Search
- Page Path
- HOME > Search
- Diagnostic value of cytology in detecting human papillomavirus–independent cervical malignancies: a nation-wide study in Korea
- Hye-Ra Jung, Junyoung Shin, Chong Woo Yoo, Eun Na Kim, Cheol Lee, Kyeongmin Kim, Ho-chang Lee, Yonghee Lee, Ji Hye Kim, Soo Jin Jung, Yumin Chung, Joo Yeon Kim, Hye Eun Park, Tae Hoen Kim, Wonae Lee, Min-Sun Cho, Ran Hong, Yoon Jung Choi, Younghee Choi, Young Sub Lee, Sang-Ryung Lee, Myunghee Kang, Young Jin Seo, Seung-Sook Lee, Yoon-Jung Hwang, Hyun-Jung Kim
- J Pathol Transl Med. 2025;59(6):444-452. Published online November 11, 2025
- DOI: https://doi.org/10.4132/jptm.2025.10.21
- 2,680 View
- 126 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) independent cervical malignancies (HPV-IDCMs) have recently been classified by the World Health Organization (WHO) 5th edition. These malignancies have historically received limited attention due to their rarity and the potential for evasion of HPV-based screening.
Methods
We retrospectively reviewed 5,854 biopsy-confirmed cervical malignancies from 22 institutions over 3 years (July 2020–June 2023). Histologic classification followed the WHO guidelines. HPV independence was confirmed by dual negativity for p16 and HPV; discordant cases (p16-positive/HPV-negative) underwent additional HPV testing using paraffin-embedded tissue. Cytological results were matched sequentially to histological confirmation.
Results
The prevalence of HPV-IDCM was 4.4% (257/5,854) overall and was 3.6% (208/5,805 cases) among primary cervical malignancy. Patient age of HPV-IDCM was 29 to 89 years (median, 57.79). Its histologic subtypes included primary adenocarcinoma (n = 116), endometrial adenocarcinoma (n = 35), squamous cell carcinoma (n = 72), metastatic carcinoma (n = 14), carcinoma, not otherwise specified (n = 10), neuroendocrine carcinoma (n = 3), and others (n = 7). Among 155 cytology-histological matched cases, the overall and primary Pap test detection rates were 85.2% (132/155) and 83.2% (104/125), respectively. The interval between cytology and histologic confirmation extended up to 38 months.
Conclusions
HPV-IDCMs comprised 3.6% of primary cervical malignancies with a high detection rate via cytology (83.2%). These findings affirm the value of cytological screening, particularly in patients with limited screening history or at risk for HPV-independent lesions, and may guide future screening protocols.
- Clinicopathologic characterization of cervical metastasis from an unknown primary tumor: a multicenter study in Korea
- Miseon Lee, Uiree Jo, Joon Seon Song, Youn Soo Lee, Chang Gok Woo, Dong-Hoon Kim, Jung Yeon Kim, Sun Och Yoon, Kyung-Ja Cho
- J Pathol Transl Med. 2023;57(3):166-177. Published online May 10, 2023
- DOI: https://doi.org/10.4132/jptm.2023.04.12
- 6,171 View
- 171 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Research regarding cervical metastasis from an unknown primary tumor (CUP) according to human papillomavirus (HPV) and Epstein-Barr virus (EBV) status in Korea has been sporadic and small-scale. This study aims to analyze and understand the characteristics of CUP in Korea according to viral and p16 and p53 status through a multicenter study.
Methods
Ninety-five cases of CUP retrieved from six hospitals in Korea between January 2006 and December 2016 were subjected to high-risk HPV detection (DNA in situ hybridization [ISH] or real-time polymerase chain reaction), EBV detection (ISH), and immunohistochemistry for p16 and p53.
Results
CUP was HPV-related in 37 cases (38.9%), EBV-related in five cases (5.3%), and unrelated to HPV or EBV in 46 cases (48.4%). HPV-related CUP cases had the best overall survival (OS) (p = .004). According to the multivariate analysis, virus-unrelated disease (p = .023) and longer smoking duration (p < .005) were prognostic factors for poor OS. Cystic change (p = .016) and basaloid pattern (p < .001) were more frequent in HPV-related cases, and lymphoepithelial lesion was frequent in EBV-related cases (p = .010). There was no significant association between viral status and p53 positivity (p = .341), smoking status (p = .728), or smoking duration (p = .187). Korean data differ from Western data in the absence of an association among HPV, p53 positivity, and smoking history.
Conclusions
Virus-unrelated CUP in Korea had the highest frequency among all CUP cases. HPV-related CUP is similar to HPV-mediated oropharyngeal cancer and EBVrelated CUP is similar to nasopharyngeal cancer in terms of characteristics, respectively. -
Citations
Citations to this article as recorded by- Differenzierung von benignen und malignen Halszysten – eine diagnostische Herausforderung
Christina Sauter, Matthias Sand, Karim Plath, Michaela Maria Plath
Laryngo-Rhino-Otologie.2025; 104(05): 296. CrossRef - Unlocking the Hidden: Advancing Imaging Techniques in Diagnosing Cancers of Unknown Primary in the Head and Neck Region
Daniela Messineo, Filippo Valentini, Giovanni Francesco Niccolini, Federica Zoccali, Francesca Ripari, Enrico Marotta, Marcello Caratozzolo, Pasquale Frisina
Applied Sciences.2025; 15(4): 2194. CrossRef - Characterization of undifferentiated carcinoma of the salivary gland: clinicopathological and immunohistochemical analyses in comparison with lymphoepithelial carcinoma
Sangjoon Choi, Gyuheon Choi, Hee Jin Lee, Joon Seon Song, Yoon Se Lee, Seung-Ho Choi, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2025; 59(6): 361. CrossRef - Management of squamous cell carcinoma of unknown primary in the head and neck: current evidence-based diagnostic and treatment strategies
Marcel Kloppenburg, Matthias Santer, Lukas Schmutzler, Felix Johnson, Benedikt Hofauer, Teresa Steinbichler
memo - Magazine of European Medical Oncology.2025;[Epub] CrossRef - Expansion of tumor-infiltrating lymphocytes from head and neck squamous cell carcinoma to assess the potential of adoptive cell therapy
Sangjoon Choi, Mofazzal Hossain, Hyun Lee, Jina Baek, Hye Seon Park, Chae-Lyul Lim, DoYeon Han, Taehyun Park, Jong Hyeok Kim, Gyungyub Gong, Mi-Na Kweon, Hee Jin Lee
Cancer Immunology, Immunotherapy.2024;[Epub] CrossRef
- Differenzierung von benignen und malignen Halszysten – eine diagnostische Herausforderung
- Evaluation of the characteristics of multiple human papillomavirus (HPV) infections identified using the BD Onclarity HPV assay and comparison with those of single HPV infection
- Jinhee Kim, Moonsik Kim, Ji Young Park
- J Pathol Transl Med. 2022;56(5):289-293. Published online September 13, 2022
- DOI: https://doi.org/10.4132/jptm.2022.08.02
- 7,908 View
- 137 Download
- 10 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Human papillomavirus (HPV) infection is a major cause of cervical cancer and associated precursor lesions. Multiple HPV genotype infections have been reported. However, their clinicopathological characteristics still remain elusive.
Methods
For this study, 814 consecutive patients who had undergone colposcopy and HPV genotyping test using BD Onclarity HPV assay were retrospectively selected. Clinicopathological parameters of multiple HPV infections were compared with those of single HPV infection.
Results
Multiple HPV infections were found in 110 out of 814 cases (13.5%). Multiple HPV infections were associated with a significantly higher incidence of high-grade intraepithelial lesions (HSILs) compared with single HPV infection. Other high-risk HPV genotypes, in addition to HPV 16, were found more frequently in the multiple HPV infections group; these included HPV 51, 52, 33/58, 56/59/66, and 35/39/68. No specific coinfection pattern was not identified. Additionally, the number of HPV genotypes in multiple HPV infections was not associated with the progression to HSIL or squamous cell carcinoma.
Conclusions
Multiple HPV infections have distinct clinicopathological characteristics (compared with single HPV infection). As their biological behavior is uncertain, close and frequent follow-up is warranted. -
Citations
Citations to this article as recorded by- The Prevalence of Multi-Type Infections Among Human Papillomavirus Types in Korean Women
Jang Mook Kim, Hee Seung Song, Jieun Hwang, Jae Kyung Kim
Pathogens.2025; 14(4): 369. CrossRef - Multiple high-risk human papillomavirus infections exacerbate cervical lesion risk: epidemiological evidence from suining, Sichuan
Yaling Jing, Jianhui Chen, Fang Lin, Xiaonan Huang, Yulin Liu, Mingcai Zhao, Chuan Ye, Lianfang Zhao, Xiaofang Liu, Jiayan Yang
Virology Journal.2025;[Epub] CrossRef - The cervical cancer related distribution, coinfection and risk of 15 HPV types in Baoan, Shenzhen, in 2017–2023
Rukai Li, Weiwei Meng, Yunhai Zuo, Yanli Xu, Shaonan Wu
Virology Journal.2024;[Epub] CrossRef - Molecular findings and virological assessment of bladder papillomavirus infection in cattle
Francesca De Falco, Anna Cutarelli, Francesca Luisa Fedele, Cornel Catoi, Sante Roperto
Veterinary Quarterly.2024; 44(1): 1. CrossRef - Patterns of single and multiple HPV infections in female: A systematic review and meta-analysis
Dan Zhou, Jing Xue, Yaqiong Sun, Liling Zhu, Ming Zhao, Meimei Cui, Min Zhang, Jingjing Jia, Limei Luo
Heliyon.2024; 10(17): e35736. CrossRef - Age distribution of patients with multiple High-Risk Human Papilloma Virus (HR-HPV) genotypes and HPV vaccine recommendations by age
Gülçin Çetin Uysal, Nil Tekin
Family Practice and Palliative Care.2024; 9(3): 80. CrossRef - Relative distribution of HPV genotypes in histological cervical samples and associated grade lesion in a women population over the last 16 years in Burgundy, France
Christelle Auvray, Serge Douvier, Odile Caritey, Jean-Baptiste Bour, Catherine Manoha
Frontiers in Medicine.2023;[Epub] CrossRef - Epidemiologic characteristics of high-risk HPV and the correlation between multiple infections and cervical lesions
Qinli Luo, Xianghua Zeng, Hanyi Luo, Ling Pan, Ying Huang, Haiyan Zhang, Na Han
BMC Infectious Diseases.2023;[Epub] CrossRef
- The Prevalence of Multi-Type Infections Among Human Papillomavirus Types in Korean Women
- Evaluation of human papillomavirus (HPV) prediction using the International Endocervical Adenocarcinoma Criteria and Classification system, compared to p16 immunohistochemistry and HPV RNA in-situ hybridization
- Hezhen Ren, Jennifer Pors, Christine Chow, Monica Ta, Simona Stolnicu, Robert Soslow, David Huntsman, Lynn Hoang
- J Pathol Transl Med. 2020;54(6):480-488. Published online August 31, 2020
- DOI: https://doi.org/10.4132/jptm.2020.07.18
- 8,426 View
- 175 Download
- 11 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The International Endocervical Adenocarcinoma Criteria and Classification (IECC) separated endocervical adenocarcinomas into human papillomavirus (HPV) associated (HPVA) and non–HPV-associated (NHPVA) categories by morphology alone. Our primary objective was to assess the accuracy of HPV prediction by the IECC system compared to p16 immunohistochemistry and HPV RNA in-situ hybridization (RISH). Our secondary goal was to directly compare p16 and HPV RISH concordance.
Methods
Cases were classified by IECC and stained for p16 and HPV RISH on tissue microarray, with discordant p16/HPV RISH cases re-stained on whole tissue sections. Remaining discordant cases (p16/HPV, IECC/p16, IECC/HPV discordances) were re-reviewed by the original pathologists (n = 3) and external expert pathologists (n = 2) blinded to the p16 and HPV RISH results. Final IECC diagnosis was assigned upon independent agreement between all reviewers.
Results
One hundred and eleven endocervical adenocarcinomas were classified originally into 94 HPVA and 17 NHPVA cases. p16 and HPV RISH was concordant in 108/111 cases (97%) independent of the IECC. HPV RISH and p16 was concordant with IECC in 103/111 (93%) and 106/111 (95%), respectively. After expert review, concordance improved to 107/111 (96%) for HPV RISH. After review of the eight discordant cases, one remained as HPVA, four were reclassified to NHPVA from HPVA, two were unclassifiable, and one possibly represented a mixed usual and gastric-type adenocarcinoma.
Conclusions
p16 and HPV RISH have excellent concordance in endocervical adenocarcinomas, and IECC can predict HPV status in most cases. Focal apical mitoses and apoptotic debris on original review led to the misclassification of several NHPVA as HPVA. -
Citations
Citations to this article as recorded by- EdgeNeXt-SEDP for cervical adenocarcinoma HPV-associated and non-HPV-associated diagnosis and decision support
Qi Chen, Hao Wang, Hao Zhang, Zhenkun Zhu, Xi Wei
Life Sciences.2025; 380: 123931. CrossRef - Cytology and histology of endocervical glandular lesions: a review with emphasis on recent developments
Natalie Banet, Karen L. Talia
Pathology.2025; 57(7): 817. CrossRef - Role of human papillomavirus status in the classification, diagnosis, and prognosis of malignant cervical epithelial tumors and precursor lesions
Simona Stolnicu
Die Pathologie.2025;[Epub] CrossRef - Joint detection of multiple HPV-testing technologies and evaluation of clinicopathological characteristics discriminate between HPV-independent and low-copy HPV-associated cervical squamous cell carcinoma (CSCC) -an analysis of 3869 cases
Linghui Lu, Tianqi Liu, Shunni Wang, Jing Li, Feiran Zhang, Yan Ning, Yiqin Wang
Gynecologic Oncology.2023; 170: 59. CrossRef - Incidence and Clinicopathologic Characteristics of Human Papillomavirus–independent Invasive Squamous Cell Carcinomas of the Cervix
Simona Stolnicu, Douglas Allison, Aaron M. Praiss, Basile Tessier-Cloutier, Amir Momeni Boroujeni, Jessica Flynn, Alexia Iasonos, Rene Serrette, Lien Hoang, Andrei Patrichi, Cristina Terinte, Anna Pesci, Claudia Mateoiu, Ricardo R. Lastra, Takako Kiyokawa
American Journal of Surgical Pathology.2023; 47(12): 1376. CrossRef - Testing Algorithms for the Diagnosis of Malignant Glandular Tumors of the Uterine Cervix Histotyped per the International Endocervical Adenocarcinoma Criteria and Classification (IECC) System
Máire A. Duggan, Qiuli Duan, Ruth M. Pfeiffer, Mary Anne Brett, Sandra Lee, Mustapha Abubakar, Martin Köbel, Monica Rodriguez, Aylin Sar
Applied Immunohistochemistry & Molecular Morphology.2022; 30(2): 91. CrossRef - Local and Metastatic Relapses in a Young Woman with Papillary Squamous Cell Carcinoma of the Uterine Cervix
Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(3): 599. CrossRef - Clinical correlation of lymphovascular invasion and Silva pattern of invasion in early-stage endocervical adenocarcinoma: proposed binary Silva classification system
Simona Stolnicu, Lien Hoang, Noorah Almadani, Louise De Brot, Glauco Baiocchi, Graziele Bovolim, Maria Jose Brito, Georgia Karpathiou, Antonio Ieni, Esther Guerra, Takako Kiyokawa, Pavel Dundr, Carlos Parra-Herran, Sofia Lérias, Ana Felix, Andres Roma, An
Pathology.2022; 54(5): 548. CrossRef - Reproducibility of Morphologic Parameters of the International Endocervical Adenocarcinoma Criteria and Classification System and Correlation With Clinicopathologic Parameters: A Multi-Institutional Study
Pinar Bulutay, Nihan Haberal, Özlem Özen, Özlem Erdem, Emine H. Zeren, İbrahim Kulac, Çagatay Taskiran, Dogan Vatansever, Ali Ayhan, Nilgün Kapucuoğlu
International Journal of Gynecological Pathology.2022; 41(5): 447. CrossRef - HPV-Negative Cervical Cancer: A Narrative Review
Francesca Arezzo, Gennaro Cormio, Vera Loizzi, Gerardo Cazzato, Viviana Cataldo, Claudio Lombardi, Giuseppe Ingravallo, Leonardo Resta, Ettore Cicinelli
Diagnostics.2021; 11(6): 952. CrossRef - International Endocervical Adenocarcinoma Criteria and Classification (IECC): An Independent Cohort With Clinical and Molecular Findings
Hezhen Ren, Noorah Almadani, Jennifer Pors, Samuel Leung, Julie Ho, Christine Chow, Monica Ta, Kay J. Park, Simona Stolnicu, Robert Soslow, David Huntsman, Blake C. Gilks, Lynn Hoang
International Journal of Gynecological Pathology.2021; 40(6): 533. CrossRef
- EdgeNeXt-SEDP for cervical adenocarcinoma HPV-associated and non-HPV-associated diagnosis and decision support
- Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
- Yuil Kim, Young-Hoon Joo, Min-Sik Kim, Youn Soo Lee
- J Pathol Transl Med. 2020;54(5):411-418. Published online July 21, 2020
- DOI: https://doi.org/10.4132/jptm.2020.06.22
- 12,161 View
- 188 Download
- 23 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
High-risk (HR) human papillomavirus (HPV) is found in a subset of head and neck (HN) squamous cell carcinomas (SCCs). For oropharyngeal SCCs, HR HPV positivity is known to be associated with good prognosis, and a separate staging system for HPV-associated carcinomas using p16 immunohistochemistry (IHC) as a surrogate test has been adopted in the 8th American Joint Committee on Cancer staging system. We examined the HR HPV status and the genotype distribution in five HN subsites.
