = 0.27) were fair, whereas the estimated molecular type showed substantial agreement (κ = 0.74). Following the training, agreement using the eight-point system significantly improved (p = 0.001).
Conclusions
The level of concordance among Indonesian pathologists in diagnosing thyroid neoplasm was relatively poor. Consensus in pathology assessment requires ongoing collaboration and education to refine diagnostic criteria. -
Citations
Citations to this article as recorded by- Nuclear pseudoinclusion is associated with BRAFV600E mutation: Analysis of nuclear features in papillary thyroid carcinoma
Agnes Stephanie Harahap, Dina Khoirunnisa, Salinah, Maria Francisca Ham
Annals of Diagnostic Pathology.2025; 75: 152434. CrossRef
- Nuclear pseudoinclusion is associated with BRAFV600E mutation: Analysis of nuclear features in papillary thyroid carcinoma
Case Study
- Colorectal cancer with a germline BRCA1 variant inherited paternally: a case report
- Kyoung Min Kim, Min Ro Lee, Ae Ri Ahn, Myoung Ja Chung
- J Pathol Transl Med. 2024;58(6):341-345. Published online September 5, 2024
- DOI: https://doi.org/10.4132/jptm.2024.08.14
- 6,769 View
- 306 Download
-
 Abstract
Abstract
 PDF
PDF - BRCA genes have well-known associations with breast and ovarian cancers. However, variations in the BRCA gene, especially germline variations, have also been reported in colorectal cancer (CRC). We present the case of a rectal cancer with a germline BRCA1 variation inherited from the paternal side. A 39-year-old male was admitted with rectal cancer. The patient underwent surgical resection and the pathologic diagnosis was adenocarcinoma. Next-generation sequencing was performed and a BRCA1 variant was detected. Reviewing the public database and considering the young age of the patient, the variant was suggested to be germline. The patient’s father had had prostate cancer and next-generation sequencing testing revealed an identical BRCA1 variant. In the BRCA cancer group, there is relatively little attention paid to male cancers. The accumulation of male CRC cases linked to BRCA variations may help clarify the potential pathological relationship between the two.
Original Articles
- Artificial intelligence algorithm for neoplastic cell percentage estimation and its application to copy number variation in urinary tract cancer
- Jinahn Jeong, Deokhoon Kim, Yeon-Mi Ryu, Ja-Min Park, Sun Young Yoon, Bokyung Ahn, Gi Hwan Kim, Se Un Jeong, Hyun-Jung Sung, Yong Il Lee, Sang-Yeob Kim, Yong Mee Cho
- J Pathol Transl Med. 2024;58(5):229-240. Published online August 9, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.13
- 4,399 View
- 276 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Bladder cancer is characterized by frequent mutations, which provide potential therapeutic targets for most patients. The effectiveness of emerging personalized therapies depends on an accurate molecular diagnosis, for which the accurate estimation of the neoplastic cell percentage (NCP) is a crucial initial step. However, the established method for determining the NCP, manual counting by a pathologist, is time-consuming and not easily executable.
Methods
To address this, artificial intelligence (AI) models were developed to estimate the NCP using nine convolutional neural networks and the scanned images of 39 cases of urinary tract cancer. The performance of the AI models was compared to that of six pathologists for 119 cases in the validation cohort. The ground truth value was obtained through multiplexed immunofluorescence. The AI model was then applied to 41 cases in the application cohort that underwent next-generation sequencing testing, and its impact on the copy number variation (CNV) was analyzed.
Results
Each AI model demonstrated high reliability, with intraclass correlation coefficients (ICCs) ranging from 0.82 to 0.88. These values were comparable or better to those of pathologists, whose ICCs ranged from 0.78 to 0.91 in urothelial carcinoma cases, both with and without divergent differentiation/ subtypes. After applying AI-driven NCP, 190 CNV (24.2%) were reclassified with 66 (8.4%) and 78 (9.9%) moved to amplification and loss, respectively, from neutral/minor CNV. The neutral/minor CNV proportion decreased by 6%.
Conclusions
These results suggest that AI models could assist human pathologists in repetitive and cumbersome NCP calculations.
- Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
- Agnes Stephanie Harahap, Chan Kwon Jung
- J Pathol Transl Med. 2024;58(5):205-213. Published online July 24, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.24
- 4,795 View
- 297 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
While fine needle aspiration cytology (FNAC) plays an essential role in the screening of thyroid nodules, core needle biopsy (CNB) acts as an alternative method to address FNAC limitations. However, diagnosing thyroid CNB samples can be challenging due to variations in background and levels of experience. Effective training is indispensable to mitigate this challenge. We aim to evaluate the impact of an educational program on improving the accuracy of CNB diagnostics.
Methods
The 2-week observational program included a host mentor pathologist with extensive experience and a visiting pathologist. The CNB classification by The Practice Guidelines Committee of the Korean Thyroid Association was used for the report. Two rounds of reviewing the case were carried out, and the level of agreement between the reviewers was analyzed.
Results
The first-round assessment showed a concordance between two pathologists for 247 thyroid CNB specimens by 84.2%, with a kappa coefficient of 0.74 (indicating substantial agreement). This finding was attributed to the discordance in the use of categories III and V. After peer learning, the two pathologists evaluated 30 new cases, which showed an overall improvement in the level of agreement. The percentage of agreement between pathologists on thyroid CNB diagnosis was 86.7%, as measured by kappa coefficient of 0.80.
Conclusions
This educational program, consisting of guided mentorship and peer learning, can substantially enhance the diagnostic accuracy of thyroid CNB. It is useful in promoting consistent diagnostic standards and contributes to the ongoing development of global pathology practices. -
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Liquid-based cytology features of pancreatic acinar cell carcinoma: comparison with other non-ductal neoplasms of the pancreas
- Minji Kwon, Seung-Mo Hong, Kyoungbun Lee, Haeryoung Kim
- J Pathol Transl Med. 2024;58(4):182-190. Published online July 9, 2024
- DOI: https://doi.org/10.4132/jptm.2024.06.25
- 3,244 View
- 248 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Acinar cell carcinoma (ACC) is a rare malignant epithelial neoplasm, which shares many cytomorphological features with other non-ductal pancreatic neoplasms such as pancreatic neuroendocrine neoplasm (PanNEN) and solid-pseudopapillary neoplasm (SPN). Due to the relative rarity of these tumors, pathologists are less familiar with the cytological features, especially on liquid-based cytology (LBC) which has been relatively recently introduced for endoscopic ultrasound-guided fine needle aspiration specimens.
Methods
We evaluated the detailed cytological features of 15 histologically confirmed ACC (7 conventional smears [CS], 8 LBC), and compared them with the LBC features of SPN (n = 9) and PanNEN (n = 9).
Results
Compared with CS, LBCs of ACC demonstrated significantly less bloody background. All ACCs demonstrated prominent nucleoli and macronucleoli on LBC. On comparison with the LBC features of SPN and PanNEN, most ACCs demonstrated a necrotic background with apoptotic debris while PanNEN and SPN did not show these features. Acinar structures were predominantly observed in ACC, while frequent pseudopapillary structures were seen only in SPN. Prominent nucleoli and macronucleoli were only seen in ACC.
Conclusions
ACC had characteristic cytological features that could be observed on LBC preparations, such as high cellularity, necrotic/apoptotic background, nuclear tangles, acinar arrangement of cells, and macronucleoli. These findings also help distinguish ACC from PanNEN and SPN on LBC. It is important to be familiar with these features, as an accurate diagnosis on endoscopic ultrasound–guided fine needle aspiration cytology would have impact on the management of the patient.
Case Study
- Intravascular schwannoma as an extremely unusual cause of vein obstruction: a case report
- Luis Miguel Chinchilla-Tábora, Beatriz Segovia Blázquez, José María Sayagués, Marta Rodríguez González, Joaquín González-Rivero, José Antonio Muñoz León, Andrea Beatriz Jiménez Pérez, Idalia González Morais, Diego Bueno-Sacristán, María Dolores Ludeña
- J Pathol Transl Med. 2024;58(5):249-254. Published online July 3, 2024
- DOI: https://doi.org/10.4132/jptm.2024.05.15
- 4,161 View
- 284 Download
-
 Abstract
Abstract
 PDF
PDF - The blood vessel lumen is an extremely rare location for a benign peripheral nerve sheath tumor like schwannoma. Less than 10 cases have been previously reported. In this report, we present a case of a 68-year-old woman who had a soft tissue nodule at the posterior calf of her left leg during a physical examination. Pathological examination was performed after complete surgical excision. The patient underwent follow-up for 12 months after surgery without evidence of recurrence or any other complication. This is the first case of intravascular schwannoma reported as a cause of vein obstruction. Microscopically, the tumor was composed of Schwann spindle cells that were immunoreactive for S100 protein and SOX10. This tumor was surrounded by a well-defined vascular smooth muscle wall. Prospective series are required to improve the knowledge on the underlying mechanisms of intravascular schwannoma development.
Original Article
- The importance of histomorphological features and ERG expression in the diagnosis of malignancy in cases with atypical small acinar proliferation
- Gizem Teoman, Ayten Livaoglu, Hatice Kucuk, Afs ¸ın Rahman Murtezaoglu
- J Pathol Transl Med. 2024;58(3):134-140. Published online May 14, 2024
- DOI: https://doi.org/10.4132/jptm.2024.03.18
- 4,151 View
- 233 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Atypical small acinar proliferation (ASAP) cases typically require rebiopsy, which are invasive and associated with increased risk of complications. Our aim in this study was to determine the importance of laboratory and histological findings and E-26 transformation-specific-related gene (ERG) expression in the diagnosis of malignancy.
Methods
Between March 2016 and March 2022, 84 patients who were diagnosed with ASAP on biopsy or rebiopsy were included in the study. Clinical-laboratory features of age, serum prostate-specific antigen level, and histopathological features were compared and included multifocality, number of suspicious acini, nuclear enlargement, nucleolar prominence, hyperchromasia, cytoplasmic amphophilia, luminal amorphous acellular secretion, crystalloid presence, infiltrative appearance, inflammation, atrophy, α-methyl acyl-CoA racemase, p63, and/or high molecular weight cytokeratin were analyzed. In addition, ERG expression was evaluated immunohistochemically.
Results
Statistically significant correlation was found between nucleolar prominence, nuclear hyperchromasia, crystalloid presence, infiltrative pattern, and prostate cancer (p < .001). In 19 of 84 cases (22.6%) ERG was positive in the nucleus. Prostate cancer was diagnosed at rebiopsy in 15 of the 19 ERG-positive cases (78.9%). A statistically significant correlation was found between ERG positivity and prostate cancer (p= .002).
Conclusions
Our findings suggest that evaluation of these markers during initial transrectal ultrasound biopsies may decrease and prevent unnecessary prostate rebiopsy.
Review
- Interpretation of PD-L1 expression in gastric cancer: summary of a consensus meeting of Korean gastrointestinal pathologists
- Soomin Ahn, Yoonjin Kwak, Gui Young Kwon, Kyoung-Mee Kim, Moonsik Kim, Hyunki Kim, Young Soo Park, Hyeon Jeong Oh, Kyoungyul Lee, Sung Hak Lee, Hye Seung Lee
- J Pathol Transl Med. 2024;58(3):103-116. Published online April 25, 2024
- DOI: https://doi.org/10.4132/jptm.2024.03.15
- 20,549 View
- 691 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Nivolumab plus chemotherapy in the first-line setting has demonstrated clinical efficacy in patients with human epidermal growth factor receptor 2–negative advanced or metastatic gastric cancer, and is currently indicated as a standard treatment. Programmed death-ligand 1 (PD-L1) expression is an important biomarker for predicting response to anti–programmed death 1/PD-L1 agents in several solid tumors, including gastric cancer. In the CheckMate-649 trial, significant clinical improvements were observed in patients with PD-L1 combined positive score (CPS) ≥ 5, determined using the 28-8 pharmDx assay. Accordingly, an accurate interpretation of PD-L1 CPS, especially at a cutoff of 5, is important. The CPS method evaluates both immune and tumor cells and provides a comprehensive assessment of PD-L1 expression in the tumor microenvironment of gastric cancer. However, CPS evaluation has several limitations, one of which is poor interobserver concordance among pathologists. Despite these limitations, clinical indications relying on PD-L1 CPS are increasing. In response, Korean gastrointestinal pathologists held a consensus meeting for the interpretation of PD-L1 CPS in gastric cancer. Eleven pathologists reviewed 20 PD-L1 slides with a CPS cutoff close to 5, stained with the 28-8 pharmDx assay, and determined the consensus scores. The issues observed in discrepant cases were discussed. In this review, we present cases of gastric cancer with consensus PD-L1 CPS. In addition, we briefly touch upon current practices and clinical issues associated with assays used for the assessment of PD-L1 expression in gastric cancer.
-
Citations
Citations to this article as recorded by- Organ Preservation for Gastroesophageal Junction and Gastric Cancers: Ready for Primetime?
Winta Mehtsun, Lola Van Doosselaere, Ugwuji N. Maduekwe
American Society of Clinical Oncology Educational Book.2026;[Epub] CrossRef - Deep Learning Analysis Based on Dual-energy CT-Derived Iodine Map for Predicting PD-L1 Expression in Gastric Cancer: A Multicenter Study
Lihong Chen, Yuncong Zhao, Xiaomin Tian, Deye Zeng, Yongxiu Tong, Haiping Xu, Yaru You, Caiming Weng, Sen Lin, Keru Chen, Yilin Chen, Yunjing Xue
Academic Radiology.2026;[Epub] CrossRef - Adjuvant immunotherapy in patients with resected gastric and oesophagogastric junction cancer following preoperative chemotherapy with high risk for recurrence (ypN+ and/or R1): European Organisation of Research and Treatment of Cancer (EORTC) 1707 VESTIG
F. Lordick, M.E. Mauer, G. Stocker, C.A. Cella, I. Ben-Aharon, G. Piessen, L. Wyrwicz, G. Al-Haidari, T. Fleitas-Kanonnikoff, V. Boige, R. Lordick Obermannová, U.M. Martens, C. Gomez-Martin, P. Thuss-Patience, V. Arrazubi, A. Avallone, K.K. Shiu, P. Artru
Annals of Oncology.2025; 36(2): 197. CrossRef - PD-L1 as a Biomarker in Gastric Cancer Immunotherapy
Yunjoo Cho, Soomin Ahn, Kyoung-Mee Kim
Journal of Gastric Cancer.2025; 25(1): 177. CrossRef - PD-L1 importance in malignancies comprehensive insights into the role of PD-L1 in malignancies: from molecular mechanisms to therapeutic opportunities
Mojdeh Soltani, Mohammad Abbaszadeh, Hamed Fouladseresht, Mark J. M. Sullman, Nahid Eskandari
Clinical and Experimental Medicine.2025;[Epub] CrossRef - CLDN18.2 expression in gastroesophageal adenocarcinoma: prevalence, heterogeneity, and prognostic implications in Spanish patients
Carolina Martinez-Ciarpaglini, María Ortega, Sandra Pérez-Buira, Aitana Bolea, Beatriz Casado Guerra, Carmen Herencia Bellido, Paula Tornero Piñero, Dolores Naranjo-Hans, Brenda Palomar, Hernán Quiceno, Amanda Sardón Fernández, Ariadna Torner Calvo, Feder
Virchows Archiv.2025; 487(6): 1337. CrossRef - Distinct clinicopathological and survival profiles of CLDN18.2 and PD-L1 expression in advanced gastric cancer and gastroesophageal junction adenocarcinoma
D.R. Castillo, M. Guo, P. Shah, M. Hazeltin, D. Tai, F. Al-Manaseer, S. Mlamba, D. Perez, S. Yeremian, S. Guzman, R. Mannan, C. Crook, C. Lau, N. Tawar, G. Brar, M. Raoof, Y. Woo, S.P. Wu, D. Li
ESMO Gastrointestinal Oncology.2025; 10: 100261. CrossRef - Best Practice PD-L1 Staining and Interpretation in Gastric Cancer Using PD-L1 IHC PharmDx 22C3 and PD-L1 IHC PharmDx 28-8 Assays, with Reference to Common Issues and Solutions
Soomin Ahn, Inwoo Hwang, Yuyeon Kim, Somin Lee, Yunjoo Cho, So Young Kang, Deok Geun Kim, Jeeyun Lee, Kyoung-Mee Kim
Biomedicines.2025; 13(11): 2824. CrossRef - Intraperitoneal immune microenvironment and efficacy of intraperitoneal chemotherapy in patients with gastric cancer and peritoneal metastasis
Tomoya Nakanishi, Motohiro Imano, Masashi Kohda, Hiroaki Kato, Naoko Kounami, Atsushi Yamada, Masuhiro Terada, Yoko Hiraki, Osamu Shiraishi, Atsushi Yasuda, Masayuki Shinkai, Takushi Yasuda
Scientific Reports.2025;[Epub] CrossRef - PD-L1 thresholds predict efficacy of immune checkpoint inhibition in first-line treatment of advanced gastroesophageal adenocarcinoma. A systematic review and meta-analysis of seven phase III randomized trials
V. Formica, C. Morelli, L. Fornaro, S. Riondino, M. Rofei, E. Fontana, E.C. Smyth, M. Roselli, H.-T. Arkenau
ESMO Open.2024; 9(11): 103967. CrossRef
- Organ Preservation for Gastroesophageal Junction and Gastric Cancers: Ready for Primetime?
