Search
- Page Path
- HOME > Search
- Low Ki-67 labeling index is a clinically useful predictive factor for recurrence-free survival in patients with papillary thyroid carcinoma
- Takashi Masui, Katsunari Yane, Ichiro Ota, Kennichi Kakudo, Tomoko Wakasa, Satoru Koike, Hirotaka Kinugawa, Ryuji Yasumatsu, Tadashi Kitahara
- J Pathol Transl Med. 2025;59(2):115-124. Published online February 18, 2025
- DOI: https://doi.org/10.4132/jptm.2024.11.08
- 1,513 View
- 199 Download
-
 Abstract
Abstract
 PDF
PDF - Background
We report a new risk stratification of invasive stage papillary thyroid carcinomas (PTCs) by combining invasive status, using extrathyroid invasion (Ex) status, and tumor growth speed using the Ki-67 labeling index (LI). Methods: We examined tumor recurrence in 167 patients with PTC who were surgically treated at the Kindai University Nara Hospital between 2010 and 2022. The patients were classified according to the degree of invasion [negative (Ex0) or positive (Ex1, Ex2, and Ex3)] and tumor growth speed expressed with Ki-67 LI, as low (<5%) or high (>5%). This study confirmed previous findings that the disease-free survival (DFS) rate in PTCs significantly differed between patients with a high and low Ki-67 index. Results: When combining Ex status (negative or positive) and Ki-67 proliferation status (low or high), the DFS rate of invasion in the negative, low Ki-67 LI group was only 1.1%, while that of invasion in the positive, high Ki-67 LI was 44.1%. This study reports for the first time that recurrence risks can be stratified accurately when combining carcinoma’s essential two features of extrathyroid invasion status and tumor growth speed. Conclusions: We believe the evidence for low tumor recurrence risk may contribute to use of more conservative treatment options for invasive-stage PTCs and help alleviate patient anxiety about tumor recurrence and death.
- A clinicopathologic and immunohistochemical study of primary and secondary breast angiosarcoma
- Evi Abada, Hyejeong Jang, Seongho Kim, Rouba Ali-Fehmi, Sudeshna Bandyopadhyay
- J Pathol Transl Med. 2022;56(6):342-353. Published online October 27, 2022
- DOI: https://doi.org/10.4132/jptm.2022.08.31
- 4,164 View
- 142 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
We aimed to study the clinicopathologic and immunohistochemical (IHC) (CD117, c-Myc, and p53) characteristics, and overall survival of primary and secondary breast angiosarcoma (BAS).
Methods
This was a retrospective study of BAS cases diagnosed between 1997 and 2020 at our institution. Hematoxylin and eosin-stained slides were reviewed for tumor morphology, margin status, and lymph node metastasis. CD117, p53, D2-40, CD31, and c-Myc IHC stains were performed on 11 viable tissue blocks. Additional clinical information was obtained from the electronic medical records.
Results
Seventeen patients with BAS were identified. Of these, five (29%) were primary and 12 (71%) were secondary BAS, respectively. The median age at diagnosis for primary BAS was 36 years. The median age at diagnosis for secondary BAS was 67 years. The median time to secondary BAS development following radiotherapy was 6.5 years (range, 2 to 12 years). There was no significant difference between primary and secondary BAS in several histopathologic parameters examined, including histologic grade, necrosis, mitotic count, lymph node metastasis, and positive tumor margins. There was also no difference in CD117, p53, D2-40, CD31, and c-Myc expression by IHC between primary and secondary BAS. During a median followup of 21 months, primary BAS had two (40%) reported deaths and secondary BAS had three (25%) reported deaths. However, this difference in survival between both groups was not statistically significant (hazard ratio, 0.51; 95% confidence interval, 0.09 to 3.28; p = .450).
Conclusions
BAS is a rare and aggressive disease. No histologic, IHC (CD117, c-Myc, and p53), or survival differences were identified between primary and secondary BAS in this study. -
Citations
Citations to this article as recorded by- Etiology, pathogenesis, and management of angiosarcoma associated with implants and foreign body: Clinical cases and research updates
Ramy Samargandi
Medicine.2024; 103(18): e37932. CrossRef - Ovarian angiosarcoma: A systematic review of literature and survival analysis
Shafi Rehman, Arya Harikrishna, Amisha Silwal, B.R. Sumie, Safdar Mohamed, Nisha Kolhe, Meghana Maddi, Linh Huynh, Jesus Gutierrez, Yoshita Rao Annepu, Ameer Mustafa Farrukh
Annals of Diagnostic Pathology.2024; 73: 152331. CrossRef - Neoadjuvant chemotherapy for radiation associated angiosarcoma (RAAS) of the breast: A retrospective single center study
Stijn J.C. van der Burg, Sophie J.M. Reijers, Anke Kuijpers, Lotte Heimans, Astrid N. Scholten, Rick L.M. Haas, Hester van Boven, Willemijn M. Kolff, Marie-Jeanne T.F.D. Vrancken Peeters, Martijn Kerst, Beatrijs A. Seinstra, Neeltje Steeghs, Winette T.A.
The Breast.2024; 78: 103825. CrossRef - Lymph node involvement in secondary breast angiosarcoma – a case presentation
Adriana Irina Ciuvică, Tiberiu Augustin Georgescu , Andrei Dennis Voichiţoiu , Angela Arsene , Luchian Marinescu , George Ionuţ Bucur , Livia Iordache , Nahedd Saba
Romanian Journal of Morphology and Embryology.2024; 65(3): 523. CrossRef - Primary ovarian angiosarcoma: Two case reports and review of literature
Ying Zhou, Yi-Wen Sun, Xiao-Yang Liu, Dan-Hua Shen
World Journal of Clinical Cases.2023; 11(21): 5122. CrossRef
- Etiology, pathogenesis, and management of angiosarcoma associated with implants and foreign body: Clinical cases and research updates
- Clinicopathologic features and survival outcomes of ocular melanoma: a series of 31 cases from a tertiary university hospital
- Selin Kestel, Feriha Pınar Uyar Göçün, Betül Öğüt, Özlem Erdem
- J Pathol Transl Med. 2022;56(4):187-198. Published online May 3, 2022
- DOI: https://doi.org/10.4132/jptm.2022.03.10
- 5,957 View
- 206 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
We aimed to determine the effect of clinicopathologic features on overall survival among Caucasian ocular melanoma patients in the Central Anatolia region of Turkey.
Methods
This single-center study included conjunctival (n = 12) and uveal (n = 19) melanoma patients diagnosed between January 2008 and March 2020. Clinicopathologic features and outcomes were reviewed retrospectively. Five cases were tested for BRAF V600 mutations with real-time polymerase chain reaction, and one case was tested with nextgeneration sequencing. Survival was calculated using the Kaplan-Meier method.
Results
Thirty-one patients had a mean initial age of 58.32 years (median, 61 years; range 25 to 78 years). There were 13 male and 18 female patients. The median follow-up time was 43.5 months (range, 6 to 155 months) for conjunctival melanoma and 35 months (range, 8 to 151 months) for uveal melanoma. When this study ended, eight of the 12 conjunctival melanoma patients (66.7%) and nine of the 19 uveal melanoma patients (47.4%) had died. The presence of tumor-infiltrating lymphocytes was related to improved overall survival in conjunctival melanoma (p = .014), whereas the presence of ulceration (p = .030), lymphovascular invasion (p = .051), tumor in the left eye (p = .012), tumor thickness of > 2 mm (p = .012), and mitotic count of >1/mm² (p = .012) reduced the overall survival in conjunctival melanoma. Uveal melanoma tumors with the largest diameter of 9.1–15 mm led to the lowest overall survival among subgroups (p = .035). Involvement of the conjunctiva (p=.005) and lens (p = .003) diminished overall survival in uveal melanoma. BRAF V600 mutation was present in one case of conjunctival melanoma, GNAQ R183Q mutation was present in one case of uveal melanoma. Patients with uveal melanoma presented with an advanced pathological tumor stage compared to those with conjunctival melanoma (p = .019).
Conclusions
This study confirmed the presence of tumor-infiltrating lymphocytes as a favorable factor in conjunctival melanoma and conjunctival and lens involvement as unfavorable prognostic factors in uveal melanoma for overall survival, respectively. -
Citations
Citations to this article as recorded by- Uveal melanoma in the Iranian population: two decades of patient management in a tertiary eye center
Hamid Riazi-Esfahani, Abdulrahim Amini, Babak Masoomian, Mehdi Yaseri, Siamak Sabour, Ali Rashidinia, Mojtaba Arjmand, Seyed Mohsen Rafizadeh, Mohammadkarim Johari, Elias Khalili Pour, Fariba Ghassemi
International Journal of Retina and Vitreous.2024;[Epub] CrossRef - Clinical features and prognosis of patients with metastatic ocular and orbital melanoma: A bi‐institutional study
Xin Liu, Han Yue, Shiyu Jiang, Lin Kong, Yu Xu, Yong Chen, Chunmeng Wang, Yan Wang, Xiaoli Zhu, Yunyi Kong, Xiaowei Zhang, Jiang Qian, Zhiguo Luo
Cancer Medicine.2023; 12(15): 16163. CrossRef - Metastatic melanoma: clinicopathologic features and overall survival comparison
Selin Kestel, Feriha Pınar Uyar Göçün, Betül Öğüt, Özlem Erdem
Acta Dermatovenerologica Alpina Pannonica et Adriatica.2022;[Epub] CrossRef
- Uveal melanoma in the Iranian population: two decades of patient management in a tertiary eye center
- Immunohistochemical expression of programmed death-ligand 1 and CD8 in glioblastomas
- Dina Mohamed El Samman, Manal Mohamed El Mahdy, Hala Sobhy Cousha, Zeinab Abd El Rahman Kamar, Khaled Abdel Karim Mohamed, Hoda Hassan Abou Gabal
- J Pathol Transl Med. 2021;55(6):388-397. Published online October 14, 2021
- DOI: https://doi.org/10.4132/jptm.2021.08.04
- 4,947 View
- 187 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Glioblastoma is the most aggressive primary malignant brain tumor in adults and is characterized by poor prognosis. Immune evasion occurs via programmed death-ligand 1 (PD-L1)/programmed death receptor 1 (PD-1) interaction. Some malignant tumors have responded to PD-L1/PD-1 blockade treatment strategies, and PD-L1 has been described as a potential predictive biomarker. This study discussed the expression of PD-L1 and CD8 in glioblastomas.
Methods
Thirty cases of glioblastoma were stained immunohistochemically for PD-L1 and CD8, where PD-L1 expression in glioblastoma tumor tissue above 1% is considered positive and CD-8 is expressed in tumor infiltrating lymphocytes. The expression of each marker was correlated with clinicopathologic parameters. Survival analysis was conducted to correlate progression-free survival (PFS) and overall survival (OS) with PD-L1 and CD8 expression.
Results
Diffuse/fibrillary PD-L1 was expressed in all cases (mean expression, 57.6%), whereas membranous PD-L1 was expressed in six of 30 cases. CD8-positive tumor-infiltrating lymphocytes (CD8+ TILs) had a median expression of 10%. PD-L1 and CD8 were positively correlated (p = .001). High PD-L1 expression was associated with worse PFS and OS (p = .026 and p = .001, respectively). Correlation of CD8+ TILs percentage with age, sex, tumor site, laterality, and outcomes were statistically insignificant. Multivariate analysis revealed that PD-L1 was the only independent factor that affected prognosis.
Conclusions
PD-L1 expression in patients with glioblastoma is robust; higher PD-L1 expression is associated with lower CD8+ TIL expression and worse prognosis. -
Citations
Citations to this article as recorded by- Pathological diagnosis of central nervous system tumours in adults: what's new?