Methods
Formalin-fixed paraffin-embedded tissue sections were used for p16 IHC and DNA extraction. HPV DNA detection and genotyping were done employing either a DNA chip-based or real-time polymerase chain reaction–based method.
Results
During 2011–2019, a total of 466 SCCs were tested for HPV DNA with 34.1% positivity for HR HPV. Among HN subsites, the oropharynx showed the highest HR HPV prevalence (149/205, 75.1%), followed by the sinonasal tract (3/14, 21.4%), larynx (5/43, 11.6%), hypopharynx (1/38, 2.6%), and oral cavity (1/166, 0.6%). The most common HPV genotype was HPV16 (84.3%) followed by HPV35 (6.9%) and HPV33 (4.4%). Compared with HR HPV status, the sensitivity and specificity of p16 IHC were 98.6% and 94.3% for the oropharynx, and 99.2% and 93.8% for the tonsil, respectively.
Conclusions
Using a Korean dataset, we confirmed that HR HPV is most frequently detected in oropharyngeal SCCs. p16 positivity showed a good concordance with HR HPV DNA for oropharyngeal and especially tonsillar carcinomas. The use of p16 IHC may further be extended to predict HR HPV positivity in sinonasal tract SCCs. -
Citations
Citations to this article as recorded by- Impact of histopathological parameters in prognosis of oral squamous cell carcinoma
R. P. Ekanayaka, W. M. Tilakaratne
Oral Diseases.2025; 31(5): 1420. CrossRef - Prevalence of human papilloma virus in head and neck mucous squamous cell carcinoma and genotypes by location: an observational study
Emilie Uhlrich, Jerzy Klijanienko, Joey Martin, Emmanuelle Jeannot, Anne Vincent-Salomon, Paul Freneaux, Christophe Le Tourneau, Olivier Choussy, Antoine Dubray-Vautrin
European Journal of Cancer Prevention.2025; 34(5): 426. CrossRef - Risk factors for cervical lymph node metastasis in oropharyngeal cancer and its impact on prognosis
Li Zhang, Zhilin Li, Jing Wang, Chen Wang, Shuxin Wen
Brazilian Journal of Otorhinolaryngology.2025; 91(2): 101520. CrossRef - Co-infection of human papillomavirus genotypes and Epstein-Barr virus in tumors of the oral cavity and oropharynx: a retrospective study in Northeastern Mexico
Gerardo del Carmen Palacios-Saucedo, Jose Manuel Vazquez-Guillen, Alondra Yamileth Alanis-Valdez, Leticia Lizeth Valdez-Treviño, Luis Roberto Galindo-Mendez, Angel Zavala-Pompa, Lydia Guadalupe Rivera-Morales, Ana Carolina Martinez-Torres, Roberto Lopez-V
IJID Regions.2025; 14: 100555. CrossRef - Rates of p16 and p53 expression in head and neck cutaneous squamous cell carcinoma vary according to human papillomavirus status
Rachid Ait Addi
World Journal of Clinical Cases.2025;[Epub] CrossRef - The epidemiological trends and survival of HPV-related oropharyngeal cancer other than tonsils and base of tongue − a systematic review and meta-analysis
Anas Mohammad Al Fadel, Kathrine Kronberg Jakobsen, Lasse Holmgaard Jensen, Amanda-Louise Fenger Carlander, Christian Grønhøj, Christian von Buchwald
Oral Oncology.2025; 165: 107311. CrossRef - Oropharyngeal Helicobacter pylori colonization increases risk and worsens prognosis of head and neck squamous cell carcinoma
Xianyao Jiang, Yongjin Huang, Changwu Li, Hongyan Jiang
Scientific Reports.2025;[Epub] CrossRef - Characteristics of human papillomavirus infection among oropharyngeal cancer patients: A systematic review and meta-analysis
Meimei Cui, Jinling Cheng, Huijuan Cheng, Ming Zhao, Dan Zhou, Min Zhang, Jingjing Jia, Limei Luo
Archives of Oral Biology.2024; 157: 105830. CrossRef - Longitudinal Screening for Oral High-Risk Non-HPV16 and Non-HPV18 Strains of Human Papillomavirus Reveals Increasing Prevalence among Adult and Pediatric Biorepository Samples: A Pilot Study
Jordan Jacobs, Eugene Chon, Karl Kingsley
Vaccines.2024; 12(8): 895. CrossRef - Position Statement about Gender-Neutral HPV Vaccination in Korea
Kyung-Jin Min, Yung-Taek Ouh, Sangrak Bae, Yong-Bae Ji, Jae-Kwan Lee, Jae-Weon Kim, Kwang-Jae Cho, Dong-Hun Im
Vaccines.2024; 12(10): 1110. CrossRef - High-risk HPV Does not Appear to be an Important Risk Factor for Sinonasal Carcinomas in Turkish Population: A Tertiary Center Experience
Evsen Apaydin Arikan, Levent Aydemir, Murat Ulusan, Dilek Yilmazbayhan, Yasemin Ozluk
International Journal of Surgical Pathology.2023; 31(2): 124. CrossRef - Practical Application of Circulating Tumor-Related DNA of Human Papillomavirus in Liquid Biopsy to Evaluate the Molecular Response in Patients with Oropharyngeal Cancer
Agnieszka M. Mazurek, Tomasz W. Rutkowski
Cancers.2023; 15(4): 1047. CrossRef - The Prevalence of HPV in Oral Cavity Squamous Cell Carcinoma
Seyed Keybud Katirachi, Mathias Peter Grønlund, Kathrine Kronberg Jakobsen, Christian Grønhøj, Christian von Buchwald
Viruses.2023; 15(2): 451. CrossRef - The Protective Role of Cranberries and Blueberries in Oral Cancer
César Esquivel-Chirino, Mario Augusto Bolaños-Carrillo, Daniela Carmona-Ruiz, Ambar Lopéz-Macay, Fernando Hernández-Sánchez, Delina Montés-Sánchez, Montserrat Escuadra-Landeros, Luis Alberto Gaitán-Cepeda, Silvia Maldonado-Frías, Beatriz Raquel Yáñez-Ocam
Plants.2023; 12(12): 2330. CrossRef - Unusual cases of sinonasal malignancies: a letter to the editor on HPV-positive sinonasal squamous cell carcinomas
Benedicte Bitsch Lauritzen, Sannia Sjöstedt, Jakob Myllerup Jensen, Katalin Kiss, Christian von Buchwald
Acta Oncologica.2023; 62(6): 608. CrossRef - Prevalence of human Papillomavirus associated oropharyngeal and oral squamous cell carcinoma in Asian countries: A systematic review and large-scale meta-analysis
Yy Jean Tan, Ken Wong Siong Hou, Galvin Sim Siang Lin, Jasmine Lim Suk Wun, Wan Nor Amira Wan Ahmad Abdul Nasir, Lynn Wei Linn Ko
Acta Marisiensis - Seria Medica.2023; 69(2): 77. CrossRef - Top 100 most cited articles on human papillomavirus-induced head and neck squamous cell carcinoma: A bibliographic review
Rahul Mohandas, Subhashree Mohapatra, Mary Oshin, ShubhangiSambhaji Hajare
Journal of International Oral Health.2023; 15(3): 219. CrossRef - Intracellular Toll-Like Receptors Modulate Adaptive Immune Responses in Head and Neck Cancer
Sangeetha K. Nayanar, Deepak Roshan V.G., Shruthi Surendran, Göran Kjeller, Bengt Hasséus, Daniel Giglio
Viral Immunology.2023; 36(10): 659. CrossRef - Positive Rate of Human Papillomavirus and Its Trend in Head and Neck Cancer in South Korea
Hyun Woong Jun, Yong Bae Ji, Chang Myeon Song, Jae Kyung Myung, Hae Jin Park, Kyung Tae
Frontiers in Surgery.2022;[Epub] CrossRef - Transcriptionally active HPV in OPMD and OSCC: A systematic review following the CAP/ASCO guidelines
Laura Borges Kirschnick, Lauren Frenzel Schuch, Maria Eduarda Pérez‐de‐Oliveira, Ana Gabriela Costa Normando, Bruno Augusto Linhares Almeida Mariz, Eliete Neves Silva Guerra, Felipe Martins Silveira, Ana Carolina Uchoa Vasconcelos, Luciana Estevam Simonat
Oral Diseases.2022; 28(8): 2309. CrossRef - Effect of National Oral Health Screening Program on the Risk of Head and Neck Cancer: A Korean National Population-Based
Chan Woo Wee, Hyo-Jung Lee, Jae-Ryun Lee, Hyejin Lee, Min-Jeong Kwoen, Woo-Jin Jeong, Keun-Yong Eom
Cancer Research and Treatment.2022; 54(3): 709. CrossRef - Expression of p16, p53, and TLR9 in HPV-Associated Head and Neck Squamous Cell Carcinoma: Clinicopathological Correlations and Potential Prognostic Significance
Shu Wang, Xibing Zhuang, Caixia Gao, Tiankui Qiao
OncoTargets and Therapy.2021; Volume 14: 867. CrossRef - The Role of Human Papilloma Virus in Dictating Outcomes in Head and Neck Squamous Cell Carcinoma
Shane Brennan, Anne-Marie Baird, Esther O’Regan, Orla Sheils
Frontiers in Molecular Biosciences.2021;[Epub] CrossRef - A Contemporary Systematic Review on Repartition of HPV-Positivity in Oropharyngeal Cancer Worldwide
Amanda F. Carlander, Kathrine K. Jakobsen, Simone K. Bendtsen, Martin Garset-Zamani, Charlotte D. Lynggaard, Jakob Schmidt Jensen, Christian Grønhøj, Christian von Buchwald
Viruses.2021; 13(7): 1326. CrossRef - The Prevalence of High- and Low-Risk Types of HPV in Patients with Squamous Cell Carcinoma of the Head and Neck, Patients with Chronic Tonsillitis, and Healthy Individuals Living in Poland
Joanna Katarzyna Strzelczyk, Krzysztof Biernacki, Jadwiga Gaździcka, Elżbieta Chełmecka, Katarzyna Miśkiewicz-Orczyk, Natalia Zięba, Janusz Strzelczyk, Maciej Misiołek
Diagnostics.2021; 11(12): 2180. CrossRef
- Impact of histopathological parameters in prognosis of oral squamous cell carcinoma
- Comparison of papanicolaou smear and human papillomavirus (HPV) test as cervical screening tools: can we rely on HPV test alone as a screening method? An 11-year retrospective experience at a single institution
- Myunghee Kang, Seung Yeon Ha, Hyun Yee Cho, Dong Hae Chung, Na Rae Kim, Jungsuk An, Sangho Lee, Jae Yeon Seok, Juhyeon Jeong
- J Pathol Transl Med. 2020;54(1):112-118. Published online January 15, 2020
- DOI: https://doi.org/10.4132/jptm.2019.11.29
- 14,130 View
- 267 Download
- 20 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The decrease in incidence of cervical dysplasia and carcinoma has not been as dramatic as expected with the development of improved research tools and test methods. The human papillomavirus (HPV) test alone has been suggested for screening in some countries. The National Cancer Screening Project in Korea has applied Papanicolaou smears (Pap smears) as the screening method for cervical dysplasia and carcinoma. We evaluated the value of Pap smear and HPV testing as diagnostic screening tools in a single institution.
Methods
Patients co-tested with HPV test and Pap smear simultaneously or within one month of each other were included in this study. Patients with only punch biopsy results were excluded because of sampling errors. A total of 999 cases were included, and the collected reports encompassed results of smear cytology, HPV subtypes, and histologic examinations.
Results
Sensitivity and specificity of detecting high-grade squamous intraepithelial lesion (HSIL) and squamous cell carcinoma (SCC) were higher for Pap smears than for HPV tests (sensitivity, 97.14%; specificity, 85.58% for Pap smears; sensitivity, 88.32%; specificity, 54.92% for HPV tests). HPV tests and Pap smears did not differ greatly in detection of low-grade squamous intraepithelial lesion (85.35% for HPV test, 80.31% for Pap smears). When atypical glandular cells were noted on Pap smears, the likelihood for histologic diagnosis of adenocarcinoma following Pap smear was higher than that of high-risk HPV test results (18.8 and 1.53, respectively).
Conclusions
Pap smears were more useful than HPV tests in the diagnosis of HSIL, SCC, and glandular lesions. -
Citations
Citations to this article as recorded by- Development of a Nano-Real-Time Polymerase Chain Reaction (RT-PCR) Kit for Detection and Genotyping of High-Risk Human Papillomavirus (HPV) Strains Using Dedicated TaqMan Probes
Mohammad Panji, Mohammad Hossein Modarresi, Zahra Azizi, Moloud Absalan, Elahe Motevaseli
Cureus.2026;[Epub] CrossRef - Detection of cervical precancerous lesions and cancer by small-scale RT-qPCR analysis of oppositely deregulated mRNAs pairs in cytological smears
Anastasia A. Artyukh, Mikhail K. Ivanov, Sergei E. Titov, Victoria V. Dzyubenko, Sergey E. Krasilnikov, Anastasia O. Shumeikina, Nikita A. Afanasev, Anastasia V. Malek, Sergei A. Glushkov, Eduard F. Agletdinov
Frontiers in Oncology.2025;[Epub] CrossRef - High burden of abnormal cervical smears in South African primary health care: health programmes implications
Olufemi B Omole, Joel M Francis, John M Musonda, Pumla P Sodo, Elizabeth Reji, Nyundu S J Phukuta, Honey L M Mabuza, Joyce S Musonda, Jimmy Akii, John V Ndimande, Olalekan A Ayo-Yusuf
Health Promotion International.2025;[Epub] CrossRef - Bibliometric analysis: a study of the microenvironment in cervical cancer (2000-2024)
Yun-Tao Zhang, Yan-Ni Wei, Chen-Chen Liu, Mai-Qing Yang
Frontiers in Oncology.2025;[Epub] CrossRef - Liquid biopsy biomarkers in cervical cancer: A systematic review and meta-analysis
Isaac Kinyua Njangiru, Bizhar Ahmed Tayeb, Hazhmat Ali, Rafl M. Kamil
The Journal of Liquid Biopsy.2025; 10: 100328. CrossRef - Diagnostic Utility of Human Papilloma Virus Testing in Comparison with Pap Cytology and Histopathology in Unvaccinated Women with Cervical High-Grade Dysplasia and Carcinoma in Botswana
Patricia Setsile Rantshabeng, Nametso Dire, Andrew Khulekani Ndlovu, Ishmael Kasvosve
Venereology.2025; 4(4): 15. CrossRef - Challenges in the diagmosis of cervical pathologies
D. Y. Chernov, O. A. Tikhonovskaya, S. V. Logvinov, I. A. Petrov, Y. S. Yuriev, A. A. Zhdankina, A. V. Gerasimov, I. V. Zingalyuk, G. A. Mikheenko
Bulletin of Siberian Medicine.2024; 22(4): 201. CrossRef - “Barriers and Advantages of Self-Sampling Tests, for HPV Diagnosis: A Qualitative Field Experience Before Implementation in a Rural Community in Ecuador”
Bernardo Vega-Crespo, Vivian Alejandra Neira, Ruth Maldonado - Rengel, Diana López, Dayanara Delgado-López, Gabriela Guerra Astudillo, Veronique Verhoeven
International Journal of Women's Health.2024; Volume 16: 947. CrossRef - Cervical Human Papillomavirus Testing
Carol N. Rizkalla, Eric C. Huang
Surgical Pathology Clinics.2024; 17(3): 431. CrossRef - Segmentation of Overlapping Cells in Cervical Cytology Images: A Survey
E Chen, Hua-Nong Ting, Joon Huang Chuah, Jun Zhao
IEEE Access.2024; 12: 114170. CrossRef - Knowledge and awareness regarding pap test and HPV typing for cervical cancer screening in Edo North, Nigeria
Amina Momodu, Johnsolomon Eghosa Ohenhen, Godfrey Innocent Iyare, Musa Abidemi Muhibi, Godwin Avwioro
Discover Public Health.2024;[Epub] CrossRef - Colposcopy Value in Young Child-bearing Women: Is New Recommendations Necessary?