Original Articles
- TRPS1 expression in non-melanocytic cutaneous neoplasms: an immunohistochemical analysis of 200 cases
- Yi A. Liu, Phyu P. Aung, Yunyi Wang, Jing Ning, Priyadharsini Nagarajan, Jonathan L. Curry, Carlos A. Torres-Cabala, Doina Ivan, Victor G. Prieto, Qingqing Ding, Woo Cheal Cho
- J Pathol Transl Med. 2024;58(2):72-80. Published online February 26, 2024
- DOI: https://doi.org/10.4132/jptm.2024.01.23
- 6,997 View
- 390 Download
- 13 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Although trichorhinophalangeal syndrome type 1 (TRPS1) was initially thought to be highly sensitive and specific for carcinomas and mesenchymal tumors of mammary origin, more recent data suggest its expression is not limited to breast neoplasms but also can be seen in other cutaneous neoplasms, such as extramammary Paget disease and squamous cell carcinoma (SCC) in situ.
Methods
Two-hundred cases of non-melanocytic cutaneous neoplasm, including basal cell carcinomas (BCCs) (n = 41), SCCs (n = 35), Merkel cell carcinomas (MCCs) (n = 25), and adnexal neoplasms (n = 99), were tested for TRPS1 expression using a monoclonal anti- TRPS1 rabbit anti-human antibody.
Results
TRPS1 expression was present in almost all cases of SCC (94%), with a median H-score of 200, while it was either absent or only focally present in most BCCs (90%), with a median H-score of 5. The difference between BCCs and SCCs in H-score was significant (p < .001). All MCCs (100%) lacked TRPS1 expression. TRPS1 expression was frequently seen in most adnexal neoplasms, benign and malignant, in variable intensity and proportion but was consistently absent in apocrine carcinomas. All endocrine mucin-producing sweat gland carcinomas (EMPSGCs) (100%, 6/6) showed diffuse and strong TRPS1 immunoreactivity, with a median H-score of 300, which was significantly different (p < .001) than that of BCCs.
Conclusions
Our study shows that TRPS1 may be an effective discriminatory marker for BCCs and SCCs. It also has a role in distinguishing BCCs from EMPSGCs. -
Citations
Citations to this article as recorded by- Metastatic Vulvar Paget's Disease Presenting in a Supraclavicular Lymph Node: A Diagnostic Challenge on Fine Needle Aspiration Cytology
Thiri Htoo Aung, Neha Seth, Anam Khan, Kasturi Das
Diagnostic Cytopathology.2026;[Epub] CrossRef - Trichorhinophalangeal syndrome type 1 (TRPS1) in breast pathology: diagnostic utility and pitfalls
Atif Ali Hashmi, Edi Brogi, Hannah Y. Wen
Diagnostic Pathology.2025;[Epub] CrossRef - Refining NTRK Fusion Detection in Papillary Thyroid Carcinoma Through Pan-TRK Immunohistochemistry and Histopathologic Features
Hyun Lee, Sue Youn Kim, Ji Min Park, Seung-Hyun Jung, Ozgur Mete, Chan Kwon Jung
Endocrine Pathology.2025;[Epub] CrossRef - Endocrine mucin-producing sweat gland carcinoma: Case report and literature review
Nan Guo, Zhenlin Fan, Yitong Chen, Qian Li, Limin Guo
European Journal of Ophthalmology.2025;[Epub] CrossRef - Updates on utility of immunohistochemistry in diagnosis of metastatic breast cancer
Hongxia Sun, Aysegul A. Sahin, Qingqing Ding
Human Pathology.2025; 162: 105821. CrossRef - Primary Cutaneous NUT Adnexal Carcinoma With BRD4::NUTM1 Fusion: A 19-Year Follow-Up
Elsayed Ibrahim, Richard K. Yang, Maria A. Gubbiotti, Victor G. Prieto, Woo Cheal Cho
The American Journal of Dermatopathology.2025; 47(9): 731. CrossRef - Primary mucinous carcinoma of the skin with co-expression of TRPS1 and GATA3: a case report
Liling Song, Ning Zhu, Lei Jiang, Dong Gao, Guohua Yu
Frontiers in Oncology.2025;[Epub] CrossRef - Diagnostic Algorithm for Secondary Extramammary Paget Disease from Institutional Cases and Literature Review
Salin Kiratikanon, Ayaka Fukui, Masahiro Hirata, Jakob M. T. Moran, Masakazu Fujimoto, Mai P. Hoang
Cancers.2025; 17(24): 4014. CrossRef - TRPS1 Expression Is Frequently Seen in a Subset of Cutaneous Mesenchymal Neoplasms and Tumors of Uncertain Differentiation: A Potential Diagnostic Pitfall
Moon Joo Kim, Yi A. Liu, Yunyi Wang, Jing Ning, Woo Cheal Cho
Dermatopathology.2024; 11(3): 200. CrossRef - TRPS1 expression in MPNST is correlated with PRC2 inactivation and loss of H3K27me3
Rossana Lazcano, Davis R. Ingram, Gauri Panse, Alexander J. Lazar, Wei-Lien Wang, Jeffrey M. Cloutier
Human Pathology.2024; 151: 105632. CrossRef - Syringocystadenoma Papilliferum-Like Features in Poroma: An Unusual Morphologic Pattern of Poroma or True Synchronous Occurrence of 2 Distinct Neoplasms?
Mouaz Alsawas, Fiorinda F. Muhaj, Phyu P. Aung, Priyadharsini Nagarajan, Woo Cheal Cho
The American Journal of Dermatopathology.2024; 46(12): 871. CrossRef - A Comprehensive Review of TRPS1 as a Diagnostic Immunohistochemical Marker for Primary Breast Carcinoma: Latest Insights and Diagnostic Pitfalls
Antonia-Carmen Georgescu, Tiberiu-Augustin Georgescu, Simona-Alina Duca-Barbu, Lucian Gheorghe Pop, Daniela Oana Toader, Nicolae Suciu, Dragos Cretoiu
Cancers.2024; 16(21): 3568. CrossRef - Expression of TRPS1 in Metastatic Tumors of the Skin: An Immunohistochemical Study of 72 Cases
Kassiani Boulogeorgou, Christos Topalidis, Triantafyllia Koletsa, Georgia Karayannopoulou, Jean Kanitakis
Dermatopathology.2024; 11(4): 293. CrossRef
- Metastatic Vulvar Paget's Disease Presenting in a Supraclavicular Lymph Node: A Diagnostic Challenge on Fine Needle Aspiration Cytology
- BRCA-mutated gastric adenocarcinomas are associated with chromosomal instability and responsiveness to platinum-based chemotherapy
- Ji Hyun Oh, Chang Ohk Sung, Hyung-Don Kim, Sung-Min Chun, Jihun Kim
- J Pathol Transl Med. 2023;57(6):323-331. Published online November 14, 2023
- DOI: https://doi.org/10.4132/jptm.2023.10.22
- 6,403 View
- 265 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Homologous recombination defect is an important biomarker of chemotherapy in certain tumor types, and the presence of pathogenic or likely pathogenic mutations involving BRCA1 or BRCA2 (p-BRCA) mutations is the most well-established marker for the homologous recombination defect. Gastric cancer, one of the most prevalent tumor types in Asia, also harbors p-BRCA mutations.
Methods
To investigate the clinical significance of p-BRCA mutations, we analyzed 366 gastric cancer cases through next-generation sequencing. We determined the zygosity of p-BRCA mutations based on the calculated tumor purity through variant allelic fraction patterns and investigated whether the presence of p-BRCA mutations is associated with platinum-based chemotherapy and a certain molecular subtype.
Results
Biallelic p-BRCA mutation was associated with better response to platinum-based chemotherapy than heterozygous p-BRCA mutation or wild type BRCA genes. The biallelic p-BRCA mutations was observed only in the chromosomal instability subtype, while all p-BRCA mutations were heterozygous in microsatellite instability subtype.
Conclusions
In conclusion, patients with gastric cancer harboring biallelic p-BRCA mutations were associated with a good initial response to platinum-based chemotherapy and those tumors were exclusively chromosomal instability subtype. Further investigation for potential association with homologous recombination defect is warranted. -
Citations
Citations to this article as recorded by- Risk prediction criteria for the primary hepatic perivascular epithelioid cell tumour family, including angiomyolipoma: analysis of 132 cases with a literature review
Youngeun Yoo, Jihun Kim, In Hye Song
Histopathology.2025; 86(6): 979. CrossRef - Presence of RB1 or Absence of LRP1B Mutation Predicts Poor Overall Survival in Patients with Gastric Neuroendocrine Carcinoma and Mixed Adenoneuroendocrine Carcinoma
In Hye Song, Bokyung Ahn, Young Soo Park, Deok Hoon Kim, Seung-Mo Hong
Cancer Research and Treatment.2025; 57(2): 492. CrossRef - Predictive value of homologous recombination-related gene mutations in survival outcomes of first-line nivolumab plus chemotherapy for gastric cancer
Yuna Lee, Hyung-Don Kim, Sun Young Lee, Hyungeun Lee, Jaewon Hyung, Meesun Moon, Jinho Shin, Young Soo Park, Tae Won Kim, Min-Hee Ryu
Gastric Cancer.2025; 28(6): 1158. CrossRef - Association of RAD51 expression with response to neoadjuvant treatment and prognosis in locally advanced gastric cancer
Serhat Sekmek, Serhat Ozan, Fahriye Tugba Kos, Hayriye Tatli Dogan, Mehmet Akif Parlar, Didem Sener Dede
Expert Review of Anticancer Therapy.2025; 25(12): 1433. CrossRef - Artificial intelligence algorithm for neoplastic cell percentage estimation and its application to copy number variation in urinary tract cancer
Jinahn Jeong, Deokhoon Kim, Yeon-Mi Ryu, Ja-Min Park, Sun Young Yoon, Bokyung Ahn, Gi Hwan Kim, Se Un Jeong, Hyun-Jung Sung, Yong Il Lee, Sang-Yeob Kim, Yong Mee Cho
Journal of Pathology and Translational Medicine.2024; 58(5): 229. CrossRef
- Risk prediction criteria for the primary hepatic perivascular epithelioid cell tumour family, including angiomyolipoma: analysis of 132 cases with a literature review
Review
- The Asian Thyroid Working Group, from 2017 to 2023
- Kennichi Kakudo, Chan Kwon Jung, Zhiyan Liu, Mitsuyoshi Hirokawa, Andrey Bychkov, Huy Gia Vuong, Somboon Keelawat, Radhika Srinivasan, Jen-Fan Hang, Chiung-Ru Lai
- J Pathol Transl Med. 2023;57(6):289-304. Published online November 14, 2023
- DOI: https://doi.org/10.4132/jptm.2023.10.04
- 8,745 View
- 305 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The Asian Thyroid Working Group was founded in 2017 at the 12th Asia Oceania Thyroid Association (AOTA) Congress in Busan, Korea. This group activity aims to characterize Asian thyroid nodule practice and establish strict diagnostic criteria for thyroid carcinomas, a reporting system for thyroid fine needle aspiration cytology without the aid of gene panel tests, and new clinical guidelines appropriate to conservative Asian thyroid nodule practice based on scientific evidence obtained from Asian patient cohorts. Asian thyroid nodule practice is usually designed for patient-centered clinical practice, which is based on the Hippocratic Oath, “First do not harm patients,” and an oriental filial piety “Do not harm one’s own body because it is a precious gift from parents,” which is remote from defensive medical practice in the West where physicians, including pathologists, suffer from severe malpractice climate. Furthermore, Asian practice emphasizes the importance of resource management in navigating the overdiagnosis of low-risk thyroid carcinomas. This article summarizes the Asian Thyroid Working Group activities in the past 7 years, from 2017 to 2023, highlighting the diversity of thyroid nodule practice between Asia and the West and the background reasons why Asian clinicians and pathologists modified Western systems significantly.
-
Citations
Citations to this article as recorded by- Performance of Two‐Tiered Subclassification of Atypia of Undetermined Significance in Thyroid Fine‐Needle Aspiration Without Routine Molecular Testing
Pocholo D. Santos, Chiung‐Ru Lai, Jen‐Fan Hang
Diagnostic Cytopathology.2026; 54(2): 78. CrossRef - Risk of Infertility in Reproductive-Age Patients With Thyroid Cancer Receiving or Not Receiving 131I Treatment
Chun-Yi Lin, Cheng-Li Lin, Chia-Hung Kao
Clinical Nuclear Medicine.2025; 50(3): 201. CrossRef - Association Between Metabolic Dysfunction-Associated Steatotic Liver Disease and Thyroid Cancer
Sang Yi Moon, Minkook Son, Jung-Hwan Cho, Hye In Kim, Ji Min Han, Ji Cheol Bae, Sunghwan Suh
Thyroid®.2025; 35(1): 79. CrossRef - Letter: “High Rates of Unnecessary Surgery for Indeterminate Thyroid Nodules in the Absence of Molecular Test and the Cost-Effectiveness of Utilizing Molecular Test in an Asian Population: A Decision Analysis” by Fung et al
Kennichi Kakudo, Andrey Bychkov, Jen-Fan Hang, Mitsuyoshi Hirokawa, Somboon Keelawat, Zhiyan Liu, Radhika Srinivasan, Chan Kwon Jung
Thyroid®.2025; 35(5): 595. CrossRef - Thyroid Nodules with Nuclear Atypia of Undetermined Significance (AUS-Nuclear) Hold a Two-Times-Higher Risk of Malignancy than AUS-Other Nodules Regardless of EU-TIRADS Class of the Nodule or Borderline Tumor Interpretation
Dorota Słowińska-Klencka, Bożena Popowicz, Joanna Duda-Szymańska, Mariusz Klencki
Cancers.2025; 17(8): 1365. CrossRef - Response to Kakudo et al.: “High Rates of Unnecessary Surgery for Indeterminate Thyroid Nodules in the Absence of Molecular Test and the Cost-Effectiveness of Utilizing Molecular Test in an Asian Population: A Decision Analysis”
Man Him Matrix Fung, Ching Tang, Gin Wai Kwok, Tin Ho Chan, Yan Luk, David Tak Wai Lui, Carlos King Ho Wong, Brian Hung Hin Lang
Thyroid®.2025; 35(5): 597. CrossRef - Molecular Testing Could Drive Smarter Decision-Marking for Indeterminate Thyroid Nodule if the Price was Right
Sarah C. Brennan, Matti L. Gild, Venessa Tsang
Clinical Thyroidology®.2025; 37(5): 165. CrossRef - Welcoming the new, revisiting the old: a brief glance at cytopathology reporting systems for lung, pancreas, and thyroid
Rita Luis, Balamurugan Thirunavukkarasu, Deepali Jain, Sule Canberk
Journal of Pathology and Translational Medicine.2024; 58(4): 165. CrossRef - Are we ready to bridge classification systems? A comprehensive review of different reporting systems in thyroid cytology
Esther Diana Rossi, Liron Pantanowitz
Cytopathology.2024; 35(6): 674. CrossRef - Aggressive Types of Malignant Thyroid Neoplasms
Maria Boudina, Eleana Zisimopoulou, Persefoni Xirou, Alexandra Chrisoulidou
Journal of Clinical Medicine.2024; 13(20): 6119. CrossRef - Fine needle aspiration cytology diagnoses of follicular thyroid carcinoma: results from a multicenter study in Asia
Hee Young Na, Miyoko Higuchi, Shinya Satoh, Kaori Kameyama, Chan Kwon Jung, Su-Jin Shin, Shipra Agarwal, Jen-Fan Hang, Yun Zhu, Zhiyan Liu, Andrey Bychkov, Kennichi Kakudo, So Yeon Park
Journal of Pathology and Translational Medicine.2024; 58(6): 331. CrossRef
- Performance of Two‐Tiered Subclassification of Atypia of Undetermined Significance in Thyroid Fine‐Needle Aspiration Without Routine Molecular Testing
Original Article
- Senescent tumor cells in colorectal cancer are characterized by elevated enzymatic activity of complexes 1 and 2 in oxidative phosphorylation
- Jun Sang Shin, Tae-Gyu Kim, Young Hwa Kim, So Yeong Eom, So Hyun Park, Dong Hyun Lee, Tae Jun Park, Soon Sang Park, Jang-Hee Kim
- J Pathol Transl Med. 2023;57(6):305-314. Published online November 7, 2023
- DOI: https://doi.org/10.4132/jptm.2023.10.09
- 6,935 View
- 315 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Cellular senescence is defined as an irreversible cell cycle arrest caused by various internal and external insults. While the metabolic dysfunction of senescent cells in normal tissue is relatively well-established, there is a lack of information regarding the metabolic features of senescent tumor cells.
Methods
Publicly available single-cell RNA-sequencing data from the GSE166555 and GSE178341 datasets were utilized to investigate the metabolic features of senescent tumor cells. To validate the single-cell RNA-sequencing data, we performed senescence-associated β-galactosidase (SA-β-Gal) staining to identify senescent tumor cells in fresh frozen colorectal cancer tissue. We also evaluated nicotinamide adenine dinucleotide dehydrogenase–tetrazolium reductase (NADH-TR) and succinate dehydrogenase (SDH) activity using enzyme histochemical methods and compared the staining with SA-β-Gal staining. MTT assay was performed to reveal the complex 1 activity of the respiratory chain in in-vitro senescence model.
Results
Single-cell RNA-sequencing data revealed an upregulation in the activity of complexes 1 and 2 in oxidative phosphorylation, despite overall mitochondrial dysfunction in senescent tumor cells. Both SA-β-Gal and enzyme histochemical staining using fresh frozen colorectal cancer tissues indicated a high correlation between SA-β-Gal positivity and NADH-TR/SDH staining positivity. MTT assay showed that senescent colorectal cancer cells exhibit higher absorbance in 600 nm wavelength.