Evert-Jan Kooi, Lukas Marcelis, Pieter Wesseling
Pathology.2025; 57(2): 144. CrossRef - Expression of Programmed Cell Death-Ligand 1 (PD-L1) in Astrocytic Tumors and Its Correlation With Histopathological Grade and Proliferative Index (Ki-67): A Cross-Sectional Study
Namita Singh, Ranjana Giri, Prita Pradhan, Diptiranjan Satapathy, Ipsita Debata
Cureus.2025;[Epub] CrossRef - Tumor-associated microenvironment, PD-L1 expression and their relationship with immunotherapy in glioblastoma, IDH-wild type: A comprehensive review with emphasis on the implications for neuropathologists
Giuseppe Broggi, Giuseppe Angelico, Jessica Farina, Giordana Tinnirello, Valeria Barresi, Magda Zanelli, Andrea Palicelli, Francesco Certo, Giuseppe Barbagallo, Gaetano Magro, Rosario Caltabiano
Pathology - Research and Practice.2024; 254: 155144. CrossRef - Immunophenotypic Profile of Adult Glioblastoma IDH-Wildtype Microenvironment: A Cohort Study
Sofia Asioli, Lidia Gatto, Uri Vardy, Claudio Agostinelli, Vincenzo Di Nunno, Simona Righi, Alicia Tosoni, Francesca Ambrosi, Stefania Bartolini, Caterina Giannini, Enrico Franceschi
Cancers.2024; 16(22): 3859. CrossRef - Analysis of PD-L1 and CD3 Expression in Glioblastoma Patients and Correlation with Outcome: A Single Center Report
Navid Sobhani, Victoria Bouchè, Giovanni Aldegheri, Andrea Rocca, Alberto D’Angelo, Fabiola Giudici, Cristina Bottin, Carmine Antonio Donofrio, Maurizio Pinamonti, Benvenuto Ferrari, Stefano Panni, Marika Cominetti, Jahard Aliaga, Marco Ungari, Antonio Fi
Biomedicines.2023; 11(2): 311. CrossRef - Immuno-PET Imaging of Tumour PD-L1 Expression in Glioblastoma
Gitanjali Sharma, Marta C. Braga, Chiara Da Pieve, Wojciech Szopa, Tatjana Starzetz, Karl H. Plate, Wojciech Kaspera, Gabriela Kramer-Marek
Cancers.2023; 15(12): 3131. CrossRef
- Pathological diagnosis of central nervous system tumours in adults: what's new?
- The Prognostic Impact of Synchronous Ipsilateral Multiple Breast Cancer: Survival Outcomes according to the Eighth American Joint Committee on Cancer Staging and Molecular Subtype
- Jinah Chu, Hyunsik Bae, Youjeong Seo, Soo Youn Cho, Seok-Hyung Kim, Eun Yoon Cho
- J Pathol Transl Med. 2018;52(6):396-403. Published online October 23, 2018
- DOI: https://doi.org/10.4132/jptm.2018.10.03
- 6,871 View
- 98 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
In the current American Joint Committee on Cancer staging system of breast cancer, only tumor size determines T-category regardless of whether the tumor is single or multiple. This study evaluated if tumor multiplicity has prognostic value and can be used to subclassify breast cancer.
Methods
We included 5,758 patients with invasive breast cancer who underwent surgery at Samsung Medical Center, Seoul, Korea, from 1995 to 2012.
Results
Patients were divided into two groups according to multiplicity (single, n = 4,744; multiple, n = 1,014). Statistically significant differences in lymph node involvement and lymphatic invasion were found between the two groups (p < .001). Patients with multiple masses tended to have luminal A molecular subtype (p < .001). On Kaplan-Meier survival analysis, patients with multiple masses had significantly poorer disease-free survival (DFS) (p = .016). The prognostic significance of multiplicity was seen in patients with anatomic staging group I and prognostic staging group IA (p = .019 and p = .032, respectively). When targeting patients with T1-2 N0 M0, hormone receptor–positive, and human epidermal growth factor receptor 2 (HER2)–negative cancer, Kaplan-Meier survival analysis also revealed significantly reduced DFS with multiple cancer (p = .031). The multivariate analysis indicated that multiplicity was independently correlated with worse DFS (hazard ratio, 1.23; 95% confidence interval, 1.03 to 1.47; p = .025). The results of this study indicate that tumor multiplicity is frequently found in luminal A subtype, is associated with frequent lymph node metastasis, and is correlated with worse DFS.
Conclusions
Tumor multiplicity has prognostic value and could be used to subclassify invasive breast cancer at early stages. Adjuvant chemotherapy would be necessary for multiple masses of T1–2 N0 M0, hormone-receptor-positive, and HER2-negative cancer. -
Citations
Citations to this article as recorded by- Prognostic Impact of Multiple Synchronous T1 Breast Cancer
Hongki Gwak, Sung Hoo Jung, Young Jin Suh, Seok Jin Nam, Jai Hong Han, Se Jeong Oh, Eun Hwa Park, Seong Hwan Kim
Cancers.2024; 16(23): 4019. CrossRef - Deep learning-based system for automatic prediction of triple-negative breast cancer from ultrasound images
Alexandre Boulenger, Yanwen Luo, Chenhui Zhang, Chenyang Zhao, Yuanjing Gao, Mengsu Xiao, Qingli Zhu, Jie Tang
Medical & Biological Engineering & Computing.2023; 61(2): 567. CrossRef - Multicentre prospective cohort study of unmet supportive care needs among patients with breast cancer throughout their cancer treatment trajectory in Penang: a PenBCNeeds Study protocol
Noorsuzana Mohd Shariff, Nizuwan Azman, Rohayu Hami, Noor Mastura Mohd Mujar, Mohammad Farris Iman Leong Bin Abdullah
BMJ Open.2021; 11(3): e044746. CrossRef - The subgross morphology of breast carcinomas: a single-institution series of 2033 consecutive cases documented in large-format histology slides
Tibor Tot, Maria Gere, Syster Hofmeyer, Annette Bauer, Ulrika Pellas
Virchows Archiv.2020; 476(3): 373. CrossRef - Editorial for “Synchronous Breast Cancer: Phenotypic Similarities on MRI”
Uma Sharma
Journal of Magnetic Resonance Imaging.2020; 52(1): 309. CrossRef - Synchronous Multiple Breast Cancers—Do We Need to Reshape Staging?
Minodora Onisâi, Adrian Dumitru, Iuliana Iordan, Cătălin Aliuș, Oana Teodor, Adrian Alexandru, Daniela Gheorghiță, Iulian Antoniac, Adriana Nica, Alexandra-Ana Mihăilescu, Sebastian Grădinaru
Medicina.2020; 56(5): 230. CrossRef - Molecular mechanism of triple‑negative breast cancer‑associated BRCA1 and the identification of signaling pathways
Feng Qi, Wen‑Xing Qin, Yuan‑Sheng Zang
Oncology Letters.2019;[Epub] CrossRef
- Prognostic Impact of Multiple Synchronous T1 Breast Cancer
- Extramural Perineural Invasion in pT3 and pT4 Gastric Carcinomas
- Alejandro España-Ferrufino, Leonardo S. Lino-Silva, Rosa A. Salcedo-Hernández
- J Pathol Transl Med. 2018;52(2):79-84. Published online November 9, 2017
- DOI: https://doi.org/10.4132/jptm.2017.11.01
- 8,694 View
- 142 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Perineural invasion (PNI) is widely studied in malignant tumors, and its prognostic significance is well demonstrated. Most studies have focused on evaluating the mural PNI (mPNI); however, extramural PNI (ePNI) may influence the prognosis in gastric cancer. We evaluated the prognostic value of ePNI compared with mPNI in gastric cancer in this observational comparative cross-sectional study.
Methods
Seventy-three pT3 and pT4 gastric carcinomas with PNI were evaluated. Forty-eight (65.7%) were in the mPNI group and the remaining in the ePNI group.
Results
Clinicopathologic characteristics between the two groups were similar, except for the outcomes. The 5-year disease-specific survival (DSS) rate was 64% for the mPNI group and 50% for the ePNI group (p=.039), a difference that did not remain significant in multivariate analysis. The only independent adverse prognostic factor in multivariate analysis was the presence of lymph node metastasis (hazard ratio, 1.757; 95% confidence interval, 1.082 to 2.854; p=.023).
Conclusions
We demonstrated the prognostic effect of ePNI for DSS in surgically resected pT3–pT4 gastric cancer patients. ePNI could be considered in the staging and prognostic systems of gastric cancer to stratify patients with a high risk of recurrence. -
Citations
Citations to this article as recorded by- Investigation of Conditioned Media-Mediated Communication between Pancreatic Cancer Cells and Neurons
Didem Karakaş
Acta Medica Nicomedia.2025; 8(1): 15. CrossRef - Innervating 3D in vitro models: bioengineering and design blueprints
Mariana-Tomás de Carvalho, Margarida Henriques-Pereira, Maria V. Monteiro, Meriem Lamghari, João F. Mano, Vítor M. Gaspar
Trends in Biotechnology.2025;[Epub] CrossRef - Neural control of tumor immunity
Burak Kizil, Francesco De Virgiliis, Christoph Scheiermann
The FEBS Journal.2024; 291(21): 4670. CrossRef - Spectral CT-based nomogram for preoperative prediction of perineural invasion in locally advanced gastric cancer: a prospective study
Jing Li, Shuning Xu, Yi Wang, Mengjie Fang, Fei Ma, Chunmiao Xu, Hailiang Li
European Radiology.2023; 33(7): 5172. CrossRef - Crosstalk between cancer cells and the nervous system
Meng Huang, Gu Gong, Yicheng Deng, Xinmiao Long, Wenyong Long, Qing Liu, Wei Zhao, Rufu Chen
Medicine Advances.2023; 1(3): 173. CrossRef - Targeting tumor innervation: premises, promises, and challenges
Xinyu Li, Xueqiang Peng, Shuo Yang, Shibo Wei, Qing Fan, Jingang Liu, Liang Yang, Hangyu Li
Cell Death Discovery.2022;[Epub] CrossRef - Cancer-Associated Neurogenesis and Nerve-Cancer Cross-talk
Deborah A. Silverman, Vena K. Martinez, Patrick M. Dougherty, Jeffrey N. Myers, George A. Calin, Moran Amit
Cancer Research.2021; 81(6): 1431. CrossRef - Perineural Invasion and Postoperative Adjuvant Chemotherapy Efficacy in Patients With Gastric Cancer
Qing Tao, Wen Zhu, Xiaohui Zhao, Mei Li, Yongqian Shu, Deqiang Wang, Xiaoqin Li
Frontiers in Oncology.2020;[Epub] CrossRef - Perineural invasion as a predictive factor for survival outcome in gastric cancer patients: a systematic review and meta-analysis
Bochao Zhao, Wu Lv, Di Mei, Rui Luo, Shiyang Bao, Baojun Huang, Jie Lin
Journal of Clinical Pathology.2020; 73(9): 544. CrossRef - Consensus-Expressed CXCL8 and MMP9 Identified by Meta-Analyzed Perineural Invasion Gene Signature in Gastric Cancer Microarray Data
Xiuzhi Jia, Minjia Lu, Chen Rui, Ying Xiao
Frontiers in Genetics.2019;[Epub] CrossRef
- Investigation of Conditioned Media-Mediated Communication between Pancreatic Cancer Cells and Neurons
- Loss of Progesterone Receptor Expression Is an Early Tumorigenesis Event Associated with Tumor Progression and Shorter Survival in Pancreatic Neuroendocrine Tumor Patients
- Sung Joo Kim, Soyeon An, Jae Hoon Lee, Joo Young Kim, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Eunsil Yu, Seung-Mo Hong
- J Pathol Transl Med. 2017;51(4):388-395. Published online June 8, 2017
- DOI: https://doi.org/10.4132/jptm.2017.03.19
- 7,864 View
- 137 Download
- 17 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Pancreatic neuroendocrine tumors (PanNETs) are the second most common pancreatic neoplasms and there is no well-elucidated biomarker to stratify their detection and prognosis. Previous studies have reported that progesterone receptor (PR) expression status was associated with poorer survival in PanNET patients.
Methods
To validate previous studies, PR protein expression was assessed in 21 neuroendocrine microadenomas and 277 PanNETs and compared with clinicopathologic factors including patient survival.
Results
PR expression was gradually decreased from normal islets (49/49 cases, 100%) to neuroendocrine microadenoma (14/21, 66.6%) to PanNETs (60/277, 21.3%; p < .001). PanNETs with loss of PR expression were associated with increased tumor size (p < .001), World Health Organization grade (p = .001), pT classification (p < .001), perineural invasion (p = .028), lymph node metastasis (p = .004), activation of alternative lengthening of telomeres (p = .005), other peptide hormonal expression (p < .001) and ATRX/DAXX expression (p = .015). PanNET patients with loss of PR expression (5-year survival rate, 64.1%) had significantly poorer recurrence-free survival outcomes than those with intact PR expression (90%) by univariate (p = .012) but not multivariate analyses. Similarly, PanNET patients with PR expression loss (5-year survival rate, 76%) had significantly poorer overall survival by univariate (p = .015) but not multivariate analyses.