Fahimeh Sabet, Avishan Aminizad, Fariba Behnamfar, Tajossadat Allameh, Seyedeh Ghazal Shahrokh, Rostami Koushan, Amirmohammad Taravati, Leila Mousavi Seresht
Advanced Biomedical Research.2024;[Epub] CrossRef - Selection of endogenous control and identification of significant microRNA deregulations in cervical cancer
T. Stverakova, I. Baranova, P. Mikyskova, B. Gajdosova, H. Vosmikova, J. Laco, V. Palicka, H. Parova
Frontiers in Oncology.2023;[Epub] CrossRef - Cytology Versus Molecular Diagnosis of HPV for Cervical Cancer Screening. Comparison of the Diagnostic Properties of Four Tests in a Rural Community of Cuenca Ecuador
Bernardo Vega Crespo, Vivian Alejandra Neira, Rocío Murillo, Cristina Ochoa Avilés
ESPOCH Congresses: The Ecuadorian Journal of S.T.E.A.M..2023; 3(1): 139. CrossRef - Attitudes towards prevention of cervical cancer and early diagnosis among female academicians
Nurhan Doğan, Gamze Fışkın
Journal of Obstetrics and Gynaecology Research.2022; 48(6): 1433. CrossRef - Role of Self-Sampling for Cervical Cancer Screening: Diagnostic Test Properties of Three Tests for the Diagnosis of HPV in Rural Communities of Cuenca, Ecuador
Bernardo Vega Crespo, Vivian Alejandra Neira, José Ortíz Segarra, Ruth Maldonado Rengel, Diana López, María Paz Orellana, Andrea Gómez, María José Vicuña, Jorge Mejía, Ina Benoy, Tesifón Parrón Carreño, Veronique Verhoeven
International Journal of Environmental Research and Public Health.2022; 19(8): 4619. CrossRef - Utility of Scoring System for Screening and Early Warning of Cervical Cancer Based on Big Data Analysis
Dan Hou, Binjie Yang, Yangdan Li, Ming Sun
Frontiers in Public Health.2022;[Epub] CrossRef - Evaluation of Urine and Vaginal Self-Sampling versus Clinician-Based Sampling for Cervical Cancer Screening: A Field Comparison of the Acceptability of Three Sampling Tests in a Rural Community of Cuenca, Ecuador
Bernardo Vega Crespo, Vivian Alejandra Neira, José Ortíz S, Ruth Maldonado-Rengel, Diana López, Andrea Gómez, María José Vicuña, Jorge Mejía, Ina Benoy, Tesifón Parrón Carreño, Veronique Verhoeven
Healthcare.2022; 10(9): 1614. CrossRef - Diagnostic distribution and pitfalls of glandular abnormalities in cervical cytology: a 25-year single-center study
Jung-A Sung, Ilias P. Nikas, Haeryoung Kim, Han Suk Ryu, Cheol Lee
Journal of Pathology and Translational Medicine.2022; 56(6): 354. CrossRef - Primary screening of cervical cancer by Pap smear in women of reproductive age group
Ruchi Mishra, Dakshina Bisht, Manisha Gupta
Journal of Family Medicine and Primary Care.2022; 11(9): 5327. CrossRef - Comparison of Learning Transfer Using Simulation Problem-Based Learning and Demonstration: An Application of Papanicolaou Smear Nursing Education
Jeongim Lee, Hae Kyoung Son
International Journal of Environmental Research and Public Health.2021; 18(4): 1765. CrossRef - Investigating host-virus interaction mechanism and phylogenetic analysis of viral proteins involved in the pathogenesis
Ahmad Abu Turab Naqvi, Farah Anjum, Alaa Shafie, Sufian Badar, Abdelbaset Mohamed Elasbali, Dharmendra Kumar Yadav, Md. Imtaiyaz Hassan, Timir Tripathi
PLOS ONE.2021; 16(12): e0261497. CrossRef - Utility of Human Papillomavirus Testing for Cervical Cancer Screening in Korea
Mee-seon Kim, Eun Hee Lee, Moon-il Park, Jae Seok Lee, Kisu Kim, Mee Sook Roh, Hyoun Wook Lee
International Journal of Environmental Research and Public Health.2020; 17(5): 1726. CrossRef
- Development of a Nano-Real-Time Polymerase Chain Reaction (RT-PCR) Kit for Detection and Genotyping of High-Risk Human Papillomavirus (HPV) Strains Using Dedicated TaqMan Probes
- Current Status of and Perspectives on Cervical Cancer Screening in Korea
- Sung-Chul Lim, Chong Woo Yoo
- J Pathol Transl Med. 2019;53(4):210-216. Published online May 16, 2019
- DOI: https://doi.org/10.4132/jptm.2019.04.11
- 14,027 View
- 278 Download
- 12 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF - Since the introduction of the Papanicolaou (Pap) smear system in 1943, cervicovaginal cytology has been used as a standard screening test for cervical cancer. The dissemination of this test contributed to reductions of the incidence and mortality of cervical cancer worldwide. In Korea, regular health check-ups for industrial workers and their family members were introduced in 1988 and were performed as part of the National Cancer Screening Program in 1999. As a result, the incidence of cervical cancer in Korea has been steadily decreasing. However, about 800 cases of cervical cancer-related deaths are reported each year due to false-negative test results. Hence, new screening methods have been proposed. Liquid-based cytology (LBC) was introduced in 1996 to overcome the limitations of conventional Pap smears. Since then, other LBC methods have been developed and utilized, including the human papilloma virus test—a method with higher sensitivity that requires fewer screenings. In this study, we review current issues and future perspectives related to cervical cancer screening in Korea.
-
Citations
Citations to this article as recorded by- Practice of Cytopathology in Korea: A 40‐Year Evolution Through Standardization, Digital Transformation, and Global Partnership
Yosep Chong, Ran Hong, Hyeong Ju Kwon, Haeryoung Kim, Lucia Kim, Soon Jae Kim, Yoon Jung Choi
Diagnostic Cytopathology.2026; 54(2): 146. CrossRef - A Study on the Workload of Cytotechnologists: Focus on Commercial Laboratories
Eun-Suk PARK
Korean Journal of Clinical Laboratory Science.2025; 57(2): 228. CrossRef - Metastatic Cervical Cancer in the Asia-Pacific Region: Current Treatment Landscape and Barriers
Jeffrey Chee-Hong Goh, Chyong-Huey Lai, Efren Javier Domingo, Jae Hoon Kim, Carmel Spiteri, Danny Hsu, Soo Yeon Ihm, Peng Peng
Cancer Research Communications.2025; 5(8): 1429. CrossRef - Mathematical Assessment of the Roles of Vaccination and Pap Screening on the Burden of HPV and Related Cancers in Korea
Soyoung Park, Hyunah Lim, Abba B. Gumel
Bulletin of Mathematical Biology.2025;[Epub] CrossRef - A questionnaire study on disparity of cervical cancer prevention programs in Asia‐Oceania
Ka Yu Tse, Kimio Ushijima, Ai Ling Tan, Perapong Intasorn, Jitendra Pariyar, Chih‐Long Chang, Efren J. Domingo, Hiralal Konar, Suresh Kumarasamy, Brahmana Askandar Tjokroprawiro, Sarikapan Wilailak
Journal of Obstetrics and Gynaecology Research.2023; 49(4): 1230. CrossRef - Current state of cytopathology residency training: a Korean national survey of pathologists
Uiju Cho, Tae Jung Kim, Wan Seop Kim, Kyo Young Lee, Hye Kyoung Yoon, Hyun Joo Choi
Journal of Pathology and Translational Medicine.2023; 57(2): 95. CrossRef - Meeting the challenges of cervical cancer screening and HPV vaccination in the UK
Roxanne Westwood, Joanna Lavery
Primary Health Care.2022; 32(01): 22. CrossRef - Local and Metastatic Relapses in a Young Woman with Papillary Squamous Cell Carcinoma of the Uterine Cervix
Ha Young Woo, Hyun-Soo Kim
Diagnostics.2022; 12(3): 599. CrossRef - Serum Human Epididymis Protein 4 as a Prognostic Marker in Cervical Cancer
Woo Yeon Hwang, Dong Hoon Suh, Kidong Kim, Yong Beom Kim, Jae Hong No
Cancer Control.2022;[Epub] CrossRef - HPV detection and/or cytological diagnostics
Sanja Milenković
Glasnik javnog zdravlja.2022; 96(3): 313. CrossRef - Clinical management of abnormal Pap tests: differences between US and Korean guidelines
Seyeon Won, Mi Kyoung Kim, Seok Ju Seong
Journal of Pathology and Translational Medicine.2020; 54(3): 213. CrossRef - Current status of cytopathology practices in Korea: annual report on the Continuous Quality Improvement program of the Korean Society for Cytopathology for 2018
Yosep Chong, Haeyoen Jung, Jung-Soo Pyo, Soon Won Hong, Hoon Kyu Oh
Journal of Pathology and Translational Medicine.2020; 54(4): 318. CrossRef - Cytomorphological Features of Hyperchromatic Crowded Groups in Liquid-Based Cervicovaginal Cytology: A Single Institutional Experience
Youngeun Lee, Cheol Lee, In Ae Park, Hyoung Jin An, Haeryoung Kim
Journal of Pathology and Translational Medicine.2019; 53(6): 393. CrossRef
- Practice of Cytopathology in Korea: A 40‐Year Evolution Through Standardization, Digital Transformation, and Global Partnership
- Detection of Human Papillomavirus in Korean Breast Cancer Patients by Real-Time Polymerase Chain Reaction and Meta-Analysis of Human Papillomavirus and Breast Cancer
- Jinhyuk Choi, Chungyeul Kim, Hye Seung Lee, Yoo Jin Choi, Ha Yeon Kim, Jinhwan Lee, Hyeyoon Chang, Aeree Kim
- J Pathol Transl Med. 2016;50(6):442-450. Published online October 10, 2016
- DOI: https://doi.org/10.4132/jptm.2016.07.08
- 14,132 View
- 225 Download
- 16 Web of Science
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) is a well-established oncogenic virus of cervical, anogenital, and oropharyngeal cancer. Various subtypes of HPV have been detected in 0% to 60% of breast cancers. The roles of HPV in the carcinogenesis of breast cancer remain controversial. This study was performed to determine the prevalence of HPV-positive breast cancer in Korean patients and to evaluate the possibility of carcinogenic effect of HPV on breast.
Methods
Meta-analysis was performed in 22 case-control studies for HPV infection in breast cancer. A total of 123 breast cancers, nine intraductal papillomas and 13 nipple tissues of patients with proven cervical HPV infection were tested by real-time polymerase chain reaction to detect 28 subtypes of HPV. Breast cancers were composed of 106 formalin-fixed and paraffin embedded (FFPE) breast cancer samples and 17 touch imprint cytology samples of breast cancers.
Results
The overall odds ratio between breast cancer and HPV infection was 5.43 (95% confidence interval, 3.24 to 9.12) with I2 = 34.5% in meta-analysis of published studies with case-control setting and it was statistically significant. HPV was detected in 22 cases of breast cancers (17.9%) and two cases of intaductal papillomas (22.2%). However, these cases had weak positivity.
Conclusions
These results failed to serve as significant evidence to support the relationship between HPV and breast cancer. Further study with larger epidemiologic population is merited to determine the relationship between HPV and breast cancer. -
Citations
Citations to this article as recorded by- HPV, APOBEC3B, and the origins of breast cancer: a narrative review and perspectives on novel mechanisms
Zhi-yong Liu, Ran Chen
Frontiers in Oncology.2026;[Epub] CrossRef - Advances in human papillomavirus detection for cervical cancer screening and diagnosis: challenges of conventional methods and opportunities for emergent tools
O. Fashedemi, Okoroike C. Ozoemena, Siwaphiwe Peteni, Aderemi B. Haruna, Leshweni J. Shai, Aicheng Chen, Frankie Rawson, Maggie E. Cruickshank, David Grant, Oluwafunmilola Ola, Kenneth I. Ozoemena
Analytical Methods.2025; 17(7): 1428. CrossRef - Bacterial-Viral Interactions in Human Orodigestive and Female Genital Tract Cancers: A Summary of Epidemiologic and Laboratory Evidence
Ikuko Kato, Jilei Zhang, Jun Sun
Cancers.2022; 14(2): 425. CrossRef - Breast cancer association with oncogenic papillomaviruses: papillomaviral DNA detection in breast cancer cells
G. M. Volgareva
Advances in Molecular Oncology.2022; 9(2): 10. CrossRef - Presence of Human Papillomavirus DNA in Malignant Neoplasia and Non-Malignant Breast Disease
Erika Maldonado-Rodríguez, Marisa Hernández-Barrales, Adrián Reyes-López, Susana Godina-González, Perla I. Gallegos-Flores, Edgar L. Esparza-Ibarra, Irma E. González-Curiel, Jesús Aguayo-Rojas, Adrián López-Saucedo, Gretel Mendoza-Almanza, Jorge L. Ayala-
Current Issues in Molecular Biology.2022; 44(8): 3648. CrossRef - Risk Role of Breast Cancer in Association with Human Papilloma Virus among Female Population in Taiwan: A Nationwide Population-Based Cohort Study
Chia-Hsin Liu, Chi-You Liao, Ming-Hsin Yeh, James Cheng-Chung Wei
Healthcare.2022; 10(11): 2235. CrossRef - HPV-Associated Breast Cancer: Myth or Fact?
Erik Kudela, Eva Kudelova, Erik Kozubík, Tomas Rokos, Terezia Pribulova, Veronika Holubekova, Kamil Biringer
Pathogens.2022; 11(12): 1510. CrossRef - Assessment of Human Papillomavirus Infection and Risk Factors in Egyptian Women With Breast Cancer
Nabila El-Sheikh, Nahla O Mousa, Amany M Tawfeik, Alaa M Saleh, Iman Elshikh, Mohamed Deyab, Faten Ragheb, Manar M Moneer, Ahmed Kawashti, Ahmed Osman, Mohamed Elrefaei
Breast Cancer: Basic and Clinical Research.2021;[Epub] CrossRef - Human Papillomavirus (HPV) Detection by Chromogenic In Situ Hybridization (CISH) and p16 Immunohistochemistry (IHC) in Breast Intraductal Papilloma and Breast Carcinoma
Hua Guo, Juan P. Idrovo, Jin Cao, Sudarshana Roychoudhury, Pooja Navale, Louis J. Auguste, Tawfiqul Bhuiya, Silvat Sheikh-Fayyaz
Clinical Breast Cancer.2021; 21(6): e638. CrossRef - Human Papillomavirus in Breast Carcinogenesis: A Passenger, a Cofactor, or a Causal Agent?