Conclusions
Senescent tumor cells exhibit distinct metabolic features, characterized by upregulation of complexes 1 and 2 in the oxidative phosphorylation pathway. NADH-TR and SDH staining represent efficient methods for detecting senescent tumor cells in colorectal cancer. -
Citations
Citations to this article as recorded by- Senescence, Aging and Disease Throughout the Gastrointestinal System
Sofia Ferreira-Gonzalez, Tomonori Matsumoto, Eiji Hara, Stuart J. Forbes
Gastroenterology.2025; 169(7): 1357. CrossRef - Cellular Aging and Senescence in Cancer: A Holistic Review of Cellular Fate Determinants
Muhammad Tufail, Yu-Qi Huang, Jia-Ju Hu, Jie Liang, Cai-Yun He, Wen-Dong Wan, Can-Hua Jiang, Hong Wu, Ning Li
Aging and disease.2024;[Epub] CrossRef - Real-time assessment of relative mitochondrial ATP synthesis response against inhibiting and stimulating substrates (MitoRAISE)
Eun Sol Chang, Kyoung Song, Ji-Young Song, Minjung Sung, Mi-Sook Lee, Jung Han Oh, Ji-Yeon Kim, Yeon Hee Park, Kyungsoo Jung, Yoon-La Choi
Cancer & Metabolism.2024;[Epub] CrossRef
- Senescence, Aging and Disease Throughout the Gastrointestinal System
Case Studies
- Diagnostic conundrums of schwannomas: two cases highlighting morphological extremes and diagnostic challenges in biopsy specimens of soft tissue tumors
- Chankyung Kim, Yang-Guk Chung, Chan Kwon Jung
- J Pathol Transl Med. 2023;57(5):278-283. Published online August 24, 2023
- DOI: https://doi.org/10.4132/jptm.2023.07.13
- 5,408 View
- 265 Download
- 3 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Schwannomas are benign, slow-growing peripheral nerve sheath tumors commonly occurring in the head, neck, and flexor regions of the extremities. Although most schwannomas are easily diagnosable, their variable morphology can occasionally create difficulty in diagnosis. Reporting pathologists should be aware that schwannomas can exhibit a broad spectrum of morphological patterns. Clinical and radiological examinations can show correlation and should be performed, in conjunction with ancillary tests, when appropriate. Furthermore, deferring a definitive diagnosis until excision may be necessary for small biopsy specimens and frozen sections. This report underscores these challenges through examination of two unique schwannoma cases, one predominantly cellular and the other myxoid, both of which posed significant challenges in histological interpretation.
-
Citations
Citations to this article as recorded by- Oral and maxillofacial schwannoma (OMSCH): An institutional study of 102 patients
Lingli Huang, Wenya Zhu, Qicheng Ye, Shengwen Liu, Hao Lu, Wenjun Yang, Wanlin Xu
Journal of Stomatology Oral and Maxillofacial Surgery.2026; 127(3): 102678. CrossRef - Plexiform Schwannoma Over the Anterior Chest Wall: A Clinicopathological Review
Debojyoti Sasmal, Saswata Barenya, Hinglaj Saha, Pankaj Kumar Halder
Amrita Journal of Medicine.2025; 21(2): 95. CrossRef - Giant Retroperitoneal Schwannoma: Case Report and Review of the Literature
Magdalena Alexieva, Evgeni V Mekov, Silvia Ivanova, Alexandrina Vlahova, Georgi Yankov
Cureus.2025;[Epub] CrossRef - Breast schwannoma: review of entity and differential diagnosis
Sandra Ixchel Sanchez, Ashley Cimino-Mathews
Journal of Pathology and Translational Medicine.2025; 59(6): 353. CrossRef
- Oral and maxillofacial schwannoma (OMSCH): An institutional study of 102 patients
- Hepatic small vessel neoplasm: not totally benign, not yet malignant
- Madison Miranda, David Howell, Tony El Jabbour
- J Pathol Transl Med. 2023;57(5):273-277. Published online August 24, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.19
- 6,742 View
- 280 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Hepatic small vessel neoplasm (HSVN) is a rare vascular tumor with few reports in the literature. While imaging findings may show characteristic enhancement patterns, limited available literature may not reveal the full potential for image-based diagnosis. Histologically, HSVN mimics other entities, though certain morphologic and immunohistochemical findings provide clues for diagnosis. However, HSVN still provides diagnostic challenges, especially on core biopsies with limited material for morphologic and molecular evaluation. While current recommendations are surgical resection and close observation, the long-term course of the tumor is unknown. We report a case of HSVN in a liver with additional feature of organized lymphoid aggregates necessitating additional hematopathology consultation and workup to rule out concurrent entities.
-
Citations
Citations to this article as recorded by- Mesenchymal Tumors of the Liver: An Update Review
Joon Hyuk Choi, Swan N. Thung
Biomedicines.2025; 13(2): 479. CrossRef - Revisiting Hepatic Small Vessel Neoplasms and Anastomosing Hemangiomas as a Unique Capillary Liver Neoplasm: A 25-Case Series With Pathomolecular Correlations
Aurélie Beaufrère, Astrid Laurent-Bellue, Antoinette Lemoine, Agnès Bourillon, Nathalie Sturm, Pierre Gosset, Virginie Cahn, Valérie Vilgrain, Maité Lewin, Valérie Paradis, Catherine Guettier
Modern Pathology.2025; 38(10): 100835. CrossRef - Imaging features of recently identified low-grade vascular neoplasia of the liver: hepatic small vessel neoplasm and anastomosing hemangioma
Maïté Lewin, Rauda Aldhaheri, Aurélie Beaufrère, Christophe Desterke, Anita Paisant, Ivan Bricault, Paul Borde, Gabriel Simon, Mickaël Lesurtel, Daniel Cherqui, Clara Prud’Homme, Valérie Vilgrain, Astrid Laurent-Bellue
European Radiology.2025;[Epub] CrossRef
- Mesenchymal Tumors of the Liver: An Update Review
Reviews
- Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
- Chan Kwon Jung
- J Pathol Transl Med. 2023;57(4):208-216. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.20
- 7,002 View
- 267 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - As the application of core needle biopsy (CNB) in evaluating thyroid nodules rises in clinical practice, the 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules have officially recognized its value for the first time. CNB procures tissue samples preserving both histologic structure and cytologic detail, thereby supplying substantial material for an accurate diagnosis and reducing the necessity for repeated biopsies or subsequent surgical interventions. The current review introduces the risk of malignancy within distinct diagnostic categories, emphasizing the implications of noninvasive follicular thyroid neoplasm with papillary-like nuclear features on these malignancy risks. Prior research has indicated diagnostic challenges associated with follicular-patterned lesions, resulting in notable variation within indeterminate diagnostic categories. The utilization of mutation-specific immunostaining in CNB enhances the accuracy of lesion classification. This review underlines the essential role of a multidisciplinary approach in diagnosing follicular-patterned lesions and the potential of mutation-specific immunostaining to strengthen diagnostic consensus and inform patient management decisions.
-
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef - Risk Stratification of Thyroid Nodules Diagnosed as Follicular Neoplasm on Core Needle Biopsy
Byeong-Joo Noh, Won Jun Kim, Jin Yub Kim, Ha Young Kim, Jong Cheol Lee, Myoung Sook Shim, Yong Jin Song, Kwang Hyun Yoon, In-Hye Jung, Hyo Sang Lee, Wooyul Paik, Dong Gyu Na
Endocrinology and Metabolism.2025; 40(4): 610. CrossRef - Diagnostic implication of thyroid spherules for cytological diagnosis of thyroid nodules
Heeseung Sohn, Kennichi Kakudo, Chan Kwon Jung
Cytopathology.2024; 35(3): 383. CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - The Diagnostic Role of Repeated Biopsy of Thyroid Nodules with Atypia of Undetermined Significance with Architectural Atypia on Core-Needle Biopsy
Hye Hyeon Moon, Sae Rom Chung, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee, Jung Hwan Baek
Endocrinology and Metabolism.2024; 39(2): 300. CrossRef - Core needle biopsy for thyroid nodules assessment-a new horizon?
David D Dolidze, Serghei Covantsev, Grigorii M Chechenin, Natalia V Pichugina, Anastasia V Bedina, Anna Bumbu
World Journal of Clinical Oncology.2024; 15(5): 580. CrossRef - Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
Agnes Stephanie Harahap, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2024; 58(5): 205. CrossRef - A simplified four-tier classification for thyroid core needle biopsy
M. Paja, J. L. Del Cura, R. Zabala, I. Korta, Mª T. Gutiérrez, A. Expósito, A. Ugalde
Journal of Endocrinological Investigation.2024; 48(4): 895. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- A stepwise approach to fine needle aspiration cytology of lymph nodes
- Yosep Chong, Gyeongsin Park, Hee Jeong Cha, Hyun-Jung Kim, Chang Suk Kang, Jamshid Abdul-Ghafar, Seung-Sook Lee
- J Pathol Transl Med. 2023;57(4):196-207. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.12
- 46,660 View
- 2,309 Download
- 11 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The cytological diagnosis of lymph node lesions is extremely challenging because of the diverse diseases that cause lymph node enlargement, including both benign and malignant or metastatic lymphoid lesions. Furthermore, the cytological findings of different lesions often resemble one another. A stepwise diagnostic approach is essential for a comprehensive diagnosis that combines: clinical findings, including age, sex, site, multiplicity, and ultrasonography findings; low-power reactive, metastatic, and lymphoma patterns; high-power population patterns, including two populations of continuous range, small monotonous pattern and large monotonous pattern; and disease-specific diagnostic clues including granulomas and lymphoglandular granules. It is also important to remember the histological features of each diagnostic category that are common in lymph node cytology and to compare them with cytological findings. It is also essential to identify a few categories of diagnostic pitfalls that often resemble lymphomas and easily lead to misdiagnosis, particularly in malignant small round cell tumors, poorly differentiated squamous cell carcinomas, and nasopharyngeal undifferentiated carcinoma. Herein, we review a stepwise approach for fine needle aspiration cytology of lymphoid diseases and suggest a diagnostic algorithm that uses this approach and the Sydney classification system.
-
Citations
Citations to this article as recorded by- Development and Validation of Explainable Artificial Intelligence System for Automatic Diagnosis of Cervical Lymphadenopathy From Ultrasound Images
Ming Xu, Yubiao Yue, Zhenzhang Li, Yinhong Li, Guoying Li, Haihua Liang, Di Liu, Xiaohong Xu, Mohamadreza (Mohammad) Khosravi
International Journal of Intelligent Systems.2025;[Epub] CrossRef - Application of the Sydney system for classification and reporting lymph node cytopathology: a retrospective analysis at a tertiary centre
Ashok Teja Kummari, Pramod Kumar Pamu, Krishna Kiran Ganna, Param Jyothi, Sadashivudu
International Journal of Research in Medical Sciences.2025;[Epub] CrossRef - Diagnostic approach to FNA biopsy of cystic lesions of the head and neck
Stefen Andrianus, Olivia Leung, Zubair Baloch
Cancer Cytopathology.2025;[Epub] CrossRef - Applicability of Fine-Needle Aspiration Biopsy of Lymph Nodes Using WHO Reporting System: Comparison between Pediatric and Adult Brazilian Populations
Leonardo Fávaro Ficoto, Deolino João Camilo Júnior, Gustavo Resende Nora, Vitor Bonetti Valente, Daniel Galera Bernabé, José Cândido Caldeira Xavier-Júnior
Acta Cytologica.2025; : 1. CrossRef - Intraoperative cytological assessment of sentinel lymph nodes in gynecologic cancer: diagnostic accuracy and limitations
O. V. Pankova, S. V. Vtorushin, M. V. Klimova, D. S. Pismenny, M. O. Ochirov, L. A. Kolomiets, V. M. Perelmuter
Siberian journal of oncology.2025; 24(5): 72. CrossRef - From smear to diagnosis: the impact of ancillary techniques in lymph node fine-needle cytology
Elisabetta Maffei, Giuseppe Di Motta, Angela D’Ardia, Riccardo Ruotolo, Valentina Giudice, Alessandro Caputo, Pio Zeppa
Journal of the American Society of Cytopathology.2025;[Epub] CrossRef - Immunocytochemical markers, molecular testing and digital cytopathology for aspiration cytology of metastatic breast carcinoma
Joshua J. X. Li, Gary M. Tse
Cytopathology.2024; 35(2): 218. CrossRef - Response to comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes”
Yosep Chong, Gyeongsin Park, Hee Jeong Cha, Hyun-Jung Kim, Chang Suk Kang, Jamshid Abdul-Ghafar, Seung-Sook Lee
Journal of Pathology and Translational Medicine.2024; 58(1): 43. CrossRef - Comment on “A stepwise approach to fine needle aspiration cytology of lymph nodes”
Elisabetta Maffei, Valeria Ciliberti, Pio Zeppa, Alessandro Caputo
Journal of Pathology and Translational Medicine.2024; 58(1): 40. CrossRef - The Incidence of Thyroid Cancer in Bethesda III Thyroid Nodules: A Retrospective Analysis at a Single Endocrine Surgery Center
Iyad Hassan, Lina Hassan, Nahed Balalaa, Mohamad Askar, Hussa Alshehhi, Mohamad Almarzooqi
Diagnostics.2024; 14(10): 1026. CrossRef - Efficiency of Fine-Needle Aspiration (FNA) in Relation to Tru-Cut Biopsy of Lateral Neck Swellings
Mohammed S Al Olaimat, Fahad S Al Qooz, Zaid R Alzoubi, Elham M Alsharaiah, Ali S Al Murdif, Mohammad O Alanazi
Cureus.2024;[Epub] CrossRef - Pitfalls in the Cytological Diagnosis of Nodal Hodgkin Lymphoma
Uma Handa, Rasheeda Mohamedali, Rajpal Singh Punia, Simrandeep Singh, Ranjeev Bhagat, Phiza Aggarwal, Manveen Kaur
Diagnostic Cytopathology.2024; 52(12): 715. CrossRef - Rapid 3D imaging at cellular resolution for digital cytopathology with a multi-camera array scanner (MCAS)
Kanghyun Kim, Amey Chaware, Clare B. Cook, Shiqi Xu, Monica Abdelmalak, Colin Cooke, Kevin C. Zhou, Mark Harfouche, Paul Reamey, Veton Saliu, Jed Doman, Clay Dugo, Gregor Horstmeyer, Richard Davis, Ian Taylor-Cho, Wen-Chi Foo, Lucas Kreiss, Xiaoyin Sara J
npj Imaging.2024;[Epub] CrossRef
- Development and Validation of Explainable Artificial Intelligence System for Automatic Diagnosis of Cervical Lymphadenopathy From Ultrasound Images
Case Study
- Metastatic choroidal melanoma in the breast: a case report and review of the literature
- Loay Abudalu, Vinisha Malhotra, Nabila Nasir, Sami Titi
- J Pathol Transl Med. 2023;57(4):238-241. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.07
- 5,001 View
- 128 Download
-
 Abstract
Abstract
 PDF
PDF - The breast is an unusual site for metastases, accounting for less than 2% of malignant breast lesions but include those from malignant melanomas, carcinomas, sarcomas, and lymphomas from various organs. We diagnosed a very rare case of metastatic choroidal melanoma for a 67-year-old female who presented with a right breast lump and who had been previously diagnosed with choroidal melanoma-monosomy 3 in 2017. To the best of our knowledge, only five such cases have been published so far, with one in a male patient.
Original Articles
- Clinicopathologic characterization of cervical metastasis from an unknown primary tumor: a multicenter study in Korea
- Miseon Lee, Uiree Jo, Joon Seon Song, Youn Soo Lee, Chang Gok Woo, Dong-Hoon Kim, Jung Yeon Kim, Sun Och Yoon, Kyung-Ja Cho
- J Pathol Transl Med. 2023;57(3):166-177. Published online May 10, 2023
- DOI: https://doi.org/10.4132/jptm.2023.04.12
- 6,160 View
- 171 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Research regarding cervical metastasis from an unknown primary tumor (CUP) according to human papillomavirus (HPV) and Epstein-Barr virus (EBV) status in Korea has been sporadic and small-scale. This study aims to analyze and understand the characteristics of CUP in Korea according to viral and p16 and p53 status through a multicenter study.
Methods
Ninety-five cases of CUP retrieved from six hospitals in Korea between January 2006 and December 2016 were subjected to high-risk HPV detection (DNA in situ hybridization [ISH] or real-time polymerase chain reaction), EBV detection (ISH), and immunohistochemistry for p16 and p53.
Results
CUP was HPV-related in 37 cases (38.9%), EBV-related in five cases (5.3%), and unrelated to HPV or EBV in 46 cases (48.4%). HPV-related CUP cases had the best overall survival (OS) (p = .004). According to the multivariate analysis, virus-unrelated disease (p = .023) and longer smoking duration (p < .005) were prognostic factors for poor OS. Cystic change (p = .016) and basaloid pattern (p < .001) were more frequent in HPV-related cases, and lymphoepithelial lesion was frequent in EBV-related cases (p = .010). There was no significant association between viral status and p53 positivity (p = .341), smoking status (p = .728), or smoking duration (p = .187). Korean data differ from Western data in the absence of an association among HPV, p53 positivity, and smoking history.
