Search
- Page Path
- HOME > Search
- Characteristics of RET gene mutations in Vietnamese medullary thyroid carcinoma patients: a single-center analysis
- Van Hung Pham, Quoc Thang Pham, Minh Nguyen, Hoa Nhat Ngo, Thao Thi Thu Luu, Nha Dao Thi Minh, Trâm Đặng, Anh Tu Thai, Hoang Anh Vu, Dat Quoc Ngo
- J Pathol Transl Med. 2025;59(2):125-132. Published online March 14, 2025
- DOI: https://doi.org/10.4132/jptm.2025.01.18
- 4,955 View
- 182 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
The RET gene point mutation is the main molecular alteration involved in medullary thyroid carcinoma (MTC) tumorigenesis. Previous studies in Vietnam mainly consisted of case reports, with limited data on larger sample sizes. In this study, we investigated RET gene mutations in exons 10, 11, and 16 and analyzed clinicopathological features of a series of Vietnamese MTC patients. Methods: We collected 33 tissue samples from patients with MTC and analyzed RET mutations using the Sanger sequencing method. The relationship between hotspot RET mutations (exons 10, 11, 16) and clinicopathological features were investigated. Results: Among the 33 analyzed cases, 17 tumors (52%) harbored RET mutations in exon 10, 11, or 16. A total of 10 distinct genetic alterations were identified, including eight missense mutations and two short indels. Of these, seven were classified as pathogenic mutations based on previous publications, with p.M918T being the most frequent (4 cases), followed by p.C634R (3 cases) and p.C618R (3 cases). Mutations were significantly associated with specific histological patterns, such as the nested/insular pattern (p=.026), giant cells (p=.007), nuclear pleomorphism (p=.018), stippled chromatin (p=.044), and amyloid deposits (p=.024). No mutations were found in germline analyses, suggesting these were somatic alterations. Conclusions: Our results provided the first comprehensive analysis of RET mutations in Vietnamese MTC patients. The most frequent mutation was p.M918T, followed by p.C634R and p.C618R. Mutations in these three exons were linked to specific histopathological features. Information on mutational profiles of patients with MTC will further aid in the development of targeted therapeutics to ensure effective disease management.
- TERT mutations and aggressive histopathologic characteristics of radioiodine-refractory papillary thyroid cancer
- Ju Yeon Pyo, Yoon Jin Cha, SoonWon Hong
- J Pathol Transl Med. 2024;58(6):310-320. Published online September 12, 2024
- DOI: https://doi.org/10.4132/jptm.2024.07.29
- 4,723 View
- 342 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Radioiodine (RI) ablation following thyroid-stimulating hormone suppression is an effective treatment for papillary thyroid cancer (PTC), typically leading to favorable outcomes. However, RI-refractory tumors exhibit aggressive behavior and poor prognoses. Recent studies highlight the role of genetic abnormalities in PTC signaling pathways, including the activation of telomerase reverse transcriptase (TERT), and the correlation of mutations with adverse outcomes.
Methods
This study analyzed mutations in BRAF V600E and the TERT-promoter genes, comparing clinicopathological features between RI-refractory and RI-responsive PTCs. Among 82 RI-refractory patients, formalin-fixed, paraffin-embedded tissues from initial surgeries were available for 26. Another 89 without distant metastasis over 5 years formed a matched RI-responsive control group.
Results
Histopathologically, RI-refractory PTCs showed increased frequencies of small tumor clusters without fibrovascular cores, hobnail features, and a high height-to-width ratio of tumor cells. These tumors were more likely to exhibit necrosis, mitosis, lymph node metastasis, extrathyroidal extension, and involvement of resection margins. TERT-promoter mutations were statistically significantly associated with these aggressive clinicopathologic features. Immunohistochemically, decreased expression of sodium iodide symporter and thyroglobulin stimulating hormone receptor proteins was common in RI-refractory PTCs, along with lower levels of oncogenic proteins such as vascular endothelial cell growth factor, vascular endothelial cell growth factor receptor 2, and nuclear factor kappa-light-chain-enhancer of activated B cells. Total loss of PTEN expression was occasionally observed. In contrast, all cases tested positive for cytoplasmic β-catenin.
Conclusions
RI-refractory PTCs are linked to TERT mutations and exhibit specific aggressive histopathologic features, particularly in tumor centers. -
Citations
Citations to this article as recorded by- Characterizing thyroid carcinomas in the elderly: Histological subtypes and TERT promoter mutation analysis based on the latest WHO classification
Myoung Ju Koh, Songmi Noh, Jin Kyong Kim, Gi Jeong Kim
Annals of Diagnostic Pathology.2026; 80: 152578. CrossRef - The ability of anexelekto (AXL) expression and TERT promoter mutation to predict radioiodine-refractory differentiated thyroid carcinoma
Hasrayati Agustina, Tutik Nur Ayni, Yohana Azhar, Erwin Affandi Soeriadi, Bethy Suryawathy Hernowo
Diagnostic Pathology.2025;[Epub] CrossRef - Clinicopathologic characteristics of papillary thyroid carcinoma, tall cell subtype and subtype with tall cell features, an institutional experience
Xueting Jin, Shunsuke Koga, Xiao Zhou, Niaz Z. Khan, Zubair W. Baloch
Human Pathology.2025; 161: 105867. CrossRef - Calcifying nested stromal-epithelial tumor of the liver: Report of two cases revealing novel WT1 mutation and distinct epigenetic features
Andrea Strakova-Peterikova, Franco Fedeli, Boris Rychly, Jiri Soukup, Michael Michal, Petr Martinek, Marian Grendar, Elaheh Mosaieby, Nikola Ptakova, Maryna Slisarenko, Michal Michal, Kvetoslava Michalova
Virchows Archiv.2025;[Epub] CrossRef - Insulin resistance and metabolic dysfunction in thyroid nodules and differentiated thyroid cancer
Stefano Iuliano, Maria Mirabelli, Stefania Giuliano, Antonio Brunetti
Current Opinion in Oncology.2025;[Epub] CrossRef
- Characterizing thyroid carcinomas in the elderly: Histological subtypes and TERT promoter mutation analysis based on the latest WHO classification
- Colorectal cancer with a germline BRCA1 variant inherited paternally: a case report
- Kyoung Min Kim, Min Ro Lee, Ae Ri Ahn, Myoung Ja Chung
- J Pathol Transl Med. 2024;58(6):341-345. Published online September 5, 2024
- DOI: https://doi.org/10.4132/jptm.2024.08.14
- 6,730 View
- 305 Download
-
 Abstract
Abstract
 PDF
PDF - BRCA genes have well-known associations with breast and ovarian cancers. However, variations in the BRCA gene, especially germline variations, have also been reported in colorectal cancer (CRC). We present the case of a rectal cancer with a germline BRCA1 variation inherited from the paternal side. A 39-year-old male was admitted with rectal cancer. The patient underwent surgical resection and the pathologic diagnosis was adenocarcinoma. Next-generation sequencing was performed and a BRCA1 variant was detected. Reviewing the public database and considering the young age of the patient, the variant was suggested to be germline. The patient’s father had had prostate cancer and next-generation sequencing testing revealed an identical BRCA1 variant. In the BRCA cancer group, there is relatively little attention paid to male cancers. The accumulation of male CRC cases linked to BRCA variations may help clarify the potential pathological relationship between the two.
- Reevaluating diagnostic categories and associated malignancy risks in thyroid core needle biopsy
- Chan Kwon Jung
- J Pathol Transl Med. 2023;57(4):208-216. Published online July 11, 2023
- DOI: https://doi.org/10.4132/jptm.2023.06.20
- 6,983 View
- 267 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF - As the application of core needle biopsy (CNB) in evaluating thyroid nodules rises in clinical practice, the 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules have officially recognized its value for the first time. CNB procures tissue samples preserving both histologic structure and cytologic detail, thereby supplying substantial material for an accurate diagnosis and reducing the necessity for repeated biopsies or subsequent surgical interventions. The current review introduces the risk of malignancy within distinct diagnostic categories, emphasizing the implications of noninvasive follicular thyroid neoplasm with papillary-like nuclear features on these malignancy risks. Prior research has indicated diagnostic challenges associated with follicular-patterned lesions, resulting in notable variation within indeterminate diagnostic categories. The utilization of mutation-specific immunostaining in CNB enhances the accuracy of lesion classification. This review underlines the essential role of a multidisciplinary approach in diagnosing follicular-patterned lesions and the potential of mutation-specific immunostaining to strengthen diagnostic consensus and inform patient management decisions.
-
Citations
Citations to this article as recorded by- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
Agnes Stephanie Harahap, Maria Francisca Ham, Retno Asti Werdhani, Erwin Danil Julian, Rafi Ilmansyah, Chloe Indira Arfelita Mangunkusumso, Tri Juli Edi Tarigan
Journal of Pathology and Translational Medicine.2025; 59(3): 149. CrossRef - Risk Stratification of Thyroid Nodules Diagnosed as Follicular Neoplasm on Core Needle Biopsy
Byeong-Joo Noh, Won Jun Kim, Jin Yub Kim, Ha Young Kim, Jong Cheol Lee, Myoung Sook Shim, Yong Jin Song, Kwang Hyun Yoon, In-Hye Jung, Hyo Sang Lee, Wooyul Paik, Dong Gyu Na
Endocrinology and Metabolism.2025; 40(4): 610. CrossRef - Diagnostic implication of thyroid spherules for cytological diagnosis of thyroid nodules
Heeseung Sohn, Kennichi Kakudo, Chan Kwon Jung
Cytopathology.2024; 35(3): 383. CrossRef - A Narrative Review of the 2023 Korean Thyroid Association Management Guideline for Patients with Thyroid Nodules
Eun Kyung Lee, Young Joo Park, Chan Kwon Jung, Dong Gyu Na
Endocrinology and Metabolism.2024; 39(1): 61. CrossRef - The Diagnostic Role of Repeated Biopsy of Thyroid Nodules with Atypia of Undetermined Significance with Architectural Atypia on Core-Needle Biopsy
Hye Hyeon Moon, Sae Rom Chung, Young Jun Choi, Tae-Yon Sung, Dong Eun Song, Tae Yong Kim, Jeong Hyun Lee, Jung Hwan Baek
Endocrinology and Metabolism.2024; 39(2): 300. CrossRef - Core needle biopsy for thyroid nodules assessment-a new horizon?
David D Dolidze, Serghei Covantsev, Grigorii M Chechenin, Natalia V Pichugina, Anastasia V Bedina, Anna Bumbu
World Journal of Clinical Oncology.2024; 15(5): 580. CrossRef - Educational exchange in thyroid core needle biopsy diagnosis: enhancing pathological interpretation through guideline integration and peer learning
Agnes Stephanie Harahap, Chan Kwon Jung
Journal of Pathology and Translational Medicine.2024; 58(5): 205. CrossRef - A simplified four-tier classification for thyroid core needle biopsy
M. Paja, J. L. Del Cura, R. Zabala, I. Korta, Mª T. Gutiérrez, A. Expósito, A. Ugalde
Journal of Endocrinological Investigation.2024; 48(4): 895. CrossRef
- Lessons learned from the first 2 years of experience with thyroid core needle biopsy at an Indonesian national referral hospital
- Founder BRCA1 mutations in Nepalese population
- Anurag Mehta, Himanshi Diwan, Garima Gupta, Shrinidhi Nathany, Shalini Agnihotri, Surender Dhanda
- J Pathol Transl Med. 2022;56(4):212-216. Published online June 15, 2022
- DOI: https://doi.org/10.4132/jptm.2022.05.02
- 6,796 View
- 137 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Founder mutation is a heritable genetic alteration observed with high frequency in a geographically and culturally isolated population where one or more ancestors becomes the forebearer of the altered gene. The current study reports two founder mutations in the BRCA1 gene in the Nepalese people.
Methods
Germline BRCA testing in all surface epithelial ovarian cancers and the selected case of breast, prostate, and pancreatic cancers has been the standard practice from 2016 to 2021. One thousand one hundred thirtythree probands were screened for germline BRCA variants by next generation sequencing. The variants were classified as per the American Society of Medical Genetics and Genomics recommendations. Pathogenic (class V) and likely pathogenic (class IV) were considered clinically relevant and utilized for cascade screening.
Results
Nepalese population made up a subcohort of 5.12% (58/1,133) of probands tested for germline BRCA1/2 variants. Twenty-seven of these 58 tested harbored pathogenic genetic alterations in BRCA1/2 genes, with 23 being BRCA1 mutant. Sixteen of 23 BRCA1 mutant cases shared one common pathogenic mutation c.2214_2215insT (p.Lys739Ter) (NM_007294.4). Additionally, a second highly recurrent mutation in BRCA1 gene c.5068A>T (p.Lys1690Ter) (NM_007294.4) was noted in six patients from this population.
Conclusions
The overwhelming abundance of the above two variants in a geographically confined population confers these two genetic alterations a status of founder mutations amongst the people of Nepal. A more extensive population-based study to reaffirm these findings will help establish a dual site-specific germline testing similar to the “Multisite-3-assay” in Ashkenazi Jews as the primary screening tool, especially in a resource-constrained environment. -
Citations
Citations to this article as recorded by- Hiding in plain sight: a partial deletion of BRCA1 exon 7 undetectable by MLPA is a Nepali founder variant
Virginia Clowes, Jenny C Taylor, Alistair T Pagnamenta
Journal of Medical Genetics.2025; 62(2): 54. CrossRef - Spectrum of BRCA1/2 pathogenic variants in Southern and Western Asia-a systematic review
Samra Khan, Ikram A. Burney, Mahrukh Nasir, Humaira Saleem, Muhammad Irfan, Muhammad Shakeel, Ishtiaq Ahmad Khan
Mutation Research - Reviews in Mutation Research.2025; 796: 108549. CrossRef - Finding significance: New perspectives in variant classification of the RAD51 regulators, BRCA2 and beyond
Hayley L. Rein, Kara A. Bernstein
DNA Repair.2023; 130: 103563. CrossRef - Digital PCR as a Highly Sensitive Diagnostic Tool: A Review
K. V. Kopylova, Ed. W. Kasparov, I. V. Marchenko, M. V. Smolnikova
Molecular Biology.2023; 57(5): 793. CrossRef - Digital PCR as a Highly Sensitive Diagnostic Tool: a Review
K. V. Kopylova, Ed. W. Kasparov, I. V. Marchenko, M. V. Smolnikova
Молекулярная биология.2023; 57(5): 771. CrossRef
- Hiding in plain sight: a partial deletion of BRCA1 exon 7 undetectable by MLPA is a Nepali founder variant
- Frequency of PIK3CA mutations in different subsites of head and neck squamous cell carcinoma in southern Thailand
- Arunee Dechaphunkul, Phatcharaporn Thongwatchara, Paramee Thongsuksai, Tanadech Dechaphunkul, Sarayut Lucien Geater
- J Pathol Transl Med. 2022;56(3):126-133. Published online February 28, 2022
- DOI: https://doi.org/10.4132/jptm.2022.01.04
- 7,575 View
- 189 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha (PIK3CA) mutations have been reported in many cancers, including head and neck squamous cell carcinoma (HNSCC). The frequency of these mutations varies among tumor locations and might be relevant to treatment outcomes among HNSCC. In this study, we examined the frequency of PIK3CA mutations in the different subsites of HNSCC.
Methods
Ninety-six fresh biopsy specimens were investigated for mutations in PIK3CA exons 4, 9, and 20 using allele-specific real-time polymerase chain reaction. Patient characteristics and survival were analyzed and compared between specimens with or without PIK3CA mutations.
Results
The study included primary tumors originating from the oral cavity (n=63), hypopharynx (n=23), and oropharynx (n=10). We identified mutations in 10.4% of patients (10 of 96 specimens). The overall mutational frequency was 17.4% (4/23) and 9.5% (6/63) in the hypopharynx and oral cavity, respectively. No patients with oropharyngeal carcinoma had mutations. Among the 10 mutant specimens, five were missense mutations (exon 9 [E545K] in two samples and exon 20 [H1047R] in three samples) and five were silent mutations in exon 20 (T1025T). Mutations were not found in exon 4. Among 84 patients with available clinical data, we found no significant differences in clinical characteristics and survival based on the presence or absence of PIK3CA mutations.
Conclusions
The results indicate that PIK3CA mutations are involved in HNSCC carcinogenesis, and the hypopharynx should be considered a primary site of interest for future studies, particularly in Southeast Asian populations. -
Citations
Citations to this article as recorded by- Comprehensive Genomic Profiling of Sinonasal Carcinomas: Identification of Common Mutations and Potential Targets for Therapy
Gabriel Bitar, Beau Hsia, Saif Alshaka, Bastien A. Valencia, Jeeho Kim, Mariko Sato, John Crawford, Michael L. Levy, Sean Polster, Vijay A. Patel
Journal of Neurological Surgery Part B: Skull Base.2025;[Epub] CrossRef - Anti-breast cancer effects of Pterocarpus soyauxii Taub aqueous extract and its compounds by integrating ADMET, network pharmacology, molecular docking, dynamic simulation, CLC-Pred and pdCSM-Cancer/PPI approaches, and in vitro validation
Owona Pascal Emmanuel, Mengue Ngadena Yolande Sandrine, Bilanda Danielle Claude, Ayissi Mbomo Rigobert-Espoir, Oluwafemi Adeleke Ojo, Ella Armand Fils, Bidingha A Goufani Ronald, Bindzi Georges Michel, Dzeufiet Djomeni Paul Désiré, Tariq Aziz, Abdulhakeem
Journal of Ethnopharmacology.2025; 353: 120407. CrossRef - A retrospective study of laryngeal squamous cell carcinoma and the significance of the PIK3CA mutation for survival
Akinobu Kubota, Nobuyuki Bandoh, Takashi Goto, Michihisa Kono, Ryosuke Sato, Shiori Suzuki, Shota Sakaue, Ryuhei Takeda, Shuto Hayashi, Misaki Hayashi, Daisuke Araki, Shogo Baba, Yasutaka Kato, Miki Takahara, Hiroshi Nishihara, Hajime Kamada
Molecular and Clinical Oncology.2025; 23(4): 1. CrossRef - An empirical review on the resistance mechanisms of epidermal growth factor receptor inhibitors and predictive molecular biomarkers in colorectal cancer
Sankha Bhattacharya
Critical Reviews in Oncology/Hematology.2023; 183: 103916. CrossRef
- Comprehensive Genomic Profiling of Sinonasal Carcinomas: Identification of Common Mutations and Potential Targets for Therapy
- Correlation of TTF-1 immunoexpression and EGFR mutation spectrum in non–small cell lung carcinoma
- Tripti Nakra, Varsha Singh, Aruna Nambirajan, Prabhat Singh Malik, Anant Mohan, Deepali Jain
- J Pathol Transl Med. 2021;55(4):279-288. Published online July 8, 2021
- DOI: https://doi.org/10.4132/jptm.2021.05.10
- 7,986 View
- 186 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Thyroid transcription factor (TTF-1) is a diagnostic marker expressed in 75%–85% of primary lung adenocarcinomas (ACs). Activating mutations in the tyrosine kinase domain of the epidermal growth factor receptor (EGFR) gene is the most common targetable driver alteration in lung AC. Previous studies have shown a positive correlation between TTF-1 and EGFR mutation status. We aimed to determine the predictive value of TTF-1 immunoexpression for underlying EGFR mutation status in a large Indian cohort.
Methods
This retrospective designed study was conducted with medical record data from 2011 to 2020. All cases of primary lung AC and non–small cell lung carcinoma not otherwise specified (NSCLC, NOS) with known TTF-1 expression diagnosed by immunohistochemistry using 8G7G3/1 antibodies and EGFR mutation status diagnosed by quantitative polymerase chain reaction were retrieved, reviewed, and the
results
were analyzed. Results: Among 909 patient samples diagnosed as lung AC and NSCLC, NOS, TTF-1 was positive in 76.8% cases (698/909) and EGFR mutations were detected in 29.6% (269/909). A strong positive correlation was present between TTF-1 positivity and EGFR mutation status (odds ratio, 3.61; p < .001), with TTF-1 positivity showing high sensitivity (90%) and negative predictive value (87%) for EGFR mutation. TTF-1 immunoexpression did not show significant correlation with uncommon/dual EGFR mutations (odds ratio, 1.69; p = .098). EGFR–tyrosine kinase inhibitor therapy was significantly superior to chemotherapy among EGFR mutant cases irrespective of TTF-1 status; however, no significant differences among survival outcomes were observed.
Conclusions
Our study confirms a strong positive correlation between TTF-1 expression and common EGFR mutations (exon 19 deletion and exon 21 L858R) in advanced lung AC with significantly high negative predictive value of TTF-1 for EGFR mutations. -
Citations
Citations to this article as recorded by- Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
Aruna Nambirajan, Amber Rathor, Hemavathi Baskarane, Anju GS, Sachin Khurana, Somagattu Sushmitha, Aparna Sharma, Prabhat Singh Malik, Deepali Jain
Virchows Archiv.2025; 487(3): 639. CrossRef - Lung Carcinoids in Adolescents and Young Adults (AYAs): A Still Overlooked Clinical Entity
Alice Laffi, Laura Pala, Chiara Catania, Marzia Locatelli, Priscilla Cascetta, Emilia Cocorocchio, Giovanni Luca Ceresoli, Daniele Laszlo, Flaminia Facella, Emily Governini, Marzia Bendoni, Giuseppe Pelosi, Fabio Conforti, Tommaso Martino De Pas
Current Oncology.2025; 32(8): 458. CrossRef - Correlation between TTF-1 expression and EGFR mutations in moroccan lung adenocarcinoma: A prospective six-year study
Sara Boukansa, Ismail Mouhrach, Fatima El Agy, Mokhtar El Mekhtoume, Laila Bouguenouch, Mounia Serraj, Bouchra Amara, Yassine Ouadnouni, Mohamed Smahi, Badreeddine Alami, Nawfel Mellas, Zineb Benbrahim, Hinde El Fatemi
Cancer Treatment and Research Communications.2025; 45: 101012. CrossRef - Mutation profile and programmed death ligand 1 status of patients with non‐small cell lung cancer diagnosed with “adenocarcinoma” and “non‐small cell carcinoma favor adenocarcinoma”
Naoko Shigeta, Tomoyuki Yokose, Shuji Murakami, Tetsuya Isaka, Kanako Shinada, Emi Yoshioka, Atsuya Narita, Kengo Katakura, Tetsuro Kondo, Terufumi Kato, Takuya Nagashima, Haruhiro Saito, Hiroyuki Ito
Thoracic Cancer.2024; 15(6): 458. CrossRef - Significance of NKX2-1 as a biomarker for clinical prognosis, immune infiltration, and drug therapy in lung squamous cell carcinoma
Huiyue Lin, Juyong Wang, Qing Shi, Minmin Wu
PeerJ.2024; 12: e17338. CrossRef - TTF-1 is a highly sensitive but not fully specific marker for pulmonary and thyroidal cancer: a tissue microarray study evaluating more than 17,000 tumors from 152 different tumor entities
Katharina Möller, Tayyaba Gulzar, Maximilian Lennartz, Florian Viehweger, Martina Kluth, Claudia Hube-Magg, Christian Bernreuther, Ahmed Abdulwahab Bawahab, Ronald Simon, Till S. Clauditz, Guido Sauter, Ria Schlichter, Andrea Hinsch, Simon Kind, Frank Jac
Virchows Archiv.2024; 485(5): 815. CrossRef - Identifying immunohistochemical biomarkers panel for non-small cell lung cancer in optimizing treatment and forecasting efficacy
Xiaoya Zhang, Junhong Meng, Mingyue Gao, Cheng Gong, Cong Peng, Duxian Liu
BMC Cancer.2024;[Epub] CrossRef - Expression landscapes in non-small cell lung cancer shaped by the thyroid transcription factor 1
Herdee Gloriane C. Luna, Marcelo Severino Imasa, Necy Juat, Katherine V. Hernandez, Treah May Sayo, Gloria Cristal-Luna, Sheena Marie Asur-Galang, Mirasol Bellengan, Kent John Duga, Bien Brian Buenaobra, Marvin I. De los Santos, Daniel Medina, Jamirah Sam
Lung Cancer.2023; 176: 121. CrossRef - Malignant pleural effusion cell blocks are reliable resources for PD-L1 analysis in advanced lung adenocarcinomas: a concordance study with matched histologic samples
Swati Mahajan, Aruna Nambirajan, Ishan Gupta, Nalini Gupta, Parikshaa Gupta, Deepali Jain
Journal of the American Society of Cytopathology.2022; 11(5): 253. CrossRef - Clinicopathologic Features and Molecular Biomarkers as Predictors of Epidermal Growth Factor Receptor Gene Mutation in Non-Small Cell Lung Cancer Patients
Lanlan Liu, Xianzhi Xiong
Current Oncology.2021; 29(1): 77. CrossRef
- Baseline retinoblastoma transcriptional corepressor 1 (Rb1) functional inactivation is a pre-requisite but not sufficient for small-cell histological transformation in epidermal growth factor receptor (EGFR) mutant lung adenocarcinomas post-tyrosine kinas
- A study of pathological characteristics and BRAF V600E status in Langerhans cell histiocytosis of Vietnamese children
- Thu Dang Anh Phan, Bao Gia Phung, Tu Thanh Duong, Vu Anh Hoang, Dat Quoc Ngo, Nguyen Dinh The Trinh, Tung Thanh Tran
- J Pathol Transl Med. 2021;55(2):112-117. Published online January 27, 2021
- DOI: https://doi.org/10.4132/jptm.2020.11.30
- 7,056 View
- 129 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Langerhans cell histiocytosis (LCH) is more common in children than adults and involves many organs. In children, the BRAF V600E mutation is associated with recurrent and high-risk LCH.