Conclusions
Loss of PR expression was noted in neuroendocrine microadenomas and was observed in the majority of PanNETs. This was associated with increased grade, tumor size, and advanced pT and pN classification; and was correlated with decreased patient survival time by univariate but not multivariate analyses. Loss of PR expression can provide additional information on shorter disease-free survival in PanNET patients. -
Citations
Citations to this article as recorded by- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
Kota Sahara, Diamantis I. Tsilimigras, Yuki Homma, Jun Kawashima, Shishir K. Maithel, Flavio Rocha, Sharon Weber, Ryan Fields, Kamran Idrees, George A. Poultsides, Cliff Cho, Itaru Endo, Timothy M. Pawlik
Journal of Surgical Oncology.2025; 131(3): 465. CrossRef - Sex Differences in the Survival of Patients with Neuroendocrine Neoplasms: A Comparative Study of Two National Databases
Mohamed Mortagy, Marie Line El Asmar, Kandiah Chandrakumaran, John Ramage
Cancers.2024; 16(13): 2376. CrossRef - Association Between Female Sex and Better Survival in Gastroenteropancreatic Neuroendocrine Tumors
Jeremy Chang, Mohammed O. Suraju, Catherine G. Tran, Carlos H.F. Chan, Po Hien Ear, James R. Howe, Scott K. Sherman
Journal of Surgical Research.2024; 302: 53. CrossRef - Venous invasion and lymphatic invasion are correlated with the postoperative prognosis of pancreatic neuroendocrine neoplasm
Sho Kiritani, Junichi Arita, Yuichiro Mihara, Rihito Nagata, Akihiko Ichida, Yoshikuni Kawaguchi, Takeaki Ishizawa, Nobuhisa Akamatsu, Junichi Kaneko, Kiyoshi Hasegawa
Surgery.2023; 173(2): 365. CrossRef - Combined Infiltrative Macroscopic Growth Pattern and Infiltrative Microscopic Tumor Border Status Is a Novel Surrogate Marker of Poor Prognosis in Patients With Pancreatic Neuroendocrine Tumor
Bokyung Ahn, Joo Young Kim, Seung-Mo Hong
Archives of Pathology & Laboratory Medicine.2023; 147(1): 100. CrossRef - HORMONET: a phase II trial of tamoxifen for estrogen/progesterone receptor-positive neuroendocrine tumors
Milton J. Barros, Jonathan Strosberg, Taymeyah Al-Toubah, Victor Hugo F. de Jesus, Lais Durant, Celso A. Mello, Tiago C. Felismino, Louise De Brot, Rodrigo G. Taboada, Mauro D. Donadio, Rachel P. Riechelmann
Therapeutic Advances in Medical Oncology.2023;[Epub] CrossRef - Diagnostic and Prognostic Impact of Progesterone Receptor Immunohistochemistry: A Study Evaluating More Than 16,000 Tumors
Florian Viehweger, Lisa-Marie Tinger, David Dum, Natalia Gorbokon, Anne Menz, Ria Uhlig, Franziska Büscheck, Andreas M. Luebke, Claudia Hube-Magg, Andrea Hinsch, Doris Höflmayer, Christoph Fraune, Patrick Lebok, Sören Weidemann, Maximilian Lennartz, Frank
Analytical Cellular Pathology.2022; 2022: 1. CrossRef - Prognostic Nomograms to Predict Overall Survival and Cancer-Specific Survival of Patients With Pancreatic Neuroendocrine Tumors
Zuoli Song, Sumei Wang, Yujing Wu, Jinjuan Zhang, Shuye Liu
Pancreas.2021; 50(3): 414. CrossRef - Pancreatic High-Grade Neuroendocrine Neoplasms in the Korean Population: A Multicenter Study
Haeryoung Kim, Soyeon An, Kyoungbun Lee, Sangjeong Ahn, Do Youn Park, Jo-Heon Kim, Dong-Wook Kang, Min-Ju Kim, Mee Soo Chang, Eun Sun Jung, Joon Mee Kim, Yoon Jung Choi, So-Young Jin, Hee Kyung Chang, Mee-Yon Cho, Yun Kyung Kang, Myunghee Kang, Soomin Ahn
Cancer Research and Treatment.2020; 52(1): 263. CrossRef - Systemic distribution of progesterone receptor subtypes in human tissues
Teeranut Asavasupreechar, Ryoko Saito, Yasuhiro Miki, Dean P. Edwards, Viroj Boonyaratanakornkit, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 199: 105599. CrossRef - Progesteron receptor expression in insulin producing cells of neuroendocrine neoplasms
Tomoyoshi Tachibana, Atsuko Kasajima, Takeshi Aoki, Tomoaki Tabata, Keely McNamara, Samaneh Yazdani, Sato Satoko, Fumiyoshi Fujishima, Fuyuhiko Motoi, Michiaki Unno, Hironobu Sasano
The Journal of Steroid Biochemistry and Molecular Biology.2020; 201: 105694. CrossRef - Prognostic and predictive factors on overall survival and surgical outcomes in pancreatic neuroendocrine tumors: recent advances and controversies
Lingaku Lee, Tetsuhide Ito, Robert T Jensen
Expert Review of Anticancer Therapy.2019; 19(12): 1029. CrossRef - Immunohistochemistry, carcinomas of unknown primary, and incidence rates
Edward B. Stelow, Hadi Yaziji
Seminars in Diagnostic Pathology.2018; 35(2): 143. CrossRef - Carbonic anhydrase 9 expression in well-differentiated pancreatic neuroendocrine neoplasms might be associated with aggressive behavior and poor survival
Joo Young Kim, Sang Hwa Lee, Soyeon An, Sung Joo Kim, You-Na Sung, Ki-Byung Song, Dae Wook Hwang, Song Cheol Kim, Seung-Mo Hong
Virchows Archiv.2018; 472(5): 739. CrossRef - Prognostic value of progesterone receptor in solid pseudopapillary neoplasm of the pancreas: evaluation of a pooled case series
Feiyang Wang, Zibo Meng, Shoukang Li, Yushun Zhang, Heshui Wu
BMC Gastroenterology.2018;[Epub] CrossRef - Estrogens modulate progesterone receptor expression and may contribute to progesterone-mediated apoptotic β-cell death
Viviane Abreu Nunes
Endocrinology&Metabolism International Journal.2018;[Epub] CrossRef
- Incidence and Prognostic Implications of Lymphovascular Invasion in Node‐Negative Pancreatic Neuroendocrine Tumors: Results From the US Neuroendocrine Study Group
- Size of Non-lepidic Invasive Pattern Predicts Recurrence in Pulmonary Mucinous Adenocarcinoma: Morphologic Analysis of 188 Resected Cases with Reappraisal of Invasion Criteria
- Soohyun Hwang, Joungho Han, Misun Choi, Myung-Ju Ahn, Yong Soo Choi
- J Pathol Transl Med. 2017;51(1):56-68. Published online October 16, 2016
- DOI: https://doi.org/10.4132/jptm.2016.09.17
- 10,709 View
- 232 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
We reviewed a series of 188 resected pulmonary mucinous adenocarcinomas (MAs) to clarify the prognostic significance of lepidic and non-lepidic patterns.
Methods
Non-lepidic patterns were divided into bland, non-distorted acini with uncertain invasiveness (pattern 1), unequivocal invasion into stroma (pattern 2), or invasion into alveolar spaces (pattern 3).
Results
The mean proportion of invasive patterns (patterns 2 and 3) was lowest in small (≤ 3 cm) tumors, and gradually increased in intermediate (> 3 cm and ≤ 7 cm) and large (> 7 cm) tumors (8.4%, 34.3%, and 50.1%, respectively). Adjusted T (aT) stage, as determined by the size of invasive patterns, was positively correlated with adverse histologic and clinical features including older age, male sex, and ever smokers. aTis tumors, which were exclusively composed of lepidic pattern (n = 9), or a mixture of lepidic and pattern 1 (n = 40) without any invasive patterns, showed 100% disease- free survival (DFS). The aT1mi tumors, with minimal (≤ 5 mm) invasive patterns (n = 63), showed a 95.2% 5-year DFS, with recurrences (n = 2) limited to tumors greater than 3 cm in total size (n = 23). Both T and aT stage were significantly associated with DFS; however, survival within the separate T-stage subgroups was stratified according to the aT stage, most notably in the intermediatestage subgroups. In multivariate analysis, the size of invasive patterns (p = .020), pleural invasion (p < .001), and vascular invasion (p = .048) were independent predictors of recurrence, whereas total size failed to achieve statistical significance (p = .121).
Conclusions
This study provides a rationale for histologic risk stratification in pulmonary MA based on the extent of invasive growth patterns with refined criteria for invasion. -
Citations
Citations to this article as recorded by- Distinct Recurrence Pattern and Survival Outcomes of Invasive Mucinous Adenocarcinoma of the Lung: The Potential Role of Local Therapy in Intrapulmonary Spread
Dong Woog Yoon, Soohyun Hwang, Tae Hee Hong, Yoon-La Choi, Hong Kwan Kim, Yong Soo Choi, Jhingook Kim, Young Mog Shim, Jong Ho Cho
Annals of Surgical Oncology.2024; 31(1): 201. CrossRef - Pulmonary invasive mucinous adenocarcinoma
Wei‐Chin Chang, Yu Zhi Zhang, Andrew G Nicholson
Histopathology.2024; 84(1): 18. CrossRef - Micropapillary Pattern in Invasive Mucinous Adenocarcinoma of the Lung: Comparison With Invasive Non-Mucinous Adenocarcinoma
Hui He, Lue Li, Yuan-yuan Wen, Li-yong Qian, Zhi-qiang Yang
International Journal of Surgical Pathology.2024; 32(5): 926. CrossRef - Radiological and clinical features of screening-detected pulmonary invasive mucinous adenocarcinoma
Dae Hyeon Kim, So Young Bae, Kwon Joong Na, Samina Park, In Kyu Park, Chang Hyun Kang, Young Tae Kim
Interactive CardioVascular and Thoracic Surgery.2022; 34(2): 229. CrossRef - Micropapillary Pattern in Invasive Mucinous Adenocarcinoma of the Lung: Comparison with Invasive Non-Mucinous Adenocarcinoma
Hui He, Yuanyuan Wen, Liyong Qian, Zhiqiang Yang
SSRN Electronic Journal .2022;[Epub] CrossRef - Optimal method for measuring invasive size that predicts survival in invasive mucinous adenocarcinoma of the lung
Tomonari Oki, Keiju Aokage, Shogo Nomura, Kenta Tane, Tomohiro Miyoshi, Norihiko Shiiya, Kazuhito Funai, Masahiro Tsuboi, Genichiro Ishii
Journal of Cancer Research and Clinical Oncology.2020; 146(5): 1291. CrossRef - Prognostic Impact of Histopathologic Features in Pulmonary Invasive Mucinous Adenocarcinomas
Wei-Chin Chang, Yu Zhi Zhang, Eric Lim, Andrew G Nicholson
American Journal of Clinical Pathology.2020; 154(1): 88. CrossRef
- Distinct Recurrence Pattern and Survival Outcomes of Invasive Mucinous Adenocarcinoma of the Lung: The Potential Role of Local Therapy in Intrapulmonary Spread
- Usual Interstitial Pneumonia with Lung Cancer: Clinicopathological Analysis of 43 Cases
- Dae Hyun Song, In Ho Choi, Sang Yun Ha, Kang Min Han, Jae Jun Lee, Min Eui Hong, Kyeongman Jeon, Man Pyo Chung, Jhingook Kim, Joungho Han
- Korean J Pathol. 2014;48(1):10-16. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.10
- 10,087 View
- 77 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Previous studies have suggested an association between usual interstitial pneumonia (UIP) and lung cancer (Ca). However, clinical and histological information is not enough to determine such an association, due to the low incidence and short survival time of patients with both conditions.
Methods We retrospectively reviewed the clinical and histological records of Ca patients with UIP between January 1999 and August 2013 at the Samsung Medical Center, Seoul, Korea. We found 43 patients who had Ca with UIP (UIP-Ca). Previously reported data of eighty-four patients with UIP-only were included as a comparison group.
Results Smoking is related to poor prognosis in patients with UIP-Ca, and the number of patients with a high smoking index of more than 30 pack-years significantly increased in UIP-Ca patients compared with UIP-only patients. There is no significant prognostic differentiation between UIP-Ca patients and UIP-only patients. Microscopically, UIP-Ca patients showed characteristically heterogeneous histological patterns and degrees of differentiation. There were many foci of squamous metaplasia or dysplasia at the peripheral area of squamous cell carcinomas.
Conclusions We report 43 cases of UIP-Ca. Our results suggest that smoking is related to cancer occurrence in UIP patients and poor prognosis in UIP-Ca patients.