Conclusions
Virus-unrelated CUP in Korea had the highest frequency among all CUP cases. HPV-related CUP is similar to HPV-mediated oropharyngeal cancer and EBVrelated CUP is similar to nasopharyngeal cancer in terms of characteristics, respectively. -
Citations
Citations to this article as recorded by- Differenzierung von benignen und malignen Halszysten – eine diagnostische Herausforderung
Christina Sauter, Matthias Sand, Karim Plath, Michaela Maria Plath
Laryngo-Rhino-Otologie.2025; 104(05): 296. CrossRef - Unlocking the Hidden: Advancing Imaging Techniques in Diagnosing Cancers of Unknown Primary in the Head and Neck Region
Daniela Messineo, Filippo Valentini, Giovanni Francesco Niccolini, Federica Zoccali, Francesca Ripari, Enrico Marotta, Marcello Caratozzolo, Pasquale Frisina
Applied Sciences.2025; 15(4): 2194. CrossRef - Characterization of undifferentiated carcinoma of the salivary gland: clinicopathological and immunohistochemical analyses in comparison with lymphoepithelial carcinoma
Sangjoon Choi, Gyuheon Choi, Hee Jin Lee, Joon Seon Song, Yoon Se Lee, Seung-Ho Choi, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2025; 59(6): 361. CrossRef - Management of squamous cell carcinoma of unknown primary in the head and neck: current evidence-based diagnostic and treatment strategies
Marcel Kloppenburg, Matthias Santer, Lukas Schmutzler, Felix Johnson, Benedikt Hofauer, Teresa Steinbichler
memo - Magazine of European Medical Oncology.2025;[Epub] CrossRef - Expansion of tumor-infiltrating lymphocytes from head and neck squamous cell carcinoma to assess the potential of adoptive cell therapy
Sangjoon Choi, Mofazzal Hossain, Hyun Lee, Jina Baek, Hye Seon Park, Chae-Lyul Lim, DoYeon Han, Taehyun Park, Jong Hyeok Kim, Gyungyub Gong, Mi-Na Kweon, Hee Jin Lee
Cancer Immunology, Immunotherapy.2024;[Epub] CrossRef
- Differenzierung von benignen und malignen Halszysten – eine diagnostische Herausforderung
- Clinicopathologic significance of the delta-like ligand 4, vascular endothelial growth factor, and hypoxia-inducible factor-2α in gallbladder cancer
- Sujin Park, Junsik Kim, Woncheol Jang, Kyoung-Mee Kim, Kee-Taek Jang
- J Pathol Transl Med. 2023;57(2):113-122. Published online March 14, 2023
- DOI: https://doi.org/10.4132/jptm.2023.02.01
- 5,482 View
- 112 Download
- 8 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Gallbladder cancer (GBC) is usually detected in advanced stages with a low 5-year survival rate. Delta-like ligand 4 (DLL4), vascular endothelial growth factor (VEGF), and hypoxia-inducible factor-2alpha (HIF2α) have been studied for their role in tumorigenesis and potential for therapeutic target, and multiple clinical trials of the agents targeting them are ongoing. We investigated the expression of these markers in surgically resected GBC and tried to reveal their association with the clinicopathologic features, mutual correlation of their expression, and prognosis of the GBC patients by their expression.
Methods
We constructed the tissue microarray blocks of 99 surgically resected GBC specimens and performed immunohistochemistry of DLL4, VEGF, and HIF2α. We used the quantitative digital image analysis to evaluate DLL4 and VEGF expression, while the expression of HIF2α was scored manually.
Results
The expression of VEGF and HIF2α showed a significant trend with tumor differentiation (p= .028 and p= .006, respectively). We found that the high DLL4 and VEGF expression were significantly correlated with lymph node metastasis (p= .047, both). The expression of VEGF and HIF2α were significantly correlated (p < .001). The GBC patients with low HIF2α expression showed shorter recurrence-free survival than those with high HIF2α expression.
Conclusions
This study suggested the possibility of the usage of DLL4 and VEGF to predict the lymph node metastasis and the possibility of VEGF and HIF2α to predict the expression level mutually. Further studies may be needed to validate our study results and eventually accelerate the introduction of the targeted therapy in GBC. -
Citations
Citations to this article as recorded by- Dedifferentiated Leiomyosarcoma of the Uterine Corpus with Heterologous Component: Clinicopathological Analysis of Five Consecutive Cases from a Single Institution and Comprehensive Literature Review
Suyeon Kim, Hyunsik Bae, Hyun-Soo Kim
Diagnostics.2024; 14(2): 160. CrossRef - Identification of Key Immune Infiltration Related Genes Involved in Aortic Dissection Using Bioinformatic Analyses and Experimental Verification
Lin Zheng, Yusi Yang, Jie Liu, Tianliang Zhao, Xin Zhang, Lihua Chen
Journal of Inflammation Research.2024; Volume 17: 2119. CrossRef
- Dedifferentiated Leiomyosarcoma of the Uterine Corpus with Heterologous Component: Clinicopathological Analysis of Five Consecutive Cases from a Single Institution and Comprehensive Literature Review
Review
- A standardized pathology report for gastric cancer: 2nd edition
- Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi, Hee Kyung Chang, Soomin Ahn, Mee Soo Chang, Song-Hee Han, Yoonjin Kwak, An Na Seo, Sung Hak Lee, Mee-Yon Cho
- J Pathol Transl Med. 2023;57(1):1-27. Published online January 15, 2023
- DOI: https://doi.org/10.4132/jptm.2022.12.23
- 34,427 View
- 1,529 Download
- 22 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - The first edition of ‘A Standardized Pathology Report for Gastric Cancer’ was initiated by the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists and published 17 years ago. Since then, significant advances have been made in the pathologic diagnosis, molecular genetics, and management of gastric cancer (GC). To reflect those changes, a committee for publishing a second edition of the report was formed within the Gastrointestinal Pathology Study Group of the Korean Society of Pathologists. This second edition consists of two parts: standard data elements and conditional data elements. The standard data elements contain the basic pathologic findings and items necessary to predict the prognosis of GC patients, and they are adequate for routine surgical pathology service. Other diagnostic and prognostic factors relevant to adjuvant therapy, including molecular biomarkers, are classified as conditional data elements to allow each pathologist to selectively choose items appropriate to the environment in their institution. We trust that the standardized pathology report will be helpful for GC diagnosis and facilitate large-scale multidisciplinary collaborative studies.
-
Citations
Citations to this article as recorded by- Spatial and Temporal Tumor Heterogeneity in Gastric Cancer: Discordance of Predictive Biomarkers
Hye Seung Lee
Journal of Gastric Cancer.2025; 25(1): 192. CrossRef - PD-L1 as a Biomarker in Gastric Cancer Immunotherapy
Yunjoo Cho, Soomin Ahn, Kyoung-Mee Kim
Journal of Gastric Cancer.2025; 25(1): 177. CrossRef - Korean Gastric Cancer Association-Led Nationwide Survey on Surgically Treated Gastric Cancers in 2023
Dong Jin Kim, Jeong Ho Song, Ji-Hyeon Park, Sojung Kim, Sin Hye Park, Cheol Min Shin, Yoonjin Kwak, Kyunghye Bang, Chung-sik Gong, Sung Eun Oh, Yoo Min Kim, Young Suk Park, Jeesun Kim, Ji Eun Jung, Mi Ran Jung, Bang Wool Eom, Ki Bum Park, Jae Hun Chung, S
Journal of Gastric Cancer.2025; 25(1): 115. CrossRef - A Comprehensive and Comparative Review of Global Gastric Cancer Treatment Guidelines: 2024 Update
Sang Soo Eom, Keun Won Ryu, Hye Sook Han, Seong-Ho Kong
Journal of Gastric Cancer.2025; 25(1): 153. CrossRef - Korea, Japan, Europe, and the United States: Why are guidelines for gastric cancer different?
Emily E. Stroobant, Seong-Ho Kong, Maria Bencivenga, Takahiro Kinoshita, Tae-Han Kim, Takeshi Sano, Giovanni de Manzoni, Han-Kwang Yang, Yuko Kitagawa, Vivian E. Strong
Gastric Cancer.2025; 28(4): 559. CrossRef - Can the Japanese guidelines for endoscopic submucosal dissection be safely applied to Korean gastric cancer patients? A multicenter retrospective study based on the Korean Gastric Cancer Association nationwide survey
Hayemin Lee, Mi Ryeong Park, Junhyun Lee
Annals of Surgical Treatment and Research.2025; 109(2): 81. CrossRef - Double optimal transport for differential gene regulatory network inference with unpaired samples
Mengyu Li, Bencong Zhu, Cheng Meng, Xiaodan Fan, Laura Cantini
Bioinformatics.2025;[Epub] CrossRef - A Randomized Controlled Trial to Evaluate the Effect of Fibrin Glue on Bleeding after Gastric Endoscopic Submucosal Dissection
Tae-Se Kim, Tae-Jun Kim, Yang Won Min, Hyuk Lee, Byung-Hoon Min, Jun Haeng Lee, Poong-Lyul Rhee, Jae J. Kim
Gut and Liver.2025; 19(5): 677. CrossRef - Diagnostic accuracy of stereomicroscopy assessment of invasion depth in ex vivo specimens of early gastric cancer
Jing Wang, Lin Chang, Dong-Feng Niu, Yan Yan, Chang-Qi Cao, Shi-Jie Li, Qi Wu
World Journal of Gastroenterology.2025;[Epub] CrossRef - SMMILe enables accurate spatial quantification in digital pathology using multiple-instance learning
Zeyu Gao, Anyu Mao, Yuxing Dong, Hannah Clayton, Jialun Wu, Jiashuai Liu, ChunBao Wang, Kai He, Tieliang Gong, Chen Li, Mireia Crispin-Ortuzar
Nature Cancer.2025; 6(12): 2025. CrossRef - Genomic and Transcriptomic Characterization of Gastric Cancer with Bone Metastasis
Sujin Oh, Soo Kyung Nam, Keun-Wook Lee, Hye Seung Lee, Yujun Park, Yoonjin Kwak, Kyu Sang Lee, Ji-Won Kim, Jin Won Kim, Minsu Kang, Young Suk Park, Sang-Hoon Ahn, Yun-Suhk Suh, Do Joong Park, Hyung Ho Kim
Cancer Research and Treatment.2024; 56(1): 219. CrossRef - Microscopic tumor mapping of post-neoadjuvant therapy pancreatic cancer specimens to predict post-surgical recurrence: A prospective cohort study
Yeshong Park, Yeon Bi Han, Jinju Kim, MeeYoung Kang, Boram Lee, Eun Sung Ahn, Saemi Han, Haeryoung Kim, Hee-Young Na, Ho-Seong Han, Yoo-Seok Yoon
Pancreatology.2024; 24(4): 562. CrossRef - Effect of Neoadjuvant Chemotherapy on Tumor-Infiltrating Lymphocytes in Resectable Gastric Cancer: Analysis from a Western Academic Center
Elliott J. Yee, Danielle Gilbert, Jeffrey Kaplan, Sachin Wani, Sunnie S. Kim, Martin D. McCarter, Camille L. Stewart
Cancers.2024; 16(7): 1428. CrossRef - Interpretation of PD-L1 expression in gastric cancer: summary of a consensus meeting of Korean gastrointestinal pathologists
Soomin Ahn, Yoonjin Kwak, Gui Young Kwon, Kyoung-Mee Kim, Moonsik Kim, Hyunki Kim, Young Soo Park, Hyeon Jeong Oh, Kyoungyul Lee, Sung Hak Lee, Hye Seung Lee
Journal of Pathology and Translational Medicine.2024; 58(3): 103. CrossRef - Expression of claudin 18.2 in poorly cohesive carcinoma and its association with clinicopathologic parameters in East Asian patients
Moonsik Kim, Byung Woog Kang, Jihyun Park, Jin Ho Baek, Jong Gwang Kim
Pathology - Research and Practice.2024; 263: 155628. CrossRef - Clinicopathological analysis of claudin 18.2 focusing on intratumoral heterogeneity and survival in patients with metastatic or unresectable gastric cancer
T.-Y. Kim, Y. Kwak, S.K. Nam, D. Han, D.-Y. Oh, S.-A. Im, H.S. Lee
ESMO Open.2024; 9(12): 104000. CrossRef - Pathological Interpretation of Gastric Tumors in Endoscopic Submucosal Dissection
Jung Yeon Kim
Journal of Digestive Cancer Research.2023; 11(1): 15. CrossRef - Histopathology of Gastric Cancer
Baek-hui Kim, Sung Hak Lee
The Korean Journal of Helicobacter and Upper Gastrointestinal Research.2023; 23(2): 143. CrossRef - Endoscopic submucosal dissection hands-on training with artificial mucosal layer EndoGEL
Tae-Se Kim, Jun Haeng Lee
Journal of Innovative Medical Technology.2023; 1(1): 5. CrossRef
- Spatial and Temporal Tumor Heterogeneity in Gastric Cancer: Discordance of Predictive Biomarkers
Original Article
- The proteomic landscape shows oncologic relevance in cystitis glandularis
- Jun Yong Kim, Dohyun Han, Hyeyoon Kim, Minsun Jung, Han Suk Ryu
- J Pathol Transl Med. 2023;57(1):67-74. Published online December 22, 2022
- DOI: https://doi.org/10.4132/jptm.2022.10.24
- 5,344 View
- 177 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The relationship between cystitis glandularis (CG) and bladder malignancy remains unclear.
Methods
We identified the oncologic significance of CG at the molecular level using liquid chromatography-tandem mass spectrometry-based proteomic analysis of 10 CG, 12 urothelial carcinoma (UC), and nine normal urothelium (NU) specimens. Differentially expressed proteins (DEPs) were identified based on an analysis of variance false discovery rate < 0.05, and their functional enrichment was analyzed using a network model, Gene Set Enrichment Analysis, and Gene Ontology annotation.
Results
We identified 9,890 proteins across all samples and 1,139 DEPs among the three entities. A substantial number of DEPs overlapped in CG/NU, distinct from UC. Interestingly, we found that a subset of DEP clusters (n = 53, 5%) was differentially expressed in NU but similarly between CG and UC. This “UC-like signature” was enriched for reactive oxygen species (ROS) and energy metabolism, growth and DNA repair, transport, motility, epithelial-mesenchymal transition, and cell survival. Using the top 10 shortlisted DEPs, including SOD2, PRKCD, CYCS, and HCLS1, we identified functional elements related to ROS metabolism, development, and transport using network analysis. The abundance of these four molecules in UC/CG than in NU was consistent with the oncologic functions in CG.
Conclusions
Using a proteomic approach, we identified a predominantly non-neoplastic landscape of CG, which was closer to NU than to UC. We also confirmed a small subset of common DEPs in UC and CG, suggesting that altered ROS metabolism might imply potential cancerous risks in CG. -
Citations
Citations to this article as recorded by- Quantitative proteomics and immunohistochemistry uncover NT5DC2 as a diagnostic biomarker for papillary urothelial carcinoma
Jun Yong Kim, Jae Seok Lee, Dohyun Han, Ilias P. Nikas, Hyeyoon Kim, Minsun Jung, Han Suk Ryu
Heliyon.2024; 10(15): e35475. CrossRef - KRT18 as a Novel Biomarker of Urothelial Papilloma while Evaluating Low-Grade Papillary Urothelial Neoplasms: Bi-Center Analysis
Minsun Jung, Bohyun Kim, Jae Seok Lee, Jun Yong Kim, Dohyun Han, Kwangsoo Kim, Sunah Yang, Eun Na Kim, Hyeyooon Kim, Ilias P. Nikas, Sohyeon Yang, Kyung Chul Moon, Hyebin Lee, Han Suk Ryu
Pathobiology.2024; : 1. CrossRef
- Quantitative proteomics and immunohistochemistry uncover NT5DC2 as a diagnostic biomarker for papillary urothelial carcinoma
Reviews
- Biomarker testing of cytology specimens in personalized medicine for lung cancer patients
- Hyojin Kim, Jin-Haeng Chung
- J Pathol Transl Med. 2022;56(6):326-333. Published online November 9, 2022
- DOI: https://doi.org/10.4132/jptm.2022.10.17
- 6,490 View
- 176 Download
- 8 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Every patient with advanced non–small cell lung cancer (NSCLC) should be tested for targetable driver mutations and gene arrangements that may open avenues for targeted therapy. As most patients with NSCLC in the advanced stage of the disease are not candidates for surgery, these tests have to be performed on small biopsies or cytology samples. A growing number of other genetic changes with targetable mutations may be treatable in the near future. To identify patients who might benefit from novel targeted therapy, relevant markers should be tested in an appropriate context. In addition, immunotherapy of lung cancer is guided by the status of programmed death-ligand 1 expression in tumor cells. The variety and versatility of cytological specimen preparations offer significant advantages for molecular testing; however, they frequently remain underused. Therefore, evaluating the utility and adequacy of cytologic specimens is important, not only from a lung cancer diagnosis, but also for the large number of ancillary studies that are necessary to provide appropriate clinical management. A large proportion of lung cancers is diagnosed by aspiration or exfoliative cytology specimens; thus, optimizing strategies to triage and best use the tissue for diagnosis and biomarker studies forms a critical component of lung cancer management. In this review, we discuss the opportunities and challenges of using cytologic specimens for biomarker testing of lung cancer and the role of cytopathology in the molecular era.