Methods
We collected paraffin blocks of 94 pediatric LCH patients to detect BRAF V600E mutation by sequencing. The relationship between BRAF V600E status and clinicopathological parameters were also critically analyzed.
Results
BRAF V600E mutation exon 15 was detected in 45 cases (47.9%). Multiple systems LCH showed a significantly higher BRAF V600E mutation rate than a single system (p=.001). No statistical significance was evident for other clinical characteristics such as age, sex, location, risk organs involvement, and CD1a expression.
Conclusions
In Vietnamese LCH children, the proportion of BRAF V600E mutational status was relatively high and related to multiple systems. -
Citations
Citations to this article as recorded by- Clinicopathological features of hepatic Langerhans cell histiocytosis: report of ten cases and review of the literature
Qian-Qian Chen, Chun-kui Shao, Yi-wang Zhang, Jian-ning Chen, Hai-feng Li, Qiong Liang
Annals of Diagnostic Pathology.2026; 81: 152586. CrossRef - Pathologic characteristics of histiocytic and dendritic cell neoplasms
Sun Och Yoon
Blood Research.2024;[Epub] CrossRef - Sulfur dots/Au@Ag nanorods array-based polarized ECL sensor for the detection of thyroid cancer biomarker
Zixuan Ding, Peilin Wang, Zhenrun Li, Yupeng Guo, Qiang Ma
Talanta.2023; 265: 124925. CrossRef
- Clinicopathological features of hepatic Langerhans cell histiocytosis: report of ten cases and review of the literature
- Highly prevalent BRAF V600E and low-frequency TERT promoter mutations underlie papillary thyroid carcinoma in Koreans
- Sue Youn Kim, Taeeun Kim, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim, Chan Kwon Jung
- J Pathol Transl Med. 2020;54(4):310-317. Published online June 15, 2020
- DOI: https://doi.org/10.4132/jptm.2020.05.12
- 11,403 View
- 199 Download
- 29 Web of Science
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
The presence of telomerase reverse transcriptase (TERT) promoter mutations have been associated with a poor prognosis in patients with papillary thyroid carcinomas (PTC). The frequency of TERT promoter mutations varies widely depending on the population and the nature of the study.
Methods
Data were prospectively collected in 724 consecutive patients who underwent thyroidectomy for PTC from 2018 to 2019. Molecular testing for BRAF V600E and TERT promoter mutations was performed in all cases.
Results
TERT promoter alterations in two hotspots (C228T and C250T) and C216T were found in 16 (2.2%) and 4 (0.6%) of all PTCs, respectively. The hotspot mutations were significantly associated with older age at diagnosis, larger tumor size, extrathyroidal extension, higher pathologic T category, lateral lymph node metastasis, and higher American Thyroid Association recurrence risk. The patients with C216T variant were younger and had a lower American Thyroid Association recurrence risk than those with hotspot mutations. Concurrent BRAF V600E was found in 19 of 20 cases with TERT promoter mutations. Of 518 microcarcinomas measuring ≤1.0 cm in size, hotspot mutations and C216T variants were detected in five (1.0%) and three (0.6%) cases, respectively.
Conclusions
Our study indicates a low frequency of TERT promoter mutations in Korean patients with PTC and supports previous findings that TERT promoter mutations are more common in older patients with unfavorable clinicopathologic features and BRAF V600E. TERT promoter mutations in patients with microcarcinoma are uncommon and may have a limited role in risk stratification. The C216T variant seems to have no clinicopathologic effect on PTC. -
Citations
Citations to this article as recorded by- The impact of C216T and hot spot mutations of the TERT promoter on the clinicopathologic characteristics and S100A10 expression in papillary thyroid carcinoma: a comparative study
Ping Li, Chuqiang Huang, Xiaoling Liu, Huihui Gui, Jian Li
Diagnostic Pathology.2025;[Epub] CrossRef - Refining NTRK Fusion Detection in Papillary Thyroid Carcinoma Through Pan-TRK Immunohistochemistry and Histopathologic Features
Hyun Lee, Sue Youn Kim, Ji Min Park, Seung-Hyun Jung, Ozgur Mete, Chan Kwon Jung
Endocrine Pathology.2025;[Epub] CrossRef - Validation of Diagnostic Utility of Washout CYFRA 21-1 in Lymph Node Metastasis of Thyroid Cancer
Jeongmin Lee, Yuri Shin, Jeongun Kwak, Hye Lim Park, Sohee Lee, Mee Kyung Kim, Ja Seong Bae, Chan Kwon Jung, So Lyung Jung, Jung-Min Lee, Sang-Ah Chang, Dong-Jun Lim
Clinical Cancer Research.2025; 31(10): 1922. CrossRef - 2025 Korean Thyroid Association Clinical Management Guideline on Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Eun Kyung Lee, Min Joo Kim, Seung Heon Kang, Bon Seok Koo, Kyungsik Kim, Mijin Kim, Bo Hyun Kim, Ji-hoon Kim, Shin Je Moon, Kyorim Back, Young Shin Song, Jong-hyuk Ahn, Hwa Young Ahn, Ho-Ryun Won, Won Sang Yoo, Min Kyoung Lee, Jeongmin Lee, Ji Ye Lee, Kyo
International Journal of Thyroidology.2025; 18(1): 30. CrossRef - 2025 Korean Thyroid Association Clinical Management Guideline on Active Surveillance for Low-Risk Papillary Thyroid Carcinoma
Eun Kyung Lee, Min Joo Kim, Seung Heon Kang, Bon Seok Koo, Kyungsik Kim, Mijin Kim, Bo Hyun Kim, Ji-hoon Kim, Shinje Moon, Kyorim Back, Young Shin Song, Jong-hyuk Ahn, Hwa Young Ahn, Ho-Ryun Won, Won Sang Yoo, Min Kyoung Lee, Jeongmin Lee, Ji Ye Lee, Kyon
Endocrinology and Metabolism.2025; 40(3): 307. CrossRef - Evaluation of BRAF V600E and TERT mutation analysis in differential thyroid cancers
Nigar Aktash, Ahmet Cem Dural, Husnu Aydin, Nuri Alper Sahbaz, Deniz Guzey, Serdar Altınay, Cevher Akarsu, Yasir Musa Kesgin, Sezer Bulut, Mehmet Karabulut
Updates in Surgery.2025;[Epub] CrossRef - Active surveillance for adult low-risk papillary thyroid microcarcinoma—a review focused on the 30-year experience of Kuma Hospital—
Yasuhiro Ito, Akira Miyauchi, Makoto Fujishima, Masashi Yamamoto, Takahiro Sasaki
Endocrine Journal.2024; 71(1): 7. CrossRef - Diagnostic utilities of washout CYFRA 21-1 combined with washout thyroglobulin for metastatic lymph nodes in thyroid cancer: a prospective study
Joonseon Park, Solji An, Kwangsoon Kim, Jeong Soo Kim, Chan Kwon Jung, Ja Seong Bae
Scientific Reports.2024;[Epub] CrossRef - Korean Thyroid Association Guidelines on the Management of Differentiated Thyroid Cancers; Part I. Initial Management of Differentiated Thyroid Cancers - Chapter 5. Evaluation of Recurrence Risk Postoperatively and Initial Risk Stratification in Different
Eun Kyung Lee, Young Shin Song, Ho-Cheol Kang, Sun Wook Kim, Dong Gyu Na, Shin Je Moon, Dong-Jun Lim, Kyong Yeun Jung, Yun Jae Chung, Chan Kwon Jung, Young Joo Park
International Journal of Thyroidology.2024; 17(1): 68. CrossRef - Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules 2024
Young Joo Park, Eun Kyung Lee, Young Shin Song, Su Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung,
International Journal of Thyroidology.2024; 17(1): 208. CrossRef - PD-L1 Expression and Its Modulating Factors in Anaplastic Thyroid Carcinoma
Shipra Agarwal, Chan Kwon Jung, Pranitha Gaddam, Mitsuyoshi Hirokawa, Takuya Higashiyama, Jen-Fan Hang, Wei-An Lai, Somboon Keelawat, Zhiyan Liu, Hee Young Na, So Yeon Park, Junya Fukuoka, Shinya Satoh, Zhanna Mussazhanova, Masahiro Nakashima, Kennichi Ka
American Journal of Surgical Pathology.2024; 48(10): 1233. CrossRef - 2023 Korean Thyroid Association Management Guidelines for Patients with Thyroid Nodules
Young Joo Park, Eun Kyung Lee, Young Shin Song, Soo Hwan Kang, Bon Seok Koo, Sun Wook Kim, Dong Gyu Na, Seung-Kuk Baek, So Won Oh, Min Kyoung Lee, Sang-Woo Lee, Young Ah Lee, Yong Sang Lee, Ji Ye Lee, Dong-Jun Lim, Leehi Joo, Yuh-Seog Jung, Chan Kwon Jung
International Journal of Thyroidology.2023; 16(1): 1. CrossRef - Incidence and risk factors for occult lesions in low-risk papillary thyroid microcarcinoma patients with tumor characteristics appropriate for thermal ablation: A retrospective study
Langping Jin, Kaijun Zhu, Changliang Xu, Jiaying Lu, Liming Huang
Medicine.2023; 102(38): e34938. CrossRef - Identification of NIFTP-Specific mRNA Markers for Reliable Molecular Diagnosis of Thyroid Tumors
So-Yeon Lee, Jong-Lyul Park, Kwangsoon Kim, Ja Seong Bae, Jae-Yoon Kim, Seon-Young Kim, Chan Kwon Jung
Endocrine Pathology.2023; 34(3): 311. CrossRef - Risk factors and predictive model for recurrence in papillary thyroid carcinoma: a single-center retrospective cohort study based on 955 cases
Yin Li, Jiahe Tian, Ke Jiang, Zhongyu Wang, Songbo Gao, Keyang Wei, Ankui Yang, Qiuli Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - BRAFV600E Positivity-Dependent Effect of Age on Papillary Thyroid Cancer Recurrence Risk
Joonseon Park, Solji An, Kwangsoon Kim, Ja Seong Bae, Jeong Soo Kim
Cancers.2023; 15(22): 5395. CrossRef - BRAFV600E mutation test on fine‐needle aspiration specimens of thyroid nodules: Clinical correlations for 4600 patients
Huang Chen, Aiping Song, Ye Wang, Yifan He, Jie Tong, Jinxi Di, Chun Li, Zhongren Zhou, Xiaopin Cai, Dingrong Zhong, Jiping Da
Cancer Medicine.2022; 11(1): 40. CrossRef - Clinicopathological indicators for TERT promoter mutation in papillary thyroid carcinoma
Hee Young Na, Hyeong Won Yu, Woochul Kim, Jae Hoon Moon, Chang Ho Ahn, Sang Il Choi, Yeo Koon Kim, June Young Choi, So Yeon Park
Clinical Endocrinology.2022; 97(1): 106. CrossRef - A Systematic Review and Meta‐analysis on the Occurrence of Biomarker Mutation in Colorectal Cancer among the Asian Population
Hafeez Afolabi, Salzihan Md Salleh, Zaidi Zakaria, Ch’ng Ewe Seng, Siti Norasikin Binti Mohd Nafil, Ahmad Aizat Bin Abdul Aziz, Yusuf Wada, Ahmad Irekeola, Syed Sameer Aga
BioMed Research International.2022;[Epub] CrossRef - A Significance of Concomitant BRAFV600E and TERT Mutations in Polish Patients with Papillary Thyroid Microcarcinoma: A Retrospective Cohort Study Based on 430 Cases
Artur Kuchareczko, Janusz Kopczyński, Artur Kowalik, Kinga Hińcza-Nowak, Agnieszka Walczyk, Iwona Pałyga, Tomasz Trybek, Monika Szymonek, Danuta Gąsior-Perczak, Klaudia Gadawska-Juszczyk, Estera Mikina, Izabela Płachta, Agnieszka Suligowska, Agnieszka Płu
Thyroid.2022; 32(11): 1372. CrossRef - Machine learning for identifying benign and malignant of thyroid tumors: A retrospective study of 2,423 patients
Yuan-yuan Guo, Zhi-jie Li, Chao Du, Jun Gong, Pu Liao, Jia-xing Zhang, Cong Shao
Frontiers in Public Health.2022;[Epub] CrossRef - TERT Promoter and BRAF V600E Mutations in Papillary Thyroid Cancer: A Single-Institution Experience in Korea
Min Jhi Kim, Jin Kyong Kim, Gi Jeong Kim, Sang-Wook Kang, Jandee Lee, Jong Ju Jeong, Woong Youn Chung, Daham Kim, Kee-Hyun Nam
Cancers.2022; 14(19): 4928. CrossRef - Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
Sue Youn Kim, Chan Kwon Jung
Endocrinology and Metabolism.2022; 37(6): 947. CrossRef - Frequency of TERT Promoter Mutations in Real-World Analysis of 2,092 Thyroid Carcinoma Patients (Endocrinol Metab 2022;37:652-63, Heera Yang et al.)
Hyunju Park, Jae Hoon Chung
Endocrinology and Metabolism.2022; 37(6): 949. CrossRef - Molecular Pathology of Non-familial Follicular Epithelial–Derived Thyroid Cancer in Adults: From RAS/BRAF-like Tumor Designations to Molecular Risk Stratification
Paula Soares, Antónia Afonso Póvoa, Miguel Melo, João Vinagre, Valdemar Máximo, Catarina Eloy, José Manuel Cameselle-Teijeiro, Manuel Sobrinho-Simões
Endocrine Pathology.2021; 32(1): 44. CrossRef - Clinicopathological Characteristics and Recurrence-Free Survival of Rare Variants of Papillary Thyroid Carcinomas in Korea: A Retrospective Study
Mijin Kim, Sun Wook Cho, Young Joo Park, Hwa Young Ahn, Hee Sung Kim, Yong Joon Suh, Dughyun Choi, Bu Kyung Kim, Go Eun Yang, Il-Seok Park, Ka Hee Yi, Chan Kwon Jung, Bo Hyun Kim
Endocrinology and Metabolism.2021; 36(3): 619. CrossRef - Clinical Application of TERT Promoter Mutations in Urothelial Carcinoma
Yujiro Hayashi, Kazutoshi Fujita, George J. Netto, Norio Nonomura
Frontiers in Oncology.2021;[Epub] CrossRef - MicroRNA Profile for Diagnostic and Prognostic Biomarkers in Thyroid Cancer
Jong-Lyul Park, Seon-Kyu Kim, Sora Jeon, Chan-Kwon Jung, Yong-Sung Kim
Cancers.2021; 13(4): 632. CrossRef - Prospective Analysis of TERT Promoter Mutations in Papillary Thyroid Carcinoma at a Single Institution
Yun-Suk Choi, Seong-Woon Choi, Jin-Wook Yi
Journal of Clinical Medicine.2021; 10(10): 2179. CrossRef - Significance of telomerase reverse-transcriptase promoter mutations in differentiated thyroid cancer
Hung-Fei Lai, Chi-Yu Kuo, Shih-Ping Cheng
Formosan Journal of Surgery.2021; 54(5): 171. CrossRef - Early Diagnosis of Low-Risk Papillary Thyroid Cancer Results Rather in Overtreatment Than a Better Survival
Jolanta Krajewska, Aleksandra Kukulska, Malgorzata Oczko-Wojciechowska, Agnieszka Kotecka-Blicharz, Katarzyna Drosik-Rutowicz, Malgorzata Haras-Gil, Barbara Jarzab, Daria Handkiewicz-Junak
Frontiers in Endocrinology.2020;[Epub] CrossRef
- The impact of C216T and hot spot mutations of the TERT promoter on the clinicopathologic characteristics and S100A10 expression in papillary thyroid carcinoma: a comparative study
- Tumor immune response and immunotherapy in gastric cancer
- Yoonjin Kwak, An Na Seo, Hee Eun Lee, Hye Seung Lee
- J Pathol Transl Med. 2020;54(1):20-33. Published online November 1, 2019
- DOI: https://doi.org/10.4132/jptm.2019.10.08
- 17,976 View
- 748 Download
- 72 Web of Science
- 67 Crossref
-
 Abstract
Abstract
 PDF
PDF - Remarkable developments in immuno-oncology have changed the landscape of gastric cancer (GC) treatment. Because immunotherapy intervenes with tumor immune response rather than directly targeting tumor cells, it is important to develop a greater understanding of tumor immunity. This review paper summarizes the tumor immune reaction and immune escape mechanisms while focusing on the role of T cells and their co-inhibitory signals, such as the immune checkpoint molecules programmed death-1 and programmed deathligand 1 (PD-L1). This paper also describes past clinical trials of immunotherapy for patients with GC and details their clinical implications. Strong predictive markers are essential to improve response to immunotherapy. Microsatellite instability, Epstein-Barr virus, PD-L1 expression, and tumor mutational burden are now regarded as potent predictive markers for immunotherapy in patients with GC. Novel immunotherapy and combination therapy targeting new immune checkpoint molecules such as lymphocyte-activation gene 3, T cell immunoglobulin, and mucin domain containing-3, and indoleamine 2,3-dioxygenase have been suggested, and trials are ongoing to evaluate their safety and efficacy. Immunotherapy is an important treatment option for patients with GC and has great potential for improving patient outcome, and further research in immuno-oncology should be carried out.