-
Citations
Citations to this article as recorded by- Treatable traits in interstitial lung disease: a narrative review
Megan Harrison, Chloe Lawler, Fiona Lake, Vidya Navaratnam, Caitlin Fermoyle, Yuben Moodley, Tamera J. Corte
Therapeutic Advances in Respiratory Disease.2025;[Epub] CrossRef - Prognosis of idiopathic pulmonary fibrosis without anti-fibrotic therapy: a systematic review
Yet H. Khor, Yvonne Ng, Hayley Barnes, Nicole S.L. Goh, Christine F. McDonald, Anne E. Holland
European Respiratory Review.2020; 29(157): 190158. CrossRef - Linfoma difuso de células B grandes pulmonar en paciente con neumonía intersticial no específica
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica.2019; 15(6): e151. CrossRef - Diffuse Large B-cell Lymphoma of the Lung in a Patient With Nonspecific Interstitial Pneumonia
Luis Gorospe Sarasúa, Paola Arrieta, Anabelle Chinea-Rodríguez, Carlos de la Puente-Bujidos
Reumatología Clínica (English Edition).2019; 15(6): e151. CrossRef - Characteristics of lung cancer among patients with idiopathic pulmonary fibrosis and interstitial lung disease – analysis of institutional and population data
Joo Heung Yoon, Mehdi Nouraie, Xiaoping Chen, Richard H Zou, Jacobo Sellares, Kristen L Veraldi, Jared Chiarchiaro, Kathleen Lindell, David O Wilson, Naftali Kaminski, Timothy Burns, Humberto Trejo Bittar, Samuel Yousem, Kevin Gibson, Daniel J Kass
Respiratory Research.2018;[Epub] CrossRef - Genomic profiles of lung cancer associated with idiopathic pulmonary fibrosis
Ji An Hwang, Deokhoon Kim, Sung‐Min Chun, SooHyun Bae, Joon Seon Song, Mi Young Kim, Hyun Jung Koo, Jin Woo Song, Woo Sung Kim, Jae Cheol Lee, Hyeong Ryul Kim, Chang‐Min Choi, Se Jin Jang
The Journal of Pathology.2018; 244(1): 25. CrossRef - Survival after repeated surgery for lung cancer with idiopathic pulmonary fibrosis: a retrospective study
Seijiro Sato, Yuki Shimizu, Tatsuya Goto, Akihiko Kitahara, Terumoto Koike, Hiroyuki Ishikawa, Takehiro Watanabe, Masanori Tsuchida
BMC Pulmonary Medicine.2018;[Epub] CrossRef - Alveolar Squamous Cell Metaplasia: Preneoplastic Lesion?
Adriana Handra-Luca
Journal of Pathology and Translational Medicine.2018; 52(6): 355. CrossRef - Low expression of long noncoding RNA CDKN2B-AS1 in patients with idiopathic pulmonary fibrosis predicts lung cancer by regulating the p53-signaling pathway
Yufeng Du, Xiaoyan Hao, Xuejun Liu
Oncology Letters.2018;[Epub] CrossRef - A clinicopathological study of surgically resected lung cancer in patients with usual interstitial pneumonia
Yasutaka Watanabe, Yoshinori Kawabata, Nobuyuki Koyama, Tomohiko Ikeya, Eishin Hoshi, Noboru Takayanagi, Shinichiro Koyama
Respiratory Medicine.2017; 129: 158. CrossRef - Risk of the preoperative underestimation of tumour size of lung cancer in patients with idiopathic interstitial pneumonias
Mariko Fukui, Kazuya Takamochi, Takeshi Matsunaga, Shiaki Oh, Katsutoshi Ando, Kazuhiro Suzuki, Atsushi Arakawa, Toshimasa Uekusa, Kenji Suzuki
European Journal of Cardio-Thoracic Surgery.2016; 50(3): 428. CrossRef - The Idiopathic Interstitial Pneumonias: Histology and Imaging
Diane C. Strollo, Teri J. Franks, Jeffrey R. Galvin
Seminars in Roentgenology.2015; 50(1): 8. CrossRef - Do Chest Expansion Exercises Aid Re‐shaping the Diaphragm Within the First 72 Hours Following Lung Transplantation in a Usual Interstitial Pneumonia Patient?
Massimiliano Polastri, Erika Venturini, Saverio Pastore, Andrea Dell'Amore
Physiotherapy Research International.2015; 20(3): 191. CrossRef - Scrotal wall metastasis from a primary lung adenocarcinoma
Marie-Louise M. Coussa-Koniski, Pia A. Maalouf, Nehme E. Raad, Noha A. Bejjani
Respiratory Medicine Case Reports.2015; 15: 77. CrossRef - The Ratio KL-6 to SLX in Serum for Prediction of the Occurrence of Drug-Induced Interstitial Lung Disease in Lung Cancer Patients with Idiopathic Interstitial Pneumonias Receiving Chemotherapy
Kosuke Kashiwabara, Hiroshi Semba, Shinji Fujii, Shinsuke Tsumura, Ryota Aoki
Cancer Investigation.2015; 33(10): 516. CrossRef - Idiopathic pulmonary fibrosis will increase the risk of lung cancer
Li Junyao, Yang Ming, Li Ping, Su Zhenzhong, Gao Peng, Zhang Jie
Chinese Medical Journal.2014; 127(17): 3142. CrossRef
- Treatable traits in interstitial lung disease: a narrative review
- Prognostic Significance of BCL9 Expression in Hepatocellular Carcinoma
- Jiyeon Hyeon, Soomin Ahn, Jae Jun Lee, Dae Hyun Song, Cheol-Keun Park
- Korean J Pathol. 2013;47(2):130-136. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.130
- 8,529 View
- 70 Download
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF Background BCL9 enhances β-catenin-mediated transcriptional activity regardless of the mutational status of the Wnt signaling components and increases the cell proliferation, migration, invasion, and metastatic potential of tumor cells. The goal of this study was to elucidate the prognostic significance of BCL9 protein expression in hepatocellular carcinoma (HCC) patients.
Methods We evaluated BCL9 protein expression by immunohistochemistry in tumor tissue from 288 primary HCC patients who underwent curative hepatectomy. The impact of BCL9 expression on the survival of the patients was analyzed. The median follow-up period was 97.1 months.
Results Nuclear BCL9 protein expression was observed in 74 (25.7%) of the 288 HCCs. BCL9 expression was significantly associated with younger age (p=0.038), higher Edmondson grade (p=0.001), microvascular invasion (p=0.013), and intrahepatic metastasis (p=0.017). Based on univariate analyses, BCL9 expression showed an unfavorable influence on both disease-free survival (DFS, p=0.012) and disease-specific survival (DSS, p=0.032). Multivariate analyses revealed that higher Barcelona Clinic Liver Cancer stage was an independent predictor of both shorter DFS (p<0.001) and shorter DSS (p<0.001). BCL9 expression tended to be an independent predictor of shorter DFS (p=0.078).
Conclusions BCL9 protein expression might be a marker of shorter DFS in HCC patients after curative hepatectomy.
-
Citations
Citations to this article as recorded by- The Wnt-dependent and Wnt-independent functions of BCL9 in development, tumorigenesis, and immunity: Implications in therapeutic opportunities
Minjie Wu, Heng Dong, Chao Xu, Mengqing Sun, Haojin Gao, Fangtian Bu, Jianxiang Chen
Genes & Diseases.2024; 11(2): 701. CrossRef - The role of BCL9 genetic variation as a biomarker for hepatitis C-related hepatocellular carcinoma in Egyptian patients
Eman Abd El Razek Abbas, Ahmed Barakat Barakat, Mohamed Hassany, Samar Samir Youssef
Journal of Genetic Engineering and Biotechnology.2022; 20(1): 4. CrossRef - Molecular Targets and Signaling Pathways of microRNA-122 in Hepatocellular Carcinoma
Kwang-Hoon Chun
Pharmaceutics.2022; 14(7): 1380. CrossRef - Wnt/β-Catenin Signalling and Its Cofactor BCL9L Have an Oncogenic Effect in Bladder Cancer Cells
Roland Kotolloshi, Mieczyslaw Gajda, Marc-Oliver Grimm, Daniel Steinbach
International Journal of Molecular Sciences.2022; 23(10): 5319. CrossRef - Bcl9 Depletion Modulates Endothelial Cell in Tumor Immune Microenvironment in Colorectal Cancer Tumor
Zhuang Wei, Mei Feng, Zhongen Wu, Shuru Shen, Di Zhu
Frontiers in Oncology.2021;[Epub] CrossRef - Wnt Signaling Pathway Is among the Drivers of Liver Metastasis
Ivana Samaržija
Livers.2021; 1(4): 180. CrossRef - Nuclear Expression of Pygo2 Correlates with Poorly Differentiated State Involving c-Myc, PCNA and Bcl9 in Myanmar Hepatocellular Carcinoma
Myo Win Htun, Yasuaki Shibata, Kyaw Soe, Takehiko Koji
ACTA HISTOCHEMICA ET CYTOCHEMICA.2021; 54(6): 195. CrossRef - Wnt status-dependent oncogenic role of BCL9 and BCL9L in hepatocellular carcinoma
Nicole Huge, Maria Sandbothe, Anna K. Schröder, Amelie Stalke, Marlies Eilers, Vera Schäffer, Brigitte Schlegelberger, Thomas Illig, Beate Vajen, Britta Skawran
Hepatology International.2020; 14(3): 373. CrossRef - Structure and function of Pygo in organ development dependent and independent Wnt signalling
Yan Shi, Xiushan Wu, Shuoji Zhu, Huanlei Huang, Jian Zhuang, Haiyun Yuan, Wuzhou Yuan, Ping Zhu
Biochemical Society Transactions.2020; 48(4): 1781. CrossRef - BCL9/BCL9L in hepatocellular carcinoma: will it or Wnt it be the next therapeutic target?
Akshata Moghe, Satdarshan P. Monga
Hepatology International.2020; 14(4): 460. CrossRef - Loss of BCL9/9l suppresses Wnt driven tumourigenesis in models that recapitulate human cancer
David M. Gay, Rachel A. Ridgway, Miryam Müller, Michael C. Hodder, Ann Hedley, William Clark, Joshua D. Leach, Rene Jackstadt, Colin Nixon, David J. Huels, Andrew D. Campbell, Thomas G. Bird, Owen J. Sansom
Nature Communications.2019;[Epub] CrossRef - Immunohistochemical Mapping of Bcl9 Using Two Antibodies that Recognize Different Epitopes Is Useful to Characterize Juvenile Development of Hepatocellular Carcinoma in Myanmar
Myat Thu Soe, Yasuaki Shibata, Myo Win Htun, Kuniko Abe, Kyaw Soe, Nay Win Than, Thann Lwin, Myat Phone Kyaw, Takehiko Koji
ACTA HISTOCHEMICA ET CYTOCHEMICA.2019; 52(1): 9. CrossRef - Low BCL9 expression inhibited ovarian epithelial malignant tumor progression by decreasing proliferation, migration, and increasing apoptosis to cancer cells
Jing Wang, Mingjun Zheng, Liancheng Zhu, Lu Deng, Xiao Li, Linging Gao, Caixia Wang, Huimin Wang, Juanjuan Liu, Bei Lin
Cancer Cell International.2019;[Epub] CrossRef - SOX7 Suppresses Wnt Signaling by Disrupting β-Catenin/BCL9 Interaction
Rong Fan, HaiYan He, Wang Yao, YanFeng Zhu, XunJie Zhou, MingTai Gui, Jing Lu, Hao Xi, ZhongLong Deng, Min Fan
DNA and Cell Biology.2018; 37(2): 126. CrossRef - Hypoxia activates Wnt/β-catenin signaling by regulating the expression of BCL9 in human hepatocellular carcinoma
Wei Xu, Wang Zhou, Mo Cheng, Jing Wang, Zhian Liu, Shaohui He, Xiangji Luo, Wending Huang, Tianrui Chen, Wangjun Yan, Jianru Xiao
Scientific Reports.2017;[Epub] CrossRef - Hepatocellular carcinoma biology predicts survival outcome after liver transplantation in the USA
Mohamed Abd El-Fattah
Indian Journal of Gastroenterology.2017; 36(2): 117. CrossRef - miR-30a acts as a tumor suppressor by double-targeting COX-2 and BCL9 in H. pylori gastric cancer models
Xuan Liu, Qing Ji, Chengcheng Zhang, Xiaowei Liu, Yanna Liu, Ningning Liu, Hua Sui, Lihong Zhou, Songpo Wang, Qi Li
Scientific Reports.2017;[Epub] CrossRef - BCL9, a coactivator for Wnt/β-catenin transcription, is targeted by miR-30c and is associated with prostate cancer progression
XIAO-HUI LING, ZHI-YUN CHEN, HONG-WEI LUO, ZE-ZHEN LIU, YING-KE LIANG, GUAN-XING CHEN, FU-NENG JIANG, WEI-DE ZHONG
Oncology Letters.2016; 11(3): 2001. CrossRef
- The Wnt-dependent and Wnt-independent functions of BCL9 in development, tumorigenesis, and immunity: Implications in therapeutic opportunities
- CHD1L Is a Marker for Poor Prognosis of Hepatocellular Carcinoma after Surgical Resection
- Jiyeon Hyeon, Soomin Ahn, Cheol-Keun Park
- Korean J Pathol. 2013;47(1):9-15. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.9
- 8,292 View
- 71 Download
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The gene for chromodomain helicase/ATPase DNA binding protein 1-like (
CHD1L ) was recently identified as a target oncogene within the 1q21 amplicon, which occurs in 46% to 86% of primary hepatocellular carcinoma (HCC) cases. However, the prognostic significance of CHD1L in HCC remains uncertain. In this study, we investigated the roles of CHD1L in the prognosis of HCC.Methods We investigated the expressions of CHD1L in tumor tissue microarrays of 281 primary HCC patients who underwent surgical resection using immunohistochemistry. Prognostic factors of HCC were examined by univariate and multivariate analyses. The median follow-up period was 75.6 months.