-
Citations
Citations to this article as recorded by- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer
Paul Hofman, Petros Christopoulos, Nicky D’Haene, John Gosney, Nicola Normanno, Ed Schuuring, Ming-Sound Tsao, Christine Quinn, Jayne Russell, Katherine E Keating, Fernando López-Ríos
Lung Cancer.2025; 201: 108107. CrossRef - Validation of ancillary procedures on formalin liquid fixed aspiration cytologic samples: from minimum to maximum
Orsolya Rideg, Tímea Dergez, Arnold Tóth, Tamás Tornóczky, Gábor Pavlovics, Endre Kálmán
American Journal of Clinical Pathology.2025;[Epub] CrossRef - Molecular testing of cytology specimens: Issues in specimen adequacy and clinical utility
Ghulam Ghous, Komal Ijaz, Magda Esebua, Lester J. Layfield
Diagnostic Cytopathology.2024; 52(2): 123. CrossRef - The updated College of American Pathologists principles of analytic validation of immunohistochemical assays: A step forward for cytopathology
Sinchita Roy‐Chowdhuri
Cancer Cytopathology.2024; 132(9): 547. CrossRef - Best-Practice Biomarker Testing of Oesophago-Gastric Cancer in the UK: Expert Consensus Recommendations Developed Using a Modified Delphi
N.P. West, W. Mansoor, P. Taniere, E. Smyth, M. Rodriguez-Justo, A. Oniscu, P. Carter
Clinical Oncology.2024; 36(11): 701. CrossRef - Next step of molecular pathology: next-generation sequencing in cytology
Ricella Souza da Silva, Fernando Schmitt
Journal of Pathology and Translational Medicine.2024; 58(6): 291. CrossRef
- Proposal of real-world solutions for the implementation of predictive biomarker testing in patients with operable non-small cell lung cancer
- Noninvasive follicular thyroid neoplasm with papillary-like nuclear features: its updated diagnostic criteria, preoperative cytologic diagnoses and impact on the risk of malignancy
- Hee Young Na, So Yeon Park
- J Pathol Transl Med. 2022;56(6):319-325. Published online November 9, 2022
- DOI: https://doi.org/10.4132/jptm.2022.09.29
- 9,312 View
- 314 Download
- 9 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF - Due to the extremely indolent behavior, a subset of noninvasive encapsulated follicular variant papillary thyroid carcinomas has been classified as “noninvasive follicular thyroid neoplasm with papillary-like nuclear features (NIFTP)” since 2016 and is no longer considered carcinoma. Since the introduction of this new terminology, changes and refinements have been made in diagnostic criteria. Initially, the incidence of NIFTP was estimated substantial. However, the reported incidence of NIFTP varies greatly among studies and regions, with higher incidence in North American and European countries than in Asian countries. Thus, the changes in the risk of malignancy (ROM) in the Bethesda System for Reporting Thyroid Cytopathology (TBSRTC) differ inevitably among regions. Because more conservative surgery is recommended for NIFTPs, distinguishing NIFTPs from papillary thyroid carcinomas in preoperative fine-needle aspiration cytology became one of the major concerns. This review will provide comprehensive overview of updates on diagnostic criteria, actual incidence and preoperative cytologic diagnoses of NIFTP, and its impact on the ROM in TBSRTC.
-
Citations
Citations to this article as recorded by- Diagnosis of invasive encapsulated follicular variant papillary thyroid carcinoma by protein-based machine learning
Truong Phan-Xuan Nguyen, Minh-Khang Le, Sittiruk Roytrakul, Shanop Shuangshoti, Nakarin Kitkumthorn, Somboon Keelawat
Journal of Pathology and Translational Medicine.2025; 59(1): 39. CrossRef - Papillae, psammoma bodies, and/or many nuclear pseudoinclusions are helpful criteria but should not be required for a definitive cytologic diagnosis of papillary thyroid carcinoma: An institutional experience of 207 cases with surgical follow up
Tarik M. Elsheikh, Matthew Thomas, Jennifer Brainard, Jessica Di Marco, Erica Manosky, Bridgette Springer, Dawn Underwood, Deborah J. Chute
Cancer Cytopathology.2024; 132(6): 348. CrossRef - ThyroSeq overview on indeterminate thyroid nodules: An institutional experience
Sam Sirotnikov, Christopher C. Griffith, Daniel Lubin, Chao Zhang, Nabil F. Saba, Dehong Li, Amanda Kornfield, Amy Chen, Qiuying Shi
Diagnostic Cytopathology.2024; 52(7): 353. CrossRef - Oncocytic Noninvasive Follicular Thyroid Neoplasm with Papillary-Like Nuclear Features: A Case Report
Kaveripakam Ajay Joseph, Sana Ahuja, Sufian Zaheer
Indian Journal of Surgical Oncology.2024; 15(S4): 606. CrossRef - Cytologic hallmarks and differential diagnosis of papillary thyroid carcinoma subtypes
Agnes Stephanie Harahap, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2024; 58(6): 265. CrossRef - Preoperative evaluation of thyroid nodules – Diagnosis and management strategies
Tapoi Dana Antonia, Lambrescu Ioana Maria, Gheorghisan-Galateanu Ancuta-Augustina
Pathology - Research and Practice.2023; 246: 154516. CrossRef - Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
Chan Kwon Jung
Journal of Pathology and Translational Medicine.2023; 57(4): 208. CrossRef - Strategies for Treatment of Thyroid Cancer
Deepika Yadav, Pramod Kumar Sharma, Rishabha Malviya, Prem Shankar Mishra
Current Drug Targets.2023; 24(5): 406. CrossRef - Identification of NIFTP-Specific mRNA Markers for Reliable Molecular Diagnosis of Thyroid Tumors
So-Yeon Lee, Jong-Lyul Park, Kwangsoon Kim, Ja Seong Bae, Jae-Yoon Kim, Seon-Young Kim, Chan Kwon Jung
Endocrine Pathology.2023; 34(3): 311. CrossRef
- Diagnosis of invasive encapsulated follicular variant papillary thyroid carcinoma by protein-based machine learning
Original Articles
- Diagnostic distribution and pitfalls of glandular abnormalities in cervical cytology: a 25-year single-center study
- Jung-A Sung, Ilias P. Nikas, Haeryoung Kim, Han Suk Ryu, Cheol Lee
- J Pathol Transl Med. 2022;56(6):354-360. Published online November 9, 2022
- DOI: https://doi.org/10.4132/jptm.2022.09.05
- 8,298 View
- 154 Download
- 5 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Detection of glandular abnormalities in Papanicolaou (Pap) tests is challenging. This study aimed to review our institute’s experience interpreting such abnormalities, assess cytohistologic concordance, and identify cytomorphologic features associated with malignancy in follow-up histology.
Methods
Patients with cytologically-detected glandular lesions identified in our pathology records from 1995 to 2020 were included in this study.
Results
Of the 683,197 Pap tests performed, 985 (0.144%) exhibited glandular abnormalities, 657 of which had tissue follow-up available. One hundred eighty-eight cases were cytologically interpreted as adenocarcinoma and histologically diagnosed as malignant tumors of various origins. There were 213 cases reported as atypical glandular cells (AGC) and nine cases as adenocarcinoma in cytology, yet they were found to be benign in follow-up histology. In addition, 48 cases diagnosed with AGC and six with adenocarcinoma cytology were found to have cervical squamous lesions in follow-up histology, including four squamous cell carcinomas. Among the cytomorphological features examined, nuclear membrane irregularity, three-dimensional clusters, single-cell pattern, and presence of mitoses were associated with malignant histology in follow-up.
Conclusions
This study showed our institute’s experience detecting glandular abnormalities in cervical cytology over a 25-year period, revealing the difficulty of this task. Nonetheless, the present study indicates that several cytological findings such as membrane irregularity, three-dimensional clusters, single-cell pattern, and evidence of proliferation could help distinguishing malignancy from a benign lesion. -
Citations
Citations to this article as recorded by- “Atypical Glandular Cells” on Cervical Cytology: Correlation Between Glandular Cell Component Volume and Histological Follow‐Up
Havva Gokce Terzioglu, Alessa Aragao, Julieta E. Barroeta
Diagnostic Cytopathology.2026; 54(2): 71. CrossRef - Expertise in Gynecological Pathology Impacts Diagnosis of Atypical Glandular Cell Category in Cervical Cytology
Havva Gökce Terzioglu, Alessa Aragao, Julieta E. Barroeta
Journal of Lower Genital Tract Disease.2025; 29(4): 297. CrossRef - Analysis of atypical glandular cells in ThinPrep Pap smear and follow-up histopathology
Tengfei Wang, Yinan Hua, Lina Liu, Bing Leng
Baylor University Medical Center Proceedings.2024; 37(3): 403. CrossRef
- “Atypical Glandular Cells” on Cervical Cytology: Correlation Between Glandular Cell Component Volume and Histological Follow‐Up
- Prognostic and clinicopathological significance of Fusobacterium nucleatum in colorectal cancer: a systemic review and meta-analysis
- Younghoon Kim, Nam Yun Cho, Gyeong Hoon Kang
- J Pathol Transl Med. 2022;56(3):144-151. Published online May 15, 2022
- DOI: https://doi.org/10.4132/jptm.2022.03.13
- 8,659 View
- 144 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Fusobacterium nucleatum has been identified to promote tumor progression in colorectal cancer (CRC). However, association between F. nucleatum and prognostic or clinicopathological features has been diverse among studies, which could be affected by type of biospecimen (formalin-fixed paraffin-embedded or fresh frozen [FF]).
Methods
Articles were systemically reviewed for studies that included the correlation between F. nucleatum and prognosis or clinicopathological features in CRC.
Results
Ten articles, eight studies with survival-related features involving 3,199 patients and nine studies with clinical features involving 2,655 patients, were eligible for the meta-analysis. Overall survival, disease-free survival, and cancer-specific survival were all associated with worse prognosis in F. nucleatum–high patients (p<.05). In subgroup analysis, only studies with FF tissues retained prognostic significance with F. nucleatum. In meta-analysis of clinicopathological variables, F. nucleatum level was associated with location within colon, pT category, MLH1 hypermethylation, microsatellite instability status, and BRAF mutation regardless of type of biospecimen. However, lymph node metastasis and KRAS mutation was only associated with F. nucleatum level in FF-based studies.
Conclusions
In conclusion, type of biospecimen could affect the role of F. nucleatum as a biomarker associated with clinicopathological features and prognosis. -
Citations
Citations to this article as recorded by- Unraveling the Role of Fusobacterium nucleatum in Colorectal Cancer: Molecular Mechanisms and Pathogenic Insights
Linda Galasso, Fabrizio Termite, Irene Mignini, Giorgio Esposto, Raffaele Borriello, Federica Vitale, Alberto Nicoletti, Mattia Paratore, Maria Elena Ainora, Antonio Gasbarrini, Maria Assunta Zocco
Cancers.2025; 17(3): 368. CrossRef - Intratumoural pks Escherichia coli is associated with risk of metachronous colorectal cancer and adenoma development in people with Lynch syndrome
Yen Lin Chu, Peter Georgeson, Mark Clendenning, Khalid Mahmood, Romy Walker, Julia Como, Sharelle Joseland, Susan G. Preston, Toni Rice, Brigid M. Lynch, Roger L. Milne, Melissa C. Southey, Graham G. Giles, Amanda I. Phipps, John L. Hopper, Aung K. Win, C
eBioMedicine.2025; 114: 105661. CrossRef - Fusobacterium nucleatum Enrichment in Colorectal Tumor Tissue: Associations With Tumor Characteristics and Survival Outcomes
Amanda I. Phipps, Courtney M. Hill, Genevieve Lin, Rachel C. Malen, Adriana M. Reedy, Orsalem Kahsai, Hamza Ammar, Keith Curtis, Ningxin Ma, Timothy W. Randolph, Jing Ma, Shuji Ogino, Polly A. Newcomb, Meredith AJ. Hullar
Gastro Hep Advances.2025; 4(6): 100644. CrossRef - Enhancing fibroblast–epithelial cell communications: Serpine2 as a key molecule in Fusobacterium nucleatum–promoted colon cancer
Xueke Li, Simin Luo, Yifang Jiang, Qiong Ma, Fengming You, Qixuan Kuang, Xi Fu, Chuan Zheng
Frontiers in Immunology.2025;[Epub] CrossRef - The presence and relative abundance of salivary Fusobacterium nucleatum are not associated with colorectal cancer: a systematic review and meta-analysis
Ellay Gutmacher, Bálint Zsombor Sárai, Petrana Martineková, Szilvia Kiss-Dala, Gergely Agócs, Péter Hegyi, Andrea Bródy, Ákos Zsembery
Scientific Reports.2025;[Epub] CrossRef - The role of oral microbiota in digestive system diseases: current advances and perspectives
Yaqi Li, Yiping Xin, Wenlu Zong, Xiaoyu Li
Journal of Oral Microbiology.2025;[Epub] CrossRef - Fusobacterium Nucleatum in Colorectal Cancer: Relationship Among Immune Modulation, Potential Biomarkers and Therapeutic Implications
Dalila Incognito, Giuliana Ciappina, Claudia Gelsomino, Antonio Picone, Pierluigi Consolo, Alessandra Scano, Tindara Franchina, Nicola Maurea, Vincenzo Quagliariello, Salvatore Berretta, Alessandro Ottaiano, Massimiliano Berretta
International Journal of Molecular Sciences.2025; 26(19): 9710. CrossRef - Intratumoral presence of the genotoxic gut bacteria pks+ E. coli, Enterotoxigenic Bacteroides fragilis, and Fusobacterium nucleatum and their association with clinicopathological and molecular features of colorectal cancer
Jihoon E. Joo, Yen Lin Chu, Peter Georgeson, Romy Walker, Khalid Mahmood, Mark Clendenning, Aaron L. Meyers, Julia Como, Sharelle Joseland, Susan G. Preston, Natalie Diepenhorst, Julie Toner, Danielle J. Ingle, Norelle L. Sherry, Andrew Metz, Brigid M. Ly
British Journal of Cancer.2024; 130(5): 728. CrossRef - The role of Fusobacterium nucleatum in cancer and its implications for clinical applications
Wanyi Luo, Juxi Han, Xian Peng, Xuedong Zhou, Tao Gong, Xin Zheng
Molecular Oral Microbiology.2024; 39(6): 417. CrossRef -
Fusobacterium nucleatum Load Correlates with KRAS Mutation and Sessile Serrated Pathogenesis in Colorectal Adenocarcinoma
Koki Takeda, Minoru Koi, Yoshiki Okita, Sija Sajibu, Temitope O. Keku, John M. Carethers
Cancer Research Communications.2023; 3(9): 1940. CrossRef - Tumour Colonisation of Parvimonas micra Is Associated with Decreased Survival in Colorectal Cancer Patients
Thyra Löwenmark, Anna Löfgren-Burström, Carl Zingmark, Ingrid Ljuslinder, Michael Dahlberg, Sofia Edin, Richard Palmqvist
Cancers.2022; 14(23): 5937. CrossRef
- Unraveling the Role of Fusobacterium nucleatum in Colorectal Cancer: Molecular Mechanisms and Pathogenic Insights
Review
- Neuropathologic features of central nervous system hemangioblastoma
- Rebecca A. Yoda, Patrick J. Cimino
- J Pathol Transl Med. 2022;56(3):115-125. Published online May 3, 2022
- DOI: https://doi.org/10.4132/jptm.2022.04.13
- 16,501 View
- 368 Download
- 18 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF - Hemangioblastoma is a benign, highly vascularized neoplasm of the central nervous system (CNS). This tumor is associated with loss of function of the VHL gene and demonstrates frequent occurrence in von Hippel-Lindau (VHL) disease. While this entity is designated CNS World Health Organization grade 1, due to its predilection for the cerebellum, brainstem, and spinal cord, it is still an important cause of morbidity and mortality in affected patients. Recognition and accurate diagnosis of hemangioblastoma is essential for the practice of surgical neuropathology. Other CNS neoplasms, including several tumors associated with VHL disease, may present as histologic mimics, making diagnosis challenging. We outline key clinical and radiologic features, pathophysiology, treatment modalities, and prognostic information for hemangioblastoma, and provide a thorough review of the gross, microscopic, immunophenotypic, and molecular features used to guide diagnosis.