-
Citations
Citations to this article as recorded by- Using glucocorticoid receptor-related genes to create and validate a survival model predicting gastric cancer
Ke Guo, Ping Huang, Jiasheng Zhang, Bo Zhang, Linyang Li, Jiaxin Li
Computational Biology and Chemistry.2026; 120: 108726. CrossRef - Mechanisms of Metabolic Reprogramming Regulating Immunosuppression in the Gastric Cancer Tumor Microenvironment
Wenting Dong, Xuepeng Qian, Honglin Liu, Jinhai Huo, Weiming Wang
Biomolecules.2026; 16(1): 160. CrossRef - FOXP3+/CD8+ ratio associated with aggressive behavior in RUNX3‐methylated diffuse esophagogastric junction tumor
Suguru Maruyama, Yu Imamura, Tasuku Toihata, Ikumi Haraguchi, Manabu Takamatsu, Makiko Yamashita, Yuichiro Nakashima, Eiji Oki, Kenichi Taguchi, Manabu Yamamoto, Shinji Mine, Akihiko Okamura, Jun Kanamori, Souya Nunobe, Takeshi Sano, Shigehisa Kitano, Tet
Cancer Science.2025; 116(1): 178. CrossRef - Immune biomarkers and predictive signatures in gastric cancer: Optimizing immunotherapy responses
Sundaram Vickram, Shofia Saghya Infant, S. Manikandan, D. Jenila Rani, C.M. Mathan Muthu, Hitesh Chopra
Pathology - Research and Practice.2025; 265: 155743. CrossRef - Korean Practice Guidelines for Gastric Cancer 2024: An Evidence-based, Multidisciplinary Approach (Update of 2022 Guideline)
In-Ho Kim, Seung Joo Kang, Wonyoung Choi, An Na Seo, Bang Wool Eom, Beodeul Kang, Bum Jun Kim, Byung-Hoon Min, Chung Hyun Tae, Chang In Choi, Choong-kun Lee, Ho Jung An, Hwa Kyung Byun, Hyeon-Su Im, Hyung-Don Kim, Jang Ho Cho, Kyoungjune Pak, Jae-Joon Kim
Journal of Gastric Cancer.2025; 25(1): 5. CrossRef - Targeted therapy and immunotherapy for gastric cancer: rational strategies, novel advancements, challenges, and future perspectives
Dong Luo, Yunmei Liu, Zhengmao Lu, Lei Huang
Molecular Medicine.2025;[Epub] CrossRef - Prognostic value of the triglyceride-glucose index in gastric cancer
Tugce Eskazan, Suat Saribas, Bekir Kocazeybek
World Journal of Gastroenterology.2025;[Epub] CrossRef - Deciphering the dual role of autophagy in gastric cancer and gastroesophageal junction cancer: from tumor suppression to cancer progression
Lili Lei, Junling Zhang, Ran Wei, Bingqi Dong, Xin Wang, Ying Zhou
Discover Oncology.2025;[Epub] CrossRef - Comparison of clinicopathological parameters with the presence of Epstein–Barr virus and the absence of DNA mismatch repair proteins in gastric adenocarcinomas
Özge Eyeoğlu, Serra Kayaçetin
Asian Biomedicine.2025; 19(2): 86. CrossRef - The impact of combined immunotherapy on the cellular composition of the tumor microenvironment in patients with gastric carcinoma
L.A. Tashireva, A.Yu. Kalinchuk, D.M. Loos, E.A. Tsarenkova, A.V. Avgustinovich, S.G. Afanas’ev, S.V. Vtorushin
Russian Journal of Archive of Pathology.2025; 87(4): 24. CrossRef - Immunotherapy in gastric adenocarcinoma – a rapidly evolving treatment landscape
Yang Wang, Geoffrey Chong
Critical Reviews in Oncology/Hematology.2025; 216: 104941. CrossRef - Ubiquilin-4 induces immune escape in gastric cancer by activating the notch signaling pathway
Quan Jiang, Hao Chen, Shixin Zhou, Tao Zhu, Wenshuai Liu, Hao Wu, Yong Zhang, Fenglin Liu, Yihong Sun
Cellular Oncology.2024; 47(1): 303. CrossRef - Expression and prognostic value of APOBEC2 in gastric adenocarcinoma and its association with tumor-infiltrating immune cells
Lipan Wei, Xiuqian Wu, Lan Wang, Ling Chen, Xuejun Wu, Tiantian Song, Yuanyuan Wang, Wenjun Chang, Aizhen Guo, Yongdong Niu, Haihua Huang
BMC Cancer.2024;[Epub] CrossRef - Identification and characterization of CLEC11A and its derived immune signature in gastric cancer
Qing Zheng, Zhenqi Gong, Baizhi Li, Runzi Cheng, Weican Luo, Cong Huang, Huaiming Wang
Frontiers in Immunology.2024;[Epub] CrossRef - Cervical cancer subtype identification and model building based on lipid metabolism and post-infection microenvironment immune landscape
Yongzhi Chen, Rongjie Cui, Dun Xiong, Yuan Zhao, Jianyu Pang, Samina Gul, Qi Qi, Yuheng Tang, Xuhong Zhou, Wenru Tang
Heliyon.2024; 10(9): e30746. CrossRef - Systematic Analysis of Tumor Stem Cell-related Gene Characteristics
to Predict the PD-L1 Immunotherapy and Prognosis of Gastric
Cancer
Chenchen Wang, Ying Chen, Ru Zhou, Ya’nan Yang, Yantian Fang
Current Medicinal Chemistry.2024; 31(17): 2467. CrossRef - Comprehensive landscape of m6A regulator-related gene patterns and tumor microenvironment infiltration characterization in gastric cancer
Bin Peng, Yinglin Lin, Gao Yi, Mingzhen Lin, Yao Xiao, Yezhenghong Qiu, Wenxia Yao, Xinke Zhou, Zhaoyu Liu
Scientific Reports.2024;[Epub] CrossRef - Distinctive Phenotypic and Microenvironmental Characteristics of Neuroendocrine Carcinoma and Adenocarcinoma Components in Gastric Mixed Adenoneuroendocrine Carcinoma
Yoonjin Kwak, Soo Kyung Nam, Yujun Park, Yun-Suhk Suh, Sang-Hoon Ahn, Seong-Ho Kong, Do Joong Park, Hyuk-Joon Lee, Hyung-Ho Kim, Han-Kwang Yang, Hye Seung Lee
Modern Pathology.2024; 37(10): 100568. CrossRef - Computed tomography-detected extramural venous invasion-related gene signature: a potential negative biomarker of immune checkpoint inhibitor treatment in patients with gastric cancer
Hao Yang, Xinyi Gou, Caizhen Feng, Yinli Zhang, Fan Chai, Nan Hong, Yingjiang Ye, Yi Wang, Bo Gao, Jin Cheng
Journal of Translational Medicine.2023;[Epub] CrossRef - A standardized pathology report for gastric cancer: 2nd edition
Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi,
Journal of Pathology and Translational Medicine.2023; 57(1): 1. CrossRef - A Standardized Pathology Report for Gastric Cancer: 2nd Edition
Young Soo Park, Myeong-Cherl Kook, Baek-hui Kim, Hye Seung Lee, Dong-Wook Kang, Mi-Jin Gu, Ok Ran Shin, Younghee Choi, Wonae Lee, Hyunki Kim, In Hye Song, Kyoung-Mee Kim, Hee Sung Kim, Guhyun Kang, Do Youn Park, So-Young Jin, Joon Mee Kim, Yoon Jung Choi,
Journal of Gastric Cancer.2023; 23(1): 107. CrossRef - Korean Practice Guidelines for Gastric Cancer 2022: An Evidence-based, Multidisciplinary Approach
Tae-Han Kim, In-Ho Kim, Seung Joo Kang, Miyoung Choi, Baek-Hui Kim, Bang Wool Eom, Bum Jun Kim, Byung-Hoon Min, Chang In Choi, Cheol Min Shin, Chung Hyun Tae, Chung sik Gong, Dong Jin Kim, Arthur Eung-Hyuck Cho, Eun Jeong Gong, Geum Jong Song, Hyeon-Su Im
Journal of Gastric Cancer.2023; 23(1): 3. CrossRef - Could Toll-like Receptor 2 Serve as Biomarker to Detect Advanced Gastric Cancer?
Marek Majewski, Kamil Torres, Paulina Mertowska, Sebastian Mertowski, Izabela Korona-Głowniak, Jan Korulczyk, Witold Zgodziński, Ewelina Grywalska
International Journal of Molecular Sciences.2023; 24(6): 5824. CrossRef - Research Progress of Immunotherapy for Gastric Cancer
Zhipeng Zhang, Ningning Liu, Mingyu Sun
Technology in Cancer Research & Treatment.2023;[Epub] CrossRef - Case Report: A rare synchronous multiple gastric carcinoma achieved progression-free disease through NGS-guided serial treatment
Xinyi Shao, Jin Yin, Di Wang, Erjiong Huang, Yini Zhang, Jiani C. Yin, Chen Huang, Hao Wu, Xiaoli Wu
Frontiers in Oncology.2023;[Epub] CrossRef - Artificial Intelligence-Enabled Gastric Cancer Interpretations
Mustafa Yousif, Liron Pantanowitz
Surgical Pathology Clinics.2023; 16(4): 673. CrossRef - The Optimal Tumor Mutational Burden Cutoff Value as a Novel Marker for Predicting the Efficacy of Programmed Cell Death-1 Checkpoint Inhibitors in Advanced Gastric Cancer
Jae Yeon Jang, Youngkyung Jeon, Sun Young Jeong, Sung Hee Lim, Won Ki Kang, Jeeyun Lee, Seung Tae Kim
Journal of Gastric Cancer.2023; 23(3): 476. CrossRef - Biomarkers for Predicting Response to Personalized Immunotherapy in Gastric Cancer
Moonsik Kim, Ji Yun Jeong, An Na Seo
Diagnostics.2023; 13(17): 2782. CrossRef - The Prognostic Value of the Prognostic Nutritional Index in Patients with Advanced or Metastatic Gastric Cancer Treated with Immunotherapy
Yuting Pan, Yue Ma, Guanghai Dai
Nutrients.2023; 15(19): 4290. CrossRef - Molecular classification of gastric cancer predicts survival in patients undergoing radical gastrectomy based on project HOPE
Kenichiro Furukawa, Keiichi Hatakeyama, Masanori Terashima, Takeshi Nagashima, Kenichi Urakami, Keiichi Ohshima, Akifumi Notsu, Takashi Sugino, Taisuke Yagi, Keiichi Fujiya, Satoshi Kamiya, Makoto Hikage, Yutaka Tanizawa, Etsuro Bando, Yae Kanai, Yasuto A
Gastric Cancer.2022; 25(1): 138. CrossRef - Immunotherapy for Gastric Cancer: A 2021 Update
Christo Kole, Nikolaos Charalampakis, Sergios Tsakatikas, Nikolaos-Iasonas Kouris, George Papaxoinis, Michalis V Karamouzis, Anna Koumarianou, Dimitrios Schizas
Immunotherapy.2022; 14(1): 41. CrossRef - The immune microenvironment in gastric adenocarcinoma
Yana Zavros, Juanita L. Merchant
Nature Reviews Gastroenterology & Hepatology.2022; 19(7): 451. CrossRef - Immunomodulation by Gut Microbiome on Gastrointestinal Cancers: Focusing on Colorectal Cancer
Raghad Khalid AL-Ishaq, Lenka Koklesova, Peter Kubatka, Dietrich Büsselberg
Cancers.2022; 14(9): 2140. CrossRef - An Immunity-Associated lncRNA Signature for Predicting Prognosis in Gastric Adenocarcinoma
Xiaowen Zhao, Pingfan Wu, Dongling Liu, Changtian Li, Ling Xue, Zhe Liu, Meng Zhu, Jie Yang, Ziyi Chen, Yaling Li, Yali She, Kathiravan Srinivasan
Journal of Healthcare Engineering.2022; 2022: 1. CrossRef - RNA modification writers influence tumor microenvironment in gastric cancer and prospects of targeted drug therapy
Peng Song, Sheng Zhou, Xiaoyang Qi, Yuwen Jiao, Yu Gong, Jie Zhao, Haojun Yang, Zhifen Qian, Jun Qian, Liming Tang
Journal of Bioinformatics and Computational Biology.2022;[Epub] CrossRef - Identification of the three subtypes and the prognostic characteristics of stomach adenocarcinoma: analysis of the hypoxia-related long non-coding RNAs
Zehua Fan, Yanqun Wang, Rong Niu
Functional & Integrative Genomics.2022; 22(5): 919. CrossRef - Complete Response of High Microsatellite Instability Gastric Cancer and Synchronous Microsatellite Stability Rectal Cancer
Zachary E Hunzeker, Pooja Bhakta, Sindusha R Gudipally, Sri Bharathi Kavuri, Rohit Venkatesan, Chukwuyejulumafor Nwanze
Cureus.2022;[Epub] CrossRef - Immune Profiling in Gastric Cancer Reveals the Dynamic Landscape of Immune Signature Underlying Tumor Progression
Yuhan Wei, Jianwei Zhang, Xueke Fan, Zhi Zheng, Xiaoyue Jiang, Dexi Chen, Yuting Lu, Yingrui Li, Miao Wang, Min Hu, Qi Du, Liuting Yang, Hongzhong Li, Yi Xiao, Yongfu Li, Jiangtao Jin, Deying Wang, Xiangliang Yuan, Qin Li
Frontiers in Immunology.2022;[Epub] CrossRef - Tumor vessel normalization and immunotherapy in gastric cancer
Xianzhe Yu, Shan He, Jian Shen, Qiushi Huang, Peng Yang, Lin Huang, Dan Pu, Li Wang, Lu Li, Jinghua Liu, Zelong Liu, Lingling Zhu
Therapeutic Advances in Medical Oncology.2022;[Epub] CrossRef - FN1 is a prognostic biomarker and correlated with immune infiltrates in gastric cancers
Han Wang, Junchang Zhang, Huan Li, Hong Yu, Songyao Chen, Shuhao Liu, Changhua Zhang, Yulong He
Frontiers in Oncology.2022;[Epub] CrossRef - Molecular Pathology of Gastric Cancer
Moonsik Kim, An Na Seo
Journal of Gastric Cancer.2022; 22(4): 264. CrossRef - Bioinformatics Analysis and Structure of Gastric Cancer Prognosis Model Based on Lipid Metabolism and Immune Microenvironment
Yongzhi Chen, Hongjun Yuan, Qian Yu, Jianyu Pang, Miaomiao Sheng, Wenru Tang
Genes.2022; 13(9): 1581. CrossRef - Clinical implications of interleukins-31, 32, and 33 in gastric cancer
Qing-Hua Liu, Ji-Wei Zhang, Lei Xia, Steven G Wise, Brett David Hambly, Kun Tao, Shi-San Bao
World Journal of Gastrointestinal Oncology.2022; 14(9): 1808. CrossRef - Microbiota and the Immune System—Actors in the Gastric Cancer Story
Marek Majewski, Paulina Mertowska, Sebastian Mertowski, Konrad Smolak, Ewelina Grywalska, Kamil Torres
Cancers.2022; 14(15): 3832. CrossRef - Bioinformatics and Experimental Analyses Reveal MAP4K4 as a Potential Marker for Gastric Cancer
Junping Zhang, Xiaoping Cai, Weifeng Cui, Zheng Wei
Genes.2022; 13(10): 1786. CrossRef - Common strategies for effective immunotherapy of gastroesophageal cancers using immune checkpoint inhibitors
Shuang Ma, Fei Chen
Pathology - Research and Practice.2022; 238: 154110. CrossRef - High-level of intratumoral GITR+ CD4 T cells associate with poor prognosis in gastric cancer
Shouyu Ke, Feng Xie, Yixian Guo, Jieqiong Chen, Zeyu Wang, Yimeng Yu, Haigang Geng, Danhua Xu, Xu Liu, Xiang Xia, Fengrong Yu, Chunchao Zhu, Zizhen Zhang, Gang Zhao, Bin Li, Wenyi Zhao
iScience.2022; 25(12): 105529. CrossRef - Characteristics of Adenosine-to-Inosine RNA editing-based subtypes and novel risk score for the prognosis and drug sensitivity in stomach adenocarcinoma
Jingjing Pan, Xinyuan Gu, Jing Luo, Xinye Qian, Qiang Gao, Tianjie Li, Longying Ye, Chenlu Li
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Inhibition of NF‐κB is required for oleanolic acid to downregulate PD‐L1 by promoting DNA demethylation in gastric cancer cells
Xirong Lu, Yuyi Li, Wei Yang, Minghao Tao, Yanmiao Dai, Jinkang Xu, Qianfei Xu
Journal of Biochemical and Molecular Toxicology.2021;[Epub] CrossRef - Prognostic Value of C-Reactive Protein to Albumin Ratio in Gastric Cancer: A Meta-Analysis
Liang Yue, Yi Lu, Yulin Li, Yilin Wang
Nutrition and Cancer.2021; 73(10): 1864. CrossRef - Immunogenic characteristics of microsatellite instability‐low esophagogastric junction adenocarcinoma based on clinicopathological, molecular, immunological and survival analyses
Yu Imamura, Tasuku Toihata, Ikumi Haraguchi, Yoko Ogata, Manabu Takamatsu, Aya Kuchiba, Norio Tanaka, Osamu Gotoh, Seiichi Mori, Yuichiro Nakashima, Eiji Oki, Masaki Mori, Yoshinao Oda, Kenichi Taguchi, Manabu Yamamoto, Masaru Morita, Naoya Yoshida, Hideo
International Journal of Cancer.2021; 148(5): 1260. CrossRef - Two Similar Signatures for Predicting the Prognosis and Immunotherapy Efficacy of Stomach Adenocarcinoma Patients
Taohua Yue, Shuai Zuo, Jing Zhu, Shihao Guo, Zhihao Huang, Jichang Li, Xin Wang, Yucun Liu, Shanwen Chen, Pengyuan Wang
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Tumor microenvironment characterization in stage IV gastric cancer
Feng Yang, Zhenbao Wang, Xianxue Zhang
Bioscience Reports.2021;[Epub] CrossRef - E2F2 inhibition induces autophagy via the PI3K/Akt/mTOR pathway in gastric cancer
Hui Li, Shufen Zhao, Liwei Shen, Peige Wang, Shihai Liu, Yingji Ma, Zhiwei Liang, Gongjun Wang, Jing Lv, Wensheng Qiu
Aging.2021; 13(10): 13626. CrossRef - Chemoradiation induces upregulation of immunogenic cell death-related molecules together with increased expression of PD-L1 and galectin-9 in gastric cancer
S. H. Petersen, L. F. Kua, S. Nakajima, W. P. Yong, K. Kono
Scientific Reports.2021;[Epub] CrossRef - Establishment of an Immune Cell Infiltration Score to Help Predict the Prognosis and Chemotherapy Responsiveness of Gastric Cancer Patients
Quan Jiang, Jie Sun, Hao Chen, Chen Ding, Zhaoqing Tang, Yuanyuan Ruan, Fenglin Liu, Yihong Sun
Frontiers in Oncology.2021;[Epub] CrossRef - Microsatellite instability in Gastric Cancer: Between lights and shadows
Elisabetta Puliga, Simona Corso, Filippo Pietrantonio, Silvia Giordano
Cancer Treatment Reviews.2021; 95: 102175. CrossRef - Survival-associated alternative splicing events interact with the immune microenvironment in stomach adenocarcinoma
Zai-Sheng Ye, Miao Zheng, Qin-Ying Liu, Yi Zeng, Sheng-Hong Wei, Yi Wang, Zhi-Tao Lin, Chen Shu, Qiu-Hong Zheng, Lu-Chuan Chen
World Journal of Gastroenterology.2021; 27(21): 2871. CrossRef - Immunotherapy of gastric cancer: Past, future perspective and challenges
Jun Xie, Liping Fu, Li Jin
Pathology - Research and Practice.2021; 218: 153322. CrossRef - Clinicopathologic and Prognostic Association of GRP94 Expression in Colorectal Cancer with Synchronous and Metachronous Metastases
Sumi Yun, Sukmook Lee, Ho-Young Lee, Hyeon Jeong Oh, Yoonjin Kwak, Hye Seung Lee
International Journal of Molecular Sciences.2021; 22(13): 7042. CrossRef - Injectable shear-thinning polylysine hydrogels for localized immunotherapy of gastric cancer through repolarization of tumor-associated macrophages
Yan Yang, Yang Yang, Meili Chen, Jianquan Chen, Jinyan Wang, Yajun Ma, Hanqing Qian
Biomaterials Science.2021; 9(19): 6597. CrossRef - Correlation between LRP1B Mutations and Tumor Mutation Burden in Gastric Cancer
Sizhe Hu, Xiaokang Zhao, Feng Qian, Cancan Jin, Kaishun Hou, Tao Huang
Computational and Mathematical Methods in Medicine.2021; 2021: 1. CrossRef - Comprehensive Analysis to Identify MAGEA3 Expression Correlated With Immune Infiltrates and Lymph Node Metastasis in Gastric Cancer
Jinji Jin, Jianxin Tu, Jiahuan Ren, Yiqi Cai, Wenjing Chen, Lifang Zhang, Qiyu Zhang, Guanbao Zhu
Frontiers in Oncology.2021;[Epub] CrossRef - Effect of P2X7 receptor on tumorigenesis and its pharmacological properties
Wen-jun Zhang, Ce-gui Hu, Zheng-ming Zhu, Hong-liang Luo
Biomedicine & Pharmacotherapy.2020; 125: 109844. CrossRef - Current status and future potential of predictive biomarkers for immune checkpoint inhibitors in gastric cancer
Byung Woog Kang, Ian Chau
ESMO Open.2020; 5(4): e000791. CrossRef - Is Ramucirumab Still the Only Second-Line Treatment in Metastatic Gastric Cancer?
Khalil El Gharib, Hampig Raphael Kourie
Pharmacogenomics.2020; 21(17): 1203. CrossRef - Deep Learning Predicts Underlying Features on Pathology Images with Therapeutic Relevance for Breast and Gastric Cancer
Renan Valieris, Lucas Amaro, Cynthia Aparecida Bueno de Toledo Osório, Adriana Passos Bueno, Rafael Andres Rosales Mitrowsky, Dirce Maria Carraro, Diana Noronha Nunes, Emmanuel Dias-Neto, Israel Tojal da Silva
Cancers.2020; 12(12): 3687. CrossRef
- Using glucocorticoid receptor-related genes to create and validate a survival model predicting gastric cancer
- Molecular and Clinicopathological Features of Gastrointestinal Stromal Tumors in Vietnamese Patients
- Quoc Dat Ngo, Quoc Thang Pham, Dang Anh Thu Phan, Anh Vu Hoang, Thi Ngoc Ha Hua, Sao Trung Nguyen
- J Pathol Transl Med. 2019;53(6):361-368. Published online September 16, 2019
- DOI: https://doi.org/10.4132/jptm.2019.08.27
- 8,068 View
- 160 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Gastrointestinal stromal tumors (GISTs) are the most frequent mesenchymal neoplasms of the gastrointestinal tract. Management of GIST patients is currently based on clinicopathological features and associated genetic changes. However, the detailed characteristics and molecular genetic features of GISTs have not yet been described in the Vietnamese population.
Methods
We first identified 155 patients with primary GIST who underwent surgery with primary curative intent between 2011 and 2014 at University Medical Center at Ho Chi Minh City, Vietnam. We evaluated the clinicopathological features and immunohistochemical reactivity to p53 and Ki-67 in these patients. Additionally, KIT genotyping was performed in 100 cases.
Results
The largest proportion of GISTs was classified as high-risk (43.2%). Of the 155 GISTs, 52 (33.5%) were positive for Ki-67, and 58 (37.4%) were positive for p53. The expression of Ki-67 and p53 were correlated with mitotic rate, tumor size, risk assessment, and tumor stage. Out of 100 GIST cases, KIT mutation was found in 68%, of which 62 (91.2%) were found in exon 11, two (2.9%) in exon 9, and four (5.8%) in exon 17. No mutation in exon 13 was identified. Additionally, KIT mutations did not correlate with any clinicopathological features.
Conclusions
The expression of Ki-67 and p53 were associated with high-risk tumors. Mutations in exon 11 were the most commonly found, followed by exon 17 and exon 9. Additionally, KIT mutation status was not correlated with any recognized clinicopathological features. -
Citations
Citations to this article as recorded by- Ki67 for evaluating the prognosis of gastrointestinal stromal tumors: A systematic review and meta‑analysis
Ji Li, An-Ran Wang, Xiao-Dong Chen, Hong Pan, Shi-Qiang Li
Oncology Letters.2022;[Epub] CrossRef - Endoscopic ultrasound‐guided fine‐needle aspiration cytology in the diagnosis of the gastrointestinal stromal tumor of the stomach
José‐Fernando Val‐Bernal, Elena Yllera, María Moris, Ihab Abdulkader Nallib, Angel Vázquez‐Boquete, María Martino
Diagnostic Cytopathology.2020; 48(9): 833. CrossRef
- Ki67 for evaluating the prognosis of gastrointestinal stromal tumors: A systematic review and meta‑analysis
- Differential MicroRNA Expression between EGFR T790M and L858R Mutated Lung Cancer
- Ji Yeon Kim, Woo Jeong Lee, Ha Young Park, Ahrong Kim, Dong Hoon Shin, Chang Hun Lee
- J Pathol Transl Med. 2018;52(5):275-282. Published online August 16, 2018
- DOI: https://doi.org/10.4132/jptm.2018.07.29
- 8,308 View
- 129 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
MicroRNAs (miRNAs) are short, non-coding RNAs that mediate post-transcriptional gene regulation. They are commonly deregulated in human malignancies, including non-small cell lung cancer (NSCLC). The aim of this study is to investigate miRNA expression in T790M-mutated NSCLC resistant to epidermal growth factor receptor (EGFR) tyrosine kinase inhibitors.
Methods
Six cases of resected NSCLC harboring the T790M mutation were examined. We performed miRNA time polymerase chain reaction (PCR) array profiling using EGFR T790M-mutated NSCLC and L858R-mutated NSCLC. Once identified, miRNAs that were differentially expressed between the two groups were validated by quantitative real-time polymerase chain reaction (qRT-PCR).
Results
miRNA PCR array profiling revealed three up-regulated miRNAs whose expression levels were altered 4.0-fold or more in the EGFR T790M mutation group than in the L858R group: miR-1 (fold change, 4.384), miR-196a (fold change, 4.138), and miR-124 (fold change, 4.132). The three differentially expressed miRNAs were validated by qRT-PCR, and they were found to be overexpressed in the T790M group relative to L858R group. In particular, expression levels of miR-1 and miR-124 were significantly higher in the T790M group (p-value of miR-1 = .004, miR-124 = .007, miR-196a = .096).