Rancés Blanco, Diego Carrillo-Beltrán, Juan P. Muñoz, Alejandro H. Corvalán, Gloria M. Calaf, Francisco Aguayo
Biology.2021; 10(8): 804. CrossRef - Systematic review and meta-analysis of the papillomavirus prevalence in breast cancer fresh tissues
Geilson Gomes de Oliveira, Ana Katherine Gonçalves, José Eleutério, Luiz Gonzaga Porto Pinheiro
Breast Disease.2021; 41(1): 123. CrossRef - Is human papillomavirus associated with breast cancer or papilloma presenting with pathologic nipple discharge?
Fatih Levent Balci, Cihan Uras, Sheldon Marc Feldman
Cancer Treatment and Research Communications.2019; 19: 100122. CrossRef - Is the HPV virus responsible for the development of breast cancer?
Erik Kudela, Marcela Nachajova, Jan Danko
The Breast Journal.2019; 25(5): 1053. CrossRef - Absence of Human Papillomavirus in Benign and Malignant Breast Tissue
Maryam Kazemi Aghdam, Seyed Alireza Nadji, Azadeh Alvandimanesh, Maliheh Khoddami, Yassaman Khademi
Iranian Journal of Pathology.2019; 14(4): 279. CrossRef - Oncogenic Viruses and Breast Cancer: Mouse Mammary Tumor Virus (MMTV), Bovine Leukemia Virus (BLV), Human Papilloma Virus (HPV), and Epstein–Barr Virus (EBV)
James S. Lawson, Brian Salmons, Wendy K. Glenn
Frontiers in Oncology.2018;[Epub] CrossRef - Viral infections and breast cancer – A current perspective
O.M. Gannon, A. Antonsson, I.C. Bennett, N.A. Saunders
Cancer Letters.2018; 420: 182. CrossRef - Prevalence of EBV, HPV and MMTV in Pakistani breast cancer patients: A possible etiological role of viruses in breast cancer
Wasifa Naushad, Orooj Surriya, Hajra Sadia
Infection, Genetics and Evolution.2017; 54: 230. CrossRef
- HPV, APOBEC3B, and the origins of breast cancer: a narrative review and perspectives on novel mechanisms
- Clinical Significance of an HPV DNA Chip Test with Emphasis on HPV-16 and/or HPV-18 Detection in Korean Gynecological Patients
- Min-Kyung Yeo, Ahwon Lee, Soo Young Hur, Jong Sup Park
- J Pathol Transl Med. 2016;50(4):294-299. Published online June 26, 2016
- DOI: https://doi.org/10.4132/jptm.2016.05.09
- 10,654 View
- 80 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) is a major risk factor for cervical cancer.
Methods
We evaluated the clinical significance of the HPV DNA chip genotyping assay (MyHPV chip, Mygene Co.) compared with the Hybrid Capture 2 (HC2) chemiluminescent nucleic acid hybridization kit (Digene Corp.) in 867 patients.
Results
The concordance rate between the MyHPV chip and HC2 was 79.4% (kappa coefficient, κ = 0.55). The sensitivity and specificity of both HPV tests were very similar (approximately 85% and 50%, respectively). The addition of HPV result (either MyHPV chip or HC2) to cytology improved the sensitivity (95%, each) but reduced the specificity (approximately 30%, each) compared with the HPV test or cytology alone. Based on the MyHPV chip results, the odds ratio (OR) for ≥ high-grade squamous intraepithelial lesions (HSILs) was 9.9 in the HPV-16/18 (+) group and 3.7 in the non-16/18 high-risk (HR)-HPV (+) group. Based on the HC2 results, the OR for ≥ HSILs was 5.9 in the HR-HPV (+) group. When considering only patients with cytological diagnoses of “negative for intraepithelial lesion or malignancy” and “atypical squamous cell or atypical glandular cell,” based on the MyHPV chip results, the ORs for ≥ HSILs were 6.8 and 11.7, respectively, in the HPV-16/18 (+) group.
Conclusions
The sensitivity and specificity of the MyHPV chip test are similar to the HC2. Detecting HPV-16/18 with an HPV DNA chip test, which is commonly used in many Asian countries, is useful in assessing the risk of high-grade cervical lesions. -
Citations
Citations to this article as recorded by- Human papilloma virus identification in ocular surface squamous neoplasia by p16 immunohistochemistry and DNA chip test
Tina Shrestha, Won Choi, Ga Eon Kim, Jee Myung Yang, Kyung Chul Yoon
Medicine.2019; 98(2): e13944. CrossRef - Comparison of the PANArray HPV Genotyping Chip Test with the Cobas 4800 HPV and Hybrid Capture 2 Tests for Detection of HPV in ASCUS Women
Eun Young Ki, Yoon Kyung Lee, Ahwon Lee, Jong Sup Park
Yonsei Medical Journal.2018; 59(5): 662. CrossRef
- Human papilloma virus identification in ocular surface squamous neoplasia by p16 immunohistochemistry and DNA chip test
- Comparison of Analytical and Clinical Performance of HPV 9G DNA Chip, PANArray HPV Genotyping Chip, and Hybrid-Capture II Assay in Cervicovaginal Swabs
- Ho Young Jung, Hye Seung Han, Hyo Bin Kim, Seo Young Oh, Sun-Joo Lee, Wook Youn Kim
- J Pathol Transl Med. 2016;50(2):138-146. Published online January 13, 2016
- DOI: https://doi.org/10.4132/jptm.2015.10.21
- 10,214 View
- 68 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Human papillomavirus (HPV) infection can be detected by using several molecular methods, including Hybrid-Capture II (HC2) assay and variable HPV DNA chip tests, although each method has different sensitivities and specificities. Methods: We performed HPV 9G DNA Chip (9G) and PANArray HPV Genotyping Chip (PANArray) tests on 118 cervicovaginal swabs and compared the results with HC2, cytology, histology, and direct sequencing results. Results: The overall and high-risk HPV (HR-HPV) positivity rates were 62.7% and 44.9% using 9G, and 61.0% and 30.5% using PANArray, respectively. The positivity rates for HR-HPV with these two chips were significantly lower than 55.1% when HC2 was used. The sensitivity of overall HPV positivity in detecting histologically confirmed low-grade cervical squamous intraepithelial lesions or higher was 88.7% for all three tests. The specificity was 58.5% for 9G and 61.5% for PANArray, which was significantly lower than the 72.3% for HC2. With the HR-HPV+ genotype threshold, the sensitivity decreased to 75.5% for 9G and 52.8% for PANArray, which was significantly lower than the 88.7% for HC2. Comparison of the two chips showed concordant results in 55.1% of the samples, compatible results in 16.9%, and discordant results in 28.0%, exhibiting poor agreement in detecting certain HPV genotypes. Compared with direct sequencing, 9G yielded no discordant results, whereas PANArray yielded 31 discordant results (26.7%). Conclusions: Compared with HC2, the HPV genotyping tests showed lower sensitivity in histologic correlation. When the two chips were compared, the 9G was more sensitive and accurate for detecting HR-HPV than the PANArray. -
Citations
Citations to this article as recorded by- Concordance of Anyplex™ II HPV HR assays with reference HPV assays in cervical cancer screening: Systematic review
Habtamu Biazin
Journal of Virological Methods.2022; 301: 114435. CrossRef - The clinical performance of human papillomavirus genotyping using PANArray HPV chip: Comparison to ThinPrep cytology alone and co-testing
Jiyoung Kim, Sun-Young Jun, Lee-So Maeng
Pathology - Research and Practice.2020; 216(9): 153121. CrossRef - Analytic performance of PANArray HPV and HPV 9G DNA chip tests for genotyping of high-risk human papillomavirus in cervical ThinPrep PreservCyt samples
Jiyoung Kim, Sun-Young Jun, Magdalena Grce
PLOS ONE.2019; 14(10): e0224483. CrossRef
- Concordance of Anyplex™ II HPV HR assays with reference HPV assays in cervical cancer screening: Systematic review
- Uncommon and Rare Human Papillomavirus Genotypes Relating to Cervical Carcinomas
- Na Rae Kim, Myunghee Kang, Soon Pyo Lee, Hyunchul Kim, Jungsuk An, Dong Hae Chung, Seung Yeon Ha, Hyun Yee Cho
- Korean J Pathol. 2014;48(1):43-49. Published online February 25, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.1.43
- 10,362 View
- 56 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Human papillomavirus (HPV) is an oncogenic virus in cervical cancer and most invasive carcinomas (ICs) are caused by HPV16 and 18. However, the roles and contributions of other uncommon and rare genotypes remain uncertain.
Methods HPV genotypes were retrospectively assessed using an HPV DNA chip that can specify up to 32 HPV genotypes. We arbitrarily regarded genotypes accounting for less than 6% of the total as uncommon and rare genotypes.
Results A total of 3,164 HPV-positive cases were enrolled. In groups 2A, 2B, 3, and unclassified HPV genotypes, 2.4% of cases with uncommon HPV genotypes (68, 26, 34, 53, 66, 69, 70, 73, 40, 42, 43, 44, 54, 55, 61, 62, 6, and 11) showed high grade squamous intraepithelial lesions and ICs. There were no HPV32- and 57-infected cases.
Conclusions We found that the uncommon and rare HPV genotypes may provide incremental etiologic contributions in cervical carcinogenesis, especially HPV68, 70, and 53. Further studies on these uncommon and rare HPV genotypes will be of importance in establishing the significance of genotypes in different regions, especially in planning a strategy for further vaccine development as well as follow-up on the effectiveness of the currently used vaccines.
-
Citations
Citations to this article as recorded by- High-risk human papillomavirus diversity among indigenous women of western Botswana with normal cervical cytology and dysplasia
Patricia S. Rantshabeng, Billy M. Tsima, Andrew K. Ndlovu, Keneilwe Motlhatlhedi, Kirthana Sharma, Carol B. Masole, Natasha O. Moraka, Kesego Motsumi, Angela K. T. Maoto-Mokote, Alemayehu B. Eshetu, Leabaneng Tawe, Tendani Gaolathe, Sikhulile Moyo, Lynnet
BMC Infectious Diseases.2024;[Epub] CrossRef - Human Papillomavirus (HPV69/HPV73) Coinfection associated with Simultaneous Squamous Cell Carcinoma of the Anus and Presumed Lung Metastasis
Stephanie Shea, Marina Muñoz, Stephen C. Ward, Mary B. Beasley, Melissa R Gitman, Michael D Nowak, Jane Houldsworth, Emilia Mia Sordillo, Juan David Ramirez, Alberto E. Paniz Mondolfi
Viruses.2020; 12(3): 349. CrossRef - Human Papillomavirus Selected Properties and Related Cervical Cancer Prevention Issues
Saule Balmagambetova, Andrea Tinelli, Ospan A. Mynbaev, Arip Koyshybaev, Olzhas Urazayev, Nurgul Kereyeva, Elnara Ismagulova
Current Pharmaceutical Design.2020; 26(18): 2073. CrossRef - Periungual Bowen's disease with a narrow longitudinal melanonychia mimicking periungual warts
Taiyo HITAKA, Michiko HASEGAWA, Akira SHIMIZU, Yuko KURIYAMA, Atsushi TAMURA
Skin Cancer.2019; 33(3): 211. CrossRef - Detection of HPV RNA molecules in stratified mucin-producing intraepithelial lesion (SMILE) with concurrent cervical intraepithelial lesion: a case report
Shiho Fukui, Kazunori Nagasaka, Naoko Iimura, Ranka Kanda, Takayuki Ichinose, Takeru Sugihara, Haruko Hiraike, Shunsuke Nakagawa, Yuko Sasajima, Takuya Ayabe
Virology Journal.2019;[Epub] CrossRef - Pitfalls of commercially available HPV tests in HPV68a detection
Hana Jaworek, Katerina Kubanova, Vladimira Koudelakova, Rastislav Slavkovsky, Jiri Drabek, Marian Hajduch, Craig Meyers
PLOS ONE.2019; 14(8): e0220373. CrossRef - Overall accuracy of cervical cytology and clinicopathological significance of LSIL cells in ASC‐H cytology
S. H. Kim, J. M. Lee, H. G. Yun, U. S. Park, S. U. Hwang, J.‐S. Pyo, J. H. Sohn
Cytopathology.2017; 28(1): 16. CrossRef - Human papillomavirus genotyping by Linear Array and Next-Generation Sequencing in cervical samples from Western Mexico
María Guadalupe Flores-Miramontes, Luis Alberto Torres-Reyes, Liliana Alvarado-Ruíz, Salvador Angel Romero-Martínez, Verenice Ramírez-Rodríguez, Luz María Adriana Balderas-Peña, Verónica Vallejo-Ruíz, Patricia Piña-Sánchez, Elva Irene Cortés-Gutiérrez, Lu
Virology Journal.2015;[Epub] CrossRef - Impact of human papillomavirus coinfections on the risk of high-grade squamous intraepithelial lesion and cervical cancer
Adela Carrillo-García, Sergio Ponce-de-León-Rosales, David Cantú-de-León, Verónica Fragoso-Ontiveros, Imelda Martínez-Ramírez, Asunción Orozco-Colín, Alejandro Mohar, Marcela Lizano
Gynecologic Oncology.2014; 134(3): 534. CrossRef - Human papillomavirus 66‐associated subungual squamous cell carcinoma
Jin Hee Kang, Hwa young Ahn, Miri Kim, Shin Taek Oh, Baik Kee Cho, Hyun Jeong Park
The Journal of Dermatology.2014; 41(12): 1119. CrossRef
- High-risk human papillomavirus diversity among indigenous women of western Botswana with normal cervical cytology and dysplasia
- Cytological Evaluation and REBA HPV-ID HPV Testing of Newly Developed Liquid-Based Cytology, EASYPREP: Comparison with SurePath
- Youn Soo Lee, Gyungyub Gong, Jin Hee Sohn, Ki Sung Ryu, Jung Hun Lee, Shin Kwang Khang, Kyung-Ja Cho, Yong-Man Kim, Chang Suk Kang
- Korean J Pathol. 2013;47(3):265-274. Published online June 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.3.265
- 11,982 View
- 98 Download
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The objective of this study was to evaluate a newly-developed EASYPREP liquid-based cytology method in cervicovaginal specimens and compare it with SurePath.
Methods Cervicovaginal specimens were prospectively collected from 1,000 patients with EASYPREP and SurePath. The specimens were first collected by brushing for SurePath and second for EASYPREP. The specimens of both methods were diagnosed according to the Bethesda System. Additionally, we performed to REBA HPV-ID genotyping and sequencing analysis for human papillomavirus (HPV) on 249 specimens.
Results EASYPREP and SurePath showed even distribution of cells and were equal in cellularity and staining quality. The diagnostic agreement between the two methods was 96.5%. Based on the standard of SurePath, the sensitivity, specificity, positive predictive value, and negative predictive value of EASYPREP were 90.7%, 99.2%, 94.8%, and 98.5%, respectively. The positivity of REBA HPV-ID was 49.4% and 95.1% in normal and abnormal cytological samples, respectively. The result of REBA HPV-ID had high concordance with sequencing analysis.
Conclusions EASYPREP provided comparable results to SurePath in the diagnosis and staining quality of cytology examinations and in HPV testing with REBA HPV-ID. EASYPREP could be another LBC method choice for the cervicovaginal specimens. Additionally, REBA HPV-ID may be a useful method for HPV genotyping.