Results CHD1L expression was observed in 48 of the 281 HCCs (17.1%). CHD1L expression was associated with a younger age (p=0.033), higher Edmondson grade (p=0.019), microvascular invasion (p<0.001), major portal vein invasion (p=0.037), higher American Joint Committee on Cancer T stage (p=0.001), lower albumin level (p=0.047), and higher α-fetoprotein level (p=0.002). Multivariate analyses revealed that CHD1L expression (p=0.027), Edmondson grade III (p=0.034), and higher Barcelona Clinic Liver Cancer stage (p<0.001) were independent predictors of shorter disease-free survival.
Conclusions CHD1L expression might be a prognostic marker of shorter disease-free survival in HCC patients after surgical resection.
-
Citations
Citations to this article as recorded by- Targeted Inhibition of CHD1L by OTI-611 Reprograms Chemotherapy and Targeted Therapy-Induced Cell Cycle Arrest and Suppresses Proliferation to Produce Synergistic Antitumor Effects in Breast and Colorectal Cancer
Hector Esquer, Qiong Zhou, Daniel V. LaBarbera
Cells.2025; 14(5): 318. CrossRef - CHD1L in cancer and beyond: structure, oncogenic functions, and therapeutic potential
Sophia Clune, Paul Awolade, Hector Esquer, Qiong Zhou, Daniel V. LaBarbera
Journal of Experimental & Clinical Cancer Research.2025;[Epub] CrossRef - The validation of new CHD1L inhibitors as a therapeutic strategy for cancer
Sophia Clune, Paul Awolade, Qiong Zhou, Hector Esquer, Brock Matter, Jeffrey T. Kearns, Timothy Kellett, Damilola Caleb Akintayo, Uday B. Kompella, Daniel V. LaBarbera
Biomedicine & Pharmacotherapy.2024; 170: 116037. CrossRef - Role of pelitinib in the regulation of migration and invasion of hepatocellular carcinoma cells via inhibition of Twist1
Sewoong Lee, Eunjeong Kang, Unju Lee, Sayeon Cho
BMC Cancer.2023;[Epub] CrossRef - Design, Synthesis, and Biological Evaluation of the First Inhibitors of Oncogenic CHD1L
Brett J. Prigaro, Hector Esquer, Qiong Zhou, Laura A. Pike, Paul Awolade, Xin-He Lai, Adedoyin D. Abraham, Joshua M. Abbott, Brock Matter, Uday B. Kompella, Wells A. Messersmith, Daniel L. Gustafson, Daniel V. LaBarbera
Journal of Medicinal Chemistry.2022; 65(5): 3943. CrossRef - Diversity roles of CHD1L in normal cell function and tumorigenesis
Xifeng Xiong, Xudong Lai, Aiguo Li, Zhihe Liu, Ningfang Ma
Biomarker Research.2021;[Epub] CrossRef - Elevated serum alpha-fetoprotein levels are associated with poor prognosis of hepatocellular carcinoma after surgical resection: A systematic review and meta-analysis
Hong-Lin Chen, Yu-Hua Chen, Lin Du, Yi-Ping Song, Bin Zhu
Arab Journal of Gastroenterology.2021; 22(1): 12. CrossRef - Genome-wide scanning for CHD1L gene in papillary thyroid carcinoma complicated with type 2 diabetes mellitus
Y. Y. Kang, J. J. Li, J. X. Sun, J. X. Wei, C. Ding, C. L. Shi, G. Wu, K. Li, Y. F. Ma, Y. Sun, H. Qiao
Clinical and Translational Oncology.2021; 23(12): 2536. CrossRef - The high expression of CHD1L and its clinical significance in human solid tumors
Long Zhang, Yufen Jiang, Panpan Jiao, Xiaohong Deng, Yuancai Xie
Medicine.2021; 100(10): e24851. CrossRef - Clinical Significance of Trk Receptor Expression as a New Therapeutic Target in Hepatocellular Carcinoma
Sangjoon Choi, Sujin Park, Yoon Ah Cho, Cheol-Keun Park, Sang Yun Ha
Pathology & Oncology Research.2020; 26(4): 2587. CrossRef - Hepatocyte ploidy and pathological mutations in hepatocellular carcinoma: impact on oncogenesis and therapeutics
Taiji Yamazoe, Taizo Mori, Sachiyo Yoshio, Tatsuya Kanto
Global Health & Medicine.2020; 2(5): 273. CrossRef - First-in-Class Inhibitors of Oncogenic CHD1L with Preclinical Activity against Colorectal Cancer
Joshua M. Abbott, Qiong Zhou, Hector Esquer, Laura Pike, Travis P. Broneske, Sébastien Rinaldetti, Adedoyin D. Abraham, Dominique A. Ramirez, Paul J. Lunghofer, Todd M. Pitts, Daniel P. Regan, Aik Choon Tan, Daniel L. Gustafson, Wells A. Messersmith, Dani
Molecular Cancer Therapeutics.2020; 19(8): 1598. CrossRef - Prognostic role of chromodomain helicase DNA binding protein 1-like protein in human solid cancers
Wanwei Liu, Jiwei Xu, Caiyun Zhang
Medicine.2018; 97(29): e11522. CrossRef - CHD1L Expression Increases Tumor Progression and Acts as a Predictive Biomarker for Poor Prognosis in Pancreatic Cancer
Chuan Liu, Xiaowei Fu, Zhiwei Zhong, Jing Zhang, Haiyan Mou, Qiong Wu, Tianle Sheng, Bo Huang, Yeqing Zou
Digestive Diseases and Sciences.2017; 62(9): 2376. CrossRef - Overexpression of CHD1L is associated with poor survival and aggressive tumor biology in esophageal carcinoma
Ze-Han Liu, Qi Zhang, Yi-Jie Ding, Ying-Hui Ren, Hui-Peng Yang, Qing Xi, Ying-Nan Cheng, Guo-Lin Miao, Hong-Kun Liu, Cai-Xia Li, Wen-Qiang Yan, Yan Li, Zhenyi Xue, Lijuan Zhang, Xin-Ye Li, Chen-Long Zhao, Yurong Da, Xian-Zhong Wu, Jun-Qiang Chen, Rongxin
Oncotarget.2017; 8(43): 74178. CrossRef - CHD1L Regulates Cell Cycle, Apoptosis, and Migration in Glioma
Jie Sun, Li Zhang, Hongyu Zhao, Xiaojun Qiu, Wenjuan Chen, Donglin Wang, Na Ban, Shaochen Fan, Chaoyan Shen, Xiaojie Xia, Bin Ji, Yuchan Wang
Cellular and Molecular Neurobiology.2016; 36(4): 565. CrossRef - Expression of DBC1 is associated with poor prognosis in hepatitis virus-related hepatocellular carcinoma
Sang Yun Ha, Jeong Hoon Kim, Jung Wook Yang, Hyunsik Bae, Hae Yon Cho, Cheol-Keun Park
Pathology - Research and Practice.2016; 212(7): 616. CrossRef - The Overexpression of CCAR1 in Hepatocellular Carcinoma Associates with Poor Prognosis
Sang Yun Ha, Jeong Hoon Kim, Jung Wook Yang, Jimin Kim, Binnari Kim, Cheol-Keun Park
Cancer Research and Treatment.2016; 48(3): 1065. CrossRef - Genetic alterations in hepatocellular carcinoma: An update
Zhao-Shan Niu, Xiao-Jun Niu, Wen-Hong Wang
World Journal of Gastroenterology.2016; 22(41): 9069. CrossRef - CHD1L is a novel independent prognostic factor for gastric cancer
Z. Su, J. Zhao, G. Xian, W. Geng, Z. Rong, Y. Wu, C. Qin
Clinical and Translational Oncology.2014; 16(8): 702. CrossRef - Presence of CHD1L Over-Expression Is Associated with Aggressive Tumor Biology and Is a Novel Prognostic Biomarker for Patient Survival in Human Breast Cancer
Jiayi Wu, Yu Zong, Xiaochun Fei, Xiaosong Chen, Ou Huang, Jianrong He, Weiguo Chen, Yafen Li, Kunwei Shen, Li Zhu, Xin-Yuan Guan
PLoS ONE.2014; 9(8): e98673. CrossRef - CHD1L: a novel oncogene
Wen Cheng, Yun Su, Feng Xu
Molecular Cancer.2013; 12(1): 170. CrossRef - Expression of CHD1L in bladder cancer and its influence on prognosis and survival
Feng Tian, Feng Xu, Zheng-Yu Zhang, Jing-Ping Ge, Zhi-Feng Wei, Xiao-Feng Xu, Wen Cheng
Tumor Biology.2013; 34(6): 3687. CrossRef
- Targeted Inhibition of CHD1L by OTI-611 Reprograms Chemotherapy and Targeted Therapy-Induced Cell Cycle Arrest and Suppresses Proliferation to Produce Synergistic Antitumor Effects in Breast and Colorectal Cancer
- Microsatellite Instability Status in Gastric Cancer: A Reappraisal of Its Clinical Significance and Relationship with Mucin Phenotypes
- Joo-Yeun Kim, Na Ri Shin, Ahrong Kim, Hyun-Jeong Lee, Won-young Park, Jee-Yeon Kim, Chang-Hun Lee, Gi-Young Huh, Do Youn Park
- Korean J Pathol. 2013;47(1):28-35. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.28
- 10,874 View
- 122 Download
- 74 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Gastric cancers with microsatellite instabilities (MSI) have been reported to be associated with favorable prognosis. However, the significance of the effect of MSI on the clinicopathological features, as well as its association with mucin phenotype, remains unclear.
Methods MSI status was assessed in 414 cases of gastric cancer using polymerase chain reaction analysis of five microsatellite loci, as recommended by National Cancer Institution criteria. The expression of mucins (MUC5AC, MUC6, MUC2, and CD10) was assessed.
Results Out of 414 total cases of gastric cancer, 380 (91.7%), 11 (2.7%), and 23 (5.6%) were microsatellite stable (MSS), low-level MSI (MSI-L), and high-level MSI (MSI-H), respectively. Compared to MSS/MSI-L, MSI-H gastric cancers were associated with older age (p=0.010), tumor size (p=0.014), excavated gross (p=0.042), intestinal type (p=0.028), aggressive behaviors (increase of T stage [p=0.009]), perineural invasion [p=0.022], and lymphovascular emboli [p=0.027]). MSI-H gastric cancers were associated with tumor necrosis (p=0.041), tumor-infiltrating lymphocytes (≥2/high power field, p<0.001), expanding growth patterns (p=0.038), gastric predominant mucin phenotypes (p=0.028), and MUC6 expression (p=0.016). Tumor necrosis (≥10% of mass, p=0.031), tumor-infiltrating lymphocytes (p<0.001), intestinal type (p=0.014), and gastric mucin phenotypes (p=0.020) could represent independent features associated with MSI-H gastric cancers. MSI-H intestinal type gastric cancers had a tendency for poor prognosis in univariate analysis (p=0.054) but no association in Cox multivariate analysis (p=0.197).
Conclusions Our data suggest that MSI-H gastric cancers exhibit distinct aggressive biologic behaviors and a gastric mucin phenotype. This contradicts previous reports that describe MSI-H gastric cancer as being associated with favorable prognosis.