Conclusions
MiR-1, miR-124, and miR-196a are overexpressed in EGFR T790M mutated NSCLC. -
Citations
Citations to this article as recorded by- Whole exome sequencing and MicroRNA profiling of lung adenocarcinoma identified risk prediction features for tumors at stage I and its substages
Hao Ho, Sung-Liang Yu, Hsuan-Yu Chen, Shin-Sheng Yuan, Kang-Yi Su, Yi-Chiung Hsu, Chung-Ping Hsu, Cheng-Yen Chuang, Ya-Hsuan Chang, Yu-Cheng Li, Chiou-Ling Cheng, Gee-Chen Chang, Pan-Chyr Yang, Ker-Chau Li
Lung Cancer.2023; 184: 107352. CrossRef - Dynamic Evaluation of Circulating miRNA Profile in EGFR-Mutated NSCLC Patients Treated with EGFR-TKIs
Alessandro Leonetti, Mjriam Capula, Roberta Minari, Giulia Mazzaschi, Alessandro Gregori, Btissame El Hassouni, Filippo Papini, Paola Bordi, Michela Verzè, Amir Avan, Marcello Tiseo, Elisa Giovannetti
Cells.2021; 10(6): 1520. CrossRef - Generation of osimertinib-resistant cells from epidermal growth factor receptor L858R/T790M mutant non-small cell lung carcinoma cell line
Nalini Devi Verusingam, Yi-Chen Chen, Heng-Fu Lin, Chao-Yu Liu, Ming-Cheng Lee, Kai-Hsi Lu, Soon-Keng Cheong, Alan Han-Kiat Ong, Shih-Hwa Chiou, Mong-Lien Wang
Journal of the Chinese Medical Association.2021; 84(3): 248. CrossRef - Cell Behavior of Non-Small Cell Lung Cancer Is at EGFR and MicroRNAs Hands
Sarah Sayed Hassanein, Sherif Abdelaziz Ibrahim, Ahmed Lotfy Abdel-Mawgood
International Journal of Molecular Sciences.2021; 22(22): 12496. CrossRef - The Roles of MicroRNA in Lung Cancer
Kuan-Li Wu, Ying-Ming Tsai, Chi-Tun Lien, Po-Lin Kuo, Jen-Yu Hung
International Journal of Molecular Sciences.2019; 20(7): 1611. CrossRef
- Whole exome sequencing and MicroRNA profiling of lung adenocarcinoma identified risk prediction features for tumors at stage I and its substages
- Utility of BRAF VE1 Immunohistochemistry as a Screening Tool for Colorectal Cancer Harboring BRAF V600E Mutation
- Jeong-Hwa Kwon, Byung-Kwan Jeong, Yong Sik Yoon, Chang Sik Yu, Jihun Kim
- J Pathol Transl Med. 2018;52(3):157-163. Published online March 29, 2018
- DOI: https://doi.org/10.4132/jptm.2018.03.28
- 9,183 View
- 206 Download
- 12 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
BRAF mutation has been recognized as an important biomarker of colorectal cancer (CRC) for targeted therapy and prognosis prediction. However, sequencing for every CRC case is not cost-effective. An antibody specific for BRAF V600E mutant protein has been introduced, and we thus examined the utility of BRAF VE1 immunohistochemistry for evaluating BRAF mutations in CRC.
Methods
Fifty-one BRAF-mutated CRCs and 100 age and sexmatched BRAF wild-type CRCs between 2005 and 2015 were selected from the archives of Asan Medical Center. Tissue microarrays were constructed and stained with BRAF VE1 antibody.
Results
Forty-nine of the 51 BRAF-mutant CRCs (96.1%) showed more than moderate cytoplasmic staining, except for two weakly stained cases. Six of 100 BRAF wild-type cases also stained positive with BRAF VE1 antibody; four stained weakly and two stained moderately. Normal colonic crypts showed nonspecific weak staining, and a few CRC cases exhibited moderate nuclear reactivity (3 BRAF-mutant and 10 BRAF wild-type cases). BRAF-mutated CRC patients had higher pathologic stages and worse survival than BRAF wild-type patients.
Conclusions
BRAF VE1 immunohistochemistry showed high sensitivity and specificity, but occasional nonspecific staining in tumor cell nuclei and normal colonic crypts may limit their routine clinical use. Thus, BRAF VE1 immunohistochemistry may be a useful screening tool for BRAF V600E mutation in CRCs, provided that additional sequencing studies can be done to confirm the mutation in BRAF VE1 antibody-positive cases. -
Citations
Citations to this article as recorded by- Next-Generation Sequencing in Oncology—A Guiding Compass for Targeted Therapy and Emerging Applications
Laurenția Nicoleta Galeș, Mihai-Andrei Păun, Ioana Butnariu, Laurentiu Simion, Loredana Sabina Cornelia Manolescu, Oana Gabriela Trifănescu, Rodica Maricela Anghel
International Journal of Molecular Sciences.2025; 26(7): 3123. CrossRef - A multi-omic analysis reveals a predictive value of tertiary lymphoid structures in improving the prognosis of colorectal cancer patients with BRAF mutation
Chao Qin, Shumin Cheng, Jingyun Ma, Lujing Li, Yun Leng, Lei Zheng, Huiying Chen, Hui Mo, Shi Li, Yuhong Liang, Yi Zhang, Wenxia Li, Jing Liang, Yuxuan Liu, Junxuan Mai, Linlin Hou, Di Wang, Ke Zhu, Bihui Huang
Frontiers in Immunology.2025;[Epub] CrossRef - The evolving landscape of tissue‐agnostic therapies in precision oncology
Vivek Subbiah, Mohamed A. Gouda, Bettina Ryll, Howard A. Burris, Razelle Kurzrock
CA: A Cancer Journal for Clinicians.2024; 74(5): 433. CrossRef - Deciphering the Role of BRAFV600E Immunohistochemistry in Breast Lesions: A Comprehensive Review
Simran Khan, Arvind Bhake, Shakti Sagar
Cureus.2024;[Epub] CrossRef - Immunohistochemistry as a Surrogate Marker of Underlying Molecular Derangements in Sporadic Colorectal Carcinoma in Children – A Series of Three Cases
Priyanka Maity, Aniket Halder, Ranajoy Ghosh, Uttara Chatterjee, Shibsankar Barman, Ruchirendra Sarkar
Fetal and Pediatric Pathology.2022; 41(1): 98. CrossRef - Risk assessment and genetic counseling for Lynch syndrome – Practice resource of the National Society of Genetic Counselors and the Collaborative Group of the Americas on Inherited Gastrointestinal Cancer
Spring Holter, Michael J. Hall, Heather Hampel, Kory Jasperson, Sonia S. Kupfer, Joy Larsen Haidle, Maureen E. Mork, Selvi Palaniapppan, Leigha Senter, Elena M. Stoffel, Scott M. Weissman, Matthew B. Yurgelun
Journal of Genetic Counseling.2022; 31(3): 568. CrossRef - Current concepts in ameloblastoma-targeted therapies in B-raf proto-oncogene serine/threonine kinase V600E mutation: Systematic review
Rogelio González-González, Sandra López-Verdín, Jesús Lavalle-Carrasco, Nelly Molina-Frechero, Mario Isiordia-Espinoza, Ramón G Carreón-Burciaga, Ronell Bologna-Molina
World Journal of Clinical Oncology.2020; 11(1): 31. CrossRef - Genetic and histopathological analysis of a case of primary intraosseous carcinoma, NOS with features of both ameloblastic carcinoma and squamous cell carcinoma
Akane Yukimori, Maiko Tsuchiya, Akane Wada, Yasuyuki Michi, Kou Kayamori, Kei Sakamoto, Tohru Ikeda
World Journal of Surgical Oncology.2020;[Epub] CrossRef
- Next-Generation Sequencing in Oncology—A Guiding Compass for Targeted Therapy and Emerging Applications
- The Significance of TROP2 Expression in Predicting BRAF Mutations in Papillary Thyroid Carcinoma
- Joon Seog Kong, Hyeon Jin Kim, Min-Jung Kim, Areumnuri Kim, Dalnim Lee, Kanghee Han, Sunhoo Park, Jae Soo Koh, Jae Kyung Myung
- J Pathol Transl Med. 2018;52(1):14-20. Published online December 11, 2017
- DOI: https://doi.org/10.4132/jptm.2017.10.17
- 10,599 View
- 249 Download
- 14 Web of Science
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Trophoblast antigen 2 (TROP2) is a human trophoblast cell-surface glycoprotein that is overexpressed in several types of epithelial cancers, and is suggested to be associated with an unfavorable prognosis. BRAF mutations are the most common genetic alteration in papillary thyroid carcinoma (PTC). We evaluated the correlation between TROP2 expression and BRAF mutation in PTC.
Methods
First, we carried out pyrosequencing for BRAF mutations and immunohistochemistry for TROP2 expression with a tissue microarray consisting of 52 PTC cases. Membranous staining in at least 5% of tumor cells was designated as positive staining and we analyzed the relationship between TROP2 expression and diverse clinicopathological factors, including BRAF mutation. Second, we tested TROP2 mRNA expression in three thyroid cancer cell lines with BRAF mutations (BCPAP, SNU790, and 8505C) and a normal thyroid cell line. Additionally, we checked TROP2 protein levels in a normal thyroid cell line after introduction of the BRAF V600E mutation.
Results
In this study, 21 of 26 cases with BRAF mutation showed TROP2 immunoreactivity, whereas all 26 cases without BRAF mutation showed no immunoreactivity for TROP2 with a statistically significant difference (p<.001). Upregulation of TROP2 mRNA was observed in all three thyroid cancer cell lines, but not in the normal thyroid cell line. Interestingly, however, the TROP2 expression was increased in the normal thyroid cell line after introduction of the BRAF V600E mutation.
Conclusions
Based on these results, we concluded that TROP2 expression is significantly associated with BRAF mutation and that TROP2 immunohistochemistry could be used for predicting BRAF mutations or diagnosing papillary thyroid carcinoma. -
Citations
Citations to this article as recorded by- Trop2-Targeted [18F]AlF-RESCA-RT4 ImmunoPET/CT in Guiding Clinical Surgeries of Thyroid Cancers: A Proof-of-Concept Study
Xinlu Yin, Wenzhi Jia, Le Xu, Wenjie Zheng, Yiqing Gao, Linglin Tang, You Zhang, Qianyun Wu, Dongsheng Xu, Shuxian An, Weijun Wei, Jianjun Liu, Qinyi Zhou, Jialin Feng, Jun Chen
Molecular Pharmaceutics.2026;[Epub] CrossRef - Evolution of TROP2: Biological insights and clinical applications
Xinyue Zhang, Hong Xiao, Fangjian Na, Jingqi Sun, Qi Guan, Ruotong Liu, Lutong Cai, Heming Li, Mingfang Zhao
European Journal of Medicinal Chemistry.2025; 296: 117863. CrossRef - Diagnostic and prognostic utility of TROP-2, SLP-2, and CXCL12 expression in papillary thyroid carcinoma
Amany Selim Attia, Samia Hussein, Hend Sameh, Amr Khalil, Ahmad Barakat Waley, Ihab Matar, Reham Sameh
Cancer Biomarkers.2024; 39(3): 211. CrossRef - BRAF mutation, selected miRNAs and genes expression in primary papillary thyroid carcinomas and local lymph node metastases
David Kalfert, Marie Ludvikova, Martin Pesta, Tommi Hakala, Lucie Dostalova, Hana Grundmannova, Jindra Windrichova, Katerina Houfkova, Tereza Knizkova, Jaroslav Ludvik, Jiri Polivka, Ivana Kholova
Pathology - Research and Practice.2024; 258: 155319. CrossRef - Unveiling the placental secrets: Exploring histopathological changes and TROP2 expression in intrahepatic cholestasis of pregnancy
Cezmi Baran Ozalp, Sozdar Akdogan, Dilan Cetinavci, Melike Nur Akin, Hulya Elbe, Burcu Kasap
Placenta.2024; 154: 201. CrossRef - Trop2-Targeted Molecular Imaging in Solid Tumors: Current Advances and Future Outlook
Yongshun Liu, Wenpeng Huang, Rachel J. Saladin, Jessica C. Hsu, Weibo Cai, Lei Kang
Molecular Pharmaceutics.2024; 21(12): 5909. CrossRef - TROP2 is a Good Indicator for Infiltrative Nature of Carcinoma Rather than Diagnosing Malignancy in Thyroid
E. Kılınc, P. Gunes, A. Doganer
Indian Journal of Otolaryngology and Head & Neck Surgery.2022; 74(S2): 2560. CrossRef - Advances in Trop2-targeted therapy: Novel agents and opportunities beyond breast cancer
Xinlin Liu, Junwen Deng, Yang Yuan, Wujun Chen, Wenshe Sun, Yanhong Wang, Haiming Huang, Bing Liang, Tao Ming, Jialian Wen, Binghuan Huang, Dongming Xing
Pharmacology & Therapeutics.2022; 239: 108296. CrossRef - Knockdown of Trop2 inhibits proliferation and migration and induces apoptosis of endometrial cancer cells via AKT/β‐catenin pathway
Xiaotong Sun, Guangyang Xing, Cui Zhang, Kun Lu, Yuqiong Wang, Xiyan He
Cell Biochemistry and Function.2020; 38(2): 141. CrossRef - Can TROP2 be used as a prognostic marker in endometrioid endometrial carcinoma?
SerkanY Celik, Özgürİlhan Çelik
Indian Journal of Pathology and Microbiology.2020; 63(3): 418. CrossRef - Diagnostic Value of TROP-2 and CK19 Expression in Papillary Thyroid Carcinoma in Both Surgical and Cytological Specimens
Asmaa Gaber Abdou, Mohammed Shabaan, Rania Abdallha, Nehal Nabil
Clinical Pathology.2019;[Epub] CrossRef - Evaluation of Diagnostic Utility of Immunohistochemistry Markers of TROP-2 and HBME-1 in the Diagnosis of Thyroid Carcinoma
Nooshin Zargari, Maral Mokhtari
European Thyroid Journal.2019; 8(1): 1. CrossRef - The diagnostic value of TROP-2, SLP-2 and CD56 expression in papillary thyroid carcinoma
Xueyang Yang, Yifang Hu, He Shi, Chengzhou Zhang, Zhixiao Wang, Xiaoyun Liu, Huanhuan Chen, Lijuan Zhang, Dai Cui
European Archives of Oto-Rhino-Laryngology.2018; 275(8): 2127. CrossRef - TROP2 promotes cell proliferation and migration in osteosarcoma through PI3K/AKT signaling
Qing‑Zhi Gu, Abulimiti Nijiati, Xing Gao, Kai‑Liang Tao, Cheng‑Duo Li, Xue‑Peng Fan, Zheng Tian
Molecular Medicine Reports.2018;[Epub] CrossRef
- Trop2-Targeted [18F]AlF-RESCA-RT4 ImmunoPET/CT in Guiding Clinical Surgeries of Thyroid Cancers: A Proof-of-Concept Study
- Protein Phosphatase Magnesium-Dependent 1δ (PPM1D) Expression as a Prognostic Marker in Adult Supratentorial Diffuse Astrocytic and Oligodendroglial Tumors
- Hui Jeong Jeong, Chang Gok Woo, Bora Lee, Shin Kwang Khang, Soo Jeong Nam, Jene Choi
- J Pathol Transl Med. 2018;52(2):71-78. Published online October 18, 2017
- DOI: https://doi.org/10.4132/jptm.2017.10.21
- 8,857 View
- 201 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Protein phosphatase magnesium-dependent 1δ (PPM1D) is a p53-induced serine/ threonine phosphatase, which is overexpressed in various human cancers. A recent study reported that a mutation in the PPM1D gene is associated with poor prognosis in brainstem gliomas. In this study, we evaluated the utility of PPM1D as a prognostic biomarker of adult supratentorial diffuse astrocytic and oligodendroglial tumors.
Methods
To investigate PPM1D protein expression, mRNA expression, and copy number changes, immunohistochemistry, RNAscope in situ hybridization, and fluorescence in situ hybridization were performed in 84 adult supratentorial diffuse gliomas. We further analyzed clinical characteristics and overall survival (OS) according to PPM1D protein expression, and examined its correlation with other glioma biomarkers such as isocitrate dehydrogenase (IDH) mutation, and p53 expression.
Results
Forty-six cases (54.8%) were PPM1D-positive. PPM1D expression levels were significantly correlated with PPM1D transcript levels (p= .035), but marginally with PPM1D gene amplification (p=.079). Patients with high-grade gliomas showed a higher frequency of PPM1D expression than those with low-grade gliomas (p <.001). Multivariate analysis demonstrated that PPM1D expression (hazard ratio [HR], 2.58; p=.032), age over 60 years (HR, 2.55; p=.018), and IDH1 mutation (HR, 0.18; p=.002) were significantly independent prognostic factors; p53 expression had no prognostic significance (p=.986). The patients with tumor expressing PPM1D showed a shorter OS (p=.003). Moreover, patients with tumor harboring wild-type IDH1 and PPM1D expression had the worst OS (p<.001).
Conclusions
Our data suggest that a subset of gliomas express PPM1D; PPM1D expression is a significant marker of poor prognosis in adult supratentorial diffuse astrocytic and oligodendroglial tumors. -
Citations
Citations to this article as recorded by- Characteristic analysis and identification of novel molecular biomarkers in elderly glioblastoma patients using the 2021 WHO Classification of Central Nervous System Tumors
Yaning Wang, Junlin Li, Yaning Cao, Wenlin Chen, Hao Xing, Xiaopeng Guo, Yixin Shi, Yuekun Wang, Tingyu Liang, Liguo Ye, Delin Liu, Tianrui Yang, Yu Wang, Wenbin Ma
Frontiers in Neuroscience.2023;[Epub] CrossRef - Metal-dependent Ser/Thr protein phosphatase PPM family: Evolution, structures, diseases and inhibitors
Rui Kamada, Fuki Kudoh, Shogo Ito, Itsumi Tani, Jose Isagani B. Janairo, James G. Omichinski, Kazuyasu Sakaguchi
Pharmacology & Therapeutics.2020; 215: 107622. CrossRef
- Characteristic analysis and identification of novel molecular biomarkers in elderly glioblastoma patients using the 2021 WHO Classification of Central Nervous System Tumors
- KRAS Mutation Test in Korean Patients with Colorectal Carcinomas: A Methodological Comparison between Sanger Sequencing and a Real-Time PCR-Based Assay
- Sung Hak Lee, Arthur Minwoo Chung, Ahwon Lee, Woo Jin Oh, Yeong Jin Choi, Youn-Soo Lee, Eun Sun Jung
- J Pathol Transl Med. 2017;51(1):24-31. Published online December 25, 2016
- DOI: https://doi.org/10.4132/jptm.2016.10.03
- 12,364 View
- 170 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material - Background
Mutations in the KRAS gene have been identified in approximately 50% of colorectal cancers (CRCs). KRAS mutations are well established biomarkers in anti–epidermal growth factor receptor therapy. Therefore, assessment of KRAS mutations is needed in CRC patients to ensure appropriate treatment.
Methods
We compared the analytical performance of the cobas test to Sanger sequencing in 264 CRC cases. In addition, discordant specimens were evaluated by 454 pyrosequencing.
Results
KRAS mutations for codons 12/13 were detected in 43.2% of cases (114/264) by Sanger sequencing. Of 257 evaluable specimens for comparison, KRAS mutations were detected in 112 cases (43.6%) by Sanger sequencing and 118 cases (45.9%) by the cobas test. Concordance between the cobas test and Sanger sequencing for each lot was 93.8% positive percent agreement (PPA) and 91.0% negative percent agreement (NPA) for codons 12/13. Results from the cobas test and Sanger sequencing were discordant for 20 cases (7.8%). Twenty discrepant cases were subsequently subjected to 454 pyrosequencing. After comprehensive analysis of the results from combined Sanger sequencing–454 pyrosequencing and the cobas test, PPA was 97.5% and NPA was 100%.