-
Citations
Citations to this article as recorded by- Virome capture sequencing for comprehensive HPV genotyping in cervical samples
Thanayod Sasivimolrattana, Sasiprapa Liewchalermwong, Wasun Chantratita, Insee Sensorn, Arkom Chaiwongkot, Parvapan Bhattarakosol
Science Progress.2025;[Epub] CrossRef - High-Risk Human Papillomavirus Detection via Cobas® 4800 and REBA HPV-ID® Assays
Sasiprapa Liewchalermwong, Shina Oranratanaphan, Wichai Termrungruanglert, Surang Triratanachat, Patou Tantbirojn, Nakarin Kitkumthorn, Parvapan Bhattarakosol, Arkom Chaiwongkot
Viruses.2022; 14(12): 2713. CrossRef - Evaluation of nuclear chromatin using grayscale intensity and thresholded percentage area in liquid‐based cervical cytology
Hyekyung Lee, Myungein Han, Taejo Yoo, Chanho Jung, Hyun‐Jin Son, Migyung Cho
Diagnostic Cytopathology.2018; 46(5): 384. CrossRef - Comparison of EASYPREP® and SurePath® in thyroid fine‐needle aspiration
Yosep Chong, Ki Hyun Baek, Jee Young Kim, Tae‐Jung Kim, Eun Jung Lee, Chang Suk Kang
Diagnostic Cytopathology.2016; 44(4): 283. CrossRef
- Virome capture sequencing for comprehensive HPV genotyping in cervical samples
- Human Papillomavirus Prevalence and Cell Cycle Related Protein Expression in Tonsillar Squamous Cell Carcinomas of Korean Patients with Clinicopathologic Analysis
- Miji Lee, Sung Bae Kim, Sang-wook Lee, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim, Kyung-Ja Cho
- Korean J Pathol. 2013;47(2):148-157. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.148
- 9,109 View
- 52 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Human papillomavirus (HPV)-related tonsillar squamous cell carcinoma (TSCC) has recently been characterized as a distinct subset with a favorable prognosis. The prevalence and clinicopathologic significance of HPV-related TSCC in Koreans are not well known.
Methods HPV
in situ hybridization (ISH) accompanied by p53, p16, pRb, and cyclin D1 immunohistochemical staining were performed on 89 resection cases of TSCC from 2000 through 2010.Results HPV was detected by ISH in 59 of 89 cases (66.3%). HPV-positive TSCCs were more common in younger ages (p=0.005), and tumor sizes were smaller in the HPV-positive compared to the HPV-negative group (p=0.040). Positive HPV staining was significantly correlated with p16 expression (p<0.001), pRb inactivation (p=0.003), and cyclin D1 down-regulation (p<0.001) but not with p53 expression (p=0.334). Seventeen cases that showed p16-immunopositivity with HPV-negativity by ISH were retested by HPV typing; HPV DNA was not detected in all cases. There was no significant difference between HPV-positive and HPV-negative patients either in the disease-specific survival (DSS, p=0.857) or overall survival (p=0.910). Furthermore, pRb-inactivated cases showed better DSS (p=0.023), and p53-positive cases showed worse DSS (p=0.001).
Conclusions Although high HPV prevalence was noted, it was not correlated with histopathologic findings or survival benefit. In addition to p53 expression, pRb inactivation along with p16 overexpression and down-regulation of cyclin D1 are thought to be important pathogenetic steps for developing TSCCs.
-
Citations
Citations to this article as recorded by- Assessment of the Mutation Profile of Tonsillar Squamous Cell Carcinomas Using Targeted Next-Generation Sequencing
Ha Young Park, Joong Seob Lee, Jee Hye Wee, Jeong Wook Kang, Eun Soo Kim, Taeryool Koo, Hee Sung Hwang, Hyo Jung Kim, Ho Suk Kang, Hyun Lim, Nan Young Kim, Eun Sook Nam, Seong Jin Cho, Mi Jung Kwon
Biomedicines.2023; 11(3): 851. CrossRef - Clinicopathologic characterization of cervical metastasis from an unknown primary tumor: a multicenter study in Korea
Miseon Lee, Uiree Jo, Joon Seon Song, Youn Soo Lee, Chang Gok Woo, Dong-Hoon Kim, Jung Yeon Kim, Sun Och Yoon, Kyung-Ja Cho
Journal of Pathology and Translational Medicine.2023; 57(3): 166. CrossRef - Negative Prognostic Implication of TERT Promoter Mutations in Human Papillomavirus–Negative Tonsillar Squamous Cell Carcinoma Under the New 8th AJCC Staging System
Hyunchul Kim, Mi Jung Kwon, Bumjung Park, Hyo Geun Choi, Eun Sook Nam, Seong Jin Cho, Kyueng-Whan Min, Eun Soo Kim, Hee Sung Hwang, Mineui Hong, Taeryool Koo, Hyo Jung Kim
Indian Journal of Surgical Oncology.2021; 12(S1): 134. CrossRef - Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
Yuil Kim, Young-Hoon Joo, Min-Sik Kim, Youn Soo Lee
Journal of Pathology and Translational Medicine.2020; 54(5): 411. CrossRef - Frequent hepatocyte growth factor overexpression and low frequency of c-Met gene amplification in human papillomavirus–negative tonsillar squamous cell carcinoma and their prognostic significances
Mi Jung Kwon, Dong Hoon Kim, Hye-Rim Park, Hyung Sik Shin, Ji Hyun Kwon, Dong Jin Lee, Jin Hwan Kim, Seong Jin Cho, Eun Sook Nam
Human Pathology.2014; 45(7): 1327. CrossRef
- Assessment of the Mutation Profile of Tonsillar Squamous Cell Carcinomas Using Targeted Next-Generation Sequencing
- Expression of c-Met Is Different along the Location and Associated with Lymph Node Metastasis of Head and Neck Carcinoma
- Ji-Young Choe, Ji Yun Yun, Soo-Jeong Nam, Ji Eun Kim
- Korean J Pathol. 2012;46(6):515-522. Published online December 26, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.6.515
- 8,958 View
- 52 Download
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Activation of the c-Met pathway is involved in cancer progression and the prognosis. We aimed to identify any association of c-Met protein expression with a number of clinicopathologic variables including infection of human papillomavirus and Epstein-Barr virus (EBV) in head and neck carcinomas (HNCa).
Methods Eighty-two cases were enrolled in this study. Expression of c-Met and p16 was investigated immunohistochemically. EBV was detected by
in situ hybridization and amplification of thec-Met gene by fluorescencein situ hybridization.Results The c-Met protein was expressed in 41.5% (34/82), and gene amplification was found in 1.4% (1/71). High expression of c-Met was associated with the primary location of the tumor; the hypopharynx showed the highest expression, followed by the oral cavity, larynx, and nasal cavity. Squamous cell carcinoma expressed c-Met more frequently than undifferentiated carcinoma. Also, p16 immunoreactivity or EBV infection was associated with the tumor location and well-differentiated histologic type, but were not linked to c-Met expression. The patients with positive c-Met expression showed frequent lymph node metastasis.
Conclusions Activation of the c-Met pathway might be involved in a subset of HNCa. Cases showing positive c-Met expression should be carefully monitored because of the high probability of lymph node metastasis.
-
Citations
Citations to this article as recorded by- Case Report: A rare case of MET-amplified gastric cancer with systemic metastasis: remarkable efficacy of crizotinib and the role of precision medicine
Yan Shen, Yaxin Xu, Jing Sun
Frontiers in Oncology.2025;[Epub] CrossRef - c-MET pathway in human malignancies and its targeting by natural compounds for cancer therapy
Chakrabhavi Dhananjaya Mohan, Muthu K Shanmugam, Siddegowda Gopalapura Shivanne Gowda, Arunachalam Chinnathambi, Kanchugarakoppal S. Rangappa, Gautam Sethi
Phytomedicine.2024; 128: 155379. CrossRef - Nadir paranazal sinüs kanserlerinde yeni tanımlanan reseptör tirozin kinaz mutasyonları ve potansiyel fonksiyonel etkileri
Bakiye GÖKER BAGCA, Sercan GÖDE, Göksel TURHAL, Neslihan Pınar ÖZATEŞ, Ali VERAL, Cumhur GÜNDÜZ, Çığır Biray AVCI
Ege Tıp Dergisi.2023; 62(1): 139. CrossRef - The Emerging Role of c-Met in Carcinogenesis and Clinical Implications as a Possible Therapeutic Target
Antonio Faiella, Ferdinando Riccardi, Giacomo Cartenì, Martina Chiurazzi, Livia Onofrio, Rengyun Liu
Journal of Oncology.2022; 2022: 1. CrossRef - NK4 Regulates Laryngeal Squamous Cell Carcinoma Cell Properties and Inhibits Tumorigenicity by Modulating the DKK1/Wnt/β-Catenin Axis
Shoukai Zhang, Hulai Wei, Xiaoqin Ha, Yueyu Zhang, Yufen Guo
Frontiers in Oncology.2021;[Epub] CrossRef - Epstein-Barr Virus-Associated Carcinoma of the Larynx: A Systematic Review with Meta-Analysis
Marcos Antonio Pereira de Lima, Álife Diêgo Lima Silva, Antônio Carlos Silva do Nascimento Filho, Thiago Lima Cordeiro, João Pedro de Souza Bezerra, Maria Aline Barroso Rocha, Sally de França Lacerda Pinheiro, Roberto Flávio Fontenelle Pinheiro Junior, Ma
Pathogens.2021; 10(11): 1429. CrossRef - The roles of PTEN, cMET, and p16 in resistance to cetuximab in head and neck squamous cell carcinoma
Alexandre A. B. A. da Costa, Felipe D’Almeida Costa, Daniel Vilarim Araújo, Marcos Pedro Guedes Camandaroba, Victor Hugo Fonseca de Jesus, Audrey Oliveira, Ana Caroline Fonseca Alves, Carlos Stecca, Larissa Machado, Andrea Cruz Feraz de Oliveira, Thiago B
Medical Oncology.2019;[Epub] CrossRef - Role of c‐Met expression on prognosis of head and neck cancer: A literature review and meta‐analysis
Lei Li, Zhijun Sun, Xin Huang, Xiao Li, Lihua Sun, Lei Zhang, Xiaodan Zhang, Longwei Ye, Jie Yuan, Limin Mao, Guolin Li
Head & Neck.2019; 41(6): 1999. CrossRef - MET Genomic Alterations in Head and Neck Squamous Cell Carcinoma (HNSCC): Rapid Response to Crizotinib in a Patient with HNSCC with a Novel MET R1004G Mutation
Lisa Pei Chu, Debra Franck, Christine A. Parachoniak, Jeffrey P. Gregg, Michael G. Moore, D. Gregory Farwell, Shyam Rao, Andreas M. Heilmann, Rachel L. Erlich, Jeffrey S. Ross, Vincent A. Miller, Siraj Ali, Jonathan W. Riess
The Oncologist.2019; 24(10): 1305. CrossRef - Understanding c-MET signalling in squamous cell carcinoma of the head & neck
P. Szturz, E. Raymond, C. Abitbol, S. Albert, A. de Gramont, S. Faivre
Critical Reviews in Oncology/Hematology.2017; 111: 39. CrossRef - Prognostic value of c-MET in head and neck cancer: A systematic review and meta-analysis of aggregate data
Petr Szturz, Marie Budíková, Jan B. Vermorken, Ivana Horová, Břetislav Gál, Eric Raymond, Armand de Gramont, Sandrine Faivre
Oral Oncology.2017; 74: 68. CrossRef - Activated HGF-c-Met Axis in Head and Neck Cancer
Levi Arnold, Jonathan Enders, Sufi Thomas
Cancers.2017; 9(12): 169. CrossRef - Clinicopathological impacts of high c-Met expression in head and neck squamous cell carcinoma: a meta-analysis and review
Jung Han Kim, Bum Jun Kim, Hyeong Su Kim
Oncotarget.2017; 8(68): 113120. CrossRef - High expression of c‑Met and EGFR is associated with poor survival of patients with glottic laryngeal squamous cell carcinoma
Mei Jiang, Hui Zhang, He Xiao, Zhimin Zhang, Dan Que, Jia Luo, Jian Li, Bijing Mao, Yuanyuan Chen, Meilin Lan, Ge Wang, Hualiang Xiao
Oncology Letters.2017;[Epub] CrossRef - Profiling of cMET and HER Family Receptor Expression in Pancreatic Ductal Adenocarcinomas and Corresponding Lymph Node Metastasis to Assess Relevant Pathways for Targeted Therapies
Alexander Muckenhuber, Galina Babitzki, Marlene Thomas, Gabriele Hölzlwimmer, Magdalena Zajac, Moritz Jesinghaus, Frank Bergmann, Jens Werner, Albrecht Stenzinger, Wilko Weichert
Pancreas.2016; 45(8): 1167. CrossRef - Absent and abundant MET immunoreactivity is associated with poor prognosis of patients with oral and oropharyngeal squamous cell carcinoma
Maria J. De Herdt, Stefan M. Willems, Berdine van der Steen, Rob Noorlag, Esther I. Verhoef, Geert J.L.H. van Leenders, Robert J.J. van Es, Senada Koljenović, Robert J. Baatenburg de Jong, Leendert H.J. Looijenga
Oncotarget.2016; 7(11): 13167. CrossRef - Biological, diagnostic and therapeutic relevance of the MET receptor signaling in head and neck cancer
Lluís Nisa, Daniel Matthias Aebersold, Roland Giger, Yitzhak Zimmer, Michaela Medová
Pharmacology & Therapeutics.2014; 143(3): 337. CrossRef - Frequent hepatocyte growth factor overexpression and low frequency of c-Met gene amplification in human papillomavirus–negative tonsillar squamous cell carcinoma and their prognostic significances
Mi Jung Kwon, Dong Hoon Kim, Hye-Rim Park, Hyung Sik Shin, Ji Hyun Kwon, Dong Jin Lee, Jin Hwan Kim, Seong Jin Cho, Eun Sook Nam
Human Pathology.2014; 45(7): 1327. CrossRef - Distinct c-Met activation mechanisms induce cell rounding or invasion through pathways involving integrins, RhoA and HIP1
Anja Mai, Ghaffar Muharram, Rachel Barrow-McGee, Habib Baghirov, Juha Rantala, Stéphanie Kermorgant, Johanna Ivaska
Journal of Cell Science.2014; 127(9): 1938. CrossRef
- Case Report: A rare case of MET-amplified gastric cancer with systemic metastasis: remarkable efficacy of crizotinib and the role of precision medicine
- Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of Relevant Literature on Korean Women
- Sung Jong Lee, Hyun Joo Choi
- Korean J Pathol. 2012;46(4):395-398. Published online August 23, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.4.395
- 9,331 View
- 82 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Primary endometrial squamous cell carcinoma (PESCC) is an extremely rare tumor with unclear pathogenesis. A 54-year-old postmenopausal woman presented with a 6-month history of vaginal bleeding. The patient was provisionally diagnosed with uterine submucosal leiomyoma. This was followed by total hysterectomy with a bilateral salpingo-oophorectomy under the laparoscopic guidance. Histopathologically, the tumor was PESCC which was accompanied by a lack of the tumor in the uterine cervix. The tumor showed positive immunoreactivity for p16INK4a. But there was no evidence of human papillomavirus (HPV) on
in situ hybridization and HPV DNA chip analysis. We also present a review of the relevant literature on Korean women.-
Citations
Citations to this article as recorded by- Primary endometrial squamous cell carcinoma (PESCC): Review of the literature and case report
Kuang-Han Liu, Chia-Chin Tsai, Krystal Baysan Lin, Pei-Shen Huang
Taiwanese Journal of Obstetrics and Gynecology.2025; 64(1): 159. CrossRef - Primary squamous cell carcinoma of the uterine wall associated with adenomyosis: A rare case report and literature review
Yang Li, Lanlan Xuan, Qiucheng Wang
International Journal of Gynecology & Obstetrics.2025;[Epub] CrossRef - p16 Block Type Overexpression, p53 Wild Type Reactivity, and Cervical Involvement do not Always Exclude the Diagnosis of Primary Endometrial Squamous Cell Carcinoma (PESCC)
Daniela Fanni, Clara Gerosa, Michele Peiretti, Valerio Mais, Elena Massa, Stefano Angioni, Gavino Faa
International Journal of Gynecological Pathology.2024; 43(2): 200. CrossRef - Pathogenetic characteristics of endometrioid adenocarcinoma of uterus at present stage
T. I. Moiseenko, S. V. Shatalova, E. M. Nepomnyashchaya, V. A. Bandovkina, M. L. Adamyan
Medical alphabet.2024; (36): 35. CrossRef - Case report: Clinicopathological characteristic of two cases of primary endometrial squamous cell carcinoma and review of the literature
Hui-Bin Zhang, Li-Hua Lin, Qiu-Ping Lin, Yuan-Qing Lin, Dan Luo, Shu-Xia Xu
Frontiers in Oncology.2024;[Epub] CrossRef - Treatment of primary squamous cell carcinoma of the endometrium and review of previous literature: A case report
Liyun Song, Qi Wu, Suning Bai, Ren Xu, Xiaona Wang, Yanyan Yang
Medicine.2023; 102(17): e33667. CrossRef -
Prevalence of
human papilloma virus
and
Chlamydia trachomatis
in endometrial and cervical carcinoma: a comparative study in North Indian women
Heena Gautam, Sumita Mehta, Nidhi Nayar, Neha Kumar, Syed Akhtar Husain, Mausumi Bharadwaj
Systems Biology in Reproductive Medicine.2023; 69(6): 399. CrossRef - PAX8 Positivity, Abnormal p53 Expression, and p16 Negativity in a Primary Endometrial Squamous Cell Carcinoma: A Case Report and Review of the Literature
Daniela Fanni, Michele Peiretti, Valerio Mais, Elena Massa, Clara Gerosa, Francesca Ledda, Maria Luisa Fais, Gavino Faa, Stefano Angioni
International Journal of Gynecological Pathology.2022; 41(4): 431. CrossRef - Molecular Analysis of HPV-independent Primary Endometrial Squamous Cell Carcinoma Reveals TP53 and CDKN2A Comutations
Mark R. Hopkins, Doreen N. Palsgrove, Brigitte M. Ronnett, Russell Vang, Jeffrey Lin, Tricia A. Murdock
American Journal of Surgical Pathology.2022; 46(12): 1611. CrossRef - Primary squamous cell carcinoma of the endometrium—Case report with cytological characteristics in direct and indirect endometrial samples
Sanda Rajhvajn, Ana Barišić, Lada Škopljanac‐Mačina, Danijela Jurič, Vesna Mahovlić
Cytopathology.2021; 32(6): 823. CrossRef - Primary squamous cell carcinoma of the endometrium associated with human papilloma virus in a young woman: a case report
Tchin Darré, Abdoul-Samadou Aboubakari, Lantam Sonhaye, Baguilane Douaguibe, Akila Bassowa, Gado Napo-Koura
Journal of Medical Case Reports.2019;[Epub] CrossRef - Primary squamous cell carcinoma of the endometrium in a woman of perimenopausal age
Chao Zhang, Hongyan Zhang, Linqing Yang, Yunfei Wang, Xiaoyu Li, Jinfeng Guo, Jing Xu
Medicine.2018; 97(48): e13418. CrossRef - S100P is Overexpressed in Squamous Cell and Adenosquamous Carcinoma Subtypes of Endometrial Cancer and Promotes Cancer Cell Proliferation and Invasion
Hongfei Jiang, Hang Hu, Fan Lin, Yoon Pin Lim, Yunfen Hua, Xiaomei Tong, Songying Zhang
Cancer Investigation.2016; 34(10): 477. CrossRef - Überraschung in der Abradatdiagnostik
U. Kellner, A. Kellner, U. Cirkel
Der Pathologe.2015; 36(3): 317. CrossRef
- Primary endometrial squamous cell carcinoma (PESCC): Review of the literature and case report
- Expression of Human Papillomavirus-Related Proteins and Its Clinical Implication in Tonsillar Squamous Cell Carcinoma
- Joon Seon Song, Min-Sik Kim, Joon Wook Park, Youn Soo Lee, Chang Suk Kang
- Korean J Pathol. 2012;46(2):177-186. Published online April 25, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.2.177
- 11,020 View
- 42 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Human papillomavirus (HPV) is known to cause of oropharyngeal squamous cell carcinoma (SqCC). HPV positive SqCCs overexpress p16 and are associated with better survival. Several markers of cell cycles and apoptosis have been reported as a prognostic value. We examined the prognostic value of HPV status, p16, cyclin D1, and Bcl-2 in patients with tonsillar SqCC.