-
Citations
Citations to this article as recorded by- Intestinal Subtype as a Biomarker of Response to Neoadjuvant Immunochemotherapy in Locally Advanced Gastric Adenocarcinoma: Insights from a Prospective Phase II Trial
Lei Wang, Mengting Sun, Jinyang Li, Linghong Wan, Yuting Tan, Shuoran Tian, Yongying Hou, Linyu Wu, Ziyi Peng, Xiao Hu, Qihua Zhang, Zening Huang, Mengyi Han, Shiyin Peng, Yuwei Pan, Yuanfeng Ren, Mengsi Zhang, Dongfeng Chen, Qin Liu, Xianfeng Li, Zhong-y
Clinical Cancer Research.2025; 31(1): 74. CrossRef - How do I treat dMMR/MSI gastro-oesophageal adenocarcinoma in 2025? A position paper from the EORTC-GITCG gastro-esophageal task force
Christelle de la Fouchardière, Antonella Cammarota, Magali Svrcek, Maria Alsina, Tania Fleitas-Kanonnikoff, Radka Lordick Obermannová, Anna Dorothea Wagner, Dominic Yap Wei Ting, Diana Enea, Angelica Petrillo, Elizabeth C. Smyth
Cancer Treatment Reviews.2025; 134: 102890. CrossRef - T-bet+CD8+ T cells govern anti-PD-1 responses in microsatellite-stable gastric cancers
Shiying Tang, Xiaofang Che, Jinyan Wang, Ce Li, Xin He, Kezuo Hou, Xiaojie Zhang, Jia Guo, Bowen Yang, Danni Li, Lili Cao, Xiujuan Qu, Zhenning Wang, Yunpeng Liu
Nature Communications.2025;[Epub] CrossRef - Isolated tumor cell clusters (ITC) in lymph nodes and PD-L1 expression on tumor-associated immune cells are prognostic factors for microsatellite instable-high gastric cancers
Menghan Cui, Yangli Zhou, Yin Han, Nannan Chen, Min Zhao, Yan Wang, Fengxia He
Translational Oncology.2025; 59: 102465. CrossRef - Microsatellite Instability and BAT-26 Marker Expression in a Mexican Prostate Cancer Population with Different Gleason Scores
Ana K. Flores-Islas, Manuel A. Rico-Méndez, Marisol Godínez-Rubí, Martha Arisbeth Villanueva-Pérez, Erick Sierra-Díaz, Ana Laura Pereira-Suárez, Saul A. Beltrán-Ontiveros, Perla Y. Gutiérrez-Arzapalo, José M. Moreno-Ortiz, Adrián Ramírez-de-Arellano
Diseases.2025; 13(7): 202. CrossRef - Non–Pure Intestinal Phenotype as an Indicator of Progression in Sporadic Nonampullary Duodenal Adenomas: A Multicenter Retrospective Cohort Study
Ryotaro Uema, Yoshito Hayashi, Masato Komori, Narihiro Shibukawa, Noriko Hayashi, Masayoshi Horimoto, Takuya Yamada, Masashi Yamamoto, Satoshi Hiyama, Kazuo Kinoshita, Hideharu Ogiyama, Shinjiro Yamaguchi, Satoshi Egawa, Takashi Kanesaka, Minoru Kato, Shu
Clinical and Translational Gastroenterology.2024; 15(1): e00649. CrossRef - Intratumoral and peritumoral CT-based radiomics for predicting the microsatellite instability in gastric cancer
Xingchi Chen, Zijian Zhuang, Lin Pen, Jing Xue, Haitao Zhu, Lirong Zhang, Dongqing Wang
Abdominal Radiology.2024; 49(5): 1363. CrossRef - The tumor immune composition of mismatch repair deficient and Epstein-Barr virus-positive gastric cancer: A systematic review
J. Bos, T.S. Groen-van Schooten, C.P. Brugman, F.S. Jamaludin, H.W.M. van Laarhoven, S. Derks
Cancer Treatment Reviews.2024; 127: 102737. CrossRef - Potent therapeutic strategy in gastric cancer with microsatellite instability-high and/or deficient mismatch repair
Akira Ooki, Hiroki Osumi, Koichiro Yoshino, Kensei Yamaguchi
Gastric Cancer.2024; 27(5): 907. CrossRef - The mechanism of RGS5 regulating gastric cancer mismatch repair protein
Zhenwei Yang, Ranran Zhang, Jialong Liu, Sufang Tian, Hailin Zhang, Lingxiu Zeng, Yangyang Zhang, Liping Gao, Meng Wang, Wenqing Shan, Jing Liu
Molecular Carcinogenesis.2024; 63(9): 1750. CrossRef - Prognostic significance of microsatellite instability in patients with resectable gastric cancer
Marina Alessandra Pereira, Marcus Fernando Kodama Pertille Ramos, Leonardo Cardili, André Roncon Dias, Venancio Avancini Ferreira Alves, Evandro Sobroza de Mello, Ulysses Ribeiro
Journal of Gastrointestinal Surgery.2024; 28(10): 1687. CrossRef - Access to radiotherapy in improving gastric cancer care quality and equality
Minmin Wang, Kepei Huang, Xiaohan Fan, Jia Wang, Yinzi Jin, Zhi-Jie Zheng
Communications Medicine.2024;[Epub] CrossRef - Prediction of a Panel of PD-1 Inhibitor-Sensitive Biomarkers Using Multi-Phase CT Imaging Textural Features: A Retrospective Cohort Analysis (Preprint)
Shiqi Wang, Na Chai, Jingji Xu, Pengfei Yu, Luguang Huang, Quan Wang, Zhifeng Zhao, Bin Yang, Jiangpeng Wei, Xiangjie Wang, Gang Ji, Minwen Zheng
JMIR Cancer.2024;[Epub] CrossRef - Deep learning captures selective features for discrimination of microsatellite instability from pathologic tissue slides of gastric cancer
Sung Hak Lee, Yujin Lee, Hyun‐Jong Jang
International Journal of Cancer.2023; 152(2): 298. CrossRef - Novel Biomarkers of Gastric Cancer: Current Research and Future Perspectives
Yasushi Sato, Koichi Okamoto, Yutaka Kawano, Akinari Kasai, Tomoyuki Kawaguchi, Tamotsu Sagawa, Masahiro Sogabe, Hiroshi Miyamoto, Tetsuji Takayama
Journal of Clinical Medicine.2023; 12(14): 4646. CrossRef - The results of treatment for resectable gastric cancer with microsatellite instability
H. Sun, S. N. Nered, A. A. Tryakin, E. V. Artamonova, A. E. Kalinin, V. E. Bugaev, A. M. Stroganova, N. S. Besova, P. P. Arkhiri, V. I. Marshall, R. Sh. Abdulaeva, I. S. Stilidi
Pelvic Surgery and Oncology.2023; 13(2): 17. CrossRef - Heterogeneity and Adjuvant Therapeutic Approaches in MSI-H/dMMR Resectable Gastric Cancer: Emerging Trends in Immunotherapy
Hui Wu, Wenyuan Ma, Congfa Jiang, Ning Li, Xin Xu, Yongfeng Ding, Haiping Jiang
Annals of Surgical Oncology.2023; 30(13): 8572. CrossRef - Dual-layer spectral-detector CT for predicting microsatellite instability status and prognosis in locally advanced gastric cancer
Yongjian Zhu, Peng Wang, Bingzhi Wang, Zhichao Jiang, Ying Li, Jun Jiang, Yuxin Zhong, Liyan Xue, Liming Jiang
Insights into Imaging.2023;[Epub] CrossRef - Concordance between microsatellite instability testing and immunohistochemistry for mismatch repair proteins and efficient screening of mismatch repair deficient gastric cancer
Gou Yamamoto, Tetsuya Ito, Okihide Suzuki, Nao Kamae, Miho Kakuta, Akemi Takahashi, Katsuya Iuchi, Tomio Arai, Hideyuki Ishida, Kiwamu Akagi
Oncology Letters.2023;[Epub] CrossRef - Low incidence of microsatellite instability in gastric cancers and its association with the clinicopathological characteristics: a comparative study
Fateme Fooladi Talari, Ali Bozorg, Sirous Zeinali, Mohammadreza Zali, Zhale Mohsenifar, Hamid Asadzadeh Aghdaei, Kaveh Baghaei
Scientific Reports.2023;[Epub] CrossRef - Mutational separation and clinical outcomes of TP53 and CDH1 in gastric cancer
He-Li Liu, Huan Peng, Chang-Hao Huang, Hai-Yan Zhou, Jie Ge
World Journal of Gastrointestinal Surgery.2023; 15(12): 2855. CrossRef - Genomic and Immunologic Markers of Intrinsic Resistance to Pembrolizumab Monotherapy in Microsatellite Instability-High Gastric Cancer: Observations from a Prospective Phase II Study
Haibo Qiu
Global Medical Genetics.2022; 09(02): 060. CrossRef - Clinicopathological features of PD-L1 protein expression, EBV positivity, and MSI status in patients with advanced gastric and esophagogastric junction adenocarcinoma in Japan
Tsutomu Yoshida, Go Ogura, Mikiko Tanabe, Takuo Hayashi, Chiho Ohbayashi, Mizutomo Azuma, Chikara Kunisaki, Yoichi Akazawa, Soji Ozawa, Sohei Matsumoto, Takayoshi Suzuki, Akira Mitoro, Tetsu Fukunaga, Akiko Shimizu, Go Fujimoto, Takashi Yao
Cancer Biology & Therapy.2022; 23(1): 191. CrossRef - Development of Tissue-Agnostic Treatments for Patients with Cancer
Steven Lemery, Lola Fashoyin-Aje, Leigh Marcus, Sandra Casak, Julie Schneider, Marc Theoret, Paul Kluetz, Richard Pazdur, Julia A. Beaver
Annual Review of Cancer Biology.2022; 6(1): 147. CrossRef - A multicenter study on the preoperative prediction of gastric cancer microsatellite instability status based on computed tomography radiomics
Xiuqun Liang, Yinbo Wu, Ying Liu, Danping Yu, Chencui Huang, Zhi Li
Abdominal Radiology.2022; 47(6): 2036. CrossRef - Combination of AKT1 and CDH1 mutations predicts primary resistance to immunotherapy in dMMR/MSI-H gastrointestinal cancer
Zhenghang Wang, Qi Zhang, Changsong Qi, Yuezong Bai, Feilong Zhao, Hui Chen, Zhongwu Li, Xicheng Wang, Mifen Chen, Jifang Gong, Zhi Peng, Xiaotian Zhang, Jinping Cai, Shiqing Chen, Xiaochen Zhao, Lin Shen, Jian Li
Journal for ImmunoTherapy of Cancer.2022; 10(6): e004703. CrossRef - Eldest gastric cancer patient with high microsatellite instability responding to pembrolizumab
Akinobu Wakasugi, Akinori Sasaki, Risa Okamoto, Yasuaki Motomura
International Cancer Conference Journal.2022; 12(1): 59. CrossRef - Baseline lesion number as an efficacy predictive and independent prognostic factor and its joint utility with TMB for PD-1 inhibitor treatment in advanced gastric cancer
Xiao-Li Wei, Jian-Ying Xu, De-Shen Wang, Dong-Liang Chen, Chao Ren, Jia-Ning Li, Feng Wang, Feng-Hua Wang, Rui-Hua Xu
Therapeutic Advances in Medical Oncology.2021;[Epub] CrossRef - Clinical and morphological portrait of tumors with microsatellite instability
A. A. Musaelyan, V. D. Nazarov, A. S. Budnikova, S. V. Lapin, S. L. Vorobyev, V. L. Emanuel, A. A. Zakharenko, S. V. Orlov
Advances in Molecular Oncology.2021; 8(2): 52. CrossRef - How to Best Exploit Immunotherapeutics in Advanced Gastric Cancer: Between Biomarkers and Novel Cell-Based Approaches
Michele Ghidini, Angelica Petrillo, Andrea Botticelli, Dario Trapani, Alessandro Parisi, Anna La Salvia, Elham Sajjadi, Roberto Piciotti, Nicola Fusco, Shelize Khakoo
Journal of Clinical Medicine.2021; 10(7): 1412. CrossRef - Microsatellite instability in Gastric Cancer: Between lights and shadows
Elisabetta Puliga, Simona Corso, Filippo Pietrantonio, Silvia Giordano
Cancer Treatment Reviews.2021; 95: 102175. CrossRef - Impact of microsatellite status on negative lymph node count and prognostic relevance after curative gastrectomy
Zhenghao Cai, Junjun Ma, Shuchun Li, Abe Fingerhut, Jing Sun, Lu Zang, Chao Yan, Wentao Liu, Zhenggang Zhu, Minhua Zheng
Journal of Surgical Oncology.2021;[Epub] CrossRef - A greater lymph node yield is required during pathological examination in microsatellite instability-high gastric cancer
Zhenghao Cai, Haiqin Song, Abe Fingerhut, Jing Sun, Junjun Ma, Luyang Zhang, Shuchun Li, Chaoran Yu, Minhua Zheng, Lu Zang
BMC Cancer.2021;[Epub] CrossRef - Determinants of Response and Intrinsic Resistance to PD-1 Blockade in Microsatellite Instability–High Gastric Cancer
Minsuk Kwon, Minae An, Samuel J. Klempner, Hyuk Lee, Kyoung-Mee Kim, Jason K. Sa, Hee Jin Cho, Jung Yong Hong, Taehyang Lee, Yang Won Min, Tae Jun Kim, Byung-Hoon Min, Woong-Yang Park, Won Ki Kang, Kyu-Tae Kim, Seung Tae Kim, Jeeyun Lee
Cancer Discovery.2021; 11(9): 2168. CrossRef - Advanced Gastric Cancer: Current Treatment Landscape and a Future Outlook for Sequential and Personalized Guide: Swiss Expert Statement Article
Alexander R. Siebenhüner, Sara De Dosso, Daniel Helbling, Christoforos Astaras, Petr Szturz, Peter Moosmann, Stefanie Pederiva, Thomas Winder, Philippe Von Burg, Markus Borner
Oncology Research and Treatment.2021; 44(9): 485. CrossRef - High homogeneity of mismatch repair deficiency in advanced prostate cancer