Conclusions
The cobas test is an accurate and sensitive test for detecting KRAS-activating mutations and has analytical power equivalent to Sanger sequencing. Prescreening using the cobas test with subsequent application of Sanger sequencing is the best strategy for routine detection of KRAS mutations in CRC. -
Citations
Citations to this article as recorded by- Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
Su Hwa Kim, Young Suk Lee, Sung Hak Lee, Yeoun Eun Sung, Ahwon Lee, Jun Kang, Jae-Sung Park, Sin Soo Jeun, Youn Soo Lee
Journal of Pathology and Translational Medicine.2023; 57(4): 217. CrossRef - Assessment of KRAS and NRAS status in metastatic colorectal cancer: Experience of the National Institute of Oncology in Rabat Morocco
Chaimaa Mounjid, Hajar El Agouri, Youssef Mahdi, Abdelilah Laraqui, En-nacer Chtati, Soumaya Ech-charif, Mouna Khmou, Youssef Bakri, Amine Souadka, Basma El Khannoussi
Annals of Cancer Research and Therapy.2022; 30(2): 80. CrossRef - The current understanding on the impact of KRAS on colorectal cancer
Mingjing Meng, Keying Zhong, Ting Jiang, Zhongqiu Liu, Hiu Yee Kwan, Tao Su
Biomedicine & Pharmacotherapy.2021; 140: 111717. CrossRef - Droplet digital PCR revealed high concordance between primary tumors and lymph node metastases in multiplex screening of KRAS mutations in colorectal cancer
Barbora Vanova, Michal Kalman, Karin Jasek, Ivana Kasubova, Tatiana Burjanivova, Anna Farkasova, Peter Kruzliak, Dietrich Busselberg, Lukas Plank, Zora Lasabova
Clinical and Experimental Medicine.2019; 19(2): 219. CrossRef - CRISPR Technology for Breast Cancer: Diagnostics, Modeling, and Therapy
Rachel L. Mintz, Madeleine A. Gao, Kahmun Lo, Yeh‐Hsing Lao, Mingqiang Li, Kam W. Leong
Advanced Biosystems.2018;[Epub] CrossRef
- Single-center study on clinicopathological and typical molecular pathologic features of metastatic brain tumor
- Evaluation of the VE1 Antibody in Thyroid Cytology Using Ex Vivo Papillary Thyroid Carcinoma Specimens
- Yon Hee Kim, Hyunee Yim, Yong-Hee Lee, Jae Ho Han, Kyi Beom Lee, Jeonghun Lee, Euy Young Soh, Seon-Yong Jeong, Jang-Hee Kim
- J Pathol Transl Med. 2016;50(1):58-66. Published online December 14, 2015
- DOI: https://doi.org/10.4132/jptm.2015.10.10
- 11,637 View
- 78 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Recently, VE1, a monoclonal antibody against the BRAFV600E mutant protein, has been investigated in terms of its detection of the BRAFV600E mutation. Although VE1 immunostaining and molecular methods used to assess papillary thyroid carcinoma in surgical specimens are in good agreement, evaluation of VE1 in thyroid cytology samples is rarely performed, and its diagnostic value in cytology has not been well established. In present study, we explored VE1 immunoexpression in cytology samples from ex vivo papillary thyroid carcinoma specimens in order to minimize limitations of low cellularity and sampling/targeting errors originated from thyroid fineneedle aspiration and compared our results with those obtained using the corresponding papillary thyroid carcinoma tissues. Methods: The VE1 antibody was evaluated in 21 cases of thyroid cytology obtained directly from ex vivo thyroid specimens. VE1 immunostaining was performed using liquid-based cytology, and the results were compared with those obtained using the corresponding tissues. Results: Of 21 cases, 19 classic papillary thyroid carcinomas had BRAFV600E mutations, whereas two follicular variants expressed wild-type BRAF. VE1 immunoexpression varied according to specimen type. In detection of the BRAFV600E mutation, VE1 immunostaining of the surgical specimen exhibited 100% sensitivity and 100% specificity, whereas VE1 immunostaining of the cytology specimen exhibited only 94.7% sensitivity and 0% specificity. Conclusions: Our data suggest that VE1 immunostaining of a cytology specimen is less specific than that of a surgical specimen for detection of the BRAFV600E mutation, and that VE1 immunostaining of a cytology specimen should be further evaluated and optimized for clinical use. -
Citations
Citations to this article as recorded by- Principles of Analytic Validation of Immunohistochemical Assays: Guideline Update
Jeffrey D. Goldsmith, Megan L. Troxell, Sinchita Roy-Chowdhuri, Carol F. Colasacco, Mary Elizabeth Edgerton, Patrick L. Fitzgibbons, Regan Fulton, Thomas Haas, Patricia L. Kandalaft, Tanja Kalicanin, Christina Lacchetti, Patti Loykasek, Nicole E. Thomas,
Archives of Pathology & Laboratory Medicine.2024; 148(6): e111. CrossRef - Inter- and Intra-observer Reproducibility of Thyroid Fine Needle Aspiration Cytology: An investigation of Bethesda 2023 Using Immunohistochemical BRAFV600E Antibody
Erdogan Bahattin, Dündar Emine, Çetin Kısmet Çivi, Yılmaz Fatih
Journal of Cytology.2024; 41(4): 221. CrossRef - VE1 immunohistochemistry is an adjunct tool for detection of BRAFV600E mutation: Validation in thyroid cancer patients
Faiza A. Rashid, Sobia Tabassum, Mosin S. Khan, Hifzur R. Ansari, Muhammad Asif, Ahmareen K. Sheikh, Syed Sameer Aga
Journal of Clinical Laboratory Analysis.2021;[Epub] CrossRef - Effective utilization of liquid-based cytology for thyroid lesions
Yukie YAMAYA
The Journal of the Japanese Society of Clinical Cytology.2021; 60(3): 164. CrossRef - Diagnostic Efficacy of BRAFV600E Immunocytochemistry in Thyroid Aspirates in Bethesda Category IV and Papillary Thyroid Carcinoma
Nidhi Anand, Tushar Agrawal, Anurag Gupta, Saumya Shukla, Roma Pradhan, Nuzhat Husain
Journal of Cytology.2021; 38(3): 113. CrossRef - The immunocytochemical expression of VE‐1 (BRAF V600E‐related) antibody identifies the aggressive variants of papillary thyroid carcinoma on liquid‐based cytology
Patrizia Straccia, Chiara Brunelli, Esther D. Rossi, Paola Lanza, Maurizio Martini, Teresa Musarra, Celestino Pio Lombardi, Alfredo Pontecorvi, Guido Fadda
Cytopathology.2019; 30(5): 460. CrossRef - Utility of the BRAF p.V600E immunoperoxidase stain in FNA direct smears and cell block preparations from patients with thyroid carcinoma
Amber L. Smith, Michelle D. Williams, John Stewart, Wei‐Lien Wang, Savitri Krishnamurthy, Maria E. Cabanillas, Sinchita Roy‐Chowdhuri
Cancer Cytopathology.2018; 126(6): 406. CrossRef - Refinement of the criteria for ultrastructural peritubular capillary basement membrane multilayering in the diagnosis of chronic active/acute antibody-mediated rejection
Heounjeong Go, Sung Shin, Young Hoon Kim, Duck Jong Han, Yong Mee Cho
Transplant International.2017; 30(4): 398. CrossRef - Thyroid Fine-Needle Aspiration Cytology Practice in Korea
Yoon Jin Cha, Ju Yeon Pyo, SoonWon Hong, Jae Yeon Seok, Kyung-Ju Kim, Jee-Young Han, Jeong Mo Bae, Hyeong Ju Kwon, Yeejeong Kim, Kyueng-Whan Min, Soonae Oak, Sunhee Chang
Journal of Pathology and Translational Medicine.2017; 51(6): 521. CrossRef - Use of monoclonal antibodies to detect specific mutations in formalin-fixed, paraffin-embedded tissue sections
Zhenying Guo, Ricardo V. Lloyd
Human Pathology.2016; 53: 168. CrossRef
- Principles of Analytic Validation of Immunohistochemical Assays: Guideline Update
- Dysembryoplastic Neuroepithelial Tumors
- Yeon-Lim Suh
- J Pathol Transl Med. 2015;49(6):438-449. Published online October 23, 2015
- DOI: https://doi.org/10.4132/jptm.2015.10.05
- 16,469 View
- 294 Download
- 26 Web of Science
- 32 Crossref
-
 Abstract
Abstract
 PDF
PDF - Dysembryoplastic neuroepithelial tumor (DNT) is a benign glioneuronal neoplasm that most commonly occurs in children and young adults and may present with medically intractable, chronic seizures. Radiologically, this tumor is characterized by a cortical topography and lack of mass effect or perilesional edema. Partial complex seizures are the most common presentation. Three histologic subtypes of DNTs have been described. Histologically, the recognition of a unique, specific glioneuronal element in brain tumor samples from patients with medically intractable, chronic epilepsy serves as a diagnostic feature for complex or simple DNT types. However, nonspecific DNT has diagnostic difficulty because its histology is indistinguishable from conventional gliomas and because a specific glioneuronal element and/or multinodularity are absent. This review will focus on the clinical, radiographic, histopathological, and immunohistochemical features as well as the molecular genetics of all three variants of DNTs. The histological and cytological differential diagnoses for this lesion, especially the nonspecific variant, will be discussed.
-
Citations
Citations to this article as recorded by- A Case of Dysembryoplastic Neuroepithelial Tumor in an HIV-Positive Adult: Diagnostic Lessons for Clinicians
Mariana Lobo, Susana Viana, Andreia Sá Lima, Isabel Monteiro, Carolina M Cerqueira, Frederico Duarte, Luís M Ribeiro, Sara Camões
Cureus.2026;[Epub] CrossRef - An Imaging Review of Common Pediatric Brain Tumors
Joseph Yang, Brandon Collins, Matthew Beniuk, Alexandra Hodder, Dani Bahnam, Angela Pickles
Roentgen Ray Review.2025;[Epub] CrossRef - Ruptured intratumoral arteriovenous malformation in a patient with dysembryoplastic neuroepithelial tumor: A case report
Takashi Aoka, Masaaki Nishimoto, Hideki Ogiwara
Surgical Neurology International.2025; 16: 375. CrossRef - Pediatric Neuroglial Tumors: A Review of Ependymoma and Dysembryoplastic Neuroepithelial Tumor
Melissa Arfuso, Sandeepkumar Kuril, Harshal Shah, Derek Hanson
Pediatric Neurology.2024; 156: 139. CrossRef - From bedside to bench: New insights in epilepsy‐associated tumors based on recent classification updates and animal models on brain tumor networks
Silvia Cases‐Cunillera, Lea L. Friker, Philipp Müller, Albert J. Becker, Gerrit H. Gielen
Molecular Oncology.2024; 18(12): 2951. CrossRef - Imaging of pediatric glioneuronal and neuronal tumors
Vivek Pai, Suzanne Laughlin, Birgit Ertl-Wagner
Child's Nervous System.2024; 40(10): 3007. CrossRef - Dysembryoplastic Neuroepithelial Tumor: A Case Report of A Benign Intracranial Lesion Masquerading as Seizure Disorder
Garima S Agarwal, Anil K Agrawal, Daksh Singhal, Jayashree Bhawani
Cureus.2024;[Epub] CrossRef - Super T2-FLAIR mismatch sign: a prognostic imaging biomarker for non-enhancing astrocytoma, IDH-mutant
Iori Ozono, Shumpei Onishi, Ushio Yonezawa, Akira Taguchi, Novita Ikbar Khairunnisa, Vishwa Jeet Amatya, Fumiyuki Yamasaki, Yukio Takeshima, Nobutaka Horie
Journal of Neuro-Oncology.2024; 169(3): 571. CrossRef - Genotype-relevant neuroimaging features in low-grade epilepsy-associated tumors
Keiya Iijima, Hiroyuki Fujii, Fumio Suzuki, Kumiko Murayama, Yu-ichi Goto, Yuko Saito, Terunori Sano, Hiroyoshi Suzuki, Hajime Miyata, Yukio Kimura, Takuma Nakashima, Hiromichi Suzuki, Masaki Iwasaki, Noriko Sato
Frontiers in Neurology.2024;[Epub] CrossRef - Extra-temporal pediatric low-grade gliomas and epilepsy
José Hinojosa, Victoria Becerra, Santiago Candela-Cantó, Mariana Alamar, Diego Culebras, Carlos Valencia, Carlos Valera, Jordi Rumiá, Jordi Muchart, Javier Aparicio
Child's Nervous System.2024; 40(10): 3309. CrossRef - Atypical Presentation of Dysembryoplastic Neuroepithelial Tumor
Varis S. Khalilov, Aleksey N. Kislyakov, Natalia A. Medvedeva, Natalia S. Serova
Annals of Clinical and Experimental Neurology.2024; 18(3): 109. CrossRef - Unusual low-grade neuroepithelial tumour in a child
Leia Salongo, Ali Nael, Pournima Navalkele, John Ross Crawford
BMJ Case Reports.2024; 17(10): e262692. CrossRef - Glioneuronal and Neuronal Tumors: Who? When? Where? An Update Based on the 2021 World Health Organization Classification
A.S. Ayres, G.A. Bandeira, S.F. Ferraciolli, J.T. Takahashi, R.A. Moreno, L.F. de Souza Godoy, Y.R. Casal, L.G.C.A. de Lima, F.P. Frasseto, L.T. Lucato
Neurographics.2023; 13(1): 1. CrossRef - Biological functions of the Olig gene family in brain cancer and therapeutic targeting
Jenny I. Szu, Igor F. Tsigelny, Alexander Wojcinski, Santosh Kesari
Frontiers in Neuroscience.2023;[Epub] CrossRef - Aspekte der Bildgebung des Hippokampus
Isabela S. Alves, Artur M. N. Coutinho, Ana Vieira, Bruno P. Rocha, Ula L. Passos, Vinicius T. Gonçalves, Paulo D. S. Silva, Malia X. Zhan, Paula C. Pinho, Daniel S. Delgado, Marcos F. L. Docema, Hae W. Lee, Bruno A. Policeni, Claudia C. Leite, Maria G. M
Neuroradiologie Scan.2023; 13(03): 197. CrossRef - T2-FLAIR Mismatch Sign in Pediatric Low-Grade Glioma
M.W. Wagner, L. Nobre, K. Namdar, F. Khalvati, U. Tabori, C. Hawkins, B.B. Ertl-Wagner
American Journal of Neuroradiology.2023; 44(7): 841. CrossRef - Clinicopathological features of dysembryoplastic neuroepithelial tumor: a case series
Shabina Rahim, Nasir Ud Din, Jamshid Abdul-Ghafar, Qurratulain Chundriger, Poonum Khan, Zubair Ahmad
Journal of Medical Case Reports.2023;[Epub] CrossRef - Imaging Aspects of the Hippocampus
Isabela S. Alves, Artur M. N. Coutinho, Ana P. F. Vieira, Bruno P. Rocha, Ula L. Passos, Vinicius T. Gonçalves, Paulo D. S. Silva, Malia X. Zhan, Paula C. Pinho, Daniel S. Delgado, Marcos F. L. Docema, Hae W. Lee, Bruno A. Policeni, Claudia C. Leite, Mari
RadioGraphics.2022; 42(3): 822. CrossRef - Dysembryoplastic neuroepithelial tumors: A single-institutional series with special reference to glutamine synthetase expression
Chiara Caporalini, Mirko Scagnet, Selene Moscardi, Gioia Di Stefano, Gianna Baroni, Flavio Giordano, Federico Mussa, Carmen Barba, Iacopo Sardi, Lorenzo Genitori, Anna Maria Buccoliero
Annals of Diagnostic Pathology.2021; 54: 151774. CrossRef - Unusual case of occipital lobe dysembryoplastic neuroepithelial tumour with GNAi1-BRAF fusion
Jennifer H Yang, Denise M Malicki, Michael L Levy, John Ross Crawford
BMJ Case Reports.2021; 14(1): e241440. CrossRef - Malformations of Cortical Development, Cognitive Involvementand Epilepsy: A Single Institution Experience in 19 Young Patients
Valeria Venti, Maria Chiara Consentino, Pierluigi Smilari, Filippo Greco, Claudia Francesca Oliva, Agata Fiumara, Raffaele Falsaperla, Martino Ruggieri, Piero Pavone
Children.2021; 8(8): 637. CrossRef - A Case of Dysembryoplastic Neuroepithelial Tumor in an Adolescent Male
Marcel Yibirin, Diana De Oliveira, Isabella Suarez, Gabriela Lombardo, Carlos Perez
Cureus.2021;[Epub] CrossRef - Clinical and histopathological profile of dysembryoplastic neuroepithelial tumor
Pooja Gupta, Fouzia Siraj, Akanksha Malik, K. B. Shankar
Journal of Cancer Research and Therapeutics.2021; 17(4): 912. CrossRef - Neuroradiological and pathomorphological features of epilepsy associated brain tumors
V. S. Khalilov, A. A. Kholin, A. N. Kisyakov, N. A. Medvedeva, B. R. Bakaeva
Diagnostic radiology and radiotherapy.2021; 12(2): 7. CrossRef - Evaluación prequirúrgica mediante resonancia magnética funcional en pacientes con tumores neuroepiteliales disembrioplásicos: una serie de casos
Natalia García-Casares, Francisco Alfaro-Rubio, José Ramón Ramos-Rodríguez, Álvaro Ocaña-Ledesma, Bernarda Márquez-Márquez, Victoria E. Fernández-Sánchez, Guillermo Ibáñez-Botella, Miguel Ángel Arráez-Sánchez, Pedro J. Serrano-Castro
Neurocirugía.2020; 31(4): 158. CrossRef - Features of the neuroradiological picture of ganglioglioma on the example of 20 clinical cases
V.S. Khalilov, A.A. Kholin, Kh.Sh. Gazdieva, A.N. Kislyakov, N.N. Zavadenko
Zhurnal nevrologii i psikhiatrii im. S.S. Korsakova.2020; 120(11): 90. CrossRef - Malignant Glial Neuronal Tumors After West Nile Virus Neuroinvasive Disease: A Coincidence or a Clue?
Akanksha Sharma, Marie F. Grill, Scott Spritzer, A. Arturo Leis, Mark Anderson, Parminder Vig, Alyx B. Porter
The Neurohospitalist.2019; 9(3): 160. CrossRef - Particularities in differential diagnostics of epileptogenic brain malformations on the low-field MRI-device
V. S. Khalilov, A. A. Kholin, B. R. Bakaeva, M. Yu. Bobylova, Kh. Sh. Gazdieva
Russian Journal of Child Neurology.2019; 13(4): 23. CrossRef - Dysembryoplastic Neuroepithelial Tumors: What You Need to Know
Sabino Luzzi, Angela Elia, Mattia Del Maestro, Samer K. Elbabaa, Sergio Carnevale, Francesco Guerrini, Massimo Caulo, Patrizia Morbini, Renato Galzio
World Neurosurgery.2019; 127: 255. CrossRef - The miR‐139‐5p regulates proliferation of supratentorial paediatric low‐grade gliomas by targeting the PI3K/AKT/mTORC1 signalling
G. Catanzaro, Z. M. Besharat, E. Miele, M. Chiacchiarini, A. Po, A. Carai, C. E. Marras, M. Antonelli, M. Badiali, A. Raso, S. Mascelli, D. Schrimpf, D. Stichel, M. Tartaglia, D. Capper, A. von Deimling, F. Giangaspero, A. Mastronuzzi, F. Locatelli, E. Fe
Neuropathology and Applied Neurobiology.2018; 44(7): 687. CrossRef - Dysembryoplastic Neuroectodermal Tumor: An Analysis from the Surveillance, Epidemiology, and End Results Program, 2004–2013
Ha Son Nguyen, Ninh Doan, Michael Gelsomino, Saman Shabani
World Neurosurgery.2017; 103: 380. CrossRef - Common Histologically Benign Tumors of the Brain
Roy E. Strowd, Jaishri O. Blakeley
Continuum.2017; 23(6): 1680. CrossRef
- A Case of Dysembryoplastic Neuroepithelial Tumor in an HIV-Positive Adult: Diagnostic Lessons for Clinicians
- Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
- Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang, The Cardiopulmonary Pathology Study Group of Korean Society of Pathologists
- J Pathol Transl Med. 2015;49(6):481-488. Published online October 13, 2015
- DOI: https://doi.org/10.4132/jptm.2015.09.14
- 12,724 View
- 108 Download
- 22 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF - Background
Analysis of mutations in the epidermal growth factor receptor gene (EGFR) is important for predicting response to EGFR tyrosine kinase inhibitors. The overall rate of EGFR mutations in Korean patients is variable. To obtain comprehensive data on the status of EGFR mutations in Korean patients with lung cancer, the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists initiated a nationwide survey. Methods: We obtained 1,753 reports on EGFR mutations in patients with lung cancer from 15 hospitals between January and December 2009. We compared EGFR mutations with patient age, sex, history of smoking, histologic diagnosis, specimen type, procurement site, tumor cell dissection, and laboratory status. Results: The overall EGFR mutation rate was 34.3% in patients with non-small cell lung cancer (NSCLC) and 43.3% in patients with adenocarcinoma. EGFR mutation rate was significantly higher in women, never smokers, patients with adenocarcinoma, and patients who had undergone excisional biopsy. EGFR mutation rates did not differ with respect to patient age or procurement site among patients with NSCLC. Conclusions: EGFR mutation rates and statuses were similar to those in published data from other East Asian countries. -
Citations
Citations to this article as recorded by- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
Minh‐Thao Tu, Hoejun Kwon, Yoon‐Jung Choi, Hyunsoon Cho
International Journal of Cancer.2026; 158(4): 951. CrossRef - Assessing mutation-clinical correlations and treatment outcomes in Vietnamese non-small cell lung cancer patients
Hoang-Bac Nguyen, Bang-Suong Nguyen-Thi, Huu-Huy Nguyen, Minh-Khoi Le, Quoc-Trung Lam, Tuan-Anh Nguyen
Practical Laboratory Medicine.2025; 45: e00477. CrossRef - Gradual Increase in Lung Cancer Risk Due to Particulate Matter Exposure in Patients With Pulmonary Function Impairments: A Nationwide Korean Database Analysis
Jongin Lee, Joon Young Choi, Jeong Uk Lim
Journal of Korean Medical Science.2025;[Epub] CrossRef - Real-world treatment outcomes in South Korean patients with epidermal growth factor receptor-mutant non-small cell lung cancer
Young Saing Kim, Eun Young Lee, Hyun Woo Lee, Jin-Hyuk Choi, Tae-Hwan Kim, Yong Won Choi, Mi Sun Ahn
The Korean Journal of Internal Medicine.2025; 40(6): 1029. CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2023; 11: 853. CrossRef - Comprehensive analysis of NGS and ARMS-PCR for detecting EGFR mutations based on 4467 cases of NSCLC patients
Changlong He, Chengcheng Wei, Jun Wen, Shi Chen, Ling Chen, Yue Wu, Yifan Shen, Huili Bai, Yangli Zhang, Xueping Chen, Xiaosong Li
Journal of Cancer Research and Clinical Oncology.2022; 148(2): 321. CrossRef - Unique characteristics of G719X and S768I compound double mutations of epidermal growth factor receptor (EGFR) gene in lung cancer of coal-producing areas of East Yunnan in Southwestern China
Jun-Ling Wang, Yu-Dong Fu, Yan-Hong Gao, Xiu-Ping Li, Qian Xiong, Rui Li, Bo Hou, Ruo-Shan Huang, Jun-Feng Wang, Jian-Kun Zhang, Jia-Ling Lv, Chao Zhang, Hong-Wei Li
Genes and Environment.2022;[Epub] CrossRef - Continuous Vaginal Bleeding Induced By EGFR-TKI in Premenopausal Female Patients With EGFR Mutant NSCLC
Min Yu, Xiaoyu Li, Xueqian Wu, Weiya Wang, Yanying Li, Yan Zhang, Shuang Zhang, Yongsheng Wang
Frontiers in Oncology.2022;[Epub] CrossRef - The role of oncogenes and tumor suppressor genes in determining survival rates of lung cancer patients in the population of North Sumatra, Indonesia
Noni Novisari Soeroso, Fannie Rizki Ananda, Johan Samuel Sitanggang, Noverita Sprinse Vinolina
F1000Research.2022; 11: 853. CrossRef - Adverse Event Profiles of Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitors in Adenocarcinoma Lung Patients in North Sumatera Population
Moh. Ramadhani Soeroso, Noni Novisari Soeroso, Setia Putra Tarigan, Elisna Syahruddin
Open Access Macedonian Journal of Medical Sciences.2022; 10(T7): 134. CrossRef - Landscape of EGFR mutations in lung adenocarcinoma: a single institute experience with comparison of PANAMutyper testing and targeted next-generation sequencing
Jeonghyo Lee, Yeon Bi Han, Hyun Jung Kwon, Song Kook Lee, Hyojin Kim, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2022; 56(5): 249. CrossRef - Traditional Chinese Medicine Syndromes are Associated with Driver Gene Mutations and Clinical Characteristics in Patients with Lung Adenocarcinoma
Jili Yang, Haiyan Lu, Niancai Jing, Bo Wang, Huanyu Guo, Shoukun Sun, Yue Zhang, Chan-Yen Kuo
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Exosome-based detection of EGFR T790M in plasma and pleural fluid of prospectively enrolled non-small cell lung cancer patients after first-line tyrosine kinase inhibitor therapy
Yoonjung Kim, Saeam Shin, Kyung-A Lee
Cancer Cell International.2021;[Epub] CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Osimertinib in Patients with T790M-Positive Advanced Non-small Cell Lung Cancer: Korean Subgroup Analysis from Phase II Studies
Myung-Ju Ahn, Ji-Youn Han, Dong-Wan Kim, Byoung Chul Cho, Jin-Hyoung Kang, Sang-We Kim, James Chih-Hsin Yang, Tetsuya Mitsudomi, Jong Seok Lee
Cancer Research and Treatment.2020; 52(1): 284. CrossRef - Long non-coding RNA ATB promotes human non-small cell lung cancer proliferation and metastasis by suppressing miR-141-3p
Guojie Lu, Yaosen Zhang, Klaus Roemer
PLOS ONE.2020; 15(2): e0229118. CrossRef - Prognostic Role of S100A8 and S100A9 Protein Expressions in Non-small Cell Carcinoma of the Lung
Hyun Min Koh, Hyo Jung An, Gyung Hyuck Ko, Jeong Hee Lee, Jong Sil Lee, Dong Chul Kim, Jung Wook Yang, Min Hye Kim, Sung Hwan Kim, Kyung Nyeo Jeon, Gyeong-Won Lee, Se Min Jang, Dae Hyun Song
Journal of Pathology and Translational Medicine.2019; 53(1): 13. CrossRef - Epidermal growth factor receptor T790M mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yuhui Ma, Hutao Shi, Yaxi Du, Yunchao Huang
Scientific Reports.2018;[Epub] CrossRef - Does the efficacy of epidermal growth factor receptor (EGFR) tyrosine kinase inhibitor differ according to the type of EGFR mutation in non-small cell lung cancer?