Methods Tissue microarrays were constructed in 56 cases of tonsillar SqCC for which we performed an immunohistochemistry and an
in situ hybridization (ISH) of the HPV.Results Of the 56 cases, 31 (55.3%) were positive for p16 and 20 (35.7%) were positive for HPV ISH. The expressions of p16, cyclin D1, and Bcl-2 were not correlated with the clinicopathologic variables including smoking status, differentiation and pT- and pN-stages. The HPV ISH positive group showed a better overall survival than the HPV negative group (p=0.04), and the p16 positive group showed a better disease free survival (DFS) than the negative group (p=0.016). Cox regression analysis showed that only p16 positivity was an independent prognostic factor for DFS (p=0.03; hazard ratio, 10.1).
Conclusions Our results indicate that both p16 expression and HPV status are useful indicators for risk stratification in patients with tonsillar SqCC.
-
Citations
Citations to this article as recorded by- Positive Rate of Human Papillomavirus and Its Trend in Head and Neck Cancer in South Korea
Hyun Woong Jun, Yong Bae Ji, Chang Myeon Song, Jae Kyung Myung, Hae Jin Park, Kyung Tae
Frontiers in Surgery.2022;[Epub] CrossRef - Negative Prognostic Implication of TERT Promoter Mutations in Human Papillomavirus–Negative Tonsillar Squamous Cell Carcinoma Under the New 8th AJCC Staging System
Hyunchul Kim, Mi Jung Kwon, Bumjung Park, Hyo Geun Choi, Eun Sook Nam, Seong Jin Cho, Kyueng-Whan Min, Eun Soo Kim, Hee Sung Hwang, Mineui Hong, Taeryool Koo, Hyo Jung Kim
Indian Journal of Surgical Oncology.2021; 12(S1): 134. CrossRef - In situ hybridization for high risk HPV E6/E7 mRNA in oropharyngeal squamous cell carcinoma
Krish Suresh, Parth V. Shah, Sydney Coates, Borislav A. Alexiev, Sandeep Samant
American Journal of Otolaryngology.2021; 42(1): 102782. CrossRef - Prevalence of high-risk human papillomavirus and its genotype distribution in head and neck squamous cell carcinomas
Yuil Kim, Young-Hoon Joo, Min-Sik Kim, Youn Soo Lee
Journal of Pathology and Translational Medicine.2020; 54(5): 411. CrossRef - Human Papillomavirus Testing in Head and Neck Carcinomas: Guideline From the College of American Pathologists
James S. Lewis, Beth Beadle, Justin A. Bishop, Rebecca D. Chernock, Carol Colasacco, Christina Lacchetti, Joel Todd Moncur, James W. Rocco, Mary R. Schwartz, Raja R. Seethala, Nicole E. Thomas, William H. Westra, William C. Faquin
Archives of Pathology & Laboratory Medicine.2018; 142(5): 559. CrossRef - Detection of HPV infection in head and neck cancers: Promise and pitfalls in the last ten years: A meta-analysis
Carolin G�tz, Clara Bischof, Klaus-Dietrich Wolff, Andreas Kolk
Molecular and Clinical Oncology.2018;[Epub] CrossRef - Frequent hepatocyte growth factor overexpression and low frequency of c-Met gene amplification in human papillomavirus–negative tonsillar squamous cell carcinoma and their prognostic significances
Mi Jung Kwon, Dong Hoon Kim, Hye-Rim Park, Hyung Sik Shin, Ji Hyun Kwon, Dong Jin Lee, Jin Hwan Kim, Seong Jin Cho, Eun Sook Nam
Human Pathology.2014; 45(7): 1327. CrossRef - Human papillomavirus‐stratified analysis of the prognostic role of miR‐21 in oral cavity and oropharyngeal squamous cell carcinoma
Yoon Ho Ko, Hye Sung Won, Der Sheng Sun, Ho Jung An, Eun Kyoung Jeon, Min Sik Kim, Han Hong Lee, Jin Hyoung Kang, Chan Kwon Jung
Pathology International.2014; 64(10): 499. CrossRef - Human Papillomavirus Prevalence and Cell Cycle Related Protein Expression in Tonsillar Squamous Cell Carcinomas of Korean Patients with Clinicopathologic Analysis
Miji Lee, Sung Bae Kim, Sang-wook Lee, Jong-Lyel Roh, Seung-Ho Choi, Soon Yuhl Nam, Sang Yoon Kim, Kyung-Ja Cho
Korean Journal of Pathology.2013; 47(2): 148. CrossRef
- Positive Rate of Human Papillomavirus and Its Trend in Head and Neck Cancer in South Korea
- Human Papillomavirus Prevalence in Gangwon Province Using Reverse Blot Hybridization Assay.
- Dongsup Lee, Sunghyun Kim, Sangjung Park, Hyunwoo Jin, Tae Ue Kim, Kwang Hwa Park, Hyeyoung Lee
- Korean J Pathol. 2011;45(4):348-353.
- DOI: https://doi.org/10.4132/KoreanJPathol.2011.45.4.348
- 4,567 View
- 31 Download
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Human papillomavirus (HPV) plays an important role in the development of cervical carcinoma. Although there is a general agreement that high levels of HPV are related to cervical cancer, the prevalence and distribution of HPV genotypes seems to vary by geographical region. This study was designed to investigate the prevalence of HPV genotypes in Gangwon Province, Korea.
METHODS
In total, 342 samples were examined by Pap smear and HPV-ID(R) reverse blot hybridization assay (REBA) (M&D, Wonju, Korea).
RESULTS
Overall HPV positivity was 80.9% and 64.4% in women with abnormal and normal cytology by REBA, respectively. The five most common HPV types were: HPV 16, 53, 58, 56, and 33 in samples with abnormal cytology, and HPV 16, 53, 58, 70, and 18 in samples with normal cytology.
CONCLUSIONS
The REBA can provide useful data regarding prevalence of HPV genotypes. Gangwon Province showed high prevalence of HPV infection in women. The most common HPV type in Gangwon Province was HPV16, and HPV 53, 58, 56, 70 were frequently present. -
Citations
Citations to this article as recorded by- Human Papillomavirus (HPV69/HPV73) Coinfection associated with Simultaneous Squamous Cell Carcinoma of the Anus and Presumed Lung Metastasis
Stephanie Shea, Marina Muñoz, Stephen C. Ward, Mary B. Beasley, Melissa R Gitman, Michael D Nowak, Jane Houldsworth, Emilia Mia Sordillo, Juan David Ramirez, Alberto E. Paniz Mondolfi
Viruses.2020; 12(3): 349. CrossRef - Distribution of Oncogenic Human Papillomavirus Genotypes at High Grade Cervical Lesions above CIN 2 Grade with Histological Diagnosis
Geehyuk Kim, Sungyoung Park, Hye-young Wang, Sunghyun Kim, Sangjung Park, Kwangmin Yu, Boohyung Lee, Seung-Ju Ahn, Eun-Joong Kim, Dongsup Lee
Biomedical Science Letters.2016; 22(2): 37. CrossRef - Human Papillomavirus Prevalence and Distribution according to Age among Korean and Chinese Women
Geehyuk Kim, Sunghyun Kim, Sunyoung Park, Sangjung Park, Han Lin, Yubo Ren, Li Yingxue, In Soo Lee, Jae Dal Lee, Dongsup Lee
Korean Journal of Clinical Laboratory Science.2015; 47(4): 259. CrossRef - Comparison of Methods for Measuring Histamine by ELISA and HPLC-MS Assay In Vitro
In Hee Lee, Yoo Hyun Kim
Korean Journal of Clinical Laboratory Science.2015; 47(4): 306. CrossRef - Diagnostic Performance of HPV E6/E7 mRNA and HPV DNA Assays for the Detection and Screening of Oncogenic Human Papillomavirus Infection among Woman with Cervical Lesions in China
Hye-young Wang, Dongsup Lee, Sunyoung Park, Geehyuk Kim, Sunghyun Kim, Lin Han, Ren Yubo, Yingxue Li, Kwang Hwa Park, Hyeyoung Lee
Asian Pacific Journal of Cancer Prevention.2015; 16(17): 7633. CrossRef - Uncommon and Rare Human Papillomavirus Genotypes Relating to Cervical Carcinomas
Na Rae Kim, Myunghee Kang, Soon Pyo Lee, Hyunchul Kim, Jungsuk An, Dong Hae Chung, Seung Yeon Ha, Hyun Yee Cho
Korean Journal of Pathology.2014; 48(1): 43. CrossRef
- Human Papillomavirus (HPV69/HPV73) Coinfection associated with Simultaneous Squamous Cell Carcinoma of the Anus and Presumed Lung Metastasis
- The Analysis and Clinical Usefulness of HPV DNA Chip Test in the Uterine Cervix.
- Joo hyeon Jeong, Hyun Yee Cho, Na Rae Kim, Dong Hae Chung, Sanghui Park, Seung Yeon Ha
- Korean J Pathol. 2010;44(1):77-82.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.1.77
- 4,450 View
- 27 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The genotypes of human papillomavirus (HPV) are important in carcinogenesis in uterine cervical cancer and may be different in geographic distribution.
METHODS
In 2,086 women, we analyzed the prevalence of HPV and HPV genotypes in uterine cervix by HPV-DNA chip test (n = 2,086), cytology (PAP smear, n = 1997) and biopsy (n = 546).
RESULTS
Of the 2,086 cases, 1,019 cases (48.8%) were HPV-positive and 1,067 cases (51.2%) were negative for HPV. Single infection occurred most commonly (72.1% of women). HPV genotypes in the high-risk and low-risk groups, respectively were HPV-16/-58/-18/-52/-53 and HPV-70/-6/-11. The detection rates of HPV-70 in subjects older than 50 years increased significantly (p < 0.05). Infection in high risk subjects was detected in high grade lesions compared with infection in low risk subjects (p < 0.05).
CONCLUSIONS
HPV-16/-58/-18/-52/-53/-70/-6/-11 genotypes were common in the patient group similar to findings in East Asia. HPV-70 infection is predominant in those older than 40 years. -
Citations
Citations to this article as recorded by- Current Status of and Perspectives on Cervical Cancer Screening in Korea
Sung-Chul Lim, Chong Woo Yoo
Journal of Pathology and Translational Medicine.2019; 53(4): 210. CrossRef - Cervical cytology of atypical squamous cells, cannot exclude high-grade squamous intra-epithelial lesion: significance of age, human papillomavirus DNA detection and previous abnormal cytology on follow-up outcomes
Chang Ohk Sung, Young Lyun Oh, Sang Yong Song
European Journal of Obstetrics & Gynecology and Reproductive Biology.2011; 159(1): 155. CrossRef - Cytomorphologic Features According to HPV DNA Type in Histologically Proven Cases of the Uterine Cervix
In Ho Choi, So-Young Jin, Dong Wha Lee, Dong Won Kim, Yoon Mi Jeen
The Korean Journal of Pathology.2011; 45(6): 612. CrossRef
- Current Status of and Perspectives on Cervical Cancer Screening in Korea
- Prevalence and Genotype Distribution of Cervical Human Papillomavirus DNA in Korean Women: A Multicenter Study.