Christoph Fraune, Ronald Simon, Doris Höflmayer, Katharina Möller, David Dum, Franziska Büscheck, Claudia Hube-Magg, Georgia Makrypidi-Fraune, Martina Kluth, Andrea Hinsch, Eike Burandt, Till Sebastian Clauditz, Waldemar Wilczak, Guido Sauter, Stefan Steu
Virchows Archiv.2020; 476(5): 745. CrossRef - High homogeneity of MMR deficiency in ovarian cancer
Christoph Fraune, Janina Rosebrock, Ronald Simon, Claudia Hube-Magg, Georgia Makrypidi-Fraune, Martina Kluth, Franziska Büscheck, Doris Höflmayer, Barbara Schmalfeldt, Volkmar Müller, Linn Wölber, Isabell Witzel, Peter Paluchowski, Christian Wilke, Uwe He
Gynecologic Oncology.2020; 156(3): 669. CrossRef - Molecular Classification of Gastric Cancer among Alaska Native People
Holly Martinson, Dominic Mallari, Christine Richter, Tsung-Teh Wu, James Tiesinga, Steven Alberts, Matthew Olnes
Cancers.2020; 12(1): 198. CrossRef - Tumor immune response and immunotherapy in gastric cancer
Yoonjin Kwak, An Na Seo, Hee Eun Lee, Hye Seung Lee
Journal of Pathology and Translational Medicine.2020; 54(1): 20. CrossRef - MMR deficiency in urothelial carcinoma of the bladder presents with temporal and spatial homogeneity throughout the tumor mass
Christoph Fraune, Ronald Simon, Claudia Hube-Magg, Georgia Makrypidi-Fraune, Christian Kähler, Martina Kluth, Doris Höflmayer, Franziska Büscheck, David Dum, Andreas M. Luebke, Eike Burandt, Till Sebastian Clauditz, Waldemar Wilczak, Guido Sauter, Stefan
Urologic Oncology: Seminars and Original Investigations.2020; 38(5): 488. CrossRef - MMR Deficiency is Homogeneous in Pancreatic Carcinoma and Associated with High Density of Cd8-Positive Lymphocytes
Christoph Fraune, Eike Burandt, Ronald Simon, Claudia Hube-Magg, Georgia Makrypidi-Fraune, Martina Kluth, Franziska Büscheck, Doris Höflmayer, Niclas Ch. Blessin, Tim Mandelkow, Wenchao Li, Daniel Perez, Jakob R. Izbicki, Waldemar Wilczak, Guido Sauter, J
Annals of Surgical Oncology.2020; 27(10): 3997. CrossRef - CD73's Potential as an Immunotherapy Target in Gastrointestinal Cancers
Jerry B. Harvey, Luan H. Phan, Oscar E. Villarreal, Jessica L. Bowser
Frontiers in Immunology.2020;[Epub] CrossRef - Tumor copy-number alterations predict response to immune-checkpoint-blockade in gastrointestinal cancer
Zhihao Lu, Huan Chen, Shuang Li, Jifang Gong, Jian Li, Jianling Zou, Lihong Wu, Jianing Yu, Wenbo Han, Huaibo Sun, Xi Jiao, Xiaotian Zhang, Zhi Peng, Ming Lu, Zhenghang Wang, Henghui Zhang, Lin Shen
Journal for ImmunoTherapy of Cancer.2020; 8(2): e000374. CrossRef - Protein expression-based classification of gastric cancer by immunohistochemistry of tissue microarray
Chong Zhao, Zhiqiang Feng, Hongzhen He, Dan Zang, Hong Du, Hongli Huang, Yanlei Du, Jie He, Yongjian Zhou, Yuqiang Nie, Girijesh Kumar Patel
PLOS ONE.2020; 15(10): e0238836. CrossRef - Clinicopathologic Characteristics and Long-Term Outcome of Gastric Cancer Patients with Family History: Seven-Year Follow-Up Study for Korean Health Check-Up Subjects
Jooyoung Lee, Su Jin Chung, Ji Min Choi, Yoo Min Han, Joo Sung Kim, Greger Lindberg
Gastroenterology Research and Practice.2020; 2020: 1. CrossRef - Implication of expression of MMR proteins and clinicopathological characteristics in gastric cancer
Renu Verma, Puja Sakhuja, Ritu Srivastava, Prakash Chand Sharma
Asia-Pacific Journal of Oncology.2020; : 1. CrossRef - Prognostic significance of microsatellite‐instability in gastric and gastroesophageal junction cancer patients undergoing neoadjuvant chemotherapy
Georg Martin Haag, Elena Czink, Aysel Ahadova, Thomas Schmidt, Leila Sisic, Susanne Blank, Ulrike Heger, Leonidas Apostolidis, Anne Katrin Berger, Christoph Springfeld, Felix Lasitschka, Dirk Jäger, Magnus von Knebel Doeberitz, Matthias Kloor
International Journal of Cancer.2019; 144(7): 1697. CrossRef - Serological Markers Associated With Response to Immune Checkpoint Blockade in Metastatic Gastrointestinal Tract Cancer
Zhihao Lu, Jianling Zou, Ying Hu, Shuang Li, Tao Zhou, Jifang Gong, Jian Li, Xiaotian Zhang, Jun Zhou, Ming Lu, Xicheng Wang, Zhi Peng, Changsong Qi, Yanyan Li, Jie Li, Yan Li, Jianyin Zou, Xiao Du, Henghui Zhang, Lin Shen
JAMA Network Open.2019; 2(7): e197621. CrossRef - Assessing molecular subtypes of gastric cancer: microsatellite unstable and Epstein-Barr virus subtypes. Methods for detection and clinical and pathological implications
Carolina Martinez-Ciarpaglini, Tania Fleitas-Kanonnikoff, Valentina Gambardella, Marta Llorca, Cristina Mongort, Regina Mengual, Gema Nieto, Lara Navarro, Marisol Huerta, Susana Rosello, Desamparados Roda, Noelia Tarazona, Samuel Navarro, Gloria Ribas, An
ESMO Open.2019; 4(3): e000470. CrossRef - The role of pembrolizumab in the treatment of PD-L1 expressing gastric and gastroesophageal junction adenocarcinoma
Gagandeep Brar, Manish A. Shah
Therapeutic Advances in Gastroenterology.2019;[Epub] CrossRef - Novel Biomarkers for Prediction of Response to Preoperative Systemic Therapies in Gastric Cancer
Alessandro Cavaliere, Valeria Merz, Simona Casalino, Camilla Zecchetto, Francesca Simionato, Hayley Louise Salt, Serena Contarelli, Raffaela Santoro, Davide Melisi
Journal of Gastric Cancer.2019; 19(4): 375. CrossRef - MICROSATELLITE INSTABILITY AND GASTRIC CARCINOMA. REVIEW OF THELITERATURE
D. L. Rotin, O. V. Paklina, I. O. Tin’kova, D. N. Grekov
Russian Journal of Biotherapy.2019; 18(4): 17. CrossRef - Meta-analysis of microsatellite instability in relation to clinicopathological characteristics and overall survival in gastric cancer
K Polom, L Marano, D Marrelli, R De Luca, G Roviello, V Savelli, P Tan, F Roviello
Journal of British Surgery.2018; 105(3): 159. CrossRef - Gastric poorly cohesive carcinoma: a correlative study of mutational signatures and prognostic significance based on histopathological subtypes
Chae H Kwon, Young K Kim, Sojeong Lee, Ahrong Kim, Hye J Park, Yuri Choi, Yeo J Won, Do Y Park, Gregory Y Lauwers
Histopathology.2018; 72(4): 556. CrossRef - Microsatellite instability in gastric cancer: molecular bases, clinical perspectives, and new treatment approaches
Margherita Ratti, Andrea Lampis, Jens C. Hahne, Rodolfo Passalacqua, Nicola Valeri
Cellular and Molecular Life Sciences.2018; 75(22): 4151. CrossRef - High-throughput Protein and mRNA Expression–based Classification of Gastric Cancers Can Identify Clinically Distinct Subtypes, Concordant With Recent Molecular Classifications
Sangjeong Ahn, So-Jeong Lee, Yonugkeum Kim, Ahrong Kim, Nari Shin, Kyung Un Choi, Chang-Hun Lee, Gi Yeong Huh, Kyong-Mee Kim, Namrata Setia, Gregory Y. Lauwers, Do Youn Park
American Journal of Surgical Pathology.2017; 41(1): 106. CrossRef - Molecular Testing for Gastrointestinal Cancer
Hye Seung Lee, Woo Ho Kim, Yoonjin Kwak, Jiwon Koh, Jeong Mo Bae, Kyoung-Mee Kim, Mee Soo Chang, Hye Seung Han, Joon Mee Kim, Hwal Woong Kim, Hee Kyung Chang, Young Hee Choi, Ji Y. Park, Mi Jin Gu, Min Jin Lhee, Jung Yeon Kim, Hee Sung Kim, Mee-Yon Cho
Journal of Pathology and Translational Medicine.2017; 51(2): 103. CrossRef - Molecular testing of gastrointestinal tumours
Matthew Evans, Matthew Smith, Brendan O'Sullivan, Philippe Taniere
Diagnostic Histopathology.2017; 23(10): 442. CrossRef - Gastric Carcinomas With Lymphoid Stroma
Raul S Gonzalez, Justin M M Cates, Frank Revetta, Loralee A McMahon, Kay Washington
American Journal of Clinical Pathology.2017; 148(6): 477. CrossRef - Meta-Analysis of Prognostic Role of Ki-67 Labeling Index in Gastric Carcinoma
Jung-Soo Pyo, Nae Yu Kim
The International Journal of Biological Markers.2017; 32(4): 447. CrossRef - Tissue-Agnostic Drug Development
Keith T. Flaherty, Dung T. Le, Steven Lemery
American Society of Clinical Oncology Educational Book.2017; (37): 222. CrossRef - Programmed death ligand-1 and MET co-expression is a poor prognostic factor in gastric cancers after resection
Mi Jung Kwon, Kab-Choong Kim, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Ji-Young Choe, Hye Kyung Lee, Ho Suk Kang, Kyueng-Whan Min
Oncotarget.2017; 8(47): 82399. CrossRef - Hypermutation and microsatellite instability in gastrointestinal cancers
Kizuki Yuza, Masayuki Nagahashi, Satoshi Watanabe, Kazuaki Takabe, Toshifumi Wakai
Oncotarget.2017; 8(67): 112103. CrossRef - The Emerging Role of Immunotherapy in Gastric and Esophageal Adenocarcinoma
Bruno Bockorny, Eirini Pectasides
Future Oncology.2016; 12(15): 1833. CrossRef - Expression of Mismatch Repair Proteins in Early and Advanced Gastric Cancer in Poland
Katarzyna Karpińska-Kaczmarczyk, Magdalena Lewandowska, Małgorzata Ławniczak, Andrzej Białek, Elżbieta Urasińska
Medical Science Monitor.2016; 22: 2886. CrossRef - Immunotherapy for Gastroesophageal Cancer
Emily Goode, Elizabeth Smyth
Journal of Clinical Medicine.2016; 5(10): 84. CrossRef - Lauren classification and individualized chemotherapy in gastric cancer
JUNLI MA, HONG SHEN, LINDA KAPESA, SHAN ZENG
Oncology Letters.2016; 11(5): 2959. CrossRef - High-risk and low-risk gastric cancer areas in Italy and its association with microsatellite instability
Karol Polom, Daniele Marrelli, Valeria Pascale, Giandomenico Roviello, Costantino Voglino, Henry Rho, Carla Vindigni, Mario Marini, Raffaele Macchiarelli, Franco Roviello
Journal of Cancer Research and Clinical Oncology.2016; 142(8): 1817. CrossRef - MUC2 Expression Is Correlated with Tumor Differentiation and Inhibits Tumor Invasion in Gastric Carcinomas: A Systematic Review and Meta-analysis
Jung-Soo Pyo, Jin Hee Sohn, Guhyun Kang, Dong-Hoon Kim, Kyungeun Kim, In-Gu Do, Dong Hyun Kim
Journal of Pathology and Translational Medicine.2015; 49(3): 249. CrossRef - Correlation between microsatellite instability-high phenotype and occult lymph node metastasis in gastric carcinoma
Jiwoon Choi, Soo Kyung Nam, Do Joong Park, Hwal Woong Kim, Hyung-Ho Kim, Woo Ho Kim, Hye Seung Lee
APMIS.2015; 123(3): 215. CrossRef - Clinicopathologic and molecular features associated with patient age in gastric cancer
Ji Yeon Seo, Eun Hyo Jin, Hyun Jin Jo, Hyuk Yoon, Cheol Min Shin, Young Soo Park, Nayoung Kim, Hyun Chae Jung, Dong Ho Lee
World Journal of Gastroenterology.2015; 21(22): 6905. CrossRef - Molecular classification of gastric cancer: Towards a pathway-driven targeted therapy
Ismael Riquelme, Kathleen Saavedra, Jaime A. Espinoza, Helga Weber, Patricia García, Bruno Nervi, Marcelo Garrido, Alejandro H. Corvalán, Juan Carlos Roa, Carolina Bizama
Oncotarget.2015; 6(28): 24750. CrossRef - A phylogenetic model for understanding the effect of gene duplication on cancer progression
Qin Ma, Jaxk H. Reeves, David A. Liberles, Lili Yu, Zheng Chang, Jing Zhao, Juan Cui, Ying Xu, Liang Liu
Nucleic Acids Research.2014; 42(5): 2870. CrossRef - The analysis of microsatellite instability in extracolonic gastrointestinal malignancy
Andrew S. Williams, Weei-Yuarn Huang
Pathology.2013; 45(6): 540. CrossRef
- Intestinal Subtype as a Biomarker of Response to Neoadjuvant Immunochemotherapy in Locally Advanced Gastric Adenocarcinoma: Insights from a Prospective Phase II Trial
- Expression of Multidrug Resistance Protein 1 in Human Hepatocellular Carcinoma.