Yong Won Choi, Jin-Hyuk Choi
The Korean Journal of Internal Medicine.2017; 32(3): 422. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - MET Exon 14 Skipping Mutations in Lung Adenocarcinoma: Clinicopathologic Implications and Prognostic Values
Geun Dong Lee, Seung Eun Lee, Doo-Yi Oh, Dan-bi Yu, Hae Min Jeong, Jooseok Kim, Sungyoul Hong, Hun Soon Jung, Ensel Oh, Ji-Young Song, Mi-Sook Lee, Mingi Kim, Kyungsoo Jung, Jhingook Kim, Young Kee Shin, Yoon-La Choi, Hyeong Ryul Kim
Journal of Thoracic Oncology.2017; 12(8): 1233. CrossRef - Epidermal growth factor receptor (EGFR) mutations in non-small cell lung cancer (NSCLC) of Yunnan in southwestern China
Yongchun Zhou, Yanlong Yang, Chenggang Yang, Yunlan Chen, Changshao Yang, Yaxi Du, Guangqiang Zhao, Yinjin Guo, Lianhua Ye, Yunchao Huang
Oncotarget.2017; 8(9): 15023. CrossRef - Detection of EGFR and KRAS Mutation by Pyrosequencing Analysis in Cytologic Samples of Non-Small Cell Lung Cancer
Seung Eun Lee, So-Young Lee, Hyung-Kyu Park, Seo-Young Oh, Hee-Joung Kim, Kye-Young Lee, Wan-Seop Kim
Journal of Korean Medical Science.2016; 31(8): 1224. CrossRef - MassARRAY, pyrosequencing, and PNA clamping for EGFR mutation detection in lung cancer tissue and cytological samples: a multicenter study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee-Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
Journal of Cancer Research and Clinical Oncology.2016; 142(10): 2209. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef
- Projected cancer burden attributable to population aging: Insight from a rapidly aging society
- Genomic Landscapes of Pancreatic Neoplasia
- Laura D. Wood, Ralph H. Hruban
- J Pathol Transl Med. 2015;49(1):13-22. Published online January 15, 2015
- DOI: https://doi.org/10.4132/jptm.2014.12.26
- 14,734 View
- 122 Download
- 19 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF - Pancreatic cancer is a deadly disease with a dismal prognosis. However, recent advances in sequencing and bioinformatic technology have led to the systematic characterization of the genomes of all major tumor types in the pancreas. This characterization has revealed the unique genomic landscape of each tumor type. This knowledge will pave the way for improved diagnostic and therapeutic approaches to pancreatic tumors that take advantage of the genetic alterations in these neoplasms.
-
Citations
Citations to this article as recorded by- c-Myc inhibition and p21 modulation contribute to unsymmetrical bisacridines-induced apoptosis and senescence in pancreatic cancer cells
Agnieszka Kurdyn, Monika Pawłowska, Ewa Paluszkiewicz, Mirosława Cichorek, Ewa Augustin
Pharmacological Reports.2025; 77(1): 182. CrossRef - Evaluation of the Value of Fine Needle Aspiration Cytology and Cell Morphology in Determining the Histogenesis of Pancreatic Lesions With Review of Literature, Overview and Cytological Experience of 25 Years: Original Research
Soudah Bisharah, Abbas Mahmoud
Health Science Reports.2025;[Epub] CrossRef - Research of immunotherapy in pancreatic cancer
Zetian Li, Y.-T. Yu, P.P. Piccaluga, S. Xie
BIO Web of Conferences.2024; 111: 02026. CrossRef - Pancreatoblastoma with a novel fusion gene ofIQSEC1‐RAF1
Hironori Goto, Yuhki Koga, Kenichi Kohashi, Hiroaki Ono, Junkichi Takemoto, Toshiharu Matsuura, Tatsuro Tajiri, Kenji Ihara, Yoshinao Oda, Shouichi Ohga
Pediatric Blood & Cancer.2023;[Epub] CrossRef - Imaging phenotype using 18F-fluorodeoxyglucose positron emission tomography–based radiomics and genetic alterations of pancreatic ductal adenocarcinoma
Chae Hong Lim, Young Seok Cho, Joon Young Choi, Kyung-Han Lee, Jong Kyun Lee, Ji Hye Min, Seung Hyup Hyun
European Journal of Nuclear Medicine and Molecular Imaging.2020; 47(9): 2113. CrossRef - NOSH-aspirin (NBS-1120) inhibits pancreatic cancer cell growth in a xenograft mouse model: Modulation of FoxM1, p53, NF-κB, iNOS, caspase-3 and ROS
Mitali Chattopadhyay, Ravinder Kodela, Gabriela Santiago, Thuy Tien C. Le, Niharika Nath, Khosrow Kashfi
Biochemical Pharmacology.2020; 176: 113857. CrossRef - Targeting Mutant KRAS in Pancreatic Cancer: Futile or Promising?
Friederike Inga Nollmann, Dietrich Alexander Ruess
Biomedicines.2020; 8(8): 281. CrossRef - Ancillary Techniques in Cytologic Specimens Obtained from Solid Lesions of the Pancreas: A Review
Jonas J. Heymann, Momin T. Siddiqui
Acta Cytologica.2020; 64(1-2): 103. CrossRef - DNA polymerase η mutational signatures are found in a variety of different types of cancer
Igor B. Rogozin, Alexander Goncearenco, Artem G. Lada, Subhajyoti De, Vyacheslav Yurchenko, German Nudelman, Anna R. Panchenko, David N. Cooper, Youri I. Pavlov
Cell Cycle.2018; 17(3): 348. CrossRef - Genetics of Pancreatic Neoplasms and Role of Screening
Venkata S. Katabathina, Omid Y. Rikhtehgar, Anil K. Dasyam, Rohan Manickam, Srinivasa R. Prasad
Magnetic Resonance Imaging Clinics of North America.2018; 26(3): 375. CrossRef - Team work and cytopathology molecular diagnosis of solid pancreatic lesions
Carlo Fabbri, Giulia Gibiino, Adele Fornelli, Vincenzo Cennamo, Daniela Grifoni, Michela Visani, Giorgia Acquaviva, Matteo Fassan, Sirio Fiorino, Silvia Giovanelli, Marco Bassi, Stefania Ghersi, Giovanni Tallini, Elio Jovine, Antonio Gasbarrini, Dario de
Digestive Endoscopy.2017; 29(6): 657. CrossRef - Mutational signatures and mutable motifs in cancer genomes
Igor B. Rogozin, Youri I. Pavlov, Alexander Goncearenco, Subhajyoti De, Artem G. Lada, Eugenia Poliakov, Anna R. Panchenko, David N. Cooper
Briefings in Bioinformatics.2017;[Epub] CrossRef - The evolving field of genomic biomarkers to characterize pancreatic cystic neoplasia by EUS-guided FNA
Ferga C. Gleeson, Michael J. Levy
Gastrointestinal Endoscopy.2016; 83(1): 149. CrossRef - MIA PaCa-2 and PANC-1 – pancreas ductal adenocarcinoma cell lines with neuroendocrine differentiation and somatostatin receptors
Rui Gradiz, Henriqueta C. Silva, Lina Carvalho, Maria Filomena Botelho, Anabela Mota-Pinto
Scientific Reports.2016;[Epub] CrossRef - p53 and p16/p19 Loss Promotes Different Pancreatic Tumor Types from PyMT-Expressing Progenitor Cells
Stephanie Azzopardi, Sharon Pang, David S. Klimstra, Yi-Chieh Nancy Du
Neoplasia.2016; 18(10): 610. CrossRef - MicroRNA-506 participates in pancreatic cancer pathogenesis by targeting PIM3
JUNDONG DU, XI ZHENG, SHOUWANG CAI, ZIMAN ZHU, JINGWANG TAN, BIN HU, ZHIQIANG HUANG, HUABO JIAO
Molecular Medicine Reports.2015; 12(4): 5121. CrossRef
- c-Myc inhibition and p21 modulation contribute to unsymmetrical bisacridines-induced apoptosis and senescence in pancreatic cancer cells
KRAS Mutation Detection in Non-small Cell Lung Cancer Using a Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping Method and Comparative Validation with Next-Generation Sequencing- Boram Lee, Boin Lee, Gangmin Han, Mi Jung Kwon, Joungho Han, Yoon-La Choi
- Korean J Pathol. 2014;48(2):100-107. Published online April 28, 2014
- DOI: https://doi.org/10.4132/KoreanJPathol.2014.48.2.100
- 14,080 View
- 104 Download
- 17 Crossref
-
 Abstract
Abstract
 PDF
PDF Background KRAS is one of commonly mutated genetic "drivers" in non-small cell lung cancers (NSCLCs). Recent studies indicate that patients withKRAS -mutated tumors do not benefit from adjuvant chemotherapy, so there is now a focus on targetingKRAS -mutated NSCLCs. A feasible mutation detection method is required in order to accurately test forKRAS status.Methods We compared direct Sanger sequencing and the peptide nucleic acid (PNA)-mediated polymerase chain reaction (PCR) clamping method in 134 NSCLCs and explored associations with clinicopathological factors. Next-generation sequencing (NGS) was used to validate the results of discordant cases. To increase the resolution of low-level somatic mutant molecules, PNA-mediated PCR clamping was used for mutant enrichment prior to NGS.
Results Twenty-one (15.7%) cases were found to have the
KRAS mutations using direct sequencing, with two additional cases by the PNA-mediated PCR clamping method. The frequencies ofKRAS mutant alleles were 2% and 4%, respectively, using conventional NGS, increasing up to 90% and 89%, using mutant-enriched NGS. TheKRAS mutation occurs more frequently in the tumors of smokers (p=.012) and in stage IV tumors (p=.032).Conclusions Direct sequencing can accurately detect mutations, but, it is not always possible to obtain a tumor sample with sufficient volume. The PNA-mediated PCR clamping can rapidly provide results with sufficient sensitivity.
-
Citations
Citations to this article as recorded by- KRAS mutated Non‐Small Lung Carcinoma: A Real World Context from the Indian subcontinent
Ullas Batra, Shrinidhi Nathany, Mansi Sharma, Amrith BP, Joslia T. Jose, Harkirat Singh, Sakshi Mattoo, Anurag Mehta
Cancer Medicine.2023; 12(3): 2869. CrossRef - Mechanism exploration and prognosis study of Astragali Radix-Spreading hedyotis herb for the treatment of lung adenocarcinoma based on bioinformatics approaches and molecular dynamics simulation
Junfeng Guo, Yuting Zhao, Xuanyu Wu, Ganggang Li, Yuwei Zhang, Yang Song, Quanyu Du
Frontiers in Chemistry.2023;[Epub] CrossRef - PEAC: An Ultrasensitive and Cost-Effective MRD Detection System in Non-small Cell Lung Cancer Using Plasma Specimen
Jianping Xu, Yue Pu, Rui Lin, Shanshan Xiao, Yingxue Fu, Tao Wang
Frontiers in Medicine.2022;[Epub] CrossRef - Potential applications of peptide nucleic acid in biomedical domain
Kshitij RB Singh, Parikipandla Sridevi, Ravindra Pratap Singh
Engineering Reports.2020;[Epub] CrossRef - A Highly Sensitive Next-Generation Sequencing-Based Genotyping Platform for EGFR Mutations in Plasma from Non-Small Cell Lung Cancer Patients
Jung-Young Shin, Jeong-Oh Kim, Mi-Ran Lee, Seo Ree Kim, Kyongmin Sarah Beck, Jin Hyoung Kang
Cancers.2020; 12(12): 3579. CrossRef - Association with PD-L1 Expression and Clinicopathological Features in 1000 Lung Cancers: A Large Single-Institution Study of Surgically Resected Lung Cancers with a High Prevalence of EGFR Mutation
Seung Eun Lee, Yu Jin Kim, Minjung Sung, Mi-Sook Lee, Joungho Han, Hong Kwan Kim, Yoon-La Choi
International Journal of Molecular Sciences.2019; 20(19): 4794. CrossRef - Peptide Nucleic Acid Clamping and Direct Sequencing in the Detection of Oncogenic Alterations in Lung Cancer: Systematic Review and Meta-Analysis
Jae-Uk Song, Jonghoo Lee
Yonsei Medical Journal.2018; 59(2): 211. CrossRef - Comparative analysis of Adam33 mutations in murine lung cancer cell lines by droplet digital PCR, real-time PCR and Insight Onco™ NGS
Soo-Jin Kim, Eunhee Kim, Kyung-Taek Rim
Molecular & Cellular Toxicology.2018; 14(2): 221. CrossRef - KRAS mutation analysis by next‐generation sequencing in endoscopic ultrasound‐guided sampling for solid liver masses
Hyun Jong Choi, Jong Ho Moon, Hee Kyung Kim, Yun Nah Lee, Tae Hoon Lee, Sang‐Woo Cha, Young Deok Cho, Sang‐Heum Park
Journal of Gastroenterology and Hepatology.2017; 32(1): 154. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Peptide nucleic acids: Advanced tools for biomedical applications
Anjali Gupta, Anuradha Mishra, Nidhi Puri
Journal of Biotechnology.2017; 259: 148. CrossRef - Application of Peptide Nucleic Acid-based Assays Toward Detection of Somatic Mosaicism
Christopher S Hong, Chunzhang Yang, Zhengping Zhuang
Molecular Therapy - Nucleic Acids.2016; 5: e314. CrossRef - Detecting Primary KIT Mutations in Presurgical Plasma of Patients with Gastrointestinal Stromal Tumor
Guhyun Kang, Byeong Seok Sohn, Jung-Soo Pyo, Jung Yeon Kim, Boram Lee, Kyoung-Mee Kim
Molecular Diagnosis & Therapy.2016; 20(4): 347. CrossRef - Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
Journal of Pathology and Translational Medicine.2016; 50(4): 258. CrossRef - Clinicopathologic characteristics of EGFR, KRAS, and ALK alterations in 6,595 lung cancers
Boram Lee, Taebum Lee, Se-Hoon Lee, Yoon-La Choi, Joungho Han
Oncotarget.2016; 7(17): 23874. CrossRef - Detection of KIT and PDGFRA mutations in the plasma of patients with gastrointestinal stromal tumor
Guhyun Kang, Byung Noe Bae, Byeong Seok Sohn, Jung-Soo Pyo, Gu Hyum Kang, Kyoung-Mee Kim
Targeted Oncology.2015; 10(4): 597. CrossRef - Low Frequency of KRAS Mutation in Pancreatic Ductal Adenocarcinomas in Korean Patients and Its Prognostic Value
Mi Jung Kwon, Jang Yong Jeon, Hye-Rim Park, Eun Sook Nam, Seong Jin Cho, Hyung Sik Shin, Ji Hyun Kwon, Joo Seop Kim, Boram Han, Dong Hoon Kim, Yoon-La Choi
Pancreas.2015; 44(3): 484. CrossRef
- KRAS mutated Non‐Small Lung Carcinoma: A Real World Context from the Indian subcontinent
- Comparison of Three
BRAF Mutation Tests in Formalin-Fixed Paraffin Embedded Clinical Samples - Soomin Ahn, Jeeyun Lee, Ji-Youn Sung, So Young Kang, Sang Yun Ha, Kee-Taek Jang, Yoon-La Choi, Jung-Sun Kim, Young Lyun Oh, Kyoung-Mee Kim
- Korean J Pathol. 2013;47(4):348-354. Published online August 26, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.4.348
- 9,846 View
- 60 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Background Recently,
BRAF inhibitors showed dramatic treatment outcomes inBRAF V600 mutant melanoma. Therefore, the accuracy ofBRAF mutation test is critical.Methods BRAF mutations were tested by dual-priming oligonucleotide-polymerase chain reaction (DPO-PCR), direct sequencing and subsequently retested with a real-time PCR assay, cobas 4800 V600 mutation test. In total, 64 tumors including 34 malignant melanomas and 16 papillary thyroid carcinomas were analyzed. DNA was extracted from formalin-fixed paraffin embedded tissue samples and the results of cobas test were directly compared with those of DPO-PCR and direct sequencing.Results BRAF mutations were found in 23 of 64 (35.9%) tumors. There was 9.4% discordance among 3 methods. Out of 6 discordant cases, 4 cases were melanomas; 3 cases wereBRAF V600E detected only by cobas test, but were not detected by DPO-PCR and direct sequencing. One melanoma patient withBRAF mutation detected only by cobas test has been on vemurafenib treatment for 6 months and showed a dramatic response to vemurafenib. DPO-PCR failed to detect V600K mutation in one case identified by both direct sequencing and cobas test.Conclusions In direct comparison of the currently available DPO-PCR, direct sequencing and real-time cobas test for
BRAF mutation, real-time PCR assay is the most sensitive method.-
Citations
Citations to this article as recorded by- Preoperative BRAFV600E mutation detection in thyroid carcinoma by immunocytochemistry
Kristine Zøylner Swan, Stine Horskær Madsen, Steen Joop Bonnema, Viveque Egsgaard Nielsen, Marie Louise Jespersen
APMIS.2022; 130(11): 627. CrossRef - Strategy to reduce unnecessary surgeries in thyroid nodules with cytology of Bethesda category III (AUS/FLUS): a retrospective analysis of 667 patients diagnosed by surgery
Yong Joon Suh, Yeon Ju Choi
Endocrine.2020; 69(3): 578. CrossRef - A new primer construction technique that effectively increases amplification of rare mutant templates in samples
Jr-Kai Huang, Ling Fan, Tao-Yeuan Wang, Pao-Shu Wu
BMC Biotechnology.2019;[Epub] CrossRef - BRAF and NRAS mutations and antitumor immunity in Korean malignant melanomas and their prognostic relevance: Gene set enrichment analysis and CIBERSORT analysis
Kyueng-Whan Min, Ji-Young Choe, Mi Jung Kwon, Hye Kyung Lee, Ho Suk Kang, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Yun Joong Kim, Nan Young Kim, Ho Young Kim
Pathology - Research and Practice.2019; 215(12): 152671. CrossRef - The association between dermoscopic features and BRAF mutational status in cutaneous melanoma: Significance of the blue-white veil
Miquel Armengot-Carbó, Eduardo Nagore, Zaida García-Casado, Rafael Botella-Estrada
Journal of the American Academy of Dermatology.2018; 78(5): 920. CrossRef - Comparison of Five Different Assays for the Detection of BRAF Mutations in Formalin-Fixed Paraffin Embedded Tissues of Patients with Metastatic Melanoma
Claire Franczak, Julia Salleron, Cindy Dubois, Pierre Filhine-Trésarrieu, Agnès Leroux, Jean-Louis Merlin, Alexandre Harlé
Molecular Diagnosis & Therapy.2017; 21(2): 209. CrossRef - Validation of an NGS mutation detection panel for melanoma
Anne Reiman, Hugh Kikuchi, Daniela Scocchia, Peter Smith, Yee Wah Tsang, David Snead, Ian A Cree
BMC Cancer.2017;[Epub] CrossRef - Transformation to Small Cell Lung Cancer of Pulmonary Adenocarcinoma: Clinicopathologic Analysis of Six Cases
Soomin Ahn, Soo Hyun Hwang, Joungho Han, Yoon-La Choi, Se-Hoon Lee, Jin Seok Ahn, Keunchil Park, Myung-Ju Ahn, Woong-Yang Park
Journal of Pathology and Translational Medicine.2016; 50(4): 258. CrossRef - Immunohistochemistry with the anti-BRAF V600E (VE1) antibody: impact of pre-analytical conditions and concordance with DNA sequencing in colorectal and papillary thyroid carcinoma
Katerina Dvorak, Birte Aggeler, John Palting, Penny McKelvie, Andrew Ruszkiewicz, Paul Waring
Pathology.2014; 46(6): 509. CrossRef
- Preoperative BRAFV600E mutation detection in thyroid carcinoma by immunocytochemistry
- Guideline Recommendations for
EGFR Mutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group - Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
- Korean J Pathol. 2013;47(2):100-106. Published online April 24, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.2.100
- 12,497 View
- 100 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF Mutations of the epidermal growth factor receptor (
EGFR ) are the strongest predictive factor for response to EGFR tyrosine kinase inhibitors (TKIs), such as gefitinib and erlotinib. EGFR TKIs are approved in Korea as a first-line treatment for lung cancer patients with mutatedEGFR . Rapid and accurateEGFR mutation testing is essential for patient selection and establishing targeted therapies with EGFR TKIs. Thus, a standard set of guideline recommendations forEGFR mutation testing suitable for the Korean medical community is necessary. In this article, we propose a set of guideline recommendations forEGFR mutation testing that was discussed and approved by the Cardiopulmonary Pathology Study Group of the Korean Society of Pathologists.-
Citations
Citations to this article as recorded by- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
Cheng-Yu Chang, Chia-Chun Tu, Shian-Ren Lin, Chih-Hao Fang, Po-Wei Tseng, Wan-En Liao, Li-Yun Huang, Shiu-Lan Wang, Wan-Yu Lai, Yee Chao, Yen-Ling Chiu, Jan-Mou Lee
Diseases.2025; 13(12): 406. CrossRef - Favorable Conditions for the Detection of EGFR T790M Mutation Using Plasma Sample in Patients with Non-Small-Cell Lung Cancer
Insu Kim, Hee Yun Seol, Soo Han Kim, Mi-Hyun Kim, Min Ki Lee, Jung Seop Eom
Cancers.2023; 15(5): 1445. CrossRef - Novel Targets, Novel Treatments: The Changing Landscape of Non-Small Cell Lung Cancer
Dorine de Jong, Jeeban P. Das, Hong Ma, Jacienta Pailey Valiplackal, Conor Prendergast, Tina Roa, Brian Braumuller, Aileen Deng, Laurent Dercle, Randy Yeh, Mary M. Salvatore, Kathleen M. Capaccione
Cancers.2023; 15(10): 2855. CrossRef - Coordination games in cancer
Péter Bayer, Robert A. Gatenby, Patricia H. McDonald, Derek R. Duckett, Kateřina Staňková, Joel S. Brown, Jun Tanimoto
PLOS ONE.2022; 17(1): e0261578. CrossRef - Molecular biomarker testing for non–small cell lung cancer: consensus statement of the Korean Cardiopulmonary Pathology Study Group
Sunhee Chang, Hyo Sup Shim, Tae Jung Kim, Yoon-La Choi, Wan Seop Kim, Dong Hoon Shin, Lucia Kim, Heae Surng Park, Geon Kook Lee, Chang Hun Lee
Journal of Pathology and Translational Medicine.2021; 55(3): 181. CrossRef - Primary HHV-8 (-) Effusion-Based Non-Germinal Center B Cell Diffuse Large B Cell Lymphoma Successfully Treated with Standard Anthracycline-Based Chemoimmunotherapy
Justin J Kuhlman, Muhamad Alhaj Moustafa, Liuyan Jiang, Han W Tun