-
Citations
Citations to this article as recorded by- Immunohistochemical Expression of PAX8 in Central Nervous System Hemangioblastomas: A Potential Diagnostic Pitfall for Neuropathologists
Giuseppe Broggi, Jessica Farina, Valeria Barresi, Francesco Certo, Giuseppe Maria Vincenzo Barbagallo, Gaetano Magro, Rosario Caltabiano
Applied Immunohistochemistry & Molecular Morphology.2025; 33(3): 160. CrossRef - Endolymphatic Sac Tumor. Post-Radiosurgery Evaluation Using Time-Resolved Imaging of Contrast Kinetics MR Angiography
Antonella Blandino, Allegra Romano, Chiara Filippi, Sofia Pizzolante, Andrea Romano, Giulia Moltoni, Edoardo Covelli, Maurizio Barbara, Alessandro Bozzao
Ear, Nose & Throat Journal.2025;[Epub] CrossRef - Stereotactic radiosurgery in the management of central nervous system hemangioblastomas: a systematic review and meta-analysis
Amirhossein Zare, Amirhessam Zare, Alireza Soltani Khaboushan, Bardia Hajikarimloo, Jason P. Sheehan
Neurosurgical Review.2025;[Epub] CrossRef - Cerebellar medullary cistern hemangioblastoma
Dahai Cao, Qiang Zhang
Asian Journal of Surgery.2025; 48(9): 5843. CrossRef - Navigating rare vascular brain tumors: A retrospective observational study
Sana Ahuja, Dipanker S Mankotia, Naveen Kumar, Vyomika Teckchandani, Sufian Zaheer
Cancer Research, Statistics, and Treatment.2025; 8(2): 92. CrossRef - A potential new entity pending further validation of pulmonary primary interstitial Tumor: Lymphangioleiomyomatosis-like
Lingyu Zhao, Xiaochen Shen, Yun Niu, Huang Chen, Dingrong Zhong
Respiratory Medicine Case Reports.2025; 57: 102241. CrossRef - Renal cell carcinoma with fibromyomatous stroma (RCC FMS) and with hemangioblastoma‐like areas is part of the RCC FMS spectrum in patients with tuberous sclerosis complex
Katherina Baranova, Jacob A Houpt, Deaglan Arnold, Andrew A House, Laura Lockau, Lindsay Ninivirta, Stephen Pautler, Haiying Chen, Madeleine Moussa, Rola Saleeb, Jose A Gomez, Asli Yilmaz, Farshid Siadat, Adrian Box, Douglas J Mahoney, Franz J Zemp, Manal
Histopathology.2025; 87(5): 687. CrossRef - Renal hemangioblastoma and renal cell carcinoma with fibromyomatous stroma and hemangioblastoma-like areas belong to the spectrum of one entity
Kiril Trpkov, Norel Salut, Inmaculada Ribera-Cortada, Elías Tasso Xipell, Isabel Trias Puigsureda, Asli Yilmaz, Arjumand Riyaz Husain, Erik Nohr, Adrian Box, Farshid Siadat, Katherina Baranova, Rola M. Saleeb, Robert Stoehr, Arndt Hartmann, Abbas Agaimy
Virchows Archiv.2025;[Epub] CrossRef - Primary hemangioblastoma of rectum: a rare case report and review of literature
Aiping Zheng, Shaojuan Zhang, Qiang Ma, Wenxu Yang, Hualiang Xiao, Xinyu Liang
Journal of Cancer Research and Clinical Oncology.2025;[Epub] CrossRef - Cerebellar Hemangioblastoma Resection Complicated by Postoperative Vasogenic Edema in the Setting of Concurrent Immunotherapy Treatment
Aashka Sheth, Nicholas Dietz, Andrea Becerril-Gaitan, Rahim Kasem, Akshitkumar Mistry, Brian J Williams, Dale Ding, Isaac Abecassis
Cureus.2025;[Epub] CrossRef - Familial Von Hippel–Lindau Disease: A Case Series of Cerebral Hemangioblastomas with MRI, Histopathological, and Genetic Correlations
Claudiu Matei, Ioana Boeras, Dan Orga Dumitriu, Cosmin Mutu, Adriana Popescu, Mihai Gabriel Cucu, Alexandru Calotă-Dobrescu, Bogdan Fetica, Diter Atasie
Life.2025; 15(11): 1649. CrossRef - Characterization of spinal hemangioblastomas in patients with and without von Hippel-Lindau, and YAP expression
Ana-Laura Calderón-Garcidueñas, Steven-Andrés Piña-Ballantyne, Eunice-Jazmín Espinosa-Aguilar, Rebeca de Jesús Ramos-Sánchez
Revista Española de Patología.2024; 57(3): 160. CrossRef - Patients With Hemangioblastoma: Mood Disorders and Sleep Quality
Ali Riazi, Yaser Emaeillou, Nima Najafi, Mohammad Hoseinimanesh, Mohammad Ibrahim Ashkaran, Donya Sheibani Tehrani
Brain Tumor Research and Treatment.2024; 12(2): 87. CrossRef - Radiosurgically Treated Recurrent Cerebellar Hemangioblastoma: A Case Report and Literature Review
François Fabi, Ève Chamberland, Myreille D’Astous, Karine Michaud, Martin Côté, Isabelle Thibault
Current Oncology.2024; 31(7): 3968. CrossRef - Dual manifestations: spinal and cerebellar hemangioblastomas indicative of von Hippel-Lindau syndrome
Nurhuda Hendra Setyawan, Rachmat Andi Hartanto, Rusdy Ghazali Malueka, Ery Kus Dwianingsih, Dito Pondra Dharma
Radiology Case Reports.2024; 19(11): 5000. CrossRef - Phenotypic and Genotypic Features of a Chinese Cohort with Retinal Hemangioblastoma
Liqin Gao, Feng Zhang, J. Fielding Hejtmancik, Xiaodong Jiao, Liyun Jia, Xiaoyan Peng, Kai Ma, Qian Li
Genes.2024; 15(9): 1192. CrossRef - Case report: Hemangioblastoma in the brainstem of a dog
Kirsten Landsgaard, Samantha St. Jean, Stephanie Lovell, Jonathan Levine, Christine Gremillion, Brian Summers, Raquel R. Rech
Frontiers in Veterinary Science.2023;[Epub] CrossRef - Intramedullary hemangioblastoma of the thoracic cord with a microsurgical approach: A case report and literature review
Eduardo Cattapan Piovesan, Werner Petry Silva, Adroaldo Baseggio Mallmann, Felipe Severo Lanzini, Bruna Zanatta de Freitas, Francisco Costa Beber Lemanski, Charles André Carazzo
Surgical Neurology International.2023; 14: 137. CrossRef - Secondary Holocord Syringomyelia Associated With Spinal Hemangioblastoma in a 29-Year-Old Female
Eric Chun-Pu Chu, Edouard Sabourdy, Benjamin Cheong
Cureus.2023;[Epub] CrossRef - Belzutifan in adults with VHL-associated central nervous system hemangioblastoma: a single-center experience
Bryan J. Neth, Mason J. Webb, Jessica White, Joon H. Uhm, Pavel N. Pichurin, Ugur Sener
Journal of Neuro-Oncology.2023; 164(1): 239. CrossRef - Resection of Intramedullary Hemangioblastoma: Timing of Surgery and Its Impact on Neurological Outcome and Quality of Life
Michael Schwake, Sarah Ricchizzi, Sophia Krahwinkel, Emanuele Maragno, Stephanie Schipmann, Walter Stummer, Marco Gallus, Markus Holling
Medicina.2023; 59(9): 1611. CrossRef
- Immunohistochemical Expression of PAX8 in Central Nervous System Hemangioblastomas: A Potential Diagnostic Pitfall for Neuropathologists
Original Article
- Expression of specific microRNAs in tissue and plasma in colorectal cancer
- Allan Fellizar, Vivencio Refuerzo, John Donnie Ramos, Pia Marie Albano
- J Pathol Transl Med. 2023;57(3):147-157. Published online May 3, 2022
- DOI: https://doi.org/10.4132/jptm.2022.02.19
- 11,306 View
- 602 Download
- 18 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
MicroRNAs (miRNA/miR) play significant roles in the regulation of cell differentiation, cell cycle progression, and apoptosis. They become dysregulated during carcinogenesis and are eventually released into the circulation, enabling their detection in body fluids. Thus, this study compared the miRNA expression in tissue and plasma samples of colorectal cancer (CRC) patients and clinically healthy controls and determined miRNA expression as a potential CRC biomarker.
Methods
Using quantitative reverse transcription polymerase chain reaction (RT-qPCR), miR-21-5p, miR-29a-3p, miR-92a-3p, miR-135b-5p, miR-196b-5p, and miR-197-3p, expression was analyzed and compared between the malignant (n = 41) and the adjacent neoplasm free mucosal tissues (n = 41) of CRC patients. The findings were validated in plasma samples (n = 36) collected from the same CRC patients prior to surgery or any form of treatment and compared to plasma from their age and sex-matched controls (n = 36).
Results
MiR-21-5p, miR-29a-3p, miR-92a-3p, and miR- 196b-5p were upregulated and miR-135b-5p was downregulated in CRC malignant tissues compared to their expression in adjacent neoplasm-free tissue. This was further observed in the plasma of the same CRC cases compared to controls. MiR-92a-3p showed itself the most sensitive (0.93; p < .001) and most specific (0.95; p < .001) in detecting CRC in tissue. In plasma, miR-196b-5p was the most sensitive (0.97; p < .001) and specific (0.94; p < .001) in detecting CRC. Plasma miR-92a-3p and miR-196b-5p were the most sensitive (0.95; p < .001) and specific (0.94; p < .001) in the early detection of CRC.
Conclusions
Results show that specific miRNAs dysregulated in malignant tissues are released and can be detected in the circulation, supporting their potential as non-invasive biomarkers of CRC. -
Citations
Citations to this article as recorded by- Liquid biopsy for the management of gastrointestinal cancers
Zeinab Salehnia, Delsuz Rezaee, Sajad Ehtiati, Mohammad Bakhtiari, Mohammad Amin Khalilzad, Sajad Najafi
Clinica Chimica Acta.2026; 578: 120474. CrossRef - Differential Circulating miRNA Responses to PM Exposure in Healthy and Diabetes Mellitus Patients: Implications for Lung Cancer Susceptibility
Moe Thi Thi Han, Nichakorn Satitpornbunpot, Naoomi Tominaga, Saranta Freeouf, Khanittha Punturee, Chidchamai Kewchareonwong, Busayamas Chewaskulyong, Ganjana Lertmemongkolchai, Ratchada Cressey
International Journal of Molecular Sciences.2026; 27(2): 613. CrossRef - Unlocking the power of non-coding RNAs: toward real-time cancer monitoring in precision oncology
Manon Chang, Thomas Papazyan, Elvire Pons-Tostivint, Delphine Fradin
Molecular Cancer.2026;[Epub] CrossRef - Except for Robust Outliers, Rapamycin Increases Lesion Burden in a Murine Model of Cerebral Cavernous Malformations
Roberto J. Alcazar-Felix, Robert Shenkar, Christian R. Benavides, Akash Bindal, Abhinav Srinath, Ying Li, Serena Kinkade, Tatiana Terranova, Evon DeBose-Scarlett, Rhonda Lightle, Dorothy DeBiasse, Hanadi Almazroue, Diana Vera Cruz, Sharbel Romanos, Aditya
Translational Stroke Research.2025; 16(3): 859. CrossRef - miR-135b: A key role in cancer biology and therapeutic targets
Yingchun Shao, Shuangshuang Zhang, Yuxin Pan, Zhan Peng, Yinying Dong
Non-coding RNA Research.2025; 12: 67. CrossRef - The role of tumor-associated fibroblast-derived exosomes in chemotherapy resistance of colorectal cancer and its application prospect
Meichen Liu, Teng-zheng Li, Congcong Xu
Biochimica et Biophysica Acta (BBA) - General Subjects.2025; 1869(6): 130796. CrossRef - A Systematic Review of MicroRNAs in Hemorrhagic Neurovascular Disease: Cerebral Cavernous Malformations as a Paradigm
Roberto J. Alcazar-Felix, Aditya Jhaveri, Javed Iqbal, Abhinav Srinath, Carolyn Bennett, Akash Bindal, Diana Vera Cruz, Sharbel Romanos, Stephanie Hage, Agnieszka Stadnik, Justine Lee, Rhonda Lightle, Robert Shenkar, Janne Koskimäki, Sean P. Polster, Romu
International Journal of Molecular Sciences.2025; 26(8): 3794. CrossRef - microRNA-196b-5p expression in cancer tissues is closely associated with clinical and pathological characteristics and prognosis of patients with non-small cell lung cancer
Wei Liu, Xiaomin Lu, Changgang Yang, Fengjun Ji, Xiaodan Wu
Journal of Cardiothoracic Surgery.2025;[Epub] CrossRef - Association of mir196a2 and mir146a polymorphisms and colorectal cancer risk: A meta-analysis
Zahraa isam jameel, Hanan Ali Kareem, Zahraa Mohammed Yahya, Ahmed Ali Hussein, zahraa abdel Kareem
Human Gene.2025; 45: 201448. CrossRef - Micro RNA in Colorectal Cancer—Potential Diagnostic and Prognostic Markers—An Updated Review
Weronika Pająk, Jakub Kleinrok, Joanna Pec, Karolina Michno, Jan Wojtas, Miłosz Badach, Barbara Teresińska, Jacek Baj
International Journal of Molecular Sciences.2025; 26(17): 8615. CrossRef - MicroRNAs in colorectal cancer: A comparative analysis of circulating and tissue microRNA levels
Iulia Andreea Pelisenco, Bogdan Trandafir, Anastasia-Maria Dobre, Andrei-Daniel Dragne, Vlad Herlea, Andrei Marian Niculae, Catalin Vasilescu, Mihail Eugen Hinescu, Elena Milanesi, Maria Dobre
World Journal of Gastrointestinal Oncology.2025;[Epub] CrossRef - Identification of miRNAs Present in Cell- and Plasma-Derived Extracellular Vesicles—Possible Biomarkers of Colorectal Cancer
Marzena Lenart, Izabela Siemińska, Rafał Szatanek, Anna Mordel, Antoni Szczepanik, Mateusz Rubinkiewicz, Maciej Siedlar, Monika Baj-Krzyworzeka
Cancers.2024; 16(13): 2464. CrossRef - The emerging role of blood-based biomarkers in early detection of colorectal cancer: A systematic review
Faris Shweikeh, Yuhao Zeng, Abdur Rahman Jabir, Erica Whittenberger, Saurav P. Kadatane, Yuting Huang, Mohamad Mouchli, Dani Ran Castillo
Cancer Treatment and Research Communications.2024; 42: 100872. CrossRef - The Role of Extracellular Vesicles in Colorectal Cancer
Yujian Xia, Chaoran Yu, Ernest Johann Helwig, Yousheng Li
Technology in Cancer Research & Treatment.2023;[Epub] CrossRef - HNRNPA2B1-Mediated MicroRNA-92a Upregulation and Section Acts as a Promising Noninvasive Diagnostic Biomarker in Colorectal Cancer
Yiling Li, Kexin Li, Xiaoying Lou, Yue Wu, Samuel Seery, Danfei Xu, Yuqing Pei, Benheng Qian, Yuxin Wu, Shuang Liang, Kui Wu, Wei Cui
Cancers.2023; 15(4): 1367. CrossRef - Role of salivary miRNAs in the diagnosis of gastrointestinal disorders: a mini-review of available evidence
Maria Oana Săsăran, Claudia Bănescu
Frontiers in Genetics.2023;[Epub] CrossRef - Exploring the Role of Circulating Cell-Free RNA in the Development of Colorectal Cancer
Chau-Ming Kan, Xiao Meng Pei, Martin Ho Yin Yeung, Nana Jin, Simon Siu Man Ng, Hin Fung Tsang, William Chi Shing Cho, Aldrin Kay-Yuen Yim, Allen Chi-Shing Yu, Sze Chuen Cesar Wong
International Journal of Molecular Sciences.2023; 24(13): 11026. CrossRef - Lynch Syndrome Biopathology and Treatment: The Potential Role of microRNAs in Clinical Practice
Serena Ascrizzi, Grazia Maria Arillotta, Katia Grillone, Giulio Caridà, Stefania Signorelli, Asad Ali, Caterina Romeo, Pierfrancesco Tassone, Pierosandro Tagliaferri
Cancers.2023; 15(15): 3930. CrossRef
- Liquid biopsy for the management of gastrointestinal cancers
Case Study
- Colorectal adenocarcinoma with enteroblastic differentiation: diagnostic challenges of a rare case encountered in clinical practice
- Evi Abada, Ifeoma C. Anaya, Othuke Abada, Anthony Lebbos, Rafic Beydoun
- J Pathol Transl Med. 2022;56(2):97-102. Published online January 21, 2022
- DOI: https://doi.org/10.4132/jptm.2021.10.28
- 8,189 View
- 207 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Colorectal adenocarcinoma with enteroblastic differentiation (CAED) is a rare subtype of colonic adenocarcinoma characterized by increased α-fetoprotein (AFP) production and the expression of at least one enteroblastic marker including AFP, glypican 3 (GPC3), or Spalt like transcription factor 4 (SALL4). We report a case of a 26-year-old female who presented with low back pain and constipation which persisted despite supportive measures. Imaging revealed multiple liver lesions and enlarged retroperitoneal nodes. Tumor markers including AFP were markedly elevated. On biopsy, samples from the liver revealed infiltrating glands lined by columnar-type epithelium with mostly eosinophilic granular to focally clear cytoplasm. By immunohistochemistry, the tumor showed immunoreactivity with AFP, hepatocyte antigen, GPC3, SALL4, CDX2, SATB2, and cytokeratin 20. A colonoscopy performed subsequently revealed a mass in the sigmoid colon and biopsy of this mass revealed a similar histology as that seen in the liver. A diagnosis of CAED was made, following the results of gene expression profiling by the tumor with next-generation sequencing which identified pathogenic variants in MUTYH, TP53, and KDM6A genes and therefore supported its colonic origin. Cases such as this underscores the use of ancillary diagnostic techniques in arriving at the correct diagnosis in lesions with overlapping clinicopathologic characteristics.