- Yun Kyung Kang
- Korean J Pathol. 2011;45(3):281-289.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.3.281
- 3,800 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Multidrug resistance protein 1 (MDR1) encoded by ATP-binding cassette, sub-family B (Mdr/Tap), member 1 (ABCB1) mediates cross-resistance to antineoplastic drugs, and its expression is related to tumor aggressiveness.
METHODS
MDR1 expression was investigated in 100 hepatocellular carcinomas (HCCs) by immunohistochemical staining. The epigenetic mechanisms underlying ABCB1 transcriptional regulation were investigated in cell lines.
RESULTS
MDR1 was normally localized in the bile canalicular surface of the hepatocytes. Among 100 HCCs, 45 showed canalicular/luminal (CL) staining similar to the normal pattern, another 45 displayed membranous/cytoplasmic (MC) overexpression, and the remaining 10 revealed loss of expression. MC pattern or null staining of HCCs correlated with a higher histological grade and had a poorer prognosis than HCCs with a CL pattern (p<0.05). They also tended to have a poor prognosis by multivariate survival analysis. The ABCB1 promoter was hypomethylated regardless of MDR1 expression or ABCB1 mRNA levels in 10 HCC cell lines. Histone deacetylase inhibitor treatment induced ABCB1 upregulation in 4 cell lines with low or moderate ABCB1 levels.
CONCLUSIONS
Our findings suggest that either an increase or a loss of MDR1 expression may contribute to the poor outcome of HCCs; histone deacetylation may be one of the epigenetic mechanisms directing the ABCB1 expression in HCCs. -
Citations
Citations to this article as recorded by- Preferential expression of prostate specific membrane in CD34 labeled Neo-vasculature of Hepatocellular carcinoma: Prognostic and therapeutic potentials
Safaa MM Abd El Khalek, Mona QR Mohammed, Amira M Al Balakosy
Egyptian Journal of Pathology.2023; 43(1): 66. CrossRef
- Preferential expression of prostate specific membrane in CD34 labeled Neo-vasculature of Hepatocellular carcinoma: Prognostic and therapeutic potentials
- Prognostic Implications of the Expression of CXCL16 in Breast Carcinoma.
- Dong Youl Choi, Ran Hong, Sung Churl Lim, Keun Hong Kee, Chae Hong Suh, Mija Lee
- Korean J Pathol. 2011;45(1):15-20.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.1.15
- 4,454 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Of the many prognostic factors for breast cancer, the relationship between an infiltration of inflammatory cells and the prognosis is debatable. Of the chemokines affecting cancer's inflammatory reactions, chemokine (C-X-C motif) ligand 16 (CXCL16) has attracted attention for its prognostic value in many cancers, including colorectal cancer and renal cell carcinoma. But the situation for breast carcinoma is unknown. The aim of this study was to examine the relationship between the prognostic factors and the CXCL16 expression in patients with breast carcinoma.
METHODS
The patients (n=106) diagnosed with invasive ductal cancer of the breast were enrolled. We reviewed the clinicopathological factors of these patients, hematoxylin and eosin stains were prepared and estrogen receptor (ER), human epidermal growth factor receptor 2 (HER2/neu) and CXCL16 immunostaining was performed.
RESULTS
The ER expression was significantly correlated with age and inflammation. A CXCL16 expression was noted in 81.1% of the cases. No association was evident between a CXCL16 expression and any other parameter, including the survival rate. Multivariate analysis did not implicate ER, HER2/neu or CXCL16 as an independent prognostic factor, but the tumor size was independent predictive factor for the patient outcome.
CONCLUSIONS
An inflammatory reaction mediated by CXCL16 is not associated with the prognosis of breast cancer or any clinicopathological factors. -
Citations
Citations to this article as recorded by- The Emerging Role of CXC Chemokines And Their Receptors in Cancer
Victoria Vinader, Kamyar Afarinkia
Future Medicinal Chemistry.2012; 4(7): 853. CrossRef
- The Emerging Role of CXC Chemokines And Their Receptors in Cancer
- Expressions of the Tumor Associated Proteins and Their Correlation with the Pathologic Features in Childhood Hepatoblastoma.
- Han Seong Kim, Hyo Seop Ahn, Kwi Won Park, Ja June Jang
- Korean J Pathol. 1997;31(6):538-545.
- 1,674 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Hepatoblastoma is a rare malignant liver tumor found in children. Its biological characteristics and prognostic factors have not been well known. We investigated 29 cases of hepatoblastoma, registered in university hospitals in Seoul from 1984 to 1996. By the immunohistochemical method, p53, Waf-1 (p21), bcl-2, heat shock protein 70 (hsp70), c-jun, transforming growth factor-alpha (TGF-alpha) expressions were studied. Those data were compared with clinico-pathologic features; age, sex, tumor size, tumor stage and histologic subtypes. Expression of p53 and bcl-2 were each observed separately in single cases. Expression of c-jun was more frequently noted in patients at higher stages. Expression of TGF-alpha decreased in the order of pure fetal, mixed, embryonal and small cell anaplastic subtypes. Cumulative survival rate was lower in females than in males and in patients with a higher tumor stage. According to histologic subtypes, survival rates decreased in the order of pure fetal, mixed, embryonal and small cell anaplastic subtypes. Survival rate was lower in patients with c-jun expression. Group of TGF-alpha labelling index under 19 showed a lower survival rate than that over 19. In conclusion, we found that tumor associated proteins, c-jun and TGF-alpha, are closely related to the prognosis of hepatoblastoma but p53 and bcl-2 may not be related to it.

 E-submission
E-submission
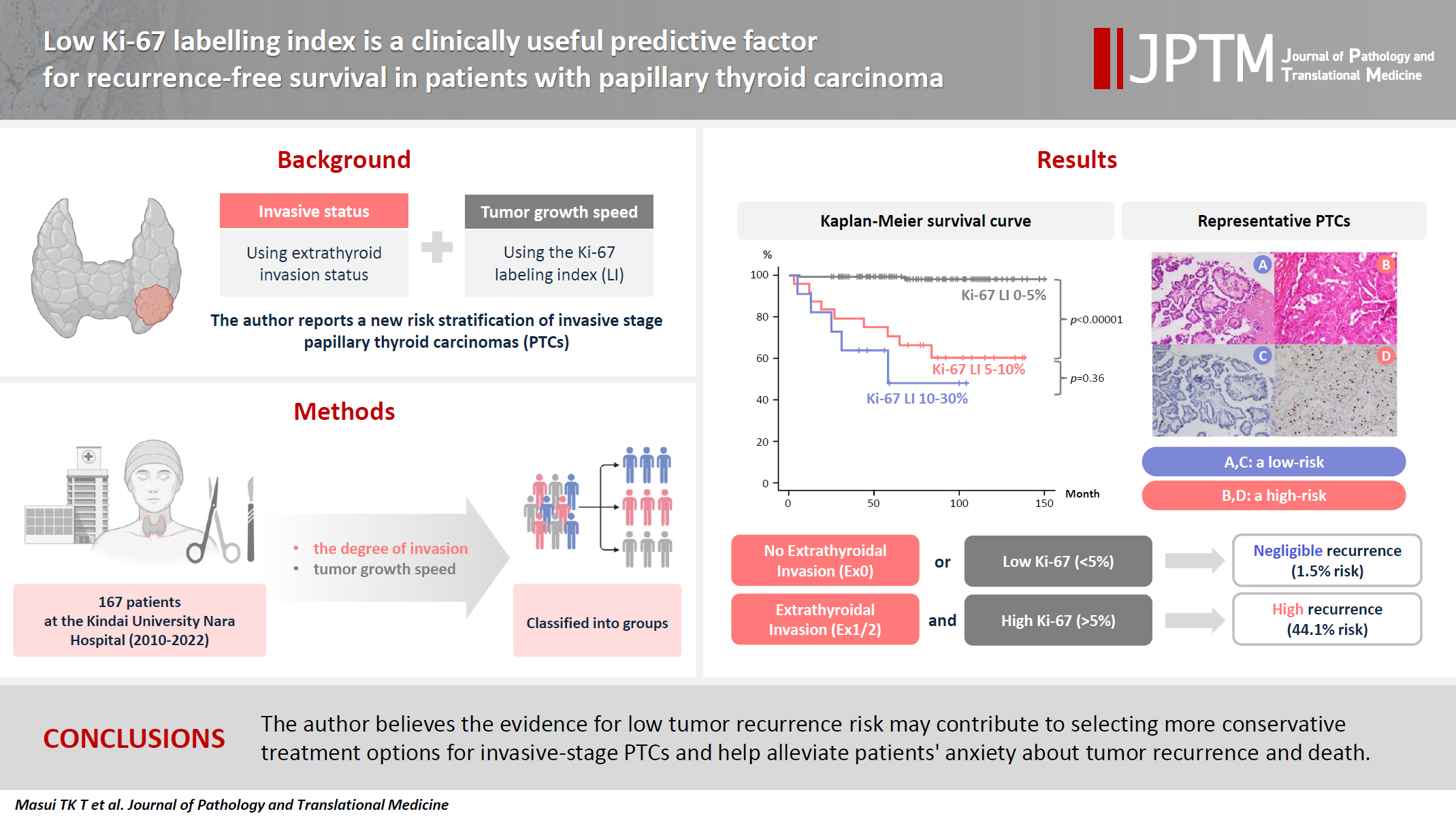




 First
First Prev
Prev