Journal of Blood Medicine.2021; Volume 12: 833. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Strategic management of transthoracic needle aspirates for histological subtyping and EGFR testing in patients with peripheral lung cancer: An institutional experience
Choonhee Son, Eun‐Ju Kang, Mee Sook Roh
Diagnostic Cytopathology.2015; 43(7): 532. CrossRef - Ultrasonography-Guided Core Biopsy of Supraclavicular Lymph Nodes for Diagnosis of Metastasis and Identification of Epidermal Growth Factor Receptor (EGFR) Mutation in Advanced Lung Cancer
Jooae Choe, Mi Young Kim, Jung Hwan Baek, Chang-Min Choi, Hwa Jung Kim
Medicine.2015; 94(29): e1209. CrossRef - Reliable EGFR mutation testing in ultrasound-guided supraclavicular lymph node fine-needle aspirates: a cohort study with diagnostic performance analysis
Amir Awwad, Sandeep Tiwari, Vishakha Sovani, David R Baldwin, Maruti Kumaran
BMJ Open Respiratory Research.2015; 2(1): e000075. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Molecular Pathology of Lung Cancer: Current Status and Future Directions
Mee Sook Roh
Tuberculosis and Respiratory Diseases.2014; 77(2): 49. CrossRef
- Establishment of a Flow Cytometry Protocol for Binarily Detecting Circulating Tumor Cells with EGFR Mutation
- Comparison of Direct Sequencing, PNA Clamping-Real Time Polymerase Chain Reaction, and Pyrosequencing Methods for the Detection of
EGFR Mutations in Non-small Cell Lung Carcinoma and the Correlation with Clinical Responses to EGFR Tyrosin - Hyun Ju Lee, Xianhua Xu, Hyojin Kim, Yan Jin, Pingli Sun, Ji Eun Kim, Jin-Haeng Chung
- Korean J Pathol. 2013;47(1):52-60. Published online February 25, 2013
- DOI: https://doi.org/10.4132/KoreanJPathol.2013.47.1.52
- 12,669 View
- 93 Download
- 31 Crossref
-
 Abstract
Abstract
 PDF
PDF Background The aims of this study were to evaluate the abilities of direct sequencing (DS), peptide nucleic acid (PNA) clamping, and pyrosequencing methods to detect epidermal growth factor receptor (
EGFR ) mutations in formalin-fixed paraffin-embedded (FFPE) non-small cell lung carcinoma (NSCLC) samples and to correlateEGFR mutational status as determined by each method with the clinical response toEGFR tyrosine kinase inhibitors (TKIs).Methods Sixty-one NSCLC patients treated with EGFR TKIs were identified to investigate somatic mutations in the
EGFR gene (exons 18-21).Results Mutations in the
EGFR gene were detected in 38 of the 61 patients (62%) by DS, 35 (57%) by PNA clamping and 37 (61%) by pyrosequencing. A total of 44 mutations (72%) were found by at least one of the three methods, and the concordances among the results were relatively high (82-85%; kappa coefficient, 0.713 to 0.736). There were 15 discordant cases (25%) among the three different methods.Conclusions All three
EGFR mutation tests had good concordance rates (over 82%) for FFPE samples. These results suggest that if the DNA quality and enrichment of tumor cells are assured, then DS, PNA clamping, and pyrosequencing are appropriate methods for the detection ofEGFR mutations.-
Citations
Citations to this article as recorded by- Recent Trends of Lung Cancer in Korea
Jae Guk Lee, Ho Cheol Kim, Chang-Min Choi
Tuberculosis and Respiratory Diseases.2021; 84(2): 89. CrossRef - Predictive value of KRAS mutation and excision repair cross-complementing 1 (ERCC1) protein overexpression in patients with colorectal cancer administered FOLFOX regimen
Sun Min Park, Sung Bong Choi, Yoon Suk Lee, In Kyu Lee
Asian Journal of Surgery.2021; 44(5): 715. CrossRef - Recent advances in diagnostic technologies in lung cancer
Hye Jung Park, Sang Hoon Lee, Yoon Soo Chang
The Korean Journal of Internal Medicine.2020; 35(2): 257. CrossRef - Afatinib is effective in the treatment of lung adenocarcinoma with uncommon EGFR p.L747P and p.L747S mutations
Sheng-Kai Liang, Jen-Chung Ko, James Chih-Hsin Yang, Jin-Yuan Shih
Lung Cancer.2019; 133: 103. CrossRef - Biomarker Testing for Patients With Advanced Non–Small Cell Lung Cancer: Real-World Issues and Tough Choices
Nathan A. Pennell, Maria E. Arcila, David R. Gandara, Howard West
American Society of Clinical Oncology Educational Book.2019; (39): 531. CrossRef - Evaluation of EGFR mutations in NSCLC with highly sensitive droplet digital PCR assays
Xi‑Wen Jiang, Wei Liu, Xiao‑Ya Zhu, Xiao‑Xie Xu
Molecular Medicine Reports.2019;[Epub] CrossRef - Peptide Nucleic Acid Clamping and Direct Sequencing in the Detection of Oncogenic Alterations in Lung Cancer: Systematic Review and Meta-Analysis
Jae-Uk Song, Jonghoo Lee
Yonsei Medical Journal.2018; 59(2): 211. CrossRef - Distribution of KRAS, DDR2, and TP53 gene mutations in lung cancer: An analysis of Iranian patients
Zahra Fathi, Seyed Ali Javad Mousavi, Raheleh Roudi, Farideh Ghazi, Sumitra Deb
PLOS ONE.2018; 13(7): e0200633. CrossRef - EGFR T790M mutation testing within the osimertinib AURA Phase I study
Simon Dearden, Helen Brown, Suzanne Jenkins, Kenneth S. Thress, Mireille Cantarini, Rebecca Cole, Malcolm Ranson, Pasi A. Jänne
Lung Cancer.2017; 109: 9. CrossRef - Molecular Testing of Lung Cancers
Hyo Sup Shim, Yoon-La Choi, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Mee Sook Roh, Tae-Jung Kim, Seung Yeon Ha, Jin-Haeng Chung, Se Jin Jang, Geon Kook Lee
Journal of Pathology and Translational Medicine.2017; 51(3): 242. CrossRef - Mutations of the Epidermal Growth Factor Receptor Gene in Triple-Negative Breast Cancer
Aeri Kim, Min Hye Jang, Soo Jung Lee, Young Kyung Bae
Journal of Breast Cancer.2017; 20(2): 150. CrossRef - Double primary lung adenocarcinoma diagnosed by epidermal growth factor receptor mutation status
Oh Jung Kwon, Min Hyeok Lee, Sung Ju Kang, Seul Gi Kim, In Beom Jeong, Ji Yun Jeong, Eun Jung Cha, Do Yeun Cho, Young Jin Kim, Ji Woong Son
Yeungnam University Journal of Medicine.2017; 34(2): 270. CrossRef - Generation of lung cancer cell lines harboring EGFR T790M mutation by CRISPR/Cas9-mediated genome editing
Mi-Young Park, Min Hee Jung, Eun Young Eo, Seokjoong Kim, Sang Hoon Lee, Yeon Joo Lee, Jong Sun Park, Young Jae Cho, Jin Haeng Chung, Cheol Hyeon Kim, Ho Il Yoon, Jae Ho Lee, Choon-Taek Lee
Oncotarget.2017; 8(22): 36331. CrossRef - Comparison of EGFR mutation detection between the tissue and cytology using direct sequencing, pyrosequencing and peptide nucleic acid clamping in lung adenocarcinoma: Korean multicentre study
Kyueng-Whan Min, Wan-Seop Kim, Se Jin Jang, Yoo Duk Choi, Sunhee Chang, Soon Hee Jung, Lucia Kim, Mee Sook Roh, Choong Sik Lee, Jung Weon Shim, Mi Jin Kim, Geon Kook Lee
QJM.2016; 109(3): 167. CrossRef - Epidermal Growth Factor Receptor Mutation and Anaplastic Lymphoma Kinase Gene Fusion: Detection in Malignant Pleural Effusion by RNA or PNA Analysis
Yi-Lin Chen, Chung-Ta Lee, Cheng-Chan Lu, Shu-Ching Yang, Wan-Li Chen, Yang-Cheng Lee, Chung-Hsien Yang, Shu-Ling Peng, Wu-Chou Su, Nan-Haw Chow, Chung-Liang Ho, Javier S Castresana
PLOS ONE.2016; 11(6): e0158125. CrossRef - IDH Mutation Analysis in Ewing Sarcoma Family Tumors
Ki Yong Na, Byeong-Joo Noh, Ji-Youn Sung, Youn Wha Kim, Eduardo Santini Araujo, Yong-Koo Park
Journal of Pathology and Translational Medicine.2015; 49(3): 257. CrossRef - Immunohistochemical demonstration of alteration of β-catenin during tumor metastasis by different mechanisms according to histology in lung cancer
XIANHUA XU, JI EUN KIM, PING-LI SUN, SEOL BONG YOO, HYOJIN KIM, YAN JIN, JIN-HAENG CHUNG
Experimental and Therapeutic Medicine.2015; 9(2): 311. CrossRef - Detection of EGFR-TK Domain–activating Mutations in NSCLC With Generic PCR-based Methods
Rajendra B. Shahi, Sylvia De Brakeleer, Jacques De Grève, Caroline Geers, Peter In’t Veld, Erik Teugels
Applied Immunohistochemistry & Molecular Morphology.2015; 23(3): 163. CrossRef - Frequent aerogenous spread with decreased E-cadherin expression of ROS1- rearranged lung cancer predicts poor disease-free survival
Yan Jin, Ping-Li Sun, Soo Young Park, Hyojin Kim, Eunhyang Park, Gilhyang Kim, Sukki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Lung Cancer.2015; 89(3): 343. CrossRef - Membranous Insulin-like Growth Factor-1 Receptor (IGF1R) Expression Is Predictive of Poor Prognosis in Patients with Epidermal Growth Factor Receptor (EGFR)-Mutant Lung Adenocarcinoma
Eunhyang Park, Soo Young Park, Hyojin Kim, Ping-Li Sun, Yan Jin, Suk Ki Cho, Kwhanmien Kim, Choon-Taek Lee, Jin-Haeng Chung
Journal of Pathology and Translational Medicine.2015; 49(5): 382. CrossRef - Peptide Nucleic Acid Clamping Versus Direct Sequencing for the Detection of EGFR Gene Mutation in Patients with Non-small Cell Lung Cancer
Seong-Hoon Yoon, Yoo-Duk Choi, In-Jae Oh, Kyu-Sik Kim, Hayoung Choi, Jinsun Chang, Hong-Joon Shin, Cheol-Kyu Park, Young-Chul Kim
Cancer Research and Treatment.2015; 47(4): 661. CrossRef - Analysis of Mutations in Epidermal Growth Factor Receptor Gene in Korean Patients with Non-small Cell Lung Cancer: Summary of a Nationwide Survey
Sang Hwa Lee, Wan Seop Kim, Yoo Duk Choi, Jeong Wook Seo, Joung Ho Han, Mi Jin Kim, Lucia Kim, Geon Kook Lee, Chang Hun Lee, Mee Hye Oh, Gou Young Kim, Sun Hee Sung, Kyo Young Lee, Sun Hee Chang, Mee Sook Rho, Han Kyeom Kim, Soon Hee Jung, Se Jin Jang
Journal of Pathology and Translational Medicine.2015; 49(6): 481. CrossRef - Novel EGFR mutation-specific antibodies for lung adenocarcinoma: Highly specific but not sensitive detection of an E746_A750 deletion in exon 19 and an L858R mutation in exon 21 by immunohistochemistry
An Na Seo, Tae-In Park, Yan Jin, Ping-Li Sun, Hyojin Kim, Hyun Chang, Jin-Haeng Chung
Lung Cancer.2014; 83(3): 316. CrossRef - Simultaneous diagnostic platform of genotyping EGFR, KRAS, and ALK in 510 Korean patients with non‐small‐cell lung cancer highlights significantly higher ALK rearrangement rate in advanced stage
Tae‐Jung Kim, Chan Kwon Park, Chang Dong Yeo, Kihoon Park, Chin Kook Rhee, Jusang Kim, Seung Joon Kim, Sang Haak Lee, Kyo‐Young Lee, Hyoung‐Kyu Yoon
Journal of Surgical Oncology.2014; 110(3): 245. CrossRef - Epidermal growth factor receptor mutations and anaplastic lymphoma kinase rearrangements in lung cancer with nodular ground-glass opacity
Sung-Jun Ko, Yeon Joo Lee, Jong Sun Park, Young-Jae Cho, Ho Il Yoon, Jin-Haeng Chung, Tae Jung Kim, Kyung Won Lee, Kwhanmien Kim, Sanghoon Jheon, Hyojin Kim, Jae Ho Lee, Choon-Taek Lee
BMC Cancer.2014;[Epub] CrossRef - Cytoplasmic YAP Expression is Associated with Prolonged Survival in Patients with Lung Adenocarcinomas and Epidermal Growth Factor Receptor Tyrosine Kinase Inhibitor Treatment
Ping-Li Sun, Ji Eun Kim, Seol Bong Yoo, Hyojin Kim, Yan Jin, Sanghoon Jheon, Kwhanmien Kim, Choon Taek Lee, Jin-Haeng Chung
Annals of Surgical Oncology.2014; 21(S4): 610. CrossRef - Sensitive methods for detection of the S768R substitution in exon 18 of the DDR2 gene in patients with central nervous system metastases of non-small cell lung cancer
Marcin Nicoś, Tomasz Powrózek, Paweł Krawczyk, Bożena Jarosz, Beata Pająk, Marek Sawicki, Krzysztof Kucharczyk, Tomasz Trojanowski, Janusz Milanowski
Medical Oncology.2014;[Epub] CrossRef - Clinicopathologic and prognostic significance of c-MYC copy number gain in lung adenocarcinomas
A N Seo, J M Yang, H Kim, S Jheon, K Kim, C T Lee, Y Jin, S Yun, J-H Chung, J H Paik
British Journal of Cancer.2014; 110(11): 2688. CrossRef - KRASMutation Detection in Non-small Cell Lung Cancer Using a Peptide Nucleic Acid-Mediated Polymerase Chain Reaction Clamping Method and Comparative Validation with Next-Generation Sequencing
Boram Lee, Boin Lee, Gangmin Han, Mi Jung Kwon, Joungho Han, Yoon-La Choi
Korean Journal of Pathology.2014; 48(2): 100. CrossRef - Guideline Recommendations forEGFRMutation Testing in Lung Cancer: Proposal of the Korean Cardiopulmonary Pathology Study Group
Hyo Sup Shim, Jin-Haeng Chung, Lucia Kim, Sunhee Chang, Wan-Seop Kim, Geon Kook Lee, Soon-Hee Jung, Se Jin Jang
Korean Journal of Pathology.2013; 47(2): 100. CrossRef - Immunohistochemical Classification of Primary and Secondary Glioblastomas
Kyu Sang Lee, Gheeyoung Choe, Kyung Han Nam, An Na Seo, Sumi Yun, Kyung Ju Kim, Hwa Jin Cho, Sung Hye Park
Korean Journal of Pathology.2013; 47(6): 541. CrossRef
- Recent Trends of Lung Cancer in Korea
- Frequency of
BRAF Mutation and Clinical Relevance for Primary Melanomas - Hyoun Wook Lee, Ki Hoon Song, Jin Woo Hong, Su Young Jeon, Dong Yeob Ko, Ki Ho Kim, Hyuk Chan Kwon, Suee Lee, Sung Hyun Kim, Dae Cheol Kim
- Korean J Pathol. 2012;46(3):246-252. Published online June 22, 2012
- DOI: https://doi.org/10.4132/KoreanJPathol.2012.46.3.246
- 10,094 View
- 59 Download
- 14 Crossref
-
 Abstract
Abstract
 PDF
PDF Background This study was conducted to clarify the frequency of the
BRAF mutation in primary melanomas and its correlation with clinicopathologic parameters.Methods We analyzed the frequency of
BRAF mutation in patients with primary cutaneous melanoma (n=58) or non-cutaneous one (n=27) by performing dual priming oligonucleotide-based multiplex real-time polymerase chain reaction to isolate and to purify the DNA from the formalin-fixed and paraffin-embedded tumors.Results The
BRAF mutation was found in 17.2% (10/58) of patients with primary cutaneous melanoma and 11.1% (3/27) of those with non-cutaneous melanoma. The frequency ofBRAF mutation was not correlated with any clinicopathologic parameters with the exception of the patient age. The frequency of theBRAF mutation was significantly higher in patients younger than 60 years as compared with those older than 60 years (p=0.005).Conclusions Compared with previous reports, our results showed that the frequency of the
BRAF mutation was relatively lower in patients with primary cutaneous melanoma. Besides, our results also showed that the frequency of theBRAF mutation had an inverse correlation with the age. Further studies are warranted to exclude methodological bias, to elucidate the difference in the frequency of theBRAF mutation from the previous reports from a Caucasian population and to provide an improved understanding of the molecular pathogenesis of malignant melanoma.-
Citations
Citations to this article as recorded by- Prevalence and clinicopathological correlation of BRAF V600E mutations in ameloblastoma: A PCR study from a tertiary centre in South India
Logeswari Jayamani, Kavitha Bottu, Leena Dennis Joseph, Ganthimathy Sekhar
Journal of Stomatology Oral and Maxillofacial Surgery.2026; 127(1): 102575. CrossRef - . Prevalence and prognostic mutation V600E in the BRAF gene in stage I cutaneous melanoma
K. S. Titov, M. V. Sorokina, D. N. Grekov, S. S. Lebedev
Bone and soft tissue sarcomas, tumors of the skin.2024; 16(3): 61. CrossRef - Clinicopathological Features of Patients with Malignant Melanoma Diagnosis and Prognostic and Predictive Importance of Neuthrophil-Lymphocyte Ratio
Yasemin SAĞDIÇ KARATEKE, Lütfiye DEMİR, Murat DİNÇER, Bülent YILDIZ
OSMANGAZİ JOURNAL OF MEDICINE.2023;[Epub] CrossRef - Genetic characteristics and response to systemic therapies of acral lentiginous melanoma at a tertiary care center—a retrospective review
Taylor Jamerson, Vito W. Rebecca, Crystal Aguh
Journal of the National Medical Association.2022; 114(1): 7. CrossRef - Comparative study of cutaneous melanoma and its associated issues between people of African decent and Caucasians
Ehiaghe L. Anaba
Dermatologic Therapy.2021;[Epub] CrossRef -
BRAF, KIT, and NRAS Mutations of Acral Melanoma in White Patients
Emi Dika, Giulia Veronesi, Annalisa Altimari, Mattia Riefolo, Giulia Maria Ravaioli, Bianca Maria Piraccini, Martina Lambertini, Elena Campione, Elisa Gruppioni, Michelangelo Fiorentino, Barbara Melotti, Manuela Ferracin, Annalisa Patrizi
American Journal of Clinical Pathology.2020; 153(5): 664. CrossRef - Clinical Application of Next-Generation Sequencing–Based Panel toBRAFWild-Type Advanced Melanoma Identifies Key Oncogenic Alterations and Therapeutic Strategies
Changhee Park, Miso Kim, Min Jung Kim, Hyeongmin Kim, Chan-Young Ock, Bhumsuk Keam, Tae Min Kim, Dong-Wan Kim, Jong-Il Kim, Dae Seog Heo
Molecular Cancer Therapeutics.2020; 19(3): 937. CrossRef - BRAF and NRAS mutations and antitumor immunity in Korean malignant melanomas and their prognostic relevance: Gene set enrichment analysis and CIBERSORT analysis
Kyueng-Whan Min, Ji-Young Choe, Mi Jung Kwon, Hye Kyung Lee, Ho Suk Kang, Eun Sook Nam, Seong Jin Cho, Hye-Rim Park, Soo Kee Min, Jinwon Seo, Yun Joong Kim, Nan Young Kim, Ho Young Kim
Pathology - Research and Practice.2019; 215(12): 152671. CrossRef - Acral melanoma: correlating the clinical presentation to the mutational status
Giulia M. Ravaioli, Emi Dika, Martina Lambertini, Marco A. Chessa, Pier Alessandro Fanti, Annalisa Patrizi
Giornale Italiano di Dermatologia e Venereologia.2019;[Epub] CrossRef - Sunrise in melanoma management: Time to focus on melanoma burden in Asia
John Wen‐Cheng Chang, Jun Guo, Chia‐Yen Hung, Si Lu, Sang Joon Shin, Richard Quek, Anthony Ying, Gwo Fuang Ho, Huu Sau Nguyen, Boman Dhabhar, Virote Sriuranpong, Maria Luisa Tiambeng, Nugroho Prayogo, Naoya Yamazaki
Asia-Pacific Journal of Clinical Oncology.2017; 13(6): 423. CrossRef - Detection ofBRAF,NRAS,KIT,GNAQ,GNA11andMAP2K1/2mutations in Russian melanoma patients using LNA PCR clamp and biochip analysis
Marina Emelyanova, Lilit Ghukasyan, Ivan Abramov, Oxana Ryabaya, Evgenia Stepanova, Anna Kudryavtseva, Asiya Sadritdinova, Cholpon Dzhumakova, Tatiana Belysheva, Sergey Surzhikov, Lyudmila Lyubchenko, Alexander Zasedatelev, Tatiana Nasedkina
Oncotarget.2017; 8(32): 52304. CrossRef - Metaanalysis of BRAF mutations and clinicopathologic characteristics in primary melanoma
Soo Young Kim, Soo Nyung Kim, Hyung Jin Hahn, Yang Won Lee, Yong Beom Choe, Kyu Joong Ahn
Journal of the American Academy of Dermatology.2015; 72(6): 1036. CrossRef - Diagnostic Effectiveness of PCR-based Tests DetectingBRAFMutation for Treating Malignant Melanoma: A Systematic Review
Hae-Won Shin, Ryeo-Jin Ko, Min Lee, Hee-Young Bang, Kye-Chul Kwon, Jong-Woo Park, Sun-Hoe Koo
Laboratory Medicine Online.2014; 4(4): 203. CrossRef - KIT, NRAS, BRAF and PTEN mutations in a sample of Swedish patients with acral lentiginous melanoma
Abdlsattar Zebary, Katarina Omholt, Ismini Vassilaki, Veronica Höiom, Diana Lindén, Lisa Viberg, Lena Kanter-Lewensohn, Carolina Hertzman Johansson, Johan Hansson
Journal of Dermatological Science.2013; 72(3): 284. CrossRef
- Prevalence and clinicopathological correlation of BRAF V600E mutations in ameloblastoma: A PCR study from a tertiary centre in South India
- Mutation and Expression of DNA2 Gene in Gastric and Colorectal Carcinomas.
- Sung Hak Lee, Yoo Ri Kim, Nam Jin Yoo, Sug Hyung Lee
- Korean J Pathol. 2010;44(4):354-359.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.4.354
- 4,801 View
- 35 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Deregulation of DNA repair and replication are involved in cancer development. DNA2 is a nuclease/helicase that plays roles in DNA repair and replication. The aim of this study was to explore DNA2 mutation and DNA2 protein expression in gastric cancers (GCs) and colorectal cancers (CRCs).
METHODS
We analyzed two mononucleotide repeats in DNA2 in 27 GCs with high microsatellite instability (MSI-H), 34 GCs with stable MSI (MSS), 29 CRCs with MSI-H and 35 CRCs with MSS by single-strand conformation polymorphism. We also analyzed DNA2 expression in GCs and CRCs either with MSI-H or MSS.
RESULTS
We found DNA2 mutations in two GCs (7.1%) and two CRCs with MSI-H (6.9%), but not in cancers with MSS. The mutations consisted of three cases of a c.2593delT and one of a c.2592_2593delTT, which would result in premature stopping of amino acid synthesis (p.Ser865Hisfsx6 and p.Ser865Thrfsx20, respectively). DNA2 expression was observed in 16 (80%) of the GCs and 15 (75%) of the CRCs with MSI-H, but all of the cancers with DNA2 frameshift mutations were weak or negative for DNA2.