- Sung Ran Hong, In Sun Kim, Dong Won Kim, Mi Jin Kim, Ae Ree Kim, Young Ok Kim, Hye Sun Kim, Seo Hee Rha, Gyeong Sin Park, Yong Koo Park, Yong Wook Park, Ho Sung Park, Kwang Sun Suh, Jin Hee Sohn, Mi Kyung Shin, Hoon Kyu Oh, Ki Jung Yun, Hye Kyoung Yoon, Shi Nae Lee, Ah Won Lee, Hyo Jin Lee, Hyun Yee Cho, Chan Choi, Woon Won Jung
- Korean J Pathol. 2009;43(4):342-350.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.342
- 6,342 View
- 63 Download
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
DNA prevalence and type distribution of human papillomavirus (HPV) varies geographically. We investigated HPV prevalence and type distribution in Korean women using the MyHPV DNA chip testing. Methods: A total of 2,368 women from five regions of the country underwent Pap smear examination and MyHPV chip testing. Results: Overall HPV positivity was 15.8% and 78.4% in women with normal and abnormal cytology, respectively. High-risk HPV infection was strongly correlated with cytological atypia. In women with abnormal cytology, the five most common HPV types were 16, 58, 18, 52, and 56/53, and HPV16 was significantly the most common type in most geographical regions. After HPV16, HPV58, and 52 were the next most frequently detected types. Women with normal cytology, in contrast, showed heterogeneity in HPV type distribution. High-grade intraepithelial lesions infected with HPV16, 18, 31 or 45 are more likely to progress to carcinoma. Conclusions: The HPV chip test can provide useful data regarding HPV positivity and type. The most common HPV type in Korean women with abnormal cytology is HPV16, with HPV58 and 52 being frequently present. Our data may have important implications for vaccination programs and the development of cervical screening. -
Citations
Citations to this article as recorded by- HPV genotyping by L1 amplicon sequencing of archived invasive cervical cancer samples: a pilot study
Charles D. Warden, Preetam Cholli, Hanjun Qin, Chao Guo, Yafan Wang, Chetan Kancharla, Angelique M. Russell, Sylvana Salvatierra, Lorraine Z. Mutsvunguma, Kerin K. Higa, Xiwei Wu, Sharon Wilczynski, Raju Pillai, Javier Gordon Ogembo
Infectious Agents and Cancer.2022;[Epub] CrossRef - Enhanced disease progression due to persistent HPV-16/58 infections in Korean women: a systematic review and the Korea HPV cohort study
Jaehyun Seong, Sangmi Ryou, JeongGyu Lee, Myeongsu Yoo, Sooyoung Hur, Byeong-Sun Choi
Virology Journal.2021;[Epub] CrossRef - Comparison of FFPE histological versus LBP cytological samples for HPV detection and typing in cervical cancer
Geehyuk Kim, Hyemi Cho, Dongsup Lee, Sunyoung Park, Jiyoung Lee, Hye-young Wang, Sunghyun Kim, Kwang Hwa Park, Hyeyoung Lee
Experimental and Molecular Pathology.2017; 102(2): 321. CrossRef - Distribution of Oncogenic Human Papillomavirus Genotypes at High Grade Cervical Lesions above CIN 2 Grade with Histological Diagnosis
Geehyuk Kim, Sungyoung Park, Hye-young Wang, Sunghyun Kim, Sangjung Park, Kwangmin Yu, Boohyung Lee, Seung-Ju Ahn, Eun-Joong Kim, Dongsup Lee
Biomedical Science Letters.2016; 22(2): 37. CrossRef - Human Papillomavirus Prevalence and Genotype Distribution in Normal and ASCUS Specimens: Comparison of a Reverse Blot Hybridization Assay with a DNA Chip Test
Sunghyun Kim, In-soo Lee, Dongsup Lee
Biomedical Science Letters.2015; 21(1): 32. CrossRef - Genotype Analysis of Human Papilloma Virus Infection in Accordance with Cytological Diagnoses
Mi-Suk Park, Hyun-Wook Cho, Jin-Gak Kim, Nan-Young Bae, Dong-Sun Oh, Ho-Hyun Park
Korean Journal of Clinical Laboratory Science.2015; 47(1): 39. CrossRef - Comparison of the Cobas 4800 HPV and HPV 9G DNA Chip Tests for Detection of High-Risk Human Papillomavirus in Cervical Specimens of Women with Consecutive Positive HPV Tests But Negative Pap Smears
Sun-Young Jun, Eun Su Park, Jiyoung Kim, Jun Kang, Jae Jun Lee, Yoonjin Bae, Sang-Il Kim, Lee-So Maeng, Magdalena Grce
PLOS ONE.2015; 10(10): e0140336. CrossRef - Uncommon and Rare Human Papillomavirus Genotypes Relating to Cervical Carcinomas
Na Rae Kim, Myunghee Kang, Soon Pyo Lee, Hyunchul Kim, Jungsuk An, Dong Hae Chung, Seung Yeon Ha, Hyun Yee Cho
Korean Journal of Pathology.2014; 48(1): 43. CrossRef - Evaluation of Human Papillomavirus Genotyping from Formalin-fixed Paraffin-embedded Specimens in Cervical Cancers
Hyunwoo Jin
Journal of Life Science.2014; 24(9): 1025. CrossRef - Comparative Evaluation of the HPV28 Detection and HPV DNA Chip Test for Detecting and Genotyping Human Papillomaviruses
Eunsim Shin, Heojin Bae, Wan-Keun Song, Sun-Kyung Jung, Yoo-Sung Hwang
Laboratory Medicine Online.2013; 3(4): 234. CrossRef - Significance of HPV-58 Infection in Women Who Are HPV-Positive, Cytology-Negative and Living in a Country with a High Prevalence of HPV-58 Infection
Joon Seon Song, Eun Ju Kim, Jene Choi, Gyungyub Gong, Chang Ohk Sung, Robert D. Burk
PLoS ONE.2013; 8(3): e58678. CrossRef - REBA HPV‐ID® for efficient genotyping of human papillomavirus in clinical samples from Korean patients
Sunghyun Kim, Dongsup Lee, Sangjung Park, Tae Ue Kim, Bo‐Young Jeon, Kwang Hwa Park, Hyeyoung Lee
Journal of Medical Virology.2012; 84(8): 1248. CrossRef - Dynamin 2 expression as a biomarker in grading of cervical intraepithelial neoplasia
Yoo-Young Lee, Sang Yong Song, In-Gu Do, Tae-Joong Kim, Byoung-Gie Kim, Jeong-Won Lee, Duk-Soo Bae
European Journal of Obstetrics & Gynecology and Reproductive Biology.2012; 164(2): 180. CrossRef - Cytomorphologic Features According to HPV DNA Type in Histologically Proven Cases of the Uterine Cervix
In Ho Choi, So-Young Jin, Dong Wha Lee, Dong Won Kim, Yoon Mi Jeen
The Korean Journal of Pathology.2011; 45(6): 612. CrossRef - Human Papillomavirus Prevalence in Gangwon Province Using Reverse Blot Hybridization Assay
Dongsup Lee, Sunghyun Kim, Sangjung Park, Hyunwoo Jin, Tae Ue Kim, Kwang Hwa Park, Hyeyoung Lee
The Korean Journal of Pathology.2011; 45(4): 348. CrossRef - Pediatric vulvar squamous cell carcinoma in a liver transplantation recipient: a case report
Na-Rae Kim, Soyi Lim, Hyun Yee Cho
Journal of Gynecologic Oncology.2011; 22(3): 207. CrossRef
- HPV genotyping by L1 amplicon sequencing of archived invasive cervical cancer samples: a pilot study
- The Usefulness of the HPV DNA Microchip Test for Women with ASC-US.
- Hee Eun Kyeong, Seung Yeon Ha, Dong Hae Chung, Na Rae Kim, Sanghui Park, Hyun Yee Cho
- Korean J Pathol. 2009;43(3):254-259.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.3.254
- 4,089 View
- 28 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
This study was performed to ascertain the usefulness of the human papillomavirus (HPV) DNA microchip test for the screening and management of women with atypical squamous cells of undetermined significance (ASC-US).
METHODS
The subject group consisted of 534 patients, and all of whom were diagnosed as ASC-US according to a Papanicolaou smear, and they all underwent concomitant HPV DNA microchip test.
RESULTS
The occurrence rates of overall squamous lesions and high risk lesion (cervical intraepithelial neoplasia grade 2 and grade 3, and invasive carcinoma) of the HPV-positive ASC-US patients were significantly higher than those of the HPV-negative ASC-US patients. High risk lesion was detected more frequently among the older patients and the patients with HPV 56, 33 or 70. On the follow-up HPV DNA microchip test, only 1 of 11 (9.1%) HPV type-switched women developed squamous lesion compared with 8 of 13 (61.6%) HPV type-persistent women who developed squamous lesion.
CONCLUSIONS
The HPV DNA microchip test is useful for the management of ASC-US patients. HPV-positive ASC-US patients should undergo a HPV DNA microchip test periodically. If the same genotype of HPV is persistent on the follow-up test, more increased surveillance is needed. -
Citations
Citations to this article as recorded by- Enhanced disease progression due to persistent HPV-16/58 infections in Korean women: a systematic review and the Korea HPV cohort study
Jaehyun Seong, Sangmi Ryou, JeongGyu Lee, Myeongsu Yoo, Sooyoung Hur, Byeong-Sun Choi
Virology Journal.2021;[Epub] CrossRef
- Enhanced disease progression due to persistent HPV-16/58 infections in Korean women: a systematic review and the Korea HPV cohort study
- Human Papillomavirus Infection and Its Relationship to Cervical Intraepithelial Neoplasia: An immunohistochemical, histopathological and Cytological Study.
- Mi Jin Kim, Won Hee Choi, Tae Sook Lee
- Korean J Pathol. 1989;23(2):240-253.
- 2,032 View
- 13 Download
-
 Abstract
Abstract
 PDF
PDF - It has suggested that a significant proportion of intraepithelial lesion of the cervix may be related to the influence of human papillomaviurs (HPV). Its etiological relation with cervical intraepithelial neoplasia (CIN) and cervical squamous cell carcinoma has recently been proposed. The 131 cases of CIN and 6 condyloma acuminata were stained by immunoperoxidase technique for HPV anigen. The results are as follows: The 18 cases (13.1%) exhibited positive staining, localized in nuclei of koilocytotic cells confined to superficial and intermediate layer of epithelium. HPV antigen was found in 1 case (16.7) of 6 condyloma acuminata, 4 cases (12.5%) of 32 mild dysplasia, 3 cases (13.6%) of 22 moderate dysplasia, 2 cases (14.3%) of 14 severe dysplasia and 8 cases (12.7%) of 63 carcinoma in situ. In the positive cases of mild and moderate dysplasia, HPV antigen was localized directly within the lesion, while those cases of severe dysplaia and carcinoma in situ contained positive cells in areas of mild or moderate dysplasia adjacent to the lesion. Of three distinct morphologic patterns, flat type was most common and papillary type was least. Histologically condylomatous lesions were present in 67 cases (51.1%) out of 131 cases of CIN. The histological and cytological feature encountered most frequently was koilocytotic arypia. Other main histological features are bi- or multinucleation, exocytosis of inflammatory cells, acanthosis, mitotic figures, dyskeratosis and epithelial pearl. On the cervical smear, the evidence of condyloma was proved in 50.0%. Cytologically in the condyloma with high degree of CIN, the nuclear atypia was so prominent that the differentiation from dysplasia or carcinoma in situ was very difficult, although the chromatin appeared somewhat smudged. The mean age of 18 cases was 42.4 years which is older than previous study. The results of this study provide common association with HPV and CIN and add great weight to the suggestion that the infection with HPV plays an important part in genesis of cervical cancer.
- Primary Squamous Cell Carcinoma of the Endometrium Covering Submucosal Leiomyoma.
- Myoung Ja Chung, Dong Geun Lee
- Korean J Pathol. 1999;33(1):65-67.
- 2,311 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - Primary squamous cell carcinoma of the endometrium is exceedingly rare. To be accepted as a primary carcinoma of the endometrium, the tumor must satisfy the criteria estalished by Fluhmann: There must be; 1) no coexisting endometrial adenocarcinoma, 2) no connection between the endometrial tumor and the squamous epithelium of the cervix, and 3) no squamous cell carcinoma of the cervix. We recently experienced a case of primary squamous cell carcinoma of the endometrium covering the submucosal leiomyoma in a 68-year-old female patient. On gross examination a submucosal leiomyoma covered by an irregular, dirty endometrium was found. On histologic examination the endometrium covering the leiomyoma revealed invasive, well differentiated squamous cell carcinoma. The uterine cervix showed no evidence of malignancy. In situ PCR using a probe for HPV 16/18 was negative in the carcinoma tissue.
- Detection of Human Papillomavirus in Lesions of Uterine Cervix Immunohistochemistry and in situ Hybridization.
- Chang Soo Park, Jong Hee Nam, Jae Hyuk Lee, Jong Soon Kim, Seung Jin Oh
- Korean J Pathol. 1997;31(4):289-297.
- 2,153 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - To evaluate the detection of HPV DNA according to subtype of lesions of uterine cervix and its clinical applicability, in situ hybridization (ISH) and immunohistochemistry for HPV were performed in 189 cases of uterine cervical lesion, including 23 cases of low grade squamous intraepithelial lesion (SIL), 115 cases of high grade SIL and 51 cases of invasive carcinoma. Positive immunostaining, brown precipitate, was mainly noted in the nucleus of koilocytes in the superficial and intermediate layer. Positivity of immunostaining was 21.7% in low grade SIL, 13.0% in high grade SIL and 9.8% in invasive carcinoma. Positive reaction in ISH, red precipitate, was noted in the nucleus of not only koilocytes but also non-koilocytes in the superficial and intermediate layer, and dot precipitate was rarely identified in the nest of squamous cell carcinoma. Based on HPV subtype, 6/11 was 21.7% in low grade SIL, 16/18 was 32.2% and 39.2% in high grade SIL and invasive carcinoma, respectively. With regard to their associated HPV types, low grade SILs were heterogeneous and high grade SILs and invasive carcinomas were related with the high oncogenic risk group only. The correlation of HPV subtypes with panHPV was 91.3% in low grade SIL, 91.3% in high grade SIL and 98.0% in invasive carcinoma. These results suggest that detection of HPV infection by ISH may be a more useful method than immunohistochemistry and application of the HPV subtype probe with the panHPV probe could improve the sensitivity of ISH.
- Detection of Human Papillomavirus DNA 16/18 in Cervical Adenocarcinomas by Polymerase Chain Reaction.
- Sang Sook Lee, Nam Jo Park, Chong Guk Yoon
- Korean J Pathol. 1995;29(4):502-510.
- 2,422 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - Twenty-five paraffin-embedded tumor tissues were analyzed for detection of HPV 16 and 18 in cervical adenocarcinoma by polymerase chain reaction with type specific primers and by non-radioactive Southern blot hybridization for confirmation . The suitability of paraffin-embedded tissue as PCR material was confirmed by successful amplification of 100% of cervical specimens with human -globin specific primer. Eighty four percent of the cervical adenocarcinoma tissues were positive for HPV 16 and/or 18. HPV 16 positive rate was 68%, HPV 18 was 60%. The double infection with HPV 16 and 18 was found in 44%. Three cases of the negative specimen in PCR for each type of HPV DNA 16 and 18 were positive in Southern blot hybridization. The total positive rate was 92% for HPV 16 and/or HPV 18, HPV 16 positive rate was 80%. HPV 18 was 72%. The double infection with HPV 16 and 18 was 60%. These results suggest that the pattern of HPV types 16 and 18 is closely associated with carcinogenesis of cervical cancers. HPV type 18 appears to be preferentially related to cervical adenocarcinoma and the poor prognosis of these patients. Therefore, determination of HPV DNA type in cervical carcinoma patients is important in treatment and prognosis.
- Immunohistochemical Expression of p53, p21, and mdm2 Proteins in Human Papillomavirus Positive and Negative Invasive Uterine Cervical Carcinomas.
- In Seo Park, Hye Seung Han, Tae Sook Kim, Jee Young Han, Joon Mee Kim, Young Chae Chu, Tae Sook Hwang
- Korean J Pathol. 2001;35(3):212-219.
- 2,313 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
In the uterine cervical carcinoma, the inactivation of p53 protein by human papillomavirus(HPV) E6 protein has been reported to play a greater role in carcinogenesis than the mutation of the p53 gene. Therefore, the mutation of the p53 gene is rare. p21 and mdm2 proteins are induced by wild-type p53 protein and are involved in the cell cycle regulatory mechanism.