-
Citations
Citations to this article as recorded by- Colorectal Adenocarcinoma with Enteroblastic Differentiation: A Report of Two Cases
Yusuke Nakamura, Hiroyuki Fukuda, Yasuo Ishida
Nihon Daicho Komonbyo Gakkai Zasshi.2026; 79(2): 82. CrossRef - Raised alpha fetoprotein in cirrhotic liver with colorectal liver metastasis mimicking hepatocellular carcinoma: case report and review of literature
Aboje Adugba, Dominic Obotu Ayegba, Mansour Al Moundhri, Kareem Al Rezk, Rawan AlMallah, Ramesh Babu Telugu, Abdallah Al Farai
Diagnosis.2026;[Epub] CrossRef - Exploring the Multifunctional Role of Alpha-Fetoprotein in Cancer Progression: Implications for Targeted Therapy in Hepatocellular Carcinoma and Beyond
Hyunjung Kim, Minji Jang, Eunmi Kim
International Journal of Molecular Sciences.2025; 26(10): 4863. CrossRef - Rectal adenocarcinoma with a yolk sac tumor component: A rare case report and review of the literature
Sato Nishida, Tomohiro Takeda, Tatsuya Shonaka, Shoichiro Mizukami, Masahide Otani, Mizuho Ohara, Chikayoshi Tani, Kimiharu Hasegawa, Yuki Kamikokura, Mishie Tanino, Hideki Yokoo
International Cancer Conference Journal.2025; 15(1): 138. CrossRef - SALL4 in gastrointestinal tract cancers: upstream and downstream regulatory mechanisms
Tairan Wang, Yan Jin, Mengyao Wang, Boya Chen, Jinyu Sun, Jiaying Zhang, Hui Yang, Xinyao Deng, Xingyue Cao, Lidong Wang, Yuanyuan Tang
Molecular Medicine.2024;[Epub] CrossRef - Gastric adenocarcinoma with enteroblastic differentiation in a
67-year-old man in Korea: a case report
Hae Rin Lee, Gwang Ha Kim, Dong Chan Joo, Moon Won Lee, Bong Eun Lee, Kyung Bin Kim
The Ewha Medical Journal.2024;[Epub] CrossRef - Colorectal adenocarcinoma with clear cell changes: immunohistological and molecular findings in three cases
Andreas Gocht, Carsten Heidel, Jutta Kirfel, Rita Vesce, Pamela Lazar-Karsten, Helen Pasternack, Madelaine Melzer, Phillip Hildebrand, Nicole Warkentin, Hendrik Schimmelpenning, Verena-Wilbeth Sailer
Virchows Archiv.2024; 485(3): 569. CrossRef - Ureteral Metastasis of Colonic Adenocarcinoma with Enteroblastic Differentiation: A Rare Case to be Distinguished from Clear Cell Adenocarcinoma of the Urinary Tract
Hiroshi Minato, Akane Yoshikawa, Sho Tsuyama, Kazuyoshi Katayanagi, Kengo Hayashi, Yusuke Sakimura, Hiroyuki Bando, Tomohiro Hori, Yosuke Kito
International Journal of Surgical Pathology.2023; 31(8): 1553. CrossRef - Beyond liver cancer, more application scenarios for alpha-fetoprotein in clinical practice
Chenyu Ma, Yuexinzi Jin, Yuhan Wang, Huaguo Xu, Jiexin Zhang
Frontiers in Oncology.2023;[Epub] CrossRef - AIEgens assisted label free DNA supersandwich immunoassay for ultrasensitive α-fetoprotein detection
Xiaowen Ou, Jingman Dai, Yiting Huang, Xiaoqin Xiong, Zhi Zheng, Xiaoding Lou, Fan Xia
Giant.2022; 11: 100110. CrossRef - Rectal carcinoma with dual differentiation toward enteroblastic and neuroendocrine features arising in a patient with ulcerative colitis: a case report
Takako Kihara, Ryuichi Kuwahara, Kurando Kusunoki, Tomohiro Minagawa, Yuki Horio, Motoi Uchino, Hiroki Ikeuchi, Seiichi Hirota
World Journal of Surgical Oncology.2022;[Epub] CrossRef
- Colorectal Adenocarcinoma with Enteroblastic Differentiation: A Report of Two Cases
Original Articles
- Fatty acid synthetase expression in triple-negative breast cancer
- Jin Hee Park, Hye Seung Han, So Dug Lim, Wook Youn Kim, Kyoung Sik Park, Young Bum Yoo, Seung Eun Lee, Wan-Seop Kim
- J Pathol Transl Med. 2022;56(2):73-80. Published online January 21, 2022
- DOI: https://doi.org/10.4132/jptm.2021.10.27
- 7,553 View
- 204 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Triple-negative breast cancer (TNBC) has a relatively poor prognosis. Research has identified potential metabolic targets, including fatty acid metabolism, in TNBC. The absence of effective target therapies for TNBC led to exploration of the role of fatty acid synthetase (FASN) as a potential target for TNBC therapy. Here, we analyzed the expression of FASN, a representative lipid metabolism–related protein, and investigated the association between FASN expression and Ki-67 and the programmed death ligand 1 (PD-L1) biomarkers in TNBC.
Methods
Immunohistochemical expression of FASN was analyzed in 166 patients with TNBC. For analytical purposes, patients with 0–1+ FASN staining were grouped as low-grade FASN and patients with 2–3+ FASN staining as high-grade FASN.
Results
FASN expression was observed in 47.1% of TNBC patients. Low and high expression of FASN was identified in 75.9% and 24.1%, respectively, and no statistically significant difference was found in T category, N category, American Joint Committee on Cancer stage, or recurrence rate between the low and high-FASN expression groups. Ki-67 proliferation level was significantly different between the low and high-FASN expression groups. FASN expression was significantly related to Ki-67 as the level increased. There was no significant difference in PD-L1 positivity between the low- and high-FASN expression groups.
Conclusions
We identified FASN expression in 166 TNBC patients. The Ki-67 proliferation index was positively correlated with FASN level, indicating higher proliferation activity as FASN increases. However, there was no statistical association with PD-L1 SP142, the currently FDA-approved assay, or FASN expression level. -
Citations
Citations to this article as recorded by- FASN at the crossroads of tumor metabolism, immune evasion, and therapy resistance: Mechanistic insights and therapeutic opportunities
Xuefeng Jiang, Guotao Fang, Wen Li, Yusheng Liu, Gang Chen, Silvio E. Perea, Yasser Perera, Rong Ma, Xiaofei Hu, Xinan Long
Critical Reviews in Oncology/Hematology.2026; 220: 105155. CrossRef - Lipid metabolism involved in progression and drug resistance of breast cancer
Wenxiang Fu, Aijun Sun, Huijuan Dai
Genes & Diseases.2025; 12(4): 101376. CrossRef - Unveiling the impact of lipid metabolism on triple-negative breast cancer growth and treatment options
Xin-xian Cai, Zhe-zhong Zhang, Xiao-xiao Yang, Wen-rui Shen, Liu-wei Yuan, Xi Ding, Ying Yu, Wen-yu Cai
Frontiers in Oncology.2025;[Epub] CrossRef - Protein biomarkers for diagnosis of breast cancer
Emeka Eze Joshua Iweala, Doris Nnenna Amuji, Faith Chinasaokwu Nnaji
Scientific African.2024; 25: e02308. CrossRef - Microarray analysis points to LMNB1 and JUN as potential target genes for predicting metastasis promotion by etoposide in colorectal cancer
Jiafei Liu, Hongjie Yang, Peng Li, Yuanda Zhou, Zhichun Zhang, Qingsheng Zeng, Xipeng Zhang, Yi Sun
Scientific Reports.2024;[Epub] CrossRef - The signature of extracellular vesicles in hypoxic breast cancer and their therapeutic engineering
Baiheng Zhu, Kehao Xiang, Tanghua Li, Xin Li, Fujun Shi
Cell Communication and Signaling.2024;[Epub] CrossRef - NFYA promotes malignant behavior of triple-negative breast cancer in mice through the regulation of lipid metabolism