CONCLUSIONS
Our data indicate that DNA2 mutation and loss of DNA2 expression occur in GCs and CRCs, and suggest that these alterations may contribute to cancer pathogenesis by deregulating DNA repair and replication. -
Citations
Citations to this article as recorded by- Multiple roles of DNA2 nuclease/helicase in DNA metabolism, genome stability and human diseases
Li Zheng, Yuan Meng, Judith L Campbell, Binghui Shen
Nucleic Acids Research.2020; 48(1): 16. CrossRef - Integration of multiple networks and pathways identifies cancer driver genes in pan-cancer analysis
Claudia Cava, Gloria Bertoli, Antonio Colaprico, Catharina Olsen, Gianluca Bontempi, Isabella Castiglioni
BMC Genomics.2018;[Epub] CrossRef - Replication intermediates that escape Dna2 activity are processed by Holliday junction resolvase Yen1
Gizem Ölmezer, Maryna Levikova, Dominique Klein, Benoît Falquet, Gabriele Alessandro Fontana, Petr Cejka, Ulrich Rass
Nature Communications.2016;[Epub] CrossRef
- Multiple roles of DNA2 nuclease/helicase in DNA metabolism, genome stability and human diseases
- Galectin-3 Expression and BRAF Mutation in Cases of Cytologically Suspicious Papillary Thyroid Carcinoma.
- Dokyung Kim, Hyunki Kim, Jinyoung Kwak, Minju Kim, Hyung Jae Jung, Ja Seung Koo, Beom Jin Lim, Chankwon Jung, SoonWon Hong
- Korean J Pathol. 2010;44(2):191-198.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.191
- 4,195 View
- 33 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Fine needle aspiration, which is known as the most accurate and cost-effective method for diagnosis of thyroid nodule, still may result in indeterminate cases that are pauci-cellular and show minor nuclear atypia, but most cases are associated with suspicion of papillary thyroid carcinoma (PTC). A B-type Raf kinase (BRAF) mutation was found in about half of PTCs and galectin-3 was expressed by malignant tumors, helping us to differentiate malignancies from benign lesions.
METHODS
Cases studied included histologically 44 confirmed PTC cases and 18 benign cases previously diagnosed as suspicious of PTC using cytologic examination. Cases were analyzed for galectin-3 expression by immunohistochemical staining and BRAF mutation by polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) with a new restriction enzyme.
RESULTS
All 44 cases of PTC and 8 of 18 benign controls expressed galectin-3. BRAF mutations were found in only 9 of the 44 PTC cases. Assessment of galectin-3 expression demonstrated high sensitivity but low specificity. Evaluation of BRAF mutation revealed high specificity and low sensitivity.
CONCLUSIONS
This study suggests that the combined application of these two methods for PTC of suspicious cytology is complementary.
- An Approach to Diagnosing Gastrointestinal Stromal Tumors Using Immunohistochemistry of c-kit and PDGFRA with Molecular Analysis.
- Jeong Shik Kim, Jae Hoon Kim, Hyun Jin Oh, In Soo Suh, Jong Gwang Kim, Byung Wook Kang, Wan Sik Yu, Ho Young Chung, Han Ik Bae
- Korean J Pathol. 2010;44(2):173-178.
- DOI: https://doi.org/10.4132/KoreanJPathol.2010.44.2.173
- 4,023 View
- 45 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Gastrointestinal stromal tumors (GIST) are the most common mesenchymal tumors in the gastrointestinal tract. Recently, many methods for the diagnosis of GIST have been developed including molecular diagnosis.
METHODS
We selected 90 cases of GIST that had presented at Kyungpook National University Hospital between 1998 and 2007. Tissue microarrays were made using core areas of tumor tissues. Immunohistochemical staining for c-kit, protein kinase C-theta, and platelet-derived growth factor receptor alpha (PDGFRA) was done. Direct sequencing of hot spot exonal areas for c-kit and PDGFRA were done using extracted DNAs of all 90 paraffin block tissues.
RESULTS
Among the 90 cases, 83.3% (75/90) were c-kit positive, 16.6% (15/90) were c-kit negative, 93.3% (84/90) were PDGFRA positive, and 6.6% (6/90) cases were PDGFRA negative. Fifteen cases of c-kit negative GIST included 1 case of PDGFRA negative and 5 cases of PDGFRA negative GIST were ckit positive. The one case in which both c-kit and PDGFRA were negative, showed a c-kit mutation in exon 11.
CONCLUSIONS
Combined immunohistochemical staining of c-kit, discovered on GIST 1 (DOG1) and PDGFRA is helpful for the diagnosis of GIST. When all staining tests are negative for immunoreactivity, c-kit mutation analysis for exon 11, 9 should be done. Genotyping of kit and PDGFRA do not need to be examined initially, if it is only for the diagnosis of GIST.
- KIT/PDGFRA Expression and Mutation in Testicular Seminoma and Ovarian Dysgerminoma.
- Song Yi Choi, Kwang Sun Suh, Yong Beom Kim, Hyun Jeong Lee, Eun Sun Kim, Mee Ja Park
- Korean J Pathol. 2009;43(6):528-534.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.6.528
- 4,694 View
- 22 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
KIT and PDGFRA are tyrosine kinase receptors. Stem cell factor/KIT-mediated signaling plays a role in normal spermatogenesis, and the alteration of KIT is important in the pathogenesis of seminomas/dysgerminomas (SD). METHODS: To determine the role of expression and mutation of the KIT and PDGFRA genes, we analyzed 16 seminoma cases, 4 spermatocytic seminoma (SS) cases and 8 dysgerminoma cases for KIT and PDGFRA expression and mutation of KIT (exons 9, 11, 13, and 17) and PDGFRA (exons 12 and 18) using PCR-SSCP methods. RESULTS: KIT was immunohistochemically positive in all 24 SD cases, and one of four (25%) SS cases. PDGFRA was immunohistochemically evident in 16 of the 24 (66.6%) SD cases, and two of the four (50%) SS cases. KIT expression was significantly reduced in SS compared with seminoma (p=0.0035). Four cases (14.3%) displayed mutation in KIT exon 17 or PDGFRA exon 12. Distant metastasis was present in three cases (10.7%), one of which had a nonsense mutation in KIT. CONCLUSIONS: These results indicate that KIT is expressed in the majority of SD cases, but not in most SS cases. However, there was no significant correlation between the clinicopathologic features and mutation or expression of KIT and PDGFRA. -
Citations
Citations to this article as recorded by- Expression of DOG1, PDGFRA, and p16 in Gastrointestinal Stromal Tumors
Sung Hee Jung, Kwang Sun Suh, Dae Young Kang, Dong Wook Kang, Young-Beum Kim, Eun-Sun Kim
Gut and Liver.2011; 5(2): 171. CrossRef
- Expression of DOG1, PDGFRA, and p16 in Gastrointestinal Stromal Tumors
- Intron 1 Polymorphism, Mutation and the Protein Expression of Epidermal Growth Factor Receptor in Relation to the Gefitinib Sensitivity of Korean Lung Cancer Patients.
- Mi Jin Kim, Kyeong Cheol Shin, Kwan Ho Lee
- Korean J Pathol. 2009;43(6):509-516.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.6.509
- 3,576 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Epidermal growth factor receptor (EGFR) intron 1 polymorphism in non-small cell lung cancer (NSCLC) has been found to have therapeutic implications for the patients treated with EGFR tyrosine kinase inhibitors. However, its clinical significance as related to gefitinib responsiveness is still controversial. We examined CA repeat polymorphism in intron 1 of the EGFR gene and its relation with the EGFR gene mutation in NSCLC patients who were treated with gefitinib. METHODS: Sixty seven patients who were treated with gefitinib were analyzed for intron 1 polymorphism in the EGFR gene, the EGFR mutations and the EGFR protein expression. Two hundred twenty seven samples of NSCLC were analyzed for EGFR mutations. RESULTS: CA repeat was low in 27 patients (40.3%) and high in 40 (59.7%) patients. The response rate for gefitinib therapy was higher in the patient population with a low number of CA repeats in the EGFR gene (p=0.047) and in the patients with the mutated type of EGFR (p=0.048), though these two factors were not related. Thirty four patients (15.0%) harbored EGFR mutations. CONCLUSIONS: This study suggests that the intron 1 CA repeat polymorphism of the EGFR gene may serve as a predictor of the clinical outcome of NSCLC patients treated with gefitinib, and this without regard for EGFR mutation. Our data further supports the importance of EGFR mutations with regard to a distinct clinical profile and the prognostic implications for NSCLC patients.
- Gastrointestinal Stromal Tumor of the Colon Mimicking Inflammatory Fibroid Polyp with a Novel 63 bp c-kit Deletion Mutation: A Case Report.
- In Gu Do, Cheol Keun Park, Sung Hyun Yoon, John Goldblum, Kyoung Mee Kim
- Korean J Pathol. 2009;43(4):374-377.
- DOI: https://doi.org/10.4132/KoreanJPathol.2009.43.4.374
- 3,581 View
- 26 Download
-
 Abstract
Abstract
 PDF
PDF - Colonic gastrointestinal stromal tumors (GISTs) are rare and behave aggressively compared to GISTs in other parts of the gastrointestinal tract. Therefore, accurate diagnosis of GISTs and their distinction from other mesenchymal tumors is important for proper patient management and follow-up. Herein, we present an unusual case of a colonic GIST mimicking an inflammatory fibroid polyp with a novel 63 bp deletion mutation in exon 11 of the c-kit gene, which has not previously been reported. The tumor consisted of loosely arranged spindle cells and many inflammatory cells scattered throughout the tumor. Immunohistochemically, the tumor cells were focally and weakly positive for c-kit and diffusely positive for CD34, but were negative for PKC-theta, SMA, S-100 protein, ALK-1, and desmin. Our case re-emphasizes the broad morphologic spectrum of GISTs.
- Ethnic Differences of the p53 Genetic Alteration in Cutaneous Malignant Melanoma.
- Won Sang Park, Eun Young Na, Sang Kyu Lee, Sug Hyung Lee, Su Young Kim, Seok Jin Kang, Kye Yong Song, Suk Woo Nam, Nam Jin Yoo, Jung Young Lee
- Korean J Pathol. 2001;35(2):158-164.
- 1,954 View
- 12 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
There are significant differences in the clincopathologic pattern including the incidence, favor site, and histopathologic type between cutaneous malignant melanomas arising from whites, asians and blacks. These differences might suggest that there is a racial difference in the molecular tumorigenesis mechanism of malignant melanoma.
METHODS
To determine the ethnic differences in tumorigenesis of malignant melanoma, we performed loss of heterozygosity (LOH) and sequencing analyses of the p53 gene in cutaneous malignant melanomas arising from 22 white American, 30 Korean and 15 black African patients.
RESULTS
The frequency of LOH of the p53 gene is only 12.5% in white American patients, but the frequency is significantly higher in Korean (42.1%) and black African (61.5%) patients. We also detected 17 mutations (nonsense: 1, missense: 16) of the p53 gene in the cutaneous malignant melanomas of Koreans and black Africans, but none in those of white Americans: among the 16 missense mutations, 10 mutations were C:G to T:A transitional mutations. Of these, we also detected one GG (CC) to AA (TT) tandem mutation at the pyrimidine sequence.
CONCLUSION
These results strongly suggest that there might be a racial difference in molecular carcinogenesis mechanisms among the cutaneous malignant melanomas occurring in white American, Korean and black African patients. But the role of the p53 genetic alteration in the genesis of melanomas in Korean and black African patients is subject to further evaluation.
- Human Papillomavirus Type 16, 18, and 33 Infection in Adenocarcinoma of the Uterine Cervix: Analysis of the p53 Gene Mutation and the Clincopathologic Correlation.
- Kwang Sun Suh, Seong Jun Cho, Sun Young Na, Heung Tae Noh, Sang Ryun Nam
- Korean J Pathol. 2004;38(5):295-300.
- 2,103 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Current evidence implicates specific types of the human papillomavirus (HPV) are involved in the development of cervical cancer. In HPV-negative cervical carcinomas, p53 mutation is thought to be a mechanism of oncogenesis. The purpose of this study was to evaluate the prevalence of p53 mutations in cervical adenocarcinomas and to investigate their correlation with HPV status and clinicopathologic parameters.
METHODS
A series of 38 primary cervical adenocarcinomas was analyzed for both HPV infection and p53 mutations. The HPV 16, 18, and 33 status was investigated by PCR amplification. The point mutations of the p53 gene were detected by the PCR-SSCP technique.
RESULTS
The prevalence of HPV 16, 18, or 33 infection was 73.7% (28/38). HPV 16 was present in 12 cases, HPV 18 was present in 15 cases, and HPV 33 was positive in one case. There was only one case that was positive for 18 as well as a p53 mutation in exon 6.
CONCLUSIONS
Our results indicate that HPV 18 infection was more common in cervical adenocarcinomas than HPV 16 infection. Mutant p53 was rarely found in cervical adenocarcinomas regardless of the type of HPV infection. There was no correlation between HPV infection and clinical stage or pathologic type of tumor.
- Comparative Analysis of Serum Mannose-Binding Lectin in Normal Population and Patients with Different Types of Cancer.
- Bum Joon Kim, Young Sik Kim, Eun Mee Han, Eung Seok Lee, Nam Hee Won, Geung Hwan Ahn, Dale Lee, Bom Woo Yeom
- Korean J Pathol. 2004;38(5):306-310.
- 2,048 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Mannose-binding lectin (MBL) is a serum protein of innate immunity. Its genetic mutations lead to deficiency of serum MBL and recurrent pyogenic infection in childhood. However, little is known about the frequency of its gene mutations or serum levels in Korean population and patients with cancers.
METHODS
We studied the mutational genotypes of MBL exon 1 codon 52, 54, and 57 or serum MBL levels from 102 normal adults and 228 cases of breast, stomach, colon, uterine cervical, and lung cancers by allele-specific PCR and enzyme-linked immunosorbent assay.
RESULTS
MBL gene mutations were found in 32 of 102 normal adults (31.4%), and were restricted only to exon 1 codon 54 showing homozygous (n=5, 4.9%) or heterozygous mutations (n=27, 26.5%). Mean and median serum MBL in the patients with cancers were increased (2,647+/-1,742 and 2,915 ng/mL, mean+/-S.D. and median) than those of normal adults (1,906+/-1,359 and 1,758 ng/mL). Serum MBL level was significantly increased in the patients with stomach, uterine cervical, colon, and lung cancers.
CONCLUSION
Our results indicate that the frequency and pattern of MBL gene mutations and its serum level is very similar among northeastern Asian populations. In addition, MBL might be involved in an immunologic response against common cancers, although further studies are needed.
- DNA Sequencing of p53 Gene Mutation in Colorectal Carcinomas.
- Young Ran Shim, Joon Hyuk Choi, Won Hee Choi
- Korean J Pathol. 1999;33(6):422-433.
- 2,280 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - Mutations in the p53 gene occur during the development of colorectal carcinomas, and play an important role in the conversion of adenoma into carcinoma. To detect the p53 gene mutation and its pattern of expression in colorectal carcinomas, polymerase chain reaction for exons 5, 6, 7, and 8, recombinant gene cloning, and automated DNA sequencing were performed with 30 fresh colorectal carcinomas. Each tissue was also analyzed by immunohistochemical staining for p53 protein. p53 protein was detected in 25 of 30 (83.3%) colorectal carcinomas by immunohistochemical study. p53 mutation was detected in 4 of 30 (13.3%) colorectal carcinomas. The distribution of these mutations among these exons investigated was as follows: Three mutations in exon 5 (66.7%) and 1 mutation in exon 7 (33.3%). One case with mutation in exon 5 had mutations at three different codons. Mutations in exon 5 were found at codon 153 (GGG to AGG: Gly to Arg), 170 (TGC to GGC: Cys to Gly), 186 (CTA to TTA: silent mutation), 158 (GCG to ACG: Ala to Thr), and 176 (ACG to ATG: Thr to Met). Mutation in exon 7 was found at codon 248 (AGG to AGA: silent mutation). Four of them were missense mutations. Two of 6 mutations were silent mutations. Five transition mutations and 1 transversion mutation were also detected. All cases with mutations by automated DNA sequencing showed positive p53 protein immunohistochemical stainining. In conclusion, p53 gene mutation was detected in 4 of 30 (13.3%) colorectal carcinomas, located in codon 153, 158, 170, 176, and 186 of exon 5 and codon 248 of exon 7. Further studies are needed to evaluate the significance of the codon 153 mutation which was not recognized in other studies on colorectal carcinomas.
- Epidermal Growth Factor Receptor Expression of Non-small Cell Carcinoma and Its Relationship with Genomic Mutation.
- Sang hee Seok, Mi Jin Kim
- Korean J Pathol. 2008;42(2):94-99.
- 2,196 View
- 27 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
It has recently been clarified that epidermal growth factor receptor (EGFR), which is a receptor tyrosine kinase of the erbB family, is abnormally activated in non-small cell lung carcinomas (NSCLC) and this fact is being utilized for creating targeted therapy. In this study, we aimed to identify the frequency of the EGFR expression and gene mutation in NSCLC, and to determine the correlation between them.
METHODS
Immunohistochemical staining for EGFR, C-erbB-2, cytokeratin 7, p53 and thyroid transcription factor-1, and EGFR mutation analysis were performed using paraffin-embedded archival tissue from 228 cases of NSCLC; this included 112 squamous cell carcinomas and 116 adenocarcinomas.
RESULTS
An EGFR expression and gene mutation occurred in 112 casees (53.5%) and 52 cases (22.8%), respectively. EGRF mutation was more frequent in the adenocarcinomas than in the squamous cell carcinomas, in non-smokers than in smokers, and in females than in males. EGFR mutation was significantly associated with an EGFR protein expression, and especially in adenocarcinomas.
CONCLUSION
The EGFR expression in NSCLC was associated with EGFR mutation, and especially in adenocarcinomas. More studies are needed to prove the clinical significance of the EGFR expression for creating targeted therapy to treat NSCLC.
- PTEN and p53 Mutations in Endometrial Carcinomas.
- Jae Sung Choi, Kwang Sun Suh, Heung Tae Noh, Yun Ee Rhee, Sun Young Na, Hye Kyung Lee
- Korean J Pathol. 2005;39(1):1-8.
- 2,694 View
- 35 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Endometrial carcinomas are pathogenetically classified into two major types; endometrioid carcinoma (EC) and serous carcinoma (SC). The most frequently altered gene in EC is the PTEN tumor suppressor gene (TSG). SC is usually associated with mutations in the p53 TSG.
METHODS
To further determine the role of PTEN and p53 mutation in endometrial carcinogenesis, the analysis of 33 endometrial carcinomas, including 28 ECs and 5 SCs, for loss of heterozygosity (LOH) on 10q23 and for mutation in all 9 coding exons of PTEN and the 5-8 exons of p53, using SSCP-PCR methods was carried out.
RESULTS
LOH was detected in at least one marker in 12 (54.5%) of 22 ECs, but in only one (20.0%) of 5 SCs. Somatic PTEN mutations were detected in 10 (35.7%) of 28 ECs. PTEN was altered in 67.9% of ECs and in 20.0% of SCs, including those with 10q23 LOH. No PTEN mutations were found among the SCs. Somatic p53 mutations were detected in 2 (7.1%) of 28 ECs and 3 (60.0%) of 5 SCs.
CONCLUSIONS
PTEN gene alterations contribute to the pathogenesis of an endometrioid subtype of endometrial carcinoma, but not to the serous type. In contrast, p53 plays an important role in the pathogenesis of SCs.
- Mutational Analysis of Proapoptotic bcl-2 Family genes in Colon Carcinomas.
- Young Hwa Soung, Jong Woo Lee, Su Young Kim, Suk Woo Nam, Won Sang Park, Jung Young Lee, Nam Jin Yoo, Sug Hyung Lee
- Korean J Pathol. 2005;39(3):168-171.
- 2,035 View
- 29 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Several lines of evidence have indicated that the deregulation of apoptosis is involved in the mechanisms of cancer development, and somatic mutations of the apoptosisrelated genes have been reported in human cancers. Members of the bcl-2 family proteins regulate the intrinsic apoptosis pathway mainly in the mitochondria. The aim of this study was to explore whether the somatic mutation of the proapoptotic bcl-2 family genes, one of the mechanisms that prolong the survival of cancer cells, occurred in colorectal carcinomas.
METHODS
In the current study, to detect the somatic mutations in the DNA sequences encoding the bcl-2 homology 3 (BH3) domain of the human bak, bid, bik, bim, PUMA, bcl-rambo, bcl-G, and bmf genes in 98 colon adenocarcinomas, we used polymerase chain reaction (PCR), single strand conformation polymorphism (SSCP), and DNA sequencing.
RESULTS
The SSCP analysis detected no evidence of somatic mutations of the genes in the coding regions of the BH3 domain in the cancers.
CONCLUSIONS
The data presented here indicate that the proapoptotic bcl-2 family genes, bak, bid, bik, bim, PUMA, bcl-rambo, bcl-G and bmf may not be somatically mutated in human colorectal carcinomas, and suggest that the colorectal cancers may not utilize mutational events of these proapoptotic bcl-2 family genes in the mechanisms for evading apoptosis.
- Mutational and Loss of Heterozygosity Analysis of the p53 and PTEN Tumor Suppressor Genes in Breast Carcinoma.
- Kwang Sun Suh, Young Ho Lee, Sun Young Na, Moon Il Park, Hun Soo Kim, Saeng Keum Lee
- Korean J Pathol. 2005;39(5):313-319.
- 3,633 View
- 36 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Although the genetic determinants of most sporadic breast cancers remain unknown, the understanding of the molecular and genetic events that contribute to breast carcinogenesis has been significantly advanced. We investigated the clinicopathologic significance of allelic imbalance or mutation of both p53 and PTEN tumor suppressor genes in sporadic breast carcinomas.
METHODS
Genomic DNA from 62 breast carcinoma cases was extracted from paraffin blocks, and PCR was performed to determine loss of heterozygosity (LOH) for DNA markers around the p53 and PTEN genes and to amplify exons 5, 6, 7, and 8 of p53 and all 9 coding axons of PTEN.
RESULTS
Somatic p53 mutations were detected in 6 (9.7%) of the 62 cases. LOH for DNA markers surrounding p53 was observed in 18 (29.0%) of the 62 cases. LOH for DNA markers surrounding PTEN was detected in 29 (46.8%) of the 62 cases. Only one case (1.6%) showed somatic PTEN mutations. Tumors with LOH on 17p or p53 mutation were large in size and negative for ER, had a high Ki-67 index, and exhibited p53 immunoreactivity (p<0.05). Tumors with LOH on 10q23 were associated with c-erbB-2 positivity (p=0.018).
CONCLUSIONS
Our results indicate that LOH at 17p and/or p53 mutation is significantly associated with the aggressive pathologic parameters of breast cancer.

 E-submission
E-submission











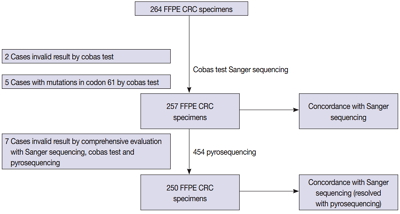
 First
First Prev
Prev