METHODS
Immunohistochemical staining for p53, p21 and mdm2 proteins was performed in 26 HPV-positive and 13 HPV-negative invasive cervical carcinomas together with 5 non-neoplastic cervical tissues.
RESULTS
The frequencies of the expression of p53, p21 and mdm2 proteins were 82.1%, 84.6% and 66.7%, respectively. The expression of p53 protein was less frequently demonstrated in HPV-positive cases than HPV-negative cases, which was statistically a negative correlation(p=0.018). The expression of p53 and p21 proteins was statistically significant(p=0.000).
CONCLUSIONS
p53, p21 and mdm2 proteins were highly expressed in both HPV-positive and HPV-negative cervical carcinomas. Significantly higher expression of p53 protain in HPV-negative cases necessitate a further study for investigating the role of p53 protein accumulation in carcinogenesis of HPV-negative cervical carcinomas. The relationship between the expression of p53 protein and p21/mdm2 proteins may indicate that p21 and mdm2 proteins also have a role in carcinogenesis, where p53 protein plays a fundamental role.
- Nasal Inverted Papilloma Associated With Squamous Cell Carcinoma: A Report of Two Cases.
- Mi Jin Gu, Dong Sug Kim, Young Kyung Bae, Yong Dae Kim
- Korean J Pathol. 2001;35(3):248-281.
- 2,123 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - Nasal inverted papilloma (IP) is a benign neoplasm that may be associated with squamous cell carcinoma (SCC). Several studies have suggested that human papilloma virus 16/18 (HPV 16/18) and p53 are closely related to the pathogenesis of IP with transformation to squamous cell carcinoma (IP-SCC). This study was conducted to investigate the role of HPV 16/18 and p53 in the pathogenesis of IP-SCC using immunohistochemistry. We studied two cases of IP-SCC and 10 cases of IP. None of the IP cases presented positivity for HPV 16/18 or p53 protein. Two cases of IP-SCC showed negative reactions for HPV 16/18. The SCC portion of the IP-SCC showed strong positivity for p53, while the IP portion of the IP-SCC was negative for p53. MIB-1 labeling index (LI) was estimated in the IP cases and the IP-SCC as well. In terms of MIB-1 LI, there was no statistical significance between IP and IP-SCC, and between the IP portion and the SCC portion in the cases of IP-SCC. In conclusion, we believe that alteration of the p53 protein is related to IP with malignant transformation, but further studies are required to investigate the correlation of HPV 16/18 and p53 in the pathogenesis of IP with malignant transformation, and the significance of the MIB-1 LI and p53 as biomarkers in IP.
- Human Papillomavirus Type 16, 18, and 33 Infection in Adenocarcinoma of the Uterine Cervix: Analysis of the p53 Gene Mutation and the Clincopathologic Correlation.
- Kwang Sun Suh, Seong Jun Cho, Sun Young Na, Heung Tae Noh, Sang Ryun Nam
- Korean J Pathol. 2004;38(5):295-300.
- 2,111 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Current evidence implicates specific types of the human papillomavirus (HPV) are involved in the development of cervical cancer. In HPV-negative cervical carcinomas, p53 mutation is thought to be a mechanism of oncogenesis. The purpose of this study was to evaluate the prevalence of p53 mutations in cervical adenocarcinomas and to investigate their correlation with HPV status and clinicopathologic parameters.
METHODS
A series of 38 primary cervical adenocarcinomas was analyzed for both HPV infection and p53 mutations. The HPV 16, 18, and 33 status was investigated by PCR amplification. The point mutations of the p53 gene were detected by the PCR-SSCP technique.
RESULTS
The prevalence of HPV 16, 18, or 33 infection was 73.7% (28/38). HPV 16 was present in 12 cases, HPV 18 was present in 15 cases, and HPV 33 was positive in one case. There was only one case that was positive for 18 as well as a p53 mutation in exon 6.
CONCLUSIONS
Our results indicate that HPV 18 infection was more common in cervical adenocarcinomas than HPV 16 infection. Mutant p53 was rarely found in cervical adenocarcinomas regardless of the type of HPV infection. There was no correlation between HPV infection and clinical stage or pathologic type of tumor.
- Histologic and Clinical Characteristics of Skin Warts According to the Human Papillomavirus Antigen Expression.
- Kun Chang Song, Kwang Gil Lee
- Korean J Pathol. 1993;27(4):379-386.
- 2,922 View
- 52 Download
-
 Abstract
Abstract
 PDF
PDF - Skin wart is an infectious disease of human papillomavirus(HPV). Its clinical and histopathologic characteristics are largely determined by lesion sties, viral type and host immunity. The infected basal cells and keratinocytes of the epidermis are induced to proliferate by the viral genome. It is, however, not well known how htose factors give rise to histopathologic alterations in the infected basal cells and keratinocytes. So, evaluation of correlation between HPV antigen expression in the wart tissues and clinical and histopathologic charateristics was done on 83 cases of skin warts. The age of patients ranged from 2 to 83 years. Thirty six(43.3%) cases were diagnosed before the age of third decade. The sex ratio was nearly same. Verruca vulgaris was most common(46 cases), followed by verruca plana(26 cases) and verruca palmoplantaris(11 cases). HPV antigen expression was observed in 43 out of total 83(51.8%). It was noted in 47.8%(22/46) of verruca vulgaris, in 46.2%(12/26) of verruca plana and in 81.8%(9/11) of verruca palmoplantaris. HPV antigen-positive groups included more younger patient's age and more higher PCNA than those of HPV negative groups. HPV positive groups also tend to have shorter duration of disease and more numerous mitoses than HPV negative groups. HPV antigen-positive groups showed lower inflammation grade than that of HPV negative groups(p<0.05). The higher the inflammaton grade is, the lower the HPV antigen expression rate. In summary, HPV antigen expression in cutaneous wart tissue is significantly correlated with the proliferative activity of the lesion. It is also significantly correlated with the inflammation that is considered to be the result of cell-mediated immune reaction.
- Atypical Condyloma of Uterine Cervix: It's Cytological Similarity to Squamous Cell Carcinoma.
- Chan Kum Park, Myung Sook Kim, Jung Dal Lee
- Korean J Pathol. 1990;24(3):310-315.
- 2,469 View
- 32 Download
-
 Abstract
Abstract
 PDF
PDF - Atypical condyloma is a variant of flat condyloma characterized by the presence of atypical koilocytes having large hyperchromatic, smudged and often bizarre nuclei. Atypical condyloma can be frequently misdiagnosed on cytologic smear and on tissue sections by its marked cellular atypia, as high grade dysplasia, in situ or even invasive squamous cell carcinoma. We described two cases of atypical condyloma of the female genital tract. The cytologic features and histologic changes were reminiscent of those of invasive squamous cell carcinoma and severe degree of dysplasia of the uterine cervix. The differential findings between atypical condyloma and squamous cell carcinoma were discussed in detail.
- Prevalence of Human Papillomavirus Infection in Women in South Korea: Incidence of Positive HPV DNA and anti-VLPs in Residents of Busan City.
- Sook Hee Hong, Duk Hee Lee, Hai Rim Shin
- J Pathol Transl Med. 2004;15(1):17-27.
- 2,195 View
- 22 Download
-
 Abstract
Abstract
 PDF
PDF - To investigate a population-based survey of the prevalence of human papillomavirus (HPV) infection in South Korea, we performed Papanicolaou smears and tests for HPV DNA and anti-HPV antibody detection in 909 sexually active general women (age range; 20-74 years, median 44 years) who were randomly selected residents from S district of Busan City. The presence of DNA of 36 different HPV types was detected by means of a GP 5+/6+ primer-mediated PCR enzyme immunoassay in cervical exfoliated cells, and IgG antibodies against L1 virus-like particles (anti-VLPs) of 5 HPV types 16, 18, 31, 33, and 58 were tested by means of enzyme linked immunoassay. The incidence of cytologic abnormality was 5.2% in Pap smear. The positive rate of HPV DNA was 10.4%, high in young women younger than 35 years old and proportionally increased according to the cytologic grades. The most often found HPV type was HPV 70, followed by HPV 16 and 33, and high-risk HPV types were more frequent in women younger than 35 years old. The most common HPV type in abnormal cytologic smears was HPV 16, followed by HPV 58 and 66. Anti-VLPs was positive in 19.7% and the frequent anti-VLPs type was against HPV 18, followed by HPV 31 and 16. The concordance between the markers for each specific HPV type was noted in 10 women and HPV 16 was the most frequent one. The incidence of multiple HPV infection was 18.9% and that of multiple anti-VLPs antibodies was 31%. Among 103 self-reported virgins, 4.9% had anti-VLP antibodies.
- The Usefulness of Concomitant High-Risk Human Papillomavirus Test and Colposcopy in Combination with the Papanicolaou Test in ASCUS Patients.
- Min Kyung Kim, Jin Hee Sohn, Chul Hwan Kim, Jong Sang Choi
- J Pathol Transl Med. 2005;16(1):18-24.
- 2,037 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - The objective of this study was to ascertain whether or not the high-risk human papillomavirus(HPV) test, when coupled with Papanicolaou(Pap) smears, would prove useful in the screening and management of patients in whom abnormal Pap smear results had been obtained. Concomitant high-risk HPV detection using the hybrid capture II test and colposcopy with a Pap smear were performed with 176 patients, all of whom had been screened for both cervical carcinoma and precancerous lesions. We concomitantly performed colposcopies on these patients. Upon the follow-ups, the histologic diagnoses of these patients were confirmed via either biopsy or hysterectomy. The rate of high-risk HPV detection was correlated with cytologic diagnoses and colposcopic findings. The group composed of the high-risk HPV-positive ASCUS patients exhibited a 55.7% rate of cervical intraepithelial neoplasia(CIN), a significantly higher rate than the 7.5% result obtained in the high-risk HPV- negative ASCUS group. HPV test showed high sensitivity(87%) and low specificity (62.6%) in detection of CIN and colposcopy also showed high sensitivity (88%) and low specificity(22%). Any combination of these tests improve sensitivity, but not specificity. High-risk HPV tests, when coupled with Pap smears, constituted a useful triage approach with regard to colposcopy-directed biopsies in patients in whom a cytologic diagnosis of ASCUS had been rendered.
- Comparison of Efficacy of Human Papilloma Virus Genotyping Assays using Restriction Fragment Mass Polymorphism and DNA Chip Analysis in Patients with Abnormal Pap Smear and Uterine Cervical Cancer.
- Hyun Jae Chung, Sung Nam Kim, Eun Hee Lee, Mi Sun Jee, Min A Kim, Sun Young Hwang, Hee Jung Cho, Soo Ok Kim, Sun Pyo Hong
- Korean J Pathol. 2006;40(6):439-447.
- 2,173 View
- 24 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
High-risk human papilloma virus (HPV) infection is the primary cause of cervical cancer; there is a need for more sensitive and reliable methods for HPV genotyping to use as screening tools for early detection and intervention. METHODS: A novel MALDI-TOF MSbased assay, termed Restriction Fragment Mass Polymorphism (RFMP) was developed for multiple HPV genotyping. Its performance was compared with DNA chip technology. The study was based on 164 cases classified as normal (n=40), ASCUS (n=53) and invasive squamous cell carcinoma (SCC, n=71) by a PAP smear and/or cervical colposcopic biopsy.
RESULTS
High-risk genotypes were detected in 7.5%, 47.2% and 97.2% in normal, ASCUS and SCC groups by RFMP, and in 20.0%, 41.5% and 90.1% using DNA chip technology, respectively. The results showed substantial concordance, with a kappa coefficient of 0.688, between the methods. Diagnostic sensitivity and specificity for cervical cancer were found to be 97.2% and 92.2% with RFMP and 90.1% and 80.0% using DNA chip microarrays.
CONCLUSIONS
RFMP and DNA chip technologies were shown to be reliable methods for HPV genotyping with a high concordance. The improved sensitivity and specificity should make RFMP a viable option for the management of women with cervical neoplastic lesions.
- Tetranucleotide Repeat Microsatellite Instability in Uterine Cervical Carcinomas.
- Yoo Duk Choi, Ji Shin Lee, Chan Choi, Chang Soo Park, Sang Woo Juhng, Ho Sun Choi, Jong Hee Nam
- Korean J Pathol. 2007;41(1):30-37.
- 2,174 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Elevated levels of microsatellite alterations at selected tetranucleotide repeat regions (EMAST) have been recently described, and they are a distinct type of microsatellite instability (MSI). We investigated the prevalence of EMAST in squamous cell carcinoma (SCC) of the uterine cervix and we determined the correlation between EMAST and the clinicopathologic parameters, HPV infection and the p53 mutation.
METHODS
We examined the 3 mono-, 3 di-, and 5 tetranucleotide repeat markers in 47 cases of SCC, and we performed immunohistochemical staining for p53. HPV detection and genotyping was performed using a commercially available HPV DNA chip.
RESULTS
Thirteen out of 47 cases (27.7%) were EMAST(+) with at least one of five tetranucleotide repeat markers. However, MSI at mono- and dinucleo- tide markers was noted in only one case (2.1%). EMAST was not related with stage, size, lymph node metastasis, vascular/lymphatic invasion or the depth of invasion. Positive immunostaining for p53 was significantly more common in EMAST(+) tumors than in the EMAST(-) tumors (p=0.04). HPV-infection was positive in 32 cases. EMAST was not correlated with the state of HPV infection state or the HPV genotype.
CONCLUSIONS
27.7% of the invasive SCCs of the uterine cervix exhibited EMAST, and EMAST in the SCC of the uterine cervix was significantly associated with the p53 mutation.
- Immunohistochemical Analysis of Midkine Expression in Preinvasive and Invasive Squamous Cell Neoplasia of the Uterine Cervix.
- Suk Jin Choi, Eun Seop Song, Lucia Kim, In Suh Park, Jee Young Han, Joon Mee Kim, Young Chae Chu
- Korean J Pathol. 2007;41(2):79-86.
- 2,091 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Midkine (MK) is a member of the heparin-binding growth factor family. Overexpression of MK is observed not only in cancerous tissue but also in precancerous lesions of the colon and the prostate. Using immunohistochemical methods, we investigated MK expression in preinvasive and invasive neoplasia of the uterine cervix.
METHODS
We performed immunohistochemical analysis of archived cone biopsy and hysterectomy specimens from 161 squamous cell lesions of the uterine cervix (29 cervical intraepithelial neoplasia 1 (CIN1), 35 CIN2, 49 CIN3, 30 microinvasive squamous cell carcinomas (MIC), and 18 invasive squamous cell carcinoma). In addition, we examined if there is a correlation between MK expression and status of human papilloma virus infection determined by a commercially available DNA chip.
RESULTS
None of the normal cervical mucosa showed MK immunostaining. The level of MK expression gradually increased according to the histologic grade. Moderate and strong expressions were most frequently observed in cervical tissue with CIN3 and MIC. MK immunostaining was more accentuated in the invasive border of MIC.
CONCLUSION
MK may play a functional role in the disease progression of cervical squamous cell neoplasia.
- Epidermoid Cyst of the Sole: A report of two cases positive for human papillomavirus.
- Eun Joo Seo, Hi Jeong Kwon, Ki Ouk Min, Hyun Jeong Lee, Byung Kee Kim
- Korean J Pathol. 2000;34(12):1025-1028.
- 1,983 View
- 25 Download
-
 Abstract
Abstract
 PDF
PDF - Epidermoid cysts occur rarely on the palms and soles, where hair is not present. These cysts have long been assumed to arise from traumatic implantation of epidermal fragment, but the pathogenesis is still controversial. Recently, with microscopic findings, immunohistochemical features, and molecular studies, the epidermoid cysts of the sole may be induced by the human papillomavirus. We report two cases of epidermoid cysts of the sole with the discussion of the pathogenesis.

 E-submission
E-submission






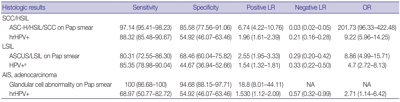
 First
First Prev
Prev