Nobuhiro Okada, Chihiro Ueki, Masahiro Shimazaki, Goki Tsujimoto, Susumu Kohno, Hayato Muranaka, Kiyotsugu Yoshikawa, Chiaki Takahashi
Communications Biology.2023;[Epub] CrossRef - Role of EGFR and FASN in breast cancer progression
Suchi Chaturvedi, Mainak Biswas, Sushabhan Sadhukhan, Avinash Sonawane
Journal of Cell Communication and Signaling.2023; 17(4): 1249. CrossRef - Bioinformatics Method Was Used to Analyze the Highly Expressed Gene FAM83A of Breast Cancer in Young Women
Yongzhe Tang, Hao Wang, Qi He, Yuanyuan Chen, Jie Wang, Fahd Abd Algalil
Applied Bionics and Biomechanics.2022; 2022: 1. CrossRef - NCAPH promotes proliferation as well as motility of breast cancer cells by activating the PI3K/AKT pathway
Ting Zhang, Peng Li, Wanying Guo, Qipeng Liu, Weiqiang Qiao, Miao Deng
Physiology International.2022;[Epub] CrossRef
- FASN at the crossroads of tumor metabolism, immune evasion, and therapy resistance: Mechanistic insights and therapeutic opportunities
- Extremely well-differentiated adenocarcinoma of the stomach: diagnostic pitfalls in endoscopic biopsy
- Jongwon Lee, In-Seob Lee, Ji Yong Ahn, Young Soo Park, Jihun Kim
- J Pathol Transl Med. 2022;56(2):63-72. Published online November 16, 2021
- DOI: https://doi.org/10.4132/jptm.2021.10.12
- 8,477 View
- 470 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Extremely well-differentiated adenocarcinoma (EWDA) is a deceptively bland-looking adenocarcinoma of the stomach. It often causes diagnostic problems, especially in endoscopic biopsy samples. To better recognize this deceptively bland lesion, we carefully reviewed a series of EWDAs treated at our institution.
Methods
A total of 55 specimens from 19 patients were obtained. Endoscopic, gross and microscopic features defining EWDA were described and documented. For comparison, hyperplastic polyp specimens were randomly selected and analyzed.
Results
Most cases (18 of 19, 94.7%) were advanced gastric cancer (AGC) and primarily located in the body of the stomach (15 of 19, 79.0%). The majority of AGCs were non-ulcerated (11 of 18, 61.1%) with an undermining growth pattern and a relatively small mucosal involvement. Specific histologic features included an irregular glandular shape, an undulating apical cytoplasmic border, disproportionately large glands, a variably distended mucinous cytoplasm. Classical features, such as small infiltrating glands or desmoplastic reactions, were barely observed. Identification of irregularly spaced nuclei and disruption of the foveolar epithelial structure, along with atypical features described above were helpful in making a diagnosis especially in gastric forceps biopsies.
Conclusions
Awareness of the histomorphologic characteristics described in this report would lead to timely diagnosis and prevent repeated endoscopic procedures. -
Citations
Citations to this article as recorded by- Artificial intelligence-assisted diagnosis of early gastric cancer: present practice and future prospects
Changda Lei, Wenqiang Sun, Kun Wang, Ruixia Weng, Xiuji Kan, Rui Li
Annals of Medicine.2025;[Epub] CrossRef - Unusual or Uncommon Histology of Gastric Cancer
Jinho Shin, Young Soo Park
Journal of Gastric Cancer.2024; 24(1): 69. CrossRef - A case of gastric adenocarcinoma with pyloric gland-type infiltrating submucosa
Kaiho Hirata, Shusuke Yagi, Hideki Miyazaki, Kazuhiko Yamada, Naoki Akazawa, Naoki Enomoto, Kyoko Nohara, Chizu Yokoi, Toru Igari, Norihiro Kokudo
Surgical Case Reports.2024;[Epub] CrossRef - Gastric-type extremely well-differentiated adenocarcinoma of the stomach: A rare tumor with diagnostic difficulties and high inter-observer variation in endoscopic pinch biopsies
Soomin Ahn, Sujin Park, Hyun Hee Koh, Han Gyeol Kim, Hyunjin Kim, Jae Yeong Son, Boram Lee, Hyunwoo Lee, Soohyun Hwang, Junhun Cho, Yun Kyung Lee, Ryoji Kushima, Amitabh Srivastava, Kyoung-Mee Kim
Pathology - Research and Practice.2024; 263: 155599. CrossRef
- Artificial intelligence-assisted diagnosis of early gastric cancer: present practice and future prospects
- Polo-like kinase 4 as a potential predictive biomarker of chemoradioresistance in locally advanced rectal cancer
- Hyunseung Oh, Soon Gu Kim, Sung Uk Bae, Sang Jun Byun, Shin Kim, Jae-Ho Lee, Ilseon Hwang, Sun Young Kwon, Hye Won Lee
- J Pathol Transl Med. 2022;56(1):40-47. Published online November 16, 2021
- DOI: https://doi.org/10.4132/jptm.2021.10.07
- 5,674 View
- 163 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Polo-like kinase 4 (PLK4) is a serine/threonine protein kinase located in the centriole of the chromosome during the cell cycle. PLK4 overexpression has been described in a variety of many common human epithelial tumors. Conversely, PLK4 acts as a haploinsufficient tumor suppressor in some situations, highlighting the importance of strict regulation of PLK4 expression, activity, and function. Meanwhile, the importance of chemoradiation resistance in rectal cancer is being emphasized more than ever. We aimed to analyze PLK4 expression and the tumor regression grade (TRG) in patients with rectal cancer, treated with chemoradiotherapy (CRT).
Methods
A retrospective study was conducted on 102 patients with rectal cancer who received preoperative CRT. Immunohistochemistry for PLK4 in paraffin-embedded tissue was performed from the biopsy and surgical specimens.
Results
We found significant association between high expression of PLK4 and poor response to neoadjuvant CRT (according to both Mandard and The Korean Society of Pathologists TRG systems) in the pre-CRT specimens. Other clinicopathologic parameters did not reveal any correlation with PLK4 expression.
Conclusions
This study revealed an association between high expression of PLK4 in the pre-CRT specimens and TRG. Our results indicated that PLK4 could potentially be a new predictor for CRT effect in patients with rectal cancer. -
Citations
Citations to this article as recorded by- Polo-like kinase 4 (PLK4) as a therapeutic target in breast cancer
Armen Parsyan, Harjot Athwal, Vasudeva Bhat, Alison L Allan
Carcinogenesis.2025;[Epub] CrossRef - Polo-like kinase 4: A molecular linchpin in cancer and its management
Durdana Muntaqua, Gagan Chhabra, Karla B. Anaya Aldrete, Nihal Ahmad
iScience.2025; 28(12): 114186. CrossRef
- Polo-like kinase 4 (PLK4) as a therapeutic target in breast cancer

 E-submission
E-submission
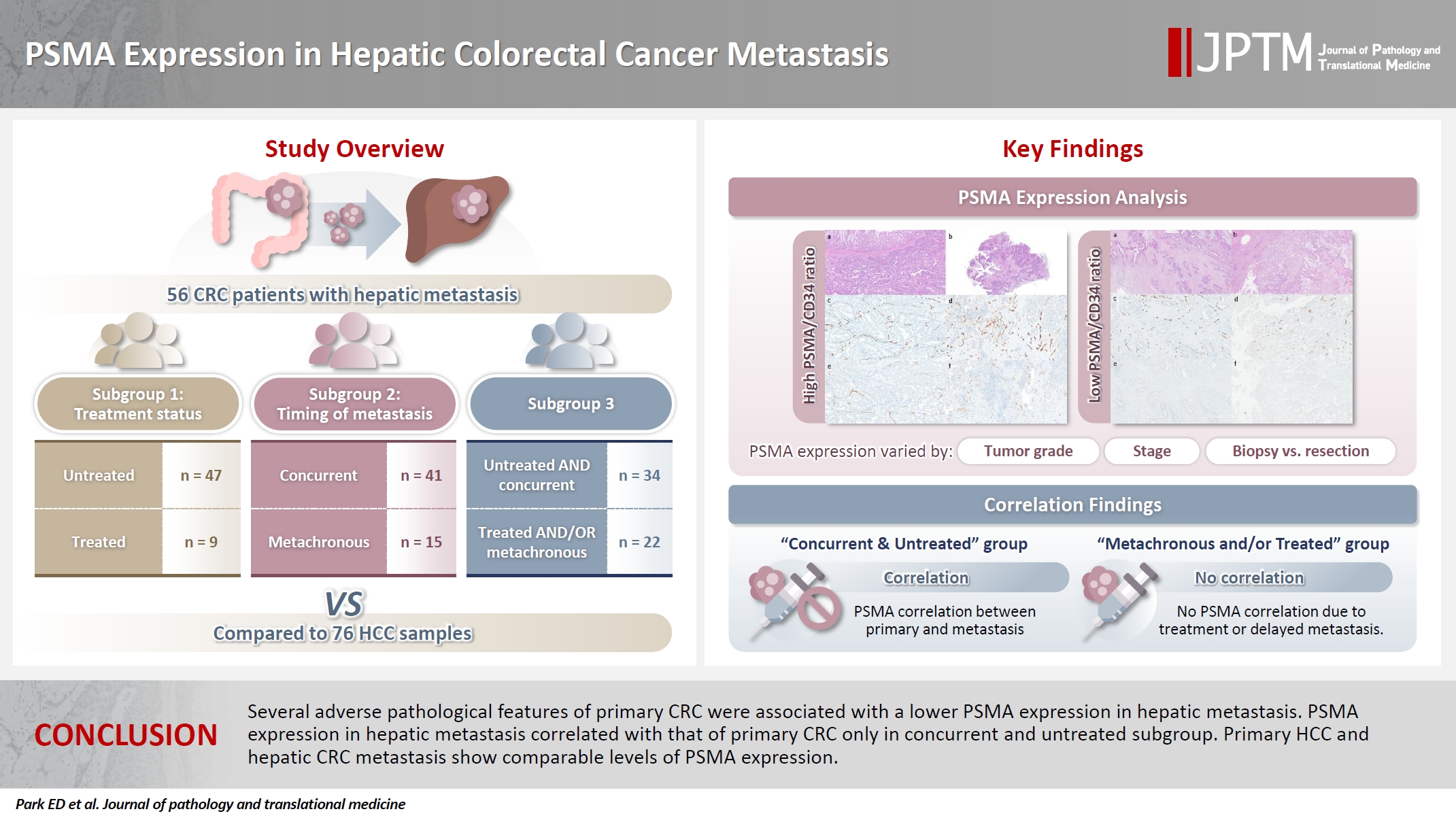
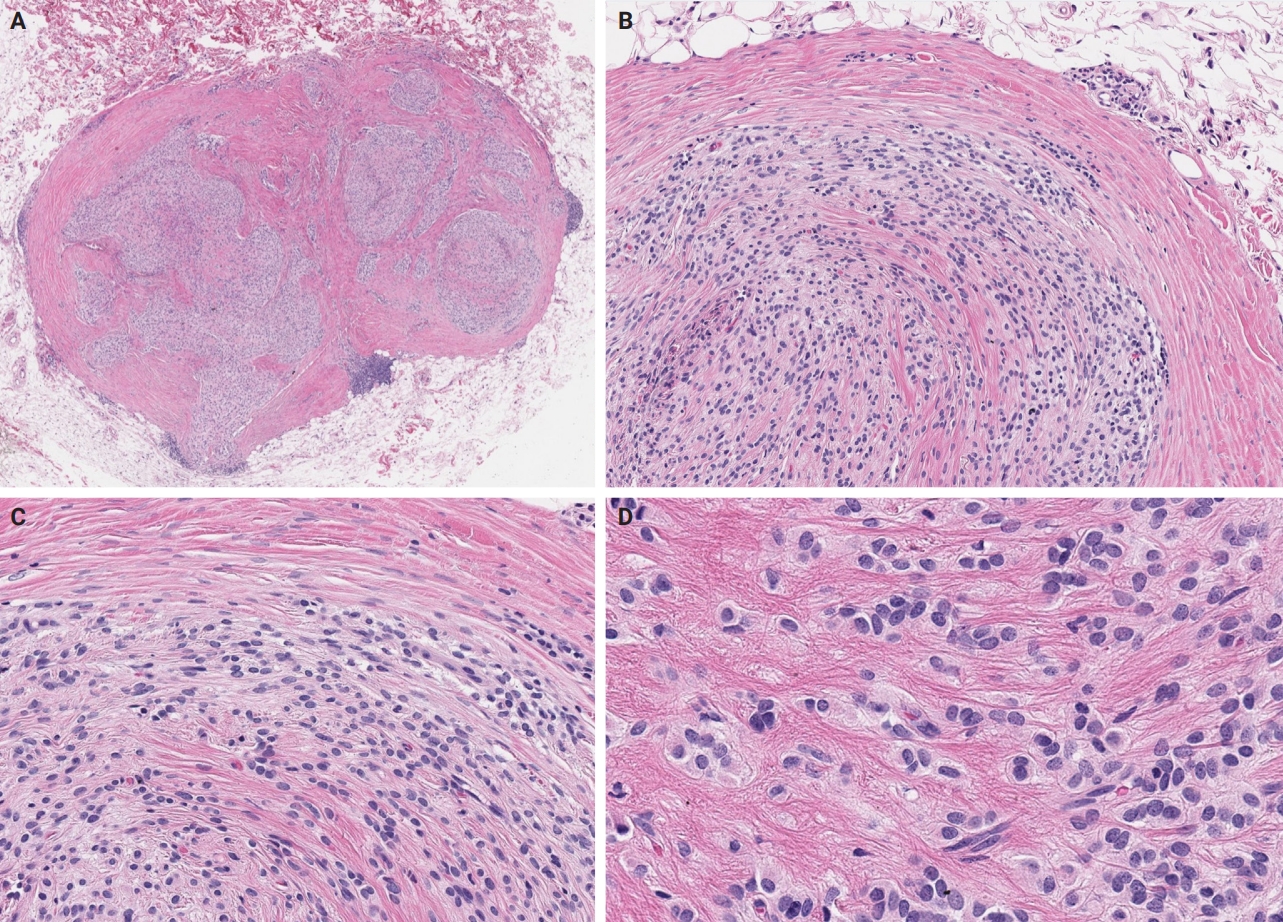
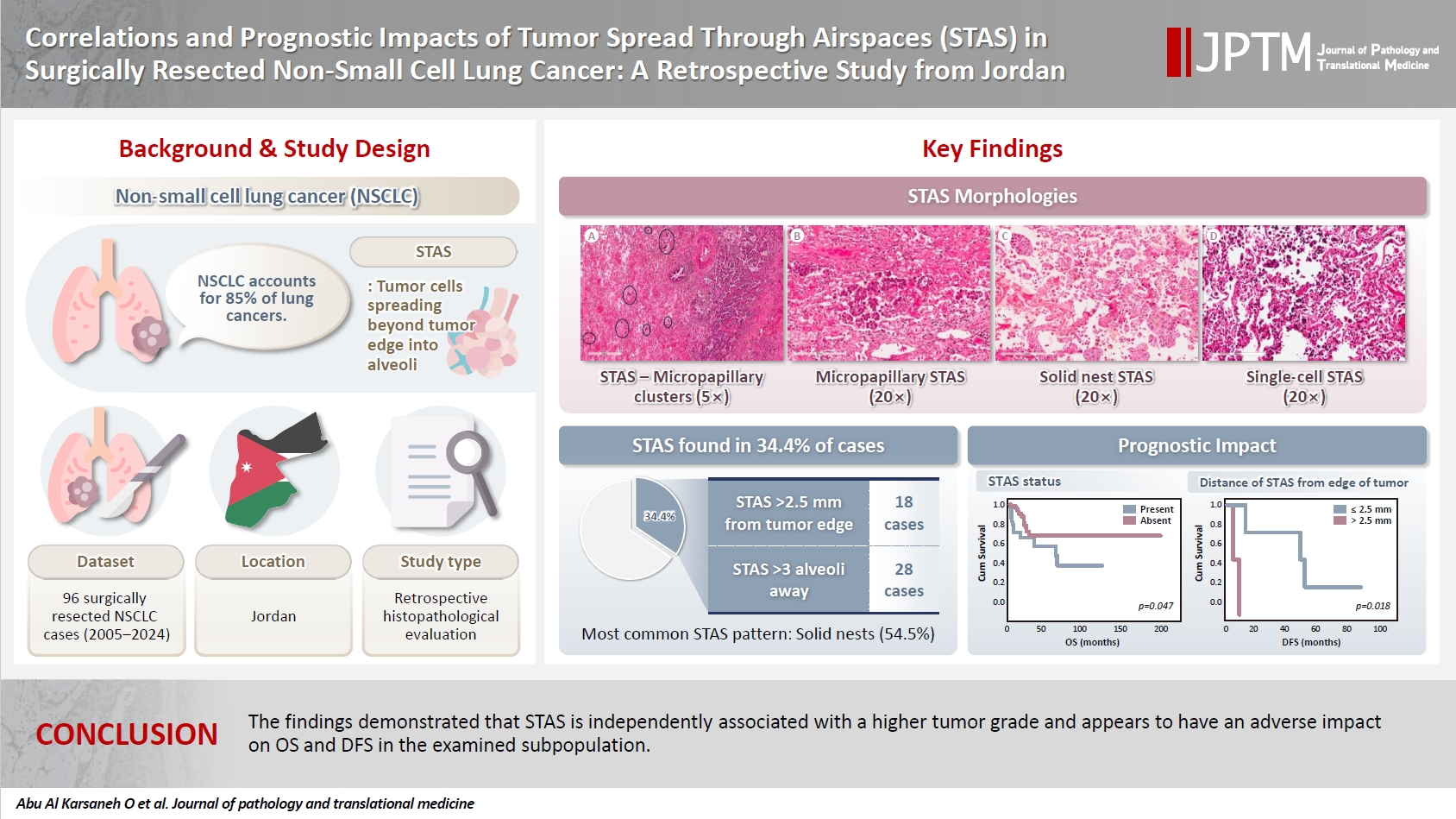


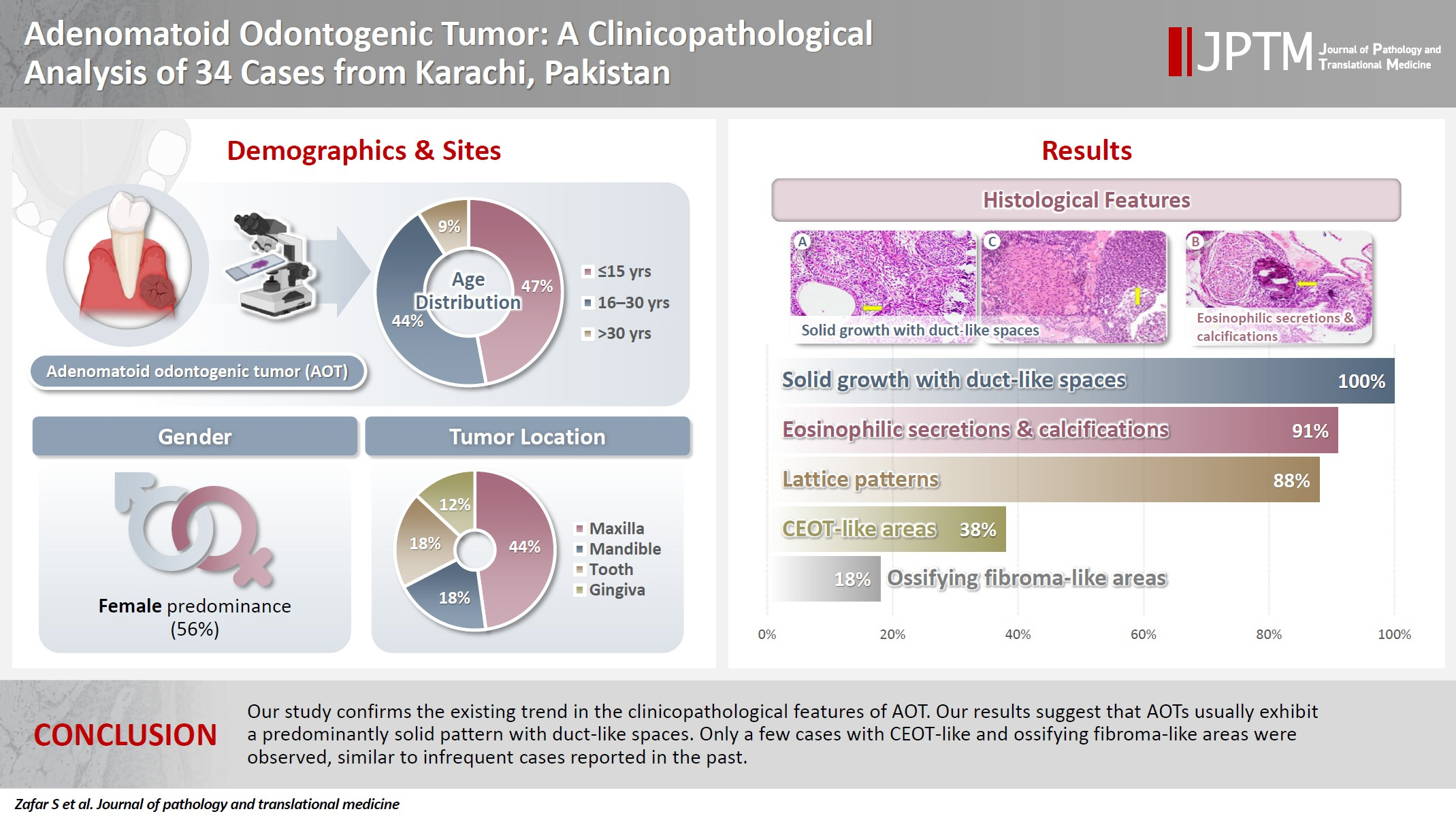
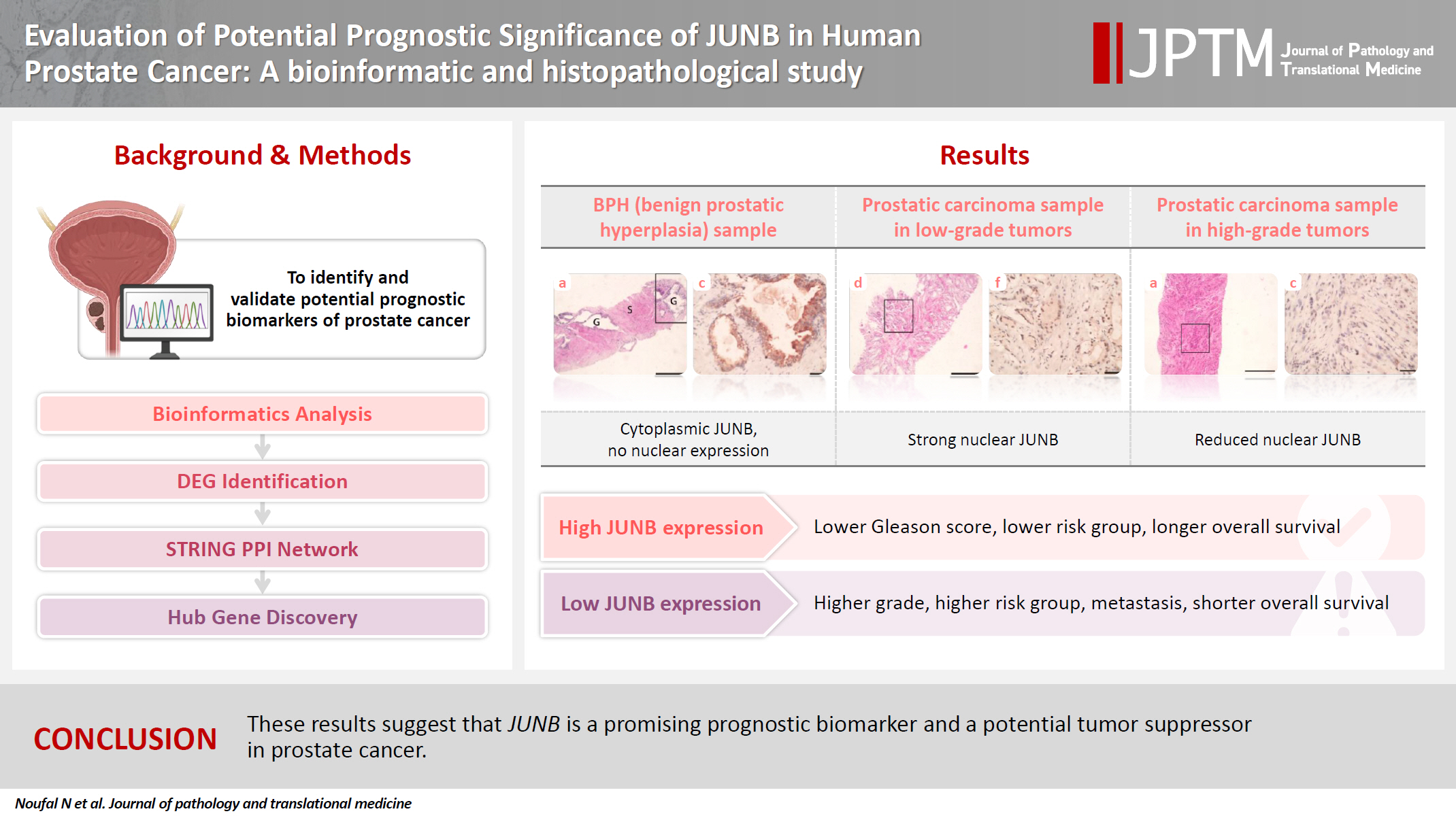

































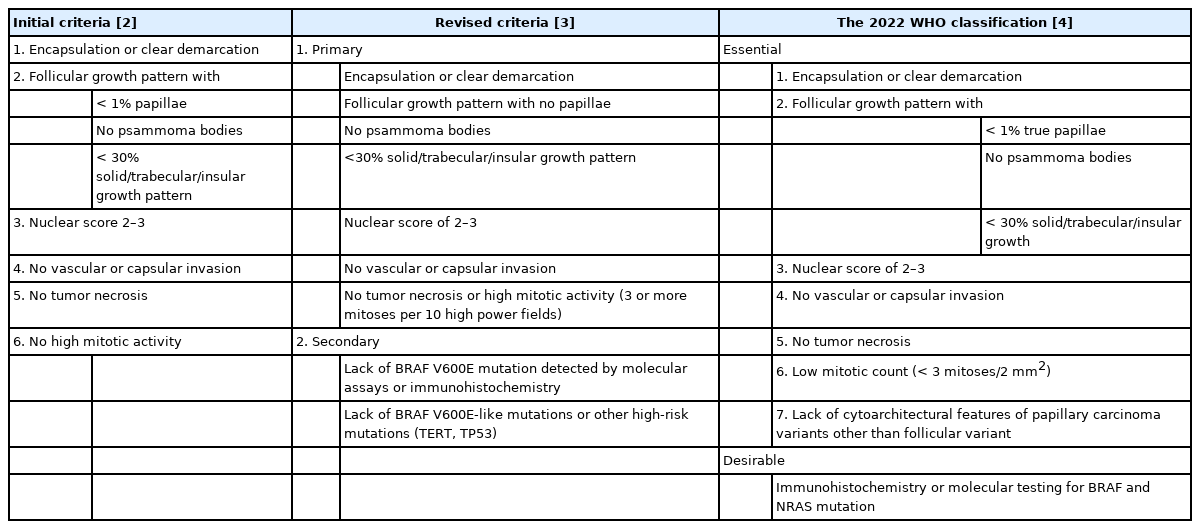

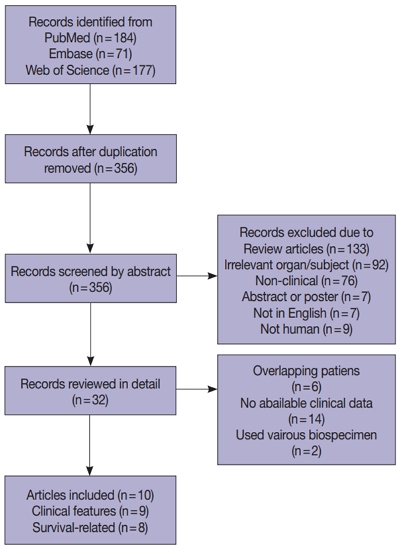
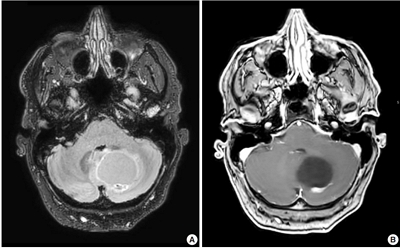





 First
First Prev
Prev



